A Randomized, Open-Label Study to Assess Efficacy of Weekly Assumption of Cholecalciferol versus Calcifediol in Older Patients with Hypovitaminosis D
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hilger, J.; Friedel, A.; Herr, R.; Rausch, T.; Roos, F.; Wahl, D.A.; Pierroz, D.D.; Weber, P.; Hoffmann, K. A systematic review of vitamin D status in populations worldwide. Br. J. Nutr. 2013, 111, 23–45. [Google Scholar] [CrossRef] [Green Version]
- Bouillon, R.; Carmeliet, G.; Verlinden, L.; van Etten, E.; Verstuyf, A.; Luderer, H.F.; Lieben, L.; Mathieu, C.; DeMay, M. Vitamin D and Human Health: Lessons from Vitamin D Receptor Null Mice. Endocr. Rev. 2008, 29, 726–776. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Vitamin D Deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef] [PubMed]
- Girgis, C.M.; Clifton-Bligh, R.; Hamrick, M.W.; Holick, M.; Gunton, J.E. The Roles of Vitamin D in Skeletal Muscle: Form, Function, and Metabolism. Endocr. Rev. 2013, 34, 33–83. [Google Scholar] [CrossRef] [Green Version]
- Wacker, M.; Holick, M.F. Vitamin D—Effects on Skeletal and Extraskeletal Health and the Need for Supplementation. Nutrients 2013, 5, 111–148. [Google Scholar] [CrossRef] [Green Version]
- Cesareo, R.; Falchetti, A.; Attanasio, R.; Tabacco, G.; Naciu, A.M.; Palermo, A. Hypovitaminosis D: Is It Time to Consider the Use of Calcifediol? Nutrients 2019, 11, 1016. [Google Scholar] [CrossRef] [Green Version]
- Sosa Henriquez, M.; Gomez de Tejada Romero, M.J. Cholecalciferol or calcifediol in the management of vitamin d deficiency. Nutrients 2020, 12, 1617. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Valverde, C.; Sosa-Henríquez, M.; Alhambra-Expósito, M.R.; Quesada-Gómez, J.M. Vitamin D3 and calcidiol are not equipotent. J. Steroid Biochem. Mol. Biol. 2016, 164, 205–208. [Google Scholar] [CrossRef]
- Mazzaferro, S.; Goldsmith, D.; Larsson, T.E.; Massy, Z.A.; Cozzolino, M. Vitamin D metabolites and/or analogs: Which D for which patient? Curr. Vasc. Pharmacol. 2014, 12, 339–349. [Google Scholar] [CrossRef]
- Quesada-Gomez, J.M.; Bouillon, R. Is calcifediol better than cholecalciferol for vitamin D supplementation? Osteoporos. Int. 2018, 29, 1697–1711. [Google Scholar] [CrossRef]
- Pappa, H.M.; Bern, E.; Kamin, D.; Grand, R.J. Vitamin D status in gastrointestinal and liver disease. Curr. Opin. Gastroenterol. 2008, 24, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Holt, P.R. Intestinal Malabsorption in the Elderly. Dig. Dis. 2007, 25, 144–150. [Google Scholar] [CrossRef]
