Non-Extraction Orthodontic Camouflage for Severe Class II Malocclusion Post-TMJ Gap Arthroplasty: A Case Report
Abstract
1. Introduction
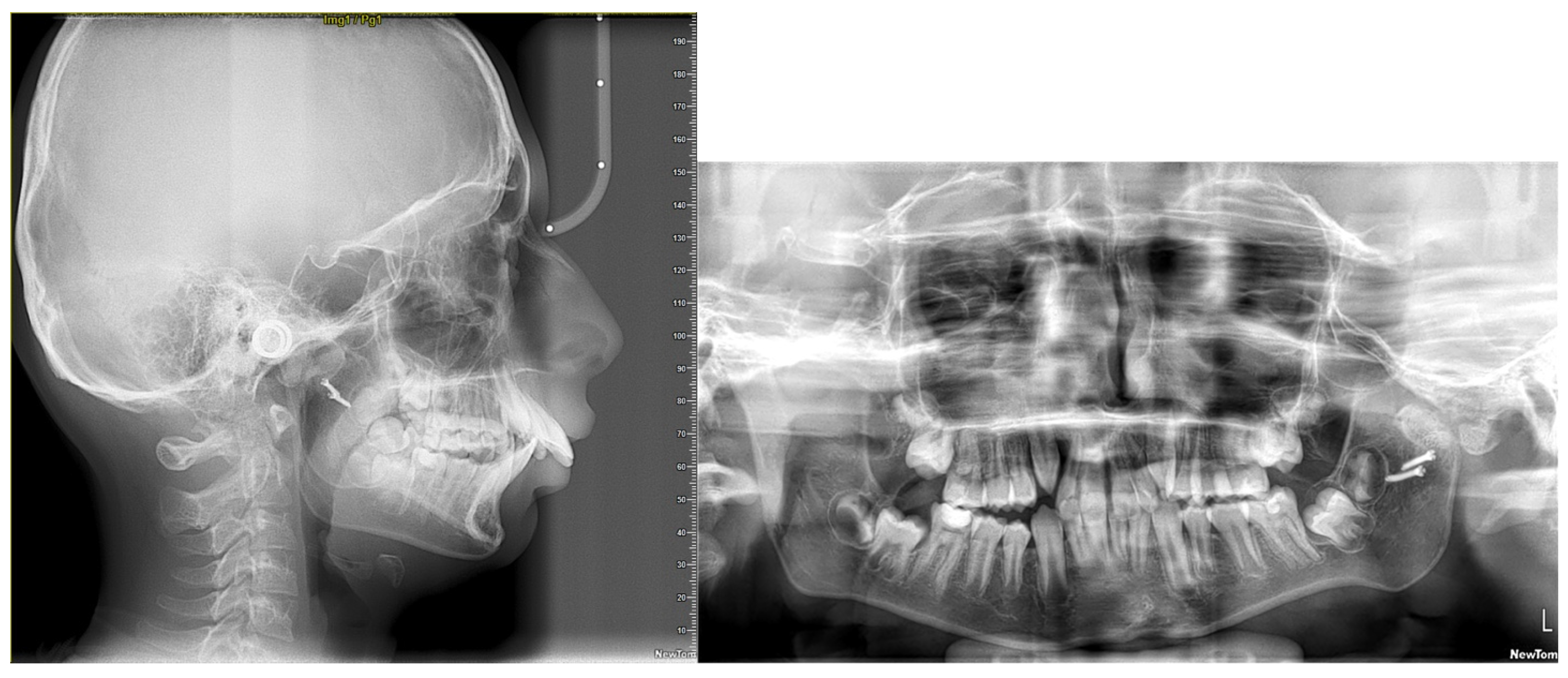
