Pediatric Medial Discoid Meniscus: Case Series and Postoperative Outcomes
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Outcome Measures
3. Results
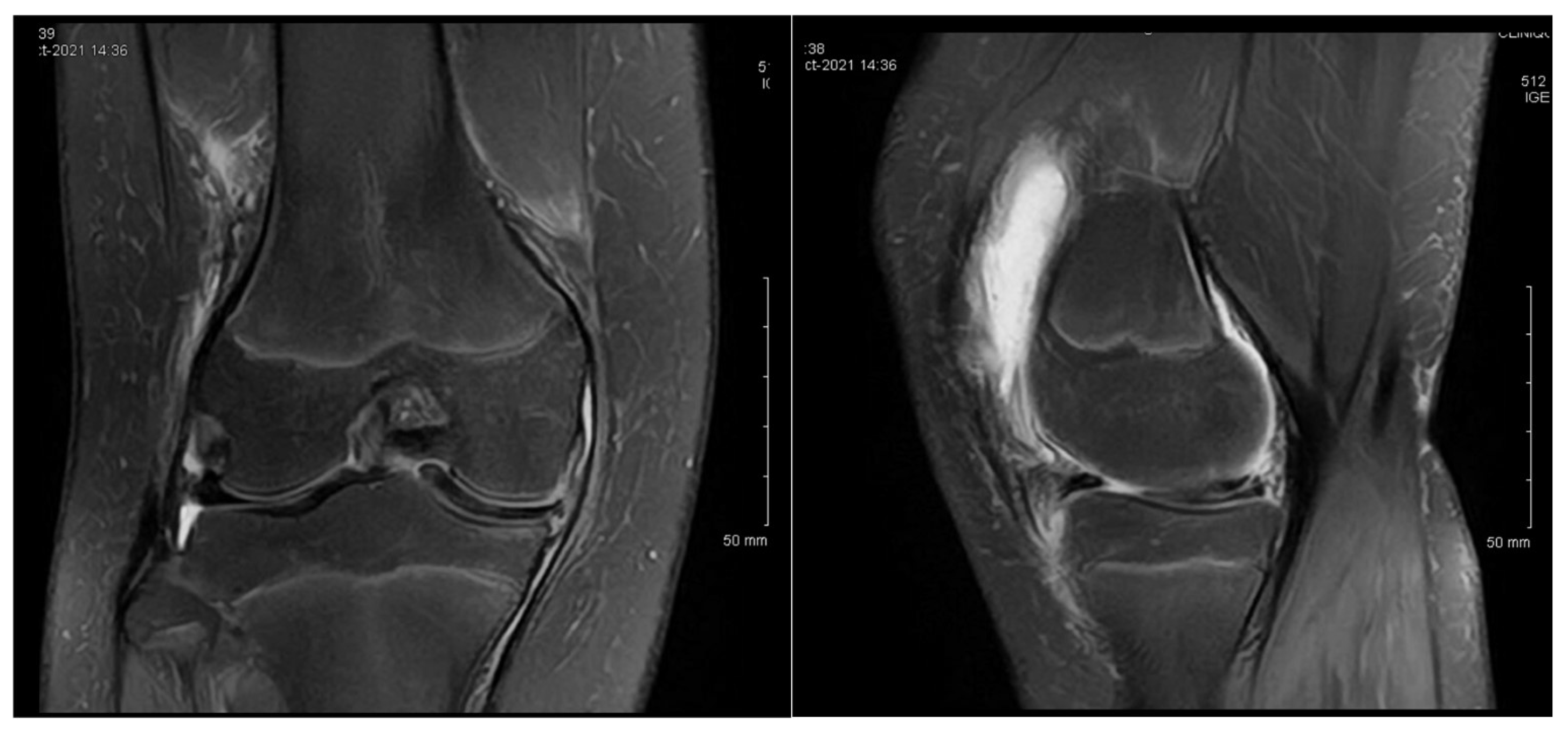
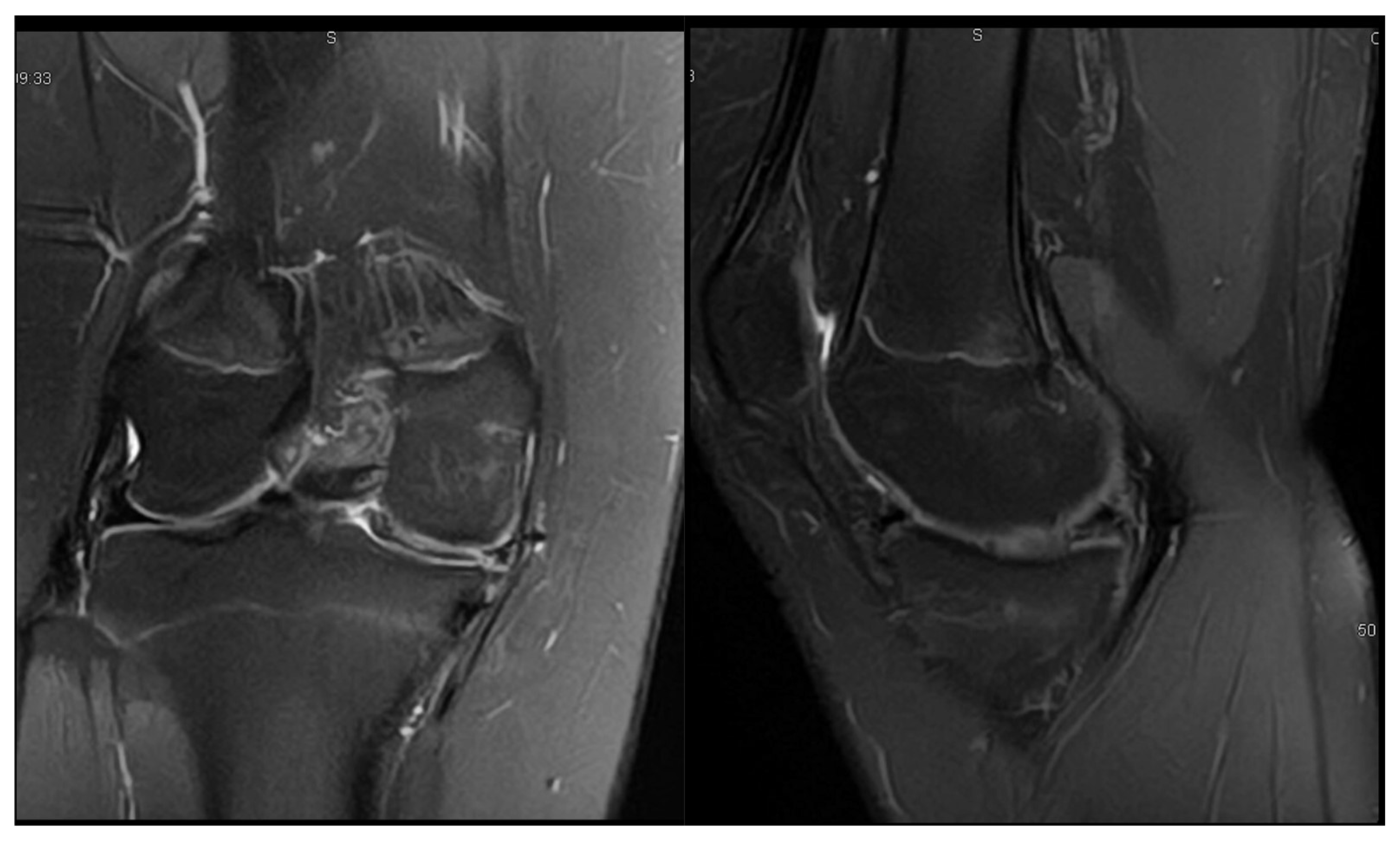
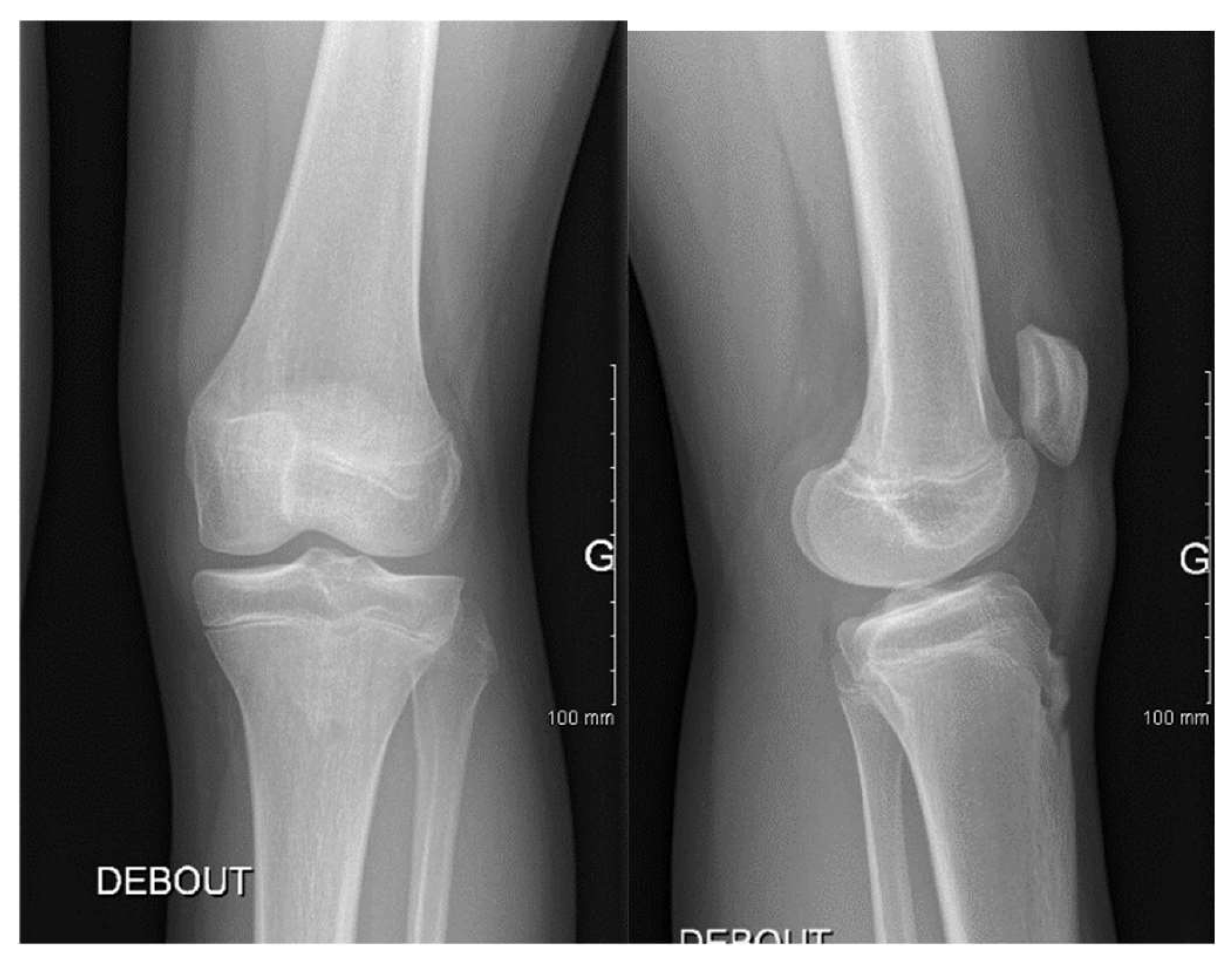
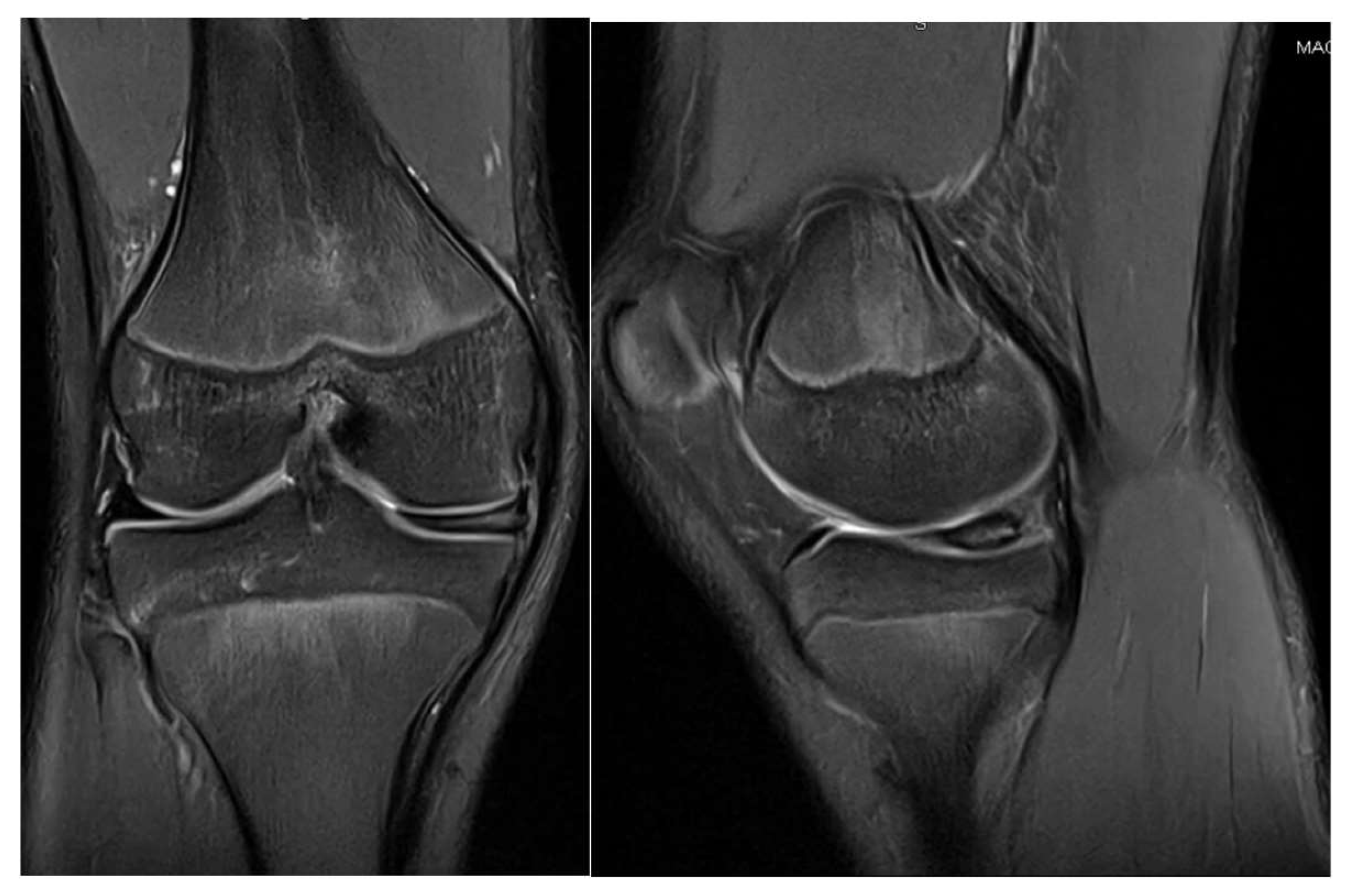
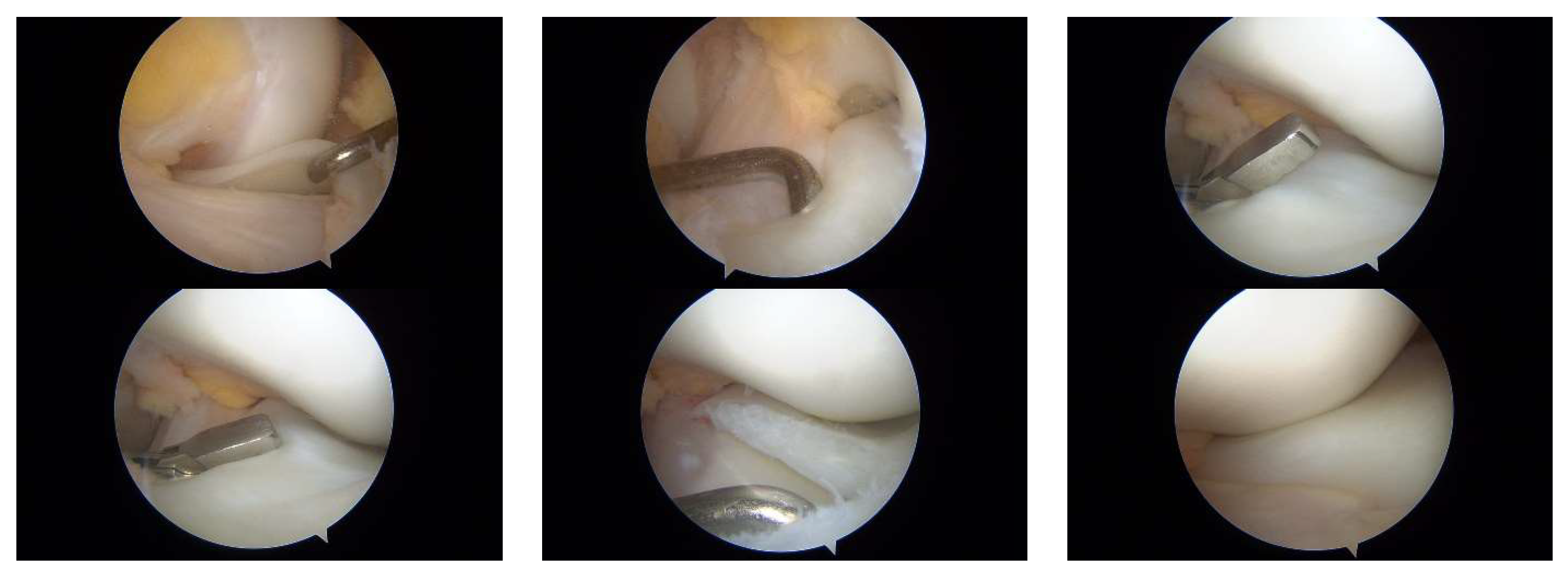
3.1. Case 1—P.E.
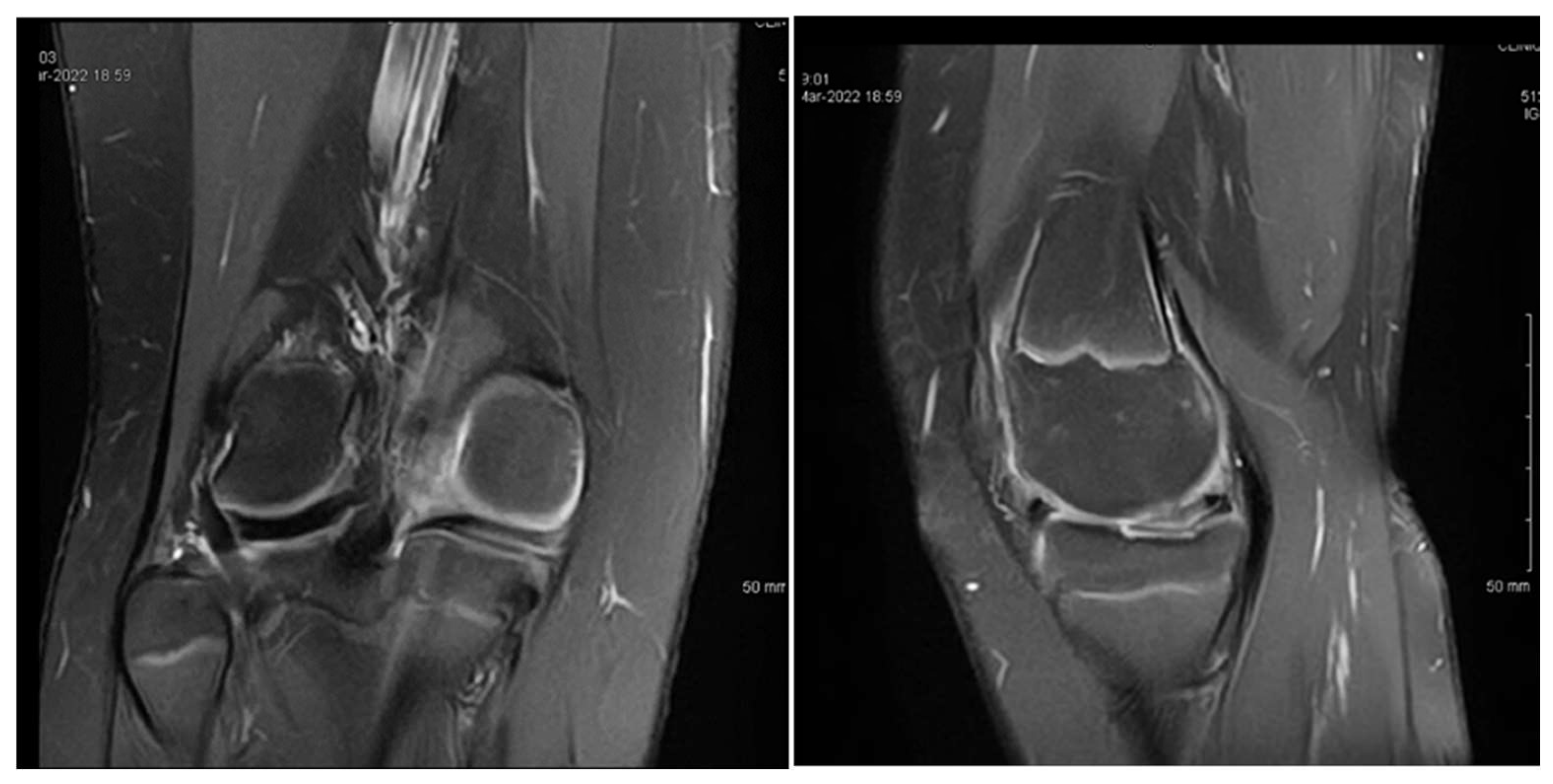
3.2. Case 2—S.C.S.
3.3. Case 3—G.L.
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ikeuchi, H. Arthroscopic treatment of discoid lateral meniscus. Technique and long-term results. Clin. Orthop. Relat. Res. 1982, 167, 19–28. [Google Scholar] [CrossRef]
- Dickason, J.M.; Del Pizzo, W.; Blazina, M.E.; Fox, J.M.; Friedman, M.J.; Snyder, S.J. A series of ten discoid medial menisci. Clin. Orthop. Relat. Res. 1982, 168, 75–79. [Google Scholar] [CrossRef]
- Niu, E.L.; Lee, R.J.; Joughin, E.; Finlayson, C.J.; Heyworth, B.E. Discoid Meniscus. Clin. Sports Med. 2022, 41, 729–747. [Google Scholar] [CrossRef] [PubMed]
