Test–Retest Reliability of Task-Oriented Strength and Object Position in a Box Lifting Task Using the Activities of Daily Living Test and Training Device (ADL-TTD) in Children with Unilateral Spastic Cerebral Palsy
Abstract
1. Introduction
2. Methods
2.1. Design
2.1.1. Inclusion Criteria
- Age between 7 and 18 years.
- Diagnosed with USCP by a pediatric neurologist.
- Gross Motor Function Classification System (GMFCS) level I–III [16].
- Manual Ability Classification System (MACS) level I–III [17].
- Manual function limitation classified as Zancolli degree I–IIb [18].
- Able to understand the test instructions and all attended regular primary or secondary school.
- Dutch speaking.
2.1.2. Exclusion Criteria
- Botulinum Toxin-A injections in one or both upper extremities within the past three months.
- UE surgery within the past six months.
2.1.3. Sample Size
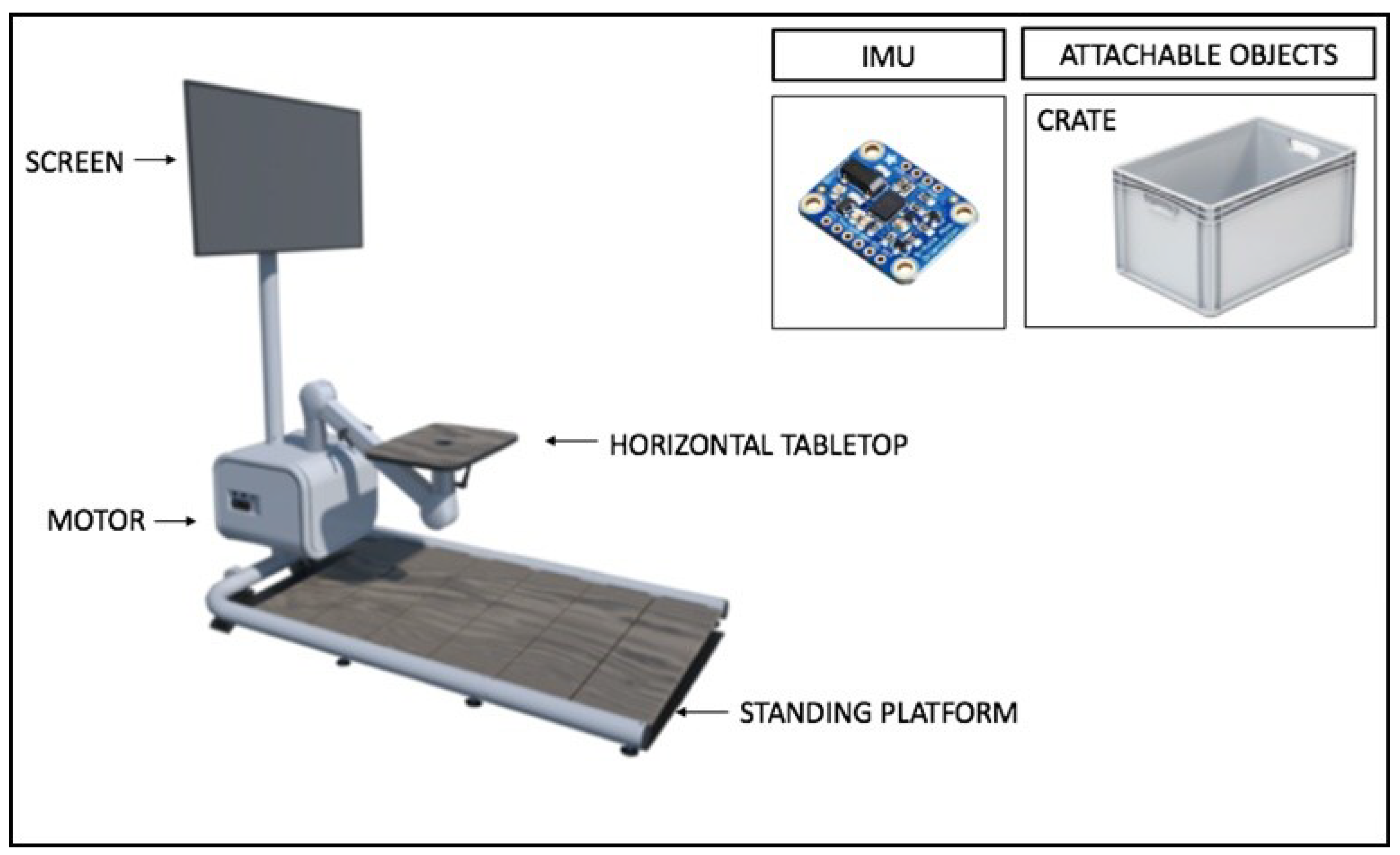
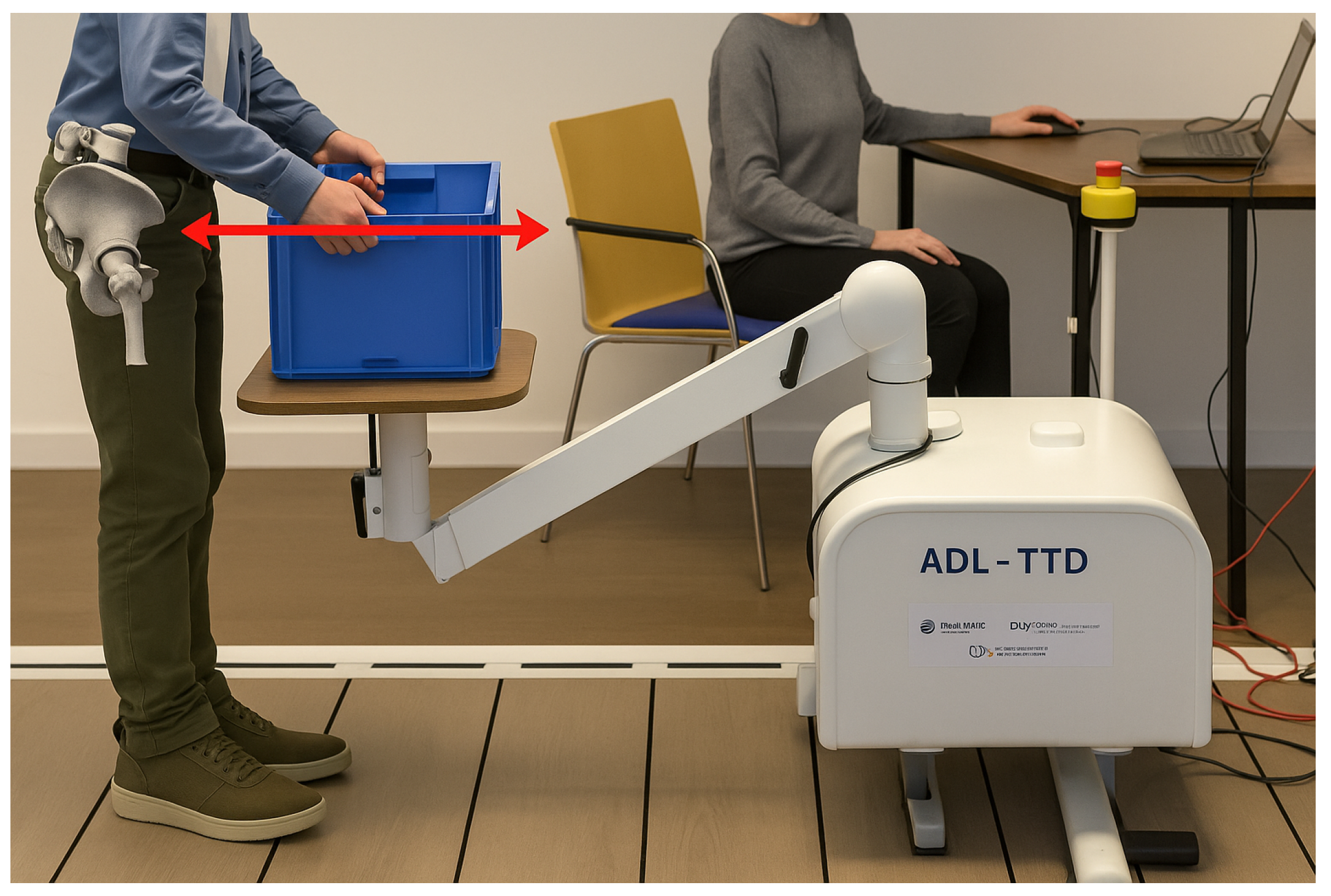
2.2. Devices
2.3. Measurement Procedure
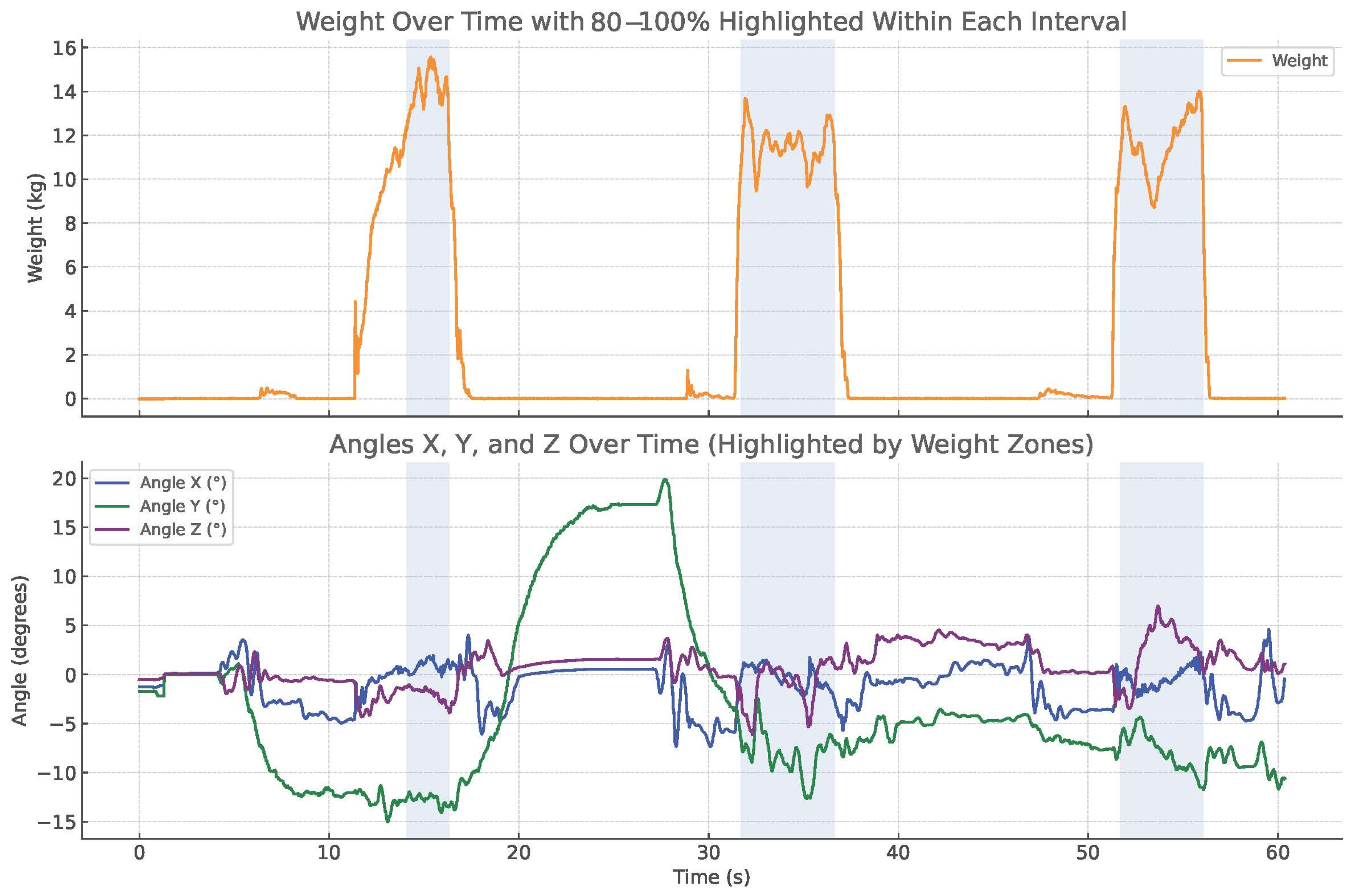
2.4. Procedure for Scoring the Outcome
2.5. Statistical Analysis
2.5.1. Descriptive Statistics of the Population
2.5.2. ICC and SEM
2.5.3. Absolute Agreement with Bland–Altman Plot
3. Results
Descriptives
4. Discussion
4.1. Reliability in MVC
4.2. Reliability in Object Position
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| USCP | Unilateral Spastic Cerebral Palsy |
| MVC | Maximum Voluntary Contraction |
| ICC | Intraclass Correlation Coefficient |
| CI | Confidence Interval |
| SEM | Standard Error of Measurement |
| ADL | Activity of Daily Living |
| IMU | Inertial Measurement Units |
| LOA | Limits of Agreement |
| AH | Affected Hand |
| NAH | Non-Affected Hand |
| ADL-TTD | Activity of Daily Living Testing and Training Device |
| TAAC | Task-oriented Arm–Hand Capacity |
