Abstract
Background: The provision of dental care in Pakistan is limited, with less than 5% of the population having access to qualified dental practitioners. The lack of contextually relevant local dental guidelines further adds to the problem. We developed clinical practice guidelines (CPGs) and referral pathways to improve primary care for common oral diseases. Methods: Using the GRADE-ADOLOPMENT approach, recommendations from source guidelines (developed in Europe and the United States) were adopted (retained as is or with minor changes), adapted (modified according to the local context), or excluded (omitted due to lack of local relevance). The guidelines included diseases such as periodontitis, dental pain, intraoral swelling, and oral cavity malignancies. The end result was a set of locally relevant CPGs, which were then used to formulate referral pathways, with the incorporated suggestions being based on a thorough evidence review process. Results: We included four recommendations, three of which were adopted with minor modifications to the referral pathway. These changes focused on assessing potentially malignant oral conditions and counseling for risk factors. No content changes were needed for the CPGs of the other two disorders. We developed referral pathways for three specific oral conditions, detailing primary care physicians’ roles in diagnosis, initial treatment, and timely referral. Conclusion: Contextually relevant dental CPGs and referral pathways can improve patient outcomes in Pakistan. Our study produced four additional recommendations focused on risk factor counselling and mitigation, which could potentially reduce the burden of oral malignancies in our local population.
1. Introduction and Background
Over the past three decades, the global burden of oral diseases has risen by an alarming 64%, currently affecting almost half the world’s population [1]. In lower-middle-income countries (LMICs), the weight of this issue is particularly heavy, with an occurrence rate totaling nearly 1.2 billion cases [2]. Dental caries stands as one of the most prevalent oral diseases in Pakistan, impacting 60% of the population [3]. Malignancies, particularly those of the lips and oral cavity, are the second most prevalent type of cancer in the country, with almost 17,000 new cases in 2020 [4]. Apart from the clinical consequences of oral diseases, they also pose significant financial [5], social [6], and emotional [7] challenges.
Clinical practice guidelines (CPGs) grounded in evidence play a crucial role in diagnosing, treating, and effectively managing oral diseases. Most CPGs used globally are created by high- income countries, including the United States [8] and several European countries [9,10,11]. These guidelines are specifically tailored to suit the healthcare systems within their respective environments, which naturally serve as the primary source for research on oral health [12]. On the other hand, LMICs face many hindrances to developing independent, evidence-based local CPGs due to insufficient financial resources and research infrastructure [13]. This presents a barrier to achieving optimal dental healthcare at a local level, as several aspects of oral diseases differ substantially in LMICs like Pakistan. These aspects include epidemiology [3,14], lack of primary oral healthcare and screening [15], unregulated dental practitioners (quacks) [14], smokeless tobacco consumption [16], sociocultural influences [17], disease-related awareness [18], health-seeking behavior [19,20], and self-care [20]. Notably, dental care is not covered by universal coverage plans, and it imposes a sizeable financial burden on patients, particularly in LMICs like Pakistan where most healthcare costs are borne directly by individuals [14,21].
It is recommended that even high-quality globally accepted CPGs should be modified according to the local context of the healthcare system that seeks to use them [13]. In LMICs, where a lack of research and resources precludes the de novo creation of CPGs, the next-best approach consists of a combination of adoption (using recommendations in their current state) and adaptation (tailoring specific recommendations through a uniform, structured process) [13]. The recently introduced term “adolopment” describes this fusion of adaptation, adoption, and de novo development [22]. Evidence to decision (EtD) tables are used for the adolopment process via GRADE (Grading of Recommendations, Assessment, Development and Evaluation)-ADOLOPMENT [13,23,24,25]. These tables present both general and context-specific evidence, using standard criteria (Supplementary Tables S1 and S2), against which experts assess the overall appropriateness of existing recommendations and suggested modifications. These modifications could involve adjustments to the targeted population or management in comparison to the primary recommendations.
In rural areas of Pakistan, there is only 1 dentist per 500,000 persons in the population, resulting in an alarmingly severe unmet need for dental healthcare [26]. In fact, it is estimated that less than 5% of Pakistan’s population of more than 220 million has access to specialist dental care [27]. There is also a severe lack of academic dentists in Pakistan, which has led to an acute shortage of dental research in the country [28]. In settings where access to dentists is limited, primary care physicians/general practitioners (GPs) can help manage the burden of oral disease by providing appropriate counseling and oral hygiene education, screening, and specialist referral [29]. In Pakistan, this may be aided by the presence of appropriate CPGs and referral pathways.
