Abstract
Virtual reality (VR) is a simulated experience in a three-dimensional (3D) computer-simulated world. Recent advances in technology position VR as a multipurpose technology in the healthcare sector and as a critical component in achieving Health 4.0. In this article, descriptive and correlationally quantitative research is carried out on the assessments made by Latin American health sciences university professors on the didactic use of virtual reality technologies. The main objective was to analyze the differences in the perceptions expressed by the public or private tenure of the universities where the professors teach. In addition, gender and age gaps were identified in the assessments obtained from each of the types of universities. The results reveal that Latin American health science professors at private universities have a higher selfconcept of their digital skills for the use of virtual reality in the lectures. This greater selfconcept also leads to a reduction in the gender and age gaps in the participating private universities with respect to the public counterparts. It is advisable to increase both faculty training in the didactic use of virtual reality and funding for its use, mainly in public universities.
1. Introduction
In 2015, with the start of the commercialization of different virtual reality (VR) devices, VR technology was positioned as one of the technologies with the highest expectations for development. However, the progress experienced in recent years by other technologies, such as augmented reality (AR) [1,2] or robotics [3], and the various drawbacks for its implementation, have gradually reduced the expectations of VR implementation [4]. In 2020, after the pandemic originated by COVID-19 [5], VR technology has increasing development expectations [6] and positions itself as the reference technology for developing the “Metaverse” [7].
Technically, VR is a computer-generated digital environment that offers three-dimensional visual opportunities with which users can interact [8,9]. This technology provides near-real and/or believable experiences in a synthetic or virtual form [10]. VR technology can be divided based on the immersion level (i.e., immersive and nonimmersive) [11]. Immersive VR typically requires the use of a headset, such as the Meta Quest 2®, the HTC Vive Pro®, or PlayStation VR® (PSVR), which are compatible with peripherals such as Leap Motion®, a device that allows the user’s movements to be identified, or a full-room display that encloses the user, referred to as a cave automatic virtual environment (CAVE) [12]. Nonimmersive VR, on the other hand, offers users a computer-generated world that typically uses a desktop or projector. Recent advances in VR technology [13] make the creation and development of VR applications feasible, and consequently, the presence of the technology is increasing every day in the main economic sectors (industry, health, education, etc.).
But there is one sector of economic activity in which VR technology is of particular interest due to the variety of applications that can be developed: the health sector [14,15,16]. In this sector, VR is positioned as a reference for multiple purposes [17,18], being a fundamental component of smart healthcare [19], also known as Health 4.0 [20]. Some other applications of Health 4.0 are the following: (i) the personalization of implants [21,22] and digital hospitals [23]; (ii) treatment monitoring [24]; (iii) augmented reality [25,26,27]; (iv) the internet of things [2,28]; (v) QR code systems [29], and (vi) the healthcare metaverse [7].
The emergence of virtual simulation applications related to the healthcare sector is continuous and is linked to the technical progress in VR. Figure 1 shows the different clinical and technical applications of VR currently being used in the healthcare sector, as well as the main references that develop them. Among the applications of VR in healthcare, it is worth highlighting (i) oral health [21,30], (ii) the treatment of diseases, disorders, disabilities, syndromes, and addictions [14,31,32,33,34,35,36,37,38,39], (iii) the treatment of injuries [18,40], (iv) preparation for surgical interventions [41], (v) the treatment of psychological problems [14,42,43,44], (vi) the improvement of the social and psychological skills of health personnel and patients [45,46,47,48,49], (vii) wellness and health care [17,50,51,52,53,54,55,56,57,58,59], (viii) training and education [60,61,62,63,64,65,66,67,68,69,70,71,72,73,74], (ix) rehabilitation [14,75,76,77,78,79,80], (x) environmental barriers [81], and (xi) pediatrics [82,83,84].
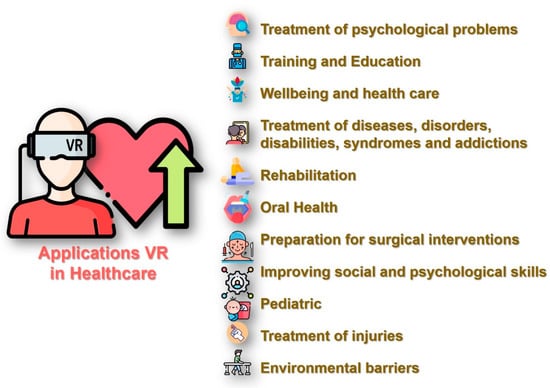
Figure 1.
VR applications in healthcare.
In recent years, there has been a shift in digital education, with the incorporation of VR applications into lectures in the various fields of higher education knowledge [85]. In engineering and construction, VR has positioned itself as a relevant technology, both for the development of technical projects [86] and in the development of education and training programs [86,87]. In medical health education, the most significant increase in virtuality occurred after the COVID-19 pandemic [5], which forced a transition from traditional educational practice [88] to online education [89,90,91,92], generating negative psychological consequences in its students [5,32]. Along with this multimodal (face-to-face and distance) pedagogical shift, there is increasing evidence that simulation improves competency [93], attitude, and behavior [94], especially in comparison with traditional didactic methods or the absence of simulation training. To aid this, innovative technologies, such as VR [95,96], are becoming ubiquitous and available for classroom use [97,98].
A simple indicator of this growing use of VR is the number of research papers including the term VR as the focus of the research. From a simple consultation of SCOPUS on the number of articles including in the title, abstract, or keyword for the words (data collected in September 2022) (i) “Virtual Reality” AND “Health” or (ii) “Virtual Reality” AND “Health” AND “Education, Figure 2 was obtained. This way, a clear growing trend is revealed (Figure 2). Between 1993 and 2021, a total of 7336 papers in the SCOPUS database includes “virtual reality” AND “Health” in the title, abstract, or keywords, and 3284 of them also include “Education”, which is approximately 45% of the total published papers. Since 2015, the speed of the increases in the results of both searches has increased significantly and incrementally each year, increasing by four times (the number of published papers) between the years 2015 and 2021. In addition, the growth in the number of articles, including the term “Education” follows a similar trend to that of the total number of articles responding to the search “Virtual Reality” AND “Health”, suggesting that research on VR applications in health education parallels the development of VR applications in healthcare.
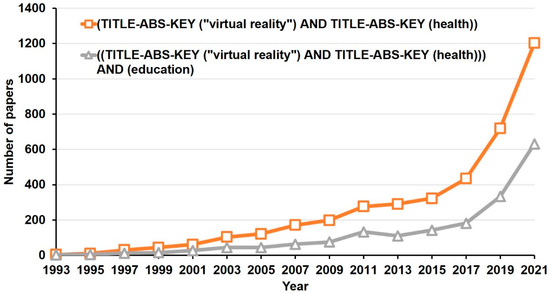
Figure 2.
Number of research papers indexed in SCOPUS related to virtual reality, health, and education (data collected in September 2022).
VR technologies allow three-dimensional simulations that have proven to be useful both in the training of physicians [99] and nurses [100] because these simulations can be adapted to realistic clinical care situations and to the recreation of complex processes, for example, surgery, generating an immersive experience. The specialized literature has abundantly proven that the use of VR in health education is didactically effective because it increases the knowledge and academic performance of students when compared with traditional methodologies based on the master class and with other forms of digital education, both online and face-to-face [101,102]. Some studies indicate that the didactic effectiveness of VR applied to health education is mainly focused on the versatility of this type of technology when designing interactive practical situations [103]. In this sense, both the professors and students of the health sciences highlight the importance of the technical and usability aspects of VR: (i) the capacity of these technologies to perform 3D simulations that allow for the realistic recreation of anatomical objects [104,105]; (ii) the realism of the simulations generated [106,107,108]; (iii) the immersive [109] and interactive [109,110] possibilities that these technologies offer; (iv) the user experience, which is highlighted mainly by students, among whom the use of VR represents a motivational incentive towards learning [102,111,112].
In addition to the technical and usability aspects, health science professors give high ratings to the didactic employability of VR in lectures due to the versatility of these technologies when used with different methodological perspectives [113,114]. It has been proven, for example, that the use of VR technologies in health science education and used within educational gamification dynamics gives very satisfactory academic results among students [104]. The specialized literature also identifies the limitations of the use of VR in health education. Some studies identify that the use of these technologies for a prolonged period, e.g., a 3D video to acquire physical exploration skills, can cause symptoms of simulator sickness in some users, which is not observed when conventional resources or 2D videos are used [115,116]. Other studies point out the danger that virtual simulations may end up replacing the practical training load for health sciences students, which would be detrimental to the development of the competencies and skills that healthcare personnel must develop and that require interaction between the student and the professor and the student’s performance in real hospitals and clinics [117]. Likewise, health sciences students themselves give higher ratings to VR as a training tool when the professor is present and participates as an active element in the learning process [118].
However, there are two disadvantages to the didactic use of VR in health education that appear most frequently in the literature: (i) the requirements posed by its use in terms of the development of technical skills on the part of the professors and students [86,119], and (ii) the heavy economic investment involved in the equipment required to integrate VR technologies in the classroom [113,117]. From the point of view of cost, there are studies that, while recognizing the initial outlay involved in equipping health education with VR technologies, there is no real increase in the cost of training students since the use of VR results in significant savings in materials and the use of laboratories [109,120]. Thus, it could be said that the implementation of VR technologies is economically efficient when applied in health education [121,122]. Health sciences professors also point out some other disadvantages that VR (applied to health education) may have, such as the need for large spaces [123]. Regarding digital competence, it is essential for professors to develop a high level of digital skills to exploit all the didactic potential of VR [124] and for students to increase their own digital competencies [125]. In contrast, the literature reports abundant works in which university professors state that their digital skills are limited and can be improved, regardless of the professor’s area of expertise [126,127]. In particular, health sciences professors admit that their digital skills are insufficient, in general, for undertaking the task of integrating VR technologies into their lectures and that they need to increase their training in this regard [128,129].
