Abstract
The aim of this study was to evaluate the relationship between visual functions and road traffic accidents (RTAs) by meta-analysis of observational studies. The analysis included all drivers of motor vehicles, regardless of age, and those using private or public transport. Self-reported visual outcomes were excluded. The risk of RTA in patients with reduced visual acuity was observed in commercial drivers in cross-sectional studies (PR 1.54, 95% CI 1.26–1.88), but not in private drivers in cohort (RR 1.04, 95% CI 0.74–1.46) or case–control studies (OR 1.04, 95% CI 0.78–1.40). A non-statistically significant association between colour vision defects and RTA was observed in cross-sectional studies (PR 1.50, 95% CI 0.91–2.45). No evidence was found for an increased risk of accidents in people with reduced stereopsis. In older adults with abnormal contrast sensitivity, a weak risk of RTA was observed in cohort studies. Evidence from low-quality cross-sectional studies suggests an increased risk of RTAs among commercial drivers with reduced visual acuity. The few case–control and cohort studies identified did not show an association between accident occurrence and visual function. Attention needs to be paid to this issue to facilitate the conduct of high-quality research that can support the development of road safety policies.
1. Introduction
The World Health Organization (WHO) reports that the annual average number of deaths from road traffic accidents (RTAs) was 1.19 million in 2021. Furthermore, RTAs were the primary cause of mortality among children and young adults aged 5–29 years, with 92% of fatalities occurring in low- and middle-income countries. This underscores the critical need to prioritise road safety as a public health concern [1].
In 2020, the United Nations General Assembly adopted resolution 74/299, thereby proclaiming the Decade of Action for Road Safety 2021–2030. This initiative was established with the objective of reducing road traffic deaths and injuries, which are recognised as posing a significant threat to the sustainable development of countries worldwide. Furthermore, it is acknowledged that road transport is a complex system, necessitating the harmonious interaction between people, vehicles, and road infrastructure to ensure a high level of safety [2].
Driving is a complex task involving motor, visual, auditory, and executive functions that are essential for human information processing and decision making. It has been estimated that 90% of this information comes from vision and is directly related to reaction time and the response to the perception of the different traffic situations faced by the driver [3]. There are significant differences in visual standards for driving between countries, including the type of tests required to obtain a driving licence and the frequency of re-assessment. Visual acuity is the most commonly used measure, but when used alone it can be a poor predictor and miss the impact of other factors [4].
In order to improve road safety, it is necessary to be aware of all the preventable risk factors for RTAs, which differ according to the age of the drivers [5]. The relationship between risk factors and vision has been studied in older adults with eye diseases such as glaucoma and cataracts, but other types of visual changes such as stereopsis, contrast sensitivity and colour vision abnormalities can affect healthy young people.
The visual system is made up of the refractive, sensory, anatomophysiological and oculomotor subsystems that interact to respond to stimuli while driving. Its functioning has therefore been the subject of worldwide research, to understand the relationship between vision and driving, and is the basis of the regulatory standards for obtaining a driving licence in all countries. A limitation of the existing literature is the use of small sample sizes in many of the studies, which may have an impact on the reliability of the findings. This makes it challenging to ascertain the likely magnitude of the effect of visual impairment on accidents, which is crucial for decision making by road safety regulators.
Conversely, it is widely recognised that, in addition to age, a number of chronic medical conditions can contribute to the deterioration of vision and, consequently, to a reduction in the ability to react effectively while driving [6]. One narrative systematic review has analysed the impact of some visual disorders and impairments on the risk of motor vehicle crashes (MVCs) [7]. Other systematic reviews with meta-analyses have shown positive associations between visual impairment and the risk of being involved in an MVC in low- and middle-income countries, with a 46% higher risk of crashing among those with poor visual acuity and a 36% higher risk among those with impaired colour vision [8]. With limited evidence based on a small number of studies, a direct association between impaired contrast sensitivity (40% higher risk), visual acuity (21% higher risk) and MVCs has also been suggested [9].
Although there appears to be sufficient evidence, the present review focuses mainly on studies conducted in healthy individuals, i.e., subjects who have not been selected for having a systemic or ocular disease, regardless of age. Paradoxically, two-thirds of traffic deaths occur in people of working age (18–59 years) [1], the age group with the highest concentration of healthy people and the largest number of people on the road every day.
This manuscript is structured as follows: Section 1 introduces the problem of road traffic accidents and the importance of studying aspects of visual function; Section 2 explicitly describes the methodology used to develop the study; Section 3 presents the qualitative and quantitative results obtained from the information collected; and Section 4 discusses the findings and the limitations of the review.
Therefore, the aim of this systematic review was to evaluate the relationship between visual functions and road traffic accidents (RTAs) through a meta-analysis of observational studies.
2. Materials and Methods
2.1. Systematic Literature Search
The electronic search was conducted in January 2022 in the databases Medline (PubMed), Embase, Cochrane Central Register of Controlled Trials (CENTRAL) (London, UK) and Cochrane Database of Systematic Reviews (Ovid) (Philadelphia, PA, USA), LILACS, APA PsycNET, CINAHL, and TRID (the TRIS and ITRD database) and in grey literature databases (Opengrey (Nancy, France), EThOS (London, UK), and TDX (Barcelona, Spain)).
The strategy used in PubMed ((Drivers OR Automobile Driving OR Motorcycles OR Motor Vehicles) AND (Vision Disorders OR visual function OR Vision, Ocular OR Night Vision OR Refractive Errors OR Visual Acuity OR Color Vision OR stereopsis OR Depth Perception OR Contrast Sensitivity OR visual abilities) AND (Accidents, Traffic OR motor vehicle collision OR motor vehicle crash)) was adapted to the other indices according to the respective thesauri. All results were exported to the collaborative web application Rayyan [10] for duplicate detection and removal and title and abstract reading.