The Pakistan Dental Association (PDA) membership consists of 90% of all registered dentists across the country and states that membership “implies an obligation for members to practice their profession in accordance with the high standards laid down by the Association” [30]. However, we were unable to find any best-practice CPGs or referral pathways developed by the PDA online. Alarmingly, less than 25% of dentists in Pakistan report adherence to CPGs of any source, with a major reason being the lack of access to suitable resources [31]. Thus, it is crucial to create local dental CPGs and referral pathways through a transparent and standardized procedure. This involves adapting existing high-quality CPGs with appropriate context-specific modifications. The implementation of these CPGs and referral pathways would move Pakistan’s healthcare system towards attaining optimal health results in dental care, enhancing credibility through transparent development processes.
Our objective is to provide a comprehensive account of our experience with the GRADE-ADOLOPMENT process, which we employed to steer the “adolopment” of evidence-based guidelines and the formulation of referral care pathways for managing oral diseases in Pakistan
2. Methods
Study Setting: This creation of guidelines was undertaken at the Aga Khan University (AKU) in Pakistan by the Center for Clinical Best Practices (CCBP) and the Section of Dental, Oral & Maxillofacial Surgery (DOMS). AKU is a non-profit institution, recognized for its leadership in healthcare and cutting-edge biomedical research endeavors [32].
CCBP is dedicated to adapting and advancing evidence-based guidelines and care pathways to standardize and enhance healthcare not only in Pakistan but also in other LMICs. In the course of this study, the CCBP, in collaboration with the Section of DOMS at AKUH, utilized the GRADE-ADOLOPMENT methods to develop dentistry guidelines specifically tailored for general practitioners in Pakistan. The idea for creating guidelines for GPs instead of dentists stems from the shortage of dentists in the country. GPs possess the ability to deliver essential primary oral healthcare and make appropriate referrals to specialists [26,27,29].
Study Members: The assemblage included CCBP staff, all of whom boast widespread experience in guideline development, along with senior personnel and practicing dentists, including the Section Head of DOMS.
Selection of a Source Guideline: The original CPGs that are subjected to the GRADE-ADOLOPMENT process in the formation of a set of country-specific CPGs are known as the source guidelines. The study team chose the European Federation of Periodontology (EFP) Stage 3 Level Guidelines for Stages I–III Periodontitis [33], the American Dental Association (ADA) Evidence-Based Clinical Practice Guidelines (EBCPG) for Urgent Management of Pulpal- and Periapical-Related Dental Pain and Intra-Oral Swelling [34], and the ADA EBCPG for the Evaluation of Potentially Malignant Disorders in the Oral Cavity [35] as the source guidelines because of their robust recommendations, holistic management approach, and meticulous production of presented data.
Guideline Content Review: Figure 1 illustrates the process used in the creation of the guidelines. Initially, we generated a table of recommendations (ToR) by isolating and listing all recommendations from the source. Two senior dentists separately assessed the source guidelines, categorizing each recommendation as either “Adopt”, “Adapt”, or “Exclude”. Disagreements were resolved through agreement with the Section Head of DOMS.
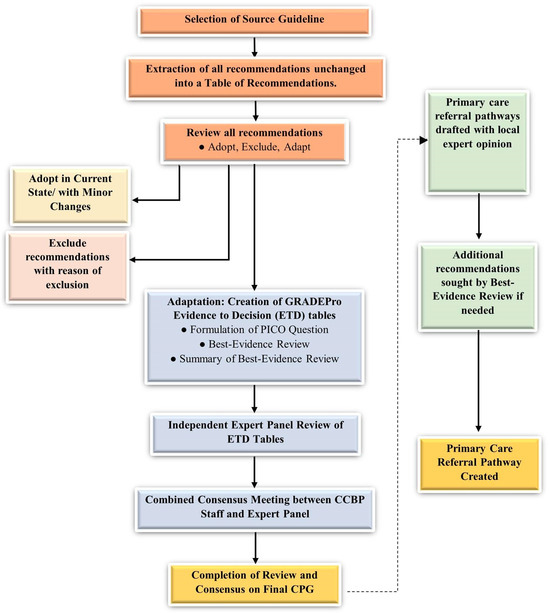
Figure 1.
Process of GRADE-ADOLOPMENT and referral pathway creation.
Recommendations from the source assessed “Adopt” were seamlessly integrated into the development of the local guideline either as is or with minor add-ons. Conversely, those labelled “Exclude” were excluded from the local guidelines, typically due to their relevance to pediatric or inpatient care, or their perceived lack of applicability to the country’s context.
Recommendations marked “Adapt” underwent change via GRADEPro (Supplementary Materials) prior to being merged into the guidelines. De novo recommendations were not created due to the lack of need for new recommendations and the insufficiency of the resources [13]. However, if additional recommendations were deemed vital for any of the referral systems, they were identified via the best-evidence review process described in the Supplementary Materials.