Despite the disadvantages of VR and its limitations, the literature attributes a solid future projection for the use of VR technologies in health higher education [130]. This future projection, however, is mainly conditioned to technological advances in VR development that allow for the sharing of simulated clinical experiences [108]. Likewise, professors suggest the need to integrate VR tools into the curricula of medicine, nursing, and dentistry to advance the introduction of these technologies in the lectures [98].
In the Latin American and Caribbean region, which is precisely where this study is located, the COVID-19 pandemic led to the accelerated development of certain health-related technologies aimed at responding to emergency situations that arose [131]. Thus, according to data from the Inter-American Development Bank, the companies most specialized in the use of “Industry 4.0” technologies used artificial intelligence to identify hot spots of virus incidence and prevent contagion and designed platforms to monitor the movements of people and chatbots to respond to medical consultations, as well as utilized 3D printing to make up for the absence of masks or respirators [131].
Specific studies on the implementation of VR in health education in Latin America are scarce, but two main ideas are very clear: (i) the need for Latin American countries and their universities to develop specific training programs on digital health, in general, for their teaching staff [132], and (ii) the convenience of establishing international cooperation programs and projects for the receipt of economic funds and technical and human capital by Latin American universities [133]. After the COVID-19 pandemic, Latin American universities carried out an intense effort to digitize their teaching processes, which has been uneven in different countries and areas of knowledge [134]. The literature shows that, in the specific region of Latin America, the ownership (private or public) of the university exerts a strong influence on the digital skills of the faculty and on the assessments expressed about the use of digital teaching resources. Specifically, professors at private universities are, in general, better prepared digitally than those at public universities and show more favorable opinions about the use of resources, such as VR, in their lectures [126]. The assessment of the use of VR has been studied in detail within a population of professors of higher technical education in Latin America, and it has been concluded that professors from private universities give a higher value to the didactic aspects of VR and its usability as a teaching resource than their colleagues from public universities, although they also find a greater degree of disadvantages than the latter [126]. Moreover, the digital gender gap, which frequently penalizes females in the field of digitization [135,136], is less intense among faculty at private universities than among those at public universities [126]. The literature attributes these gaps to differences in the funding of both types of centers and to the fact that Latin American private universities are more at the forefront of the implementation of digital learning environments since the proportion of their student body that attends online classes is higher than in public universities [137,138]. However, as far as it has been possible to explore, there has been no similar study carried out on a population of professors within the health sciences, so this is an original and novel contribution provided by the present work.
Considering the scientific interest in the use of VR in health and education (exposed above), this article carries out descriptive and correlationally quantitative research on the assessments made by university professors of the health sciences on the didactic use of VR technologies. The main objective was to analyze the differences in the perceptions expressed by the public or private ownership of the universities where the professors teach.
2. Materials and Methods
2.1. Participants
The sample of the participants in the study was selected by means of a nonprobabilistic convenience sampling process. The authors gave a training lecture on the didactic use of VR technologies in higher education, which was repeated every two weeks from January to June 2022, aimed at university professors from different Latin American countries. The contents of the initial training carried out were the following: (i) notions of VR, basic concepts, types of VR, and taxonomies, including the distinction between immersive and nonimmersive VR, (ii) the technical characteristics of VR, and (iii) the presentation of real VR didactic tools and the educational experiences carried out with them. Consequently, it can be assumed that the participants had homogeneous and sufficient knowledge of the basic concepts of VR.
The potential population was formed by those professors enrolled and attending the training, to whom the research purpose of this project was explained, and who were sent the questionnaire used as an instrument through a GoogleForms® link. The criteria for inclusion in the study were as follows: (i) being a specialist in one of the areas of the health sciences, which includes the different subareas included in the 72nd area of the UNESCO International Standard Classification of Education (ISCED) [139], medicine, nursing, or dental services and being an active university professor at a Latin American university in one of these fields, and (ii) having attended a training talk on the didactic use of VR given by the authors. A total of 274 responses to the questionnaire were obtained, of which 270 were considered valid.
Among the participants, there were slightly more than twice as many females as males (68.15% females versus 31.85% males), which implies the existence of a certain gender bias, given that the distribution of the participants is not homogeneous (chi-square = 35.57, df = 1, p-value < 0.0001). The mean age was 50.22 years, with a standard deviation of 10.66 and skewness to the left of –0.31. The median age was 50 years. As can be seen in Figure 3, among the participants, there are representatives from 14 Latin American and Caribbean countries, although the most represented are Argentina, Chile, Mexico, and Peru, which account for 76.30% of the sample. The distribution of participants by country is also not homogeneous (chi-square = 369.54, df = 13, p-value < 0.0001).
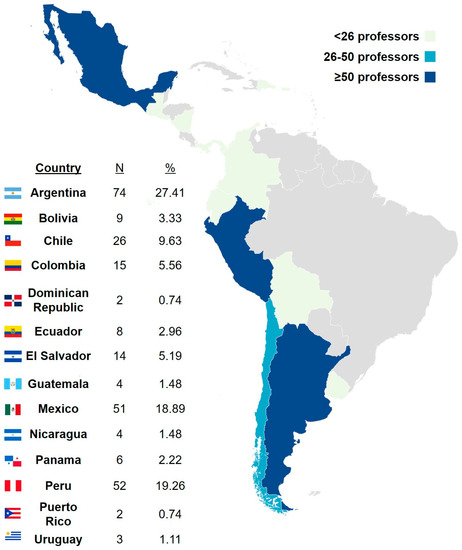
Figure 3.
Distribution of the participants by their country of origin.
Among the participants, 52.22% teach at private universities and 47.78% at public universities, which represents a homogeneous distribution by university tenure (chi-square = 0.5333, df = 1, p-value = 0.4652). In both types of universities, the sample is made up of mostly females (Figure 4). Although this majority is larger in the case of private universities, the gender bias in the sample is similar in both private and public universities (chi-square = 3.2663, df = 1, p-value = 0.0707). The mean age in private universities (46.60 years, with a standard deviation of 10.41) is almost 8 years lower than that of the participants in public universities (54.19 years, with a standard deviation of 9.48). Also, the left skewness of the ages of private university participants (−0.28, Figure 4a) is slightly higher than that of the public university professors (−0.26, Figure 4b).
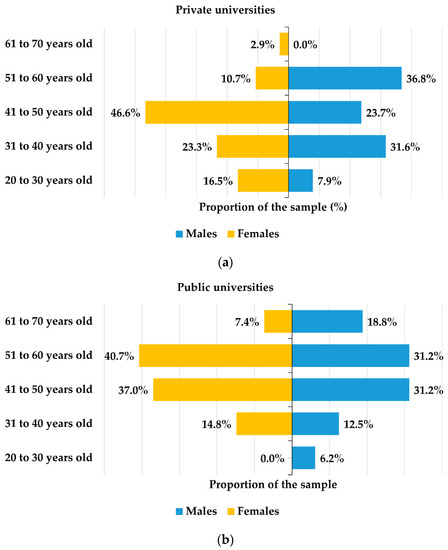
Figure 4.
Distribution of participants by gender in percentages (%) in (a) private universities and (b) public universities.
2.2. Objectives and Variables
The general objective of this paper is to analyze the assessment of Latin American university professors in the health sciences about the didactic use of VR technologies. Specifically, the following specific objectives are pursued: (i) to study the existence of differences in health sciences professors’ assessments of VR technologies by university tenure; (ii) to identify gender gaps in the assessments of VR between health sciences professors from private and public universities; (iii) to analyze the influence of age on the assessments of the participating professors from private and public universities.
To achieve the above objectives, the main explanatory variable considered was the participants’ university tenure, which is a dichotomous variable for which the possible values are private or public. As secondary explanatory variables, the gender and age of the participants were considered. Gender is a dichotomous variable for which the values are female or male. Age is an ordinal quantitative variable. In addition, the following explained variables are defined (Figure 5): (i) participants’ selfperception of digital competence for the use of VR; (ii) an assessment of the technical aspects of VR technologies; (iii) the usability of VR in the classroom; (iv) the perceived drawbacks of VR use; (v) the perceived future projection of the use of VR technologies in the classroom, and (vi) didactic interest in the use of VR in the classroom. All explained variables are ordinally quantitative and were measured on a Likert scale from 1 to 5: 1—null; 2—low; 3—moderate; 4—high; 5—very high.
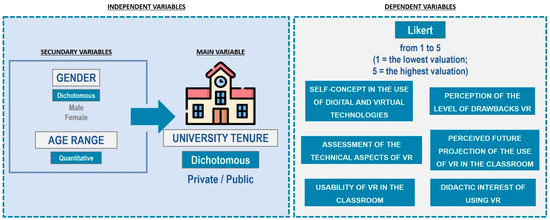
Figure 5.
Research variables.
2.3. Instrument
For this research, a validated questionnaire on the assessment of the use of VR technologies in higher education was used [126]. The questionnaire consists of 22 questions that ask for a rating of the aspect of VR indicated in each of them on a Likert scale from 1 to 5, where 1 expresses the lowest rating and 5 corresponds to the highest. The factor analysis identifies 6 factors or families of questions that explain the questionnaire, which correspond to the 6 explained variables defined in this study.