- Tapasvi, S.; Shekhar, A.; Eriksson, K. Discoid lateral meniscus: Current concepts. J. ISAKOS 2021, 6, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Saavedra, M.; Sepúlveda, M.; Jesús Tuca, M.; Birrer, E. Discoid meniscus: Current concepts. EFORT Open Rev. 2020, 5, 371–379. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Albishi, W.; Albaroudi, A.; Alaseem, A.M.; Aljasser, S.; Alshaygy, I.; Addar, A. Discoid meniscus: Treatment considerations and updates. World J. Orthop. 2024, 15, 520–528. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Turati, M.; Anghilieri, F.M.; Accadbled, F.; Piatti, M.; Di Benedetto, P.; Moltrasio, F.; Zatti, G.; Zanchi, N.; Bigoni, M. Discoid meniscus in human fetuses: A systematic review. Knee 2021, 30, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Aydın Kabakçı, A.D.; Büyükmumcu, M.; Akın, D.; Bilge, O. Morphological structure and variations of fetal lateral meniscus: The significance in convenient diagnosis and treatment. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3364–3373. [Google Scholar] [CrossRef]
- Yang, S.; Zhang, S.; Li, R.; Yang, C.; Zheng, J.; Wang, C.; Lu, J.; Zhang, Z.; Shang, X.; Zhang, H.; et al. Chinese Experts Consensus and Practice Guideline on Discoid Lateral Meniscus. Orthop. Surg. 2023, 15, 915–929. [Google Scholar] [CrossRef]
- Kim, J.H.; Ahn, J.H.; Kim, J.H.; Wang, J.H. Discoid lateral meniscus: Importance, diagnosis, and treatment. J. Exp. Orthop. 2020, 7, 81. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hampton, M.; Hancock, G.; Christou, A.; Ali, F.; Nicolaou, N. Clinical presentation, MRI and clinical outcome scores do not accurately predict an important meniscal tear in a symptomatic discoid meniscus. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 3133–3138. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.L.; Pace, J.L.; Mandelbaum, B.R. Discoid Lateral Meniscus. Curr. Rev. Musculoskelet Med. 2023, 16, 154–161. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Young, R.B. The external semilunar cartilage as a complete disc. In Memoirs and Memoranda in Anatomy; Cleland, J., MacKay, J.Y., Young, R.B., Eds.; Williams and Norgate: London, UK, 1889; Volume 1, p. 179. [Google Scholar]
