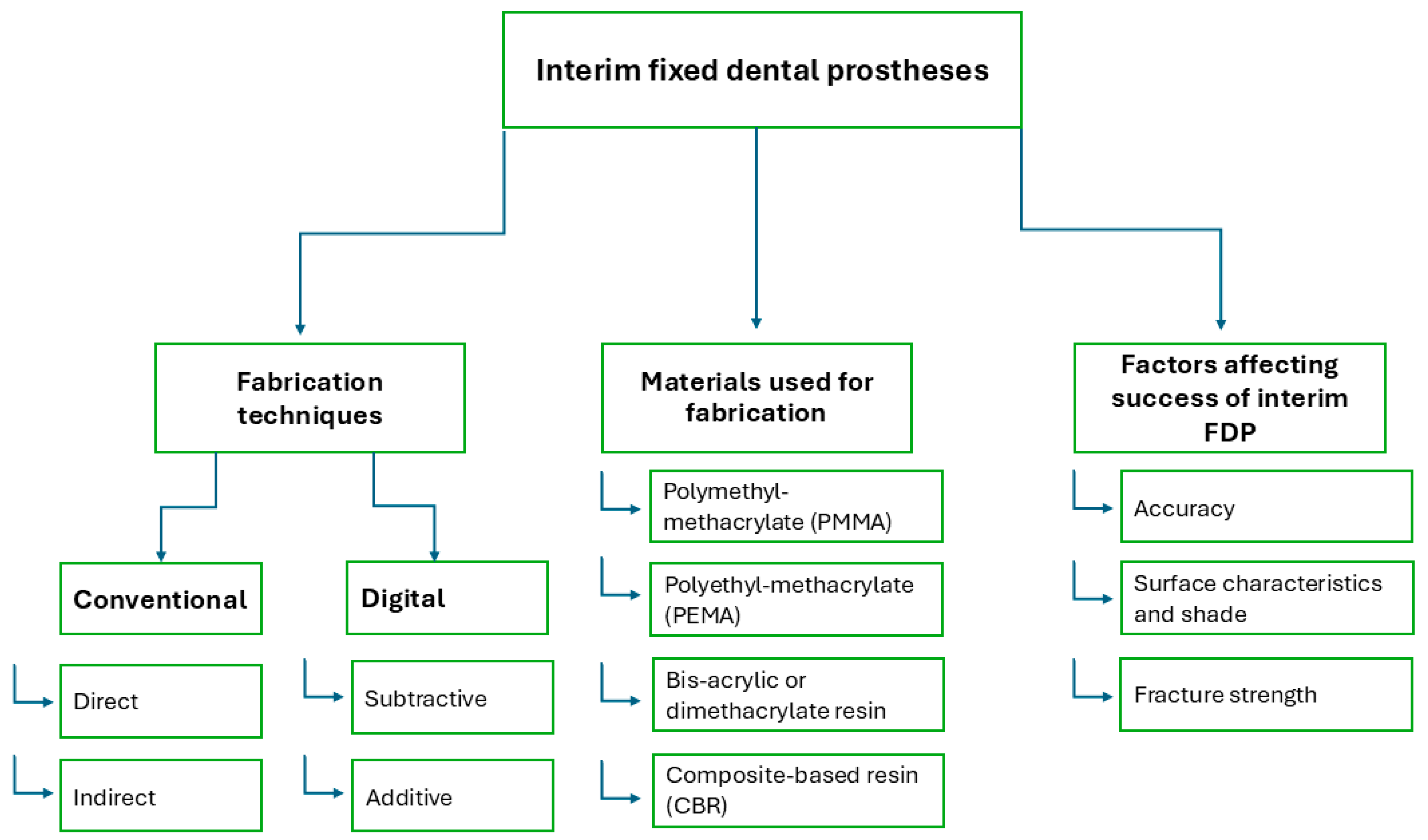
Interim Fixed Dental Prostheses Fabrication Techniques and Factors Affecting Their Success: A Narrative Review
Abstract
1. Introduction
2. Methods of Fabrication of Interim FDPs
2.1. Conventional Fabrication
2.1.1. Direct (Chairside)
2.1.2. Indirect (Laboratory) Fabrication
2.2. Digital Fabrication
2.2.1. Subtractive Technique (Milling)
2.2.2. Additive Technique (3D Printing)
3. Materials Available for Interim FDPs
4. Factors Affecting the Success of Interim FDPs
4.1. Accuracy of Interim FDPs
4.1.1. Marginal Adaptation
4.1.2. Internal Fit
4.1.3. Occlusal Surface Accuracy
4.2. Surface Characteristics and Shade
4.3. Fracture Strength
4.4. Clinical Performance
5. Conclusions
6. Clinical Recommendations
- The conventional fabrication technique for interim FDPs is recommended for cases with short span lengths and when the prosthesis is intended for short-term use.
