1. Introduction
Odontogenic cysts (OCs) are common lesions in the maxillofacial region. They can develop from remnants of the odontogenic epithelium within the jaws. OCs can be categorized as developmental or inflammatory cysts based on their pathogenesis. Radicular cysts are the most prevalent among odontogenic inflammatory cysts, whereas residual cysts rarely occur [
1]. Residual cysts can develop from incomplete odontogenic cyst enucleation or incomplete tooth extractions, where remnants of a dental follicle or tooth root fragments are left behind. This type of cyst is frequently localized in the anterior maxilla [
1]. Residual cysts in the jaws are typically asymptomatic and are often discovered incidentally in an edentulous area. In cases of infection and growth of a cyst, pain, swelling, and tooth displacement occur. The nature and intensity of clinical manifestations vary according to the specific anatomical site of cyst formation [
2,
3]. Histopathological assessment, supplemented by imaging examinations, remains pivotal in diagnosing these lesions. Nevertheless, odontogenic cysts with extensive inflammation pose significant diagnostic difficulties, as inflammatory changes can mask typical cyst features. Depending on the duration of a cyst’s presence and the intensity of inflammatory processes, histopathological images can vary significantly and may include different elements. The thin epithelial lining of residual cysts complicates identification by histological examination. Residual cysts display clinical and pathological features similar to those of other lesions within the jaws, including other cysts, benign tumors, and even malignancies [
4,
5]. Moreover, they have the potential to remain unnoticed for extended periods and progressively damage surrounding bone and soft tissues, including the orbit, nasal cavity, and skull base. The proximity to the skull base is also a concerning factor. These cysts can grow covertly, reaching significant sizes. Nevertheless, radicular cysts, including residual ones, seldom lead to severe conditions beyond the deformation of surrounding bones and tissues. Life-threatening situations resulting from them have not been extensively described in the literature. Nonetheless, due to their locations, they are routinely removed.
Managing odontogenic inflammatory cysts involves surgical treatment, including removal through enucleation, marsupialization, curettage, and occasionally decompression to alleviate the cyst contents [
6,
7,
8]. Odontogenic cysts that extend into the maxillary sinus can be removed through functional endoscopic sinus surgery (FESS) [
9].
2. Case Report
A 67-year-old man was urgently admitted to the hospital due to severe bleeding from a tumor of the right maxilla. The tumor had been observed in his oral cavity by the patient for two months and had been noted for its progressive growth, accompanied by occasional minor bleeding. The patient reported no pain. The suspicious mass was subjected to biopsy by the oral surgery department without complications five days earlier.
The patient had a history of arterial hypertension, type II diabetes, hyperuricemia, gastritis, and alcoholic liver disease with esophageal varices. His dental history is unknown, as the patient did not have regular dental appointments. His daily medication regimen consisted of bisoprolol, ramipril, iron sulfate with vitamin C, folic acid, levomepromazine, omeprazole, and a combination of isophane and lispro insulin. The patient reported abstaining from alcohol for four years, had undergone a polypectomy for colonic polyps, and had cataract surgery two years prior.