In addition, the bibliographic references of all the selected articles were checked.
2.2. Criteria for Study Selection
Observational studies that had evaluated the association between a visual function (visual acuity, stereopsis, colour vision, or contrast sensitivity) and the occurrence of RTAs in drivers of all ages, in private or public transport, and in any type of motor vehicle were included. Visual functions could have been assessed with any type of test or be expressed on any measurement scale, but those studies based on self-reported outcomes were excluded from this meta-analysis.
The outcome of interest was RTAs reported through police records or self-report, regardless of whether the driver was at fault or whether the event resulted in injury.
Publications in English or Spanish were included. No date restrictions were imposed.
The initial selection was made by independent reading of titles and abstracts (DG and FR) and disagreements were resolved by consensus.
2.3. Data Extraction and Quality Assessment of Studies
Information was extracted independently by two of the authors (DG and FR) using Microsoft Excel with the following data: author, title, year, country, study design, number of participants, age, sex, time of follow-up (cohorts), type of transport and vehicle, definition and outcome of each visual function assessed, definition and frequency of RTAs, measure of association (odds ratio [OR], risk ratio [RR], prevalence ratio [PR] and hazard ratio [HR]) or data for its calculation, and adjustment variables used.
For visual acuity, colour vision, and contrast sensitivity outcomes, preference was given to data from both eyes or, alternatively, from the eye with better vision.
If the information required by the study protocol was not described in the report analysed, previous reports of the same study were consulted.
Publications with data from the same study were excluded to ensure that only a single report was included.
Study quality was assessed using the National Heart, Lung, and Blood Institute tool, which assigns a quality rating of good, fair, or poor. The tool includes 14 criteria for observational cohort and cross-sectional studies and 12 criteria for case–control studies [11]. For cohort and cross-sectional studies, a score of 12–14 was considered good quality, 9–11 as fair quality, and ≤8 as poor quality. For case–control studies, a score of 11–12 was considered good quality, 8–10 as fair quality and ≤7 as poor quality. Each study was assessed by two authors (DG and FR), and conflicting assessments were adjudicated by a third author (EI).
2.4. Statistical Analysis
Estimates of association (OR, RR, PR, and HR) and their 95% confidence intervals (CIs) were combined using random-effect models (DerSimonian–Laird method). Statistical heterogeneity was assessed using the I2 test, which was considered high when >75% [12]. Publication bias was estimated using Egger’s regression method for subgroups with at least 10 studies.
The meta-analysis was performed separately for each visual function and by type of driver (private or commercial), as commercial drivers have much more driving exposure than non-commercial drivers. The analysis of studies with motorcyclists was also performed separately.
All statistical analyses were performed using Stata, v. 12 (StataCorp, College Station, TX, USA).
3. Results
3.1. Results of the Search
The initial search yielded 2398 results, and after excluding duplicates and checking compliance with the selection criteria, 39 articles were selected (Figure 1). Of the studies included in the qualitative synthesis, 35 were combined into different meta-analyses based on the visual function analysed, the type of observational study, and the measure of association reported. Five of the selected studies were not finally included in the quantitative synthesis, either because they did not report data for exposed and injured subjects in their results [13,14,15], or because they did not report data for unexposed subjects [16], or because the authors reported visual acuity results as mean and standard deviation rather than as categorical data comparable to the other studies [17].
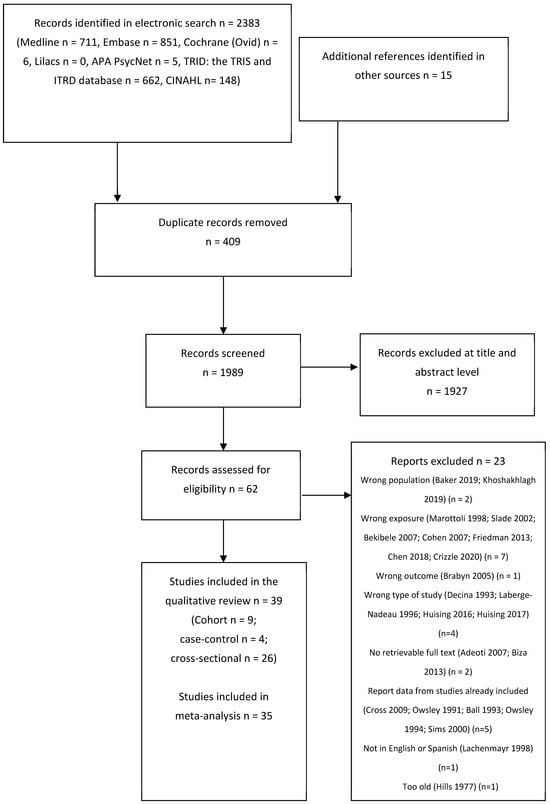
Figure 1.
PRISMA flow diagram of the systematic literature review search process.
3.2. Characteristics of the Included Studies
Nine cohort studies published between 1998 and 2018 were included, all of which were conducted in high-income countries (six in the USA) (Table 1). In addition, four case–control studies published between 1987 and 1998 were included, three of which were conducted in high-income countries (two in the USA) (Table 2). Of the 26 cross-sectional studies published between 1985 and 2022, 23 were from low- and middle-income countries (including 13 from Nigeria and 3 from India) (Table 3).

Table 1.
Characteristics of the cohort studies included in the qualitative review.

Table 2.
Characteristics of the case–control studies included in the qualitative review.

Table 3.
Characteristics of the cross-sectional studies included in the qualitative review.
Of the 39 studies retrieved for the qualitative review, 2 (5.1%) assessed the four visual functions of interest for this study, 8 (20.5%) assessed three functions, 17 (43.6%) assessed two functions and 12 (30.8%) assessed only one visual function.
Three of the included articles—one case–control study [29] and two cohort studies [18,19]—corresponded to the same study and were included because they reported data on different visual functions or were collected at different times.