| COSMIN | COnsensus-based Standards for the Selection of Health Measurement INstruments |
| SD | Standard Deviation |
| MACS | Manual Ability Classification System |
| GMFCS | Gross Motor Function Classification System |
| HHD | Hand-Held Dynamometry |
| MDC | Minimal Detectable Change |
| UE | Upper Extremity |
Appendix A
| Specification | Value |
|---|---|
| Dimensions (L × W × H) | 180 × 100 × 80 cm |
| Height adjustment range | 60–120 cm (height of tabletop) |
| Weight of device | 75 kg |
| Accuracy of lifting (height) | ±2 mm |
| Accuracy of lifting (weight) | To lift 5 kg: ±10 g From 5 kg to 40 kg: ±0.5% |
| Maximum lifting height from tabletop | 70 cm |
| Maximum lifting weight | 40 kg |
| Power supply | 240 V, 50/60 Hz |
| Measurement | Specifications |
|---|---|
| Absolute Orientation (Euler) | → Euler Vector, 100 Hz Three-axis orientation data based on a 360° sphere |
| Absolute Orientation (Quaternion) | → Quaternion, 100 Hz Four-point quaternion output for more accurate data manipulation |
| Angular Velocity Vector | → 100 Hz Three-axis rotation speed in rad/s |
| Acceleration Vector | → 100 Hz Three-axis acceleration (gravity + linear motion) in m/s2 |
| Magnetic Field Strength Vector | → 20 Hz Three-axis magnetic field sensing in microteslas (μT) |
| Linear Acceleration Vector | → 100 Hz Three-axis linear acceleration data (acceleration minus gravity) in m/s2 |
| Gravity Vector | → 100 Hz Three-axis gravitational acceleration (minus any movement) in m/s2 |
| Temperature | → 1 Hz Ambient temperature in degrees Celsius |
References
- Pakula, A.T.; Braun, K.V.N.; Yeargin-Allsopp, M. Cerebral palsy: Classification and epidemiology. Phys. Med. Rehabil. Clin. 2009, 20, 425–452. [Google Scholar] [CrossRef]