Specifically, the different factors studied by the questionnaire, with their corresponding items, are the following: (i) digital skills for the use of VR (3 items)–selfperception of digital competence, level of knowledge of VR, and assessment of the training received on VR use; (ii) assessment of the technical aspects of VR (3 items)–3D design, immersiveness, and realism; (iii) assessment of the usability of VR (3 items)–interaction, user experience, and employability; (iv) disadvantages of VR (5 items)–costs, space limitations, human and technical resource requirements, teacher training needs, and equipment obsolescence; (v) future projection of VR in health science education (2 items)–future projection of immersive and nonimmersive virtual reality; and (vi) the didactic aspects of VR (6 items)–didactic usefulness, possibility for your university to implement VR technologies, expected acceptance by students, expected improvement in academic performance, motivation, and improvement in lecture delivery. Considering the values of the Cronbach’s alpha parameters that have been computed, all of which are greater than 0.70 (Table 1), it can be deduced that all the families of questions that have been defined enjoy good levels of internal reliability [140].

Table 1.
Cronbach’s alpha parameters of the different factors of the questionnaire.
The confirmatory factor analysis (CFA) statistics [141] computed confirm the theoretical model just defined and validated by the factor analysis [126]. Indeed, the incremental fit indices are good (AGFI = 0.7253; NFI = 0.7271; TLI = 0.8163; CFI = 0.7729; IFI = 0.7758), and the absolute fit indices are also appropriate (GFI = 0.7894; RMSEA = 0.1120; AIC = 961.5221; chi-square/df = 4.3481).
2.4. Design and Statistical Analysis
In this work, quantitative descriptive research was carried out based on the responses of the participating health sciences professors to the questionnaire used as an instrument. The research was structured in the following phases (Figure 6): (i) the formulation of the objectives and definition of the research variables; (ii) the sampling and collection of the responses to the questionnaire; (iii) the statistical analysis of the data obtained, and (iv) drawing conclusions.
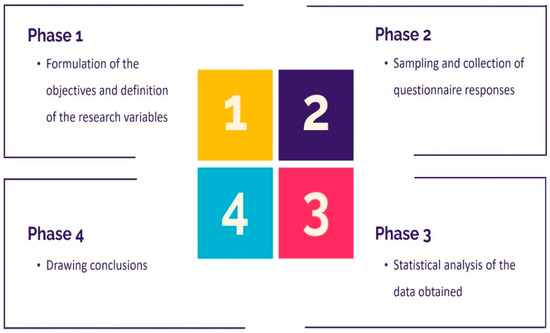
Figure 6.
Research phases.
For the statistical analysis, descriptive statistics were obtained for the responses to the different factors that explain the questionnaire. Since the sample size exceeds 50 participants, the parametric t-test was chosen to be used to compare the mean responses of the professors from private and public universities. To analyze the existence of gender gaps in each of these types of universities, the multifactor analysis of variance (MANOVA) test was used. Finally, linear regression models were computed for each of the factors of the questionnaire with respect to age, among the participants from private and public universities, to analyze the influence of the age of the health sciences professors at each type of university on the assessments of VR. All statistical tests were performed at the 0.05 level of significance.
3. Results
The participating health sciences professors gave very high ratings to the use of VR technologies in the classroom, mainly in terms of their usability and didactic usability and, slightly below this, their technical aspects (Table 2). However, the average level of perceived disadvantages is intermediate–high, although the variation in the responses for the factor measuring disadvantages is the second highest of all factors (46.42%, Table 2). The mean selfconcept regarding digital competence for the use of VR technologies is intermediate–low, this factor being the one with the highest variation relative to the mean (43.46%, Table 2) and the only one for which the responses show positive, although weak, asymmetry. All the other factors show moderate left skewness (Table 2).

Table 2.
Descriptive statistics of the responses (270 participants).
From the Pearson correlation coefficients computed between the responses to the different factors of the questionnaire, we deduce the following observations (Table 3): (i) the only negative correlation is between the factors of selfperception of digital competence and assessment of technical aspects, indicating that a higher rating of technical aspects leads to a lower selfconcept of digital competence; (ii) the level of perceived disadvantages is positively correlated, mainly, with participants’ selfconcept of digital competence, so that a higher selfperception of digital competence leads the participants to identify with a higher degree of the possible disadvantages of using VR; (iii) the strongest correlation is between the factors valuing the technical aspects and usability, indicating that participants link the employability of VR in the classroom to technical features, such as 3D design, realism, and immersiveness, and (iv) valuing the didactic usefulness of VR technologies is moderately correlated with all the other factors analyzed. All the correlation coefficients indicated in Table 3 are statistically significant.

Table 3.
Pearson correlation coefficients of the responses to the different factors of the questionnaire (270 participants).
The two-sample bilateral t-test does not allow for assumptions that there are significant differences between the mean responses to the factors of selfconcept of digital competence, technical aspects, usability, and the disadvantages of VR between Latin American professors from private and public universities (Table 4). However, significant differences by university tenure were identified in terms of the future perception of VR and the assessment of its didactic usability in the health sciences. Specifically, participating professors from public universities rate the future projection of VR technologies 5% higher than their colleagues from private universities, but it is the Latin American professors from private universities who rate its didactic applicability in lectures more highly; they rate it 3% higher than Latin American professors from public universities (Table 4).

Table 4.
Mean responses (out of five) and the statistics of the bilateral t-test for the comparison of the means for independent samples when participants are differentiated by their university tenure (270 participants).
Although there are significant gaps between Latin American private and public universities in the assessment of the didactic aspects and the future projection of VR, no gender differences were identified between the two types of universities (Table 5). In contrast, there are gender gaps in the ratings of selfconcept of digital competence, usability, and the difficulties of using VR (Table 5). While the selfconcept of digital competence of Latin American private university professors is approximately homogeneous between females and males, in Latin American public universities, these competence scores are 25.83% higher in males than in females.

Table 5.
Mean responses (out of 5) and the statistics of the MANOVA test for the comparison of means when participants are differentiated by their university tenure and gender (270 participants).
In the participating private universities, females rate VR usability 7.29% higher than males, while in the participating public universities, there is hardly any difference between females and males. Latin American female professors from public universities rate the level of the disadvantages of VR use 13.29% higher than males, while in the participating private universities, males gave the highest score to the disadvantages of VR, although the difference to females is small (4.76%). The linear regression model performed on the responses of the participating private university professors reveals that age is not a significant explanatory variable for any of the factors in the questionnaire, except for the factor on the assessment of the didactic usefulness of VR (Table 6). However, even in this case, the slope is positive but very close to 0, indicating that the assessment of the didactic use of VR grows very weakly as the age of the participating health sciences professor increases.

Table 6.
Statistics of the linear regression model of the different factors of the questionnaire with respect to the age of the participants among the professors from private universities (270 participants).
In Latin American public universities, on the other hand, age is an explanatory variable for the ratings of the technical aspects, employability, and disadvantages of the didactic use of VR in health sciences lectures (Table 7). For the three factors indicated, the slope of the linear regression model is positive but very close to 0. Consequently, as the age of Latin American professors at public universities increases, the assessment of the technical aspects and usability of VR increases slightly, but so does the level of the perceived disadvantages.

Table 7.
Statistics of the linear regression model of the different factors of the questionnaire with respect to the age of the participants among the professors from public universities (270 participants).
4. Discussion
Latin American health sciences professors report having an intermediate or low selfconcept of digital skills (Table 2). This fact shows that there are no significant differences between health sciences faculty and higher education faculty (in general) in the Latin American region in terms of their selfperception of digital skills [123,124,125,126,127,136]. Likewise, this observation supports the results of previous studies analyzing the selfconcept of digital competence in specific populations of health sciences faculty, which conclude a need to strengthen these digital skills [33,127,128]. However, the variation observed here around the assessment of the selfconcept of digital competence responses (43.46%, Table 2) is the largest of the variations present in the families of responses analyzed, suggesting that there are important differences in the selfconcept of digital skills among participating health sciences faculty. This aspect has not been observed previously in faculty from other areas [126], so it is suggested that a study be conducted to check whether there are differences between the dispersions of the responses on the selfconcept of digital competence among faculty from different areas of knowledge. This would make it possible to confirm whether the dispersion observed here is a phenomenon specific to the area of health sciences and, if so, to identify the underlying reasons for this phenomenon.
Despite expressing a selfconcept of digital competence that could be improved, the participating professors gave high or very high ratings to the use of VR in their lectures (Table 2). In this sense, the highest ratings were obtained for the aspects of usability in the classroom and didactic usefulness. These results are in line with previous works [46,47,67,68,69,70,71,72,73,74,99,100,101,102,113,114], with the exception of the works that focus on professors in engineering areas that also highlight the technical aspects of VR, which is explained by the area of specialization of the professors [116,126]. The level of the perceived disadvantages of VR is intermediate–high, which is lower in any case than the assessment of VR tools (Table 2). This observation is in line with previous work focused on professors in other fields [126] or on higher education faculty in general [114,115,116,117,118,142].
Moreover, the high ratings of VR and the intermediate–high ratings of its disadvantages are compatible observations, given that the literature shows that there are some limitations of VR, such as the technical and human capital requirements, space needs, and faculty training, which are persistent disadvantages, but for which professors do not understand as detracting from the effectiveness of using VR [86,113,117,119]. This fact could explain why the factor valuing disadvantages is weakly correlated with the rest of the factors analyzed (Table 3).
