1. Introduction
The dual effects of education expenditure on life expectancy arise from the competing forces of crowding-out and complementarity within public resource allocation. The crowding-out effect occurs when higher education expenditure diverts limited fiscal resources from the health sector, thereby constraining healthcare access and weakening health outcomes. Conversely, the complementarity effect reflects the human-capital framework, which views education and health as mutually reinforcing components of human productivity. Education improves health literacy, income potential, and the capacity to adopt preventive health behaviours, while good health enhances learning efficiency and labour participation. Early theoretical work by
Grossman (
1972,
1999) conceptualized health as a durable capital stock, with education increasing the efficiency of health investment.
Galama and van Kippersluis (
2015) further formalized this relationship, showing that investments in skill-capital and health-capital are multiplicative and jointly enhance longevity. Empirical studies across OECD countries confirm that educational attainment is positively associated with population health and life expectancy (
Ahmed et al., 2020), while long-term analyses show that both education and health spending promote longevity, though with varying strength across development stages (
Zhou et al., 2024). Thus, whether education spending crowds out or complements health outcomes depends on a nation’s fiscal capacity and stage of development, determining if the two sectors act as substitutes or synergistic drivers of population longevity.
The summary statistics reveal marked cross-country variation in education and health expenditure, consistent with recent global data from the
World Bank (
2024b) and
WHO (
2024). High-income countries (HICs) allocate the highest mean shares of GDP to education (4.7%) and government health expenditure (5.8%), supporting life expectancy levels above 77 years. By contrast, low-income countries (LICs) spend far less—about 3.3% on education and only 1.9% on health—accompanied by an average life expectancy of 53.9 years. This gap mirrors contemporary trends, where OECD members collectively invest over 5% of GDP in education and 7–9% in health, while Sub-Saharan African nations average just 3–4% and 2%, respectively. The broad ranges and standard deviations in public spending on health underscore fiscal heterogeneity and the persistence of inequality in public investment priorities across income groups.
The intermediate categories—upper-middle-income (UMCs) and lower-middle-income countries (LMCs)—display transitional patterns, spending around 4.2% and 3.8% of GDP on education, and 3.9% and 2.5% on health, respectively, yielding life expectancies near 70 and 64 years. These figures align with recent regional patterns reported by
UNESCO Institute for Statistics (
2024), where rising education budgets in East Asia and Latin America coincide with gradual improvements in life expectancy. However, large expenditure ranges (up to 25 percentage points for health and 14 for education) suggest volatility and uneven fiscal commitment. Together, these results highlight the dual dynamics motivating this study: while wealthier nations demonstrate a mature complementarity between education and health spending, developing economies often face trade-offs that risk crowding-out effects. Understanding these disparities is essential for designing coordinated human-capital policies that balance investment efficiency with social equity.
The crowding-out effect occurs when increased government spending in one area leads to a decrease in spending in another. In the context of education expenditure, this effect may manifest if governments increase their spending on education at the expense of other sectors, such as healthcare. When public education expenditure rises, it may divert resources away from healthcare, resulting in lower healthcare spending and potentially negatively affecting life expectancy. Conversely, increased educational spending could directly improve life expectancy by improving literacy and health outcomes. Life Expectancy is a crucial indicator of a country’s public health and overall well-being. It is influenced by a range of factors, including access to healthcare, economic conditions, nutrition, and education. Education has been shown to correlate positively with life expectancy, as more educated populations tend to make healthier choices, have better access to healthcare, and earn higher incomes. Addressing this issue requires a balanced approach to public spending, in which both education and healthcare receive adequate attention to maximize the long-term well-being and life expectancy of the population.
Government spending on education and health plays a pivotal role in fostering economic growth and in enhancing social outcomes. Extensive research indicates that such investments significantly contribute to human capital development, which, in turn, drives productivity and long-term economic growth. To understand the crowding-out effect of educational expenditure on life expectancy, several key economic and policy theories are relevant. According to Public Budget Constraint Theory, governments operate within budget constraints, meaning that an increase in spending on one area (e.g., education) often leads to a reduction in other areas (e.g., healthcare). If education expenditure increases significantly, it may crowd out healthcare spending, potentially reducing access to healthcare services and negatively affecting life expectancy (
Musgrave & Musgrave, 1989). The Human Capital Theory suggests that investment in education enhances the skills and productivity of the workforce, leading to higher incomes and improved health outcomes. However, if education expenditure reduces healthcare spending, the broader societal benefits of education in improving public health may be compromised (
Schultz, 1961). According to the Public Goods and Externalities Theory, education and healthcare are both public goods that provide positive externalities to society. If an increase in education spending leads to reduced healthcare investment, the positive externalities of education, such as healthier and more productive populations, could be undermined by a lack of investment in public health (
Musgrave, 1959). The Preston Curve (
Preston, 1975), along with subsequent extensions (e.g.,
Lutz & Kebede, 2018), demonstrates a non-linear yet positive relationship between income, educational attainment, and reductions in mortality. However, the benefits of these factors tend to taper off, indicating diminishing returns at higher income and education levels.