- Gordon, A.M.; Bleyenheuft, Y.; Steenbergen, B. Pathophysiology of impaired hand function in children with unilateral cerebral palsy. Dev. Med. Child Neurol. 2013, 55, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Gordon, A.M. Impaired voluntary movement control and its rehabilitation in cerebral palsy. In Progress in Motor Control Theories and Translations; Springer: Cham, Switzerland, 2016; pp. 291–311. [Google Scholar] [CrossRef]
- Gutterman, J.; Lee-Miller, T.; Friel, K.M.; Dimitropoulou, K.; Gordon, A.M. Anticipatory motor planning and control of grasp in children with unilateral spastic cerebral palsy. Brain Sci. 2021, 11, 1161. [Google Scholar] [CrossRef] [PubMed]
- Chin, T.Y.; Duncan, J.A.; Johnstone, B.R.; Graham, H.K. Management of the upper limb in cerebral palsy. J. Pediatr. Orthop. B 2005, 14, 389–404. [Google Scholar] [CrossRef]
- Sakzewski, L.; Ziviani, J.; Boyd, R. The relationship between unimanual capacity and bimanual performance in children with congenital hemiplegia. Dev. Med. Child Neurol. 2010, 52, 811–816. [Google Scholar] [CrossRef]
- Dekkers, K.; Janssen-Potten, Y.; Gordon, A.M.; Speth, L.; Smeets, R.; Rameckers, E. Reliability of maximum isometric arm, grip and pinch strength measurements in children (7–12 years) with unilateral spastic cerebral palsy. Disabil. Rehabil. 2020, 42, 1448–1453. [Google Scholar] [CrossRef]
- Jackman, M.; Sakzewski, L.; Morgan, C.; Boyd, R.N.; Brennan, S.E.; Langdon, K.; Toovey, R.A.; Greaves, S.; Thorley, M.; Novak, I. Interventions to improve physical function for children and young people with cerebral palsy: International clinical practice guideline. Dev. Med. Child Neurol. 2022, 64, 536–549. [Google Scholar] [CrossRef]
- Dekkers, K.J.; Rameckers, E.A.; Smeets, R.J.; Gordon, A.M.; Speth, L.A.; Ferre, C.L.; Janssen-Potten, Y.J. Upper extremity muscle strength in children with unilateral spastic cerebral palsy: A bilateral problem? Phys. Ther. 2020, 100, 2205–2216. [Google Scholar] [CrossRef]