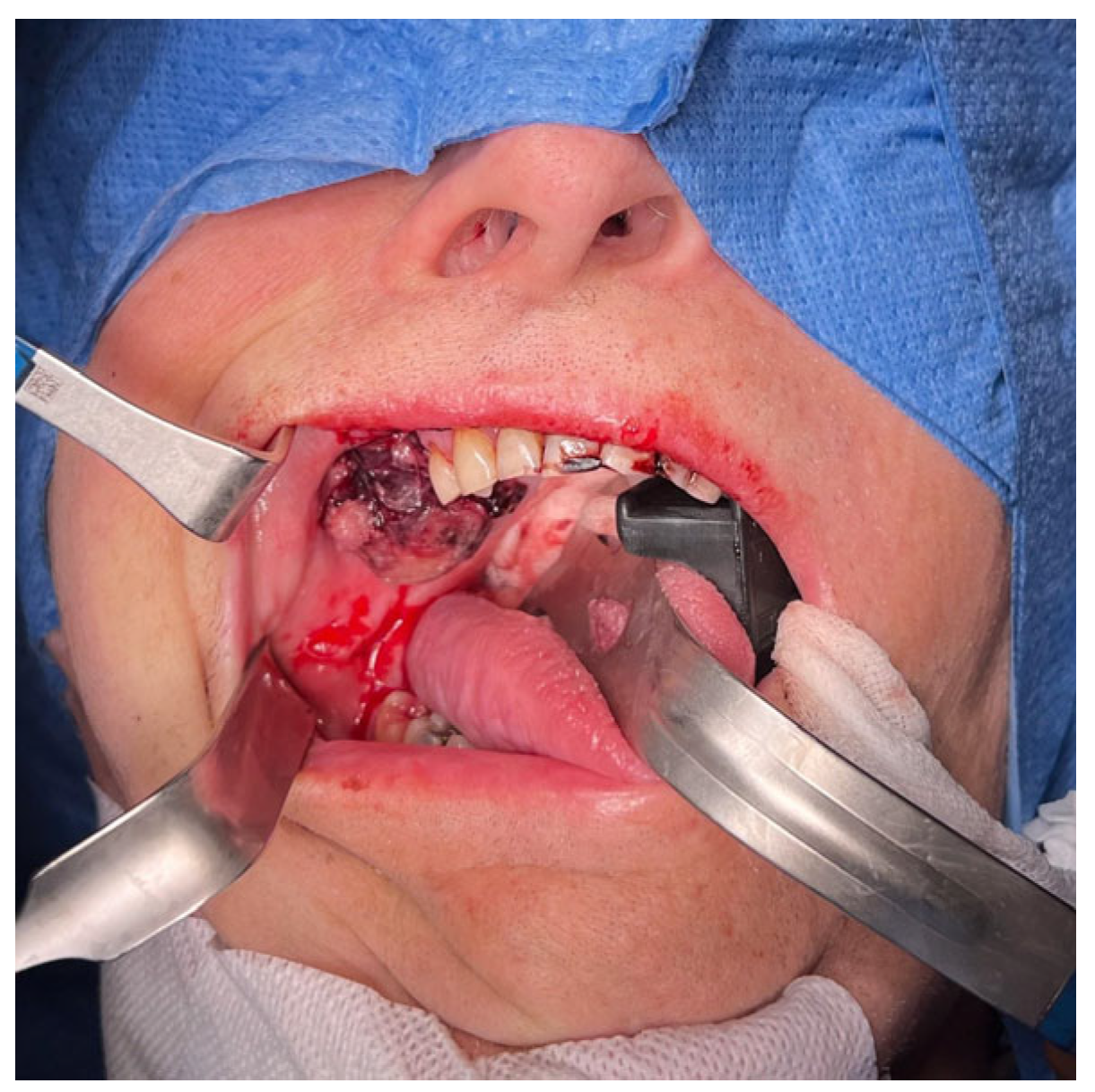
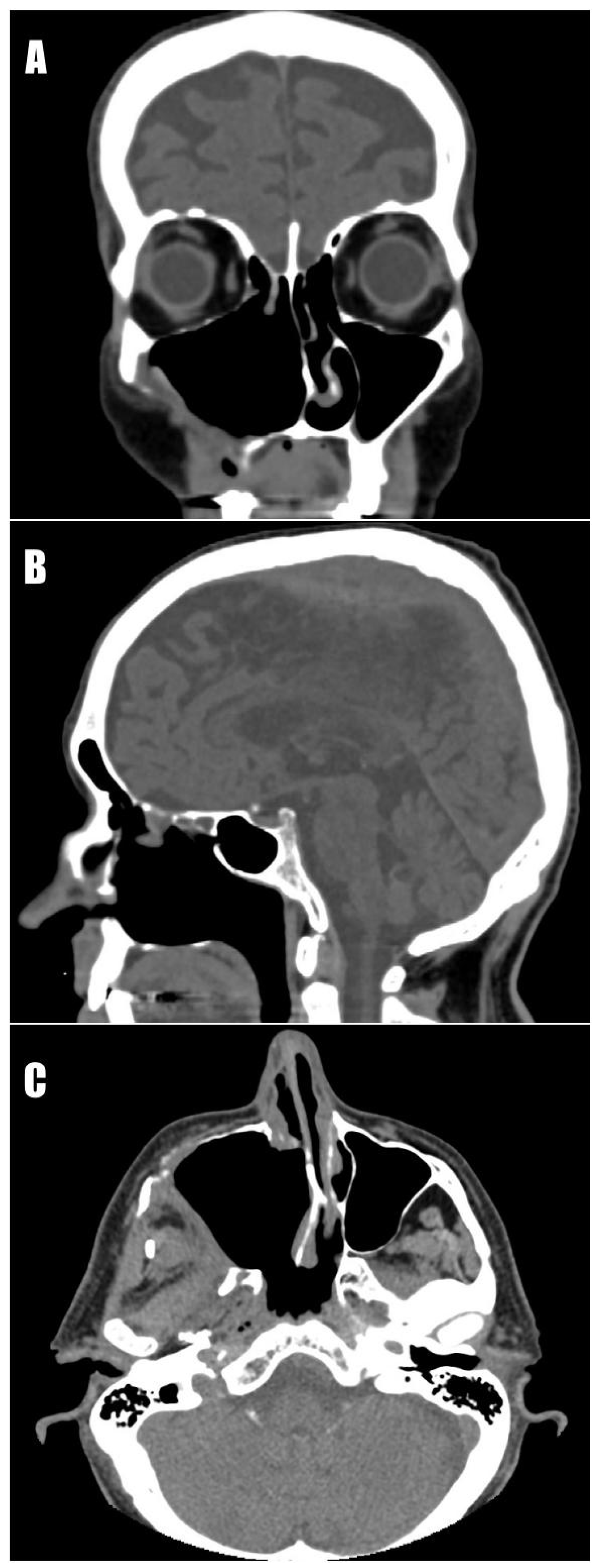
The mass was located near the alveolar process, in the region of missing teeth 14–18, and was expanding into the soft tissues of the cheek and maxillary sinus (
Figure 1). Upon physical examination, protrusion of the eyeball, narrowing of the right nasal passage, and asymmetry of the face were observed. Apart from changes within the maxillofacial area, ascites and ulceration on the left shin were noticed.
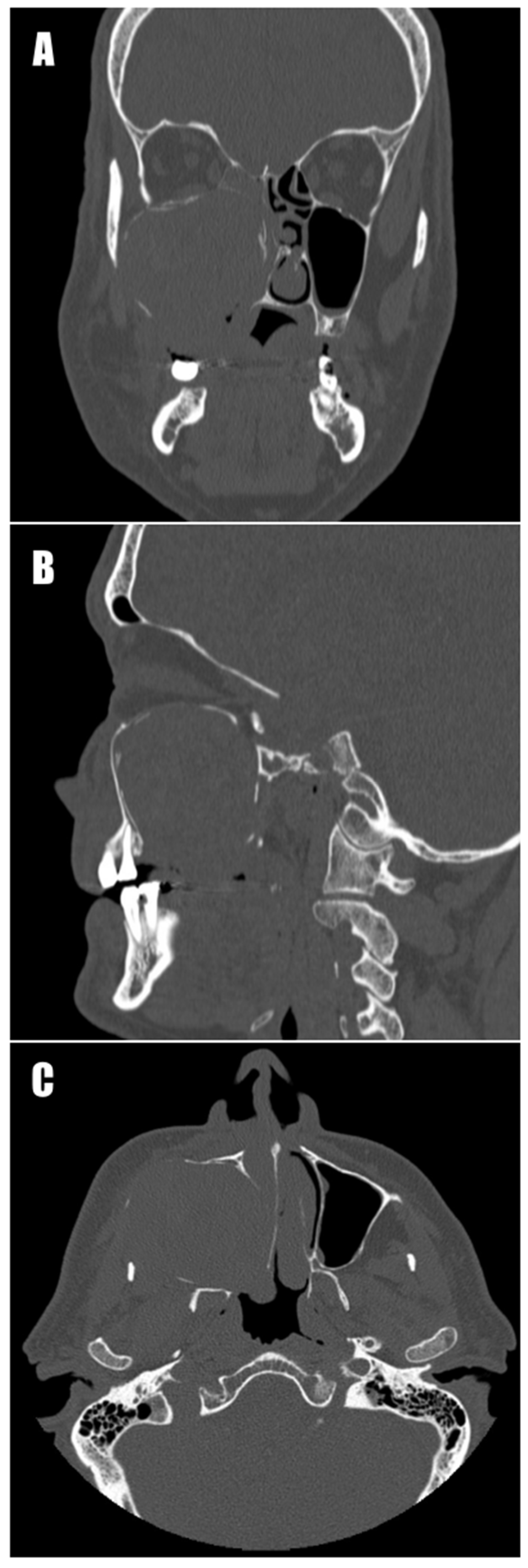
Due to suspicion of a neoplastic process, computed tomography (CT) of the head, neck, chest, abdominal cavity, and pelvis was performed. CT of the maxillofacial region revealed a pathological tissue mass (51 × 43 × 56 mm) with heterogeneous shadowing and hemorrhagic areas. It showed heterogeneous solid contrast enhancement, occupied the right maxillary sinus with an expansive growth pattern, and widened the sinus contours in every direction (
Figure 2). On the right side of the neck, enlarged lymph nodes of groups Ib (up to 12 mm on the short axis), IIa (up to 11 mm), and V (up to 10 mm) were observed. On the left side, lymph nodes were not present. Additionally, inflammatory