The Edmonton Obesity Staging System for Pediatrics (EOSS-P) in Mexican Children and Adolescents Living with Obesity: Beyond BMI Obesity Classes
Highlights
- What are the main findings?
- •
- More than half of the children were classified in stage 3, the most severe stage of the EOSS-P.
- •
- There is a weak association between EOSS-P staging and BMI-based obesity classification in children.
- What is the implication of the main finding?
- •
- The assessment of obesity in children should go beyond BMI and include metabolic, mechanical, mental, and social domains
- •
- The EOSS-P is a valuable tool for the comprehensive assessment of obesity that could be adapted to different contexts.
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Obesity Diagnosis
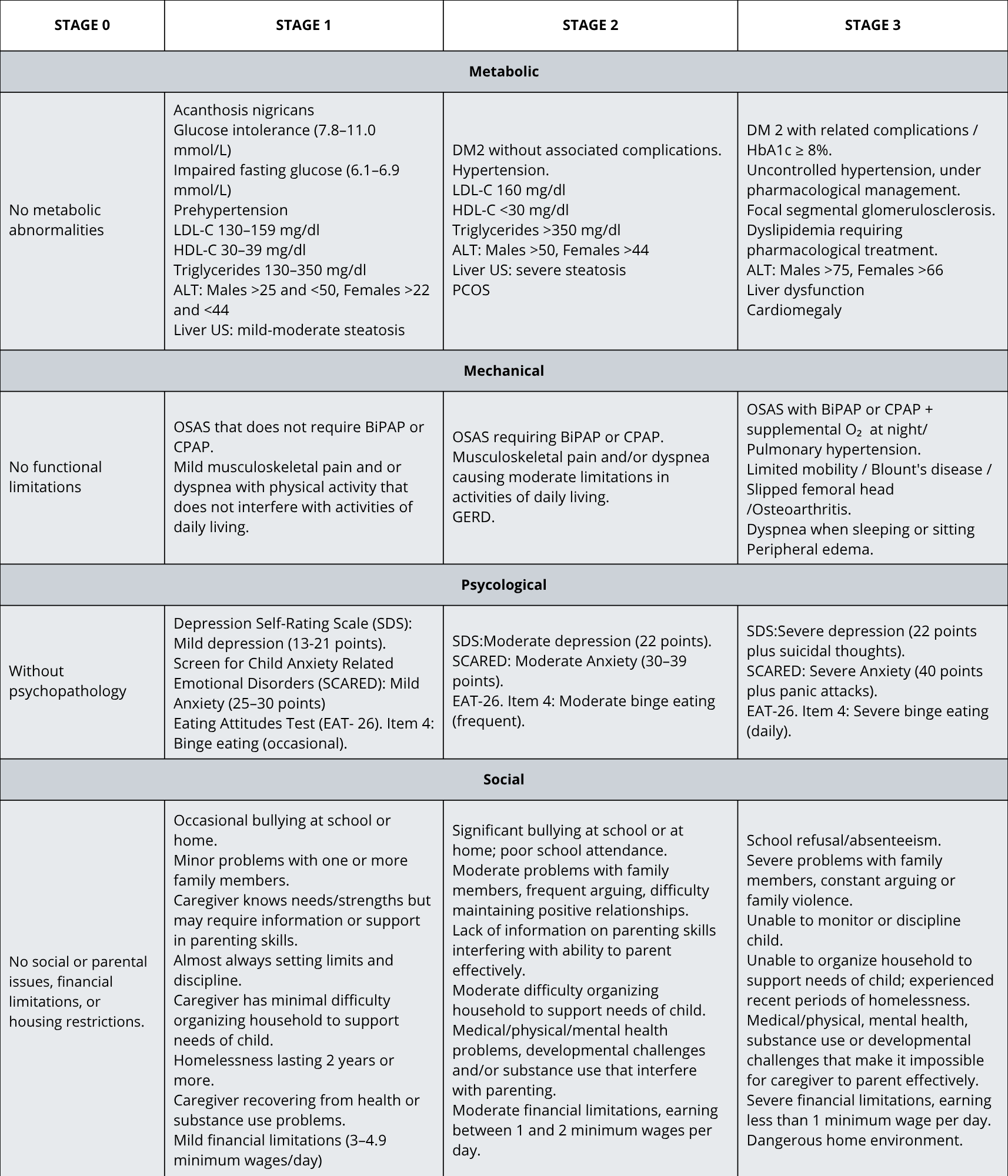
2.3. EOSS-P
- -
- Acanthosis nigricans. A pediatrician determined the presence of acanthosis on the neck, armpits, and groin and used the classification proposed by Burke and cols [21].