- Geijen, M.; Rameckers, E.; Schnackers, M.; Bastiaenen, C.; Gordon, A.; Speth, L.; Smeets, R. Reproducibility of task-oriented bimanual and unimanual strength measurement in children with unilateral cerebral palsy. Phys. Occup. Ther. Pediatr. 2019, 39, 420–432. [Google Scholar] [CrossRef] [PubMed]
- Klingels, K.; Demeyere, I.; Jaspers, E.; De Cock, P.; Molenaers, G.; Boyd, R.; Feys, H. Upper limb impairments and their impact on activity measures in children with unilateral cerebral palsy. Eur. J. Paediatr. Neurol. 2012, 16, 475–484. [Google Scholar] [CrossRef]
- Berger, M. Geometry I; Springer Science & Business Media: Berlin, Germany, 2009. [Google Scholar]
- Ahmad, N.; Ghazilla, R.A.R.; Khairi, N.M.; Kasi, V. Reviews on various inertial measurement unit (IMU) sensor applications. Int. J. Signal Process. Syst. 2013, 1, 256–262. [Google Scholar] [CrossRef]
- Guo, H.; Heus, I.; Smeets, R.J.E.M.; Rameckers, E.A.A. The Technology Used in Assessment or Training of Task-Specific Strength in the Upper Extremity: A Scoping Review. EC Paediatr. 2023, 12, 1–22. [Google Scholar]
- Terwee, C.B.; Mokkink, L.B.; Knol, D.L.; Ostelo, R.W.; Bouter, L.M.; de Vet, H.C. Rating the methodological quality in systematic reviews of studies on measurement properties: A scoring system for the COSMIN checklist. Qual. Life Res. 2012, 21, 651–657. [Google Scholar] [CrossRef] [PubMed]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef]
- Eliasson, A.C.; Krumlinde-Sundholm, L.; Rösblad, B.; Beckung, E.; Arner, M.; Öhrvall, A.M.; Rosenbaum, P. The Manual Ability Classification System (MACS) for children with cerebral palsy: Scale development and evidence of validity and reliability. Dev. Med. Child Neurol. 2006, 48, 549–554. [Google Scholar] [CrossRef] [PubMed]
- Zancolli, E.A.; Goldner, L.J.; Swanson, A.B. Surgery of the spastic hand in cerebral palsy: Report of the Committee on Spastic Hand Evaluation. J. Hand Surg. 1983, 8, 766–772. [Google Scholar] [CrossRef]