Referral Care Pathway Creation: Recommendations present in the three CPGs were used to create a management algorithm for primary care practitioners. The focus was on early identification and diagnosis, primary care management, and timely referral to specialist dental practitioners.
Final Recommendation Revisions and Synthesis: In this meeting, the referral care pathways for each oral health condition were also presented and discussed, and necessary modifications were incorporated. The final versions of the created CPGs and the referral care pathways were shown to the Section Head of DOMS, after which the recommendations were merged for the local guidelines with an outline of the unanimity judgment.
Final Meeting to Recognize Challenges and Explore Resolutions: To elucidate the challenges encountered during the “adolopment” process and explore potential solutions, focus group discussions (FGDs) were conducted. The FGDs were facilitated by a member of the CCBP, with participation from CCBP and the Section Head of DOMS. The experts engaged in individual brainstorming sessions to identify difficult encounters and propose resolutions, which were subsequently examined within the FGD. Challenges were collectively classified as minor or major through consensus judgment. The CCBP team then organized the final list of difficult encounters into broader categories and provided corresponding resolutions.
These guidelines were created as part of AKU’s ongoing effort to standardize medical practice across Pakistan. A similar methodology has been used to create Pakistani management guidelines for diabetes [36].
3. Results
The procedure led to content changes in one of the three created CPGs [35], with no content changes deemed necessary for the other two [33,34] (Figure 2). Three recommendations were adopted with minute changes for Evaluation of Potentially Malignant Disorders in the Oral Cavity (Supplementary Table S3). A brief summary is given below:
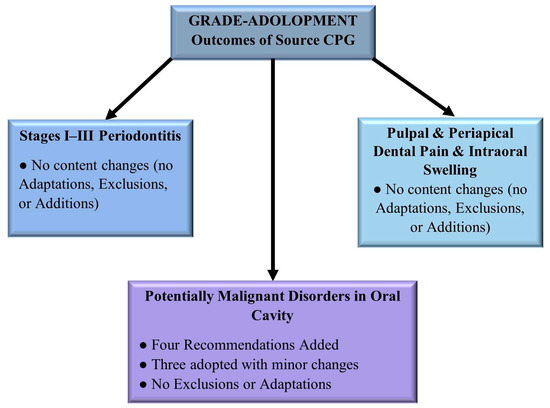
Figure 2.
Content changes to the created Pakistani CPGs.
3.1. Follow-Up and Referral for Potentially Malignant Lesions
Original recommendation: “Clinicians should perform a biopsy and refer the patient if a clinically evident oral mucosal lesion with an unknown diagnosis persists”.
Revised recommendation: “Clinicians should refer for a biopsy of the lesion and also refer the patient to a specialist if the lesion has not resolved and the diagnosis of a potentially malignant disorder cannot be ruled out”.
3.2. Biopsy and Referral for Suspicious Lesions
Original recommendation: “Clinicians should perform a biopsy and refer the patient if a clinically evident oral mucosal lesion is suspicious of a potentially malignant or malignant disorder”.
Revised recommendation: “Clinicians should refer for a biopsy of the lesion and also refer the patient to a specialist if the lesion is considered suspicious of a potentially malignant or malignant disorder”.
3.3. No Action for Patients without Lesions, Symptoms, or Risk Factors
Original recommendation: “No further action is necessary for patients with no clinically evident lesions or symptoms”.
Revised recommendation: “No further action is necessary for patients with no clinically evident lesions, symptoms, or risk factors”.
The referral care pathways designed for the three oral conditions are shown in Figure 3, Figure 4 and Figure 5. Four additional recommendations were incorporated in the referral care pathway for Evaluation of Potentially Malignant Disorders in the Oral Cavity (Supplementary Table S3):
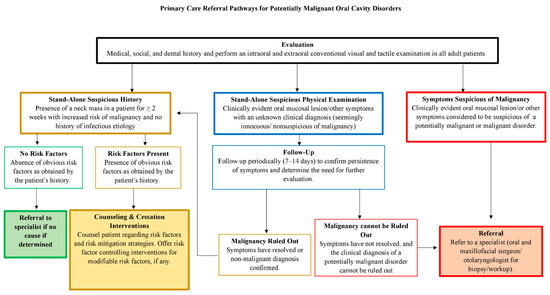
Figure 3.
Primary care referral pathways for potentially malignant oral cavity disorders.
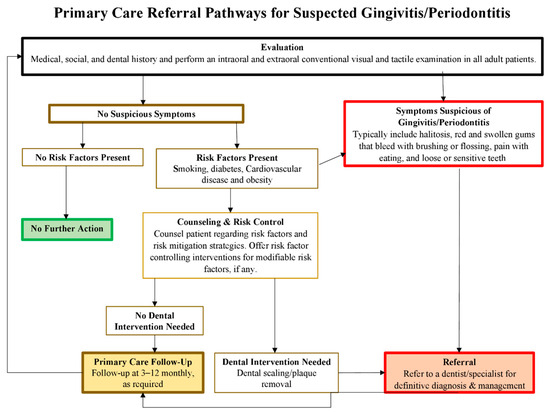
Figure 4.
