Abstract
Illicit (unrecorded) alcohol is a critical global public health issue because it is produced without regulatory and market oversight with increased risk of safety, quality and adulteration issues. Undertaking iterative research to draw together academic, contemporary and historic evidence, this paper reviews one specific toxicological issue, methanol, in order to identify the policy mitigation strategies of interest. A typology of illicit alcohol products, including legal products, illegal products and surrogate products, is created. A policy landscape matrix is produced that synthesizes the drivers of illicit alcohol production, distribution, sale and consumption, policy measures and activity related signals in order to inform policy development. The matrix illustrates the interaction between capabilities, motivations and opportunities and factors such as access, culture, community norms and behavior, economic drivers and knowledge and information and gives insight into mitigation strategies against illicit alcohol sale and consumption, which may prove of value for policymakers in various parts of the world.
1. Introduction
Alcohol is consumed before, during and after meals; to celebrate birth and mourn death; to socialize and is used as a relaxant and as a deliriant [1]. Globally, alcohol use is one of the important risk factors for non-communicable human disease [2,3]. The harmful use of alcohol results in around 2.5 million deaths a year, and alcohol consumption is the third-highest risk factor for disease and disability. In middle-income countries, alcohol is the biggest risk factor, often related to multiple social problems, including dependence [4]. A reduction in alcohol consumption is associated with a lower risk of heart disease and cancer. There are some studies that indicate that moderate alcohol intake has a preventive effect on cardiovascular disease [5], but negative consequences of regular consumption of alcohol often exceed the benefits. Alcohol is addictive, lacks nutrition value and may be a key cultural component in the human obesity dilemma [6,7], but the exact impact is unclear [8,9].
Global consumption of alcohol in 2005 was an average of 6.13 L of pure alcohol per individual aged 15 years or over, with 28.6% of this amount being unrecorded alcohol, i.e., illegally produced or homemade or sold outside government controls and jurisdiction [4]. The World Health Organization (WHO) estimates consumption increased to 6.4 L in 2016, an increase of 4.4% compared to 2005 [10]. Drinking patterns and associated social norms vary between countries and social groups, and, consequently, the harmful use of alcohol disproportionately affects certain individuals, families and communities more than others [11]. In 2015, European regions had the highest prevalence of heavy episodic alcohol use [2], six times more per capita than Southeast Asia and 20 times more than the Eastern Mediterranean, the region with a high Muslim majority [4]. Cultural norms of abstinence in some communities, often driven by religious beliefs and restrictions, influence the social norms around alcohol consumption [12]. When considering deaths attributed to alcohol, the more significant health burden is with men, showing 7.4% of all male deaths being attributed to alcohol consumption compared to 1.4% with women, and lower socioeconomic status and educational levels are linked to a greater risk [4,13].
Over a quarter of the total alcohol consumed globally is unrecorded, illicit or otherwise described as unreported [3,10]. The WHO describes unrecorded alcohol as “alcohol that is not taxed and is outside the usual system of governmental control, because it is produced, distributed and sold outside formal channels” [5].
Whilst the proportion of unrecorded alcohol in Europe is about 21.9% of total per capita alcohol consumption, this rises to 56.2% in the Eastern Mediterranean and to 69% of consumption in Southeast Asia [4,14]. The proportion of unrecorded alcohol as a percentage of total alcohol is as high as 59% in Bhutan, 44.4% in Kuwait, 42.3% in Uganda and 40.1% in the Republic of Moldova [3]. Thus, illicit alcohol sales form a large proportion of total sales in many countries, are unregulated and there is an associated public health risk that is worthy of further research. Undertaking an iterative narrative review of the literature to draw together academic, contemporary and historic evidence, this paper reviews one specific toxicological issue associated with unreported alcohol, methanol contamination, in order to identify the policy mechanisms of interest that can be explored in further research. A typology of illicit (unrecorded, unreported) alcohol products is created, and a policy landscape matrix synthesizes the drivers of illicit (unrecorded, unreported) alcohol production, distribution, sale and consumption in order to inform policy development.
2. Illicit Alcohol Production
Alcohol is one of the top four most reported fraudulent commodities after meat, seafood and milk [15]. Illicit alcoholic products are a significant health challenge, especially where adulterants, such as methanol, have the potential to cause harm [16,17]. Adulteration is described here as when a drink contains additional material, such as methanol, or is adjusted using extraneous, substandard or inferior ingredients which are often undeclared to the purchaser, thus rendering the product fraudulent [18,19]. Activities to circumvent religious restrictions, alcohol-related taxes or simply individuals motivated by an economic gain to produce and then sell illicit products have led to the multiple fatal case study incidents that form the focus of this study. False declaration associated with wine is a major issue of concern [20,21,22]. Adulteration of alcohol includes the non-disclosed use of ethylene glycol and methanol to fortify (raise the alcohol level) and/ or improve taste [23,24,25,26]. However, despite improved detection methods [27,28,29], the adulteration of alcohol products remains a concern at local, national and international scales. The 2018 European Union (EU) Report on the EU customs enforcement of intellectual property rights (IPR) shows that there has been a significant increase (>50% increase compared to 2016) in the numbers of alcohol beverages detained at the EU border in 2017 [30]. The Republic of Moldova was the main country of provenance for alcoholic beverages suspected of infringing one or more intellectual property rights (IPR) arriving in the EU.
Traditionally, discussion on the food safety issues associated with alcoholic beverages has focused on chemical and physical food safety hazards such as glass or metal from the processing line. Carcinogenic components in alcoholic beverages, such as acetaldehyde, ethyl carbamate, formaldehyde and acrylamide are of concern as well as heavy metals being present [31,32]. However, one of the main concerns is methanol, and this is now considered.