- Digital techniques are recommended for fabricating interim FDPs intended for long-term use.
- Milled interim FDPs are preferred in cases with high esthetic demands, expected heavy occlusal forces, periodontal diseases, or poor oral hygiene.
- 3D–printed FDPs are best suited for cases involving longer span lengths or full-arch rehabilitation as try-in restorations due to their precise accuracy compared to milled long-span bridges. However, reduced mechanical properties may limit their long-term use as interim FDPs.
- 3D–printed interim crowns demonstrated reliable clinical durability and efficiency. However, longer span FDPs might not meet the required clinical standards in terms of fracture resistance.
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Peng, C.C.; Chung, K.H.; Yau, H.T.; Ramos, V. Assessment of the internal fit and marginal integrity of interim crowns made by different manufacturing methods. J. Prosthet. Dent. 2020, 123, 514–522. [Google Scholar] [CrossRef]
- Sadighpour, L.; Geramipanah, F.; Falahchai, M.; Tadbiri, H. Marginal adaptation of three-unit interim restorations fabricated by the CAD-CAM systems and the direct method before and after thermocycling. J. Clin. Exp. Dent. 2021, 13, e572–e579. [Google Scholar] [CrossRef]
- Mârțu, I.; Murariu, A.; Baciu, E.R.; Savin, C.N.; Foia, I.; Tatarciuc, M.; Diaconu-Popa, D. An Interdisciplinary Study Regarding the Characteristics of Dental Resins Used for Temporary Bridges. Medicina 2022, 58, 811. [Google Scholar] [CrossRef]
- Alharbi, N.; Alharbi, S.; Cuijpers, V.M.J.I.; Osman, R.B.; Wismeijer, D. Three-dimensional evaluation of marginal and internal fit of 3D-printed interim restorations fabricated on different finish line designs. J. Prosthodont. Res. 2018, 62, 218–226. [Google Scholar] [CrossRef]
- Emetwaly el shazly, M.; Abdelhamid, T.; Atta, M.O. Marginal Integrity of Temporary Bridges Constructed by CAD/CAM, Three Dimentional Printer and Conventional Method. Dent. Sci. Updates 2023, 4, 357–365. [Google Scholar] [CrossRef]
- Huettig, F.; Prutscher, A.; Goldammer, C.; Kreutzer, C.A.; Weber, H. First clinical experiences with CAD/CAM-fabricated PMMA-based fixed dental prostheses as long-term temporaries. Clin. Oral Investig. 2016, 20, 161–168. [Google Scholar] [CrossRef]
- Abdullah, A.O.; Pollington, S.; Liu, Y. Comparison between direct chairside and digitally fabricated temporary crowns. Dent. Mater. J. 2018, 37, 957–963. [Google Scholar] [CrossRef]
- Sakr, O.A.; Mandour, M.H.; Gabal, Z.A. Fracture Resistance of Provisional Crowns Fabricated by Conventional, CAD/CAM, and 3D Printing Techniques. Al-Azhar Dent. J. Girls 2022, 9, 623–630. [Google Scholar] [CrossRef]
- Al Twal, E.Q.H.; Chadwick, R.G. Fibre reinforcement of two temporary composite bridge materials—Effect upon flexural properties. J. Dent. 2012, 40, 1044–1051. [Google Scholar] [CrossRef]
- Peñate, L.; Basilio, J.; Roig, M.; Mercadé, M. Comparative study of interim materials for direct fixed dental prostheses and their fabrication with CAD/CAM technique. J. Prosthet. Dent. 2015, 114, 248–253. [Google Scholar] [CrossRef]
