Abstract
Dermal melanocytic disorders present as bluish pigmentation on the skin. Several entities including Mongolian spot, aberrant Mongolian spot, nevus of Ota, and nevus of Ito have been reported. It is often difficult to distinguish between the different entities from their overlapping features. Although they share similar etiologies and histologic findings, their co-morbidities and prognosis differ. In this paper, we report four cases of dermal melanocytic disorders of which we were not able to make a clear-cut diagnosis. Also, we briefly review the dermal melanocytic disorders.
1. Introduction
Dermal melanocytic disorders present with blue to gray pigmentation and are prevalent in Asians. There are several clinical entities that include the Mongolian spot, aberrant Mongolian spot, nevus of Ota, and nevus of Ito. They share a common histopathological finding (i.e., melanocytes in the dermis), but their prognoses differ. A typical Mongolian spot is present on the coccygeosacral area and usually disappears within the first decade, whereas the aberrant Mongolian spot, nevus of Ota, and nevus of Ito tend to persist and at times even have a potential for malignant transformation [1,2]. Therefore, a proper diagnosis is crucial in managing dermal melanocytosis. At times, however, it is difficult to pinpoint a diagnosis if the lesion has overlapping features. In this paper, we share four cases of dermal melanocytic disorders with mixed features.
2. Cases
2.1. Case 1: Bilateral Nevus of Ota or Aberrant Mongolian Spot
A 16-month-old Korea male presented with asymptomatic blue patches on the right forehead, both temporal areas and cheeks which have been present since birth (Figure 1a–c). His right sclera was also involved. The patient had no family history of pigment disorders, and his physical and mental development was normal. A skin biopsy from the lesion showed increased melanocytes in the dermis that were positive to S-100 stain (Figure 1d,e). Based on the findings, we made a diagnosis of bilateral nevus of Ota with a differential diagnosis of aberrant Mongolian spot. The patient underwent a single session of Q-switched neodymium yttrium aluminum garnet (Nd:YAG) laser treatment and is currently lost for follow-up.
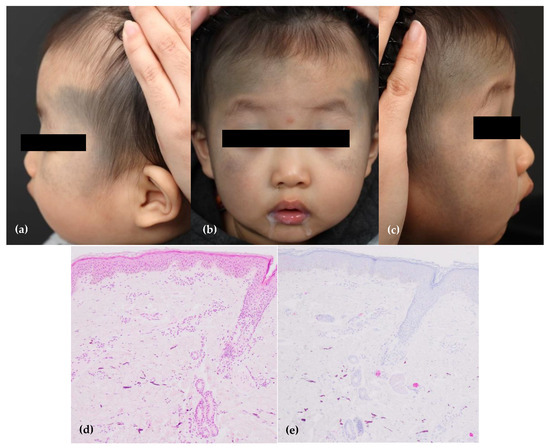
Figure 1.
A patient with either the bilateral nevus of Ota or the aberrant Mongolian spot. (a–c) Dermal melanocytosis on the face. (d,e) The melanocytes are positive for S-100 (×40).
2.2. Case 2: Nevus of Ito or Aberrant Mongolian Spot
A 5-month-old Korean male presented with congenital blue patches on the right anterior supraclavicular area (Figure 2a–c). There was also a similar blue patch on his coccyx suggestive of a Mongolian spot. He did not have any other medical or dermatologic problems. Histopathological findings showed dendritic melanocytes in the dermis (Figure 2d). Immunohistochemical analysis showed melanin pigments that were positive to Fontana-Masson staining (Figure 2e). He was diagnosed with the nevus of Ito, with aberrant Mongolian spot as a differential diagnosis for his supraclavicular lesion.
