Abstract
Background/Objectives: The association between sexual dysfunctions and diabetes is largely known, but few studies investigated its prevalence in Type 1 Diabetes (T1D). The aim of this study was to evaluate the prevalence of sexual dysfunction in a group of men with T1D regardless of their age and to compare the prevalence in men treated with different intensive insulin regimens. Methods: The study population included 68 men affected by T1D, of whom 17 were on Multiple Daily Injections (MDI) and 51 were on Continuous Subcutaneous Insulin Infusion (41 on Advanced Hybrid Closed Loop System with catheters and 10 on patch pumps). All participants completed the International Index of Erectile Function (IIEF-15), which evaluates several domains of sexual function. Another questionnaire that evaluated general features, diabetes-specific features, and sexual-specific features was proposed to every participant. Results: The overall prevalence of erectile dysfunction was 48.5%, and the overall prevalence of a severe grade of erectile dysfunction was 26.5%. Correlations were demonstrated between the prevalence of erectile dysfunction and age and between the prevalence of erectile dysfunction and dyadic status. Age and dyadic status were also correlated with lower scores in several other domains of the IIEF-15 questionnaire. Conclusions: Men with Type 1 Diabetes present a high prevalence of erectile dysfunction, independent of glycometabolic control of the disease and insulin regimens; on the contrary, a great correlation is demonstrated with age and dyadic status.
1. Introduction
Diabetes mellitus (DM) is a group of metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion and/or insulin action. DM is globally considered as one of the world’s major public health problems [1]. The most prevalent form is represented by Type 2 Diabetes (T2D); however, Type 1 Diabetes (T1D) constitutes 5–10% of the forms of diabetes, and it is one of the most common chronic diseases of childhood. T1D is an autoimmune disease in which pancreatic beta cells are destroyed, resulting in a defect of insulin secretion. T1D has been characterized as a lifelong disease, frequently diagnosed in youth, which requires a daily therapy with insulin [2]. Globally, the male-to-female ratio with a diagnosis of T1D in young adulthood is approximately 1.5:1 [3]. Long-term complications of T1D include macrovascular comorbidity, such as atherosclerotic cardiovascular and peripheral arterial disease, and microvascular comorbidity, such as cerebrovascular disease, retinopathy, nephropathy, and peripheral and autonomic neuropathy [4]. A further complication, caused by neurological and vascular complications associated with hormonal imbalance and psychological challenges related to living with T1D, is sexual dysfunction [5]. The management of T1D has changed substantially over the past years. Evolving technologies offer the potential to highly improve glycemic control. Systems that integrate insulin infusion with continuous glucose monitoring (CGM) are now widely used by T1D patients [6]. Currently, the CGM parameters indicating good glycemic control are defined by the International Consensus as Time in Range (TIR) (70–180 mg/dL) > 70%, Time below Range (TBR) (<70 mg/dL) < 4%, TBR < 54 mg/dL < 1%, Time Above Range (TAR) (>180 mg/dL) < 25%, and TAR > 250 mg/dL < 1% [7]. Erectile dysfunction (ED) is defined as the consistent or recurrent inability to achieve or maintain an erection sufficient for satisfactory sexual performance [8]. ED is considered the most frequent sexual dysfunction in men, with a prevalence increasing with age and reaching the highest values in men older than 70 years [9]. Apart from aging, diabetes is the most common risk factor for ED [10], leading to its onset 10–15 years earlier than in the general population [11]. Focusing on T1D, a study conducted by Fedele et al. in Italy showed a prevalence of ED in subjects with T1D of 26% [12], and similarly, a recent meta-analysis showed that the prevalence rate of ED in patients with T1D was 37.5% [13]. Several other studies evaluated the prevalence of ED in T1D, showing similar prevalence rates [14,15]. The METRO study, a single-center, longitudinal observational study born with the aim to evaluate the metabolic and endocrinological profile of young patients with T1D [16], showed a prevalence rate of ED of 37% in 18–35-year-old male subjects; no differences between using a Continuous Subcutaneous Insulin Infusion (CSII) therapy and subjects in treatment with Multiple Daily Injections (MDI) of insulin were observed in terms of the prevalence of severity rate of ED [16]. In this context, the aims of this study were to evaluate (1) the prevalence of ED in a cohort of men affected by T1D independently of their age; (2) differences in sexual function between different types of insulin therapy, including MDI and CSII with Advanced Hybrid Closed Loop System with catheter (c-CSII) or with patch pump (pp-CSII); (3) association between the prevalence of ED and biochemical parameters commonly used in clinical practice; and (4) correlation between different domains of sexual function and T1D characteristics.
