Abstract
(1) Background: Emerging fungal infections associated with Scedosporium spp. and Lomentospora prolificans (S/L) are becoming more frequent and are very difficult to treat. Our objective was to analyze the frequency and management of S/L isolates in lung transplant (LTx) recipients, the patient outcomes and in vitro antifungal sensitivity. (2) Methods: We included all patients with S/L isolation during post-transplant follow-up. Data were collected from electronic medical records. All samples were cultivated on Sabouraud Chloramphenicol agar. Isolations of S/L were submitted to in vitro susceptibility tests. (3) Results: A total of 11 (2%) of the 576 LTx recipients included had at least one isolation of S/L. Classification for the 11 cases were colonization (4; 36%) and infection (7; 65%). Five infections were pulmonary (71%) and two were disseminated (29%). S. apiospermum complex was the most frequently occurring isolation in patients with pulmonary disease while L. prolificans was the most frequent in patients with disseminated disease. Ten patients were treated. The most frequent antifungal drugs used were voriconazole (n = 8) and terbinafine (n = 6). Seven patients (70%) received more than one drug. The mortality rate associated with L. prolificans isolation was 50% for colonization and 100% for disseminated disease. (4) Conclusions: Scedosporium spp. and L. prolificans infections are associated with high morbidity and mortality rates. New diagnostic and therapeutic tools are required to reduce the impact of these infections.
1. Introduction
Infectious complications are a frequent cause of morbidity and mortality in lung transplant recipients. The constant exposure of the lung graft to the external environment and the high levels of immunosuppression required to prevent acute and chronic graft rejection are the main predisposing factors to infections [1,2].
Fungal infections are less prevalent than bacterial or viral infections but have been associated with a higher mortality rate [1,3]. Aspergillus is the most frequently isolated fungus, but in recent years, there has been a progressive increase in infections caused by other emerging fungi, such as Scedosporium spp. and Lomentospora prolificans. The limited therapeutic options available against these emerging fungi are associated with high mortality and represent a challenge for clinicians.
Scedosporium spp. and Lomentospora prolificans are ubiquitous pathogenic fungi primarily found in soil and wastewater. These fungi have a particular ability to colonize the respiratory tract of patients with pulmonary disease and are commonly isolated in respiratory samples before and after lung transplantation. Fungal colonization is especially frequent among lung transplant candidates with cystic fibrosis. After Aspergillus fumigatus, Scedosporium spp. and Lomentospora are the second most frequently isolated fungal group in these patients [4,5,6].
In the post-transplant period, a significant percentage of lung transplant recipients (20–50%) show fungal colonization, with rates of invasive disease reaching up to 14% [6]. The infection develops as a result of a complex interaction between the fungus and the host’s immune system. In immunocompetent individuals, the innate immune response plays a crucial role, and infections are typically limited [7,8]. However, in patients with compromised immune systems, Scedosporium spp. and Lomentospora prolificans can produce invasive pulmonary disease and hematogenous dissemination. The ineffective immune response of the host, together with the intrinsic resistance of these fungi to most of the antifungal drugs currently available, are the main causes of the high mortality rate associated with these infections [9,10].
In the context of lung transplantation, the distinction between colonization and disease is particularly difficult. Colonization always precedes infection but is not necessarily synonymous with disease. The diagnosis of disease can be challenging due to the nonspecific nature of symptoms and the complexity of interpreting radiological findings. Histological confirmation is not always feasible in patients with compromised respiratory status and/or coagulation abnormalities. Consequently, clinicians face a dilemma when it comes to the isolation of these fungi during patient follow-up: whether to treat or not to treat—this is the question. Due to the risk of mortality, therapeutic withholding is not an option. However, the available pharmacological options are limited, and preventive treatment exposes the patient to significant adverse effects and multiple drug interactions.
The objectives of this study were to analyze the frequency of isolation of Scedosporium spp. and Lomentospora prolificans in our lung transplant recipients, the clinical management of these isolations and the short- and long-term outcomes of patients. We also looked at the in vitro sensitivity of the isolates to the currently available antifungal drugs.
2. Materials and Methods
2.1. Study Design and Patient Population
We designed an observational, retrospective, and analytical study that included all patients aged ≥18 years transplanted at the Hospital Universitario Puerta de Hierro, Majadahonda (Madrid, Spain) between 1 January 2010 and 31 December 2023 who had post-surgical isolation of Scedosporium spp. or Lomentospora prolificans. The study protocol was approved by our center’s Ethics Committee on 27 January 2025 (No. 02/2025). Prior to the collection of data, patients were required to provide written informed consent.
In the pre-transplant period, sputum samples are periodically obtained for fungal and bacterial culture. On the day of the transplant, a bronchoscopy is routinely performed to obtain respiratory samples before the implantation of the graft. After the transplant, a bronchoscopy is performed routinely before the patient is discharged. Additional sputum samples and bronchoscopy are collected based on clinical evolution.