Primary care referral pathways for suspected periodontitis.
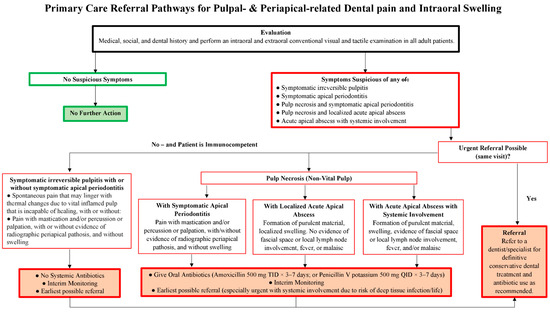
Figure 5.
Primary care referral pathways for pulpal- and periapical-related dental pain and intraoral swelling.
- Risk Factor Mitigation for Asymptomatic Patients:
“For patients without clinically evident lesions or symptoms but with risk factors for oral malignancies, the focus should be on counseling and mitigating these risk factors.”
- 2.
- Tobacco Cessation Counseling:
“All adults using tobacco or smoking should be counseled to stop these habits.”
- 3.
- Behavioral Interventions and Pharmacotherapy for Tobacco Cessation:
“Offer or refer nonpregnant adults using tobacco for behavioral interventions and provide approved pharmacotherapy to support tobacco cessation efforts.”
- 4.
- Environmental Tobacco Smoke Exposure Counseling:
“Consider counseling on the reduction of environmental tobacco smoke exposure or second-hand smoking, taking into account the level of exposure and potential benefits of the intervention in terms of reducing the burden of exposure and associated health risks.”
The difficulties encountered were classified into four main topics (Supplementary Table S4). The full CPG for all three conditions can be found in Supplementary Tables S5–S7.
4. Discussion
Our study aimed to create evidence-based CPGs to be used by GPs for oral diseases in Pakistan and develop referral pathways to guide the management of these conditions. The results of our “adolopment” process yielded the addition of four recommendations to the referral pathway for the evaluation of potentially malignant oral conditions. These concerned modifiable risk factors (primarily tobacco use) cessation counseling, providing cessation interventions, and decreasing second-hand/environmental tobacco smoke exposure. The clinical pathways created delineated initial diagnosis, preliminary treatment to be provided by GPs, and indications for specialist referral.
In Pakistan, almost 20% of adults use tobacco in some form [37]. Furthermore, workplaces and public transport expose over 70% of adults to second-hand smoke [37]. Worryingly, tobacco use in Pakistan continues to grow, spurred by poor understanding about its risks, lower costs, and the relentless marketing efforts of the tobacco industry [38]. It is thus unsurprising that the incidence of oral cancer in Pakistan is among the highest in the world [39]. Overall, tobacco accounts for >100,000 deaths annually in the country, with second-hand exposure accounting for almost 20% of tobacco-related deaths [40]. Attempts to quit smoking in Pakistan are made by fewer than a quarter of smokers, and the success rate of quitting is less than 3% [41,42]. Moreover, only 10% of quitters report using a cessation aid [43]. In addition, although alcohol is forbidden for most of Pakistan’s Muslim-majority population, it is still sold illegally and increasingly consumed across the country [44]. The recommendations added to our clinical referral pathway aim to educate and counsel patients with risk factors regarding the importance of and need for cessation of tobacco and alcohol use, while also offering interventions to aid quitting. These recommendations were “adoloped” from existing recommendations in CPGs published in Canada, the United States, and the United Kingdom [45,46,47] and are a crucial addition to the management of possibly malignant conditions in the oral cavity in Pakistan, where the burden of oral malignant disease is high. In addition, GPs could also be encouraged to stock and provide basic cessation aids, such as nicotine chewing gums, and provide these to patients who use cigarettes or other products. This support at the level of GPs has been shown to significantly increase the likelihood of cessation [48].
There is a severe shortage of dentists in Pakistan, with only 1 dentist per 500,000 persons in the population [26]. Apart from a huge burden of unmet dental care, this scarcity of dentists also results in an overload of patients for the few practicing dentists [49]. Referral systems have been developed across the world [50,51,52] and have been shown to be successful in the triage and management of patients with oral diseases. Through this process of triage, GPs can not only alleviate some of the burden on existing dental care set-ups but can also ensure that basic oral healthcare is accessible to more people. Prevention and detection, particularly, are in the scope of management by a general medical practitioner [53]. The Oral Health Delivery Framework [54] delineates the role of a GP similarly to the referral care pathways created in our study. The strengths of our referral care pathways include their feasibility of implementation, as they do not need additional expertise, resources, or personnel. In addition, our pathways also promote care centralization, whereby patients are encouraged to maintain regular follow-ups with their GP after having received definitive management with an oral/dental specialist. However, challenges to implementation include the development of referral networks, particularly in rural settings, and ensuring that patients referred to a specialist can access one without unreasonable financial or geographic barriers.
