Abstract
Klippel-Trenaunay syndrome (KTS) is a rare complex vascular syndrome with limb hypertrophy. KTS is diagnosed if at least two of the three features of capillary malformation, venous malformation, and soft tissue and/or bone overgrowth are present. Of these, capillary malformation (i.e., port-wine stain) is the most commonly observed feature but may be absent in atypical KTS. We herein report a case of atypical KTS with venous malformation and unilateral soft tissue hypertrophy.
1. Introduction
Klippel-Trenaunay Syndrome (KTS) is a rare congenital disease characterized by a combination of capillary-lymphatic-venous malformation and limb hypertrophy [1]. The triad includes capillary malformation (i.e., port-wine stain), venous malformation, and hypertrophy of soft tissue and/or bone. KTS can be diagnosed if at least two of the three features are present. About two thirds of patients present all three features and the remaining one third satisfy two features [2]. Port-wine stain is the most common manifestation of KTS and is observed in about 98% of patients. Thus, KTS patients without capillary malformation are very rare and such cases are termed atypical KTS. Herein, we introduce a case of an atypical KTS patient.
2. Case
A 17-year-old girl presented with unilateral hypertrophy of the right lower limb and the lower back with tumefactions of 7.0 cm to 25.0 cm long, composed of grouped blue blebs (Figure 1). The lesion was present since birth and gradually increased in size. She was taking iron supplements for persistent asymptomatic iron deficiency anemia. Otherwise, no systemic or developmental defect was noted. Results of abdomen and pelvis computed tomography (CT) showed extensive unilateral soft tissue masses with macrocalcifications along the intramuscular and subcutaneous regions of the right lower back, buttock, and the anterolateral portion of the proximal thigh (Figure 2). Venous malformations and splenomegaly with multiple small vascular malformations were also noted. Endoscopy revealed nodular gastritis and colonoscopy showed normal findings. From the findings, a diagnosis of atypical KTS was made.
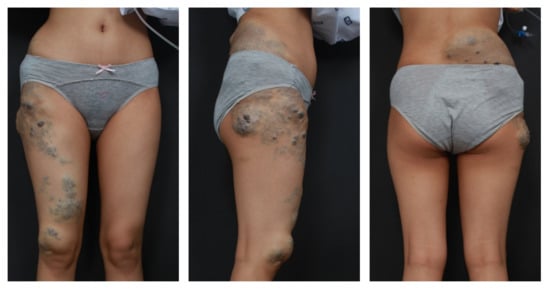
Figure 1.
The unilateral hypertrophy of the right lateral thigh and lower back with grouped blue blebs supports a diagnosis of Klippel-Trenaunay syndrome in spite of the absence of capillary malformations.
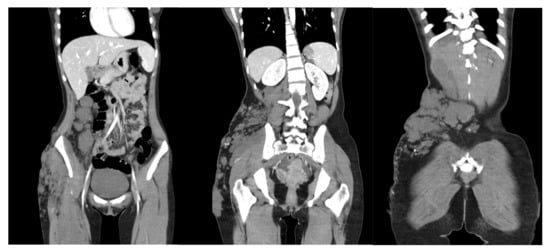
Figure 2.
Abdominal and pelvic CT shows unilateral soft tissue hypertrophy with calcifications on the right side of the lower abdomen, lower back, buttock, and proximal thigh. Venous malformation in the right gluteal muscle and splenomegaly with multiple small vascular malformations were observed.
3. Discussion
KTS is a rare disorder of capillary-lymphatic-venous malformation with limb hypertrophy [1]. It was first described in 1900 by two French physicians, Klippel and Trenaunay, with two patients who had port-wine stains, varicose veins, and bony and soft tissue hypertrophy [3]. The etiology of KTS is not well known. KTS is generally sporadic but familial cases have been reported [4]. The overall estimated incidence is about 2–5/100,000 without sex predilection.
The clinical manifestation of KTS includes a triad of capillary malformation (e.g., port-wine stain or nevus flammeus), atypical varicose vein or venous malformation, and soft tissue or bony hypertrophy of the extremities. KTS can be diagnosed when two of the three features are present. Imaging, including computed tomography (CT), magnetic resonance imaging (MRI), venography, and ultrasonography, helps diagnose and evaluate the severity of the disease. KTS patients with arteriovenous fistula had been diagnosed with Klippel-Trenaunay-Weber syndrome in the past, which is essentially misleading as the current consensus uses two different names to denote two different syndromes. Parkes Weber syndrome is characterized by arteriovenous fistulae and lesser musculoskeletal involvement with no marginal vein or lymphatic malformation, which is a distinguishable aspect of KTS [1]. As our patient presented with a clinically indefinite soft tissue hypertrophy, the diffuse venous malformation with pelvic involvement can be considered as a differential diagnosis.