- Montoro-Huguet, M.; Belloc, B.; Domínguez-Cajal, M. Small and Large Intestine (I): Malabsorption of Nutrients. Nutrients 2021, 13, 1254. [Google Scholar] [CrossRef]
- Bischoff-Ferrari, H.A.; Dawson-Hughes, B.; Stöcklin, E.; Sidelnikov, E.; Willett, W.C.; Edel, J.O.; Stähelin, H.B.; Wolfram, S.; Jetter, A.; Schwager, J.; et al. Oral supplementation with 25(OH)D3versus vitamin D3: Effects on 25(OH)D levels, lower extremity function, blood pressure, and markers of innate immunity. J. Bone Miner. Res. 2012, 27, 160–169. [Google Scholar] [CrossRef]
- Cashman, K.D.; Seamans, K.M.; Lucey, A.J.; Stöcklin, E.; Weber, P.; Kiely, M.; Hill, T.R. Relative effectiveness of oral 25-hydroxyvitamin D3 and vitamin D3 in raising wintertime serum 25-hydroxyvitamin D in older adults. Am. J. Clin. Nutr. 2012, 95, 1350–1356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pérez-Castrillón, J.L.; Dueñas-Laita, A.; Brandi, M.L.; Jódar, E.; del Pino-Montes, J.; Quesada-Gómez, J.M.; Castro, F.C.; Gómez-Alonso, C.; López, L.G.; Martínez, J.M.O.; et al. Calcifediol is superior to cholecalciferol in improving vitamin D status in postmenopausal women: A randomized trial. J. Bone Miner. Res. 2021, 36, 1967–1978. [Google Scholar] [CrossRef]
- Shieh, A.; Ma, C.; Chun, R.F.; Witzel, S.; Rafison, B.; Contreras, H.; Wittwer-Schegg, J.; Swinkels, L.; Huijs, T.; Hewison, M.; et al. Effects of Cholecalciferol vs Calcifediol on Total and Free 25-Hydroxyvitamin D and Parathyroid Hormone. J. Clin. Endocrinol. Metab. 2017, 102, 1133–1140. [Google Scholar] [CrossRef] [PubMed]
- Vaes, A.M.; Tieland, M.; de Regt, M.F.; Wittwer, J.; van Loon, L.J.; de Groot, L.C. Dose–response effects of supplementation with calcifediol on serum 25-hydroxyvitamin D status and its metabolites: A randomized controlled trial in older adults. Clin. Nutr. 2018, 37, 808–814. [Google Scholar] [CrossRef]
- Ruggiero, C.; Baroni, M.; Bini, V.; Brozzetti, A.; Parretti, L.; Zengarini, E.; Lapenna, M.; Antinolfi, P.; Falorni, A.; Mecocci, P.; et al. Effects of Weekly Supplementation of Cholecalciferol and Calcifediol among the Oldest-Old People: Findings From a Randomized Pragmatic Clinical Trial. Nutrients 2019, 11, 2778. [Google Scholar] [CrossRef] [Green Version]