- Cave, E.F.; Staples, O.S. Congenital discoid meniscus: A cause of internal derangement of the knee. Am. J. Surg. 1941, 54, 371–376. [Google Scholar] [CrossRef]
- Sevillano-Perez, E.; Espejo-Reina, A.; Espejo-Reina, M.J. Symptomatic Bilateral Torn Discoid Medial Meniscus Treated with Saucerization and Suture. Case Rep. Orthop. 2016, 2016, 8487194. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kini, S.G.; Walker, P.; Bruce, W. Bilateral symptomatic discoid medial meniscus of the knee-case report and review of literature. Arch. Trauma Res. 2015, 4, e27115. [Google Scholar] [CrossRef]
- Yang, X.; Shao, D. Bilateral discoid medial Meniscus: Two case reports. Medicine 2019, 98, e15182. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rodríguez-Rodríguez, I.F.; Navarro-Torres-Arpi, P.; Dryjanski-Lerner, A.; Gómez-Mont-Landerreche, J.G.; Levy-Holden, G.A.; Gil-Orbezo, F. Menisco discoide medial en paciente pediátrico. Presentación de un caso y revisión de la literatura [Medial discoid meniscus in a pediatric patient. Case report and review of the literature]. Acta Ortop. Mex. 2024, 38, 52–56. (In Spanish) [Google Scholar] [CrossRef] [PubMed]
- Flouzat-Lachaniette, C.H.; Pujol, N.; Boisrenoult, P.; Beaufils, P. Discoid medial meniscus: Report of four cases and literature review. Orthop. Traumatol. Surg. Res. 2011, 97, 826–832. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chen, L.X.; Ao, Y.F.; Yu, J.K.; Miao, Y.; Leung, K.K.M.; Wang, H.J.; Lin, L. Clinical features and prognosis of discoid medial meniscus. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 398–402. [Google Scholar] [CrossRef]
- Tachibana, Y.; Yamazaki, Y.; Ninomiya, S. Discoid medial meniscus. Arthroscopy 2003, 19, e59–e65. [Google Scholar] [CrossRef] [PubMed]
- Yaniv, M.; Blumberg, N. The discoid meniscus. J. Child. Orthop. 2007, 1, 89–96. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, S.J.; Seo, Y.J. Bilateral discoid medial menisci: Incomplete type in one knee and complete type in opposite knee. Knee 2006, 13, 255–257. [Google Scholar] [CrossRef] [PubMed]