Of the cross-sectional studies, 57.7% included only men, 88.5% were from low- and middle-income countries, 73.1% were from African countries, and 88.5% included public transport drivers. Of the cohort and case–control studies, 92.3% were conducted in high-income countries and in older adult populations. One case–control study [21] included only women. The occurrence of RTAs was self-reported in 96.2% of the cross-sectional studies and 22.2% of the cohort studies. Two cross-sectional studies [38,41] and one cohort study [25] evaluated motorcyclists.
The occurrence of RTAs was self-reported in 92.3% of the cross-sectional studies and in 22.2% of the cohort studies; none of the case–control studies used surveys to measure the outcomes. The definition of RTA was reported in 26.9% of the cross-sectional studies, 75% of the case–control studies and 88.9% of the cohort studies. The frequency of accidents was heterogeneously reported, with prevalence values ranging from 4% in the last 5 years [13] to 67.4% in an undefined period [47]. The cumulative incidence ranged from 5.1% in 2 years [17] to 33.7% in 1 year [25] (Table 1, Table 2 and Table 3).
Regarding the assessment of methodological quality by study type, 55.6% and 44.4% of the cohort studies were good and fair, respectively. The least met criteria were not assessing exposure more than once (66.7%) or not assessing different levels of exposure or treating it as a continuous variable (44.4%). For case–control studies, 50% were of good quality and 50% were of fair quality; the least common criterion was the ability to show that exposure occurred before the outcome (50%). For the cross-sectional studies, 92.3% were of poor quality and 7.7% were of fair quality; all of them assessed self-reported outcomes, and 96.2% did not adjust for other variables.
3.3. Visual Acuity
Only one study did not report visual acuity (VA) results [33]. Of those that did report VA, the most common methods used were Snellen optotypes (47.4%), ETDRS (15.4%), or other types of visual acuity testing (15.8%). In addition, 29.0% used data from both eyes and 36.8% used data from the eye with better vision. Each study reported different cut-off points for classifying subjects with reduced VA, the most common being <6/12 (42.1%), <6/18 (26.3%), and <6/9 (23.7%).
The meta-analysis included 18 cross-sectional studies (16 of commercial drivers and 2 of private drivers), 3 case–control studies (private drivers) and 5 cohort studies (private drivers). In the cohort of private drivers (RR 1.04, 95% CI 0.74–1.46; I2 = 0.0%; n = 2172 and HR 1.08, 95% CI 0.85–1.36; I2 = 0.0%; n = 3317) and case–control (OR 1.04, 95% CI 0.78–1.40; I2 = 0.0%; n = 5013) studies, the risk of RTA was not increased when VA was reduced (Figure 2). Cross-sectional studies found a non-statistically significant higher risk was found for private drivers (PR 3.00, 95% CI 0.53–17.07; I2 = 84.5%; n = 3379), but a statistically significant higher risk for commercial drivers (PR 1.54, 95% CI 1.26–1.88; I2 = 72.0%; n = 5714), with significant heterogeneity and no evidence of publication bias (Egger’s test p = 0.709) (Figure 3).
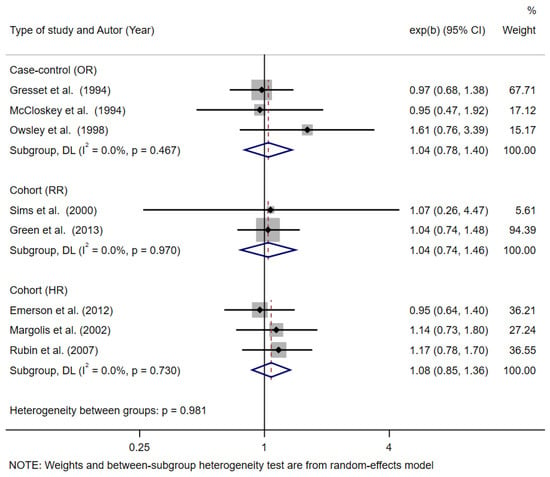
Figure 2.
Forest plot of risk of road traffic accident (police-reported) among private drivers with reduced visual acuity by type of observational study [19,21,22,23,24,27,28,29].
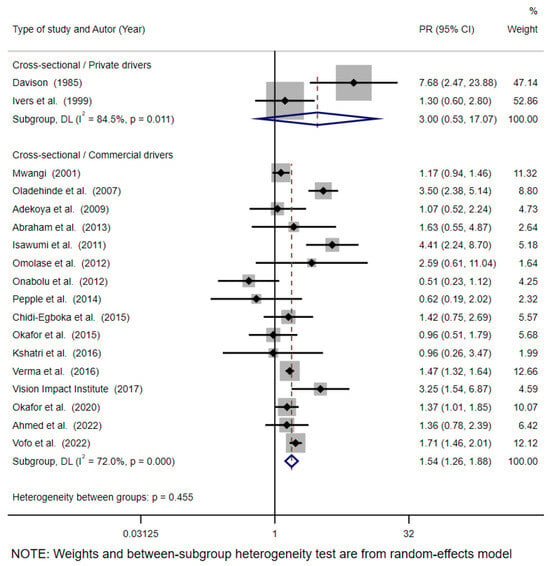
Figure 3.
Forest plot of risk of road traffic accident (self-reported) among private and commercial drivers with reduced visual acuity in cross-sectional studies [30,31,32,34,35,36,37,39,40,42,43,44,46,47,48,49,50,51].
3.4. Colour Vision
Nineteen studies (48.7%) included colour vision testing; 94.7% were cross-sectional, and all of them assessed commercial drivers. The most commonly used test was the Ishihara test (73.7%), with the frequency of alterations ranging from 0% to 10.4%. Only 57.9% of the studies reported results on the risk of RTA in the presence of abnormal colour vision.