- -
- Blood pressure (BP). BP was measured in a sitting position, after a 5 min rest, and with an arm support so that the antecubital fossa was at the level of the heart. The sphygmomanometer was long enough to cover 80–100% of the arm circumference at the midpoint between the olecranon and the acromion and had a width equivalent to 2/3 of the circumference. Two measurements were taken during the consultation, and the average of these was obtained. To identify the presence of prehypertension or hypertension, BP was classified according to percentiles [22].
- -
- Biochemical data. Fasting serum concentrations of glucose, insulin, total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, and alanine aminotransferase (ALT) were determined by standardized methods. When fasting glucose was >100 mg/dL, an oral glucose tolerance test was performed to identify Type 2 diabetes mellitus or prediabetes.
- -
- Liver steatosis. Liver ultrasound was requested for all patients.
- -
- Polycystic Ovary Syndrome (PCOS). PCOS was diagnosed in females according to the Rotterdam criteria [23], requiring the presence of at least two of the following: clinical or biochemical hyperandrogenism, oligo/anovulation, or polycystic ovarian morphology on ultrasound. Hirsutism was assessed using the Ferriman–Gallwey scoring system for women [24], which evaluates nine androgen-sensitive body areas, each scored from 0 to 4. A total score of ≥8 was considered indicative of generalized hirsutism.
- -
- Depression Self-Rating Scale. This scale evaluates moderate to severe depression in childhood. The total score of the scale was classified as follows: (1) without psychopathology: 0–12 points; (2) mild depression: 13–21 points; (3) moderate depression: 22 points; (4) severe depression: 22 points plus suicidal thoughts. These cut-off points were proposed in a study conducted among Peruvian children to validate a modified version of the Depression Self-Rating Scale [30].
- -
- Screen for Child Anxiety Related Emotional Disorders (SCARED). This self-report instrument was developed to screen anxiety disorders in children [28]. The total score was categorized as follows: without psychopathology (0–24 points), mild anxiety (25–30 points), moderate anxiety (30–39 points), and severe anxiety (40 points plus panic attacks).
- -
- Eating Attitudes Test (EAT-26). EAT-26 is a standardized self-report tool to measure symptoms and characteristics of eating disorders [29]. To evaluate the presence and frequency of binge, we considered item four of this scale (Have gone on eating binges where I felt that I may not be able to stop).