- Morin, M.; Hébert, L.J.; Perron, M.; Petitclerc, É.; Lake, S.R.; Duchesne, E. Psychometric properties of a standardized protocol of muscle strength assessment by hand-held dynamometry in healthy adults: A reliability study. BMC Musculoskelet. Disord. 2023, 24, 294. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Gajdosik, C.G. Ability of very young children to produce reliable isometric force measurements. Pediatr. Phys. Ther. 2005, 17, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Schreuders, T.; Roebroeck, M.; Van Der Kar, T.J.; Soeters, J.; Hovius, S.; Stam, H. Strength of the intrinsic muscles of the hand measured with a hand-held dynamometer: Reliability in patients with ulnar and median nerve paralysis. J. Hand Surg. Br. Eur. Vol. 2000, 25, 560–565. [Google Scholar] [CrossRef]
- Hansen, C.; Ortlieb, C.; Romijnders, R.; Warmerdam, E.; Welzel, J.; Geritz, J.; Maetzler, W. Reliability of IMU-derived temporal gait parameters in neurological diseases. Sensors 2022, 22, 2304. [Google Scholar] [CrossRef] [PubMed]
- Kaszyński, J.; Baka, C.; Białecka, M.; Lubiatowski, P. Shoulder range of motion measurement using inertial measurement unit–concurrent validity and reliability. Sensors 2023, 23, 7499. [Google Scholar] [CrossRef]
- Kim, H.; Shin, S.H.; Kim, J.K.; Park, Y.J.; Oh, H.S.; Park, Y.B. Cervical coupling motion characteristics in healthy people using a wireless inertial measurement unit. Evid.-Based Complement. Altern. Med. 2013, 2013, 570428. [Google Scholar] [CrossRef] [PubMed]
- Lemay, J.F.; Noamani, A.; Unger, J.; Houston, D.J.; Rouhani, H.; Musselmann, K.E. Using wearable sensors to characterize gait after spinal cord injury: Evaluation of test–retest reliability and construct validity. Spinal Cord 2021, 59, 675–683. [Google Scholar] [CrossRef]