mucosal changes within the ethmoid sinus and the ostium of the right frontal sinus were visualized. The increased density of the right parotid gland was noted, with possible inflammatory changes. In the differential diagnosis, invasive fungal infection; odontogenic cysts; and neoplastic processes, including malignant mesenchymal tumors, were considered [
10].
In the abdominal CT scan, the liver structure showed signs of cirrhotic remodeling with increased intensity compared to previous examinations. Features of portal hypertension were present, with dilation of the portal vein, inferior mesenteric vein, and splenic vein, along with significant splenomegaly and collateral circulation vessels around the spleen. Esophageal varices and a small amount of fluid in the peritoneal cavity were also present.
The initial histological examination conducted by the oral surgery department was inconclusive. The biopsied specimens ruled out malignant tumors and fungal infections, indicating that the mass primarily comprised granulation tissue and blood clots.
However, the patient’s overall condition deteriorated due to liver failure, resulting in severe bleeding from the lesion a few days after the incisional biopsy. Blood tests showed a drop in hemoglobin to 8.0 g/dL, a decrease in hematocrit to 24%, a reduction in erythrocyte count to 2.68 × 10
6 cells/µL, a decrease in platelet count to 95 × 10
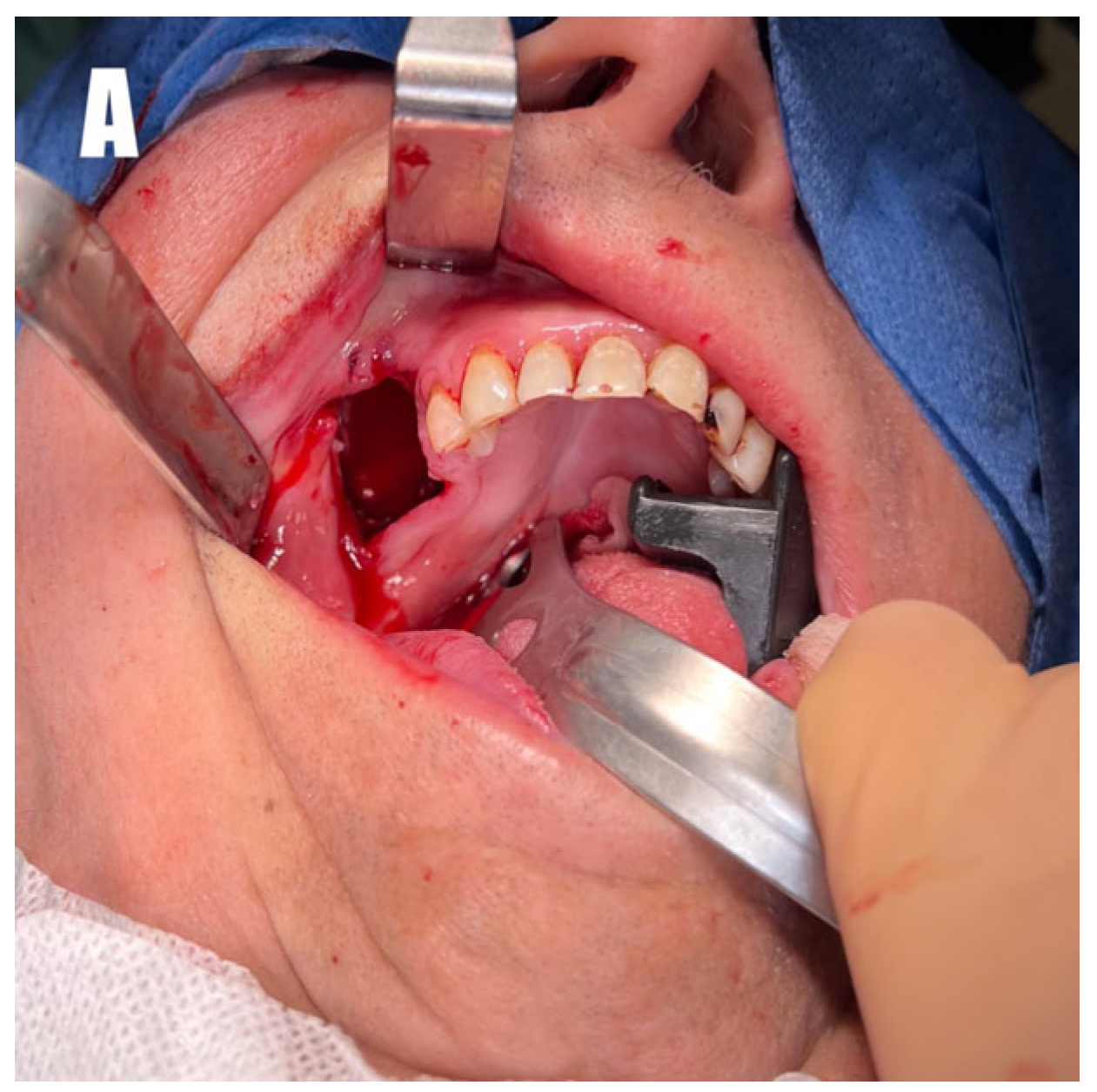
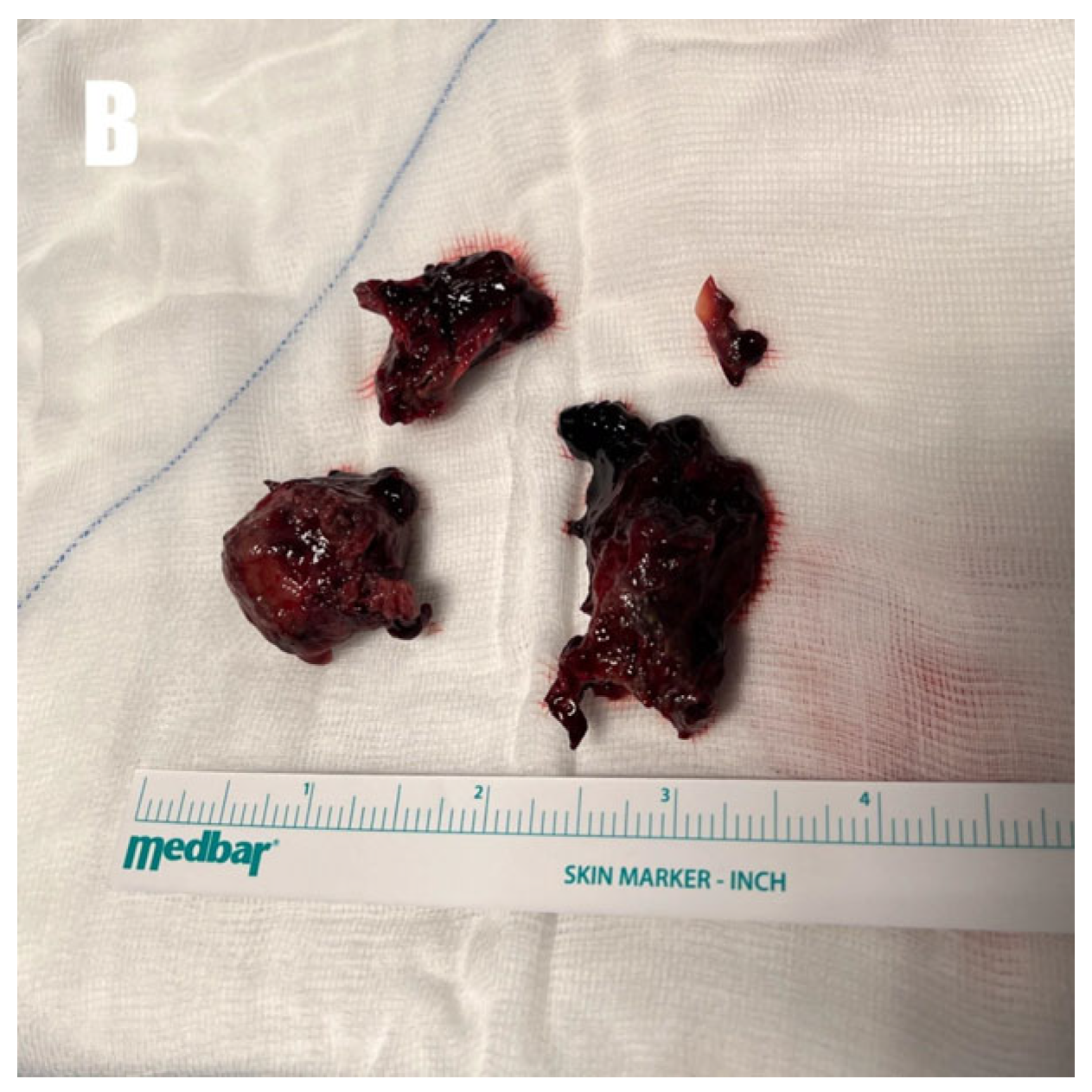
3/µL, and an RDW-CV of 14.8%. To manage his escalating breathing difficulties and the risk of upper airway obstruction, as well as to prevent complications from bleeding, several procedures were performed. These included ligations of the ipsilateral external carotid artery, tracheotomy, percutaneous endoscopic gastrostomy (PEG), and red blood cell transfusions. Intraoperatively, bleeding from the entire surface of the tumor with necrotic–hemorrhagic changes was identified. The tumor was easily removed through curettage due to the fragility of its structure, leaving pseudo-capsule remnants (
Figure 3). The residual masses were removed via functional endoscopic sinus surgery (FESS), with preservation of the floor of the right orbit. Within the cavity, individual spots with active bleeding were identified and coagulated. The medial wall of the maxilla was removed, creating a broad connection with the nasal cavity. The