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
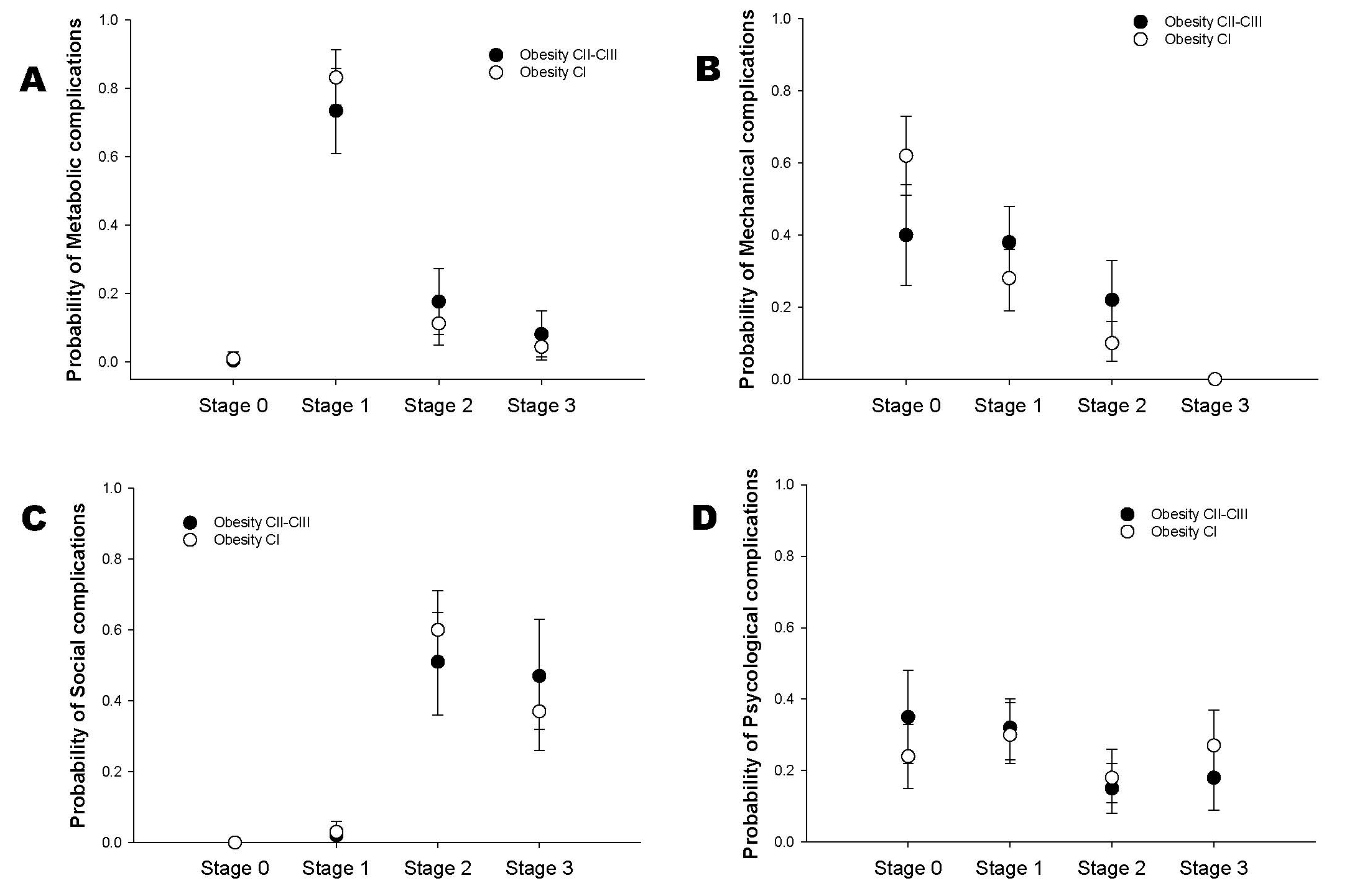
3.2. EOSS-P Staging
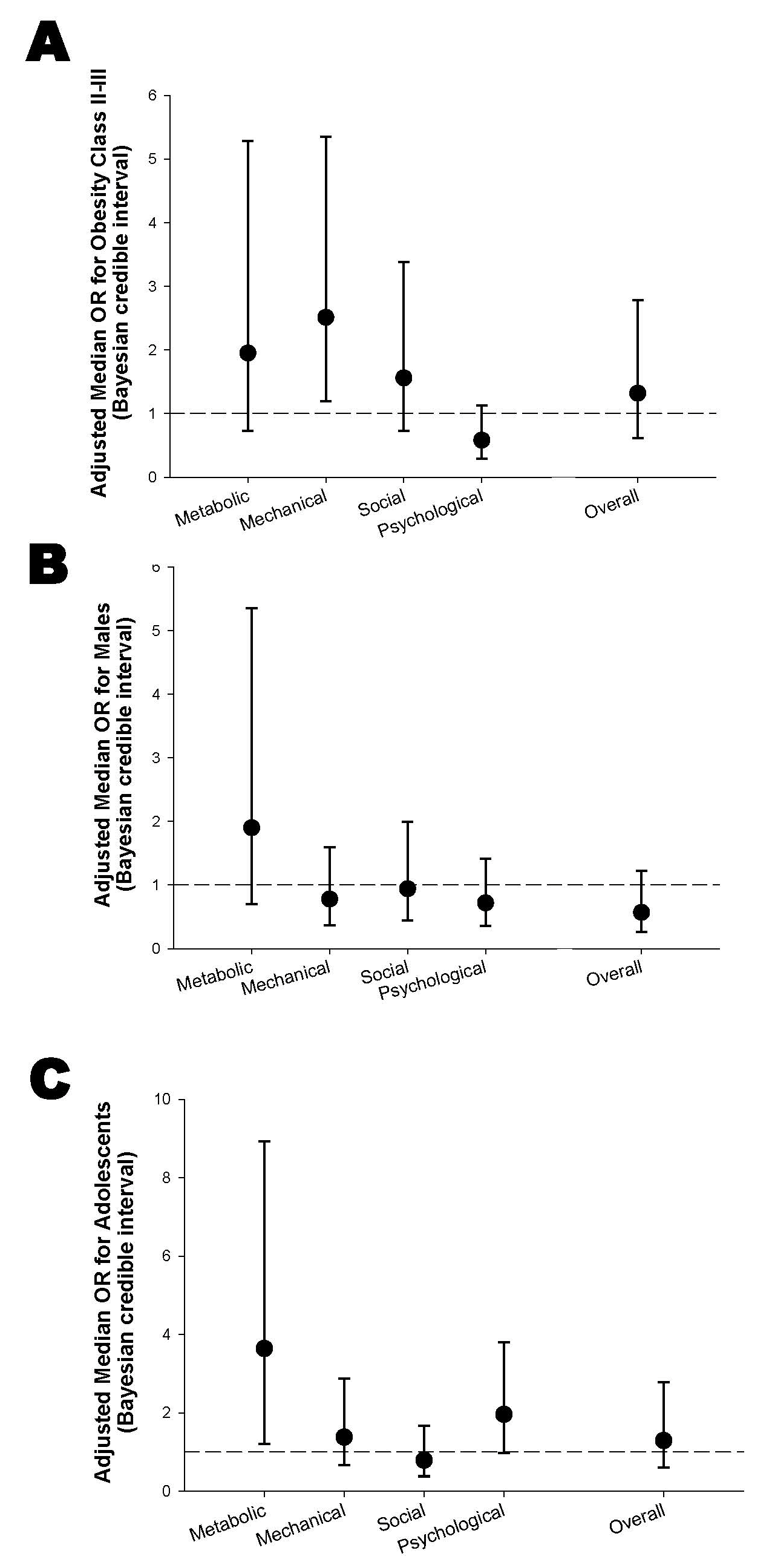
3.3. Association Between Obesity Classes and EOSS-P Staging
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BP | Blood Pressure |
| BMI | Body Mass Index |
| EOSS-P | Edmonton Obesity Staging System—Pediatric |
| PCOS | Polycystic Ovary Syndrome |
| ALT | Alanine transaminase |
| CPAP | Continuous positive airway pressure |
| DM2 | type 2 diabetes mellitus |
| GERD | gastroesophageal reflux disease |
| HDL-C | high-density lipoprotein cholesterol |
| LDL-C | low-density lipoprotein cholesterol |
| OSAS | obstructive sleep apnea syndrome |
| SD | Standard deviation |
References
- Obesity and Overweight [Internet]. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 7 August 2024).
- World Obesity Federation [Internet]. Global Atlas on Childhood Obesity. Available online: https://www.worldobesity.org/membersarea/global-atlas-on-childhood-obesity (accessed on 7 August 2024).
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [PubMed]
- The Heavy Burden of Obesity: Mexico [Internet]. 2019. Available online: https://www.oecd.org/en/publications/the-heavy-burden-of-obesity-country-notes_e2bd6a2c-en/mexico_b2906d73-en.html (accessed on 24 September 2025).
- Shamah-Levy, T.; Gaona-Pineda, E.B.; Cuevas-Nasu, L.; Morales-Ruan, C.; Valenzuela-Bravo, D.G.; Méndez-Gómez Humaran, I.; Ávila-Arcos, M.A. Prevalencias de sobrepeso y obesidad en población escolar y adolescente de México. Ensanut Continua 2020–2022. Salud Pública México 2023, 65, s218–s224. [Google Scholar] [CrossRef] [PubMed]
- Jebeile, H.; Kelly, A.S.; O’Malley, G.; Baur, L.A. Obesity in children and adolescents: Epidemiology, causes, assessment, and management. Lancet Diabetes Endocrinol. 2022, 10, 351–365. [Google Scholar] [CrossRef]
- Lister, N.B.; Baur, L.A.; Felix, J.F.; Hill, A.J.; Marcus, C.; Reinehr, T.; Summerbell, C.; Wabitsch, M. Child and adolescent obesity. Nat. Rev. Dis. Primers 2023, 9, 24. [Google Scholar] [CrossRef]
- Hampl, S.E.; Hassink, S.G.; Skinner, A.C.; Armstrong, S.C.; Barlow, S.E.; Bolling, C.F.; Edwards, K.C.A.; Eneli, I.; Hamre, R.; Joseph, M.M.; et al. Clinical Practice Guideline for the Evaluation and Treatment of Children and Adolescents with Obesity. Pediatrics 2023, 151, e2022060640. [Google Scholar] [CrossRef]
- Freedman, D.S.; Zemel, B.S.; Dietz, W.H.; Daymont, C. Screening Accuracy of BMI for Adiposity Among 8- to 19-Year-Olds. Pediatrics 2024, 154, e2024065960. [Google Scholar] [CrossRef]