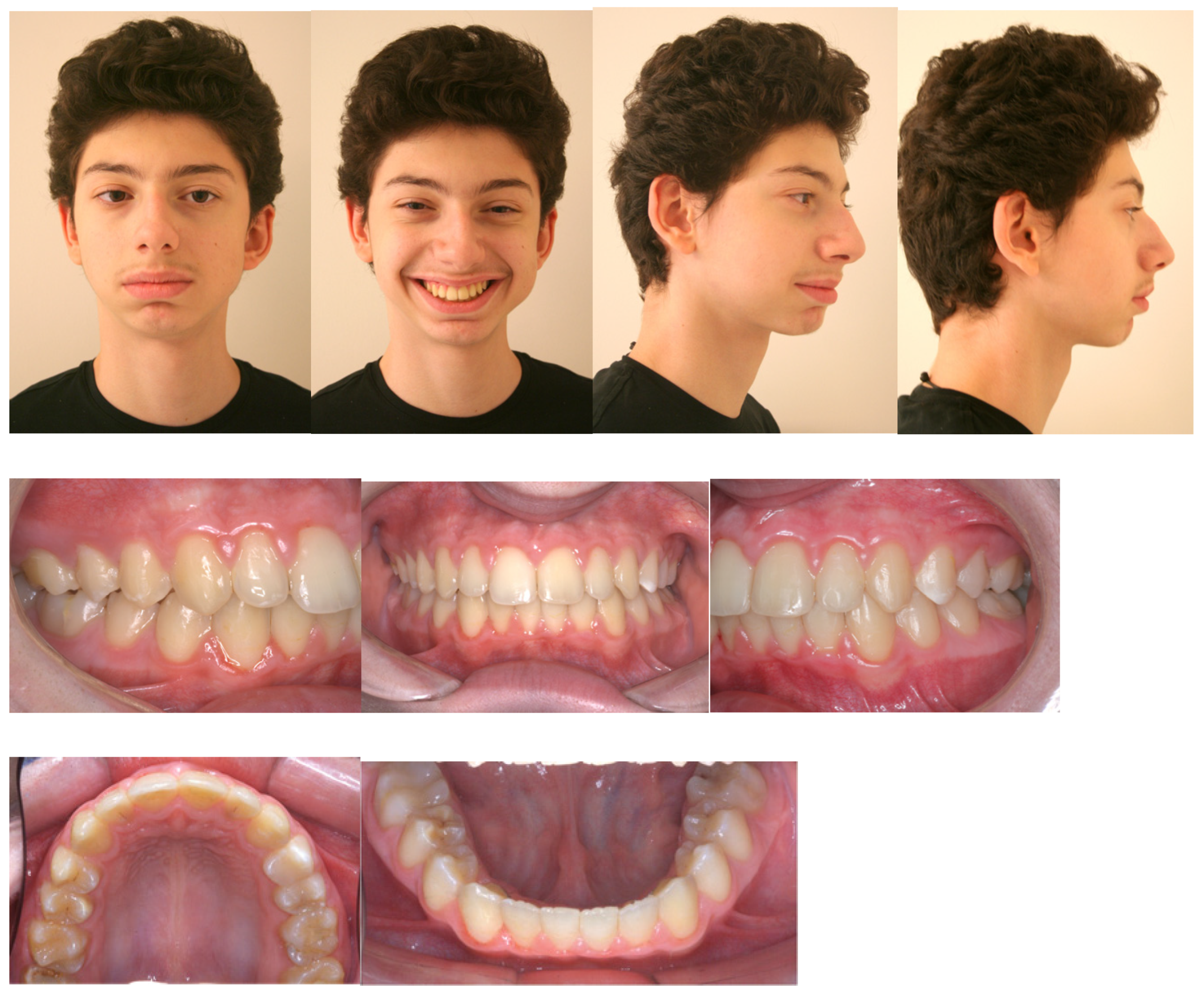
2. Diagnosis and Etiology
3. Treatment Objectives
- Improve the skeletal Class II by addressing the retrognathic mandible.