Life Expectancy is a critical indicator of a nation’s public health and overall well-being. It is influenced by a range of factors, including access to healthcare, economic conditions, nutrition, and education. Numerous studies suggest a positive correlation between education and life expectancy; individuals in more educated populations tend to make healthier lifestyle choices, have better access to healthcare, and enjoy higher incomes, all of which contribute to longer life expectancy. However, a significant concern arises when increased government spending on education leads to a reduction in funding for other sectors, such as healthcare. This phenomenon, known as the “crowding-out effect,” has profound implications for public health and life expectancy.
Understanding the Crowding-Out Effect
The crowding-out effect refers to a situation in which an increase in government expenditure in one area, such as education, results in a decrease in spending in another area, typically because of limited budgetary resources. When a government reallocates its budget to increase spending on education, it might reduce its healthcare budget, which could negatively affect public health services and, consequently, life expectancy. While educational expenditure may directly contribute to life expectancy by improving literacy and raising awareness about health issues, the crowding-out effect can mitigate these benefits by limiting investment in healthcare.
The relationship between education expenditure and life expectancy is complex and influenced by both direct and indirect effects. Educational spending could improve life expectancy by promoting better health literacy, promoting healthier lifestyles, and reducing mortality rates. However, if an increase in education expenditure leads to reduced healthcare funding, the benefits of education could be undermined by a decline in healthcare access and quality, ultimately resulting in a lower life expectancy.
Educational expenditure has a direct and positive impact on life expectancy by enhancing public awareness of health issues, encouraging healthier behaviors, and reducing mortality rates. Greater investment in education leads to higher levels of educational attainment, which in turn improves economic opportunities and access to health care. Collectively, these factors contribute to better individual and public health outcomes, thereby directly extending life expectancy.
Despite potential trade-offs, education can continue to influence health, even when healthcare spending is positively constrained. Enhanced education fosters long-term health improvements by increasing health literacy and encouraging individuals to make informed health-related decisions. This interaction suggests that the impact of education on life expectancy extends beyond direct funding for healthcare and is rooted in the broader societal and behavioral benefits of a well-educated population.
Drawing on the dual-effect framework of education expenditure, this study examines both the potential crowding-out and complementarity relationships between education, healthcare, and life expectancy across income groups. Firstly, it is hypothesized that higher education expenditure (EEXP) may exert a negative direct effect on healthcare expenditure (DGGHE), particularly in low-income (LICs) and lower-middle-income countries (LMCs) where fiscal resources are limited. If education spending significantly reduces health spending, this would confirm a crowding-out effect, suggesting that budgetary expansion in the education sector comes at the expense of healthcare provision.
Secondly, education expenditure is expected to have a positive direct effect on life expectancy (LEXPT). Greater investment in education enhances health literacy, income potential, and preventive health behaviours, which collectively improve population longevity. This positive association is likely to be stronger in lower-middle-income (LMCs) and upper-middle-income countries (UMCs), where educational expansion yields higher human-capital returns, and weaker in high-income countries (HICs), where marginal gains from education are smaller.
Thirdly, education expenditure may also affect life expectancy indirectly through its influence on healthcare expenditure. A positive mediated effect would indicate a crowding-in mechanism, whereby investment in education stimulates public health spending, which subsequently raises life expectancy. This indirect effect is anticipated to be strongest in LMCs and UMCs, reflecting fiscal and institutional complementarities between education and health systems, while remaining weaker in LICs where resource constraints persist. To verify these relationships, the study employs a two-stage least squares (2SLS) estimation and bootstrap mediation analysis to decompose the total effect of education expenditure into direct and indirect components across income groups.
The remainder of this paper is organized as follows.
Section 2 provides a brief review of the relevant literature.
Section 3 presents the data set, model, and methods used in this study.
Section 4 reports the findings of this analysis. Finally,
Section 5 concludes the research and summarizes the essential findings and their implications.