In this study, it has been observed that Latin American health sciences professors at public universities perceive a greater future projection for VR than those in private universities (Table 4). This may be explained by the fact that it is precisely in public universities where there is less implementation of digital technologies [137,138]. However, no significant differences were found by university tenure in the selfconcept of digital competence of health sciences faculty or in the didactic assessment of VR (Table 4). These results differ from those found in previous work on engineering faculty populations, in which the faculty from private universities rated VR significantly higher in terms of its didactic aspects and employability in the classroom than their colleagues from public universities [126]. This proves, therefore, that the area of knowledge is an explanatory variable of VR ratings, as has already been observed in more restricted geographical contexts than the one studied here [142]. It also suggests the need for digital faculty training to be specifically focused on the specific didactic needs of each knowledge area [33,60,66,114].
It has also been shown that the digital gender gap behaves differently among Latin American health sciences professors in private and public universities. Specifically, in the participating public universities, there is a strong gender gap that disadvantages females in terms of their selfperception of digital skills (Table 5). This is consistent with the results on the digital gender gap that have been observed, in general, in Latin American universities [135,136] and with the results obtained among professors in technical areas [126], which identify a wider gender gap in the faculty of public universities. Likewise, it has been found here that, in the participating public universities, there is a certain digital age gap among Latin American health sciences professors (Table 6) that is not found in private universities (Table 7).
This observation is consistent with the results of previous work [126]. In some works, the generation to which the professors belong had been identified as an explanatory variable of the assessments that university professors, in general, make of VR, but without distinguishing by university tenure [142]. Here it has been found that this observation is not made in the same way in Latin American private and public universities, at least among health sciences faculty. This may be due, again, to the different level of digitization that both types of centers have [137,138].
5. Limitations and Lines of Future Research
The quantitative nature of this research limits the scope of its results in the sense that the methodology itself prevents the identification of the reasons for some of the results obtained, such as gender gaps. Consequently, we suggest a qualitative study to complete the analysis carried out here, identifying the reasons for the gender and age gaps found and the reasons for the observed low selfconcept of digital competence of Latin American health sciences professors. In addition, the initial training provided on VR was general and not specifically aimed at the health sciences area. It is suggested that an analogous study be carried out, starting with training specifically on VR in health science education, which would probably generate greater optimism in the participants regarding the didactic use of VR technologies.
Likewise, it would be interesting to extend the sample of participants to other geographical regions and other areas of knowledge so that a differential analysis of the results can be carried out. Likewise, a study should be carried out to evaluate, by means of a specific, validated, and appropriate instrument, the real digital competence of professors, to compare the level of concordance between the selfconcept of their digital skills and their actual digital competence. Finally, it would be useful to complete the results with those resulting from the experience expressed by health sciences students regarding the use of VR technologies.
6. Conclusions
The novel results of the present research relate to the description of the Latin American health sciences professors’ assessment of VR as a didactic resource. Specifically, these professors give high ratings to VR but identify a high level of disadvantages in its use and a low selfconcept of their digital competence. The aspects of VR most valued by Latin American health sciences professors are its user experience characteristics and its didactic employability, unlike, for example, what was found in other studies with engineering professors, whose best ratings correspond to the technical characteristics of VR. In addition, there is a strong inequality in the selfconcept of digital skills expressed by professors. Regarding the mean ratings of VR, there are no significant differences between Latin American health sciences professors from private or public universities, although health sciences professors from public universities see a higher projection for the future use of VR in university teaching than their colleagues from private universities. The behavior of gender and age gaps in the perceptions of VR was different in the participating private and public universities. There is a wider gender gap among public university professors that disadvantages females and a digital age gap that favors younger professors among public university professors, which does not occur in private universities.
Finally, it is recommended that universities increase the digital training of health sciences faculty and that this training be oriented in two directions: (i) work with digital tools such as VR, and (ii) carrying out an approach to this training that is specific to health sciences and to the development of the technopedagogical skills of its faculty.
Author Contributions
Conceptualization, Á.A.-S., P.F.-A., and D.V.; methodology, Á.A.-S., P.F.-A. and D.V.; formal analysis, Á.A.-S., P.F.-A. and D.V.; investigation, Á.A.-S., P.F.-A. and D.V.; data curation, Á.A.-S.; writing—original draft preparation, Á.A.-S., P.F.-A. and D.V.; writing—review and editing, Á.A.-S., P.F.-A. and D.V.; supervision, Á.A.-S., P.F.-A. and D.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The protocol was approved by the Ethics Committee of the Project “Influence of COVID-19 on teaching: digitization of laboratory practices at UCAV” (24 January 2022).
Informed Consent Statement
All participants were informed about the anonymous nature of their participation, why the research is being conducted, how their data will be used, and that under no circumstances would their data be used to identify them.
Data Availability Statement
The data are not publicly available because they are part of a larger project involving more researchers. If you have any questions, please ask the contact author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wang, S.; Parsons, M.; Stone-McLean, J.; Rogers, P.; Boyd, S.; Hoover, K.; Meruvia-Pastor, O.; Gong, M.; Smith, A. Augmented Reality as a Telemedicine Platform for Remote Procedural Training. Sensors 2017, 17, 2294. [Google Scholar] [CrossRef] [PubMed]
- Koulouris, D.; Menychtas, A.; Maglogiannis, I. An IoT-Enabled Platform for the Assessment of Physical and Mental Activities Utilizing Augmented Reality Exergaming. Sensors 2022, 22, 3181. [Google Scholar] [CrossRef] [PubMed]
- Dahl, T.S.; Boulos, M.N.K. Robots in Health and Social Care: A Complementary Technology to Home Care and Telehealthcare? Robotics 2014, 3, 1–21. [Google Scholar] [CrossRef]
- Vergara-Rodríguez, D.; Gómez-Asenjo, A.; Fernández-Arias, P.; Gómez-Vallecillo, A.I.; Lamas-Álvarez, V.E.; Santos-Iglesia, C. Immersive vs. Non-Immersive Virtual Reality Learning Environments. In Proceedings of the 2021 XI International Conference on Virtual Campus (JICV), Salamanca, Spain, 30 September 2021–1 October 2021; pp. 1–3. [Google Scholar] [CrossRef]