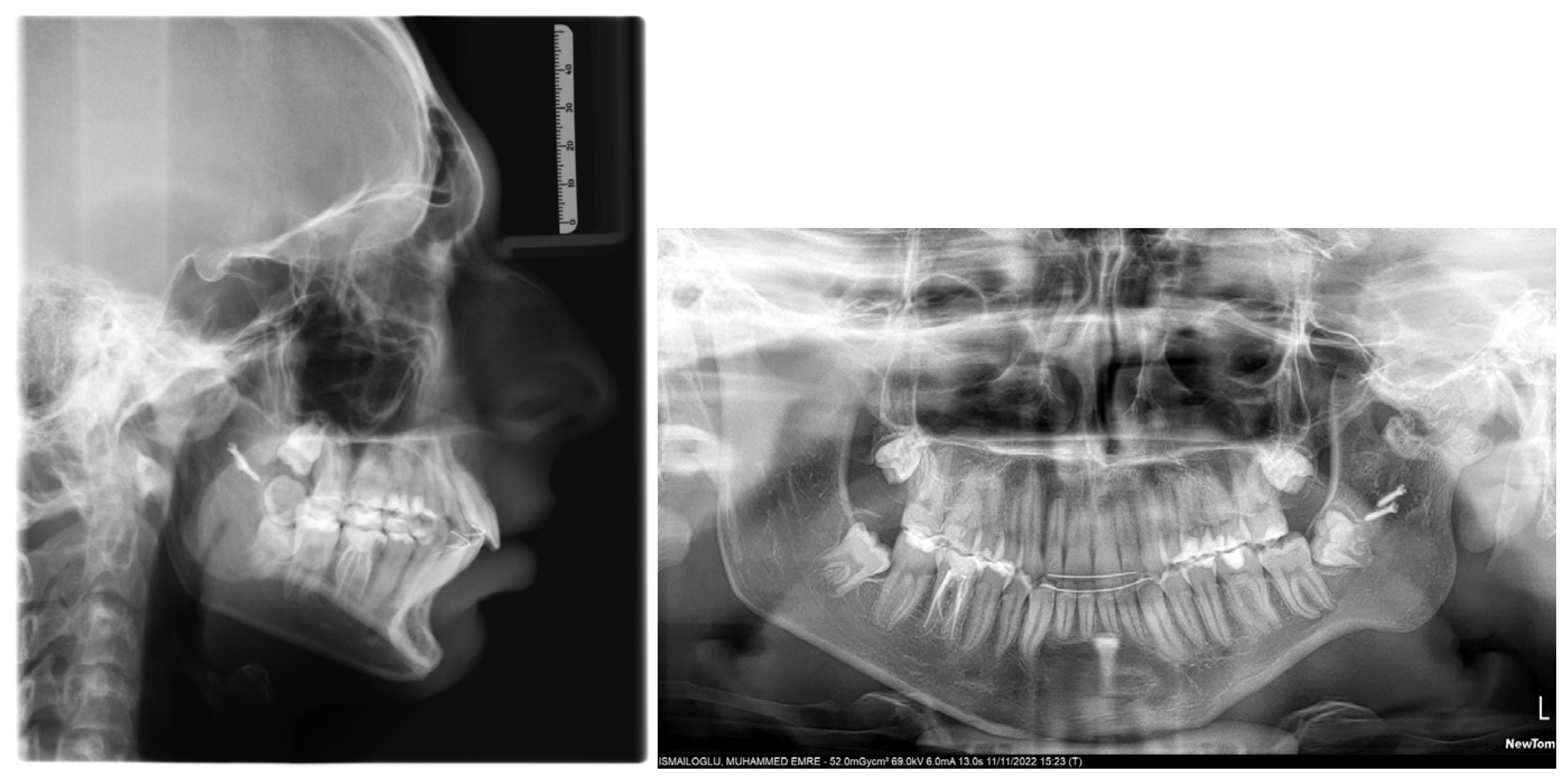
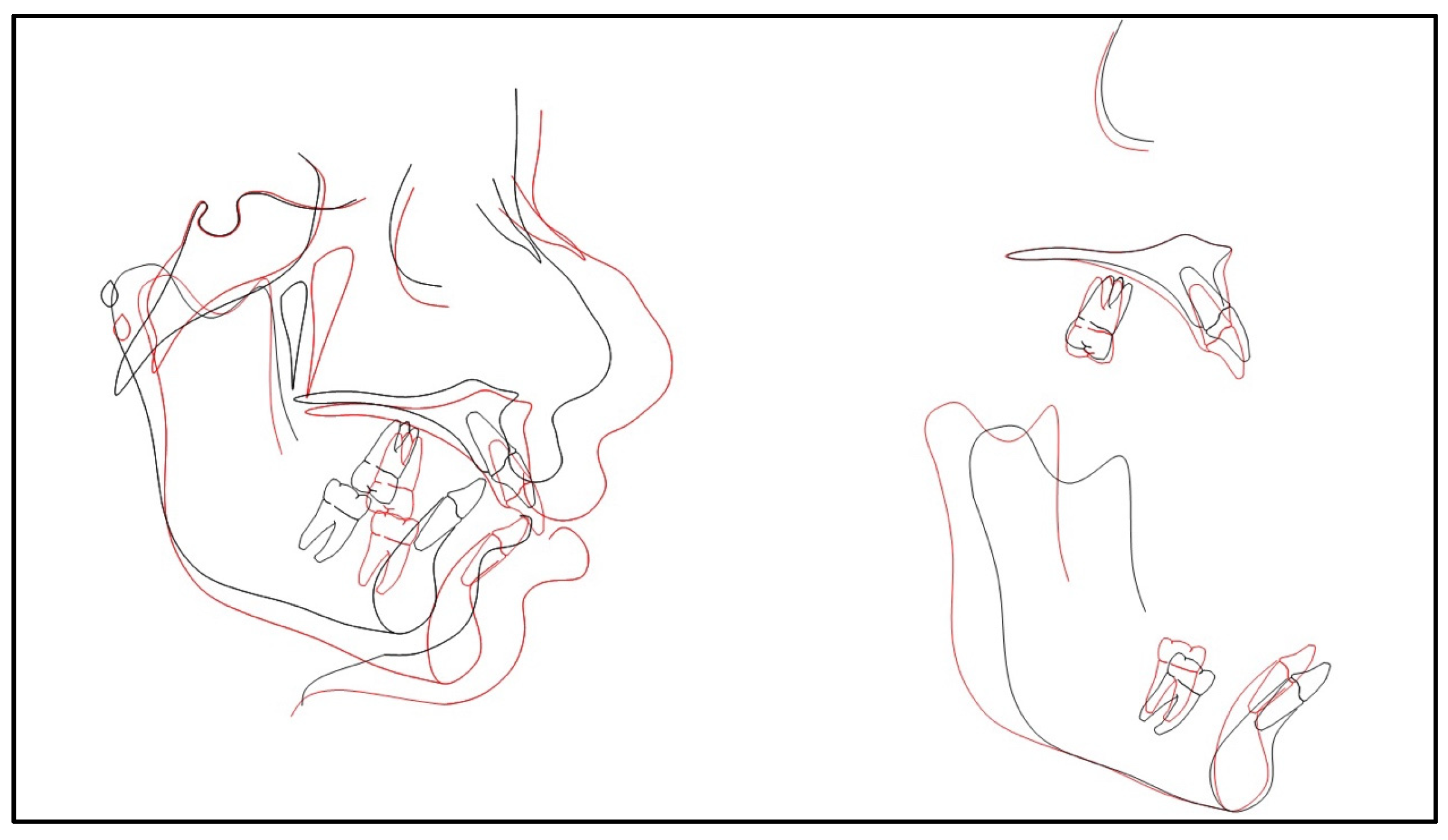
- Improve the convex facial profile.
- Establish lip competency.
- Improve upper incisor proclination.
- Close upper spacing.
- Relieve lower crowding.
- Level and align the teeth.
- Improve the occlusal cant.
- Improve the overjet.
- Improve the overbite.
- Improve molar and canine relationships.
- Monitor third molar development.
- Monitor the left TMJ.
- Retain final alignment and occlusion.
4. Treatment Alternatives
- Bilateral sagittal split osteotomy
- Mandibular distraction osteogenesis
- Genioplasty
- Extractions and orthodontic camouflage
5. Treatment Progress
6. Treatment Results
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Papadopoulos, M.A. Non-compliance approaches for management of Class II malocclusion. In Skeletal Anchorage in Orthodontic Treatment of Class II Malocclusion; Papadopoulos, M.A., Ed.; Mosby: Maryland Heights, MO, USA, 2015; pp. 6–21. [Google Scholar] [CrossRef]
- Kaieda, A.K.; Lima, I.F.P.; Scanavini, M.A.; Coqueiro, R.S.; Pithon, M.M.; Rode, S.M.; Paranhos, L.R. Perception, knowledge and attitudes of Brazilian orthodontists on the treatment of Class II malocclusions. An. Acad. Bras. Cienc. 2017, 89, 2875–2885. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.W.; Wang, Y.Y.; He, Z.F.; Lu, M.X.; Li, G.F.; Li, H. Orthodontic-surgical treatment for severe skeletal class II malocclusion with vertical maxillary excess and four premolars extraction: A case report. World J. Clin. Cases 2023, 11, 1106–1114. [Google Scholar] [CrossRef] [PubMed]
- Mihalik, C.A.; Proffit, W.R.; Phillips, C. Long-term follow-up of Class II adults treated with orthodontic camouflage: A comparison with orthognathic surgery outcomes. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 266–278. [Google Scholar] [CrossRef] [PubMed]
- Naragond, A.; Kenganal, S.; Sagarkar, R.; Sugaradday. Orthodontic Camouflage Treatment in an Adult Patient with a Class II, Division 1 Malocclusion—A Case Report. J. Clin. Diagn. Res. 2013, 7, 395–400. [Google Scholar] [CrossRef]
- Demir, A.; Uysal, T.; Sari, Z.; Basciftci, F.A. Effects of camouflage treatment on dentofacial structures in Class II division 1 mandibular retrognathic patients. Eur. J. Orthod. 2005, 27, 524–531. [Google Scholar] [CrossRef]
- Upadhyay, M.; Yadav, S.; Nagaraj, K.; Uribe, F.; Nanda, R. Mini-implants vs fixed functional appliances for treatment of young adult Class II female patients: A prospective clinical trial. Angle Orthod. 2012, 82, 294–303. [Google Scholar] [CrossRef]