2. Materials and Methods
2.1. Participants
In the present transversal observational study, an anonymous questionnaire was proposed to all men who attended the outpatient clinic of the Diabetology Clinic of IRCCS Ospedale Policlinico San Martino and the Diabetology Clinic of IRCCS Istituto Giannina Gaslini during the period December 2022—April 2023. The inclusion criteria were age ≥ 18 years, diagnosis of T1D according to American Diabetes Association (ADA) criteria for at least 6 months, and insulin therapy with CSII or MDI for at least 3 months. The questionnaire was not proposed to subjects with major health problems other than complications of diabetes, including neoplasms, major depression or other psychiatric disorders, severe neurological diseases, or drug or alcohol abuse.
2.2. Questionnaire and Data Collection
In men, sexual function was assessed by completing the International Index of Erectile Function (IIEF-15), a validated self-report questionnaire including 15 items subdivided into five domains (orgasmic function, sexual desire, intercourse satisfaction, overall satisfaction, and erectile function) referring to sexual activity in the last 4 weeks [17]. For each response, a higher score indicates a better function. Six of the 15 questions concern erectile function, and in this specific domain, a total score between 1 and 30 is possible: Scores between 1 and 10 pertain to a severe form of ED; scores between 11 and 16 pertain to a moderate form of ED; scores between 17 and 25 pertain to a mild form of ED; and scores between 26 and 30 pertain to an absence of ED [18]. A questionnaire that investigated personal characteristics of the subjects was associated with IIEF-15. The questions concerned general information, such as age and dyadic status; diabetes-specific features, such as type of therapy, duration of ongoing therapy, and use of a continuous glucose monitoring system (CGM); and sexual-specific features, such as hypoglycemic events or tendency to remove the insulin pump during intercourse. The study was proposed to subjects who met inclusion criteria during the scheduled visits. The questionnaires were administered anonymously. The informed consent form already signed by patients, in which they agree to the use of clinical data for research purposes, was used. In addition, all patients filled out a specific informed consent form for the collection of data. The study was conducted in accordance with the Declaration of Helsinki and the International Conference on Harmonization Good Clinical Practice. In order to obtain truthful responses and give participants more perception of anonymity, questions exploring body mass index, cigarette consumption, and other factors impacting sexual function and ED were not included in the questionnaire [5]. For the same reason, the questionnaire provided interval responses (For example: How old are you? A. 18–25 years old; B. 26–40 years old; C. 41–60 years old; D. more than 60 years old), and therefore it was not possible to obtain statistical findings such as median or standard deviation for the specific features.
2.3. Statistical Methods
Descriptive statistics were generated for the whole cohort. Data were expressed as mean and standard deviation for continuous variables and as absolute or relative frequencies for categorical variables. The distribution of the data were analyzed using the Kolmogorov–Smirnov test. Non-parametric statistics were considered as appropriate. Differences between groups were evaluated using the Mann–Whitney U-test for continuous variables and the χ2 or Fisher exact test for categorical variables. A p-value of <0.05 was considered statistically significant; all p-values were based on two-tailed tests. Statistical analysis was performed using the Statistical Package for the Social Sciences for Windows 11 (SPSS Inc., Chicago, IL, USA).