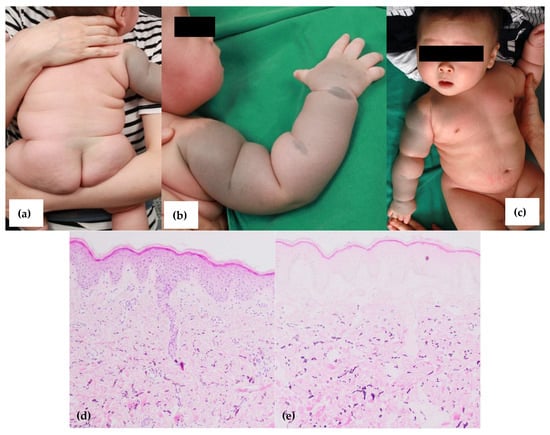
Figure 2.
A patient with either the nevus of Ito or the aberrant Mongolian spot. (a–c) Dermal melanocytoses on the right anterior on the right anterior supraclavicular and coccygeal areas. (d,e) The melanin pigments are positive with the Fontana-Masson stain (×40).
2.3. Case 3: Aberrant Mongolian Spot or Nevus of Ota with Co-Existing Congenital Melanocytic Nevus and Hemangioma
A 1-month-old Korean female presented with a blue patch on the right side of the forehead since birth (Figure 3a). The patient also had a solitary round red nodule on the middle of her forehead and brown hairy patch on the occiput, each suggestive of an infantile hemangioma and congenital melanocytic nevus (Figure 3b,c). The sclerae was not involved. These skin problems were congenital, and not associated with any other medical or dermatologic problems. A skin biopsy was recommended, but refused. A clinical diagnosis of an aberrant Mongolian spot or the nevus of Ota was made. She was treated with a pulsed dye laser for the hemangioma several times, but the blue patch was left untreated. During the treatment period (i.e., 8 months), the blue patch was followed up on regularly; the size of the lesion increased as the patient grew, but the color did not dramatically darken or fade.
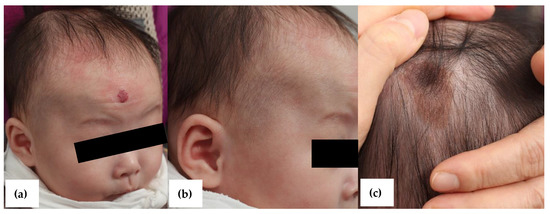
Figure 3.
A patient with either the aberrant Mongolian spot or the nevus of Ota. (a,b) Dermal melanocytosis on the right side of face and infantile hemangioma on the forehead. (c) Congenital melanocytic nevus on the occiput.
2.4. Case 4: Nevus of Ito or Aberrant Mongolian Spot
A 15-month-old Korean female patient presented with dark blue patches on the posterior neck, right shoulder, and upper arm since birth (Figure 4a,b). The patient denied any other medical or dermatologic problems. Histopathologic findings from the shoulder showed increased basal pigment in the epidermis and melanocytes in the dermis (Figure 4c,d). She was diagnosed with the nevus of Ito with a differential diagnosis of aberrant Mongolian spot and underwent treatment with the Q-switched Nd:YAG laser. After 14 sessions of treatment, the lesion showed marked improvement (Figure 4e,f).
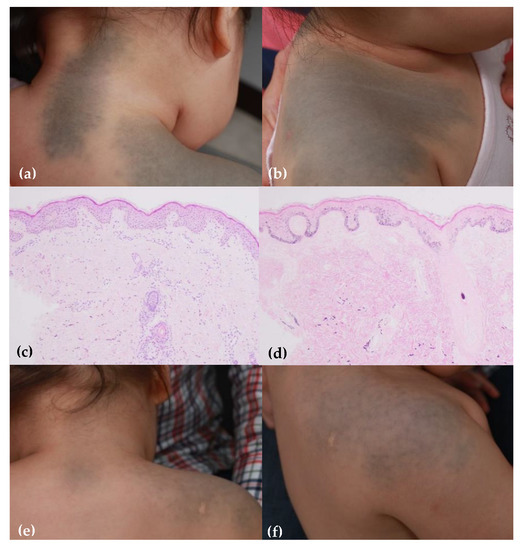
Figure 4.