- Rattanakoch, J.; Samala, M.; Limroongreungrat, W.; Guerra, G.; Tharawadeepimuk, K.; Nanbancha, A.; Niamsang, W.; Kerdsomnuek, P.; Suwanmana, S. Validity and reliability of inertial measurement unit (IMU)-derived 3D joint kinematics in persons wearing transtibial prosthesis. Sensors 2023, 23, 1738. [Google Scholar] [CrossRef]
- Antunes, R.; Jacob, P.; Meyer, A.; Conditt, M.A.; Roche, M.W.; Verstraete, M.A. Accuracy of measuring knee flexion after TKA through wearable IMU sensors. J. Funct. Morphol. Kinesiol. 2021, 6, 60. [Google Scholar] [CrossRef]
- Held, J.P.; Klaassen, B.; Eenhoorn, A.; Beijnum, B.J.F.v.; Buurke, J.H.; Veltink, P.H.; Luft, A.R. Inertial sensor measurements of upper-limb kinematics in stroke patients in clinic and home environment. Front. Bioeng. Biotechnol. 2018, 6, 27. [Google Scholar] [CrossRef] [PubMed]
- De Vet, H.C.; Terwee, C.B.; Mokkink, L.B.; Knol, D.L. Measurement in Medicine: A Practical Guide; Cambridge University Press: Cambridge, UK, 2011. [Google Scholar]



| Characteristic | Value | ||
|---|---|---|---|
| Sex (Male/Female) | 20 (46.5%) | 23 (53.5%) | |
| Mean Age (SD) | 12.5 (2.4) | ||
| Affected Hand (Right/Left) | 27 (62%) | 16 (38%) | |
| GMFCS Level (I/II) | 37 (86%) | 6 (14%) | |
| MACS Level (I/II/III) | 12 (28%) | 26 (60%) | 5 (12%) |
| Zancolli Grade (1/2a/2b) | 26 (60%) | 14 (33%) | 3 (7%) |
| Parameters | Mean T0 | Mean T1 | Absolute Difference (SD) |
|---|---|---|---|
| MVC (kg) | 10.58 | 9.93 | 0.65 (2.67) |
| Posterior tilt (°) | 7.17 | 6.40 | 0.77 (3.47) |
| NAH forward rotation (°) | 5.04 | 5.25 | 3.05 (4.76) |
| AH downward tilt (°) | 4.30 | 3.69 | 1.81 (0.27) |
| Parameter | ICCagreement | 95% CI | SEMagreement | SEM% | MDC95 |
|---|---|---|---|---|---|
| MVC (kg) | 0.95 | 0.91 to 0.97 | 5.94 kg | 57.9% | 16.45 kg |
| Posterior tilt (°) | 0.82 | 0.67 to 0.90 | 0.71 | 9.9% | 1.99° |