- Ball, G.D.C.; Merdad, R.; Birken, C.S.; Cohen, T.R.; Goodman, B.; Hadjiyannakis, S.; Hamilton, J.; Henderson, M.; Lammey, J.; Morrison, K.M.; et al. Managing obesity in children: A clinical practice guideline. Can. Med Assoc. J. 2025, 197, E372–E389. [Google Scholar] [CrossRef]
- Sharma, A.M.; Kushner, R.F. A proposed clinical staging system for obesity. Int. J. Obes. 2009, 33, 289–295. [Google Scholar] [CrossRef]
- Hadjiyannakis, S.; Buchholz, A.; Chanoine, J.-P.; Jetha, M.M.; Gaboury, L.; Hamilton, J.; Birken, C.; Morrison, K.M.; Legault, L.; Bridger, T.; et al. The Edmonton Obesity Staging System for Pediatrics: A proposed clinical staging system for paediatric obesity. Paediatr. Child Health 2016, 21, 21–26. [Google Scholar] [CrossRef]
- Kuk, J.L.; Ardern, C.I.; Church, T.S.; Sharma, A.M.; Padwal, R.; Sui, X.; Blair, S.N. Edmonton Obesity Staging System: Association with weight history and mortality risk. Appl. Physiol. Nutr. Metab. 2011, 36, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Padwal, R.S.; Pajewski, N.M.; Allison, D.B.; Sharma, A.M. Using the Edmonton obesity staging system to predict mortality in a population-representative cohort of people with overweight and obesity. Can. Med Assoc. J. 2011, 183, E1059–E1066. [Google Scholar] [CrossRef]
- Rodríguez-Flores, M.; Goicochea-Turcott, E.W.; Mancillas-Adame, L.; Garibay-Nieto, N.; López-Cervantes, M.; Rojas-Russell, M.E.; Castro-Porras, L.V.; Gutiérrez-León, E.; Campos-Calderón, L.F.; Pedraza-Escudero, K.; et al. The utility of the Edmonton Obesity Staging System for the prediction of COVID-19 outcomes: A multi-centre study. Int. J. Obes. 2022, 46, 661–668. [Google Scholar] [CrossRef]
- Hadjiyannakis, S.; Ibrahim, Q.; Li, J.; Ball, G.D.C.; Buchholz, A.; Hamilton, J.K.; Zenlea, I.; Ho, J.; Legault, L.; Laberge, A.-M.; et al. Obesity class versus the Edmonton Obesity Staging System for Pediatrics to define health risk in childhood obesity: Results from the CANPWR cross-sectional study. Lancet Child Adolesc. Health 2019, 3, 398–407. [Google Scholar] [CrossRef]
- Grammatikopoulou, M.G.; Chourdakis, M.; Gkiouras, K.; Roumeli, P.; Poulimeneas, D.; Apostolidou, E.; Chountalas, I.; Tirodimos, I.; Filippou, O.; Papadakou-Lagogianni, S.; et al. Edmonton obesity staging system among pediatric patients: A validation and obesogenic risk factor analysis. J. Endocrinol. Investig. 2018, 41, 947–957. [Google Scholar] [CrossRef] [PubMed]