The meta-analysis was performed with eight cross-sectional studies and found no increased risk of RTA with abnormal colour vision (PR 1.50, 95% CI 0.91–2.45; I2 = 92.0%; n = 4367); there was a considerable degree of heterogeneity (Figure 4).
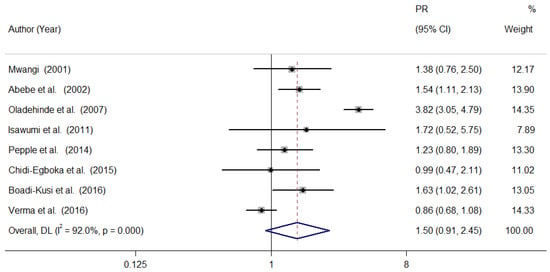
Figure 4.
Forest plot of the risk of a road traffic accident (self-reported) in commercial drivers with abnormal colour vision, according to cross-sectional studies [32,33,34,36,42,43,45,47].
3.5. Stereopsis
Twelve studies (30.8%) assessed stereopsis using various vision screeners (33.3%), the TNO (25%) and Randot (16.7%) tests.
The meta-analysis included with four cross-sectional studies, two case–control studies and two cohort studies. In the cross-sectional studies, no risk of RTA was found in commercial drivers where reduced stereopsis was evidenced (PR 1.40, 95% CI 0.99–1.99; I2 = 44.8; n = 1749), with moderate heterogeneity. No risk was observed in case–control studies (OR 1.42, 95% CI 0.89–2.28; I2 = 0.0%; n = 4330) or cohort studies (HR 1.12, 95% CI 0.82–1.52; I2 = 52.2%; n = 3213) (Figure 5).
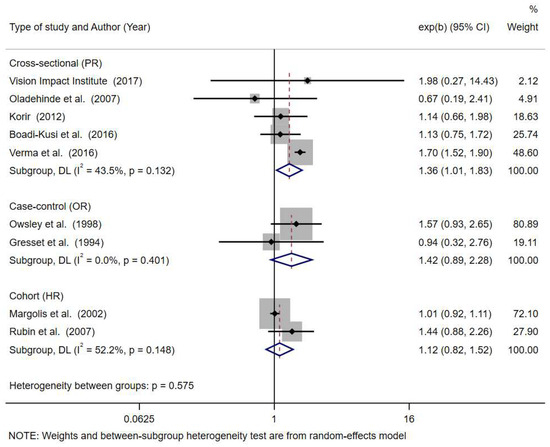
Figure 5.
Forest plot of the risk of road traffic accidents in commercial and private drivers with reduced stereopsis, according to the type of observational study [21,22,27,29,34,38,45,47,48].
3.6. Contrast Sensitivity
Ten studies (25.6%) reported contrast sensitivity outcomes, of which 60% of these were cohort studies and 60% used the Pelli–Robson test.
Three cross-sectional studies reported contrast sensitivity data [14,31,48] but did not assess the association with accident rates. A small risk of RTA was seen in older adults with impaired contrast sensitivity and in cohort studies reporting the cumulative incidence (RR 1.42, 95% CI 1.01–2.00; I2 = 0.0%; n = 2172), but not in those reporting HR (HR 1.01, 95% CI 0.91–1.11; I2 = 0.0%; n = 3313) (Figure 6).
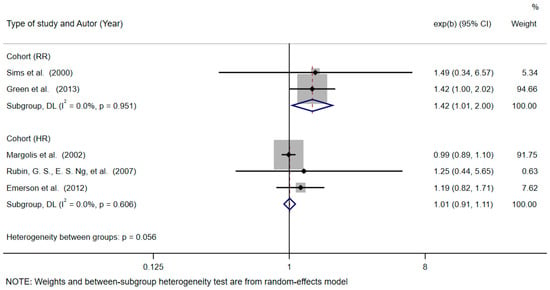
Figure 6.
Forest plot of the risk of road traffic accidents (police-reported) in drivers with reduced contrast sensitivity, with cohort studies [19,21,22,23,24].
4. Discussion
This systematic review and meta-analysis identified the risk of RTA based on the status of several visual functions that are assessed in common driving tests, which is specifically related to ocular pathology. A small number of cohort or case–control studies were found and were conducted in high-income countries and in populations of older adults. Conversely, cross-sectional studies have been conducted in low- and middle-income countries, often involving public service drivers, and the subjects have been predominantly male. This finding reflects the interest in issues related to the licencing of commercial drivers, who have very high exposure to driving, often in heavy traffic conditions. The other group of interest has been older adults with physical and functional comorbidities. There has been one review of the impact of visual function in the general population [14,47] and only three of the studies [25,38,41] have assessed motorcyclists. Studies conducted in commercial drivers or older adults could not be extrapolated to other types of drivers.
An association between impaired VA and RTAs has been found in cross-sectional studies, but not in cohort and case–control studies. However, only one cross-sectional study performed a multivariate analysis on aspects related to the general health status of the drivers [31].
Only two of the studies [47,48] reported the outcomes for the four visual functions of interest for this review, probably due to the use of vision screeners for measure them. Some studies measured all four variables but did not report the results of all of them in the study [13,26,34]. Others only reported VA results [13,14,15,20,25,28,30,38,45,50,51,52], so aspects of the visual function that may be important during driving are missing. This systematic review found a significant but weak association between reduced VA and RTAs in commercial drivers, according to cross-sectional studies. This finding follows the same trend as the results of Piyasena et al. (RR 1.41, 95% CI 1.26–1.59), although they had different selection criteria and included the same subjects more than once in their meta-analysis in order to use different cut-off points [8]. Although the ability to resolve details is the mandatory test for obtaining a driving licence and it has face validity, research on driving safety has produced results with significant but weak or no significant associations, partly due to inadequate sample sizes. In addition, static VA, measured under high contrast and high lighting conditions, does not reflect the visual complexity required for driving; for example, it does not take into account peripheral vision, movement, or changes in contrast levels. Another explanation for the results obtained is that visually impaired drivers may voluntarily stop driving [6].