- Martínez, M.F.E.; López, S.R.; Fontela, J.V.; García, S.O.; Quevedo, M.M. A new technique for direct fabrication of fiber-reinforced composite bridge: A long-term clinical observation. Dent. J. 2020, 8, 48. [Google Scholar] [CrossRef]
- Karabekmez, D.; Aktas, G. Single anterior tooth replacement with direct fiber-reinforced composite bridges: A report of three cases. Niger J. Clin. Pract. 2020, 23, 434–436. [Google Scholar] [CrossRef]
- Lee, J.; Clark, S.R.; Tantbirojn, D.; Korioth, T.V.P.; Hill, A.E.; Versluis, A. Strength and stiffness of interim materials and interim fixed dental prostheses when tested at different loading rates. J. Prosthet. Dent. 2022, 127, 161–167. [Google Scholar] [CrossRef]
- Cattoni, F.; Teté, G.; Calloni, A.M.; Manazza, F.; Gastaldi, G.; Capparè, P. Milled versus moulded mock-ups based on the superimposition of 3D meshes from digital oral impressions: A comparative in vitro study in the aesthetic area. BMC Oral Health 2019, 29, 230. [Google Scholar] [CrossRef]
- Davidowitz, G.; Kotick, P.G. The Use of CAD/CAM in Dentistry. Dent. Clin. N. Am. 2011, 55, 559–570. [Google Scholar] [CrossRef]
- Cuschieri, L.A.; Casha, A.; No-Cortes, J.; Ferreira Lima, J.; Cortes, A.R.G. Patient Satisfaction with Anterior Interim CAD-CAM Rehabilitations Designed by CAD Technician versus Trained Dentist—A Clinical Preliminary Study. Appl. Sci. 2023, 13, 8243. [Google Scholar] [CrossRef]
- Jandyal, A.; Chaturvedi, I.; Wazir, I.; Raina, A.; Ul Haq, M.I. 3D printing—A review of processes, materials and applications in industry 4.0. Sustain. Oper. Comput. 2022, 3, 33–42. [Google Scholar] [CrossRef]
- Jain, S.; Sayed, M.E.; Shetty, M.; Alqahtani, S.M.; Al Wadei, M.H.D.; Gupta, S.G.; Othman, A.A.A.; Alshehri, A.H.; Alqarni, H.; Mobarki, A.H.; et al. Physical and Mechanical Properties of 3D-Printed Provisional Crowns and Fixed Dental Prosthesis Resins Compared to CAD/CAM Milled and Conventional Provisional Resins: A Systematic Review and Meta-Analysis. Polymers 2022, 14, 2691. [Google Scholar] [CrossRef]
- Nestler, N.; Wesemann, C.; Spies, B.C.; Beuer, F.; Bumann, A. Dimensional accuracy of extrusion- and photopolymerization-based 3D printers: In vitro study comparing printed casts. J. Prosthet. Dent. 2021, 125, 103–110. [Google Scholar] [CrossRef]
- Resende, C.C.D.; Barbosa, T.A.Q.; Moura, G.F.; Rizzante, F.A.P.; Mendonça, G.; Zancopé, K.; das Neves, F.D. Cost and effectiveness of 3-dimensionally printed model using three different printing layer parameters and two resins. J. Prosthet. Dent. 2023, 129, 350–353. [Google Scholar] [CrossRef]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.S.; Jiang, H.B. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef]
- Kakinuma, H.; Izumita, K.; Yoda, N.; Egusa, H.; Sasaki, K. Comparison of the accuracy of resin-composite crowns fabricated by three-dimensional printing and milling methods. Dent. Mater. J. 2022, 41, 808–815. [Google Scholar] [CrossRef]
- Son, K.; Lee, J.H.; Lee, K.B. Comparison of intaglio surface trueness of interim dental crowns fabricated with sla 3d printing, dlp 3d printing, and milling technologies. Healthcare 2021, 9, 983. [Google Scholar] [CrossRef]