Homemade or informally produced alcoholic beverages are mostly fermented beverages made from sorghum, millet, maize, rice, wheat or fruits [4]. Methanol can be produced in the fermentation process, and its presence along with ethanol in distilled spirits might be a health hazard [26]. The consumption of methanol causes not only death, but also blindness [24], although the problems usually stem from illegal methanol addition to spirits (alcoholic drinks). Methanol is also a raw material found in a variety of products, including antifreeze, solvents, paints, varnishes [25,26], hand sanitizer, cough mixtures, rubbing products and mouthwash, so if these products are intentionally consumed, it can prove fatal. Antifreeze, windscreen wash fluid and other products containing ethylene glycol and methanol are low-cost [24] compared to alcohol and freely available globally. Direct consumption of alcohol-based products has also led to fatalities, including consumption of cologne/perfume [33,34], bath lotion [35], methylated spirits [36] and direct consumption of windscreen wash fluid [37]. In their research from 1992 to 2001 in Turkey, Yayci et al. [33] note a gender influence with methanol poisoning, with men having the predominant fatalities (89.1%) compared to females (10.9%). In Africa, methanol poisoning from illicit alcohol production and sale is a particular health concern [23,38,39,40]. In 1963 in Spain, methanol was used to adulterate mixed alcohol liqueurs, and this incident led to 51 deaths [41]. However, this issue is also a contemporary challenge, as in Iran in 2018, 76 people died, 460 were hospitalized and 768 were made ill from a methanol-poisoning incident [42]. These illicit alcohol products are made in a domestic setting or in semi-industrialized illegal stills [23], and during the COVID-19 pandemic, some false and misleading information about the positive effect of drinking alcohol on preventing or curing a possible infection was disseminated in (social) media [43]. This resulted in a methanol-related mass poisoning outbreak in Iran, where nearly 300 people died in March 2020 [44]. For a wider perspective of the impact of methanol poisoning, a search of academic and grey literature to determine public health incidents () associated with methanol-related poisoning is synthesized in Table 1. This table has been collated before the COVID-19 outbreak so that the potential impact of the pandemic on the supply chain and social behavior is excluded from the analysis.

Table 1.
Examples of toxic methanol incidents (1963–2020) highlighted in the academic literature and the media search ().
This historic and contemporary evidence positions the social and economic impact of illicit alcohol supply where methanol is the key adulterant. The next section of the paper considers the methodology used and how to create a typology for illicit alcohol products.
3. Materials and Methods
The aim of this iterative narrative review is to critique existing literature and frame the context of illicit (unrecorded) alcohol production that is emergent from the academic and grey literature searches. A case-study-based narrative is developed to identify the nature of the incident, country, year incident occurred and the number of casualties (Table 1). The cases are designed to be qualitative and indicative rather than a quantitative representation. Search terms such as “alcohol AND illegal AND unreported AND methanol AND deaths AND casualties” were used to create a snowball academic literature review until data saturation was reached, i.e., no more incidents could be found or further material did not add to the emergent narrative or evidence base. The search was undertaken in the English language only. This is a limitation of the study because, in many countries where methanol poisoning is a public health issue, English is not the first language. However, the common language of the researchers was English. Further work could be undertaken in the future, extending the search string and then searching in a range of languages. The databases used in the search were Science Direct, Google Scholar and Google for the grey literature sources. There was no limitation on age of source in the search, but relevance was considered and any sources deemed not to be relevant were excluded. The case study approach allows for a more holistic inquiry that seeks to be exploratory, explanatory and descriptive [57] in order to drive a causal investigation [58]. Case study analysis is an accepted method for considering business fraud [59,60,61]. A limitation of this approach is the risk of selection bias, and this is considered in the analysis of the findings.
The second stage was to develop a typology of illicit alcohol products. The typology uses four categories. Illicit alcohol products can be summarized into four main categories: (1) illegally produced or smuggled alcohol products (including illegal homemade alcohol), (2) alcohol products that are legitimate, but not in the jurisdiction of their consumption, (3) legal but homemade and (4) surrogate non-beverage alcohol products not intended for human consumption, e.g., industrial alcohol or alcohol-based mouthwash, perfume, etc. [62,63]. These characterizations focus on the products themselves rather than considering their modes of distribution. Illicit trade can also be considered in terms of both the product (legal/illegal) and the modes of distribution (legal/illegal; within-borders or cross-borders), i.e., (1) legal products being illegally distributed within national boundaries, (2) illegal products being distributed within national boundaries, (3) legal products being illegally distributed across borders and (4) illegal products being distributed across borders [64]. Based on these elements and the incidents in Table 1, a typology has been developed (Table 2) that extends product type and product description and considers mode of distribution either within national borders or between countries.

Table 2.
Typology of illicit (unrecorded, unreported) alcohol production (Adapted from [62,63,64]).
4. Results
Within the typology, there are three categories where illicit alcohol is produced, distributed, sold and consumed: legally produced products that can then access an alternative or illicit market/supply chain; illegally produced products that can be sold in an alternative supply chain or can pass into a legal supply chain and third, surrogate products that are not produced for human consumption. It is worth noting that the production of illicit alcohol is often carried out in unhygienic and uncontrolled conditions, and contraband/smuggled alcohol products are beyond the safeguards of the official control of imported foodstuffs. Workers in facilities producing illicit alcohol, and the general public in the area, can be exposed to the risk of industrial accidents, e.g., explosion [65]. Therefore, having described the typology, how can governance frameworks be developed to address illegal alcohol production and sales?
There is a strong economic driver for individuals and organizations to engage in illicit practices [16]. Factors that frame and incentivize this activity include weak public and private institutions, corruption, low Gross Domestic Product (GDP), low tax morale, high taxes or complex tax systems [66,67] and the price differential between illegal and legal alternatives [67]. The classic “fraud diamond” model proposes that four factors influence the potential for illicit behavior: motivation, capability, opportunity and pressure [68]. The main motivation for illicit behavior may be the economic gain derived, to circumvent cultural or religious restrictions on access to alcohol and/or to support an individual’s own alcohol dependence. Capability, i.e., the ability of an individual or organization to undertake deceptive activities requires both the knowledge and equipment to produce alcohol for home use, evading the associated taxes and excise duty or otherwise to distribute and sell illicit alcohol. The opportunity to supply illicit alcohol, either to themselves or others, is also a factor of influence and such opportunity is mediated by the level of regulatory governance in particular countries. Thus, there are both economic and social drivers of illicit alcohol production, distribution and sale, and these form pressure that leads to the development of socioeconomic networks with inter-related strategies, activities and dynamic components that drive illicit alcohol consumption or other forms of alcohol-based product abuse [69]. In order to understand these drivers and their interrelationship in more depth, a conceptual policy landscape matrix has been postulated (Figure 1) that illustrates the interaction between capabilities, motivations and opportunities and factors such as access, culture, community norms and behavior, economic drivers and knowledge and information. Pressure was not taken into consideration as a single issue here, but seen to be embedded implicitly in all aspects of the policy landscape matrix. The matrix provides an opportunity to consider policy implications for reducing illicit alcohol production, distribution, sale and consumption, policy measures that could be employed at the state (public) and the market (private) level and the potential data sources (signals) that can arise.