2. Literature Review
Life Expectancy is a widely recognized indicator of population health and socioeconomic progress. A rich body of empirical literature demonstrates that improvements in life expectancy are shaped by multiple structural factors, including economic growth (
Aksan & Chakraborty, 2023), social policy (
Reynolds & Avendano, 2018), access (
van den Heuvel & Olaroiu, 2017), education (
Baker et al., 2011;
Lutz & Kebede, 2018), institutional quality (
Nica et al., 2023), and environmental conditions. Over recent decades, life expectancy has generally improved across countries, driven by expansions in education, rising incomes, public health interventions, and increased investments in the health and social sectors (
OECD, 2024;
World Health Organization, 2024). However, these improvements are often shaped by fiscal-policy trade-offs between education and health. When governments expand education budgets under fiscal constraints, resources may be diverted from healthcare, limiting immediate access to medical services and dampening gains in longevity. Conversely, coordinated or complementary investment across both sectors can create reinforcing effects: education enhances health literacy, income potential, and preventive behaviour, while health spending ensures the realization of these human-capital returns through longer, healthier lives. The
OECD (
2017) working paper documents significant life-expectancy gaps between high- and low-education groups—about eight years for men and five for women at age 25—underscoring how education and health investments jointly determine long-term welfare and inequality outcomes, with cardiovascular disease being a significant cause of mortality differences.
The IMF study by
Baldacci et al. (
2004) provides early evidence that public spending on education enhances attainment while health expenditure reduces infant and child mortality, underscoring the developmental role of both sectors. Subsequent research has expanded on these foundations, emphasizing that the effectiveness of social spending depends on cross-sectoral coordination and fiscal efficiency rather than the magnitude of expenditure alone. More recent analyses highlight that since 2015, countries have increasingly faced interlinked investment challenges, as governments seek to balance rising education demands with the need for resilient healthcare systems. Empirical trends reveal that when educational and health investments are jointly scaled, long-term gains in life expectancy and productivity are stronger and more equitable. However, under fragmented or constrained budgets, expansion in one sector can inadvertently crowd out the other, diminishing aggregate welfare effects.
Batbold et al. (
2022) illustrate this tension at the household level in Mongolia, where out-of-pocket health costs reduce essential consumption yet spur compensatory spending on education, reflecting differing perceptions of long-term returns. Similarly,
Sijabat (
2022) shows that the combined effects of health and education expenditure on human development in Indonesia are contingent on fiscal capacity and institutional effectiveness. Together, these findings suggest that contemporary policy debates have shifted toward optimizing joint investment strategies to sustain human capital accumulation and improve health outcomes over the long run.
Among these determinants, education is prominently featured as a long-term enhancer of health outcomes. Education enhances health literacy, promotes healthier behaviors, and contributes to increased earnings, all of which are positively associated with longevity (
Baker et al., 2011;
Balaj et al., 2024). The Preston Curve (
Preston, 1975) and its later iterations (e.g.,
Lutz & Kebede, 2018) illustrate a non-linear but positive association between income, education, and mortality reduction. However, these relationships are subject to diminishing returns, especially at higher educational attainment and income. This raises an underexplored yet essential policy question: can increasing educational expenditure beyond a certain threshold lead to reduced fiscal space for health investment, thereby attenuating or even reversing gains in life expectancy?
This concern falls within the framework of the crowding-out effect, a well-established concept in public finance that suggests that prioritizing spending in one domain (e.g., education) may reduce available resources for others (e.g., health). Despite its theoretical grounding, empirical investigation of the crowding-out effects of education expenditure on life expectancy remains limited and fragmented.
For instance,
Smith and Lee (
2023) analyzed OECD countries from 2005 to 2021. They found that while social, educational, and health expenditures all contributed positively to life expectancy, health spending and GDP per capita had more potent effects than educational expenditure. Although not explicitly labeled as crowding-out, their findings suggest possible inefficiencies or diminishing returns when reallocating public resources to education at the expense of health.
Reynolds and Avendano (
2018) and
Dutton et al. (
2018) further explore the trade-offs among different categories of public spending. While Reynolds and Avendano found positive associations between education and life expectancy, they also acknowledged that education and health expenditure may not be equally effective at all stages of development, hinting at the possibility of reallocation effects.
Dutton et al. (
2018), without directly invoking the term “crowding-out,” examined how budget allocations among health, education, and social services influence health outcomes and found that certain forms of social spending (e.g., housing or incapacity benefits) may outperform education in improving health metrics.