All the studies that looked at colour vision were cross-sectional and were carried out in low- and middle-income countries. The most commonly used test for diagnosis was Ishihara, but most of the studies did not specify the type of abnormality found. The results obtained in this study do not indicate an increased risk of RTA in those with colour vision abnormalities. This is similar to the observations of Piyasena et al. (RR 1.36 (95% CI 1.01–1.82)), who provide more reliable results by including data from the same study twice to use different cut-offs [8]. In our study, if cross-sectional studies of motorcyclists were included, a statistically significant association would be found (RP 1.47 95% CI 1.03–2.10). Colour vision deficiency is a risk factor for RTA, particularly in the case of protanopia, as it can affect the ability to react to traffic lights and require the driver to adjust their driving accordingly [53]. Normal colour vision ensures that drivers can correctly identify the traffic devices and coloured signals on the road, in particular the rear lights [6].
No association was found between reduced stereopsis and accidents. This seems strange because stereopsis provides information about the distances between objects, the volume of objects, and the bumps or unevenness of the road and is an indicator of the state of binocularity. Other reviews have reported contradictory results in people with poor stereopsis and in monocular individuals, and clinical studies have also found no significant differences in accident rates according to stereopsis [54]. Therefore, as of now, there is currently insufficient evidence to conclude that reduced stereopsis is a hazard in normal everyday driving for non-commercial drivers [55].
Contrast sensitivity was only reported by studies from high-income countries, and a significant but weak association with RTAs was observed. A prospective study of older adults in the USA, which was not included in this review because it was based on naturalistic driving data, found no association between photopic contrast sensitivity and higher rates of motor vehicle accidents, although an association was found with mesopic contrast sensitivity. Assessment of this function is relevant, given the large variability in road lighting levels, both during the day and at night. Drivers with impaired photopic contrast sensitivity are more likely to avoid challenging driving situations and reduce driving exposure (i.e., mileage) and are at higher risk of retiring from driving [56].
The results for stereopsis and contrast sensitivity are based on a very small number of studies, which may affect their reliability, so caution should be exercised in generalising them.
Data from cross-sectional studies do not allow comparisons of crash risk based on driver age. Piyasena et al. made this comparison based on the mean age (<40 years and ≥40 years) but found no difference [8].
With age, functional changes occur in VA, contrast sensitivity, and depth perception as well as in refractive error, dark adaptation, and glare recovery [57]. The cohort studies included in this review only measured visual functions once at baseline, but these may have changed during follow-up, especially in older adults. The studies could not conclude whether the more severe the change, the more severe the RTAs.
This review was focused on the behaviour of vision in healthy subjects, both in terms of ocular conditions and motor and cognitive aspects. Visual field alterations occur in several eye diseases, such as glaucoma, age-related macular degeneration, retinitis pigmentosa, and optic pathway lesions, and there is ample evidence of their impact on visual function [8,9]. Therefore, the visual field was not included in the visual functions analysed.
This review excluded studies that only included patients with systemic diseases, such as diabetes, Parkinson’s disease, or rheumatoid arthritis, and eye diseases, such as glaucoma, age-related macular degeneration, or cataracts.
Several biases were present in the included studies, especially in the cross-sectional studies. The reporting of VA was very variable, with binocular results, or results from the better eye, or only from the right eye. In most cases, it was not clear whether the data were taken with or without optical correction, or whether the driver was wearing their glasses at the time of the crash. There was also no mention of the lighting conditions of the optotypes or the locations where the tests were carried out. In addition, the type of test used and the cut-off points were different in each study. The same was true for colour vision, stereopsis, and contrast sensitivity. Also, all of the studies included in the meta-analysis were considered to be of low quality, so there is a need for cross-sectional studies using very rigorous methods and with better and more complete descriptions in the reports. Cohort studies in which accidents are reported by the police are particularly needed.
Regarding the measurement of outcomes, most of the articles did not specify the definition of RTA used. Very few of them distinguished whether the driver was at fault [14,18,19,23,24,29] and whether the accident was serious or minor [27,38]. In addition, self-reporting is likely to have underestimated the frequency of RTAs, so that only less serious accidents in which the subjects survived were included. It was clear that not all countries had data from police accident records.
Despite the increase in the number of vehicles and RTAs worldwide, which has become a public health issue, few studies were found from Asia and none from Latin America. Therefore, the organisations or institutions concerned, such as the road safety agencies, should promote studies that include the visual function of drivers, in addition to other relevant variables involved in the act of driving.
RTAs can be caused by human, vehicle, and environmental factors, among others [40], but only seven studies in the review present multivariate analysis models, demonstrating the need for adequate control of confounding variables to obtain valid results. Not only VA but also contrast sensitivity, colour vision, stereopsis and type of refractive error need to be considered to fully reflect the complexity of the visual system. Studies need to include detailed and clear methodological aspects, such as the tests used, conditions of use and cut-off points, to provide a complete insight into the visual aspects of driving. In addition, studies should, as far as possible, be based on objective accident reports that allow identification of the type of accident (minor or serious, at fault or not) and the period analysed, even in cross-sectional studies.
Research conducted in low- and middle-income countries has provided information through descriptive studies that report crash risk based on VA or colour vision alone. Conversely, studies from high-income countries show the importance of analysing complex variables that include visual processing speed and divided attention [6]. Of relevance are the studies by the University of Alabama Department of Ophthalmology group, conducted between 1993 and 2000, with retrospective and prospective results from the same group of patients. Some of these were excluded from this review because they did not present their results using measures of association [58,59]. The appropriate methodology for developing research to support decision making in road safety and vision should be adapted to the social and economic context of countries, especially low- and middle-income countries, so that the results can be implemented by policy makers and accepted by the interested public. In this regard, cohort and case–control studies of motorcyclists, who are generally young and visually healthy, would be very useful; this is a growing population in middle- and low-income countries.