- Miguel, C.; Castro, L.; Marques dos Santos, J.P.; Serrão, C.; Duarte, I. Impact of COVID-19 on Medicine Lecturers’ Mental Health and Emergency Remote Teaching Challenges. Int. J. Environ. Res. Public Health 2021, 18, 6792. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.P.; Javaid, M.; Kataria, R.; Tyagi, M.; Haleem, A.; Suman, R. Significant Applications of Virtual Reality for COVID-19 Pandemic. Diabetes Metab. Syndr. 2020, 14, 661–664. [Google Scholar] [CrossRef]
- Petrigna, L.; Musumeci, G. The Metaverse: A New Challenge for the Healthcare System: A Scoping Review. J. Funct. Morphol. Kinesiol. 2022, 7, 63. [Google Scholar] [CrossRef]
- Sánchez-Cabrero, R.; Arigita-García, A.; Barrientos-Fernández, A.; León-Mejía, A.C. Online Explorative Study on the Learning Uses of Virtual Reality Among Early Adopters. JoVE (J. Vis. Exp.) 2019, 153, e60188. [Google Scholar] [CrossRef]
- Sánchez-Cabrero, R.; Costa-Román, O.; Pericacho-Gomez, F.J.; Novillo-López, M.A.; Arigita-García, A.; Barrientos-Fernandez, A. Early Virtual Reality Adopters in Spain: Sociodemographic Profile and Interest in the Use of Virtual Reality as a Learning Tool. Heliyon 2019, 5, 01338. [Google Scholar] [CrossRef]
- Rutkowski, S. Management Challenges in Chronic Obstructive Pulmonary Disease in the COVID-19 Pandemic: Telehealth and Virtual Reality. J. Clin. Med. 2021, 10, 1261. [Google Scholar] [CrossRef]
- Vergara, D.; Rubio, M.P.; Lorenzo, M. On the Design of Virtual Reality Learning Environments in Engineering. Multimodal Technol. Interact. 2017, 1, 11. [Google Scholar] [CrossRef]
- Muhanna, M.A. Virtual Reality and the CAVE: Taxonomy, Interaction Challenges and Research Directions. J. King Saud Univ.-Comput. Inf. Sci. 2015, 27, 344–361. [Google Scholar] [CrossRef]
- Gu, C. Short-Range Noncontact Sensors for Healthcare and Other Emerging Applications: A Review. Sensors 2016, 16, 1169. [Google Scholar] [CrossRef]
- Caponnetto, P.; Casu, M. Update on Cyber Health Psychology: Virtual Reality and Mobile Health Tools in Psychotherapy, Clinical Rehabilitation, and Addiction Treatment. Int. J. Environ. Res. Public Health 2022, 19, 3516. [Google Scholar] [CrossRef]
- Bopp, T.; Stellefson, M. Practical and Ethical Considerations for Schools Using Social Media to Promote Physical Literacy in Youth. Int. J. Environ. Res. Public Health 2020, 17, 1225. [Google Scholar] [CrossRef]
- Riva, G. From Telehealth to E-Health: Internet and Distributed Virtual Reality in Health Care. CyberPsychology Behav. 2000, 3, 989–998. [Google Scholar] [CrossRef]
- Matamala-Gomez, M.; Maselli, A.; Malighetti, C.; Realdon, O.; Mantovani, F.; Riva, G. Virtual Body Ownership Illusions for Mental Health: A Narrative Review. J. Clin. Med. 2021, 10, 139. [Google Scholar] [CrossRef]
- Morimoto, T.; Kobayashi, T.; Hirata, H.; Otani, K.; Sugimoto, M.; Tsukamoto, M.; Yoshihara, T.; Ueno, M.; Mawatari, M. XR (Extended Reality: Virtual Reality, Augmented Reality, Mixed Reality) Technology in Spine Medicine: Status Quo and Quo Vadis. J. Clin. Med. 2022, 11, 470. [Google Scholar] [CrossRef]
- Tian, S.; Yang, W.; Grange, J.M.L.; Wang, P.; Huang, W.; Ye, Z. Smart healthcare: Making medical care more intelligent. Glob. Health J. 2019, 3, 62–65. [Google Scholar] [CrossRef]
- Liu, Z.; Ren, L.; Xiao, C.; Zhang, K.; Demian, P. Virtual Reality Aided Therapy towards Health 4.0: A Two-Decade Bibliometric Analysis. Int. J. Environ. Res. Public Health 2022, 19, 1525. [Google Scholar] [CrossRef]
- Alauddin, M.S.; Baharuddin, A.S.; Mohd Ghazali, M.I. The Modern and Digital Transformation of Oral Health Care: A Mini Review. Healthcare 2021, 9, 118. [Google Scholar] [CrossRef]
- Carpinello, A.; Vezzetti, E.; Ramieri, G.; Moos, S.; Novaresio, A.; Zavattero, E.; Borbon, C. Evaluation of HMDs by QFD for Augmented Reality Applications in the Maxillofacial Surgery Domain. Appl. Sci. 2021, 11, 11053. [Google Scholar] [CrossRef]
- Wu, I.-C.; Lin, Y.-C.; Yien, H.-W.; Shih, F.-Y. Constructing Constraint-Based Simulation System for Creating Emergency Evacuation Plans: A Case of an Outpatient Chemotherapy Area at a Cancer Medical Center. Healthcare 2020, 8, 137. [Google Scholar] [CrossRef] [PubMed]
- Tlapa, D.; Tortorella, G.; Fogliatto, F.; Kumar, M.; Mac Cawley, A.; Vassolo, R.; Enberg, L.; Baez-Lopez, Y. Effects of Lean Interventions Supported by Digital Technologies on Healthcare Services: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 9018. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.N.; Kim, M.J.; Hwang, W.J. Potential of Augmented Reality and Virtual Reality Technologies to Promote Wellbeing in Older Adults. Appl. Sci. 2019, 9, 3556. [Google Scholar] [CrossRef]
- González, F.C.J.; Villegas, O.O.V.; Ramírez, D.E.T.; Sánchez, V.G.C.; Domínguez, H.O. Smart Multi-Level Tool for Remote Patient Monitoring Based on a Wireless Sensor Network and Mobile Augmented Reality. Sensors 2014, 14, 17212–17234. [Google Scholar] [CrossRef] [PubMed]
- Berton, A.; Longo, U.G.; Candela, V.; Fioravanti, S.; Giannone, L.; Arcangeli, V.; Alciati, V.; Berton, C.; Facchinetti, G.; Marchetti, A.; et al. Virtual Reality, Augmented Reality, Gamification, and Telerehabilitation: Psychological Impact on Orthopedic Patients’ Rehabilitation. J. Clin. Med. 2020, 9, 2567. [Google Scholar] [CrossRef]
- Obinikpo, A.A.; Kantarci, B. Big Sensed Data Meets Deep Learning for Smarter Health Care in Smart Cities. J. Sens. Actuator Netw. 2017, 6, 26. [Google Scholar] [CrossRef]
- Yang, Y.; Chan, A.P.C.; Shan, M.; Gao, R.; Bao, F.; Lyu, S.; Zhang, Q.; Guan, J. Opportunities and Challenges for Construction Health and Safety Technologies under the COVID-19 Pandemic in Chinese Construction Projects. Int. J. Environ. Res. Public Health 2021, 18, 13038. [Google Scholar] [CrossRef]
- Chang, A.-H.; Lin, P.-C.; Lin, P.-C.; Lin, Y.-C.; Kabasawa, Y.; Lin, C.-Y.; Huang, H.-L. Effectiveness of Virtual Reality-Based Training on Oral Healthcare for Disabled Elderly Persons: A Randomized Controlled Trial. J. Pers. Med. 2022, 12, 218. [Google Scholar] [CrossRef]
- Hatta, M.H.; Sidi, H.; Siew Koon, C.; Che Roos, N.A.; Sharip, S.; Abdul Samad, F.D.; Wan Xi, O.; Das, S.; Mohamed Saini, S. Virtual Reality (VR) Technology for Treatment of Mental Health Problems during COVID-19: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 5389. [Google Scholar] [CrossRef]
- Riva, G.; Bernardelli, L.; Castelnuovo, G.; Di Lernia, D.; Tuena, C.; Clementi, A.; Pedroli, E.; Malighetti, C.; Sforza, F.; Wiederhold, B.K.; et al. A Virtual Reality-Based Self-Help Intervention for Dealing with the Psychological Distress Associated with the COVID-19 Lockdown: An Effectiveness Study with a Two-Week Follow-Up. Int. J. Environ. Res. Public Health 2021, 18, 8188. [Google Scholar] [CrossRef]
- Fleming, M.; Olsen, D.; Stathes, H.; Boteler, L.; Grossberg, P.; Pfeifer, J.; Schiro, S.; Banning, J.; Skochelak, S. Virtual Reality Skills Training for Health Care Professionals in Alcohol Screening and Brief Intervention. J. Am. Board Fam. Med. 2009, 22, 387–398. [Google Scholar] [CrossRef]
- Bayahya, A.Y.; Alhalabi, W.; AlAmri, S.H. Smart Health System to Detect Dementia Disorders Using Virtual Reality. Healthcare 2021, 9, 810. [Google Scholar] [CrossRef]
- Leemhuis, E.; Giuffrida, V.; Giannini, A.M.; Pazzaglia, M. A Therapeutic Matrix: Virtual Reality as a Clinical Tool for Spinal Cord Injury-Induced Neuropathic Pain. Brain Sci. 2021, 11, 1201. [Google Scholar] [CrossRef]
- Ahmad, M.A.; Singh, D.K.A.; Mohd Nordin, N.A.; Hooi Nee, K.; Ibrahim, N. Virtual Reality Games as an Adjunct in Improving Upper Limb Function and General Health among Stroke Survivors. Int. J. Environ. Res. Public Health 2019, 16, 5144. [Google Scholar] [CrossRef]
- Sánchez-Herrera-Baeza, P.; Cano-de-la-Cuerda, R.; Oña-Simbaña, E.D.; Palacios-Ceña, D.; Pérez-Corrales, J.; Cuenca-Zaldivar, J.N.; Gueita-Rodriguez, J.; Balaguer-Bernaldo de Quirós, C.; Jardón-Huete, A.; Cuesta-Gomez, A. The Impact of a Novel Immersive Virtual Reality Technology Associated with Serious Games in Parkinson’s Disease Patients on Upper Limb Rehabilitation: A Mixed Methods Intervention Study. Sensors 2020, 20, 2168. [Google Scholar] [CrossRef]
- Riaz, W.; Khan, Z.Y.; Jawaid, A.; Shahid, S. Virtual Reality (VR)-Based Environmental Enrichment in Older Adults with Mild Cognitive Impairment (MCI) and Mild Dementia. Brain Sci. 2021, 11, 1103. [Google Scholar] [CrossRef]