Similarly,
Khan and Bashar (
2015) used Granger causality and cointegration models to investigate the relationship between public expenditures and economic growth in Australia and New Zealand. Although life expectancy was not a direct outcome, the study highlighted significant interactions between the types of public spending, supporting the idea that trade-offs may exist between sectors.
Conceptual support for this view is also found by
Giouli (
2022), who discusses the constraints of budgetary allocation in fostering economic growth and innovation. Focusing on the Greek economy and the role of human capital, the analysis highlights the budgetary tension between funding education and other critical sectors, particularly healthcare.
Notably, the Preston Curve literature (
Preston, 1975;
Lutz & Kebede, 2018) also indirectly supports the potential crowding-out hypothesis. This shows the health benefits of increasing income and education plateau beyond a certain level, implying that continued expansion of education spending may yield fewer health returns and could even divert essential resources away from more impactful health investments.
Despite these fragmented insights, there is currently no unified or systematic empirical framework that examines whether increasing education expenditure crowds out health spending and adversely impacts life expectancy. This absence constitutes a critical research gap in the literature.
Furthermore, most existing studies rely on traditional panel data techniques, such as fixed effects, ARDL, and GMM (
Khan & Bashar, 2015;
Ketenci & Murthy, 2018), without adequately addressing endogeneity and allocation trade-offs. The use of instrumental variable methods, such as Two-Stage Least Squares (2SLS), remains rare in the literature despite their suitability for disentangling causal relationships under budget constraints. While some studies (e.g.,
Roffia et al., 2023) address endogeneity using dynamic panels such as the Arellano–Bond estimators, none have employed 2SLS to directly analyze the crowding-out effect between education and health investment in the context of life expectancy.
The temporal and geographic scope of existing research is also limited. Many datasets ended before the COVID-19 pandemic, excluding a major shock that reshaped fiscal priorities and exposed weaknesses in public health infrastructure (
Welsh et al., 2021). Additionally, while high-income and OECD countries are frequently studied, evidence from developing regions, especially sub-Saharan Africa, South Asia, and Latin America, remains scarce (
Bein & Coker-Farrell, 2020;
Hassan et al., 2017). These are precisely the settings where crowding-out effects are likely to be most acute, given more constrained public budgets and competing development priorities.
In summary, while education is undeniably a vital determinant of health, its fiscal trade-offs with health expenditures and the potential unintended consequences for life expectancy are often overlooked in empirical research. The existing literature confirms the multifactorial nature of life expectancy determinants. However, it rarely explores whether and when education investment reaches a point of diminishing or even negative returns through the crowding-out of health resources. This study aims to fill this gap by explicitly modelling the crowding-out effects of educational expenditure on life expectancy using robust causal inference methods (e.g., 2SLS) and up-to-date cross-country panel data. By doing so, it contributes to a more nuanced understanding of how governments can balance investment in human capital and health to optimize population well-being.
3. Methodology
This study utilized panel data from 158 countries covering the period 1990–2023, comprising 54 high-income countries (HICs), 39 upper-middle-income countries (UMCs), 46 lower-middle-income countries (LMCs), and 19 low-income countries (LICs). The data were obtained from the World Bank’s World Development Indicators (
World Bank, 2025b). The classification of countries follows the World Bank’s Atlas method, which categorizes economies based on their Gross National Income (GNI) per capita adjusted for exchange rate fluctuations. According to the World Bank’s (
World Bank, 2025a) 2023 classification (effective 1 July 2023), the income thresholds were low-income (
$1135 or less), lower-middle-income (
$1136–
$4465), upper-middle-income (
$4466–
$13,845), and high-income (
$13,846 or more). The list of countries classified under each income group is provided in the
Appendix A.
This study utilizes an unbalanced panel dataset covering four income groups—high-, upper-middle-, lower-middle-, and low-income countries—from 1990 to 2023. All variables were obtained from the World Development Indicators (
World Bank, 2025b), ensuring international comparability. Life expectancy at birth (LEXPT), measured in years, serves as the primary indicator of population health. Government expenditure on education (EEXP) and domestic general government health expenditure (DGGHE) are both expressed as percentages of gross domestic product (GDP) and capture national investment priorities in human capital. GDP per capita (GDPC), measured in purchasing power parity (PPP)–adjusted constant 2021 international USD, represents economic development and was converted into real terms to account for inflation. Unemployment (UNEM) and urban population share (URBP) are measured as percentages of the total labor force and total population, respectively, reflecting labor-market and demographic conditions. Inflation (INFL) is defined as the annual percentage change in consumer prices, while income inequality (GINI) is represented by the Gini coefficient on a 0–100 scale. Finally, a time trend (TREND) variable was constructed to capture long-term structural and technological progress.