3. Results
From the 84 potential participants, six were excluded (three due to psychiatric disorder, two due to drug abuse, and one due to concomitant neoplasm), and 10 refused to complete the questionnaire. Therefore, a total of 68 participants were included in the study, of whom 17 were in treatment with MDI, 41 were in treatment with c-CSII (CSII with catheter), and 10 were in treatment with pp-CSII (CSII with patch pump) (Figure 1).
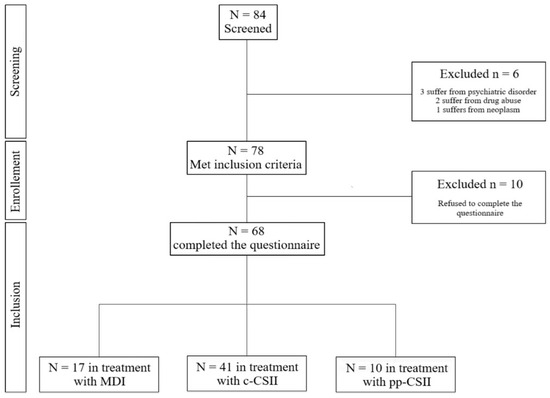
Figure 1.
Flow diagram of the study.
The characteristics of the study group and the comparison of individuals in different therapeutic regimes are shown in Table S1. Statistically significant differences were demonstrated in terms of the duration of ongoing therapy (MDI vs. c-CSII and MDI vs. pp-CSII, both with p < 0.01) and in terms of glycometabolic control of the disease: subjects with MDI had a lower frequency of TIR ≥ 50% and TIR ≥ 70% compared with subjects in treatment with c-CSII (p < 0.01 and p < 0.01, respectively).
Based on the prevalence of ED, indicated by a score < 26 in the specific section of the IIEF-15 questionnaire, Figure 2 showed percentages of diagnosis: the overall prevalence of ED was 48.5% (33/68), of which 14.7% (10/68) were in a mild grade, 7.4% (5/68) in a moderate grade, and 26.5% (18/68) in a severe grade.
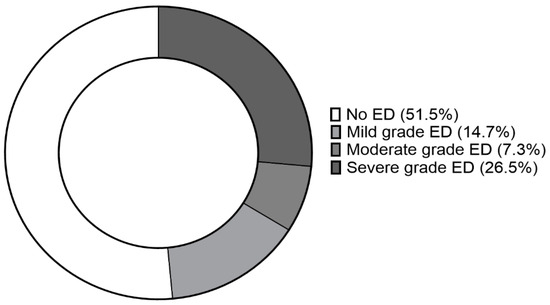
Figure 2.
Prevalence of erectile dysfunction (ED) and grade of condition of study group.
The scores of IIEF-15 questionnaires in the different evaluable domains and prevalence of ED with a comparison of different therapies were shown in Table 1. No statistically significant differences were observed in MDI, c-CSII, and pp-CSII groups in terms of prevalence of erectile dysfunction (29.4%, 51.2%, and 70.0%, respectively). A statistically significant difference was observed only in the intercourse satisfaction domain between subjects in treatment with MDI vs. subjects in treatment with c-CSII (p = 0.03).

Table 1.
IIEF-15 domain scores, prevalence of ED, and grade of dysfunction of study group and comparison between different treatment groups. * p-values related to differences between MDI and c-CSII groups = 0.03.
Based upon age ranges, differences in several scores of IIEF-15 domains were found to be statistically significant, as shown in Table 2. In the 18–25-year-old group, scores of erectile function and overall satisfaction domains were statistically significantly higher compared to the 41–60-year-old group (p = 0.05 and p = 0.01, respectively). Additionally, in the 26–40-year-old group, scores concerning erectile function, intercourse satisfaction, and overall satisfaction domains were statistically significantly higher compared to the 41–60-year-old group (p = 0.02, p = 0.03, and p = 0.05, respectively). No statistically significant difference was observed in IIEF-15 domain scores between the 18–25-year-old group and the 26–40-year-old group. A statistically significant difference between the prevalence of diagnosis of ED was also observed between the 18–25-year-old group and the 41–60-year-old group (p = 0.05) and between the 26–40-year-old group and the 41–60-year-old group (p = 0.04).