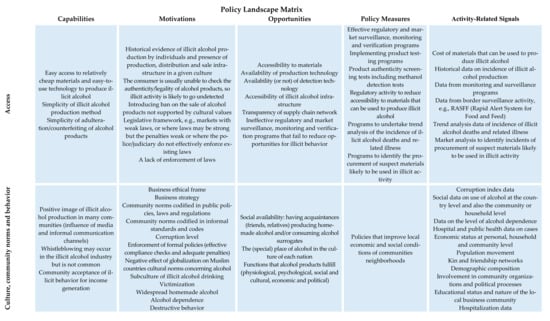
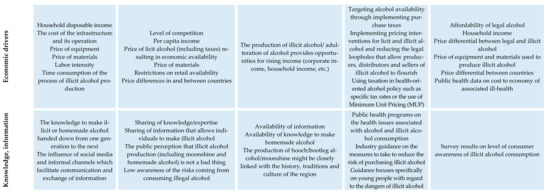
Figure 1.
Drivers of illicit alcohol production, distribution, sale and consumption, policy measures and activity-related signals (Adapted from [38,65,69,70,71,72,73,74,75]).
The policy implications are addressed in the four areas of the policy landscape matrix (Figure 1): with policy measures related to access, knowledge and information; economic drivers and culture; community norms and behavior—and these are now considered in turn.
- Access-related policy measures
Effective regulatory and market surveillance, monitoring and verification programs reduce opportunities for illicit behavior to remain undetected. Policy measures such as implementing product testing programs as part of a wider policy initiative will identify harmful alcohol at the point of production, sale or distribution. Non-targeted product authenticity screening tests are of value as well as targeted adulterant-specific testing such as for the presence of methanol [76,77,78]. A coordinated surveillance program is required across specific trading areas such as the EU; otherwise, if one member state is contributing less to systems such as the RASFF database, or there is a variance in national arrangements of food control systems (in accordance with “Official Control Regulation”), this creates the possibility for a member state to become a “back door” for allowing illicit alcohol products to then have free movement of food within the EU [79,80]. Regulatory activity to reduce accessibility to materials that can be used to produce illicit alcohol should be introduced as well as programs to identify the procurement of suspect materials likely to be used in illicit activity. Further, as part of wider public health surveillance, there should be programs adopted to ensure trend analysis of the incidence of illicit alcohol deaths and related illnesses through the integration of public health data from hospitals and the community.
- Knowledge- and information-related policy measures
Following the methanol poisoning in Iran in 2018, Aghababaeian et al. [42] state that incidents often occur in low-income Islamic countries, and so effective educational programs are required to raise public awareness of the health issues involved. These programs can use a range of media and communication channels to explain the dangers of production, consumption, distribution and sale of illicit alcohol. Abramowicz et al. [80] underline in their study that activities undertaken via education/prevention schemes should be aimed at a particular group of consumers, appropriately profiled and fully tailored to their needs. Growing children and adolescents are a key target group here since they often undertake new forms of behavior and experimentation, including using alcohol, in order to determine their place in society [81].
Industry guidance on the measures to take to reduce the risk of purchasing illicit alcohol is also important. Shapira et al. [82], in their study on methanol levels in illegal alcoholic beverages sold in a low socioeconomic area of Tel-Aviv, state there is a need to inform shopkeepers about labeling regulations and “make information and health warnings accessible to the foreign-born population residing in the area,”, i.e., that information must be accessible, context-specific and available if required in a range of languages. The more alcohol marketing that young people are exposed to, the more alcohol they will consume; indeed, restrictions on access to alcohol for young people may actually promote this illicit parallel market [83], creating an “underground economy” as demand remains the same, but can no longer be met through legal supply routes.
- Economic-related policy measures
Economic related policy measures that have, or could be adopted include: targeting alcohol availability, implementing purchase taxes [38], implementing pricing interventions for licit and illicit alcohol and reducing the legal loopholes that allow producers, distributors and sellers of illicit alcohol to flourish [70]. In Europe, there is a long-standing debate about the effectiveness of using taxation in health-oriented alcohol policy such as specific tax rates or the use of Minimum Unit Pricing (MUP) [75], as in Australia and the UK, including Scotland [84]. In Canada, Social Reference Prices (SRPs) for alcoholic beverages, i.e., “floor” or “minimum” prices for a given “unit” or “standard drink”, have been set [85]. As inter alia alcohol tax regimes vary across territorial domains and product categories; this leads to differential pricing of similar products between markets and between products categories within a given market. This might increase the incentive for illicit behavior.
The main opposition to this policy approach comes from the alcohol industry and free-market-oriented think tanks [84]. Transnational alcohol corporations, in contrast to tobacco corporations in their market sector, continue to have a significant impact on alcohol policy globally [75,86,87]. As a rule, consumption of licit alcohol declines as price increases [71]. Consumption of illicit alcohol may grow as licit alcohol price increases; however, raising taxes on licit (recorded) alcohol together with reinforcing measures against unrecorded alcohol might lead to a decline in total alcohol consumption. Moreover, when restrictions are placed on the retail availability of licit alcohol, whilst consumption of licit alcohol decrease [71], consumption of illicit alcohol may increase unless the protection against unrecorded alcohol sale and consumption is strengthened. Furthermore, producers of illicit alcohol tend to increase prices when recorded alcohol beverages prices are on the rise. These phenomena limit the effectiveness of economic policy measures and make it hard to find the optimum fiscal solution.