5. Conclusions
In our study, we utilized the GRADE-ADOLOPMENT method to develop CPGs for three oral conditions: periodontitis, dental pain and intraoral swelling, and potentially malignant disorders in the mouth. Additionally, we formulated referral systems for the management of these oral diseases, outlining the role of GPs in diagnosis, basic management, and prompt referral. The integration of four specific recommendations focusing on risk factor counseling and cessation intervention has the potential to contribute to the reduction in the substantial burden of oral cancers in Pakistan. The widespread implementation of these CPGs and referral systems within Pakistan’s oral healthcare system holds the promise of alleviating the significant impact of oral diseases in the country.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/oral4030028/s1, Table S1: Criteria evaluated in the evidence to decision (ETD) tables; Table S2: Dummy evidence to decision (ETD) table; Table S3: Recommendations added or adopted with minor changes in the CPGs for potentially malignant disorders in the oral cavity; Table S4: Challenges faced and proposed solutions; Table S5: Malignant disorders in the oral cavity (table of recommendations); Table S6: Periodontitis (table of recommendations); Table S7: Antibiotic use for the urgent management of pulpal- and periapical-related dental pain and intraoral swelling (table of recommendations). References [35,45,46,47,55,56,57] are cited in the Supplementary Materials.
Author Contributions
Conceptualization, A.H.H., S.N., N.A.R. and S.M.R.K.; methodology, S.M.R.K., S.S.H., N.A.R., M.A.M., F.U., H.K.S., A.S., S.S.A. and A.A.R.; software, S.M.R.K., N.A.R., M.A.M., F.U., H.K.S., A.S., S.S.A., S.S.H. and A.A.R.; writing—original draft preparation, R.S.M., R.A. and A.P.; writing—review and editing, R.S.M., R.A. and A.P.; visualization, R.S.M. and A.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Due to the absence of participation of patients or other human subjects, we secured a waiver for ethical approval and informed consent from the Ethics Review Committee of the Aga Khan University. All procedures adhered to the utmost ethical standards as delineated in the 1964 Declaration of Helsinki and its subsequent amendments.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data used in the study are provided in the manuscript and the Supplementary Materials.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| AKU | Aga Khan University |
| CCBP | Center for Clinical Best Practices |
| CITRIC | Clinical and Translational Research Incubator |
| CPGs | Clinical practice guidelines |
| DOMS | Dental, Oral & Maxillofacial Surgery |
| EtD | Evidence to decision table |
| FGD | Focus group discussion |
| GP | General physician |
| GRADE | Grading of Recommendations, Assessment, Development, and Evaluation |
| LMIC | Lower-middle-income country |
| PDA | Pakistan Dental Association |
| ToR | Table of recommendations |
References
- WHO. Oral Health. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/oral-health (accessed on 15 January 2024).
- Bernabe, E.; Marcenes, W.; Hernandez, C.R.; Bailey, J.; Abreu, L.G.; Alipour, V.; Amini, S.; Arabloo, J.; Arefi, Z.; GBD 2017 Oral Disorders Collaborators; et al. Global, Regional, and National Levels and Trends in Burden of Oral Conditions from 1990 to 2017: A Systematic Analysis for the Global Burden of Disease 2017 Study. J. Dent. Res. 2020, 99, 362–373. [Google Scholar] [PubMed]
- Siddiqui, A.A.; Alshammary, F.; Mulla, M.; Al-Zubaidi, S.M.; Afroze, E.; Amin, J.; Amin, S.; Shaikh, S.; Madfa, A.A.; Alam, M.K. Prevalence of dental caries in Pakistan: A systematic review and meta-analysis. BMC Oral Health 2021, 21, 450. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F.; Bsc, M.F.B.; Me, J.F.; Soerjomataram, M.I.; et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Righolt, A.; Jevdjevic, M.; Marcenes, W.; Listl, S. Global-, regional-, and country-level economic impacts of dental diseases in 2015. J. Dent. Res. 2018, 97, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Gift, H.C.; Atchison, K.A. Oral health, health, and health-related quality of life. Med. Care 1995, 33, NS57–NS77. [Google Scholar] [CrossRef] [PubMed]
- Kisely, S. No Mental Health without Oral Health. Can. J. Psychiatry Rev. Can. Psychiatr. 2016, 61, 277–282. [Google Scholar] [CrossRef] [PubMed]
- ADA. Clinical Practice Guidelines and Dental Evidence. 2022. Available online: https://www.ada.org/resources/research/science-and-research-institute/evidence-based-dental-research (accessed on 15 January 2024).