- Giannetti, L.; Apponi, R.; Mordini, L.; Presti, S.; Breschi, L.; Mintrone, F. The occlusal precision of milled versus printed provisional crowns. J. Dent. 2022, 1, 117. [Google Scholar] [CrossRef]
- Aldahian, N.; Khan, R.; Mustafa, M.; Vohra, F.; Alrahlah, A. Influence of Conventional, CAD-CAM, and 3D Printing Fabrication Techniques on the Marginal Integrity and Surface Roughness and Wear of Interim Crowns. Appl. Sci. 2021, 11, 8964. [Google Scholar] [CrossRef]
- Shalaby, M.; Wahba, M.; Mohamed, A. Assessment of the Effect of two Different Digital Fabrication Techniques on Marginal and Internal Fit of Interim Fixed Dental Prothesis. Future Dent. J. 2023, 9, 65–72. [Google Scholar] [CrossRef]
- Kessler, A.; Reymus, M.; Hickel, R.; Kunzelmann, K.H. Three-body wear of 3D printed temporary materials. Dent. Mater. 2019, 35, 1805–1812. [Google Scholar] [CrossRef]
- Al-Qahtani, A.S.; Tulbah, H.I.; Binhasan, M.; Abbasi, M.S.; Ahmed, N.; Shabib, S.; Farooq, I.; Aldahian, N.; Nisar, S.S.; Tanveer, S.A.; et al. Surface properties of polymer resins fabricated with subtractive and additive manufacturing techniques. Polymers 2021, 13, 4077. [Google Scholar] [CrossRef]
- Karaokutan, I.; Sayin, G.; Kara, O. In vitro study of fracture strength of provisional crown materials. J. Adv. Prosthodont. 2015, 7, 27–31. [Google Scholar] [CrossRef]
- Berghaus, E.; Klocke, T.; Maletz, R.; Petersen, S. Degree of conversion and residual monomer elution of 3D-printed, milled and self-cured resin-based composite materials for temporary dental crowns and bridges. J. Mater. Sci. Mater. Med. 2023, 34, 23. [Google Scholar] [CrossRef]
- Ghavami-Lahiji, M.; Falahchai, M.; Habibi Arbastan, A.; Arbastan, H. Review Paper: Different ways to measure marginal fit and internal adaptation of restorations in dentistry Citation. J. Dentomaxillofac. Radiol. Pathol. Surg. 2023, 12, 16–23. [Google Scholar]
- Bousnaki, M.; Chatziparaskeva, M.; Bakopoulou, A.; Pissiotis, A.; Koidis, P. Variables affecting the fit of zirconia fixed partial dentures: A systematic review. J. Prosthet. Dent. 2020, 123, 686–692. [Google Scholar] [CrossRef]
- Sachs, C.; Groesser, J.; Stadelmann, M.; Schweiger, J.; Erdelt, K.; Beuer, F. Full-arch prostheses from translucent zirconia: Accuracy of fit. Dent. Mater. 2014, 30, 817–823. [Google Scholar] [CrossRef]
- Akçin, E.T.; Güncü, M.B.; Aktaş, G.; Aslan, Y. Effect of manufacturing techniques on the marginal and internal fit of cobalt-chromium implant-supported multiunit frameworks. J. Prosthet. Dent. 2018, 120, 715–720. [Google Scholar] [CrossRef]
- Kim, W.K.; Kim, S. Effect of number of pontics and impression technique on the accuracy of four-unit monolithic zirconia fixed dental prostheses. J. Prosthet. Dent. 2018, 119, 860.e1–860.e7. [Google Scholar] [CrossRef]
- Kim, M.W.; Kim, J.Y.; Shim, J.S.; Kim, S. Effect of the number of splinted abutments on the accuracy of zirconia copings. J. Prosthet. Dent. 2018, 120, 790.e1–790.e7. [Google Scholar] [CrossRef]
- Borba, M.; Cesar, P.F.; Griggs, J.A.; Della Bona, Á. Adaptation of all-ceramic fixed partial dentures. Dent. Mater. 2011, 27, 1119–1126. [Google Scholar] [CrossRef]