- Culture, community norms and behavior-related policy measures
Illicit alcohol use, as with drug use, is associated with specific social networks, so social causation and neighborhood mitigation processes may discourage illicit alcohol use [72]. Madureira-Lima and Galea [88] created an Alcohol Control Policy Index (ACPI), including policies from the WHO’s Global Strategy to Reduce the Harmful Use of Alcohol. These are leadership, awareness and commitment; health services’ response; community action; drink driving policies and countermeasures; availability of alcohol; marketing of alcoholic beverages; pricing policies; monitoring and surveillance, reducing the negative consequences of drinking and alcohol intoxication and the focus of this study, reducing the public health impact of illicit alcohol and illegally produced alcohol. In Iran, 9 out of the 10 policy measures have been introduced, excluding pricing policy [89]. However, some communities, especially low-income groups, have an innate cultural relationship with illicit alcohol consumption, and in these social groups, addressing illicit alcohol within a wider alcohol management plan is of value [90,91]. Thus, for policies to be effective, they need to reflect the social context in which they are adopted.
- Early warning systems (EWSs) to reduce illicit alcohol sale and consumption
The development of an EWS is an essential policy measure to mitigate illicit alcohol sale and consumption. EWSs allow health officials to be alerted so they can minimize the health impact of an illicit alcohol or methanol incident on the population. Recognizing the types of signals of concern underpins the development of an EWS for illicit alcohol sale and consumption. Some signals may be weak, i.e., imprecise early indicators of an impending event, or they may provide stronger evidence of a potential incident [92,93]. The process of developing an EWS can be broken down into the following elements:
- Monitoring phase—considering specific criteria and ensuring the data can be collected and is of the required granularity;
- Analysis phase—assessing data, indicators, trends in order to be able to differentiate critical events;
- Prediction phase—depending on the level of criticality, early warning information is generated and communicated to relevant stakeholders; and
- Implementation phase—appropriate measures are defined and implemented [94].
Signal detection theory reflects the challenging issue of detecting a given signal against a background of noise, i.e., in a situation of uncertainty [95]. Signals or indicators can be monitored to determine any trends and if these trends give cause for concern (Phase 1). The analysis phase (Phase 2) requires signals to be assessed to determine any associations with other variables, e.g., gender, age, location, frequency, distribution, symptoms, duration of illness, severity and outcome [96]. The policy landscape matrix developed in this research requires the translation of discrete signals and their amplification to develop a risk signal. The signal can be characterized by its degree of relevance and also by its strength, i.e., the magnitude of evidence, single or multi-dimensional [97]. The signal. as a result, can be validated to ensure that the information received is sufficient to suggest causal association and support further action based on the information. Thus, regulatory sampling can provide some signals, but other signals will come from both social and economic factors that influence illicit behavior. Signal detection and the wider policy program need to be linked to sufficient resources that underpin information systems, policy measures and reporting systems designed to reduce the risk of illicit alcohol to public health.
In 2018, the WHO launched the SAFER initiative alongside the United Nations’ third high-level meeting on prevention and control of non-communicable diseases (NCDs) to provide support in reducing the harmful use of alcohol through: (1) strengthening restrictions on alcohol availability; (2) advancing and enforcing drink-driving countermeasures; (3) facilitating access to screening, brief interventions and treatment; (4) enforcing bans or comprehensive restrictions on alcohol advertising, sponsorship and promotion; (5) raising prices on alcohol through excise taxes and other pricing policies [98]. The WHO’s document suggests eradicating illicit alcohol or bringing it under government control in countries where informal markets are the main source of alcohol. Another suggestion is to develop tax policies that make low-alcohol and non-alcoholic variations of culturally preferred beverages more attractive and to introduce tax stamps to show that duty has been paid on informal products.
5. Conclusions
Illegal and unrecorded alcohol and its illicit substitutes lack the regulatory and market oversight that legal alcohol products would have, increasing the risk of safety, quality and fraud issues. As illicit alcohol is produced without the management controls and verification systems that are used in the legitimate supply chain, it is a cause of global concern as it presents a clear personal risk to those that consume it. This research has drawn together academic, contemporary and historic evidence on the impact of illicit alcohol production, distribution and consumption. The policy mechanisms that can be explored in further research are identified. A typology of illicit alcohol products is created, and a policy landscape matrix synthesizes the drivers of illicit alcohol production, distribution, sale and consumption in order to inform policy development. Policy measures are addressed in four areas: (1) access; (2) culture, community norms and behavior; (3) economic drivers; and (4) knowledge and information. Methanol, one of the main agents that cause alcohol-related disability or fatality, is shown in this work to be a significant and widely distributed concern as a food-related toxin with global impact. This public health harm needs to be addressed by concerted action at regulatory and market levels. Further, the level of reported illicit alcohol-related health incidents identified in the academic literature, grey literature and media sources described herein has provided strong supporting evidence within a synthesized timeline of the locations and size of this global public health problem.
Author Contributions
L.M. and A.K. were involved in all stages of the research, including conceptualization, methodology, formal analysis, writing original draft preparation, writing and review and editing. Both authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
The study did not involve humans.
Data Availability Statement
Data sharing not applicable.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Cnossen, S. Alcohol taxation and regulation in the European Union. Int. Tax Public Financ. 2007, 14, 699–732. [Google Scholar] [CrossRef]
- Peacock, A.; Leung, J.; Larney, S.; Colledge, S.; Hickman, M.; Rehm, J.; Giovino, G.A.; West, R.; Hall, W.; Griffiths, P.; et al. Global statistics on alcohol, tobacco and illicit drug use: 2017 status report. Addiction 2018, 113, 1905–1926. [Google Scholar] [CrossRef]
- Probst, C.; Manthey, J.; Merey, A.; Rylett, M.; Rehm, J. Unrecorded alcohol use: A global modelling study based on nominal group assessments and survey data. Addiction 2018, 113, 1231–1241. [Google Scholar] [CrossRef] [PubMed]
- WHO (World Health Organization). Global Status Report on Alcohol and Health; WHO: Geneva, Switzerland, 2011; p. 5. Available online: https://www.who.int/substance_abuse/publications/global_alcohol_report/msbgsruprofiles.pdf (accessed on 10 September 2019).