Table 2.
IIEF-15 domain scores, prevalence of ED, and grade of dysfunction in different age groups. * p-values related to differences between age ranges.
Evaluating glycometabolic control, Figure 3 showed the differences in IIEF-15 domain scores between different ranges of TIR and different percentages of HbA1c: a statistically significant difference was evident regarding the intercourse satisfaction domain both with TIR ≥ 50% vs. TIR < 50% and TIR ≥ 70% vs. TIR < 70% (p = 0.03 and p = 0.02, respectively); also, the sexual desire domain showed a statistically significant difference between TIR ≥ 50% vs. TIR < 50% (p = 0.05); on the other hand, no statistically significant differences were demonstrated regarding HbA1c ≤ 7% vs. HbA1c > 7%. No statistically significant differences were demonstrated also in terms of prevalence of ED.
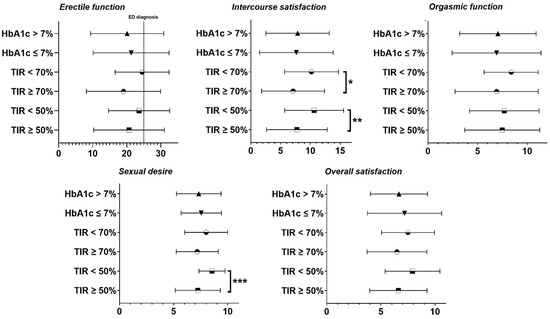
Figure 3.
IIEF-15 domains in groups with different percentages of TIR and HbA1c enlightened in mean ± standard deviation. * p = 0.02; ** p = 0.03; *** p = 0.05.
Dividing the subjects into groups regarding dyadic status, most of the IIEF-15 domain scores were found to be statistically significantly higher in subjects in a relationship than in subjects not in a relationship, as presented in Figure 4. Moreover, subjects in Group B (in a relationship for less than one year) presented higher scores in most of the IIEF-15 domains also compared to subjects in Group C (in a relationship for more than one year but for less than five years) and compared to subjects in Group D (in a relationship for more than five years). Both erectile function domain scores and prevalence of ED showed differences between subjects in a relationship apart from duration and subjects not in a relationship.
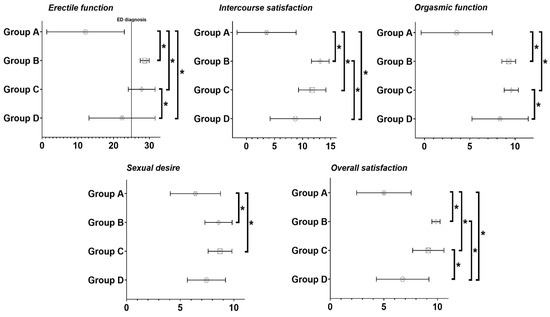
Figure 4.
IIEF-15 domain scores in groups with different dyadic statuses enlightened in mean ± standard deviation. Group A: subjects not in a relationship; Group B: subjects in a relationship for less than one year; Group C: subjects in a relationship for more than a year but less than five years; Group D: subjects in a relationship for more than five years. * p < 0.05.
As highlighted in Table 3, a comparison of subjects that experienced a hypoglycemic event during intercourse and subjects that did not experience the event demonstrated differences in most of the IIEF-15 domain scores. Erectile function, intercourse satisfaction, and overall satisfaction domain scores were statistically significantly higher in subjects that experienced a hypoglycemic event during intercourse (p = 0.02, p = 0.01, and p = 0.01, respectively). Statistically significant differences were observed also in terms of prevalence of ED between the two groups (p = 0.01).

Table 3.