In rare cases (as in ours), capillary malformations may be absent and are classified as “atypical KTS”. Capillary malformation is the most prevalent feature according to a study of 252 KTS patients from the Mayo Clinic, where capillary malformation (port-wine stain) was observed in 246 patients (98%), varicosities or venous malformation in 182 (72%), and limb hypertrophy in 170 (67%) [2]. A total of 159 (63%) patients had all three features and the remaining patients (37%) showed two features. The most commonly affected site was the lower extremities (88%); among them, about a quarter were bilateral. The pelvis or abdomen were involved in 18% of the patients.
The treatment is aimed at symptom management and prevention of complications, which depends on the severity of disease. Complications of KTS include gastrointestinal or genitourinary hemorrhage in cases of visceral involvement, and coagulative matters such as thrombosis and pulmonary embolism. Endoscopic investigation of the gastrointestinal tract is recommended in KTS patients with anemia or blood in stool. Female patients should be advised of an increased risk of thrombosis during pregnancy. Treatment options include conservative treatment (compression), as well as surgical removal of dysplastic veins and sclerosis (also of intramuscular or subcutaneous dysplastic vascular areas) [5]. If a patient presents limb length differences, orthopedic procedures such as epiphysiodesis can be considered to stop the length overgrowth of the involved limb and correct the difference [6]. Based on a recent demonstration of PIK3CA mutations in KTS, there is potential interest in sirolimus as a treatment option [7]. If the limb hypertrophy is severe with limited mobility, de-bulking surgeries may be required [8].
We herein share a case of atypical KTS (i.e., lacking capillary malformation), which emphasizes the need of whole-body imaging and regular follow-up.
Author Contributions
Conceptualization, H.-S.K.; methodology, Y.H.; validation, S.-H.C., J.-D.L. and Y.-R.W.; formal analysis, Y.H.; investigation, Y.H. and S.-H.L.; resources, M.C.; data curation, Y.H.; writing—original draft preparation, Y.H.; writing—review and editing, Y.-R.W. and H.-S.K.; visualization, Y.H.; supervision, H.-S.K.; project administration, M.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research study received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Institutional Review Board of Incheon St. Mary’s Hospital, Incheon, South Korea (OC21ZISI005, 11 June 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Redondo, P.; Aguado, L.; Martínez-Cuesta, A. Diagnosis and management of extensive vascular malformations of the lower limb: Part I. Clinical diagnosis. J. Am. Acad. Dermatol. 2011, 65, 893–908. [Google Scholar] [CrossRef] [PubMed]
- Jacob, A.G.; Driscoll, D.J.; Shaughnessy, W.J.; Stanson, A.W.; Clay, R.P.; Gloviczki, P. Klippel-Trénaunay syndrome: Spectrum and management. Mayo Clin. Proc. 1998, 73, 28–36. [Google Scholar] [CrossRef]
- Klippel, M.; Trenaunay, P. Du noevus variqueux osteohypertrophiques. Arch. Gen. Med. 1900, 3, 641–672. [Google Scholar]
- Craven, N.; Wright, A.L. Familial Klippel-Trenaunay syndrome: A case report. Clin. Exp. Dermatol. 1995, 20, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Asghar, F.; Aqeel, R.; Farooque, U.; Haq, A.; Taimur, M. Presentation and Management of Klippel-Trenaunay Syndrome: A Review of Available Data. Cureus 2020, 12, e8023. [Google Scholar] [CrossRef] [PubMed]
- Schoch, J.J.; Nguyen, H.; Schoch, B.S.; Anderson, K.R.; Stans, A.A.; Driscoll, D.; Tollefson, M. Orthopaedic diagnoses in patients with Klippel-Trenaunay syndrome. J. Child. Orthop. 2019, 13, 457–462. [Google Scholar] [CrossRef] [PubMed]
- Hammer, J.; Seront, E.; Duez, S.; Dupont, S.; Van Damme, A.; Schmitz, S.; Hoyoux, C.; Chopinet, C.; Clapuyt, P.; Hammer, F.; et al. Sirolimus is efficacious in treatment for extensive and/or complex slow-flow vascular malformations: A monocentric prospective phase II study. Orphanet J. Rare Dis. 2018, 13, 191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- John, P.R. Klippel-Trenaunay Syndrome. Tech. Vasc. Interv. Radiol. 2019, 22, 100634. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).