- Manik, P.K.; Kumar, M.; Yadav, A.; Dawar, M. Management of class II malocclusion in an adolescent patient with “The Poosh Appliance”: An in office fabricated fixed functional appliance. J. Indian Orthod. Soc. 2017, 51, 119–126. [Google Scholar] [CrossRef]
- Ruf, S.; Pancherz, H. Orthognathic surgery and dentofacial orthopedics in adult Class II Division 1 treatment: Mandibular sagittal split osteotomy versus Herbst appliance. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 140–152. [Google Scholar] [CrossRef]
- Upadhyay, M.; Yadav, S.; Nagaraj, K.; Nanda, R. Dentoskeletal and soft tissue effects of mini-implants in Class II division 1 patients. Angle Orthod. 2009, 79, 240–247. [Google Scholar] [CrossRef]
- Bolio Casas, M.; Guzmán Valdivia, I. Orthodontic-surgical treatment of a class II division 1 patient. Case report. Rev. Mex. Orthod. 2017, 5, e240–e248. [Google Scholar] [CrossRef]
- Sundararajan, S.; Parameswaran, R.; Vijayalakshmi, D. Orthognathic Surgical Approach for Management of Skeletal Class II Vertical Malocclusion. Contemp. Clin. Dent. 2018, 9 (Suppl. 1), 173–176. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Bai, Y.; Li, S. Treatment of a Class II Division 1 malocclusion with miniscrew anchorage. Am. J. Orthod. Dentofac. Orthop. 2012, 141, e85–e93. [Google Scholar] [CrossRef] [PubMed]
- Lopatiene, K.; Dumbravaite, A. Relationship between tooth size discrepancies and malocclusion. Stomatologija 2009, 11, 119–124. [Google Scholar] [PubMed]
- Othman, S.A.; Harradine, N.W.T. Tooth-size discrepancy and Bolton’s ratios: A literature review. J. Orthod. 2006, 33, 45–51. [Google Scholar] [CrossRef]
- Othman, S.; Harradine, N. Tooth size discrepancies in an orthodontic population. Angle Orthod. 2007, 77, 668–674. [Google Scholar] [CrossRef]
- Aldrees, A.M.; Al-Shujaa, A.M.; Alqahtani, M.A.; Aljhani, A.S. Is arch form influenced by sagittal molar relationship or Bolton tooth-size discrepancy? BMC Oral Health 2015, 15, 70. [Google Scholar] [CrossRef]
- Alajlan, S.S.; Alsaleh, M.K.; Alshammari, A.F.; Alharbi, S.M.; Alshammari, A.K.; Alshammari, R.R. The prevalence of malocclusion and orthodontic treatment need of school children in Northern Saudi Arabia. J. Orthod. Sci. 2019, 8, 10. [Google Scholar] [CrossRef]
- Incorvati, C.; Gulotta, C.; Mirabile, F.M.C.; Badiali, G.; Marchetti, C. Current Trends in Skeletal Borderline Patients: Surgical versus Orthodontic Treatment Decisions—What Is the Evidence? Appl. Sci. 2022, 12, 4636. [Google Scholar] [CrossRef]