To empirically assess the crowding-out effect of educational expenditure on life expectancy, a combination of regression analysis and econometric models can be used. The following steps outline a typical approach: This type of model is appropriate because both education expenditure and healthcare expenditures can simultaneously affect life expectancy. A simultaneous equation model allows us to test the interdependencies between these variables. This system of equations accounts for the possibility that educational spending can have a direct impact on both healthcare spending and life expectancy. To model Equations (1) and (2) with a time trend, we introduce a time variable (Trend) to account for the general upward or downward movement in life expectancy and governmental health expenditure over time. The time trend helps capture long-term effects that are not explicitly explained by other variables, such as medical advancements or evolving policy changes.
3.1. Two-Stage Least Squares Analysis
To address potential endogeneity, the study employed the Two-Stage Least Squares (2SLS) estimation technique—also known as Instrumental Variables (IV) estimation—using internal instruments, specifically the lagged values of the endogenous variables. These lagged terms are assumed to be correlated with the endogenous regressors but uncorrelated with the contemporaneous error term, thereby improving the consistency of the estimated parameters. We treated GDP per capita (gdpc), health expenditure (eexp), and government health expenditure (dgghe) as endogenous variables in the life expectancy equation and used their lagged values as instruments. Similarly, in the health equation, gdpc and eexp were considered endogenous, with their respective lagged terms employed as instruments.
2SLS is commonly applied when there is potential reverse causality or omitted variable bias, which violates the assumptions of ordinary least squares (OLS) regression (
Greene, 2018). Identification in a system of simultaneous equations refers to sufficient information to estimate the model’s parameters based on its specified functional form. The identification strategy in 2SLS involves ensuring that each equation in the system is appropriately identified before estimation, which requires satisfying certain conditions to ensure that the model parameters can be uniquely estimated. The key elements of the identification strategy are as follows.
Each structural equation in the model must include at least as many excluded exogenous variables as there are endogenous right-hand-side variables to satisfy the order and rank conditions for identification. In this study, the GINI variable was excluded from the first equation, while the urban population ratio (URBP) was excluded from the second Equation to ensure that both equations had sufficient instruments for valid identification.
Because the 2SLS method estimates all equations simultaneously, it is essential to verify the identification conditions for each equation individually. If any equation were underidentified, it could compromise the identification of the entire system. Both Equations (1) and (2) satisfied the identification requirements, allowing a well-specified system of simultaneous equations to be obtained. Meeting these conditions enables 2SLS to consistently and efficiently estimate the parameters while accounting for potential correlations among the disturbance terms.
The exclusion restrictions were guided by theoretical and empirical reasoning. The GINI coefficient, which measures income inequality, affects health outcomes—such as life expectancy—through social determinants of health and disparities in resource access. However, once macroeconomic variables like GDP per capita and unemployment are controlled for, GINI is not expected to have a direct impact on government healthcare expenditure. Accordingly, GINI was excluded from the healthcare expenditure equation but retained in the life expectancy equation.
Conversely, the URBP variable captures the degree of urbanization, which directly influences government healthcare spending through infrastructure development and service delivery demands. Its effect on life expectancy is more indirect once education and healthcare expenditure are accounted for. Therefore, URBP was included in the healthcare expenditure equation but excluded from the life expectancy equation. These theoretically grounded exclusions satisfy the order and rank conditions, ensuring that each equation is at least exactly identified and suitable for consistent estimation using the 2SLS method.
To investigate the interrelationships among education expenditure, healthcare expenditure, and life expectancy, two econometric model equations were estimated. The first model examines how government healthcare expenditure is influenced by education expenditure and other macroeconomic and demographic factors, while the second model explores how life expectancy responds to variations in both education and healthcare expenditure, alongside broader socioeconomic conditions. This dual-equation framework allows for testing both the direct and indirect pathways through which education affects population health outcomes.