A patient with either the nevus of Ito or the aberrant Mongolian spot. (a,b) Dermal melanocytosis on the posterior neck, right shoulder, and upper arm. (c,d) After 14 sessions of Q-switched Nd:YAG laser treatment. (e) The lesion shows dendritic melanocytes in dermis (H&E stain, ×40). (f) The melanin pigments are positive for Fontana-Masson stain (×40).
3. Discussion
3.1. Mongolian Spot and Aberrant Mongolian Spot
The Mongolian spot is a congenital blue patch located on the coccygeosacral area. The aberrant Mongolian spot, also known as an extrasacral Mongolian spot, is a congenital blue patch that occurs on aberrant sites such as the back, shoulder, extremities, and face. Although the Mongolian spot usually fades and disappears during the first few years of life, the aberrant Mongolian spot tends to persist [1]. The etiology of both the Mongolian and aberrant Mongolian spot involves failure of migration of dermal melanocytes to the epidermis and their delayed disappearance from the dermal layer. The gray-blue color of the lesion results from the Tyndall effect, a phenomenon where light is scattered by particles of matter in its path.
Both the Mongolian and aberrant Mongolian spots are common in Asians and Africans, but are rare in Caucasians. The Mongolian spot has been reported to be seen in 100% of Asian children, 96% of black children, 46% of Hispanic children, and 9.5% of Caucasian children [3]. The racial differences are explained by the differences in the number of melanocytes, rates of completely melanized melnosomes, and duration of dermal melanocyte production [4]. The prevalence of the aberrant Mongolian spot is not studied well compared to the Mongolian spot, but according to a study from India, the prevalence of the aberrant Mongolian spot was found to be one fourth of that of the Mongolian spot [1]. The relative prevalence of the aberrant Mongolian spot is expected to vary between different races and needs to be investigated further.
Sites of involvements of the aberrant Mongolian spot vary from the head and neck to the lower extremities. Although the commonly involved sites differ from study to study, the back and the limbs were more common than the head and neck [5,6,7]. Diagnosing an aberrant Mongolian spot is sometimes difficult due to its presence on various body sites, whereas the Mongolian spot is comparatively easy to diagnose with its fixed location on the sacral area and fading nature. The differential diagnosis of an aberrant Mongolian spot includes the nevus of Ota and Ito, and their characteristics are summarized in Table 1.

Table 1.
Differential diagnosis of dermal melanocytic disorders.
Patients who have dermal melanocytic disorders such as the Mongolian spot and the aberrant Mongolian spot along with certain vascular lesions are diagnosed with phacomatosis pigmentovascularis (PPV). PPV is defined as an association of a widespread vascular nevus with an extensive pigmentary nevus and is thought of as an embryogenic anomaly affecting the vasomotor nerves and the melanocytes, both of which are derived from neural crest [8]. If a blue spot co-exists with nevus flammeus, diagnosis of PPV type II or phacomatosis cesioflammea is made. If a blue spot co-exists with cutis marmorata telangiectatica congenita, it is called PPV type V or phacomatosis cesiomarmorata. The blue spot can also include the nevus of Ota and nevus of Ito.
The association with inborn error of metabolism such as the Hunter’s syndrome and GM1 gangliosidosis have also been reported with an aberrant Mongolian spot and in patients with extensive Mongolian spots [9,10]. The relationship between these diseases arouses new interest on the comorbidities of the Mongolian and aberrant Mongolian spots.
As mentioned earlier, Mongolian spot naturally fades while the aberrant Mongolian spot tends to persist. Hence it is necessary to consider early active intervention on the aberrant Mongolian spot using pigment lasers (i.e., Q-switched lasers) to reduce the psychological stress that the patients may receive as they grow. Previous studies about the Q-switched alexandrite laser and ruby laser showed that children tend to show better results and less post-inflammatory hyperpigmentation than adults due to the nature of their skin (i.e., thinner and less pigmented) [11]. It has also been shown that the Q-switched laser is more effective in aberrant Mongolian spots on exposed areas compared to those on non-exposed sites [12]. The result is related to the fact that the skin of the exposed region is thinner and the size of the lesion on the exposed site is usually smaller compared to that on non-exposed areas.