- Southcombe, F.; Vivekanandarajah, S.; Krstic, S.; Lin, F.; Chay, P.; Williams, M.; Khan, J.R.; Hu, N.; Eapen, V.; Dennis, S.; et al. More than just body mass index: Using the Edmonton obesity staging system for pediatrics to define obesity severity in a multi-ethnic Australian pediatric clinical cohort. Obes. Sci. Pr. 2023, 9, 285–295. [Google Scholar] [CrossRef]
- Kakon, G.A.; Hadjiyannakis, S.; Sigal, R.J.; Doucette, S.; Goldfield, G.S.; Kenny, G.P.; Prud’HOmme, D.; Buchholz, A.; Lamb, M.; Alberga, A.S. Edmonton Obesity Staging System for Pediatrics, quality of life and fitness in adolescents with obesity. Obes. Sci. Pr. 2019, 5, 449–458. [Google Scholar] [CrossRef]
- Gulati, A.K.; Kaplan, D.W.; Daniels, S.R. Clinical tracking of severely obese children: A new growth chart. Pediatrics 2012, 130, 1136–1140. [Google Scholar] [CrossRef] [PubMed]
- Burke, J.P.; E Hale, D.; Hazuda, H.P.; Stern, M.P. A quantitative scale of acanthosis nigricans. Diabetes Care 1999, 22, 1655–1659. [Google Scholar] [CrossRef]
- Flynn, J.T.; Kaelber, D.C.; Baker-Smith, C.M.; Blowey, D.; Carroll, A.E.; Daniels, S.R.; de Ferranti, S.D.; Dionne, J.M.; Falkner, B.; Flinn, S.K.; et al. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics 2017, 140, e20171904. [Google Scholar]
- Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum. Reprod. 2004, 19, 41–47. [CrossRef] [PubMed]
- Ferriman, D.D.; Gallwey, J.D. Clinical assessment of body hair growth in women. J. Clin. Endocrinol. Metab. 1961, 21, 1440–1447. [Google Scholar] [CrossRef]
- Chervin, R.D.; Hedger, K.; E Dillon, J.; Pituch, K.J. Pediatric sleep questionnaire (PSQ): Validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems. Sleep Med. 2000, 1, 21–32. [Google Scholar] [CrossRef]
- Ross, R.D. The Ross classification for heart failure in children after 25 years: A review and an age-stratified revision. Pediatr. Cardiol. 2012, 33, 1295–1300. [Google Scholar] [CrossRef]
- Birleson, P.; Hudson, I.; Buchanan, D.G.; Wolff, S. Clinical evaluation of a self-rating scale for depressive disorder in childhood (Depression Self-Rating Scale). J. Child Psychol. Psychiatry 1987, 28, 43–60. [Google Scholar] [CrossRef]
- Birmaher, B.; Khetarpal, S.; Brent, D.; Cully, M.; Balach, L.; Kaufman, J.; Neer, S.M. The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 545–553. [Google Scholar] [CrossRef]
- Garner, D.M.; Olmsted, M.P.; Bohr, Y.; Garfinkel, P.E. The eating attitudes test: Psychometric features and clinical correlates. Psychol. Med. 1982, 12, 871–878. [Google Scholar] [CrossRef] [PubMed]
- Vivar, R.; Pacheco, Z.; Adrianzén, C.; Macciotta, B.; Marchena, C. Validación de la Escala de Birleson modificada para trastornos depresivos en niños y adolescentes peruanos. Rev. Peru. Pediatría 2005, 58, 24–30. [Google Scholar] [CrossRef]