- (NICE) NIfHaCE. Oral and Dental Health. 2022. Available online: https://www.nice.org.uk/guidance/conditions-and-diseases/oral-and-dental-health (accessed on 15 January 2024).
- (RCS) RCoSoE. Clinical Guidelines. 2022. Available online: https://www.rcseng.ac.uk/dental-faculties/fds/publications-guidelines/clinical-guidelines/ (accessed on 15 January 2024).
- Kravitz, A.; Bullock, A.; Cowpe, J.; Barnes, E. EU Manual of Dental Practice 2015; The Council of European Dentists: Cardiffy, UK, 2015. [Google Scholar]
- Kaur, H.; Gupta, B.M. Mapping of dental science research in India: A scientometric analysis of India’s research output, 1999–2008. Scientometrics 2010, 85, 361–376. [Google Scholar] [CrossRef]
- Schünemann, H.J.; Wiercioch, W.; Brozek, J.; Etxeandia-Ikobaltzeta, I.; Mustafa, R.A.; Manja, V.; Brignardello-Petersen, R.; Brignardello-Petersen, R.; Falavigna, M.; Falavigna, M.; et al. GRADE Evidence to Decision (EtD) frameworks for adoption, adaptation, and de novo development of trustworthy recommendations: GRADE-ADOLOPMENT. J. Clin. Epidemiol. 2017, 81, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Niaz, M.O.; Naseem, M.; Siddiqui, S.N.; Khurshid, Z. An outline of the oral health challenges in “Pakistani” population and a discussion of approaches to these challenges. JPDA 2013, 21, 1–8. [Google Scholar]
- Basharat, S.; Shaikh, B.T. Primary oral health care: A missing link in public health in Pakistan. East. Mediterr. Health J. La Rev. Sante La Mediterr. Orient.=Al-Majallah Al-Sihhiyah Li-Sharq Al-Mutawassit 2016, 22, 703–706. [Google Scholar] [CrossRef]
- Niaz, K.; Maqbool, F.; Khan, F.; Bahadar, H.; Ismail Hassan, F.; Abdollahi, M. Smokeless tobacco (paan and gutkha) consumption, prevalence, and contribution to oral cancer. Epidemiol. Health 2017, 39, e2017009. [Google Scholar] [CrossRef]
- Khan, S.A.; Dawani, N.; Bilal, S. Perceptions and myths regarding oral health care amongst strata of low socio economic community in Karachi, Pakistan. JPMA J. Pak. Med. Assoc. 2012, 62, 1198–1203. [Google Scholar] [PubMed]
- Hussain, P.; Anjum, Q.; Iqbal, Z. Oral Hygiene Awareness among the Patients visiting the Dental Centers of a Rural Area of the Province Punjab, Pakistan. Biomedica 2017, 33, 20. [Google Scholar]
- Basharat, S.; Shaikh, B.T.; Rashid, H.U.; Rashid, M. Health seeking behaviour, delayed presentation and its impact among oral cancer patients in Pakistan: A retrospective qualitative study. BMC Health Serv. Res. 2019, 19, 715. [Google Scholar]
- Qadir, S.A.; Shahzad, M.; Yousafzai, Y.M. Assessment of oral health related knowledge, attitude, and self-reported practices of families residing in Peshawar, Pakistan. Adv. Basic Med. Sci. 2019, 3, 54–58. [Google Scholar]
- Bernabé, E.; Masood, M.; Vujicic, M. The impact of out-of-pocket payments for dental care on household finances in low and middle income countries. BMC Public Health 2017, 17, 109. [Google Scholar] [CrossRef] [PubMed]
- Tugwell, P.; Knottnerus, J.A. Adolopment—A new term added to the Clinical Epidemiology Lexicon. J. Clin. Epidemiol. 2017, 81, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Andrews, J.C.; Schünemann, H.J.; Oxman, A.D.; Pottie, K.; Meerpohl, J.J.; Coello, P.A.; Rind, D.; Montori, V.M.; Brito, J.P.; Norris, S.; et al. GRADE guidelines: 15. Going from evidence to recommendation—Determinants of a recommendation’s direction and strength. J. Clin. Epidemiol. 2013, 66, 726–735. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Coello, P.; Oxman, A.D.; Moberg, J.; Brignardello-Petersen, R.; Akl, E.A.; Davoli, M.; Treweek, S.; Mustafa, R.A.; Vandvik, P.O.; Meerpohl, J.; et al. GRADE Evidence to Decision (EtD) frameworks: A systematic and transparent approach to making well informed healthcare choices. 2: Clinical practice guidelines. BMJ 2016, 353, i2089. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Coello, P.; Schünemann, H.J.; Moberg, J.; Brignardello-Petersen, R.; Akl, E.A.; Davoli, M.; Treweek, S.; Mustafa, R.A.; Vandvik, P.O.; Meerpohl, J.; et al. GRADE Evidence to Decision (EtD) frameworks: A systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ 2016, 353, i2016. [Google Scholar] [CrossRef] [PubMed]
- Junaidi, I. Ratio of dental surgeon versus population in Pakistan deplorable: PM’s aide. Dawn, 2 March 2021. [Google Scholar]
- Khan, A.A. Dentistry in Pakistan-Standing at the Crossroads Facing Numerous Challenges with an Uncertain Future. J. Pak. Dent. Assoc. 2018, 25, 1–2. [Google Scholar]
- Jawaid, S.A. Plight of Dentistry in Pakistan. Pak. J. Med. Sci. 2020, 36, 299–302. [Google Scholar] [CrossRef] [PubMed]
- Douglass, A.B.; Maier, R. Promoting Oral Health: The Family Physicians’ Role. Am. Fam. Physician 2008, 78, 814. [Google Scholar] [PubMed]
- (JPDA) JotPDA. About Pakistan Dental Association (PDA). 2016. Available online: https://archive.jpda.com.pk/about-us/ (accessed on 15 January 2024).