Patients are followed up after surgery in the outpatient clinic of the pulmonology department weekly for the first two weeks, monthly for the first three months, bimonthly for the first year and every three months thereafter.
Our standard approach to immunosuppression includes baliliximab and a life-time triple immunosuppression regimen with tacrolimus, mycopnenolate mofetil and prednisone.
Antibacterial prophylaxis is adjusted to the isolates obtained from samples of the donor and recipient at the time of surgery. The empirical administration of broad-spectrum antibiotics is suspended after 7–10 days.
Antifungal prophylaxis is based on the administration of nebulized liposomal amphotericin B (6 mL) every 48 h until discharge and weekly thereafter [11,12,13]. Our standard approach is to pre-emptively treat any fungal isolation. The antifungal combination initially chosen for patients with Scedosporium or Lomentospora isolation is voriconazole and terbinafine. Posaconazole or isavuconazole are chosen for patients intolerant to voriconazole or with relevant drug interactions.
2.2. Laboratory Fungal Isolation and Susceptibility Testing
Respiratory samples were cultivated on Sabouraud Chloramphenicol agar (Becton Dickinson™, Franklin Lakes, NJ, USA) and incubated at 25 °C and 37 °C for 14 days. Microorganism identification was performed by macroscopic and microscopic visualization as well as MALDI-TOF® mass spectrometry (Bruker™, Berlin, Germany).
Species identification was confirmed at the Reference and Research Mycology Laboratory of the National Microbiology Center (ISCIII) by PCR amplification and sequencing of two regions (ITS region and β-tubulin). Susceptibility testing was performed by the microdilution method according to the EUCAST E. Def 9.4 protocol.
2.3. Definitions
The following definitions are based on the 2015 International Society for Heart and Lung Transplantation (ISHLT) Guidelines for the management of fungal infections in patients with mechanical circulatory support and cardiothoracic organ transplants. These definitions classify fungal presence and infections in transplant recipients as follows [6]:
Pre-transplant colonization: The presence of fungi in lower respiratory tract samples detected via culture prior to transplantation, in the absence of symptoms or radiological/endobronchial changes.
Post-transplant colonization: The presence of fungi in lower respiratory tract samples detected via culture after transplantation, in the absence of symptoms or radiological/endobronchial changes.
Localized infection: The presence of fungi in lower respiratory tract samples detected via culture, accompanied by symptoms and radiological or endobronchial changes.
Invasive fungal infection: The presence of fungi in lower respiratory tract samples detected via culture, accompanied by symptoms and radiological or endobronchial changes, along with histological evidence of tissue invasion.
Additionally, chronic lung allograft dysfunction (CLAD) is defined as a substantial and persistent decline (≥20%) in the measured forced expiratory volume (FEV1) value relative to the baseline. The baseline is determined as the mean of the two highest post-operative FEV1 measurements taken at least three weeks apart [14].
The electronic medical data and laboratory values recorded were demographic data, underlying disease, type of transplant, date of the first S/L isolate, antifungal treatment, diagnosis of CLAD and acute rejection and date and cause of death.
2.4. Statistical Analysis
Continuous variables are presented as mean (standard deviation, SD) or as median (interquartile range, IQR) when not normally distributed. Categorical variables are expressed as frequency (percentage, %). For univariable comparisons, the Student’s t-test or Mann–Whitney U test was used, depending on whether the assumptions of normality were met for numerical variables. For categorical data, Pearson’s chi-square test or Fisher’s exact test was applied, as appropriate. A 95% confidence interval (95% CI) was calculated to estimate the incidence of Scedosporium spp. or Lomentospora prolificans during the post-transplant follow-up period.
Post-transplant overall survival was analyzed using the Kaplan–Meier method, and group comparisons were assessed with the log-rank test. Statistical significance was defined as a p-value less than 0.05, and all tests were two-sided. Statistical analyses were performed using Stata version 18.0 (StataCorp. 2023. Stata Statistical Software: Release 18, StataCorp LLC, College Station, TX, USA).
3. Results
3.1. Characteristics of the Study Population
A total of 11 (2%, 95% CI 0.8; 3.0) of 576 patients who underwent lung transplantation in our unit between 1 January 2010 and 31 December 2023 had at least one isolation of Scedosporium spp. or Lomentospora prolificans (S/L) during the post-transplant follow-up period (Table 1).

Table 1.
Scedosporium spp. and Lomentospora prolificans in lung transplant recipients: clinical features, microbiological findings and outcomes.
The clinical and demographic characteristics of patients with or without S/L isolation are described in Table 2. No significant differences were observed between patients with and without isolates in relation to age, sex, underlying disease or type of transplant.

Table 2.
Demographic characteristics according to S/L isolation.