oroantral fistula was closed in two layers using Bichat’s fat pad and a trapezoidal mucoperiosteal flap. The material was sent for mycological, bacteriological, and histological examination.
The histological examination revealed fragments of connective tissue stroma, partially stroma covered by non-keratinizing stratified squamous epithelium and, in other regions, glandular epithelium characteristic of the upper respiratory tract. These fragments were associated with extensive hemorrhages and aggregations of nonspecific granulation tissue as well as numerous clusters of blood vessels, some with dilated lumens. Additionally, adjacent bone fragments were present with areas of thickened trabeculae intersected by bands of fibrous connective tissue, among which numerous blood vessels were also visible. Surrounding these vessels were rejuvenated, regenerating trabeculae and fragments of new bone. Chronic inflammation obscured the visualization of typical cystic features during the final histological examination, and hemangioma was suggested for the differential diagnosis. A follow-up computed tomography scan revealed complete removal of the tumor (
Figure 4). During further hospitalization, the patient developed secondary anemia, necessitating transfusion of another unit of red blood cell concentrate. Additionally, Clostridium perfringens was isolated from an ulceration on the patient’s left lower leg, requiring antibiotic treatment. This wound healed before the patient was discharged from the unit.
The healing process was uneventful. The patient regained respiratory efficiency, allowing for removal of the tracheostomy tube on the fourth day after the operation. However, it was decided to leave the PEG tube in place for patient nutrition. Before his discharge from the maxillofacial department, his blood morphology showed a hemoglobin level of 9.9 g/dL, hematocrit at 29.1%, MCH at 28.5 pg, MCV at 83.9 fL, MCHC at 34.0 g/dL, RDW-CV at 16.1%, and erythrocytes at 3.47 × 106/µL. His INR time was 1.21 s, his APTT was 35.3 s, and his prothrombin time was 13.6 s. His AST/ALT was within the normal range. His serum albumin level was 33.70 g/L, and his total protein was 64.3 g/L. After the surgical treatment, the patient was transferred directly to the Department of Internal Medicine and the Toxicology Department for further treatment. The patient died six months later due to liver failure.