- Léger, M.T.; Mekari, S. Simulating the Benefits of Nature Exposure on Cognitive Performance in Virtual Reality: A Window into Possibilities for Education and Cognitive Health. Brain Sci. 2022, 12, 725. [Google Scholar] [CrossRef]
- Baeza-Barragán, M.R.; Labajos, M.T.; Ruiz, C.; Casuso-Holgado, M.J.; Martín-Valero, R. The Use of Virtual Reality Technologies in the Treatment of Duchenne Muscular Dystrophy: Systematic Review. JMIR Mhealth Uhealth 2020, 8, e21576. [Google Scholar] [CrossRef]
- Mishra, R.; Narayanan, M.D.K.; Umana, G.E.; Montemurro, N.; Chaurasia, B.; Deora, H. Virtual Reality in Neurosurgery: Beyond Neurosurgical Planning. Int. J. Environ. Res. Public Health 2022, 19, 1719. [Google Scholar] [CrossRef]
- Rogers, C.; Lau, J.; Huynh, D.; Albertson, S.; Beem, J.; Qian, E. Capturing the Perceived Phantom Limb through Virtual Reality. Adv. Hum.-Comput. Interact. 2016, 2016, 8608972. [Google Scholar] [CrossRef]
- Lin, A.P.C.; Trappey, C.V.; Luan, C.-C.; Trappey, A.J.C.; Tu, K.L.K. A Test Platform for Managing School Stress Using a Virtual Reality Group Chatbot Counseling System. Appl. Sci. 2021, 11, 9071. [Google Scholar] [CrossRef]
- Zeng, N.; Pope, Z.; Lee, J.E.; Gao, Z. Virtual Reality Exercise for Anxiety and Depression: A Preliminary Review of Current Research in an Emerging Field. J. Clin. Med. 2018, 7, 42. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-Y.; Lee, J.-H.; Lee, E.-H. Virtual Experience of Perioperative Patients: Walking in the Patients’ Shoes Using Virtual Reality and Blended Learning. Int. J. Environ. Res. Public Health 2021, 18, 6457. [Google Scholar] [CrossRef] [PubMed]
- Pandrangi, V.C.; Gaston, B.; Appelbaum, N.P.; Albuquerque, F.C.; Levy, M.M.; Larson, R.A. The Application of Virtual Reality in Patient Education. Ann. Vasc. Surg. 2019, 59, 184–189. [Google Scholar] [CrossRef]
- Van der Kruk, S.R.; Zielinski, R.; MacDougall, H.; Hughes-Barton, D.; Gunn, K.M. Virtual reality as a patient education tool in healthcare: A scoping review. Patient Educ. Couns. 2022, 105, 1928–1942. [Google Scholar] [CrossRef]
- Sheperd, T.; Trinder, M.; Theophilus, M. Does Virtual Reality in the Perioperative Setting for Patient Education Improve Understanding? A Scoping Review. Surg. Pract. Sci. 2022, 10, 100101. [Google Scholar] [CrossRef]
- Habak, S.; Bennett, J.; Davies, A.; Davies, M.; Christensen, H.; Boydell, K.M. Edge of the Present: A Virtual Reality Tool to Cultivate Future Thinking, Positive Mood and Wellbeing. Int. J. Environ. Res. Public Health 2021, 18, 140. [Google Scholar] [CrossRef]
- Lim, S.-G.; Jung, S.-H.; Huh, J.-H. Visual Algorithm of VR E-Sports for Online Health Care. Healthcare 2021, 9, 824. [Google Scholar] [CrossRef]
- Dębska, M.; Polechoński, J.; Mynarski, A.; Polechoński, P. Enjoyment and Intensity of Physical Activity in Immersive Virtual Reality Performed on Innovative Training Devices in Compliance with Recommendations for Health. Int. J. Environ. Res. Public Health 2019, 16, 3673. [Google Scholar] [CrossRef]
- Hughes, S.; Warren-Norton, K.; Spadafora, P.; Tsotsos, L.E. Supporting Optimal Aging through the Innovative Use of Virtual Reality Technology. Multimodal Technol. Interact. 2017, 1, 23. [Google Scholar] [CrossRef]
- Montana, J.I.; Matamala-Gomez, M.; Maisto, M.; Mavrodiev, P.A.; Cavalera, C.M.; Diana, B.; Mantovani, F.; Realdon, O. The Benefits of emotion Regulation Interventions in Virtual Reality for the Improvement of Wellbeing in Adults and Older Adults: A Systematic Review. J. Clin. Med. 2020, 9, 500. [Google Scholar] [CrossRef]
- Nobari, H.; Rezaei, S.; Sheikh, M.; Fuentes-García, J.P.; Pérez-Gómez, J. Effect of Virtual Reality Exercises on the Cognitive Status and Dual Motor Task Performance of the Aging Population. Int. J. Environ. Res. Public Health 2021, 18, 8005. [Google Scholar] [CrossRef]
- Nichols, S.; Patel, H. Health and Safety Implications of Virtual Reality: A Review of Empirical Evidence. Appl. Ergon. 2002, 33, 251–271. [Google Scholar] [CrossRef]
- Behm-Morawitz, E. Mirrored selves: The Influence of Self-Presence in a Virtual World on Health, Appearance, and Well-Being. Comput. Hum. Behav. 2013, 29, 119–128. [Google Scholar] [CrossRef]
- Gourlay, D.; Lun, K.C.; Liya, G. Virtual Reality and Telemedicine for Home Health Care. Comput. Graph. 2000, 24, 695–699. [Google Scholar] [CrossRef]
- Brown-Johnson, C.G.; Berrean, B.; Cataldo, J.K. Development and Usability Evaluation of the mHealth Tool for Lung Cancer (mHealth TLC): A Virtual World Health Game for Lung Cancer Patients. Patient Educ. Couns. 2015, 98, 506–511. [Google Scholar] [CrossRef]
- Liu, Z.; Yang, Z.; Xiao, C.; Zhang, K.; Osmani, M. An Investigation into Art Therapy Aided Health and Well-Being Research: A 75-Year Bibliometric Analysis. Int. J. Environ. Res. Public Health 2022, 19, 232. [Google Scholar] [CrossRef]
- Mantovani, F.; Castelnuovo, G.; Gaggioli, A.; Riva, G. Virtual Reality Training for Health-Care Professionals. CyberPsychology Behav. 2003, 6, 389–395. [Google Scholar] [CrossRef]
- Patterson, D.R.; Drever, S.; Soltani, M.; Sharar, S.R.; Wiechman, S.; Meyer, W.J.; Hoffman, H.G. A Comparison of Interactive Immersive Virtual Reality and Still Nature Pictures as Distraction-Based Analgesia in Burn Wound Care. Burns, 2022; in press. [Google Scholar] [CrossRef]
- O’Connor, M.; Stowe, J.; Potocnik, J.; Giannotti, N.; Murphy, S.; Rainford, L. 3D Virtual Reality Simulation in Radiography Education: The Students’ Experience. Radiography 2020, 27, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Partner, A.; Shiner, N.; Hyde, E.; Errett, S. First Year Student Radiographers’ Perceptions of a One-Week Simulation-Based Education Package Designed to Increase Clinical Placement Capacity. Radiography 2022, 28, 577–585. [Google Scholar] [CrossRef] [PubMed]
- Sapkaroski, D.; Mundy, M.; Dimmock, M.R. Virtual Reality versus Conventional Clinical Role-Play for Radiographic Positioning Training: A Students’ Perception Study. Radiography 2020, 26, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Viglialoro, R.M.; Condino, S.; Turini, G.; Carbone, M.; Ferrari, V.; Gesi, M. Augmented Reality, Mixed Reality, and Hybrid Approach in Healthcare Simulation: A Systematic Review. Appl. Sci. 2021, 11, 2338. [Google Scholar] [CrossRef]
- Birckhead, B.; Khalil, C.; Liu, X.; Conovitz, S.; Rizzo, A.; Danovitch, I.; Bullock, K.; Spiegel, B. Recommendations for Methodology of Virtual Reality Clinical Trials in Health Care by an International Working Group: Iterative Study. JMIR Ment Health 2019, 6, e11973. [Google Scholar] [CrossRef]
- Balian, S.; McGovern, S.K.; Abella, B.S.; Blewer, A.L.; Leary, M. Feasibility of an Augmented Reality Cardiopulmonary Resuscitation Training System for Health Care Providers. Heliyon 2019, 5, e02205. [Google Scholar] [CrossRef]
- Carlson, K.J.; Gagnon, D.J. Augmented Reality Integrated Simulation Education in Health Care. Clin. Simul. Nurs. 2016, 12, 123–127. [Google Scholar] [CrossRef]
- Hirt, J.; Beer, T. Use and Impact of Virtual Reality Simulation in Dementia Care Education: A Scoping Review. Nurse Educ. Today 2020, 84, 104207. [Google Scholar] [CrossRef]
- Shorey, S.; Debby, E. The Use of Virtual Reality Simulation among Nursing Students and Registered Nurses: A Systematic Review. Nurse Educ. Today 2020, 98, 104662. [Google Scholar] [CrossRef]
- McCarthy, C.J.; Uppot, R.N. Advances in Virtual and Augmented Reality—Exploring the Role in Health-care Education. J. Radiol. Nurs. 2019, 38, 104–105. [Google Scholar] [CrossRef]
- Liaw, S.Y.; Wu, L.T.; Soh, S.L.H.; Ringsted, C.; Lau, T.C.; Lim, W.S. Virtual Reality Simulation in Interprofessional Round Training for Health Care Students: A Qualitative Evaluation Study. Clin. Simul. Nurs. 2020, 45, 42–46. [Google Scholar] [CrossRef]
- Plotzky, C.; Lindwedel, U.; Sorber, M.; Loessl, B.; König, P.; Kunze, C.; Kugler, C.; Meng, M. Virtual Reality Simulations in Nurse Education: A Systematic Mapping Review. Nurse Educ. Today 2021, 101, 104868. [Google Scholar] [CrossRef]