3.2. Microbiological Findings
During the study period, we obtained 143 S/L isolates. Samples with S/L isolation were as follows: bronchial aspirate (n = 65; 45%), sputum (n = 30; 21%), pleural fluid (n = 19; 13%), bronchoalveolar lavage (n = 14; 10%), blood (n = 4; 3%) and others (n = 11; 8%). The median time from transplantation to the first isolation was 535 days (IQR 157–1294 days). Three patients also had isolations of S/L prior to surgery.
The most frequently identified species were L. prolificans (four patients), S. apiospermum (three patients), S. boydii (three patients) and S. ellipsoidea (one patient). In two recipients, S. apiospermum and L. prolificans were isolated concomitantly in the same sample.
Coinfections with other microorganisms were detected in five recipients (45%), and two of them had more than one detected at the same time as S/L. The most frequent coinfected germens were Cytomegalovirus (n = 3; 27%), Aspergillus (n = 2; 18%), Pseudomonas aeruginosa (n = 1; 9%), Stenotrophomonas maltophilia (n = 1; 9%), Staphylococcus aureus (n = 1; 9%) and Nocardia farcinica (n = 1; 9%).
3.3. Type of Infection and Clinical Presentation
According to the ISHLT diagnostic criteria, the isolation was classified as colonization in four recipients (36%) and infection in seven (64%). The infection was limited to the lung in five patients and was disseminated in two. The fungus isolated most frequently in patients with pulmonary disease was the S. apiospermum complex, while Lomentospora prolificans was the fungus isolated in the two disseminated cases.
Radiological findings associated with the S/L infection were pulmonary infiltrates (n = 4; 57%), pleural effusion (n = 2; 29%), pulmonary nodules and/or micronodules (n = 2; 29%), mediastinitis (n = 1; 14%), tree-in-bud pattern (n = 1; 14%) and pulmonary thromboembolism (n = 1; 14%).
3.4. Antifungal Treatment and Outcomes
Ten of the eleven patients with isolation of S/L received antifungal treatment. Voriconazole (n = 8, 73%) and terbinafine (n = 6, 55%) were the most frequently used drugs. Other antifungals used were posaconazole (n = 3, 27%), echinocandins (n = 3, 27%) and amphotericin B (n = 2, 18%). Seven patients (70%) were treated with more than one drug, and the most common combination was voriconazole and terbinafine.
The eradication of fungi was achieved in seven patients (64%). Six of them received antifungal treatment and one experienced spontaneous resolution without treatment. Eradication was not achieved in two patients with pulmonary disease related to the S. apiospermum complex. Despite extensive combined antifungal treatment, two of the four patients with L. prolificans isolation died from disseminated disease.
During the post-transplant follow-up period, eight patients (73%) died. The cause of death was directly related to fungal infection in two recipients, both due to disseminated Lomentospora prolificans infection. Other causes of mortality included progressive chronic lung allograft dysfunction (four cases), COVID-19 (one case) and multiorgan failure (one case).
No significant differences in survival were observed among patients who had at least one post-transplant S/L isolate and those who did not (p log-rank test = 0.073) (Figure 1). However, the mortality rate among patients with Lomentospora prolificans infection was 50% for colonization and 100% for disseminated disease.
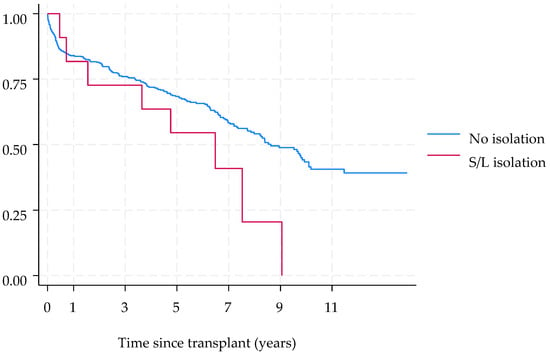
Figure 1.
Survival of lung transplant recipients according to Scedosporium spp. and L. prolificans isolation.
3.5. Antifungal Susceptibility Profiles
The in vitro antifungal susceptibility tests performed for Lomentospora prolificans and Scedosporium spp. against various antifungal agents are shown in Table 3.

Table 3.
In vitro susceptibilities of Scedosporium apiospermum isolates, Scedosporium boydii isolates and Lomentospora prolificans isolates.
Lomentospora prolificans showed in vitro resistance to all azoles, terbinafine and amphotericin B. The minimum inhibitory concentration (MIC) values for echinocandins ranged from 0.03 to >4 mg/L, with MIC50 values of 0.12 mg/L for anidulafungin, 1 mg/L for caspofungin and 0.06 mg/L for micafungin.
Regarding Scedosporium apiospermum, voriconazole exhibited the highest activity among azoles, with MIC values ranging from 0.25 to >8 mg/L and an MIC50 of 0.5 mg/L. The MIC50 values for amphotericin B and terbinafine were 4 mg/L and >16 mg/L, respectively. Regarding echinocandins, micafungin had an MIC50 of 0.06 mg/L, anidulafungin 0.12 mg/L and caspofungin 0.5 mg/L.