- Ali Shah, S.M.; Saquib, K.M.; Omer, S.A.; Mirza, D.; Ali, A. Awareness, knowledge & practice of evidence-based dentistry amongest dentists in Karachi. Pak. Oral Dent. J. 2015, 35, 265. [Google Scholar]
- Haq, I.U.; Rehman, Z.U. Medical Research in Pakistan; A Bibliometric Evaluation from 2001 to 2020. Libr. Philos. Pract. 2021, 1–13. [Google Scholar]
- Sanz, M.; Herrera, D.; Kebschull, M.; Chapple, I.; Jepsen, S.; Berglundh, T.; Sculean, A.; Tonetti, M.S.; On behalf of the EFP Workshop Participants and Methodological Consultants. Treatment of stage I–III periodontitis—The EFP S3 level clinical practice guideline. J. Clin. Periodontol. 2020, 47, 4–60. [Google Scholar] [CrossRef] [PubMed]
- Lockhart, P.B.; Tampi, M.P.; Abt, E.; Aminoshariae, A.; Durkin, M.J.; Fouad, A.F.; Gopal, P.; Hatten, B.W.; Kennedy, E.; Lang, M.S.; et al. Evidence- based clinical practice guideline on antibiotic use for the urgent management of pulpal-and periapical-related dental pain and intraoral swelling: A report from the American Dental Association. J. Am. Dent. Assoc. 2019, 150, 906–921.e12. [Google Scholar] [CrossRef] [PubMed]
- Lingen, M.W.; Abt, E.; Agrawal, N.; Chaturvedi, A.K.; Cohen, E.; D’Souza, G.; Gurenlian, J.; Kalmar, J.R.; Kerr, A.R.; Lambert, P.M.; et al. Evidence-based clinical practice guideline for the evaluation of potentially malignant disorders in the oral cavity: A report of the American Dental Association. J. Am. Dent. Assoc. 2017, 148, 712–727.e10. [Google Scholar] [CrossRef] [PubMed]
- Martins, R.S.; Masood, M.Q.; Mahmud, O.; Rizvi, N.A.; Sheikh, A.; Islam, N.; Khowaja, A.N.A.; Ram, N.; Furqan, S.; Mustafa, M.A.; et al. Adolopment of adult diabetes mellitus management guidelines for a Pakistani context: Methodology and challenges. Front. Endocrinol. 2022, 13, 1081361. [Google Scholar] [CrossRef] [PubMed]
- Saqib, M.A.N.; Rafique, I.; Qureshi, H.; Munir, M.A.; Bashir, R.; Arif, B.W.; Bhatti, K.; Ahmed, S.A.K.; Bhatti, L. Burden of tobacco in Pakistan: Findings from global adult tobacco survey 2014. Nicotine Tob. Res. 2018, 20, 1138–1143. [Google Scholar] [CrossRef] [PubMed]
- Musaddique Hussain, A.M.; Imran, I.; Rasool, M.F.; Hussain, I.; Barkat, Q.; Wu, X. Pakistan: Time for Stronger Enforcement on Tobacco Control. BMJ. Available online: https://blogs.bmj.com/tc/2019/12/12/pakistan-time-for-stronger-enforcement-on-tobacco-control/ (accessed on 1 August 2024).