- Van Dooren, C.; Marinussen, M.; Blonk, H.; Aiking, H.; Vellinga, P. Exploring dietary guidelines based on ecological and nutritional values: A comparison of six dietary patterns. Food Policy 2014, 44, 36–46. [Google Scholar] [CrossRef]
- Yeomans, M.R. Alcohol, appetite and energy balance: Is alcohol intake a risk factor for obesity? Physiol. Behav. 2010, 100, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Kate, B.T.L.S.; Battista, K.; Leatherdale, S.T. Estimating how extra calories from alcohol consumption are likely an overlooked contributor to youth obesity. Health Promot. Chronic Dis. Prev. Can. 2017, 37, 194–200. [Google Scholar] [CrossRef]
- Traversy, G.; Chaput, J.-P. Alcohol Consumption and Obesity: An Update. Curr. Obes. Rep. 2015, 4, 122–130. [Google Scholar] [CrossRef]
- O’Donovan, G.; Stamatakis, E.; Hamer, M. Associations between alcohol and obesity in more than 100 000 adults in England and Scotland. Br. J. Nutr. 2018, 119, 222–227. [Google Scholar] [CrossRef]
- World Health Organization. Global Health Observatory. Global Information System on Alcohol and Health. Available online: https://www.who.int/gho/alcohol/en/ (accessed on 20 March 2021).
- Chaiyasong, S.; Huckle, T.; Mackintosh, A.M.; Meier, P.; Parry, C.D.; Callinan, S.; Casswell, S. Drinking patterns vary by gender, age and country-level income: Cross-country analysis of the International Alcohol Control Study. Drug Alcohol Rev. 2018, 37, S53–S62. [Google Scholar] [CrossRef]
- Heiman, A.; Gordon, B.; Zilberman, D. Food beliefs and food supply chains: The impact of religion and religiosity in Israel. Food Policy 2019, 83, 363–369. [Google Scholar] [CrossRef]
- MacKenbach, J.P.; Kulhánová, I.; Bopp, M.; Borrell, C.; Deboosere, P.; Kovács, K.; Looman, C.W.N.; Leinsalu, M.; Mäkelä, P.; Martikainen, P.; et al. Inequalities in Alcohol-Related Mortality in 17 European Countries: A Retrospective Analysis of Mortality Registers. PLoS Med. 2015, 12, e1001909. [Google Scholar] [CrossRef]
- WHO (World Health Organization). Global Status Report on Alcohol and Health; WHO: Geneva, Switzerland, 2018; Available online: https://apps.who.int/iris/bitstream/handle/10665/274603/9789241565639-eng.pdf (accessed on 12 May 2019).
- Bouzembrak, Y.; Steen, B.; Neslo, R.; Linge, J.; Mojtahed, V.; Marvin, H. Development of food fraud media monitoring system based on text mining. Food Control. 2018, 93, 283–296. [Google Scholar] [CrossRef]
- Soon, J.M.; Manning, L. Developing anti-counterfeiting measures: The role of smart packaging. Food Res. Int. 2019, 123, 135–143. [Google Scholar] [CrossRef]
- Lachenmeier, D.W.; Neufeld, M.; Rehm, J. The impact of unrecorded alcohol use on health: What do we know in 2020? J. Stud. Alcohol Drugs 2021, 82, 28–41. [Google Scholar] [CrossRef]
- Spink, J.; Moyer, D.C. Defining the Public Health Threat of Food Fraud. J. Food Sci. 2011, 76, R157–R163. [Google Scholar] [CrossRef]
- Manning, L.; Soon, J.M. Developing systems to control food adulteration. Food Policy 2014, 49, 23–32. [Google Scholar] [CrossRef]
- Feher, I.; Magdas, D.A.; Dehelean, A.; Sârbu, C. Characterization and classification of wines according to geographical origin, vintage and specific variety based on elemental content: A new chemometric approach. J. Food Sci. Technol. 2019, 56, 5225–5233. [Google Scholar] [CrossRef]
- Uttl, L.; Hurkova, K.; Kocourek, V.; Pulkrabova, J.; Tomaniova, M.; Hajslova, J. Metabolomics-based authentication of wines according to grape variety. Czech. J. Food Sci. 2019, 37, 239–245. [Google Scholar] [CrossRef]
- de Lima, C.M.; Fernandes, D.D.S.; Pereira, G.E.; de Araújo Gomes, A.; de Araújo, M.C.U.; Diniz, P.H.G.D. Digital image-based tracing of geographic origin, winemaker, and grape type for red wine authentication. Food Chem. 2020, 312, 126060. [Google Scholar] [CrossRef]
- Laher, A.; Goldstein, L.; Wells, M.; Dufourq, N.; Moodley, P. Unwell after drinking homemade alcohol—A case of ethylene glycol poisoning. Afr. J. Emerg. Med. 2013, 3, 71–74. [Google Scholar] [CrossRef][Green Version]
- Neufeld, M.; Lachenmeier, D.; Hausler, T.; Rehm, J. Surrogate alcohol containing methanol, social deprivation and public health in Novosibirsk, Russia. Int. J. Drug Pol. 2016, 37, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Rostrup, M.; Edwards, J.K.; Abukalish, M.; Ezzabi, M.; Some, D.; Ritter, H.; Lind, K. The methanol poisoning outbreaks in Libya 2013 and Kenya. PLoS ONE 2016, 11, e0152676. [Google Scholar]
- Shafi, H.; Imran, M.; Usman, H.F.; Sarwar, M.; Tahir, M.A. Eight fatalities due to drinking methanol-tainted alcohol in Pakistan: A case report. Egypt. J. Forensic Sci. 2016, 6, 515–519. [Google Scholar] [CrossRef]
- Barroso, J.; Díez-Buitrago, B.; Saa, L.; Möller, M.; Briz, N.; Pavlov, V. Specific bioanalytical optical and photoelectrochemical assays for detection of methanol in alcoholic beverages. Biosens. Bioelectron. 2018, 101, 116–122. [Google Scholar] [CrossRef] [PubMed]
- Hassanian-Moghaddam, H.; Rafizadeh, A.; Shariati, S.; Rafizadeh, M.; Zamani, N. Evaluation of methanol content of beverages using an easy modified chromotropic acid method. Food Chem. Toxicol. 2018, 121, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Martínez, N.J.; Gómez-Ojea, R.; Tomás-Huercio, O.; Herráez-Hernández, R.; Campíns-Falcó, P. Colorimetric determination of alcohols in spirit drinks using a reversible solid sensor. Food Control. 2018, 94, 7–16. [Google Scholar] [CrossRef]
- EU (European Union). Report on the EU Customs Enforcement of Intellectual Property Rights: Results at the EU border; Publications Office of the European Union: Luxembourg, 2017; Available online: https://ec.europa.eu/taxation_customs/sites/taxation/files/report_on_eu_customs_enforcement_of_ipr_2017_en.pdf (accessed on 21 May 2019).