In relation to Scedosporium boydii, voriconazole was found to be the most active azole, with MIC values ranging from 0.5 to >8 mg/L and an MIC50 of 1.5 mg/L. In contrast, terbinafine demonstrated no in vitro antifungal activity, with MIC values > 16 mg/L. The MIC50 values for echinocandins were 1 mg/L for both caspofungin and anidulafungin and 0.25 mg/L for micafungin.
Scedosporium ellipsoidea exhibited MIC50 values of 0.5 mg/L for itraconazole, posaconazole and voriconazole, and 8 mg/L for isavuconazole. The MIC50 values for echinocandins were found to be 0.06 mg/L for anidulafungin, 0.25 mg/L for caspofungin and 0.03 mg/L for micafungin.
4. Discussion
In our study, we observed that the isolation of S/L is infrequent in lung transplant recipients. Nevertheless, its management remains very challenging due to the paucity of available therapeutic options. The majority of our patients developed localized pulmonary infections with positive outcomes. However, two of the four recipients infected with L. prolificans died of disseminated disease despite the administration of several combined antifungal drugs. The in vitro susceptibility tests performed showed resistance to the majority of antifungal drugs currently available.
Lung transplant recipients have an increased susceptibility to lower respiratory tract infections with S/L due to the continuous contact of the graft with air and the profound immunosuppression required to prevent acute and chronic rejection [15]. Moreover, the development of these multi-drug fungal infections is also promoted by the frequent exposure of these patients to broad-spectrum antifungal drugs during prophylaxis or empirical treatments. The percentage of isolation of S/L observed in our study was low (2%) and similar to that described by other authors [16,17]. The diagnostic value of these isolates should always be interpreted with caution in conjunction with clinical, radiological and histological findings. However, since invasive infection has been associated with a high mortality rate, the protocol in our center is to treat all patients with any fungal isolation. That is the reason why antifungal treatment was started for each patient except for one who eradicated the germ spontaneously.
Differentiation between colonization and infection can be complex. After applying the ISHLT diagnostic criteria [6], the isolates of S/L were classified as colonization in 36% of our patients and infection in 64%. The five cases classified as localized pulmonary disease were caused by S. apiospermum complex (S. apiospermum and S. boydii) and successfully treated with antifungal drugs. However, despite several combined antifungal treatments, two of the four patients infected with L. prolificans died as a result of hematogenous dissemination of the disease.
The capacity of L. prolificans to germinate, form conidia, penetrate blood vessels and disseminate rapidly in host tissues could provide a plausible explanation for the rapid progression of the infection and its high mortality rate. Furthermore, the intrinsic resistance of the fungi to most of the antifungal drugs currently available limits therapeutic options.
Four patients in our study had isolates of L. prolificans, three before and one after surgery. The isolation in the pre-transplant period is considered a poor prognostic factor, and there is controversy regarding the contraindication of transplantation in previously colonized patients [18,19]. Two patients with cystic fibrosis had L. prolificans isolation prior to surgery and were transplanted under preventive treatment with voriconazole. One of them eradicated the fungi after surgery, but the other died due to disseminated disease regardless of the antifungal treatment.
The isolation of L. prolificans in the third case was achieved from samples obtained in the operating room before the implantation of the graft. The patient underwent an emergency transplant due to pulmonary fibrosis and died in the post-transplant period despite the administration of several antifungal drugs.
The fourth patient with L. prolificans acquired the infection in the post-transplant period and was able to achieve eradication with a combined course of treatment.
The mortality rate associated with L. prolificans isolation in our patients was 50% for colonization and 100% for disseminated disease, which is consistent with the findings observed by other authors [20,21,22]. In order to reduce mortality and avoid unnecessary treatments, it is essential to improve the currently available diagnostic criteria for disease [23,24,25].
Regarding the susceptibility profiles, our results are similar to those previously described [26,27]. The S. apiospermum complex exhibits resistance to amphotericin B and reduced susceptibility to echinocandins [8]. Voriconazole was found to be the most active azole, with MIC50 values of 0.5 mg/L for S. apiospermum and 1.5 mg/L for S. boydii. These values were lower than those of isavuconazole and posaconazole, a finding that has been previously described by other authors. In this regard, our results support the use of voriconazole as a first-line antifungal for the treatment of infections caused by these fungi [23,24,26,28]. Most of our patients received combination therapy. While the synergy and fungicidal effect of the combination of terbinafine and azoles has been demonstrated in in vitro studies, no greater efficacy has been shown in vivo when these drugs are combined with other antifungals, such as terbinafine or echinocandins [15,23,25,29].