- de Camargo Cancela, M.; Voti, L.; Guerra-Yi, M.; Chapuis, F.; Mazuir, M.; Curado, M.P. Oral cavity cancer in developed and in developing countries: Population-based incidence. Head Neck 2010, 32, 357–367. [Google Scholar] [CrossRef]
- Burki, S.J.; Pasha, A.; Pasha, H.; John, R.; Jha, P.; Baloch, A.; Kamboh, G.N.; Cherukupalli, R.; Chaloupka, F.J. The Economics of Tobacco and Tobacco Taxation in Pakistan; International Union against Tuberculosis and Lung Disease: Paris, France, 2013. [Google Scholar]
- Irfan, M.; Haque, A.S.; Awan, S.; Khan, J.A. Reasons of failure to quit smoking: A cross sectional survey in major cities of Pakistan. Eur. Respir. J. 2014, 44 (Suppl. S58), 4466. [Google Scholar]
- Shaheen, K.; Oyebode, O.; Masud, H. Experiences of young smokers in quitting smoking in twin cities of Pakistan: A phenomenological study. BMC Public Health 2018, 18, 466. [Google Scholar] [CrossRef] [PubMed]
- Martins, R.S.; Junaid, M.U.; Khan, M.S.; Aziz, N.; Fazal, Z.Z.; Umoodi, M.; Shah, F.; Khan, J.A. Factors motivating smoking cessation: A cross-sectional study in a lower-middle-income country. BMC Public Health 2021, 21, 1419. [Google Scholar] [CrossRef]
- Ghazal, P. The growing problem of alcoholism in Pakistan: An overview of current situation and treatment options. Int. J. Endors. Health Sci. Res. 2015, 3, 15–21. [Google Scholar]
- Taylor, M.; Dingle, J.J. Prevention of tobacco-caused disease. Can. Task Force Period. Health Exam. 1994, 500–511. Available online: https://canadiantaskforce.ca/wp-content/uploads/2016/09/1994-red-brick-en.pdf (accessed on 1 August 2024).
- National Institute for Health and Care Excellence (NICE). Tobacco: Preventing Uptake, Promoting Quitting and Treating Dependence; National Institute for Health and Care Excellence (NICE): London, UK, 2021. [Google Scholar]
- USPSTF. Tobacco Smoking Cessation in Adults, Including Pregnant Persons: Interventions; USPSTF: Washington, DC, USA, 2020; Available online: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions (accessed on 15 January 2024).
- Russell, M.A.; Merriman, R.; Stapleton, J.; Taylor, W. Effect of nicotine chewing gum as an adjunct to general practitioner’s advice against smoking. Br. Med. J. (Clin. Res. Ed.) 1983, 287, 1782–1785. [Google Scholar] [CrossRef][Green Version]
- Ashfaq Ahmed, S.H. Oral Health Care Systems Analysis in Pakistan: The Challenges Based on the WHO Building Blocks Framework and the Way Forward. Pak. J. Public Health 2015, 5, 8–11. [Google Scholar]
- Atchison, K.A.; Rozier, R.G.; Weintraub, J.A. Integration of Oral Health and Primary Care: Communication, Coordination and Referral. NAM Perspect. Available online: https://nam.edu/integration-of-oral-health-and-primary-care-communication-coordination-and-referral/ (accessed on 1 August 2024).
- Guan, G.; Lau, J.; Yew, V.; U, J.; Qu, W.; Lam, J.; Polonowita, A.; Mei, L. Referrals by general dental practitioners and medical practitioners to oral medicine specialists in New Zealand: A study to develop protocol guidelines. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2020, 130, 43–51.e5. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S. How do primary care doctors compare to dentists in the referral of oral cancer? Evid.-Based Dent. 2021, 22, 94–95. [Google Scholar] [CrossRef]
- Phillips, K.E.; Hummel, J. Oral Health in Primary Care: A Framework for Action. JDR Clin. Transl. Res. 2016, 1, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Hummel, J.; Phillips, K.; Holt, B.; Hayes, C. Oral Health: An Essential Component of Primary Care; Qualis Health: Seattle, WA, USA, 2015. [Google Scholar]
- GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University and Evidence Prime. 2024. Available online: https://www.gradepro.org (accessed on 1 August 2024).
- Griffiths, P. Evidence informing practice: Introducing the mini-review. Br. J. Community Nurs. 2002, 7, 38–39. [Google Scholar] [CrossRef] [PubMed]
- Rethman, M.P.; Carpenter, W.; Cohen, E.E.; Epstein, J.; Evans, C.A.; Flaitz, C.M.; Graham, F.J.; Hujoel, P.P.; Kalmar, J.R.; Koch, W.M.; et al. Evidence-based clinical recommendations regarding screening for oral squamous cell carcinomas. J. Am. Dent. Assoc. (1939) 2010, 141, 509–520. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).