- Son, K.; Lee, S.; Kang, S.H.; Park, J.; Lee, K.B.; Jeon, M.; Yun, B.J. A comparison study of marginal and internal fit assessment methods for fixed dental prostheses. J. Clin. Med. 2019, 8, 785. [Google Scholar] [CrossRef]
- Attia, M.A.; Blunt, L.; Bills, P.; Tawfik, A.; Radawn, M. Micro-CT analysis of marginal and internal fit of milled and pressed polyetheretherketone single crowns. J. Prosthet. Dent. 2023, 129, 906.e1–906.e10. [Google Scholar] [CrossRef]
- Wadhwani, V.; Sivaswamy, V.; Rajaraman, V. Surface roughness and marginal adaptation of stereolithography versus digital light processing three-dimensional printed resins: An in-vitro study. J. Indian Prosthodont. Soc. 2022, 22, 377. [Google Scholar]
- Gantz, L.; Fauxpoint, G.; Arntz, Y.; Pelletier, H.; Etienne, O. In vitro comparison of the surface roughness of polymethyl methacrylate and bis-acrylic resins for interim restorations before and after polishing. J. Prosthet. Dent. 2021, 125, 833.e1–833.e10. [Google Scholar] [CrossRef]
- Alikhasi, M.; Jafarian, Z. Additional Manufactured Interim Restorations: A Review on the Literature. J. Dent. 2022, 23, 424–437. [Google Scholar]
- Revilla-León, M.; Umorin, M.; Özcan, M.; Piedra-Cascón, W. Color dimensions of additive manufactured interim restorative dental material. J. Prosthet. Dent. 2021, 123, 754–760. [Google Scholar] [CrossRef]
- Ellakany, P.; Fouda, S.M.; AlGhamdi, M.A.; Aly, N.M. Comparison of the color stability and surface roughness of 3-unit provisional fixed partial dentures fabricated by milling, conventional and different 3D printing fabrication techniques. J. Dent. 2023, 131, 104458. [Google Scholar] [CrossRef]
- Yao, Q.; Morton, D.; Eckert, G.J.; Lin, W.S. The effect of surface treatments on the color stability of CAD-CAM interim fixed dental prostheses. J. Prosthet. Dent. 2021, 126, 248–253. [Google Scholar] [CrossRef]
- Al-Wahadni, A.; Abu Rashed, B.O.; Al-Fodeh, R.; Tabanjah, A.; Hatamleh, M. Marginal and Internal Gaps, Surface Roughness and Fracture Resistance of Provisional Crowns Fabricated With 3D Printing and Milling Systems. Oper. Dent. 2023, 48, 464–471. [Google Scholar] [CrossRef]
- Ribeiro, A.K.C.; de Freitas, R.F.C.P.; de Carvalho, I.H.G.; de Miranda, L.M.; da Silva, N.R.; de Fátima Dantas de Almeida, L.; Zhang, Y.; da Fonte Porto Carreiro, A.; de Assunção e Souza, R.O. Flexural strength, surface roughness, micro-CT analysis, and microbiological adhesion of a 3D-printed temporary crown material. Clin. Oral Investig. 2023, 27, 2207–2220. [Google Scholar] [CrossRef]
- Radwan, H.; Elnaggar, G.; El Deen, I.S. Surface roughness and color stability of 3D printed temporary crown material in different oral media (In vitro study). Int. J. Appl. Dent. Sci. 2021, 7, 327–334. [Google Scholar] [CrossRef]
- Alsarani, M.M. Influence of aging process and restoration thickness on the fracture resistance of provisional crowns: A comparative study. Saudi Dent. J. 2023, 35, 939–945. [Google Scholar] [CrossRef]
- Alshamrani, A.; Alhotan, A.; Owais, A.; Ellakwa, A. The Clinical Potential of 3D-Printed Crowns Reinforced with Zirconia and Glass Silica Microfillers. J. Funct. Biomater. 2023, 14, 267. [Google Scholar] [CrossRef]