- Feroe, A.G.; Hussain, Z.B.; Stupay, K.L.; Kocher, S.D.; Williams, K.A.; Micheli, L.J.; Kocher, M.S. Surgical Management of Medial Discoid Meniscus in Pediatric and Adolescent Patients. J. Pediatr. Orthop. 2021, 41, e804–e809. [Google Scholar] [CrossRef] [PubMed]
- Desai, B.; Warren, M.; Lavie, L.G.; Nammour, M.; Waldron, S. Arthroscopic Saucerization of a Symptomatic Posterior Horn Tear in a Discoid Medial Meniscus. Ochsner J. 2021, 21, 115–118. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al Saedi, Z.S.; Alzubaidi, B.K.; Mirza, H.A.; Alhothali, M.K.; Alhijjy, M.M.; Mirza, A.A. Medial Discoid Meniscus: A Rare Case Report. Cureus 2023, 15, e39971. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Herdea, A.; Struta, A.; Derihaci, R.P.; Ulici, A.; Costache, A.; Furtunescu, F.; Toma, A.; Charkaoui, A. Efficiency of platelet-rich plasma therapy for healing sports injuries in young athletes. Exp. Ther. Med. 2022, 23, 215. [Google Scholar] [CrossRef]
- Farlett, J.; Wood, J.R. Ipsilateral Medial and Lateral Discoid Menisci: A Rare Combination of Infrequent Anatomic Variants. J. Clin. Imaging Sci. 2020, 10, 11. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lukas, K.; Livock, H.; Kontio, K.; Carsen, S. Bilateral Discoid Medial Menisci: A Case Report and Review of the Literature. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2020, 4, e20.00069. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]



| Patient | Age at Diagnosis | Knee(s) Involved | Initial Symptoms | Sports Activity | Surgical History | Follow-Up Outcome |
|---|---|---|---|---|---|---|
| P.E. | 12 | Bilateral (symptomatic right) | Chronic pain, effusion, normal ROM | None | 3 surgeries: partial meniscectomy (12 years), suture for horizontal tear (13 years), suture for radial tear (14 years) | 1 year after third surgery: symptom-free, resumed school sports |
| S.C.S. | 13 | Left | Pain, occasional locking, normal ROM | Dancing | 1 surgery: partial meniscectomy and suture for horizontal tear (13) | 6 months: symptom-free, full ROM, resumed dancing |
| G.L. | 14 | Bilateral (symptomatic right) | Pain, medial tenderness, normal ROM | Basketball | 1 surgery: partial meniscectomy and suture for horizontal tear (14) | 6 months: symptom-free, full ROM |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Accadbled, F.; Sygacz, O.; Rassi, J.; Herdea, A. Pediatric Medial Discoid Meniscus: Case Series and Postoperative Outcomes. Children 2025, 12, 646. https://doi.org/10.3390/children12050646
Accadbled F, Sygacz O, Rassi J, Herdea A. Pediatric Medial Discoid Meniscus: Case Series and Postoperative Outcomes. Children. 2025; 12(5):646. https://doi.org/10.3390/children12050646
Chicago/Turabian StyleAccadbled, Franck, Oliwer Sygacz, Joe Rassi, and Alexandru Herdea. 2025. "Pediatric Medial Discoid Meniscus: Case Series and Postoperative Outcomes" Children 12, no. 5: 646. https://doi.org/10.3390/children12050646
APA StyleAccadbled, F., Sygacz, O., Rassi, J., & Herdea, A. (2025). Pediatric Medial Discoid Meniscus: Case Series and Postoperative Outcomes. Children, 12(5), 646. https://doi.org/10.3390/children12050646