The first model, presented in Equation (1), specifies the determinants of government health expenditure (DGGHE):
Equation (1) models the logarithm of government health expenditure () for country i in year t as a function of several explanatory variables. Education expenditure () represents the government’s financial commitment to education, which may either complement or substitute healthcare spending depending on policy priorities. Inflation () captures macroeconomic stability and cost pressures that can affect the real value of government budgets. The lagged share of the urban population () reflects urbanization and its effect on the demand for public health services. GDP per capita () serves as a measure of national income and fiscal capacity, while the unemployment rate () represents labor market conditions that may influence social welfare spending. Finally, the time trend () captures structural and technological changes in healthcare systems over time, and denotes the random disturbance term. A negative and statistically significant coefficient would suggest a “crowding-out” effect, indicating that higher education expenditure reduces healthcare spending, whereas a positive coefficient would imply that education and health expenditures are complementary.
The second model, shown in Equation (2), examines the determinants of life expectancy and incorporates both education and healthcare expenditure as explanatory variables:
In Equation (2), the dependent variable is life expectancy at birth (), an indicator of overall population health. Education expenditure () captures the effect of human capital investment on longevity, while government healthcare expenditure () represents the direct provision of medical services and is treated as an endogenous regressor due to potential reverse causality between health spending and life expectancy. Income inequality () reflects disparities in income distribution that may limit equitable access to healthcare and health-enhancing resources. Inflation (), GDP per capita (), and unemployment () retain the same interpretations as in Equation (1), controlling for broader macroeconomic and labor market conditions. The time trend () captures persistent improvements in healthcare technology and living standards over time, while represents the error term. A positive and significant coefficient would indicate that greater healthcare expenditure contributes to higher life expectancy, while a positive would imply that investment in education independently enhances longevity through improved awareness, behavior, and social outcomes.
Together, these two equations allow for testing the mediating role of healthcare expenditure in the relationship between education expenditure and life expectancy. The indirect effect is computed as the product . A negative and statistically significant value of this product indicates that higher education spending reduces healthcare expenditure, which in turn lowers life expectancy—a crowding-out effect. The significance of this mediated pathway can be tested using the Sobel test, which evaluates whether the indirect effect differs significantly from zero based on the standard errors of and . This approach provides a rigorous means of determining whether healthcare expenditure acts as a significant mediator in the education–health nexus.
The overall framework recognizes the complex and bidirectional relationships among education, health spending, and population well-being. On one hand, increased health expenditure enhances life expectancy through better access to healthcare services, infrastructure, and disease prevention. On the other hand, rising life expectancy, especially in aging populations, can increase the demand for healthcare resources. These interactions are further shaped by macroeconomic conditions such as inequality, inflation, and unemployment. Accordingly, estimation techniques such as 2SLS are appropriate to account for endogeneity and to obtain consistent coefficient estimates. The two model equations together provide a coherent structure for understanding how educational investment and economic context jointly determine health expenditure patterns and life expectancy outcomes across countries. The key variables and their descriptions are presented in
Table 1.
To address potential endogeneity arising from reverse causality and omitted variable bias, the study employs the 2SLS estimator. Endogeneity is a major concern in models linking education, health expenditure, and life expectancy, as these variables are mutually reinforcing over time. Accordingly, GDP per capita (GDPC), education expenditure (EEXP), and government health expenditure (DGGHE) were treated as endogenous in the life expectancy equation, and their lagged values were used as instruments. Similarly, in the health expenditure equation, GDPC and EEXP were considered endogenous, with their respective lagged terms serving as instruments. The use of lagged instruments is justified on theoretical grounds, as past values of these variables influence current expenditure patterns but are less likely to correlate with contemporaneous error terms (
Wooldridge, 2010;
Stock & Watson, 2020). Instrument relevance was confirmed through first-stage F-statistics exceeding the conventional threshold of 10, indicating strong correlation with endogenous regressors (
Staiger & Stock, 1997). No overidentifying restrictions were observed, consistent with a just-identified specification. These diagnostics collectively support the validity of the chosen instruments and the robustness of the 2SLS estimates in mitigating endogeneity bias.
Endogeneity was empirically addressed using a 2SLS approach, where lagged values of the potentially endogenous variables were employed as instruments. This technique helps to mitigate bias arising from simultaneity or reverse causality. However, we also note that while 2SLS reduces endogeneity concerns, it may not entirely eliminate them if the instruments are weak or only partially exogenous. Future research could further strengthen causal identification by exploring alternative or external instruments and robustness checks using GMM or system-based estimators.