- Othman, A.; Sandmair, M.; Alevizakos, V.; von See, C. The fracture resistance of 3D-printed versus milled provisional crowns: An in vitro study. PLoS ONE 2023, 18, e0285760. [Google Scholar] [CrossRef]
- Abdullah, A.O.; Tsitrou, E.A.; Pollington, S. Comparative in vitro evaluation of CAD/CAM vs conventional provisional crowns. J. Appl. Oral Sci. 2016, 24, 258–263. [Google Scholar] [CrossRef]
- Abad-Coronel, C.; Carrera, E.; Córdova, N.M.; Fajardo, J.I.; Aliaga, P. Comparative analysis of fracture resistance between cad/cam materials for interim fixed prosthesis. Materials 2021, 14, 7791. [Google Scholar] [CrossRef]
- Falahchai, M.; Rahimabadi, S.; Khabazkar, G.; Babaee Hemmati, Y.; Neshandar Asli, H. Marginal and internal fit and fracture resistance of three-unit provisional restorations fabricated by additive, subtractive, and conventional methods. Clin. Exp. Dent. Res. 2022, 8, 1404–1412. [Google Scholar] [CrossRef]
- Greuling, A.; Matthies, A.; Eisenburger, M. Fracture load of 4-unit interim fixed partial dentures using 3D-printed and traditionally manufactured materials. J. Prosthet. Dent. 2023, 129, 607.e1–607.e8. [Google Scholar] [CrossRef]
- Rand, A.; Kohorst, P.; Greuling, A.; Borchers, L.; Stiesch, M. Stress distribution in all-ceramic posterior 4-unit fixed dental prostheses supported in different ways: Finite element analysis. Implant. Dent. 2016, 25, 485–491. [Google Scholar] [CrossRef]
- Cheng, C.W.; Ye, S.Y.; Chien, C.H.; Chen, C.J.; Papaspyridakos, P.; Ko, C.C. Randomized clinical trial of a conventional and a digital workflow for the fabrication of interim crowns: An evaluation of treatment efficiency, fit, and the effect of clinician experience. J. Prosthet. Dent. 2021, 125, 73–81. [Google Scholar] [CrossRef]
- de Souza, F.A.; Blois, M.C.; Collares, K.; dos Santos, M.B.F. 3D-printed and conventional provisional single crown fabrication on anterior implants: A randomized clinical trial. Dent. Mater. 2024, 40, 340–347. [Google Scholar] [CrossRef]
- del Hougne, M.; Di Lorenzo, I.; Höhne, C.; Schmitter, M. A retrospective cohort study on 3D printed temporary crowns. Sci. Rep. 2024, 14, 17295. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdelmohsen, N.; Bourauel, C.; Elshazly, T.M. Interim Fixed Dental Prostheses Fabrication Techniques and Factors Affecting Their Success: A Narrative Review. Oral 2025, 5, 44. https://doi.org/10.3390/oral5020044
Abdelmohsen N, Bourauel C, Elshazly TM. Interim Fixed Dental Prostheses Fabrication Techniques and Factors Affecting Their Success: A Narrative Review. Oral. 2025; 5(2):44. https://doi.org/10.3390/oral5020044
Chicago/Turabian StyleAbdelmohsen, Nour, Christoph Bourauel, and Tarek M. Elshazly. 2025. "Interim Fixed Dental Prostheses Fabrication Techniques and Factors Affecting Their Success: A Narrative Review" Oral 5, no. 2: 44. https://doi.org/10.3390/oral5020044
APA StyleAbdelmohsen, N., Bourauel, C., & Elshazly, T. M. (2025). Interim Fixed Dental Prostheses Fabrication Techniques and Factors Affecting Their Success: A Narrative Review. Oral, 5(2), 44. https://doi.org/10.3390/oral5020044