IIEF-15 domain scores, prevalence of ED, and grade of dysfunction in groups with and without hypoglycemic events during intercourse. * p-values related to differences between groups.
4. Discussion
The present study aimed to investigate the association between T1D and ED. In recent years, many studies have been carried out regarding this topic [11,12,13,14], most of them utilizing a modified version of IIEF-15 that evaluates only the erectile function domain with 5 items, called IIEF-5 [19]. The prevalence of ED in our study was 48.5%, greater than the prevalence in a recent meta-analysis of Kouidrat et al., where it was 37.5%, as well as a prevalence of 42.9% found in a study of Kamiński et al. and an overall prevalence of 37% in a study of Maiorino et al. [13,15,16]. A possible explanation of this more frequent occurrence could be that our study involves subjects affected by T1D independently of their age; the cohort of Kamiński et al. presented a mean age of 39.0 years, while the cohort of Maiorino et al. presented a mean age of 22.8 years; instead, a percentage of 38.2% in our cohort is more than 40 years old. In support of this hypothesis, a percentage of 26.5% of subjects in our overall cohort presented a severe grade of ED, instead of most of the subjects in previous studies who only presented a mild ED [15,16]. Age has proven to be a great non-modifiable factor for ED: in our cohort, both the 18–25-year-old group and the 26–40-year-old group had a less frequent occurrence of ED compared to the 40–60-year-old group. The DCCT and EDIC study was designed with the purpose of comparing different therapy regimes in T1D subjects involving a great number of subjects regardless of their age: some of the participants were also involved in completing the IIEF-15 questionnaire [14], and it is the only comparable study with an evaluation of the IIEF-15 domain scores. In the DCCT/EDIC study, results were interpreted by defining ED as a score < 20 on the erectile function domain, low sexual desire as a score < 7 on the desire domain, and orgasmic dysfunction as a score < 7 on the orgasmic domain of the IIEF-15: the overall prevalence of ED, low sexual desire, and orgasmic dysfunction was 34%, 55%, and 20%, respectively. Utilizing those arbitrary parameters, our cohort presented a low sexual desire prevalence of 50% (34/68) and an orgasmic dysfunction of 35.2% (24/68). In the present study, the prevalence rate of ED as well as the IIEF-15 domain scores, were similar in subjects with T1D in treatment with MDI, c-CSII, or pp-CSII: the only difference was noted in the intercourse satisfaction domain of IIEF-15 between MDI and c-CSII treatment. Only the study of Maiorino et al. described sexual function in T1D subjects according to different intensified insulin regimens, and any differences were described in subjects in treatment with MDI or CSII independently from administration with conventional catheter or patch pump [16]. The intercourse satisfaction domain presented differences also according to TIR%, both utilizing 50% and 70% as limits to assembling groups: TIR is considered useful as a clinical target and outcome measurement that complements HbA1c in diabetes management [7]. Otherwise, no differences were observed in IIEF-15 domains and in ED prevalence according to different HbA1c percentages. No association was demonstrated in the present study between the conventional parameters used in the management of T1D, such as TIR and HbA1c percentages, and sexual dysfunction recurrence: a possible explanation could be that ED and other sexual dysfunctions are multifactorial conditions that involve numerous unmodifiable and modifiable factors, which are often present at the same time and can influence each other, like age, diabetes mellitus, metabolic syndrome, obesity, cardiovascular disease, hypertension, and dyslipidemia [20]; an important contribution is also related to psychological factors and dyadic status [21]. In fact, in the present study an important difference according to dyadic status was noted in every IIEF-15 domain between the group of subjects not in a relationship and groups of subjects in a relationship regardless of duration. Partners of T1D subjects were often involved in diabetes-related issues, and a great impact in reducing diabetes-related distress was demonstrated by some authors in a context where partners presented an active engagement related to diabetes [22]. Another correlation was demonstrated regarding the occurrence of hypoglycemic events during intercourse: the subjects that experienced the condition presented higher scores in most of the IIEF-15 domains. To the best of our knowledge, this is the first study that evaluates the occurrence of hypoglycemic events during intercourse in T1D male subjects. A significant positive association between hypoglycemic events and negative psychological outcomes such as fear of hypoglycemia, diabetes-related distress, and reduced general emotional well-being was demonstrated [23].