3. Discussion
Inflammatory cysts are commonly encountered in the maxillofacial region. The estimated global prevalence of OCs is 11.62%, of which radicular cysts constitute as much as 54.26% [
11]. According to the fifth edition of the World Health Organization (WHO) Classification of Head and Neck Tumors published in 2022, residual cysts are categorized among radicular cysts [
12]. The term “residual cyst” primarily refers to a radicular cyst that persists after the associated tooth has been extracted. This implies that the frequency of residual cysts among all odontogenic cysts is relatively low [
3].
The clinical case presented here aligns with the essential diagnostic criteria outlined by the WHO classification, including an edentulous area for a residual cyst and the presence of non-keratinized stratified squamous lining epithelium. Additionally, the classification suggests that this type of cyst occurs more frequently in men, typically in the 4th to 5th decade of life, and is localized in the anterior maxillary sinus. These characteristics align with this clinical case, except for the patient’s age, as the described man was older. These cysts are generally asymptomatic and are detected incidentally during radiographic examinations. Still, long-standing cases may show acute exacerbation of the cystic lesion and develop signs and symptoms such as swelling, pain, tooth mobility, and displacement [
3].
In this case report, facial asymmetry was observed, yet the individual did not experience pain. Inflammatory cysts can destroy surrounding bone and soft tissues, leading to facial deformities, especially when they grow covertly for an extended period. The giant cyst caused extensive bone atrophy and soft tissue destruction in this clinical case. A residual cyst is distinguished from chronic inflammatory processes by its diverse characteristic features. Apart from specific lining epithelium, the literature has also described scattered mucous cells, calcifications, hyaline bodies, cholesterol clefts, dense fibrous connective tissue, and spicules of remodeling bone [
2,
13,
14]. The composition of the epithelial lining can vary depending on the age or developmental stage of the cyst, as well as the intensity of inflammation, which can complicate the diagnostic pathway [
2].
In this case, microscopic examination revealed a poorly expressed epithelial lining due to secondary inflammatory and hemorrhagic changes, with areas of fibrous connective tissue and spicules of remodeling bone. An atypical feature was the presence of numerous clusters of blood vessels, some with dilated lumens, with thrombi organizing within some of them, which are not characteristic of a cyst.
This case was also distinguished by the considerable cyst size and the development of a life-threatening hemorrhage from the lesion, necessitating other interventions. Occurrences of bleeding associated with a residual cyst are not documented in the literature. The likely key factors that triggered such intense bleeding from the cyst were progressive liver failure and the densification of the dilated small vessels within the cyst mass. Due to the rapid deterioration of the patient’s condition, aggressive and swift interventions were necessary, such as red blood cell transfusion due to blood loss, ligating the external carotid artery to reduce bleeding intensity, tracheotomy to secure the airways from complete obstruction, and percutaneous endoscopic gastrostomy when the patient was unable to ingest food orally. These measures, which were critical in managing immediate life-threatening situations, also emphasize the need for early detection and appropriate management of inflammatory cysts to prevent such acute exacerbations. Collaboration within the medical team and prompt, decisive actions in life-threatening situations were also essential.
Residual cysts are typically removed surgically. In the case of large cysts, gradual decompression followed by cystectomy may be considered [
15,
16]. However, in this patient’s case, due to the dynamic changes in the patient’s health status, timely curettage, combined with FESS surgery, resulted in the complete and safe removal of the residual cyst.
This paper underscores the critical importance of dental and medical preventive care, emphasizing that neglecting dental treatment, particularly in the context of deteriorating overall health, can result in fatal outcomes. The presented case demonstrates that a potentially benign and easily treatable condition, such as a residual cyst, can mimic an aggressive neoplasm and lead to an unfavorable outcome despite successful surgical intervention. If the patient had taken proper care of their health and attended regular dental check-ups, the lesion could have been detected and treated earlier.