- Parmelee, P.A.; Thuras, P.D.; Katz, I.R.; Lawton, M.P. Validation of the Cumulative Illness Rating Scale in a Geriatric Residential Population. J. Am. Geriatr. Soc. 1995, 43, 130–137. [Google Scholar] [CrossRef]
- Katz, S.; Ford, A.B.; Moskowitz, R.W.; Jackson, B.A.; Jaffe, M.W. Studies of Illness in the Aged. The index of Adl: A standardized measure of biological and phychological funcation. JAMA 1963, 185, 914–919. [Google Scholar] [CrossRef]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Nurs. Res. 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Pfeiffer, E. A Short Portable Mental Status Questionnaire for the Assessment of Organic Brain Deficit in Elderly Patients. J. Am. Geriatr. Soc. 1975, 23, 433–441. [Google Scholar] [CrossRef]
- Guigoz, P.Y.; Vellas, M.B.; Garry, P.P.J. Assessing the Nutritional Status of the Elderly: The Mini Nutritional Assessment as Part of the Geriatric Evaluation. Nutr. Rev. 1996, 54, S59–S65. [Google Scholar] [CrossRef] [PubMed]
- Bliss, M.R.; McLaren, R.; Exton-Smith, A.N. Mattresses for preventing pressure sores in geriatric patients. Mon. Bull. Minist. Health Public Health Lab. Serv. 1966, 25, 238–268. [Google Scholar]
- Pilotto, A.; Rengo, F.; Marchionni, N.; Sancarlo, D.; Fontana, A.; Panza, F.; Ferrucci, L.; The FIRI-SIGG Study Group. Comparing the Prognostic Accuracy for All-Cause Mortality of Frailty Instruments: A Multicentre 1-Year Follow-Up in Hospitalized Older Patients. PLoS ONE 2012, 7, e29090. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.H.; Gong, H.S. Measurement and Interpretation of Handgrip Strength for Research on Sarcopenia and Osteoporosis. J. Bone Metab. 2020, 27, 85–96. [Google Scholar] [CrossRef]
- Ross, A.C.; Taylor, C.L.; Yaktine, A.L.; del Valle, H.B. Dietary Reference Intakes for CALCIUM and Vitamin D; Reports funded by National Institutes of Health; The National Academies Collection: Washington, DC, USA, 2011. [Google Scholar]
- Bischoff-Ferrari, H.; Willett, W.C.; Orav, E.J.; Lips, P.; Meunier, P.J.; Lyons, R.A.; Flicker, L.; Wark, J.; Jackson, R.D.; Cauley, J.A.; et al. A Pooled Analysis of Vitamin D Dose Requirements for Fracture Prevention. N. Engl. J. Med. 2012, 367, 40–49. [Google Scholar] [CrossRef] [Green Version]
- Bischoff-Ferrari, H.A.; Willett, W.C.; Wong, J.B.; Stuck, A.E.; Staehelin, H.B.; Orav, E.J.; Thoma, A.; Kiel, D.; Henschkowski, J. Prevention of Nonvertebral Fractures with Oral Vitamin D and Dose Dependency: A meta-analysis of randomized controlled trials. Arch. Intern. Med. 2009, 169, 551–561. [Google Scholar] [CrossRef] [Green Version]