5. Conclusions
As suggested by the World Health Organization, sexual health is strictly connected to health in a universal manner, and including subjects without age limitations in our study has this clear purpose [24]. Despite that, in our cohort 76.5% (52/68) of subjects enrolled in the study had never talked to diabetologists about sexual health before the start of the study; to the best of our knowledge, this is the first study that evaluated this aspect. The possibility to include an evaluation of sexual health during follow-up visits could allow the diagnosis of erectile dysfunction and other sexual dysfunctions in men with T1D. This study presented several limitations: lack of evaluation of potential factors with a demonstrated impact on sexual function and ED recurrence, such as body mass index, cigarette consumption, and psychological factors; data mostly obtained with interval responses and with a self-reported questionnaire; cross-sectional nature of the study; and heterogeneity of the subjects enrolled. The study demonstrated a high prevalence of ED in subjects affected by T1D independently of their age. No correlations were demonstrated either between sexual dysfunction in men affected by T1D in treatment with different insulin therapy regimens or between sexual dysfunction and conventional parameters utilized in the management of T1D, such as TIR and HbA1c percentages. Further studies that overcome the limitations mentioned above and with a larger population are needed in order to demonstrate the impact of T1D on the occurrence of sexual dysfunction in males.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/diabetology6050034/s1, Table S1: Characteristic of study group and comparison between different treatment groups.
Author Contributions
Conceptualization: M.B., D.C.M. and N.M.; Methodology: C.P. and G.S.; Formal analysis and investigation: M.G.C.; Writing—original draft preparation: C.P.; Writing—review and editing: F.C. and M.B.; Resources: C.P. and E.D.C.; Supervision: N.M., D.C.M., D.F. and M.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable, since this study did not require ethical approval.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data used to support the findings of this study are included within the article.
Acknowledgments
We are extremely grateful to patients and their families who constantly collaborate in the progress of clinical research by participating in the studies proposed by the diabetes team of our institute.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| DM | Diabetes Mellitus |
| T1D | Type 1 Diabetes |
| T2D | Type 2 Diabetes |
| MDI | Multiple Daily Injections |
| CGM | Continuous Glucose Monitoring |
| IIEF-15 | International Index of Erectile Function |
| ED | Erectile Disfunction |
| TIR | Time In Range |
| TAR | Time Above Range |
| TBR | Time Below Range |
| CSII | Continuous Subcutaneous Insulin Infusion |
| ppCSII | Continuous Subcutaneous Insulin Infusion with Patch Pump |
| cCSII | Continuous Subcutaneous Insulin Infusion with Catheter |
| ADA | American Diabetes Association |
| IRCCS | Istituto di Ricovero e Cura a Carattere Scientifico |
| HbA1c | Glycated Hemoglobin |
References