The first-line treatment recommended by the guidelines for patients with L. prolificans infection is the combination of voriconazole and terbinafine [23,24,25]. This combination has demonstrated superior response rates and better survival outcomes in in vitro antifungal synergy [30]. In the present study, the strains of L. prolificans isolated exhibited panfungal resistance to azoles, terbinafine and amphotericin B, while echinocandins demonstrated moderate in vitro activity, which is consistent with previously reported findings [26].
In addition to exhibiting reduced sensitivity to antifungal agents commonly used in clinical practice, these fungi are influenced by several factors that contribute to resistance and therapeutic failure, including host immunosuppression, lack of source control or suboptimal antifungal pharmacokinetics [31]. The high mortality rate of these infections highlights the need for the development of new antifungal drugs and the promotion of multicenter clinical trials with drugs such as fosmanogepix and olorofim, which have shown good in vitro activity against Scedosporium and Lomentospora [32,33,34]. Notably, in vitro studies evaluating the efficacy of olorofim against Scedosporium/Lomentospora have reported MICs lower than those observed for voriconazole and posaconazole [15,35]. In addition to their in vitro efficacy, these agents have exhibited a positive response in patients with severe disseminated infections, thus supporting their potential for use in clinical practice [36,37]. However, the low number of infections produced by these fungi limits the development of clinical trials [38].
Limitations
The major limitation of this study was its retrospective and single-center nature. The low number of Scedosporium/Lomentospora isolations did not allow us to identify risk factors. Comparison to other studies was difficult due to the complexity of differentiating between colonization and infection. Our findings are a retrospective experience of a clinical practice, and the great diversity of antifungal drugs and combinations used throughout the study made it very difficult to draw conclusions in relation to efficacy.
Fungal cultures were performed using Sabouraud Chloramphenicol agar. Although specific media can enhance Scedosporium/Lomentospora isolation by inhibiting faster-growing fungi like Aspergillus, especially in cystic fibrosis patients [39,40], our detection rates were consistent with previous studies [16,17].
5. Conclusions
Infections with Scedosporium spp. and Lomentospora prolificans are infrequent. The high mortality due to invasive disease highlights the need for early diagnosis and appropriate antifungal treatment. To improve the prognosis of these infections it is necessary to develop new diagnostic and therapeutic tools.
Author Contributions
S.G.-M.F., R.L., C.G.F., M.A., M.C.P., A.A.-I., I.S.R. and P.U.G. collected, analyzed and interpreted the data; P.U.G. conceptualized the study; S.G.-M.F. and P.U.G. delineated the hypothesis, designed the study and wrote the manuscript; A.R. performed the statistical analysis; I.S.R. carried out the visualization; S.G.-M.F. and P.U.G. edited the manuscript; P.U.G. reviewed the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Hospital Puerta de Hierro, Majadahonda (protocol code. 02/2025) 27 January 2025.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Samanta, P.; Clancy, C.J.; Nguyen, M.H. Fungal Infections in Lung Transplantation. J. Thorac. Dis. 2021, 13, 6695–6707. [Google Scholar] [CrossRef] [PubMed]
- Puerta-Alcalde, P.; Garcia-Vidal, C. Non-Aspergillus Mould Lung Infections. Eur. Respir. Rev. 2022, 31, 220104. [Google Scholar] [CrossRef] [PubMed]
- Cobo, F.; Lara-Oya, A.; Rodríguez-Granger, J.; Sampedro, A.; Aliaga-Martínez, L.; Navarro-Marí, J.M. Infections Caused by Scedosporium/Lomentospora Species: Clinical and Microbiological Findings in 21 Cases. Med. Mycol. 2018, 56, 917–925. [Google Scholar] [CrossRef]