- Paiano, V.; Bianchi, G.; Davoli, E.; Negri, E.; Fanelli, R.; Fattore, E. Risk assessment for the Italian population of acetaldehyde in alcoholic and non-alcoholic beverages. Food Chem. 2014, 154, 26–31. [Google Scholar] [CrossRef]
- Jayakody, L.N.; Lane, S.; Kim, H.; Jin, Y.-S. Mitigating health risks associated with alcoholic beverages through metabolic engineering. Curr. Opin. Biotechnol. 2016, 37, 173–181. [Google Scholar] [CrossRef]
- Yayci, N.; Ağritmiş, H.; Turla, A.; Koç, S. Fatalities due to methyl alcohol intoxication in Turkey: An 8-year study. Forensic Sci. Int. 2003, 131, 36–41. [Google Scholar] [CrossRef]
- Zhang, G.; Crews, K.; Wiseman, H.; Bates, N.; Hovda, K.E.; Archer, J.R.; Dargan, P.I. Application to Include Fomepizole on the WHO Model List of Essential Medicines. Available online: https://www.who.int/selection_medicines/committees/expert/19/applications/Fomepizole_4_2_AC_Ad.pdf (accessed on 17 October 2019).
- Nechepurenko, I. In Russia, Dozens Die After Drinking Alcohol Substitute. Available online: https://www.nytimes.com/2016/12/19/world/europe/russia-bath-lotion-deaths.html (accessed on 10 May 2019).
- Scrimgeour, E.M. Outbreak of methanol and isopropanol poisoning in new britain, papua new guinea. Med. J. Aust. 1980, 2, 36–38. [Google Scholar] [CrossRef]
- Davis, L.E.; Hudson, D.; Benson, B.E.; Easom, L.A.J.; Coleman, J.K. Methanol Poisoning Exposures in the United States: 1993. J. Toxicol. Clin. Toxicol. 2002, 40, 499–505. [Google Scholar] [CrossRef]
- Mkuu, R.; Barry, A.E.; Swahn, M.H.; Nafukho, F. Unrecorded alcohol in East Africa: A case study of Kenya. Int. J. Drug Policy 2019, 63, 12–17. [Google Scholar] [CrossRef]
- Namondwe, T.; Ching’Anda, C.; Gama, A.P.; Matumba, L.; Namomdwe, T. Consumption of illegal home-made alcohol in Malawi: A neglected public health threat. Alcohol 2019, 75, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Okaru, A.O.; Abuga, K.O.; Kibwage, I.O.; Lachenmeier, D.W. High Ethanol Contents of Spirit Drinks in Kibera Slums, Kenya: Implications for Public Health. Foods 2017, 6, 89. [Google Scholar] [CrossRef] [PubMed]
- Sequeiro, N. Os Esquecidos do Metílico. Available online: http://www.galiciahoxe.com/vivir-hoxe-sociedade/gh/esquecidos-do-metilico/idEdicion-2010-09-27/idNoticia-593940 (accessed on 10 May 2019).
- Aghababaeian, H.; Ahvazi, L.A.; Ostadtaghizadeh, A. The Methanol Poisoning Outbreaks in Iran 2018. Alcohol Alcohol. 2019, 54, 128–130. [Google Scholar] [CrossRef] [PubMed]
- Iranpour, P.; Firoozi, H.; Haseli, S. Methanol Poisoning Emerging as the Result of COVID-19 Outbreak; Radiologic Perspective. Acad. Radiol. 2020, 27, 755–756. [Google Scholar] [CrossRef] [PubMed]
- Soltaninejad, K. Methanol Mass Poisoning Outbreak, a Consequence of COVID-19 Pandemic and Misleading Messages on Social Media. Int. J. Occup. Environ. Med. 2020, 11, 148–150. [Google Scholar] [CrossRef]
- BBC. Who, What, Why: Why are Indians Dying from Alcohol Poisoning? Available online: https://www.bbc.co.uk/news/magazine-16197280 (accessed on 10 May 2019).
- Levy, P.; Hexdall, A.; Gordon, P.; Boeriu, C.; Heller, M.; Nelson, L. Methanol contamination of Romanian home-distilled alcohol. J. Toxicol. Clin. Toxicol. 2003, 41, 23–28. [Google Scholar] [CrossRef]
- BBC. Deadly brew hits Madagascar. Available online: http://news.bbc.co.uk/1/hi/world/africa/1900624.stm (accessed on 10 May 2019).
- Paasma, R.; Hovda, K.; Tikkerberi, A.; Jacobsen, D.; Paasma, R.; Hovda, K.; Tikkerberi, A.; Jacobsen, D. Methanol mass poisoning in Estonia: Outbreak in 154 patients. Clin. Toxicol. 2007, 45, 152–157. [Google Scholar] [CrossRef]
- Abdul-Rahim, F.A.; Al Shiekh, A. Substance abuse and homelessness: Mass methanol poisoning in Khartoum. Sud. Med. J. 2012, 48, 1–6. [Google Scholar]
- Zakharov, S.; Pelclova, D.; Navratil, T.; Belacek, J.; Kurcova, I.; Komzak, O.; Salek, T.; Latta, J.; Turek, R.; Bocek, R.; et al. Intermittent hemodialysis is superior to continuous veno-venous hemodialysis/hemodiafiltration to eliminate methanol and formate during treatment for methanol poisoning. Kidney Int. 2014, 86, 199–207. [Google Scholar] [CrossRef]
- Zakharov, S.; Nurieva, O.; Navratil, T.; Diblík, P.; Kuthan, P.; Pelclova, D. Acute methanol poisonings: Folates administration and visual sequelae. J. Appl. Biomed. 2014, 12, 309–316. [Google Scholar] [CrossRef]
- Ohimain, E.I. Methanol contamination in traditionally fermented alcoholic beverages: The microbial dimension. SpringerPlus 2016, 5, 1–10. [Google Scholar] [CrossRef] [PubMed]
- BBC. Indian Toxic Alcohol: At Least 130 Tea Workers Dead from Bootleg Drink. Available online: https://www.bbc.co.uk/news/world-asia-india-47341941 (accessed on 10 May 2019).