- Díaz-Ríos, L.K.; Chapman-Novakofski, K.; Malacara, J.M.; Bollero, G.; Aradillas-García, C.; Garay-Sevilla, E. Metabolic and nutritional profile differences among Mexican, Mexican-American and Non-Hispanic White children. Rev. Investig. Clin. 2014, 66, 31–44. [Google Scholar]
- Messiah, S.E.; Xie, L.; Kapti, E.G.; Chandrasekhar, A.; Srikanth, N.; Hill, K.; Williams, S.; Reid, A.; Mathew, M.S.; E Barlow, S. Prevalence of the metabolic syndrome by household food insecurity status in the United States adolescent population, 2001–2020: A cross-sectional study. Am. J. Clin. Nutr. 2023, 119, 354–361. [Google Scholar] [CrossRef]
- Flores-Viveros, K.L.; Aguilar-Galarza, B.A.; Ordóñez-Sánchez, M.L.; Anaya-Loyola, M.A.; Moreno-Celis, U.; Vázquez-Cárdenas, P.; García-Gasca, T. Contribution of genetic, biochemical and environmental factors on insulin resistance and obesity in Mexican young adults. Obes. Res. Clin. Pr. 2019, 13, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Rivas-Gomez, B.; Almeda-Valdés, P.; Tussié-Luna, M.T.; Aguilar-Salinas, C.A. Dyslipidemia in Mexico, A Call for Action. Rev. Investig. Clínica 2018, 70, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Luo, D.; Li, M.; Tang, B. Insulin Resistance in Pediatric Obesity: From Mechanisms to Treatment Strategies. Pediatr. Diabetes 2024, 2024, 2298306. [Google Scholar] [CrossRef]
- Park, H.; Choi, J.E.; Jun, S.; Lee, H.; Kim, H.S.; Lee, H.A.; Park, H. Metabolic complications of obesity in children and adolescents. Clin. Exp. Pediatr. 2023, 67, 347–355. [Google Scholar] [CrossRef]
- Caliendo, C.; Femiano, R.; Umano, G.R.; Martina, S.; Nucci, L.; Perillo, L.; Grassia, V. Effect of Obesity on the Respiratory Parameters in Children with Obstructive Sleep Apnea Syndrome. Children 2023, 10, 1874. [Google Scholar] [CrossRef]
- Dehlink, E.; Tan, H.L. Update on paediatric obstructive sleep apnoea. J. Thorac. Dis. 2016, 8, 224. [Google Scholar]
- Godina-Flores, N.L.; Gutierrez-Gómez, Y.Y.; García-Botello, M.; López-Cruz, L.; Moreno-García, C.F.; Aceves-Martins, M. Obesity and its association with mental health among Mexican children and adolescents: Systematic review. Nutr. Rev. 2022, 81, 658–669. [Google Scholar] [CrossRef] [PubMed]
- Rao, W.-W.; Zong, Q.-Q.; Zhang, J.W.; An, F.R.; Jackson, T.; Ungvari, G.S.; Xiang, Y.; Su, Y.-Y.; D’Arcy, C.; Xiang, Y.-T. Obesity increases the risk of depression in children and adolescents: Results from a systematic review and meta-analysis. J. Affect. Disord. 2020, 267, 78–85. [Google Scholar] [CrossRef]