- Blyth, C.C.; Middleton, P.G.; Harun, A.; Sorrell, T.C.; Meyer, W.; Chen, S.C.-A. Clinical Associations and Prevalence of Scedosporium Spp. in Australian Cystic Fibrosis Patients: Identification of Novel Risk Factors? Med. Mycol. 2010, 48 (Suppl. S1), S37–S44. [Google Scholar] [CrossRef]
- Ravenel, K.; Guegan, H.; Gastebois, A.; Bouchara, J.-P.; Gangneux, J.-P.; Giraud, S. Fungal Colonization of the Airways of Patients with Cystic Fibrosis: The Role of the Environmental Reservoirs. Mycopathologia 2024, 189, 19. [Google Scholar] [CrossRef]
- Husain, S.; Sole, A.; Alexander, B.D.; Aslam, S.; Avery, R.; Benden, C.; Billaud, E.M.; Chambers, D.; Danziger-Isakov, L.; Fedson, S.; et al. The 2015 International Society for Heart and Lung Transplantation Guidelines for the Management of Fungal Infections in Mechanical Circulatory Support and Cardiothoracic Organ Transplant Recipients: Executive Summary. J. Heart Lung Transplant. 2016, 35, 261–282. [Google Scholar] [CrossRef]
- Cortez, K.J.; Roilides, E.; Quiroz-Telles, F.; Meletiadis, J.; Antachopoulos, C.; Knudsen, T.; Buchanan, W.; Milanovich, J.; Sutton, D.A.; Fothergill, A.; et al. Infections Caused by Scedosporium Spp. Clin. Microbiol. Rev. 2008, 21, 157–197. [Google Scholar] [CrossRef]
- Ramirez-Garcia, A.; Pellon, A.; Rementeria, A.; Buldain, I.; Barreto-Bergter, E.; Rollin-Pinheiro, R.; de Meirelles, J.V.; Xisto, M.I.D.S.; Ranque, S.; Havlicek, V.; et al. Scedosporium and Lomentospora: An Updated Overview of Underrated Opportunists. Med. Mycol. 2018, 56, 102–125. [Google Scholar] [CrossRef]
- Konsoula, A.; Tsioutis, C.; Markaki, I.; Papadakis, M.; Agouridis, A.P.; Spernovasilis, N. Lomentospora Prolificans: An Emerging Opportunistic Fungal Pathogen. Microorganisms 2022, 10, 1317. [Google Scholar] [CrossRef]
- Johnson, L.S.; Shields, R.K.; Clancy, C.J. Epidemiology, Clinical Manifestations, and Outcomes of Scedosporium Infections among Solid Organ Transplant Recipients. Transpl. Infect. Dis. 2014, 16, 578–587. [Google Scholar] [CrossRef]
- Huggins, J.P.; Pease, R.; Stanly, K.; Workman, A.; Reynolds, J.; Alexander, B.D. Safety of Inhaled Amphotericin B Lipid Complex as Antifungal Prophylaxis in Lung Transplant Recipients. Antimicrob. Agents Chemother. 2022, 66, e0028322. [Google Scholar] [CrossRef] [PubMed]
- Borro, J.M.; Solé, A.; de la Torre, M.; Pastor, A.; Fernandez, R.; Saura, A.; Delgado, M.; Monte, E.; Gonzalez, D. Efficiency and Safety of Inhaled Amphotericin B Lipid Complex (Abelcet) in the Prophylaxis of Invasive Fungal Infections Following Lung Transplantation. Transplant. Proc. 2008, 40, 3090–3093. [Google Scholar] [CrossRef] [PubMed]
- Monforte, V.; Roman, A.; Gavalda, J.; Bravo, C.; Tenorio, L.; Ferrer, A.; Maestre, J.; Morell, F. Nebulized Amphotericin B Prophylaxis for Aspergillus Infection in Lung Transplantation: Study of Risk Factors. J. Heart Lung Transplant. 2001, 20, 1274–1281. [Google Scholar] [CrossRef] [PubMed]
- Verleden, G.M.; Glanville, A.R.; Lease, E.D.; Fisher, A.J.; Calabrese, F.; Corris, P.A.; Ensor, C.R.; Gottlieb, J.; Hachem, R.R.; Lama, V.; et al. Chronic Lung Allograft Dysfunction: Definition, Diagnostic Criteria, and Approaches to Treatment-A Consensus Report from the Pulmonary Council of the ISHLT. J. Heart Lung Transplant. 2019, 38, 493–503. [Google Scholar] [CrossRef]
- Seidel, D.; Meißner, A.; Lackner, M.; Piepenbrock, E.; Salmanton-García, J.; Stecher, M.; Mellinghoff, S.; Hamprecht, A.; Durán Graeff, L.; Köhler, P.; et al. Prognostic Factors in 264 Adults with Invasive Scedosporium Spp. and Lomentospora Prolificans Infection Reported in the Literature and FungiScope®. Crit. Rev. Microbiol. 2019, 45, 1–21. [Google Scholar] [CrossRef]
- Vazirani, J.; Westall, G.P.; Snell, G.I.; Morrissey, C.O. Scedosporium Apiospermum and Lomentospora Prolificans in Lung Transplant Patients—A Single Center Experience over 24 Years. Transpl. Infect. Dis. 2021, 23, e13546. [Google Scholar] [CrossRef]