- Gregory, G.A.; Robinson, T.I.G.; Linklater, S.E.; Wang, F.; Colagiuri, S.; de Beaufort, C.; Donaghue, K.C.; International Diabetes Federation Diabetes Atlas Type 1 Diabetes in Adults Special Interest Group; Magliano, D.J.; Maniam, J.; et al. Global incidence, prevalence, and mortality of type 1 diabetes in 2021 with projection to 2040: A modelling study. Lancet Diabetes Endocrinol. 2022, 10, 741–760. [Google Scholar] [CrossRef] [PubMed]
- Holt, R.I.G.; DeVries, J.H.; Hess-Fischl, A.; Hirsch, I.B.; Kirkman, M.S.; Klupa, T.; Ludwig, B.; Nørgaard, K.; Pettus, J.; Renard, E.; et al. The management of type 1 diabetes in adults. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2021, 64, 2609–2652. [Google Scholar] [CrossRef]
- Diaz-Valencia, P.A.; Bougnères, P.; Valleron, A.J. Global epidemiology of type 1 diabetes in young adults and adults: A systematic review. BMC Public Health 2015, 15, 255. [Google Scholar] [CrossRef]
- Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N. Engl. J. Med. 1993, 329, 977–986. [Google Scholar] [CrossRef] [PubMed]
- Lewis, R.W.; Fugl-Meyer, K.S.; Corona, G.; Hayes, R.D.; Laumann, E.O.; Moreira, E.D., Jr.; Rellini, A.H.; Segraves, T. Definitions/epidemiology/risk factors for sexual dysfunction. J. Sex. Med. 2010, 7, 1598–1607. [Google Scholar] [CrossRef] [PubMed]
- Bassi, M.; Franzone, D.; Dufour, F.; Strati, M.F.; Scalas, M.; Tantari, G.; Aloi, C.; Salina, A.; d’Annunzio, G.; Ma-ghnie, M.; et al. Automated Insulin Delivery (AID) Systems: Use and efficacy in children and adults with type 1 diabetes and other forms of diabetes in europe in early 2023. Life 2023, 13, 783. [Google Scholar] [CrossRef]
- Battelino, T.; Danne, T.; Bergenstal, R.M.; Amiel, S.A.; Beck, R.; Biester, T.; Bosi, E.; Buckingham, B.A.; Cefalu, W.T.; Close, K.L.; et al. Clinical targets for continuous glucose monitoring data interpretation: Recommendations from the international consensus on time in range. Diabetes Care 2019, 42, 1593–1603. [Google Scholar] [CrossRef]
- Corona, G.; Cucinotta, D.; Di Lorenzo, G.; Ferlin, A.; Giagulli, V.A.; Gnessi, L.; Isidori, A.M.; Maiorino, M.I.; Miserendino, P.; Murrone, A.; et al. The Italian Society of Andrology and Sexual Medicine (SIAMS), along with ten other Italian Scientific Societies, guidelines on the diagnosis and management of erectile dysfunction. J. Endocrinol. Investig. 2023, 46, 1241–1274. [Google Scholar] [CrossRef]
- McCabe, M.P.; Sharlip, I.D.; Lewis, R.; Atalla, E.; Balon, R.; Fisher, A.D.; Laumann, E.; Lee, S.W.; Segraves, R.T. Incidence and prevalence of sexual dysfunction in women and men: A consensus statement from the fourth In-ternational consultation on sexual medicine 2015. J. Sex. Med. 2016, 13, 144–152. [Google Scholar] [CrossRef]
- Maiorino, M.I.; Bellastella, G.; Esposito, K. Diabetes and sexual dysfunction: Current perspectives. Diabetes Metab. Syndr. Obes. 2014, 7, 95–105. [Google Scholar] [CrossRef]
- Johannes, C.B.; Araujo, A.B.; Feldman, H.A.; Derby, C.A.; Kleinman, K.P.; McKinlay, J.B. Incidence of erectile dys-function in men 40 to 69 years old: Longitudinal results from the Massachusetts male aging study. J. Urol. 2000, 163, 460–463. [Google Scholar] [CrossRef] [PubMed]
- Fedele, D.; Coscelli, C.; Cucinotta, D.; Forti, G.; Santeusanio, F.; Viaggi, S.; Fiori, G.; Velonà, T.; Lavezzari, M.; Diade Study Group. Incidence of erectile dysfunction in Italian men with diabetes. J. Urol. 2001, 166, 1368–1371. [Google Scholar] [CrossRef] [PubMed]