- Aceves-Martins, M.; Gutierrez-Gómez, Y.Y.; Moreno-García, C.F. Socioeconomic determinants of overweight and obesity among Mexican children and adolescents: Systematic review and meta-analysis. Obes. Rev. 2025, 26, e13926. [Google Scholar] [CrossRef]
- Ayala, G.X.; Monge-Rojas, R.; King, A.C.; Hunter, R.; Berge, J.M. The social environment and childhood obesity: Implications for research and practice in the United States and countries in Latin America. Obes. Rev. 2021, 22 (Suppl. S3), e13246. [Google Scholar] [CrossRef]
- Lemstra, M.E.; Rogers, M. Mental health and socioeconomic status impact adherence to youth activity and dietary programs: A meta-analysis. Obes. Res. Clin. Pract. 2021, 15, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Jayadevan, C.M.; Trung Hoang, N. Healthcare spending in high-income and upper-middle-income countries: A cross-country analysis. Discov. Heal. Syst. 2024, 3, 37. [Google Scholar] [CrossRef]
- Karabukayeva, A.; Anderson, J.L.; Hall, A.G.; Feldman, S.S.; Mehta, T. Exploring a Need for a Cardiometabolic Disease Staging System as a Computerized Clinical Decision Support Tool: Qualitative Study. JMIR Form. Res. 2022, 6, e37456. [Google Scholar] [CrossRef] [PubMed]
- Swaleh, R.; McGuckin, T.; Myroniuk, T.W.; Manca, D.; Lee, K.; Sharma, A.M.; Campbell-Scherer, D.; Yeung, R.O. Using the Edmonton Obesity Staging System in the real world: A feasibility study based on cross-sectional data. CMAJ Open 2021, 9, E1141–E1148. [Google Scholar] [CrossRef] [PubMed]
| Total n = 118 Mean (SD) | Females n = 51 Mean (SD) | Males n = 67 Mean (SD) | p-Value | |
|---|---|---|---|---|
| Age (years) | 11.4 (2.5) | 11.9 (2.4) | 11.0 (2.4) | 0.057 |
| Height (cm) | 150.5 (12.7) | 151.2 (12.1) | 150.0 (13.6) | 0.620 |
| BMI Z-score | 2.1 (0.32) | 2.1 (0.25) | 2.1 (0.37) | 0.444 |
| Obesity diagnosis | n (%) | n (%) | n (% ) | p-value |
| Obesity Class I | 76 (64.4) | 37 (72.5) | 39 (58.2) | 0.205 |
| Obesity Class II | 33 (28.0) | 10 (19.6) | 23 (34.3) | |
| Obesity Class III | 9 (7.6) | 4 (7.8) | 5 (7.5) | |
| Group age | n (%) | n (%) | n (%) | p-value |
| School age children | 66 (56%) | 24 (47.1) | 42 (62.7) | 0.090 |
| Adolescents | 52 (44%) | 27 (52.9) | 25 (37.3) |
| EOSS Domains | Total n = 118 n (%) | Obesity Class I n = 76 n (%) | Obesity Class II/III n = 42 n (%) | p-Value |
|---|---|---|---|---|
| Metabolic domain stage | ||||
| 0 | 1 (0.8) | 1 (1.2) | 0 (0.0) | 0.489 |
| 1 | 94 (79.7) | 63 (82.9) | 31 (73.8) | |
| 2 | 16 (13.6) | 8 (10.5) | 8 (19.1) | |
| 3 | 7 (5.9) | 4 (5.3) | 3 (7.1) | |
| Mechanical domain stage | ||||