3.2. Nevus of Ota
The nevus of Ota was first described by Ota in 1939 and shows a bluish pigmentation in the areas innervated by the first two branches of the trigeminal nerve [13]. The nevus of Ota is subclassified into four types: Type 1 (mild: periocular area, zygomatic area, forehead, or nose), Type 2 (moderate: similar to Type 1 but worse), Type 3 (intensive: periocular, nose, and scalp), and Type 4 (bilateral). As can be seen from the classification, bilateral cases are rarely seen (i.e., 5–10% of all patients). Whereas the nasolabial fold is not involved, the sclera is affected in two-thirds of the patients, and patients have an increased risk of glaucoma and uveal melanoma.
Histologically, the nevus of Ota shows evenly spread spindle-shaped or dendritic melanocytes scattered throughout the dermis within undisturbed collagen bundles. The melanocytes are more superficially located compared to that of the Mongolian spot, which are usually found in the deeper dermis.
The nevus of Ota is mostly sporadic and familial cases are rarely reported. Although it can occur in all races, the Asian population is most commonly affected, with a prevalence of 0.01~0.6% and with female dominance [14,15]. The exact etiology is unknown, but the failure of melanocyte to migrate from neural crest cells to the basal layer of the epidermis is thought to be a cause like other dermal melanocytosis.
Several studies have looked into the relation between the nevus of Ota and malignancy. Although the nevus of Ota rarely undergoes malignant transformation, when it occurs, it usually present as a melanoma of the uveal tract, orbit, and meninges. Uveal melanoma has been reported in 0.25% of the patients with the nevus of Ota [14]. Activating guanine nucleotide-binding protein G(q) subunit alpha (GNAQ) or G protein subunit alpha 11 (GNAQ) mutation, which behaves similar to oncogenes, are observed in 6–15% of the nevus of Ota and 46–85% in uveal melanoma patients, suggesting their association [16,17]. Homozygous loss of BAP1, located on the chromosome 3p21.1 locus, contributes to the progression for metastatic change in uveal melanoma [17]. Although rare, cutaneous melanoma may develop from the nevus lesion itself, and in this case, newly developed rapidly growing nodule within a lesion is observed.
Although treatment is not necessary for the nevus of Ota, active intervention is often needed because of its location (i.e., face) and persistent nature, which can cause psychological stress. Q-switched lasers including ruby, alexandrite, and Nd:YAG treatment showed acceptable results in many cases [18]. Better results were obtained in younger patients and lighter lesions compared to adult patients and darker patches [19]. A regular follow up by an ophthalmologist is required to check the presence of glaucoma or melanoma.
3.3. Nevus of Ito
The nevus of Ito was first described by Ito in 1954 as blue patches on the posterior supraclavicular area, a region innervated by the acromioclavicular nerve. The nevus of Ito is less common than the nevus of Ota, and although the exact prevalence is unknown, it is considered to be more common in the Asian population and in females. The nevus of Ota and Ito rarely occur together [20,21].
Similar to other dermal melanocytosis, the nevus of Ito is thought to be a result of migration failure of melanocytes to the epidermis. The histopathologic findings are also similar to the nevus of Ota, which is superficial dermal proliferation of dendritic melanocytes. Similarly, this may be the differential point between the nevus of Ito and the aberrant Mongolian spot.
Although most dermal melanocytic disorders show a benign course, rare cases of malignant transformation have been reported. One study identified 13 reported cases of primary cutaneous melanoma arising in dermal melanocytoses [22]. Among those cases, 3 cases developed from the nevus of Ito, while the other 10 cases were from the nevi of Ota. Again, alterations in the GNAQ and BAP1 genes are thought to be involved in the malignant transformation of the nevus of Ito [22,23].
The nevus of Ito is also persistent, but treatment is not mandatory because of its benign nature. If a patient seeks active intervention for cosmetic purpose, pigment lasers (i.e., Q-switched lasers) are frequently used as in the other dermal melanocytosis with satisfactory results [18]. Interestingly, in a study using Q-switched alexandrite laser, the treatment response of the nevus of Ito was reported to be lower than that of the nevus of Ota (response rates were 25% and 92%, respectively) [23].