- Cosman, F.; De Beur, S.J.; LeBoff, M.S.; Lewiecki, E.M.; Tanner, B.; Randall, S.; Lindsay, R.; National Osteoporosis Foundation. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos. Int. 2014, 25, 2359–2381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Veleva, B.I.; Chel, V.G.; Achterberg, W.P. Efficacy of daily 800 IU vitamin D supplementation in reaching vitamin D sufficiency in nursing home residents: Cross-sectional patient file study. BMC Geriatr. 2014, 14, 103. [Google Scholar] [CrossRef] [Green Version]
- Barger-Lux, M.J.; Heaney, R.P.; Dowell, S.; Chen, T.; Holick, M. Vitamin D and its Major Metabolites: Serum Levels after Graded Oral Dosing in Healthy Men. Osteoporos. Int. 1998, 8, 222–230. [Google Scholar] [CrossRef]
- Jetter, A.; Egli, A.; Dawson-Hughes, B.; Staehelin, H.B.; Stoecklin, E.; Goessl, R.; Henschkowski, J.; Bischoff-Ferrari, H.A. Pharmacokinetics of oral vitamin D(3) and calcifediol. Bone 2014, 59, 14–19. [Google Scholar] [CrossRef]
- Bhoora, S.; Punchoo, R. Policing Cancer: Vitamin D Arrests the Cell Cycle. Int. J. Mol. Sci. 2020, 21, 9296. [Google Scholar] [CrossRef]
- Liu, N.; Su, H.; Zhang, Y.; Kong, J. The protective effect of 1,25(OH)2D3 against cardiac hypertrophy is mediated by the cyclin-dependent kinase inhibitor p21. Eur. J. Pharmacol. 2020, 888, 173510. [Google Scholar] [CrossRef]
- Vanoirbeek, E.; Krishnan, A.; Eelen, G.; Verlinden, L.; Bouillon, R.; Feldman, D.; Verstuyf, A. The anti-cancer and anti-inflammatory actions of 1,25(OH)2D3. Best Pract. Res. Clin. Endocrinol. Metab. 2011, 25, 593–604. [Google Scholar] [CrossRef] [Green Version]
- Bikle, D.D. Vitamin D and Bone. Curr. Osteoporos. Rep. 2012, 10, 151–159. [Google Scholar] [CrossRef] [Green Version]
- Pike, J.W.; Christakos, S. Biology and Mechanisms of Action of the Vitamin D Hormone. Endocrinol. Metab. Clin. N. Am. 2017, 46, 815–843. [Google Scholar] [CrossRef]
- Turner, A.; Hanrath, M.A.; Morris, H.A.; Atkins, G.; Anderson, P. The local production of 1,25(OH)2D3 promotes osteoblast and osteocyte maturation. J. Steroid Biochem. Mol. Biol. 2014, 144 Pt A, 114–118. [Google Scholar] [CrossRef]
- Dawson-Hughes, B. Vitamin D and muscle function. J. Steroid Biochem. Mol. Biol. 2017, 173, 313–316. [Google Scholar] [CrossRef]