The trend in new research in developed countries on road safety and its relationship to vision is moving towards autonomous vehicles and artificial intelligence. In the developing world, however, the study of human visual function will continue to be fundamental to decision making on policies to improve road safety. In low- and middle-income countries, lack of access to eye care can lead to a higher number of crashes due to untreated problems. It is important that road safety research takes into account local characteristics in terms of risk factors such as the prevalence of visual impairment, access to eye care, and local beliefs. Road safety policies should recognise this reality and promote measures such as regular eye examinations for drivers, subsidies for spectacles and awareness campaigns on the importance of eye health.
In conclusion, according to cross-sectional studies, there is a higher risk of RTA in drivers with impaired VA than in those with normal vision. The few case–control and cohort studies do not show an association between the occurrence of accidents and these visual functions. It is necessary to draw attention to this issue so that quality research can be conducted to support the formulation of road safety policies related to the visual health of drivers. The studies analysed, most of which are cross-sectional, may not be sufficient to take preventive action.
Author Contributions
According to CRediT, the individual contributions to the paper have been the following: D.G.-L.: conceptualization, formal analysis, investigation, validation, methodology, visualisation, writing—original draft, writing—review and editing. F.R.-P.: conceptualization, investigation, methodology, writing—original draft, writing—review and editing. E.I.-P.: methodology, formal analysis, writing—original draft, writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
The translation costs and the APC was funded by Universidad El Bosque.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Acknowledgments
To Judith Marcano Williams, Head of Advocacy & Partnerships, The Americas, OneSight EssilorLuxottica Foundation, for her guidance and support during the development of the research.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization. Global Status Report on Road Safety 2023; World Health Organization: Geneva, Switzerland, 2023; Available online: https://iris.who.int/handle/10665/375016 (accessed on 2 March 2024).
- Organización Mundial de la Salud. Plan Mundial Para el Decenio de Acción Para la Seguridad Vial 2021–2030; Organización Mundial de la Salud: Geneva, Switzerland, 2021; p. 36. Available online: https://www.who.int/es/publications/m/item/global-plan-for-the-decade-of-action-for-road-safety-2021-2030 (accessed on 18 August 2023).
- Ortiz-Peregrina, S. Influencia del Rendimiento Visual y Factores de Accidentabilidad Durante la Conducción en Sujetos con Visión Normal y con Patología Ocular. Ph.D. Thesis, Universidad de Granada, Granada, Spain, 2020. Available online: https://n9.cl/u2qc4 (accessed on 20 September 2023).
- Hawley, C.; Roberts, C.; Fosdick, T.; Ursachi, G. Vision and health as factors contributing to injury collisions in Great Britain: Comparisons between older and younger drivers. Optom. Pract. 2020, 21, 1–11. [Google Scholar]
- Rolison, J.J.; Regev, S.; Moutari, S.; Feeney, A. What are the factors that contribute to road accidents? An assessment of law enforcement views, ordinary drivers’ opinions, and road accident records. Accid. Anal. Prev. 2018, 115, 11–24. [Google Scholar] [CrossRef]
- Owsley, C.; McGwin, G. Vision and driving. Vis. Res. 2010, 50, 2348–2361. [Google Scholar] [CrossRef]
- Wood, J.M.; Black, A.A.; Dingle, K.; Rutter, C.; DiStefano, M.; Koppel, S.; Charlton, J.L.; Bentley, S.A. Impact of vision disorders and vision impairment on motor vehicle crash risk and on-road driving performance: A systematic review. Acta Ophthalmol. 2022, 100, e339–e367. [Google Scholar] [CrossRef] [PubMed]
- Piyasena, P.; Olvera-Herrera, V.O.; Chan, V.F.; Clarke, M.; Wright, D.M.; MacKenzie, G.; Virgili, G.; Congdon, N. Vision impairment and traffic safety outcomes in low-income and middle-income countries: A systematic review and meta-analysis. Lancet Glob. Health 2021, 9, e1411–e1422. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.; Di Tanna, G.L.; Coxon, K.; Brown, J.; Ren, K.; Ramke, J.; Burton, M.J.; Gordon, I.; Zhang, J.H.; Furtado, J.; et al. Associations between vision impairment and vision-related interventions on crash risk and driving cessation: Systematic review and meta-analysis. BMJ Open 2023, 13, e065210. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- NHLBI. Study Quality Assessment Tools; National Heart, Lung and Blood Institute: Bethesda, MD, USA, 2021. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 15 March 2022).