- Ibáñez-Martínez, E.; Solé, A.; Cañada-Martínez, A.; Muñoz-Núñez, C.F.; Pastor, A.; Montull, B.; Falomir-Salcedo, P.; Valentín, A.; López-Hontangas, J.L.; Pemán, J. Invasive Scedosporiosis in Lung Transplant Recipients: A Nine-Year Retrospective Study in a Tertiary Care Hospital. Rev. Iberoam. Micol. 2021, 38, 184–187. [Google Scholar] [CrossRef]
- Rammaert, B.; Puyade, M.; Cornely, O.A.; Seidel, D.; Grossi, P.; Husain, S.; Picard, C.; Lass-Flörl, C.; Manuel, O.; Le Pavec, J.; et al. Perspectives on Scedosporium Species and Lomentospora Prolificans in Lung Transplantation: Results of an International Practice Survey from ESCMID Fungal Infection Study Group and Study Group for Infections in Compromised Hosts, and European Confederation of Medical Mycology. Transpl. Infect. Dis. 2019, 21, e13141. [Google Scholar] [CrossRef]
- Peghin, M.; Monforte, V.; Martin-Gomez, M.T.; Ruiz-Camps, I.; Berastegui, C.; Saez, B.; Riera, J.; Solé, J.; Gavaldá, J.; Roman, A. Epidemiology of Invasive Respiratory Disease Caused by Emerging Non-Aspergillus Molds in Lung Transplant Recipients. Transpl. Infect. Dis. 2016, 18, 70–78. [Google Scholar] [CrossRef]
- Rodriguez-Tudela, J.L.; Berenguer, J.; Guarro, J.; Kantarcioglu, A.S.; Horre, R.; de Hoog, G.S.; Cuenca-Estrella, M. Epidemiology and Outcome of Scedosporium Prolificans Infection, a Review of 162 Cases. Med. Mycol. 2009, 47, 359–370. [Google Scholar] [CrossRef]
- Konsoula, A.; Agouridis, A.P.; Markaki, L.; Tsioutis, C.; Spernovasilis, N. Lomentospora Prolificans Disseminated Infections: A Systematic Review of Reported Cases. Pathogens 2022, 12, 67. [Google Scholar] [CrossRef] [PubMed]
- Neoh, C.F.; Chen, S.C.A.; Crowe, A.; Hamilton, K.; Nguyen, Q.A.; Marriott, D.; Trubiano, J.A.; Spelman, T.; Kong, D.C.M.; Slavin, M.A. Invasive Scedosporium and Lomentospora Prolificans Infections in Australia: A Multicenter Retrospective Cohort Study. Open Forum Infect. Dis. 2023, 10, ofad059. [Google Scholar] [CrossRef] [PubMed]
- Tortorano, A.M.; Richardson, M.; Roilides, E.; van Diepeningen, A.; Caira, M.; Munoz, P.; Johnson, E.; Meletiadis, J.; Pana, Z.-D.; Lackner, M.; et al. ESCMID and ECMM Joint Guidelines on Diagnosis and Management of Hyalohyphomycosis: Fusarium Spp., Scedosporium Spp. and Others. Clin. Microbiol. Infect. 2014, 20 (Suppl. S3), 27–46. [Google Scholar] [CrossRef] [PubMed]
- Hoenigl, M.; Salmanton-García, J.; Walsh, T.J.; Nucci, M.; Neoh, C.F.; Jenks, J.D.; Lackner, M.; Sprute, R.; Al-Hatmi, A.M.S.; Bassetti, M.; et al. Global Guideline for the Diagnosis and Management of Rare Mould Infections: An Initiative of the European Confederation of Medical Mycology in Cooperation with the International Society for Human and Animal Mycology and the American Society for Microbiology. Lancet Infect. Dis. 2021, 21, e246–e257. [Google Scholar] [CrossRef]
- Bupha-Intr, O.; Butters, C.; Reynolds, G.; Kennedy, K.; Meyer, W.; Patil, S.; Bryant, P.; Morrissey, C.O.; Australasian Antifungal Guidelines Steering Committee. Consensus Guidelines for the Diagnosis and Management of Invasive Fungal Disease Due to Moulds Other than Aspergillus in the Haematology/Oncology Setting, 2021. Intern. Med. J. 2021, 51 (Suppl. S7), 177–219. [Google Scholar] [CrossRef]
- Lackner, M.; de Hoog, G.S.; Verweij, P.E.; Najafzadeh, M.J.; Curfs-Breuker, I.; Klaassen, C.H.; Meis, J.F. Species-Specific Antifungal Susceptibility Patterns of Scedosporium and Pseudallescheria Species. Antimicrob. Agents Chemother. 2012, 56, 2635–2642. [Google Scholar] [CrossRef]
- Lackner, M.; Rezusta, A.; Villuendas, M.C.; Palacian, M.P.; Meis, J.F.; Klaassen, C.H. Infection and Colonisation Due to Scedosporium in Northern Spain. An in Vitro Antifungal Susceptibility and Molecular Epidemiology Study of 60 Isolates. Mycoses 2011, 54 (Suppl. S3), 12–21. [Google Scholar] [CrossRef]