- El Hajj, C.; Fares, S.; Chardigny, J.M.; Boirie, Y.; Walrand, S. Vitamin D supplementation and muscle strength in pre-sarcopenic elderly Lebanese people: A randomized controlled trial. Arch. Osteoporos. 2018, 14, 4. [Google Scholar] [CrossRef]
- Manoy, P.; Yuktanandana, P.; Tanavalee, A.; Anomasiri, W.; Ngarmukos, S.; Tanpowpong, T.; Honsawek, S. Vitamin D Supplementation Improves Quality of Life and Physical Performance in Osteoarthritis Patients. Nutrients 2017, 9, 799. [Google Scholar] [CrossRef] [Green Version]
- Davies, M.; Mawer, E.B.; Krawitt, E.L. Comparative absorption of vitamin D3 and 25-hydroxyvitamin D3 in intestinal disease. Gut 1980, 21, 287–292. [Google Scholar] [CrossRef] [Green Version]
- Thompson, G.R.; Lewis, B.; Booth, C.C. Absorption of vitamin D3-3H in control subjects and patients with intestinal malabsorption. J. Clin. Investig. 1966, 45, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Maislos, M.; Silver, J.; Fainaru, M. Intestinal absorption of vitamin D sterols: Differential absorption into lymph and portal blood in the rat. Gastroenterology 1981, 80, 1528–1534. [Google Scholar] [CrossRef]
- Schiller, L.R. Maldigestion Versus Malabsorption in the Elderly. Curr. Gastroenterol. Rep. 2020, 22, 33. [Google Scholar] [CrossRef]

| All Patients N = 140 | Cholecalciferol N = 69 | Calcifediol N = 71 | p-Value | |
|---|---|---|---|---|
| Female (%) | 81 (57.8) | 39 (56.5) | 42 (59.1) | 0.75 |
| Age (years, mean, SD) | 83.8 (6.6) | 84.9 (6.4) | 82.7 (6.7) | 0.052 |
| BMI (median, IQR) | 24.4 (6.1) | 23.7 (7.2) | 25 (5.6) | 0.95 |
| ADL (median, IQR) | 6 (2) | 5 (2) | 6 (1) | 0.42 |
| IADL (median, IQR) | 4 (5) | 4 (5) | 5 (4) | 0.42 |
| MNA (median, IQR) | 25 (5) | 23 (8) | 25 (6) | 0.55 |
| Exton Smith Scale (median, IQR) | 18 (3) | 17 (3) | 18 (3) | 0.74 |
| SPMSQ (median, IQR) | 2 (2) | 2 (2) | 2 (3) | 0.68 |
| CIRS–C (median, IQR) | 3 (2) | 3 (2) | 3 (3) | 0.37 |
| MPI (mean, SD) | 0.35 (0.19) | 0.39 (0.20) | 0.32 (0.18) | 0.37 |
| Arterial hypertension (%) | 98 (70) | 48 (69.6) | 50 (70.4) | 0.33 |
| CAD (%) | 15 (10) | 8 (11.6) | 7 (9.9) | 0.32 |
| AF (%) | 26 (18.6) | 12 (17.4) | 14 (19.7) | 0.77 |
| Heart failure (%) | 57 (40.7) | 29 (42) | 28 (39.4) | 0.57 |
| Diabetes (%) CKD (%) | 29 (20.7) 32 (22.8) | 14 (20.3) 16 (23.2) | 15 (21.1) 16 (22.5) | 0.42 0.30 |
| COPD (%) | 13 (9.3) | 6 (8.6) | 7 (9.8) | 0.54 |
| Number of drugs (median, IQR) | 6 (3) | 7 (3) | 6 (3) | 0.65 |