- Bayram, S.B.; Caliskan, N. Effect of a Game-Based Virtual Reality Phone Application on Tracheostomy Care Education for Nursing Students: A Randomized Controlled Trial. Nurse Educ. Today 2019, 79, 25–31. [Google Scholar] [CrossRef]
- Park, J.-S.; Jung, Y.-J.; Lee, G. Virtual Reality-Based Cognitive–Motor Rehabilitation in Older Adults with Mild Cognitive Impairment: A Randomized Controlled Study on Motivation and Cognitive Function. Healthcare 2020, 8, 335. [Google Scholar] [CrossRef]
- Gachet Páez, D.; Aparicio, F.; De Buenaga, M.; Padrón, V. Personalized Health Care System with Virtual Reality Rehabilitation and Appropriate Information for Seniors. Sensors 2012, 12, 5502–5516. [Google Scholar] [CrossRef]
- Varela-Aldás, J.; Buele, J.; Ramos Lorente, P.; García-Magariño, I.; Palacios-Navarro, G. A Virtual Reality-Based Cognitive Telerehabilitation System for Use in the COVID-19 Pandemic. Sustainability 2021, 13, 2183. [Google Scholar] [CrossRef]
- Aloyuni, S.; Alharbi, R.; Kashoo, F.; Alqahtani, M.; Alanazi, A.; Alzhrani, M.; Ahmad, M. Knowledge, Attitude, and Barriers to Telerehabilitation-Based Physical Therapy Practice in Saudi Arabia. Healthcare 2020, 8, 460. [Google Scholar] [CrossRef]
- Norouzi-Gheidari, N.; Hernandez, A.; Archambault, P.S.; Higgins, J.; Poissant, L.; Kairy, D. Feasibility, Safety and Efficacy of a Virtual Reality Exergame System to Supplement Upper Extremity Rehabilitation Post-Stroke: A Pilot Randomized Clinical Trial and Proof of Principle. Int. J. Environ. Res. Public Health 2020, 17, 113. [Google Scholar] [CrossRef]
- Demolder, C.; Molina, A.; Hammond, F.L.; Yeo, W.-H. Recent Advances in Wearable Biosensing Gloves and Sensory Feedback Biosystems for Enhancing Rehabilitation, Prostheses, Healthcare, and Virtual Reality. Biosens. Bioelectron. 2021, 190, 113443. [Google Scholar] [CrossRef]
- Hwang, N.-K.; Shim, S.-H. Use of Virtual Reality Technology to Support the Home Modification Process: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 11096. [Google Scholar] [CrossRef]
- Kim, S.-H.; Kim, H.J.; Shin, G. Self-Management Mobile Virtual Reality Program for Women with Gestational Diabetes. Int. J. Environ. Res. Public Health 2021, 18, 1539. [Google Scholar] [CrossRef] [PubMed]
- Won, A.S.; Bailey, J.; Bailenson, J.; Tataru, C.; Yoon, I.A.; Golianu, B. Immersive Virtual Reality for Pediatric Pain. Children 2017, 4, 52. [Google Scholar] [CrossRef] [PubMed]
- Klas, J.; Grzywacz, A.; Kulszo, K.; Grunwald, A.; Kluz, N.; Makaryczew, M.; Samardakiewicz, M. Challenges in the Medical and Psychosocial Care of the Paediatric Refugee—A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 10656. [Google Scholar] [CrossRef] [PubMed]
- Antón-Sancho, Á.; Fernández-Arias, P.; Vergara, D. Assessment of Virtual Reality among University Professors: Influence of the Digital Generation. Computers 2022, 11, 92. [Google Scholar] [CrossRef]
- Noghabaei, M.; Heydarian, A.; Balali, V.; Han, K. Trend Analysis on Adoption of Virtual and Augmented Reality in the Architecture, Engineering, and Construction Industry. Data 2020, 5, 26. [Google Scholar] [CrossRef]
- Wang, P.; Wu, P.; Wang, J.; Chi, H.-L.; Wang, X. A Critical Review of the Use of Virtual Reality in Construction Engineering Education and Training. Int. J. Environ. Res. Public Health 2018, 15, 1204. [Google Scholar] [CrossRef]
- Moro, C.; McLean, M. Supporting Students’ Transition to University and Problem-Based Learning. Med. Sci. Educ. 2017, 27, 353–361. [Google Scholar] [CrossRef]
- Vergara-Rodríguez, D.; Antón-Sancho, Á.; Fernández-Arias, P. Variables Influencing Professors’ Adaptation to Digital Learning Environments during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 3732. [Google Scholar] [CrossRef]
- Kasurinen, J. Usability Issues of Virtual Reality Learning Simulator in Healthcare and Cybersecurity. Procedia Comput. Sci. 2017, 119, 341–349. [Google Scholar] [CrossRef]
- Castiblanco, I.A.; Cepeda, L.C.; Violante, M.G.; Marcolin, F.; Vezzetti, E. Commonly Used External TAM Variables in e-Learning, Agriculture and Virtual Reality Applications. Future Internet 2021, 13, 7. [Google Scholar] [CrossRef]
- Kovacevic, A.; Bär, S.; Starystach, S.; Elsässer, M.; van der Locht, T.; Mohammadi Motlagh, A.; Ostermayer, E.; Oberhoffer-Fritz, R.; Ewert, P.; Gorenflo, M.; et al. Fetal Cardiac Services during the COVID-19 Pandemic: How Does It Affect Parental Counseling? J. Clin. Med. 2021, 10, 3423. [Google Scholar] [CrossRef]
- Fernández-Arias, P.; Antón-Sancho, Á.; Vergara, D.; Barrientos, A. Soft Skills of American University Teachers: Self-Concept. Sustainability 2021, 13, 12397. [Google Scholar] [CrossRef]
- Gillespie, G.L.; Farra, S.; Regan, S.L.; Brammer, S.V. Impact of Immersive Virtual Reality Simulations for Changing Knowledge, Attitudes, And Behaviors. Nurse Educ. Today 2021, 105, 105025. [Google Scholar] [CrossRef]
- Qiao, J.; Xu, J.; Li, L.; Ouyang, Y.-Q. The Integration of Immersive Virtual Reality Simulation in Interprofessional Education: A Scoping Review. Nurse Educ. Today 2021, 98, 104773. [Google Scholar] [CrossRef]
- Riva, G. Virtual Reality for Health Care: The Status of Research. CyberPsychology Behav. 2002, 5, 219–225. [Google Scholar] [CrossRef]
- Birt, J.; Stromberga, Z.; Cowling, M.; Moro, C. Mobile Mixed Reality for Experiential Learning and Simulation in Medical and Health Sciences Education. Information 2018, 9, 31. [Google Scholar] [CrossRef]
- Liaw, S.Y.; Ooi, S.L.; Mildon, R.; Ang, E.N.K.; Lau, T.C.; Chua, W.L. Translation of an Evidence-Based Virtual Reality Simulation-Based Interprofessional Education into Health Education Curriculums: An Implementation Science Method. Nurse Educ. Today 2022, 110, 105262. [Google Scholar] [CrossRef]
- Kamińska, D.; Sapiński, T.; Wiak, S.; Tikk, T.; Haamer, R.E.; Avots, E.; Helmi, A.; Ozcinar, C.; Anbarjafari, G. Virtual Reality and Its Applications in Education: Survey. Information 2019, 10, 318. [Google Scholar] [CrossRef]
- Chen, F.; Leng, Y.; Ge, J.; Wang, D.; Li, C.; Chen, B.; Sun, Z. Effectiveness of Virtual Reality in Nursing Education: Meta-Analysis. J. Med. Internet Res. 2020, 22, e18290. [Google Scholar] [CrossRef]
- Kyaw, B.M.; Saxena, N.; Posadzki, P.; Vseteckova, J.; Nikolaou, C.K.; George, P.P.; Divakar, U.; Masiello, I.; Kononowicz, A.A.; Zary, N.; et al. Virtual Reality for Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e12959. [Google Scholar] [CrossRef]
- Mäkinen, H.; Haavisto, E.; Havola, S.; Koivisto, J.-M. User Experiences of Virtual Reality Technologies for Healthcare in Learning: An Integrative Review. Behav. Inf. Technol. 2022, 41, 1–17. [Google Scholar] [CrossRef]
- King, D.; Tee, S.; Falconer, L.; Angell, C.; Holley, D.; Mills, A. Virtual Health Education: Scaling Practice to Transform Student Learning: Using Virtual Reality Learning Environments in Healthcare Education to Bridge the Theory/Practice Gap and Improve Patient Safety. Nurse Educ. Today 2018, 71, 7–9. [Google Scholar] [CrossRef] [PubMed]
- López-Chávez, O.; Rodríguez, L.-F.; Gutierrez-Garcia, J.-O. A Comparative Case Study of 2D, 3D and Immersive-Virtual-Reality Applications for Healthcare Education. Int. J. Med. Inform. 2020, 141, 104226. [Google Scholar] [CrossRef] [PubMed]
- Nakai, K.; Terada, S.; Takahara, A.; Hage, D.; Tubbs, R.S.; Iwanaga, J. Anatomy Education for Medical Students in a Virtual Reality Workspace: A Pilot Study. Clin. Anat. 2022, 35, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y. Virtual Reality Simulation for Disaster Preparedness Training in Hospitals: Integrated Review. J. Med. Internet Res. 2022, 24, e30600. [Google Scholar] [CrossRef]
- Touloudi, E.; Hassandra, M.; Galanis, E.; Goudas, M.; Theodorakis, Y. Applicability of an Immersive Virtual Reality Exercise Training System for Office Workers during Working Hours. Sports 2022, 10, 104. [Google Scholar] [CrossRef]
- Alam, F.; Matava, C. A New Virtual World? The Future of Immersive Environments in Anesthesiology. Anesth. Analg. 2022, 135, 230–238. [Google Scholar] [CrossRef]