- Boutin, C.-A.; Luong, M.-L. Update on Therapeutic Approaches for Invasive Fungal Infections in Adults. Ther. Adv. Infect. Dis. 2024, 11, 20499361231224980. [Google Scholar] [CrossRef]
- Ryder, N.S.; Leitner, I. Synergistic Interaction of Terbinafine with Triazoles or Amphotericin B against Aspergillus Species. Med. Mycol. 2001, 39, 91–95. [Google Scholar] [CrossRef]
- Jenks, J.D.; Seidel, D.; Cornely, O.A.; Chen, S.; van Hal, S.; Kauffman, C.; Miceli, M.H.; Heinemann, M.; Christner, M.; Jover Sáenz, A.; et al. Voriconazole plus Terbinafine Combination Antifungal Therapy for Invasive Lomentospora Prolificans Infections: Analysis of 41 Patients from the FungiScope® Registry 2008-2019. Clin. Microbiol. Infect. 2020, 26, e1–e784. [Google Scholar] [CrossRef]
- Gow, N.A.R.; Johnson, C.; Berman, J.; Coste, A.T.; Cuomo, C.A.; Perlin, D.S.; Bicanic, T.; Harrison, T.S.; Wiederhold, N.; Bromley, M.; et al. The Importance of Antimicrobial Resistance in Medical Mycology. Nat. Commun. 2022, 13, 5352. [Google Scholar] [CrossRef] [PubMed]
- Rivero-Menendez, O.; Cuenca-Estrella, M.; Alastruey-Izquierdo, A. In Vitro Activity of Olorofim against Clinical Isolates of Scedosporium Species and Lomentospora Prolificans Using EUCAST and CLSI Methodologies. J. Antimicrob. Chemother. 2020, 75, 3582–3585. [Google Scholar] [CrossRef] [PubMed]
- Kirchhoff, L.; Dittmer, S.; Buer, J.; Rath, P.-M.; Steinmann, J. In Vitro Activity of Olorofim (F901318) against Fungi of the Genus, Scedosporium and Rasamsonia as Well as against Lomentospora Prolificans, Exophiala Dermatitidis and Azole-Resistant Aspergillus Fumigatus. Int. J. Antimicrob. Agents 2020, 56, 106105. [Google Scholar] [CrossRef] [PubMed]
- Almajid, A.; Bazroon, A.; Al-Awami, H.M.; Albarbari, H.; Alqahtani, I.; Almutairi, R.; Alsuwayj, A.; Alahmadi, F.; Aljawad, J.; Alnimer, R.; et al. Fosmanogepix: The Novel Anti-Fungal Agent’s Comprehensive Review of in Vitro, in Vivo, and Current Insights From Advancing Clinical Trials. Cureus 2024, 16, e59210. [Google Scholar] [CrossRef]
- Georgacopoulos, O.; Nunnally, N.; Law, D.; Birch, M.; Berkow, E.L.; Lockhart, S.R. In Vitro Activity of the Novel Antifungal Olorofim against Scedosporium and Lomentospora Prolificans. Microbiol. Spectr. 2023, 11, e0278922. [Google Scholar] [CrossRef]
- Febles Leyva, S.; Sierra Yuste, M.; Bujaldón Querejeta, N.; De La Pinta Zazo, C.; Belso Candela, A.; Wikman-Jorgensen, P. A Difficult-to-Treat Septic Arthritis by Scedosporium Apiospermum Successfully Treated with Olorofim. J. Antimicrob. Chemother. 2024, 79, 3358–3359. [Google Scholar] [CrossRef]
- Cobo, F.; González-Sierra, P.A.; Ortega-Gavilán, M.C.; Castellano-Sánchez, L.; Navarro-Marí, J.M. Two Cases of Fungemia Due to Lomentospora Prolificans in Haematological Patients with Different Outcome. Diagn. Microbiol. Infect. Dis. 2024, 110, 116527. [Google Scholar] [CrossRef]
- Neoh, C.F.; Chen, S.C.-A.; Lanternier, F.; Tio, S.Y.; Halliday, C.L.; Kidd, S.E.; Kong, D.C.M.; Meyer, W.; Hoenigl, M.; Slavin, M.A. Scedosporiosis and Lomentosporiosis: Modern Perspectives on These Difficult-to-Treat Rare Mold Infections. Clin. Microbiol. Rev. 2024, 37, e0000423. [Google Scholar] [CrossRef]
- Horré, R.; Marklein, G.; Siekmeier, R.; Nidermajer, S.; Reiffert, S.M. Selective Isolation of Pseudallescheria and Scedosporium Species from Respiratory Tract Specimens of Cystic Fibrosis Patients. Respir. Int. Rev. Thorac. Dis. 2009, 77, 320–324. [Google Scholar] [CrossRef]
- Coron, N.; Pihet, M.; Fréalle, E.; Lemeille, Y.; Pinel, C.; Pelloux, H.; Gargala, G.; Favennec, L.; Accoceberry, I.; Durand-Joly, I.; et al. Toward the Standardization of Mycological Examination of Sputum Samples in Cystic Fibrosis: Results from a French Multicenter Prospective Study. Mycopathologia 2018, 183, 101–117. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).