3.4. Discussion on Our Cases
As in our cases, an accurate diagnosis does not seem to be always possible. In Case 1, the nevus of Ota was considered because the blue patch were observed on the periocular area and sclera, however, the skin biopsy revealed that the melanocytes increased mainly in the deeper dermis, so the authors could not rule out the aberrant Mongolian spot. In Case 2, similarly, the skin lesions on the scapular area could be considered as the nevus of Ito, but the entire right arm was involved, and the increased dendritic melanocytes were observed in the mid and deep dermis showing the features of the aberrant Mongolian spot. In Case 3, the patient presented a blue patch on her unilateral forehead similar to the nevus of Ota, but the distribution was not characteristic, and the skin specimen was not obtained, thus no further diagnosis could be made. In Case 4, the blue patches on the scapular area resembled the nevus of Ito, but the posterior neck was also involved and the skin biopsy showed that the melanocytes were increased in the deep dermis as in that of the aberrant Mongolian spot.
4. Conclusions
Dermal melanocytic disorders are grey to blue patches, which are usually seen in Asians. The key characteristics of dermal melanocytic disorders mentioned in this paper are summarized in Table 1. Except for the typical Mongolian spot, other dermal melanocytosis are presented on the exposed areas and tend to persist longer, and therefore can cause serious psychological stress on patients. Since active treatment is associated with a better outcome in children than adults, an accurate diagnosis is important, which can be hard at times due to the overlapping features.
Author Contributions
Conceptualization, H.-S.K.; methodology, Y.H.; validation, S.-H.C., J.-D.L. and Y.-R.W.; formal analysis, Y.H.; investigation, Y.H. and S.-H.L.; resources, M.C.; data curation, Y.H.; writing—original draft preparation, Y.H.; writing—review and editing, Y.-R.W. and H.-S.K.; visualization, Y.H.; supervision, H.-S.K.; project administration, M.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Incheon St. Mary’s hospital, Incheon, South Korea (OC21RASI0056, 11 June 2021).
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Gupta, D.; Thappa, D.M. Mongolian Spots-A Prospective Study. Pediatric Dermatol. 2013, 30, 683–688. [Google Scholar] [CrossRef]
- Agarwal, P.; Patel, B.C. Nevus of Ota and Ito. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Cordova, A. The Mongolian spot: A study of ethnic differences and a literature review. Clin. Pediatrics 1981, 20, 714–719. [Google Scholar] [CrossRef]
- Kikuchi, I. What is a Mongolian spot? Int. J. Dermatol. 1982, 21, 131–133. [Google Scholar] [CrossRef] [PubMed]
- Egemen, A.; Ikizoğlu, T.; Ergör, S.; Asar, G.M.; Yilmaz, O. Frequency and characteristics of mongolian spots among Turkish children in Aegean region. Turk. J. Pediatrics 2006, 48, 232–236. [Google Scholar]
- Reza, A.M.; Farahnaz, G.Z.; Hamideh, S.; SeyedAlinaghi, S.; Saeed, Z.; Mostafa, H. Incidence of Mongolian Spots and its Common Sites at Two University Hospitals in Tehran, Iran. Pediatric Dermatol. 2010, 27, 397–398. [Google Scholar] [CrossRef] [PubMed]
- Leung, A.K.C. Mongolian Spots in Chinese Children. Int. J. Dermatol. 1988, 27, 106–108. [Google Scholar] [CrossRef] [PubMed]
- Happle, R. Phacomatosis Pigmentovascularis Revisited and Reclassified. Arch. Dermatol. 2005, 141, 385–388. [Google Scholar] [CrossRef]