3.2. Fully Modified Ordinary Least Squares (FMOLS)
The analysis employs the Fully Modified Ordinary Least Squares (FMOLS) estimator to examine the long-run relationship between life expectancy and its determinants. Developed by
Phillips and Hansen (
1990) and later extended to panel settings by
Pedroni (
2000,
2001), FMOLS corrects for endogeneity and serial correlation that typically arise in non-stationary macroeconomic panels. It applies semi-parametric corrections to both the bias in the OLS estimator and the long-run covariance matrix, yielding consistent and efficient parameter estimates even when regressors are cointegrated with the error term. This property makes FMOLS particularly suitable for the present 33-year (1990–2023) dataset, where education and health spending evolve gradually and may simultaneously influence life expectancy. Furthermore, FMOLS accommodates cross-country heterogeneity while maintaining comparability across income groups, allowing for a reliable estimation of equilibrium relationships. Its robustness to mixed order integration I(0) and I(1)) and long-run dependence justifies its application in assessing how fiscal allocations to education and health jointly influence sustainable improvements in population longevity (
Pedroni, 2004;
Kao & Chiang, 2000).
3.3. Bootstrap Estimation
To enhance the reliability of statistical inference, this study employs a bootstrap regression procedure based on a user-defined R-class program (lexpt_model) that returns the coefficients of interest from the life-expectancy equation. The program estimates a fixed-effects panel model and stores the resulting coefficients for education expenditure (EEXP) and government health expenditure (DGGHE) in r(b_eexp) and r(b_dgghe) for resampling. Bootstrap resampling was conducted at the country (panel) level to preserve within-group dependence and account for serial correlation. A total of 1000 iterations were performed, with each replication drawing a random sample (with replacement) of countries and re-estimating the model to generate an empirical distribution of the coefficients.
Inference relies on bias-corrected and accelerated (BCa) 95 per cent confidence intervals, which adjust for both bias and skewness in the bootstrap distribution, providing more accurate coverage probabilities than conventional percentile intervals. Reported standard errors and
p-values are therefore bootstrap-based, while the baseline specification and instruments remain constant across replications. This resampling design captures the sampling uncertainty associated with endogeneity, cross-sectional heterogeneity, and deviations from normal error distributions, yielding robust and stable inference for both the direct and indirect effects in the life-expectancy model. Following established econometric guidance (
Davidson & MacKinnon, 2007;
Godfrey, 2009;
Horowitz, 2018), the bootstrap implementation provides asymptotic refinements that improve the accuracy of hypothesis testing and confidence intervals relative to traditional parametric methods.
In this study, the bootstrap was used to obtain robust standard errors for the fixed-effects panel estimator while preserving the time-series structure within each country. Specifically, resampling was performed in a way that maintained the panel organization defined by the country–year structure, ensuring that each replication preserved the within-country dependence across time. Thus, the bootstrap procedure generated empirical distributions of the coefficient estimates based on repeated re-estimation of the panel model rather than reshuffling individual time observations.
3.4. Test for Stationarity (Unit Roots) and Cointegration
We must ensure that the variables are stationary or non-stationary before analyzing the long-run relationships between the variables in our panel data. We must apply panel unit root tests that account for the data’s time series and cross-sectional dimensions for panel data. We used the second-generation CIPS unit root test (
Pesaran, 2007) and the second-generation cointegration test (
Westerlund & Edgerton, 2007). Once we have established that the variables are non-stationary, we can apply a cointegration test to determine whether there are long-run relationships. If the variables are non-stationary but cointegrated, they imply a long-term equilibrium relationship. This test is preferred if we expect the long-run relationship to be homogeneous across panel units (i.e., the same for all cross-sectional units). We can apply 2SLS even if cointegration is found. If no cointegration is found, we may need to focus on short-run dynamics instead.