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Bekibele, C.; Fawole, O.; Bamgboye, A.; Adekunle, L.; Ajav, R.; Baiyeroju, A. Risk factors for road traffic accidents among drivers of public institutions in Ibadan, Nigeria. Afr. J. Health Sci. 2008, 14, 137–142. [Google Scholar] [CrossRef]
- Okamura, K.; Iwase, A.; Matsumoto, C.; Fukuda, T.; Kunimatsu-Sanuki, S.; Fujita, G.; Kihira, M.; Kosuge, R. Association between visual field impairment and involvement in motor vehicle collision among a sample of Japanese drivers. Transp. Res. Part F Traffic Psychol. Behav. 2019, 62, 99–114. [Google Scholar] [CrossRef]
- Ojabo, C.O.; Adeniyi, O.S.; Ojo, B.A. An Assessment of Visual Acuity of Commercial Vehicle Drivers in Makurdi, Benue State, North-Central Nigeria. Curr. J. Appl. Sci. Technol. 2020, 39, 61–67. [Google Scholar] [CrossRef]
- Ovenseri-Ogomo, G.; Adofo, M. Poor vision, refractive errors and barriers to treatment among commercial vehicle drivers in the Cape Coast municipality. Afr. Health Sci. 2011, 11, 97–102. [Google Scholar]
- Woolnough, A.; Salim, D.; Marshall, S.C.; Weegar, K.; Porter, M.M.; Rapoport, M.J.; Man-Son-Hing, M.; Bédard, M.; Gélinas, I.; Korner-Bitensky, N.; et al. Determining the validity of the AMA guide: A historical cohort analysis of the Assessment of Driving Related Skills and crash rate among older drivers. Accid. Anal. Prev. 2013, 61, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Owsley, C.; Ball, K.; McGwin, G.J.; Sloane, M.E.; Roenker, D.L.; White, M.F.; Overley, E.T. Visual processing impairment and risk of motor vehicle crash among older adults. JAMA 1998, 279, 1083–1088. [Google Scholar] [CrossRef] [PubMed]
- Sims, R.V.; McGwin, G.J.; Allman, R.M.; Ball, K.; Owsley, C. Exploratory study of incident vehicle crashes among older drivers. J. Gerontol. A Biol. Sci. Med. Sci. 2000, 55, M22–M27. [Google Scholar]
- Keeffe, J.E.; Jin, C.F.; Weih, L.M.; McCarty, C.A.; Taylor, H.R. Vision impairment and older drivers: Who’s driving? Br. J. Ophthalmol. 2002, 86, 1118–1121. [Google Scholar] [CrossRef] [PubMed]
- Margolis, K.L.; Kerani, R.P.; McGovern, P.; Songer, T.; Cauley, J.A.; Ensrud, K.E. Risk factors for motor vehicle crashes in older women. J. Gerontol. A Biol. Sci. Med. Sci. 2002, 57, M186–M191. [Google Scholar] [CrossRef]
- Rubin, G.S.; Ng, E.S.W.; Bandeen-Roche, K.; Keyl, P.M.; Freeman, E.E.; West, S.K. A prospective, population-based study of the role of visual impairment in motor vehicle crashes among older drivers: The SEE study. Invest. Ophthalmol. Vis. Sci. 2007, 48, 1483–1491. [Google Scholar] [CrossRef]
- Emerson, J.L.; Johnson, A.M.; Dawson, J.D.; Uc, E.Y.; Anderson, S.W.; Rizzo, M. Predictors of driving outcomes in advancing age. Psychol. Aging 2012, 27, 550–559. [Google Scholar] [CrossRef]
- Green, K.A.; McGwin, G.; Owsley, C. Associations between visual, hearing, and dual sensory impairments and history of motor vehicle collision involvement of older drivers. J. Am. Geriatr. Soc. 2013, 61, 252–257. [Google Scholar] [CrossRef]
- Chen, S.J.; Chen, C.Y.; Lin, M.R. Risk factors for crash involvement in older motorcycle riders. Accid. Anal. Prev. 2018, 111, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Humphriss, D. Three South African studies on the relation between road accidents and drivers’ vision. Ophthalmic Physiol. Opt. 1987, 7, 73–79. [Google Scholar] [CrossRef]
- Gresset, J.A.; Meyer, F.M. Risk of accidents among elderly car drivers with visual acuity equal to 6/12 or 6/15 and lack of binocular vision. Ophthalmic Physiol. Opt. 1994, 14, 33–37. [Google Scholar] [CrossRef]
- McCloskey, L.W.; Koepsell, T.D.; Wolf, M.E.; Buchner, D.M. Motor vehicle collision injuries and sensory impairments of older drivers. Age Ageing 1994, 23, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Owsley, C.; McGwin, G.J.; Ball, K. Vision impairment, eye disease, and injurious motor vehicle crashes in the elderly. Ophthalmic Epidemiol. 1998, 5, 101–113. [Google Scholar] [CrossRef]
- Davison, P.A. Inter-relationships between British drivers’ visual abilities, age and road accident histories. Ophthalmic Physiol. Opt. 1985, 5, 195–204. [Google Scholar] [PubMed]
- Ivers, R.Q.; Mitchell, P.; Cumming, R.G. Sensory impairment and driving: The Blue Mountains Eye Study. Am. J. Public. Health 1999, 89, 85–87. [Google Scholar] [CrossRef]
- Mwangi, C. Vision Assessment of Public Service Vehicle Drivers in Nairobi. Ph.D. Thesis, University of Nairobi, Nairobi, Kenya, 2001. [Google Scholar]
- Abebe, Y.; Wondmikun, Y. Defective color perception among car drivers in Addis Ababa, Ethiopia. Traffic Inj. Prev. 2002, 3, 294–297. [Google Scholar] [CrossRef]
- Oladehinde, M.K.; Adeoye, A.O.; Adegbehingbe, B.O.; Onakoya, A.O. Visual functions of commercial drivers in relation to road accidents in Nigeria. Indian J. Occup. Environ. Med. 2007, 11, 71–75. [Google Scholar]
- Adekoya, B.J.; Owoeye, J.F.A.; Adepoju, F.G.; Ajaiyeoba, A.I. Visual function survey of commercial intercity vehicle drivers in Ilorin, Nigeria. Can. J. Ophthalmol. 2009, 44, 261–264. [Google Scholar] [CrossRef]