| Creatinine mg/dl (mean, SD) | 1.15 (0.53) | 1.15 (0.92) | 1.21 (1.02) | 0.24 |
| PTH ng/dL (mean, SD) | 55.3 (38.3) | 48.1 (39.6) | 60.7 (36.9) | 0.17 |
| Serum Calcium mg/dl (mean, SD) | 8.9 (0.4) | 8.8 (0.4) | 9.0 (0.4) | 0.052 |
| Serum Phosphate mg/dl (mean, SD) | 3.25 (0.8) | 3.2 (0.5) | 3.3 (0.8) | 0.35 |
| Serum Albumin g/dl (mean, SD) | 3.5 (0.4) | 3.5 (0.4) | 3.5 (0.4) | 0.64 |
| Handgrip test (mean, SD) Males Females | 17.4 (7.4) 25.9 (5.7) 13.9 (4.8) | 17.5 (7.2) 24.3 (5.4) 13.7 (4.4) | 17.3 (7.2) 27.1 (6,2) 14.1 (5.3) | 0.92 0.34 0.82 |
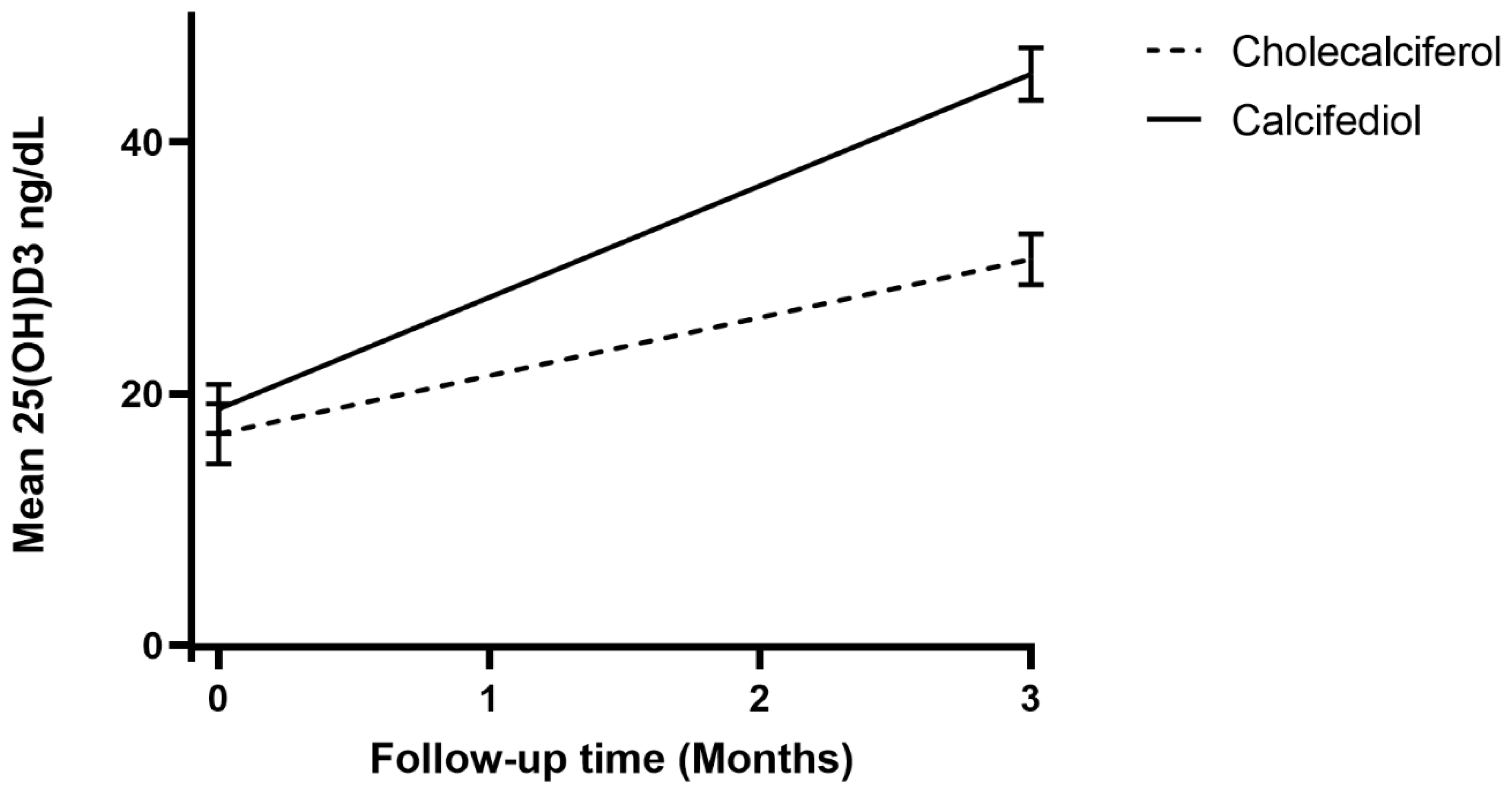
| 25OHVitD at study enrollment (ng/mL) | 17.8 (11.7) | 16.8 (9.9) | 18.8 (13.3) | 0.31 |
| 25OHVitD at 3-month follow-up (ng/mL) | 38.1 (18.3) | 30.7 (8.4) | 45.4 (9.8) | <0.001 |
| 25OHVitD3 mean difference at 3 months (SEM) | 20.2 (+17.8; +23.2) | 13.7 (+11.8; +15.3) | 26.6 (+22.9; +30.1) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okoye, C.; Calsolaro, V.; Niccolai, F.; Calabrese, A.M.; Franchi, R.; Rogani, S.; Coppini, G.; Morelli, V.; Caraccio, N.; Monzani, F. A Randomized, Open-Label Study to Assess Efficacy of Weekly Assumption of Cholecalciferol versus Calcifediol in Older Patients with Hypovitaminosis D. Geriatrics 2022, 7, 13. https://doi.org/10.3390/geriatrics7010013
Okoye C, Calsolaro V, Niccolai F, Calabrese AM, Franchi R, Rogani S, Coppini G, Morelli V, Caraccio N, Monzani F. A Randomized, Open-Label Study to Assess Efficacy of Weekly Assumption of Cholecalciferol versus Calcifediol in Older Patients with Hypovitaminosis D. Geriatrics. 2022; 7(1):13. https://doi.org/10.3390/geriatrics7010013
Chicago/Turabian StyleOkoye, Chukwuma, Valeria Calsolaro, Filippo Niccolai, Alessia Maria Calabrese, Riccardo Franchi, Sara Rogani, Giulia Coppini, Virginia Morelli, Nadia Caraccio, and Fabio Monzani. 2022. "A Randomized, Open-Label Study to Assess Efficacy of Weekly Assumption of Cholecalciferol versus Calcifediol in Older Patients with Hypovitaminosis D" Geriatrics 7, no. 1: 13. https://doi.org/10.3390/geriatrics7010013
APA StyleOkoye, C., Calsolaro, V., Niccolai, F., Calabrese, A. M., Franchi, R., Rogani, S., Coppini, G., Morelli, V., Caraccio, N., & Monzani, F. (2022). A Randomized, Open-Label Study to Assess Efficacy of Weekly Assumption of Cholecalciferol versus Calcifediol in Older Patients with Hypovitaminosis D. Geriatrics, 7(1), 13. https://doi.org/10.3390/geriatrics7010013