- Ochiai, T.; Suzuki, Y.; Kato, T.; Shichino, H.; Chin, M.; Mugishima, H.; Orii, T. Natural history of extensive Mongolian spots in mucopolysaccharidosis type II (Hunter syndrome): A survey among 52 Japanese patients. J. Eur. Acad. Dermatol. Venereol. 2007, 21, 1082–1085. [Google Scholar] [CrossRef]
- Su, F.; Li, F.; Jin, H.-Z. Extensive Mongolian spots in a child with mucolipidosis II. Int. J. Dermatol. 2010, 49, 438–440. [Google Scholar] [CrossRef]
- Kagami, S.; Asahina, A.; Watanabe, R.; Mimura, Y.; Shirai, A.; Hattori, N.; Watanabe, T.; Tamaki, K. Laser treatment of 26 Japanese patients with Mongolian spots. Dermatol. Surg. 2008, 34, 1689–1694. [Google Scholar]
- Shirakawa, M.; Ozawa, T.; Ohasi, N.; Ishii, M.; Harada, T. Comparison of regional efficacy and complications in the treatment of aberrant Mongolian spots with the Q-switched ruby laser. J. Cosmet. Laser Ther. 2010, 12, 138–142. [Google Scholar] [CrossRef]
- Ota, M. Naevus fusco-caeruleus ophthalmo-maxillaris. Jpn. J. Dermatol. 1939, 46, 360. [Google Scholar]
- Ho, S.G.; Chan, H.H. The Asian dermatologic patient: Review of common pigmentary disorders and cutaneous diseases. Am. J. Clin. Dermatol. 2009, 10, 153–168. [Google Scholar] [CrossRef] [PubMed]
- Van Raamsdonk, C.D.; Bezrookove, V.; Green, G.; Bauer, J.; Gaugler, L.; O’Brien, J.M.; Simpson, E.M.; Barsh, G.S.; Bastian, B.C. Frequent somatic mutations of GNAQ in uveal melanoma and blue naevi. Nature 2009, 457, 599–602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Konstantinov, N.K.; Berry, T.M.; Elwood, H.R.; Zlotoff, B.J. Nevus of Ota associated with a primary uveal melanoma and intracranial melanoma metastasis. Cutis 2018, 102, E2–E4. [Google Scholar] [PubMed]
- Polder, K.D.; Landau, J.M.; Vergilis-Kalner, I.J.; Goldberg, L.H.; Friedman, P.M.; Bruce, S. Laser Eradication of Pigmented Lesions: A Review. Dermatol. Surg. 2011, 37, 572–595. [Google Scholar] [CrossRef]
- Sami, L.; Changzheng, H.; Yan, L. Factors affecting response, number of laser sessions and complications in nevus of Ota treated by Q-switched alexandrite laser: A retrospective study. G Ital. Dermatol. Venereol. 2015, 151, 160–168. [Google Scholar]
- Dekio, S.; Koike, S.; Jidoi, J. Nevus of ota with nevus of Ito—Report of a case with cataract. J. Dermatol. 1989, 16, 164–166. [Google Scholar] [CrossRef]
- Kumar, M.A. Nevus Ota associated with nevus of Ito. Indian J. Dermatol. Venereol. Leprol. 2004, 70, 112–113. [Google Scholar]
- Tse, J.Y.; Walls, B.E.; Pomerantz, H.; Yoon, C.H.; Buchbinder, E.I.; Werchniak, A.E.; Dong, F.; Lian, C.G.; Granter, S.R. Melanoma arising in a nevus of Ito: Novel genetic mutations and a review of the literature on cutaneous malignant transformation of dermal melanocytosis. J. Cutan. Pathol. 2015, 43, 57–63. [Google Scholar] [CrossRef]
- Yeh, I.; Mully, T.W.; Wiesner, T.; Vemula, S.S.; Mirza, S.A.; Sparatta, A.J.; McCalmont, T.H.; Bastian, B.; LeBoit, P.E. Ambiguous Melanocytic Tumors with Loss of 3p21. Am. J. Surg. Pathol. 2014, 38, 1088–1095. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.W.; Wang, J.B.; Liu, Y.H.; Zuo, Y.G.; Jin, H.Z.; Jiang, G.T.; Li, H.C.; Ma, D.L. Clinical efficacy of Q-switched Alexandrite laser for pigmentary skin diseases in 4656 patients. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 2006, 28, 202–205. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).