- Hunt, O.; Johnston, C.; Hepper, P.; Burden, D.; Stevenson, M. The influence of maxillary gingival exposure on dental attractiveness ratings. Eur. J. Orthod. 2002, 24, 199–204. [Google Scholar] [CrossRef]
- Chidzonga, M.M. Temporomandibular joint ankylosis: Review of thirty-two cases. Br. J. Oral Maxillofac. Surg. 1999, 37, 123–126. [Google Scholar] [CrossRef]
- Arakeri, G.; Kusanale, A.; Zaki, G.A.; Brennan, P.A. Pathogenesis of post-traumatic ankylosis of the temporomandibular joint: A critical review. Br. J. Oral Maxillofac. Surg. 2012, 50, 8–12. [Google Scholar] [CrossRef] [PubMed]
- el-Sheikh, M.M.; Medra, A.M. Management of unilateral temporomandibular ankylosis associated with facial asymmetry. J. Craniomaxillofac. Surg. 1997, 25, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Das, U.M.; Keerthi, R.; Ashwin, D.P.; VenkataSubramanian, R.; Reddy, D.; Shiggaon, N. Ankylosis of temporomandibular joint in children. J. Indian Soc. Pedod. Prev. Dent. 2009, 27, 116–120. [Google Scholar] [CrossRef]
- Jung, S.Y.; Park, J.H.; Park, H.S.; Baik, H.S. Transport distraction osteogenesis combined with orthodontic treatment in a patient with unilateral temporomandibular joint ankylosis. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 372–383. [Google Scholar] [CrossRef]
- Al-Rawee, R.Y.; Al-Khayat, A.M.S.; Saeed, S.S. True bony TMJ ankylosis in children: Case report. Int. J. Surg. Case Rep. 2019, 61, 67–72. [Google Scholar] [CrossRef]
- Elgazzar, R.F.; Abdelhady, A.I.; Saad, K.A.; Elshaal, M.A.; Hussain, M.M.; Abdelal, S.E.; Sadakah, A.A. Treatment modalities of TMJ ankylosis: Experience in Delta Nile, Egypt. Int. J. Oral Maxillofac. Surg. 2010, 39, 333–342. [Google Scholar] [CrossRef]
- de Paula-Júnior, D.F.; Santos, N.C.; da Silva, E.T.; Nunes, M.F.; Leles, C.R. Psychosocial impact of dental esthetics on quality of life in adolescents. Angle Orthod. 2009, 79, 1188–1193. [Google Scholar] [CrossRef]
- Jovanovic, J.; Lerner, R.M.; Lerner, J.V. Objective and subjective attractiveness and early adolescent adjustment. J. Adolesc. 1989, 12, 225–229. [Google Scholar] [CrossRef]
- Phillips, C.; Beal, K.N. Self-concept and the perception of facial appearance in children and adolescents seeking orthodontic treatment. Angle Orthod. 2009, 79, 12–16. [Google Scholar] [CrossRef]
- Clauser, L.; Curioni, C.; Spanio, S. The use of the temporalis muscle flap in facial and craniofacial reconstructive surgery. A review of 182 cases. J. Craniomaxillofac. Surg. 1995, 23, 203–214. [Google Scholar] [CrossRef]