| NAH forward rotation (°) | 0.83 | 0.69 to 0.91 | 5.39 | 104.3% | 14.91° |
| AH downward tilt (°) | 0.86 | 0.75 to 0.91 | 3.43 | 79.8% | 9.41° |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guo, H.; Heus, I.; Snijders, B.; Land, N.E.; van der Holst, M.; Smeets, R.J.E.M.; Bastiaenen, C.H.G.; Rameckers, E.A.A. Test–Retest Reliability of Task-Oriented Strength and Object Position in a Box Lifting Task Using the Activities of Daily Living Test and Training Device (ADL-TTD) in Children with Unilateral Spastic Cerebral Palsy. Children 2025, 12, 1030. https://doi.org/10.3390/children12081030
Guo H, Heus I, Snijders B, Land NE, van der Holst M, Smeets RJEM, Bastiaenen CHG, Rameckers EAA. Test–Retest Reliability of Task-Oriented Strength and Object Position in a Box Lifting Task Using the Activities of Daily Living Test and Training Device (ADL-TTD) in Children with Unilateral Spastic Cerebral Palsy. Children. 2025; 12(8):1030. https://doi.org/10.3390/children12081030
Chicago/Turabian StyleGuo, Haowei, Inge Heus, Bart Snijders, Nanne E. Land, Menno van der Holst, Rob. J. E. M. Smeets, Caroline H. G. Bastiaenen, and Eugene A. A. Rameckers. 2025. "Test–Retest Reliability of Task-Oriented Strength and Object Position in a Box Lifting Task Using the Activities of Daily Living Test and Training Device (ADL-TTD) in Children with Unilateral Spastic Cerebral Palsy" Children 12, no. 8: 1030. https://doi.org/10.3390/children12081030
APA StyleGuo, H., Heus, I., Snijders, B., Land, N. E., van der Holst, M., Smeets, R. J. E. M., Bastiaenen, C. H. G., & Rameckers, E. A. A. (2025). Test–Retest Reliability of Task-Oriented Strength and Object Position in a Box Lifting Task Using the Activities of Daily Living Test and Training Device (ADL-TTD) in Children with Unilateral Spastic Cerebral Palsy. Children, 12(8), 1030. https://doi.org/10.3390/children12081030