- Kouidrat, Y.; Pizzol, D.; Cosco, T.; Thompson, T.; Carnaghi, M.; Bertoldo, A.; Solmi, M.; Stubbs, B.; Veronese, N. High prevalence of erectile dysfunction in diabetes: A systematic review and meta-analysis of 145 studies. Diabet. Med. 2017, 34, 1185–1192. [Google Scholar] [CrossRef] [PubMed]
- Penson, D.F.; Wessells, H.; Cleary, P.; Rutledge, B.N.; Diabetes control and complications trial/epidemiology of diabetes interventions and complications research group. Sexual dysfunction and symptom impact in men with long-standing type 1 diabetes in the DCCT/EDIC cohort. J. Sex. Med. 2009, 6, 1969–1978. [Google Scholar] [CrossRef]
- Kamiński, M.; Kulecki, M.; Lachowski, P.; Kasprzak, D.; Kulczycka, A.; Kozłowska, M.; Klause, D.; Uruska, A.; Michalski, M.; Zozulińska-Ziółkiewicz, D. Erectile dysfunction in individuals with type 1 diabetes is associated with long-term metabolic control and diabetic complications: A cross-sectional study. Int. J. Angiol. 2022, 31, 97–106. [Google Scholar] [CrossRef]
- Maiorino, M.I.; Bellastella, G.; Della Volpe, E.; Casciano, O.; Scappaticcio, L.; Cirillo, P.; Giugliano, D.; Esposito, K. Erectile dysfunction in young men with type 1 diabetes. Int. J. Impot. Res. 2017, 29, 17–22. [Google Scholar] [CrossRef]
- Rosen, R.C.; Riley, A.; Wagner, G.; Osterloh, I.H.; Kirkpatrick, J.; Mishra, A. The international index of erectile function (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology 1997, 49, 822–830. [Google Scholar] [CrossRef]
- Cappelleri, J.C.; Rosen, R.C.; Smith, M.D.; Mishra, A.; Osterloh, I.H. Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology 1999, 54, 346–351. [Google Scholar] [CrossRef]
- Rosen, R.C.; Cappelleri, J.C.; Smith, M.D.; Lipsky, J.; Peña, B.M. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int. J. Impot. Res. 1999, 11, 319–326. [Google Scholar] [CrossRef]
- Defeudis, G.; Mazzilli, R.; Tenuta, M.; Rossini, G.; Zamponi, V.; Olana, S.; Faggiano, A.; Pozzilli, P.; Isidori, A.M.; Gianfrilli, D. Erectile dysfunction and diabetes: A melting pot of circumstances and treatments. Diabetes. Metab. Res. Rev. 2022, 38, e3494. [Google Scholar] [CrossRef]
- Brotto, L.; Atallah, S.; Johnson-Agbakwu, C.; Rosenbaum, T.; Abdo, C.; Byers, E.S.; Graham, C.; Nobre, P.; Wylie, K. Psychological and interpersonal dimensions of sexual function and dysfunction. J. Sex. Med. 2016, 13, 538–571. [Google Scholar] [CrossRef] [PubMed]
- Trief, P.M.; Jiang, Y.; Beck, R.; Huckfeldt, P.J.; Knight, T.; Miller, K.M.; Weinstock, R.S. Adults with type 1 diabetes: Partner relationships and outcomes. J. Health Psychol. 2017, 22, 446–456. [Google Scholar] [CrossRef] [PubMed]
- Chatwin, H.; Broadley, M.; Speight, J.; Cantrell, A.; Sutton, A.; Heller, S.; de Galan, B.; Hendrieckx, C.; Pouwer, F.; Hypo-RESOLVE Consortium. The impact of hypoglycaemia on quality of life outcomes among adults with type 1 diabetes: A systematic review. Diabetes Res. Clin. Pr. 2021, 174, 108752. [Google Scholar] [CrossRef] [PubMed]
- Narasimhan, M.; Logie, C.H.; Gauntley, A.; Gomez Ponce de Leon, R.; Gholbzouri, K.; Siegfried, N.; Abela, H.; Ouedraogo, L. Self-care interventions for sexual and reproductive health and rights for advancing universal health coverage. Sex. Reprod. Health Matters 2020, 28, 1778610. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).