- Isawumi, M.A.; Adeoti, C.O.; Ubah, J.N.; Oluwatimilehin, I.O.; Raji, R.A. Ocular status of commercial drivers in Osun State, Nigeria. Afr. J. Med. Med. Sci. 2011, 40, 405–411. [Google Scholar] [PubMed]
- Onabolu, O.O.; Bodunde, O.T.; Otulana, T.O.; Ajibode, H.A.; Awodein, O.G.; Onadipe, O.J.; Jagun, O.A. Visual acuity of commercial motor drivers in Ogun State of Nigeria. Niger. Postgrad. Med. J. 2012, 19, 225–229. [Google Scholar] [CrossRef] [PubMed]
- Korir, F. Vision Among Bodaboda Motorcycle Riders in Kisumu. Master Thesis, University of Nairobi, Nairobi, Kenya, 2012. [Google Scholar]
- Omolase, C.O. Ocular Status of Commercial Drivers in a Nigerian Community. J. Community Med. Heal. Educ. 2012, 2, 2–5. [Google Scholar] [CrossRef]
- Abraham, E.G.; Umanah, I.N.; Abraham, E.G. Prevalence of visual impairment among commercial motor vehicle drivers in Uyo, South-South Nigeria. J. Environ. Occup. Sci. 2013, 2, 55–60. [Google Scholar] [CrossRef]
- Achigbu, E.O.; Fiebai, B. Visual defects and commercial motorcycle accidents in south eastern Nigeria. Niger. J. Med. 2013, 22, 299–303. [Google Scholar]
- Pepple, G.; Adio, A. Visual function of drivers and its relationship to road traffic accidents in Urban Africa. Springerplus 2014, 3, 47. [Google Scholar] [CrossRef]
- Chidi-Egboka, N.C.; Bolarinwa, O.A.; Ademola Awoyemi, O. Visual function test among commercial drivers in a North Central State of Nigeria. Health Sci. J. 2015, 9, 11. [Google Scholar]
- Okafor, I.P.; Odeyemi, K.A.; Aribaba, O.T.; Dolapo, D.C.; Ogunyemi, A.O. Visual acuity, safe/unsafe practices and self-reported road traffic crash experiences among commuter bus drivers from two motor parks in Lagos, Nigeria. West Afr. J. Med. 2015, 34, 118–124. [Google Scholar] [PubMed]
- Boadi-Kusi, S.B.; Kyei, S.; Asare, F.A.; Owusu-Ansah, A.; Awuah, A.; Darko-Takyi, C. Visual function among commercial vehicle drivers in the central region of Ghana. J. Optom. 2016, 9, 54–63. [Google Scholar] [CrossRef]
- Kshatri, J.; Pradhan, P.; Patro, S.; Tripathy, R. Ocular Status of Inter-State Commercial Drivers: A Cross Sectional Study in Odisha, India. Int. J. Ophthalmic Res. 2016, 2, 188–191. [Google Scholar] [CrossRef]
- Verma, A.; Chakrabarty, N.; Velmurugan, S.; Prithvi Bhat, B.; Dinesh Kumar, H.D.; Nishanthi, B. Assessment of driver vision functions in relation to their crash involvement in India. Curr. Sci. 2016, 110, 1063–1072. [Google Scholar] [CrossRef]
- Vision Impact Institute. Assesment of Visual Limitations of Commercial Drivers in Metropolitan Cities in India; Vision Impact Institute: New Delhi, India, 2017; Available online: https://onesight.essilorluxottica.com/research/assessment-of-visual-limitations-of-commercial-drivers-in-metropolitan-cities-in-india-(interim-report) (accessed on 7 July 2021).
- Okafor, K.; Awunor, N.; Otabor-Olubor, O.; Okojie, O. Assessment of visual acuity of commercial long-distance drivers in Benin City, Edo State, Nigeria. Delta J. Ophthalmol. 2020, 21, 57. [Google Scholar]
- Ahmed, M.; Patnaik, J.L.; Whitestone, N.; Hossain, M.A.; Alauddin, M.; Husain, L.; Hossain, M.P.; Islam, M.S.; Hossain, M.I.; Imdad, K.; et al. Visual Impairment and Risk of Self-Reported Road Traffic Crashes Among Bus Drivers in Bangladesh. Asia Pac. J. Ophthalmol. 2022, 11, 72–78. [Google Scholar] [CrossRef]
- Vofo, B.N.; Ayuk, D.A.; Pe’er, J.; Chichom-Mefire, A.; Tendongfor, N.; Nche, E.N. Visual assessment of commercial drivers in the South West Region of Cameroon. BMC Ophthalmol. 2021, 21, 148. [Google Scholar] [CrossRef]
- Cole, B.L. Colour blindness and driving. Clin. Exp. Optom. 2016, 99, 484–487. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Peregrina, C.; Martinez-Perez, C.; Villa-Collar, C.; Sánchez-Tena, M.Á. Influence of vision on drivers: A pilot study. Int. J. Environ. Res. Public Health 2021, 18, 12116. [Google Scholar] [CrossRef]
- Dakroub, M.; Boueiri, M.; Al-Haddad, C. A review of driving and binocularity. J. Pediatr. Ophthalmol. Strabismus 2022, 59, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Owsley, C.; Swain, T.; Liu, R.; McGwin, G.; Kwon, M.Y. Association of Photopic and Mesopic Contrast Sensitivity in older drivers with risk of motor vehicle collision using naturalistic driving data. BMC Ophthalmol. 2020, 20, 47. [Google Scholar] [CrossRef]
- Lord, S.R.; Delbaere, K.I.M.; Sturnieks, D.L. Aging. In Handbook of Clinical Neurology, 3rd ed.; Day, B., Lord, S., Eds.; Elsevier: Melbourne, Australia, 2018; pp. 157–171. [Google Scholar]
- Ball, K.; Owsley, C.; Sloane, M.E.; Roenker, D.L.; Bruni, J.R. Visual attention problems as a predictor of vehicle crashes in older drivers. Investig. Ophthalmol. Vis. Sci. 1993, 34, 3110–3123. [Google Scholar]
- Owsley, C. Vision and driving in the elderly. Optom. Vis. Sci. 1994, 71, 727–735. [Google Scholar] [CrossRef]
- Sims, R.V.; Owsley, C.; Allman, R.M.; Ball, K.; Smoot, T.M. A preliminary assessment of the medical and functional factors associated with vehicle crashes by older adults. J. Am. Geriatr. Soc. 1998, 46, 556–561. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).