- Gao, X.; Wang, T.; Song, J. Orthodontic and surgical management of a patient with severe skeletal Class II deformity and facial asymmetry: A case report with a 5-year follow-up. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 779–792. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Kumar, S.; Singh, G.; Jain, S. Sequential treatment of unilateral temporo-mandibular joint ankylosis with distraction osteogenesis—A case report. Int. Orthod. 2020, 18, 584–592. [Google Scholar] [CrossRef] [PubMed]
- Damon, D. Damon System: The Workbook; Ormco: Orange, CA, USA, 2004. [Google Scholar]
- Thomas, W.W. Variable Torque for Optimal Inclination. Clin. Impress 2009, 17, 21–27. [Google Scholar]
- Sultana, N.; Hasan, M.N.; Hassan, G.S.; Naim, M.A.; Akther, N. Orthodontic camouflage management of a class II malocclusion with excessive overjet- A case report. Update Dent. Coll. J. 2014, 3, 41–45. [Google Scholar] [CrossRef]
- Thomas, P.M. Orthodontic camouflage versus orthognathic surgery in the treatment of mandibular deficiency. J. Oral Maxillofac. Surg. 1995, 53, 579–587. [Google Scholar] [CrossRef]
- Sicari, F.; Merlo, E.M.; Gentile, G.; Nucera, R.; Portelli, M.; Settineri, S.; Myles, L.A.M.; Militi, A. Body Image and Psychological Impact of Dental Appearance in Adolescents with Malocclusion: A Preliminary Exploratory Study. Children 2023, 10, 1691. [Google Scholar] [CrossRef]
- Kharbanda, O.P.; Chaurasia, S. Functional jaw orthopedics for Class II malocclusion: Where do we stand today? J. Indian Orthod. Soc. 2015, 49, 33–41. [Google Scholar] [CrossRef]
- Raposo, R.; Peleteiro, B.; Paço, M.; Pinho, T. Orthodontic camouflage versus orthodontic-orthognathic surgical treatment in class II malocclusion: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2018, 47, 445–455. [Google Scholar] [CrossRef]
- Phillips, C. Patient-centered outcomes in surgical and orthodontic treatment. Semin. Orthod. 1999, 5, 223–230. [Google Scholar] [CrossRef]
- Anantanarayanan, P.; Narayanan, V.; Manikandhan, R.; Kumar, D. Primary mandibular distraction for management of nocturnal desaturations secondary to temporomandibular joint (TMJ) ankylosis. Int. J. Pediatr. Otorhinolaryngol. 2008, 72, 385–389. [Google Scholar] [CrossRef]
- López, E.N.; Dogliotti, P.L. Treatment of temporomandibular joint ankylosis in children: Is it necessary to perform mandibular distraction simultaneously? J. Craniofac. Surg. 2004, 15, 879–885. [Google Scholar] [CrossRef] [PubMed]