- Gasteiger, N.; Van-der-Veer, S.N.; Wilson, P.; Dowding, D. How, for Whom, and in Which Contexts or Conditions Augmented and Virtual Reality Training Works in Upskilling Health Care Workers: Realist Synthesis. JMIR Serious Games 2022, 10, e31644. [Google Scholar] [CrossRef]
- Jiang, H.; Vimalesvaran, S.; Wang, J.K.; Lim, K.B.; Mogali, S.R.; Car, L.T. Virtual Reality in Medical Students’ Education: Scoping Review. JMIR Med. Educ. 2022, 8, e34860. [Google Scholar] [CrossRef]
- Spreij, L.A.; Visser-Meily, J.M.A.; Sibbel, J.; Gosselt, I.K.; Nijboer, T.C.W. Feasibility and User-Experience of Virtual Reality in Neuropsychological Assessment Following Stroke. Neuropsychol. Rehabil. 2022, 32, 499–519. [Google Scholar] [CrossRef]
- Pardini, S.; Gabrielli, S.; Dianti, M.; Novara, C.; Zucco, G.M.; Mich, O.; Forti, S. The Role of Personalization in the User Experience, Preferences and Engagement with Virtual Reality Environments for Relaxation. Int. J. Environ. Res. Public Health 2022, 19, 7237. [Google Scholar] [CrossRef]
- Saxena, N.; Kyaw, B.M.; Vseteckova, J.; Dev, P.; Paul, P.; Lim, K.T.K.; Kononowicz, A.A.; Masiello, I.; Tudor-Car, L.; Nikolaou, C.K.; et al. Virtual Reality Environments for Health Professional Education. Cochrane Database Syst. Rev. 2018, 2, CD012090. [Google Scholar] [CrossRef]
- Vergara, D.; Antón-Sancho, Á.; Extremera, J.; Fernández-Arias, P. Assessment of Virtual Reality as a Didactic Resource in Higher Education. Sustainability 2021, 13, 12730. [Google Scholar] [CrossRef]
- Hsin, L.J.; Chao, Y.P.; Chuang, H.H.; Kuo, T.B.J.; Yang, C.C.H.; Huang, C.-G.; Kang, C.J.; Lin, W.-N.; Fang, T.-J.; Li, H.-Y.; et al. Mild Simulator Sickness Can Alter Heart Rate Variability, Mental Workload, and Learning Outcomes in a 360° Virtual Reality Application for Medical Education: A Post Hoc Analysis of a Randomized Controlled Trial. Virtual Real. 2022. [Google Scholar] [CrossRef]
- Chao, Y.P.; Kang, C.J.; Chuang, H.H.; Hsieh, M.-J.; Chang, Y.-C.; Kuo, T.B.J.; Yang, C.C.H.; Huang, C.-G.; Fang, T.-J.; Li, H.-Y.; et al. Comparison of the Effect of 360° versus Two-Dimensional Virtual Reality Video on History Taking and Physical Examination Skills Learning among Undergraduate Medical Students: A Randomized Controlled Trial. Virtual Real. 2022. [Google Scholar] [CrossRef]
- Muñoz, E.G.; Fabregat, R.; Bacca-Acosta, J.; Duque-Méndez, N.; Avila-Garzon, C. Augmented Reality, Virtual Reality, and Game Technologies in Ophthalmology Training. Information 2022, 13, 222. [Google Scholar] [CrossRef]
- Ojala, S.; Sirola, J.; Nykopp, T.; Kröger, H.; Nuutinen, H. The Impact of Teacher’s Presence on Learning Basic Surgical Tasks with Virtual Reality Headset among Medical Students. Med. Educ. Online 2022, 27, 2050345. [Google Scholar] [CrossRef]
- Saab, M.M.; Landers, M.; Murphy, D.; O’Mahony, B.; Cooke, E.; O’Driscoll, M.; Hegarty, J. Nursing Students’ Views of Using Virtual Reality in Healthcare: A Qualitative Study. J. Clin. Nurs. 2022, 31, 1228–1242. [Google Scholar] [CrossRef]
- Chang, C.-Y.; Sung, H.-Y.; Guo, J.-L.; Chang, B.-Y.; Kuo, F.-R. Effects of Spherical Video-Based Virtual Reality on Nursing Students’ Learning Performance in Childbirth Education Training. Interact. Learn. Environ. 2022, 30, 400–416. [Google Scholar] [CrossRef]
- Behmadi, S.; Asadi, F.; Okhovati, M.; Ershad-Sarabi, R. Virtual Reality-Based Medical Education Versus Lecture-Based Method in Teaching Start Triage Lessons in Emergency Medical Students: Virtual Reality in Medical Education. J. Adv. Med. Educ. Prof. 2022, 10, 48–53. [Google Scholar] [CrossRef]
- Dincelli, E.; Yayla, A. Immersive Virtual Reality in the Age of the Metaverse: A Hybrid-Narrative Review Based on the Technology Affordance Perspective. J. Strateg. Inform. Syst. 2022, 31, 101717. [Google Scholar] [CrossRef]
- Yu, M.; Yang, M.R. Effectiveness and Utility of Virtual Reality Infection Control Simulation for Children with COVID-19: Quasi-Experimental Study. JMIR Serious Games 2022, 10, e36707. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Car, L.; Poon, S.; Kyaw, B.M.; Cook, D.A.; Ward, V.; Atun, R.; Majeed, A.; Johnston, J.; Van-der-Kleij, R.M.J.J.; Molokhia, M.V.; et al. Digital Education for Health Professionals: An Evidence Map, Conceptual Framework, and Research Agenda. J. Med. Internet Res. 2022, 24, e31977. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Poyato, M.J.; Eito-Mateo, A.; Mira-Tamayo, D.C.; Matías-Solanilla, A. Digital Skills, ICTs and Students’ Needs: A Case Study in Social Work Degree, University of Zaragoza (Aragón-Spain). Educ. Sci. 2022, 12, 443. [Google Scholar] [CrossRef]
- Vergara, D.; Antón-Sancho, A.; Dávila, L.P.; Fernández-Arias, P. Virtual Reality as a Didactic Resource from the Perspective of Engineering Teachers. Comput. Appl. Eng. Educ. 2022, 30, 1086–1101. [Google Scholar] [CrossRef]
- Antón-Sancho, Á.; Sánchez-Calvo, M. Influence of Knowledge Area on the Use of Digital Tools during the COVID-19 Pandemic among Latin American Professors. Educ. Sci. 2022, 12, 635. [Google Scholar] [CrossRef]
- Kröplin, J.; Huber, T.; Geis, C.; Braun, B.; Fritz, T. eSurgery—Digital Transformation in Surgery, Surgical Education and Training: Survey Analysis of the Status Quo in Germany. Eur. Surg. 2022, 54, 249–258. [Google Scholar] [CrossRef]
- Whewell, E.; Caldwell, H.; Frydenberg, M.; Andone, D. Changemakers as Digital Makers: Connecting and Co-Creating. Educ. Inf. Technol. 2022, 27, 6691–6713. [Google Scholar] [CrossRef]
- Pottle, J. Virtual Reality and the Transformation of Medical Education. Future Health J. 2019, 6, 181–185. [Google Scholar] [CrossRef]
- Basco, A.I.; Lavena, C. Competencias y Habilidades Para la Cuarta Revolución Industrial en El Contexto de Pandemia; Inter-American Development Bank (IDB): Washington, DC, USA, 2021. [Google Scholar] [CrossRef]
- Curioso, W.H. Building Capacity and Training for Digital Health: Challenges and Opportunities in Latin America. J. Med. Internet Res. 2019, 21, e16513. [Google Scholar] [CrossRef]
- Luo, X.; Wu, W.; Zúñiga-Cañón, C.; Lozano-Garzón, C. From Great Wall to the Andes: Sino-Latin America Collaborations on Urban Computing, Virtual Reality, and Visualization Research. In Proceedings of the 2016 International Conference on Virtual Reality and Visualization (ICVRV), Hangzhou, China, 24–26 September 2016; pp. 346–349. [Google Scholar] [CrossRef]
- Medina-Romero, M.A. Legal Framework for Hasty Digitization in Educational Institutions of Latin American Countries during the COVID-19 Epidemic. J. Posit. Sch. Psychol. 2022, 6, 5392–5404. [Google Scholar] [CrossRef]
- Rodríguez-Abitia, G.; Martínez-Pérez, S.; Ramirez-Montoya, M.S.; Lopez-Caudana, E. Digital Gap in Universities and Challenges for Quality Education: A Diagnostic Study in Mexico and Spain. Sustainability 2020, 12, 9069. [Google Scholar] [CrossRef]
- Antón-Sancho, Á.; Vergara, D.; Lamas-Álvarez, V.E.; Fernández-Arias, P. Digital Content Creation Tools: American University Teachers’ Perception. Appl. Sci. 2021, 11, 11649. [Google Scholar] [CrossRef]
- Rama, C. University Virtualisation in Latin America. Int. J. Educ. Technol. High. Educ. 2014, 11, 32–41. [Google Scholar] [CrossRef][Green Version]
- Vergara, D.; Antón-Sancho, A.; Fernández-Arias, P. Player Profiles for Game-Based Applications in Engineering Education. Comput. Appl. Eng. Educ. 2022. [Google Scholar] [CrossRef]
- UNESCO Institute for Statistics. International Standard Classification of Education ISCED 2011; UNESCO-UIS: Montreal, QC, Canada, 2012; Available online: http://uis.unesco.org/sites/default/files/documents/international-standard-classification-of-education-isced-2011-en.pdf (accessed on 23 October 2022).
- Streiner, D.L. Starting at the Beginning: An Introduction to Coefficient Alpha and Internal Consistency. J. Pers. Med. 2003, 80, 99–103. [Google Scholar] [CrossRef]
- Schmitt, T.A. Current Methodological Considerations in Exploratory and Confirmatory Factor Analysis. J. Psychoeduc. Assess. 2011, 29, 304–321. [Google Scholar] [CrossRef]
- Antón-Sancho, Á.; Vergara, D.; Fernández-Arias, P.; Ariza-Echeverri, E.A. Didactic Use of Virtual Reality in Colombian Universities: Professors’ Perspective. Multimodal Technol. Interact. 2022, 6, 38. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).