- Mackintosh, E.; Dominquez, C.; McCluskey, M. Tainted Alcohol Kills 19 in Costa Rica Ministry Says, Urging Caution. Available online: https://edition.cnn.com/2019/07/21/americas/costa-rica-alcohol-poisoning-methanol-intl/index.html (accessed on 11 August 2019).
- Plante, S.B. Tourist Deaths in the Dominican Republic are Sparking Concern Among Travellers. Available online: https://www.vox.com/the-goods/2019/6/26/18759843/dominican-republic-tourist-deaths (accessed on 10 August 2019).
- Outbreak News Today. Methanol Poisoning Cluster in Malaysia. Available online: http://outbreaknewstoday.com/methanol-poisoning-cluster-in-malaysia-89090/ (accessed on 10 August 2019).
- Yin, R.K. Applications of Case Study Research; SAGE Publications: Newbury Park, CA, USA, 1993. [Google Scholar]
- Tellis, W. Application of a Case Study Methodology. Qual. Rep. 1997, 3, 1–19. [Google Scholar] [CrossRef]
- Jans, M.; Lybaert, N.; Vanhoof, K. Internal fraud risk reduction: Results of a data mining case study. Int. J. Account. Inf. Syst. 2010, 11, 17–41. [Google Scholar] [CrossRef]
- Amara, I.; Ben Amar, A.; Jarboui, A. Detection of Fraud in Financial Statements: French Companies as a Case Study. Int. J. Acad. Res. Account. Financ. Manag. Sci. 2013, 3. [Google Scholar] [CrossRef]
- Bosley, S.; Knorr, M. Pyramids, Ponzis and fraud prevention: Lessons from a case study. J. Financ. Crime 2018, 25, 81–94. [Google Scholar] [CrossRef]
- Lachenmeier, D.W.; Rehm, J. Unrecorded alcohol: A threat to public health? Addiction 2009, 104, 875–877. [Google Scholar]
- Lachenmeier, D.W.; Sarsh, B.; Rehm, J. The Composition of Alcohol Products from Markets in Lithuania and Hungary, and Potential Health Consequences: A Pilot Study. Alcohol Alcohol. 2008, 44, 93–102. [Google Scholar] [CrossRef]
- Joossens, L.; Raw, M. From cigarette smuggling to illicit tobacco trade. Tobacco Control. 2012, 21, 230–234. [Google Scholar] [CrossRef] [PubMed]
- Skehan, P.; Sanchez, I.; Hastings, L. The size, impacts and drivers of illicit trade in alcohol. In OECD, Illicit Trade: Converging Criminal Networks; OECD Publishing: Paris, France, 2019; pp. 217–246. [Google Scholar]
- Snowdon, C. Drinking in the Shadow Economy. IEA Discussion Paper No. 43; The Institute of Economic Affairs: London, UK, 2012; Available online: https://iea.org.uk/wp-content/uploads/2016/07/Drinking%20in%20the%20Shadow%20Economy_0.pdf (accessed on 25 May 2019).
- Soon, J.M.; Manning, L.; Smith, R. Advancing understanding of pinch-points and crime prevention in the food supply chain. Crime Prev. Community Saf. 2019, 21, 42–60. [Google Scholar] [CrossRef]
- Wolfe, D.T.; Hermanson, D.R. The Fraud Diamond: Considering the Four Elements of Fraud. CPA J. 2004, 74, 38–42. [Google Scholar]
- Manning, L.; Soon, J.M.; de Aguiar, L.K.; Eastham, J.F.; Higashi, S.Y. Pressure: Driving illicit behaviour in the food supply chain. 2017. In Proceedings of the 12th Research Workshop on Institutions and Organisations (12th RWIO), Brasilia, Brazil, 10–11 July 2017. [Google Scholar]
- Neufeld, M.; Rehm, J. Effectiveness of policy changes to reduce harm from unrecorded alcohol in Russia between 2005 and now. Int. J. Drug Policy 2018, 51, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Birckmayer, J.D.; Holder, H.D.; Yacoubian, J.G.S.; Friend, K.B. A General Causal Model to Guide Alcohol, Tobacco, and Illicit Drug Prevention: Assessing the Research Evidence. J. Drug Educ. 2004, 34, 121–153. [Google Scholar] [CrossRef]
- Linton, S.L.; Haley, D.F.; Hunter-Jones, J.; Ross, Z.; Cooper, H.L. Social causation and neighborhood selection underlie associations of neighborhood factors with illicit drug-using social networks and illicit drug use among adults relocated from public housing. Soc. Sci. Med. 2017, 185, 81–90. [Google Scholar] [CrossRef]
- Gorman, D.M.; Labouvie, E.W. Using social indicators to inform community drug and alcohol prevention policy. J. Public Health Policy 2000, 21, 428. [Google Scholar] [CrossRef]
- Van Ruth, S.M.; Huisman, W.; Luning, P.A. Food fraud vulnerability and its key factors. Trends Food Sci. Technol. 2017, 67, 70–75. [Google Scholar] [CrossRef]
- Zatoński, M.; Hawkins, B.; McKee, M. Framing the policy debate over spirits excise tax in Poland. Health Promot. Int. 2016, 33, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Abegg, S.; Magro, L.; Broek, J.V.D.; Pratsinis, S.E.; Güntner, A.T. A pocket-sized device enables detection of methanol adulteration in alcoholic beverages. Nat. Food 2020, 1, s43016–s43020. [Google Scholar] [CrossRef]
- Lachenmeier, D.W. Advances in the Detection of the Adulteration of Alcoholic Beverages Including Unrecorded Alcohol. In Advances in Food Authenticity Testing; Woodhead Publishing: Sawston, UK, 2016; pp. 565–584. [Google Scholar] [CrossRef]
- Kowalska, A.; Manning, L. Using the rapid alert system for food and feed: Potential benefits and problems on data interpretation. Crit. Rev. Food Sci. Nutr. 2020, 61, 906–919. [Google Scholar] [CrossRef]