- Resnick, C.M. Temporomandibular Joint Reconstruction in the Growing Child. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 109–121. [Google Scholar] [CrossRef] [PubMed]
- Fariña, R.; Canto, L.; Gunckel, R.; Alister, J.P.; Uribe, F. Temporomandibular joint ankylosis: Algorithm of treatment. J. Craniofac. Surg. 2018, 29, 427–431. [Google Scholar] [CrossRef] [PubMed]
- Temerek, A.; Fahd, A. Conservative gap arthroplasty without interpositioning material for management of temporomandibular joint ankylosis in children: Clinical and Radiographic Outcomes in Upper Egypt. Egypt. Dent. J. 2019, 65, 143–148. [Google Scholar] [CrossRef]
- Passi, D.; Singh, G.; Singh, S.; Mehta, G.; Dutta, S.; Sharma, S. Advances in temporomandibular joint reconstruction in TMJ ankylosis: Our experiences and literature review. Int. J. Dent. Res. 2014, 2, 45–49. [Google Scholar] [CrossRef]
- Guruprasad, Y.; Chauhan, D.S.; Cariappa, K.M. A Retrospective Study of Temporalis Muscle and Fascia Flap in Treatment of TMJ Ankylosis. J. Maxillofac. Oral Surg. 2010, 9, 363–368. [Google Scholar] [CrossRef]
- Agarwal, A.; Ruparelia, B.; Kubawat, A.; Patel, S.; Gupta, S. Modified gap arthroplasty and Myrhaug’s incision as a treatment option in management of temporomandibular joint ankylosis: A study of 10 cases. J. Contemp. Dent. Pract. 2011, 12, 295–300. [Google Scholar] [CrossRef]
- Cho, J.-W.; Park, J.-H.; Kim, J.-W.; Kim, S.-J. The sequential management of recurrent temporomandibular joint ankylosis in a growing child: A case report. Maxillofac. Plast. Reconstr. Surg. 2016, 38, 39. [Google Scholar] [CrossRef]
- Sandhu, A.; Sakaria, B.A.; Patel, S.D.; Ahuja, G.; Jadeja, N.; Mehta, A.; Kakkad, D. The Impact of Early Orthodontic Intervention on Dental and Skeletal Development in Children with Mixed Dentition. J. Pharm. Bioallied. Sci. 2024, 16 (Suppl. 1), S818–S820. [Google Scholar] [CrossRef]
- Sinha, A.; Subashree, S.; Avirachan, T.V.; Imran, M.; Chidambaram, D.; Prasad, S.M.V. Effect of Early Orthodontic Treatment on Long-Term Stability of Class II Malocclusions. J. Pharm. Bioallied. Sci. 2024, 16 (Suppl. 2), S1808–S1810. [Google Scholar] [CrossRef]
- Fivez, S.; Politis, C.; Dormaar, J.T.; Cadenas de Llano-Pérula, M. Surgical and Orthodontic Approach to Temporomandibular Joint Ankylosis After Ear Infection: A Case Series. J. Oral Maxillofac. Surg. 2020, 78, 2235–2246. [Google Scholar] [CrossRef]
- Quinzi, V.; Paskay, L.C.; D’andrea, N.; Albani, A.; Monaco, A.; Saccomanno, S. Evaluation of the Nasolabial Angle in Orthodontic Diagnosis: A Systematic Review. Appl. Sci. 2021, 11, 2531. [Google Scholar] [CrossRef]