| 0 | 64 (54.2) | 47 (61.9) | 17 (40.5) | 0.065 |
| 1 | 37 (31.4) | 21 (27.6) | 16 (38.1) | |
| 2 | 17 (14.4) | 8 (10.5) | 9 (21.4) | |
| 3 | 0 | |||
| Psychological domain stage | ||||
| 0 | 33 (28.0) | 19 (25.0) | 14 (33.3) | 0.318 |
| 1 | 37 (31.4) | 22 (28.9) | 15 (35.7) | |
| 2 | 20 (16.9) | 13 (17.1) | 7 (16.7) | |
| 3 | 28 (23.7) | 22 (28.9) | 6 (14.3) | |
| Social domain stage | ||||
| 0 | 0 | 0 | 0 | 0.541 |
| 1 | 3 (2.5) | 2 (2.6) | 1 (2.4) | |
| 2 | 67 (56.8) | 46 (60.5) | 21 (50.0) | |
| 3 | 48 (40.7) | 28 (36.8) | 20 (47.6) | |
| Overall EOSS-P stage | ||||
| 0 | 0 | 0 | 0 | 0.796 |
| 1 | 2 (1.7) | 1 (1.3) | 1 (2.4) | |
| 2 | 49 (41.5) | 33 (43.4) | 16 (38.1) | |
| 3 | 67 (56.8) | 42 (55.3) | 25 (59.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Omaña-Guzmán, I.; Rodríguez Quintero, R.C.; Ruíz-Arroyo, A.; Prado Díaz, E.; López-Alvarenga, J.C.; Hernández López, A.M.; Fuentes Corona, Z.; Aguilar Cuarto, K.; Pedraza Escudero, K.; Ruíz Barranco, A.; et al. The Edmonton Obesity Staging System for Pediatrics (EOSS-P) in Mexican Children and Adolescents Living with Obesity: Beyond BMI Obesity Classes. Children 2025, 12, 1556. https://doi.org/10.3390/children12111556
Omaña-Guzmán I, Rodríguez Quintero RC, Ruíz-Arroyo A, Prado Díaz E, López-Alvarenga JC, Hernández López AM, Fuentes Corona Z, Aguilar Cuarto K, Pedraza Escudero K, Ruíz Barranco A, et al. The Edmonton Obesity Staging System for Pediatrics (EOSS-P) in Mexican Children and Adolescents Living with Obesity: Beyond BMI Obesity Classes. Children. 2025; 12(11):1556. https://doi.org/10.3390/children12111556
Chicago/Turabian StyleOmaña-Guzmán, Isabel, Roberto Carlos Rodríguez Quintero, Arturo Ruíz-Arroyo, Edith Prado Díaz, Juan Carlos López-Alvarenga, Ana María Hernández López, Zendy Fuentes Corona, Karina Aguilar Cuarto, Karen Pedraza Escudero, Alejandra Ruíz Barranco, and et al. 2025. "The Edmonton Obesity Staging System for Pediatrics (EOSS-P) in Mexican Children and Adolescents Living with Obesity: Beyond BMI Obesity Classes" Children 12, no. 11: 1556. https://doi.org/10.3390/children12111556
APA StyleOmaña-Guzmán, I., Rodríguez Quintero, R. C., Ruíz-Arroyo, A., Prado Díaz, E., López-Alvarenga, J. C., Hernández López, A. M., Fuentes Corona, Z., Aguilar Cuarto, K., Pedraza Escudero, K., Ruíz Barranco, A., Villanueva-Ortega, E., & Garibay-Nieto, N. (2025). The Edmonton Obesity Staging System for Pediatrics (EOSS-P) in Mexican Children and Adolescents Living with Obesity: Beyond BMI Obesity Classes. Children, 12(11), 1556. https://doi.org/10.3390/children12111556