- Kowalska, A.; Bieniek, M.; Manning, L. Food supplements’ non-conformity in Europe—Poland: A case study. Trend. Food Sci. Technol. 2019, 93, 262–270. [Google Scholar] [CrossRef]
- Abramowicz, M.; Brosz, M.; Bykowska-Godlewska, B.; Michalski, T.; Strzałkowska, A. Wzorce Konsumpcji Alkoholu. Studium Socjologiczne; Wydawnictwo Zakładu Realizacji Badań Społecznych Q&Q: Kawle Dolne, Poland, 2018. [Google Scholar]
- Jankowiak, B.; Wojtynkiewicz, E. Kształtowanie się tożsamości w okresie adolescencji a podejmowanie zachowań ryzykownych w obszarze używania alkoholu przez młodzież. Stud. Edukacyjne 2018, 48, 169–185. [Google Scholar] [CrossRef]
- Shapira, B.; Schaefer, E.; Poperno, A.; Hess, Z.; Rosca, P.; Berkovitz, R. The methanol content of illicit alcoholic beverages seized in a low socio-economic area of Tel-Aviv: Public health impact and policy implications. J. Public Health 2018, 27, 37–42. [Google Scholar] [CrossRef]
- WHO (World Health Organization). Subregional Training for Leadership and Advocacy Teams to Reduce Alcohol Harm in Young People, Module 1, Da Nang, Viet Nam, 14–16 November 2017: Training Report; WHO Regional Office for the Western Pacific: Manila, Phillippines, 2017; Available online: https://iris.wpro.who.int/bitstream/handle/10665.1/13999/RS-2017-GE-64-VNM-eng.pdf (accessed on 15 April 2020).
- Holmes, J.; Meng, Y.; Meier, P.S.; Brennan, A.; Angus, C.; Campbell-Burton, A.; Guo, Y.; Hill-McManus, D.; Purshouse, R.C. Effects of minimum unit pricing for alcohol on different income and socioeconomic groups: A modelling study. Lancet 2014, 383, 1655–1664. [Google Scholar] [CrossRef]
- National Alcohol Strategy Advisory Committee. Social Reference Prices for Alcohol: A Tool for Canadian Governments to Promote a Culture of Moderation; Canadian Centre on Substance Abuse: Ottawa, ON, Canada, 2015; Available online: https://www.ccsa.ca/sites/default/files/2019-04/CCSA-Social-Reference-Prices-for-Alcohol-Canada-Report-2015-en.pdf (accessed on 15 October 2019).
- Knai, C.; Petticrew, M.; Durand, M.A.; Scott, C.; James, L.; Mehrotra, A.; Mays, N. The Public Health Responsibility deal: Has a public–private partnership brought about action on alcohol reduction? Addiction 2015, 110, 1217–1225. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, B.; Holden, C.; Eckhardt, J.; Lee, K. Reassessing policy paradigms: A comparison of the global tobacco and alcohol industries. Glob. Public Health 2016, 13, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Madureira-Lima, J.; Galea, S. Alcohol control policies and alcohol consumption: An international comparison of 167 countries. J. Epidemiology Community Health 2017, 72, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Al-Ansari, B.; Thow, A.-M.; Mirzaie, M.; Day, C.A.; Conigrave, K.M. Alcohol policy in Iran: Policy content analysis. Int. J. Drug Policy 2019, 73, 185–198. [Google Scholar] [CrossRef] [PubMed]
- Clough, A.R.; Margolis, S.A.; Miller, A.; Shakeshaft, A.; Doran, C.M.; McDermott, R.; Sanson-Fisher, R.; Towle, S.; Martin, D.; Ypinazar, V.; et al. Alcohol control policies in Indigenous communities: A qualitative study of the perceptions of their effectiveness among service providers, stakeholders and community leaders in Queensland (Australia). Int. J. Drug Policy 2016, 36, 67–75. [Google Scholar] [CrossRef] [PubMed]
- McCartney, G.; Bouttell, J.; Craig, N.; Craig, P.; Graham, L.; Lakha, F.; Lewsey, J.; McAdams, R.; MacPherson, M.; Minton, J.; et al. Explaining trends in alcohol-related harms in Scotland, 1991–2011 (I): The role of incomes, effects of socio-economic and political adversity and demographic change. Public Health 2016, 132, 13–23. [Google Scholar] [CrossRef]
- Ansoff, H.I.; McDonnell, E.J. Implanting Strategic Management, 2nd ed.; Prentice-Hall International: Cambridge, UK, 1990. [Google Scholar]
- Hauben, M.; Aronson, J.K. Defining ‘Signal’ and its Subtypes in Pharmacovigilance Based on a Systematic Review of Previous Definitions. Drug Saf. 2009, 32, 99–110. [Google Scholar] [CrossRef] [PubMed]
- Genc, E.; Duffie, N.; Reinhart, G. Event-based Supply Chain Early Warning System for an Adaptive Production Control. Procedia CIRP 2014, 19, 39–44. [Google Scholar] [CrossRef]
- Puranam, P.; Powell, B.C.; Singh, H. Due diligence failure as a signal detection problem. Strat. Organ. 2006, 4, 319–348. [Google Scholar] [CrossRef]
- European Medicines Agency. Guideline on Good Pharmacovigilance Practices (GVP) Module IX—Signal Management (Rev 1). Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-good-pharmacovigilance-practices-gvp-module-ix-signal-management-rev-1_en.pdf (accessed on 10 June 2021).
- Gottschalk, P.; Gunnesdal, L. White-Collar Crime Detection. In White-Collar Crime in the Shadow Economy; Palgrave Pivot: Chamdem, UK, 2018; pp. 111–134. [Google Scholar]
- WHO (World Health Organization). The Technical Package SAFER. A World Free from Alcohol Related Harms; WHO: Geneva, Switzerland, 2019; Available online: https://www.who.int/publications/i/item/the-safer-technical-package (accessed on 28 June 2021).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).