| Variable | Pre-Treatment | Post-Treatment | |||
|---|---|---|---|---|---|
| Value | Norm | SD | Value | Change | |
| SNA (°) | 83.0 | 82.0 | 3.5 | 84.4 | 1.4 |
| SNB (°) | 72.7 | 80.0 | 3.0 | 77.7 | 5.0 |
| ANB (°) | 10.3 | 2.0 | 2.4 | 8.8 | −1.5 |
| Wits appraisal (mm) | 15.8 | −1.0 | 1.0 | 10.3 | −5.5 |
| Maxillary-mandibular planes angle (°) | 19.0 | 25.0 | 6.0 | 23,7 | 4.7 |
| SN-maxillary planes angle (°) | 7.1 | 8.2 | 3.3 | 6.5 | −0.6 |
| Lower face height ratio (%) | 52.9 | 55.0 | 3.0 | 54.8 | 1.9 |
| Upper incisors to maxillary plane (°) | 121.9 | 110.0 | 5.0 | 114.5 | −7.4 |
| IMPA (°) | 117.3 | 95.0 | 7.0 | 113.0 | −4.5 |
| Interincisal angle (°) | 101.7 | 130.0 | 5.0 | 108.9 | 7.2 |
| L1-Apo (mm) | 1.1 | 2.7 | 1.7 | 4.2 | 3.1 |
| Upper lip to E-Plane (mm) | 1.5 | −3.0 | 2.0 | −0.2 | −1.7 |
| Lower lip to E-Plane (mm) | 1.5 | −2.0 | 2.0 | 4.9 | 3.4 |
| A-N perpendicular (mm) | 2.6 | 0.0 | 2.0 | 1.8 | −0.8 |
| Pog-N perpendicular (mm) | −11.6 | 2.0 | 4.0 | −9.7 | 1.9 |
| SN-GoGn (°) | 22.2 | 32.9 | 5.2 | 25.9 | 3.7 |
| U1-SN (°) | 114.9 | 103.0 | 5.5 | 108.0 | −6.9 |
| U1-NA (°) | 31.9 | 22.8 | 5.0 | 23.6 | −8.3 |
| U1-NA (mm) | 7.0 | 4.3 | 2.7 | 2.3 | −4.7 |
| L1-NB (°) | 36.1 | 25.3 | 6.0 | 38.8 | 2.7 |
| L1-NB (mm) | 8.7 | 4.0 | 1.8 | 11.5 | 2.8 |
| Overjet (mm) | 10.8 | 2.5 | 2.5 | 3.2 | −7.6 |
| Overbite (mm) | 6.5 | 2.5 | 2.0 | 3.4 | −3.1 |
| NLA (°) | 119.0 | 102.0 | 8.0 | 142.2 | 23.2 |
| U lip-S line (mm) | 3.3 | 0.0 | 2.0 | 1.0 | −2.3 |
| L lip-S line (mm) | 2.4 | 0.0 | 2.0 | 5.5 | 3.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nalbantoglu, E.R.; Uckan, S.; Singh, P. Non-Extraction Orthodontic Camouflage for Severe Class II Malocclusion Post-TMJ Gap Arthroplasty: A Case Report. Oral 2025, 5, 45. https://doi.org/10.3390/oral5020045
Nalbantoglu ER, Uckan S, Singh P. Non-Extraction Orthodontic Camouflage for Severe Class II Malocclusion Post-TMJ Gap Arthroplasty: A Case Report. Oral. 2025; 5(2):45. https://doi.org/10.3390/oral5020045
Chicago/Turabian StyleNalbantoglu, Eser Rengin, Sina Uckan, and Parmjit Singh. 2025. "Non-Extraction Orthodontic Camouflage for Severe Class II Malocclusion Post-TMJ Gap Arthroplasty: A Case Report" Oral 5, no. 2: 45. https://doi.org/10.3390/oral5020045
APA StyleNalbantoglu, E. R., Uckan, S., & Singh, P. (2025). Non-Extraction Orthodontic Camouflage for Severe Class II Malocclusion Post-TMJ Gap Arthroplasty: A Case Report. Oral, 5(2), 45. https://doi.org/10.3390/oral5020045