4. Descriptive Analysis
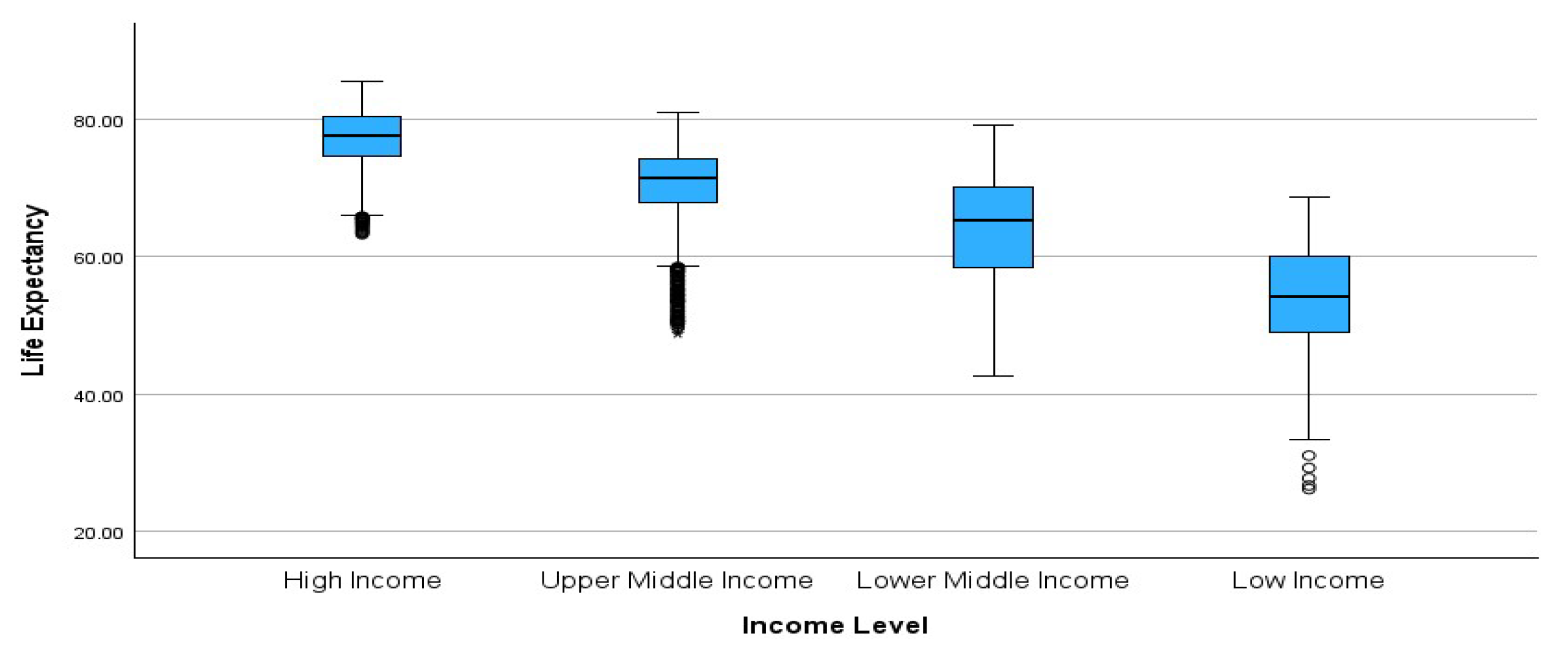
This boxplot (
Figure 1) aggregates life expectancy data across 34 years, showing the distribution of the values for each income group over time. It reflects both central tendency (median) and variation (spread and outliers), providing insights into how stable or volatile life expectancy has been within each group. For high-income groups, a high and stable life expectancy (median ~80 years) and a narrow interquartile range (IQR) suggest consistency over time and across countries. A few persistent low outliers may represent specific years or countries that experienced temporary setbacks (e.g., pandemics, political instability); however, these are exceptions, indicating strong healthcare systems, sustained investment, and high living standards over the 34 years.
For UMCs, the median is approximately 75 years, which is slightly lower than that for HICs, with a wider IQR indicating more within-group variation over time. Numerous low outliers suggest that some countries or years experienced shocks such as economic downturns or limited access to healthcare. Reflects progress, vulnerability to volatility in development and health outcomes. For LMCs, the median life expectancy is approximately 65–68 years, but there is a much wider range of values over these 34 years. Long whiskers and a broader IQR reflect significant differences between countries and over time; some improve rapidly, while others stagnate. This suggests the uneven development and implementation of health policies. For LICs, the median is the lowest (below 60 years), with a very broad IQR and extreme outliers (life expectancy in some years/countries is below 30). It shows high temporal and cross-country variability, indicating limited access to healthcare, ongoing crises, and developmental challenges. The pattern suggests gradual improvements, but it is still far from parity with the other groups (
Figure 1).
Income-based inequality in life expectancy has persisted for more than three decades. HICs have demonstrated sustained improvements in health, whereas LICs remain volatile and vulnerable to health issues. These disparities suggest the importance of targeted, long-term investments in education, healthcare infrastructure, and poverty reduction in low and middle-income countries. Over the past 34 years, the life expectancy gap between high- and low-income countries has remained substantial, although some convergence has been evident in middle-income countries. The distributional spread and outliers further reveal that economic status continues to shape health outcomes and, without consistent development policies, many low-income countries remain at risk of being left behind in terms of longevity and quality of life.
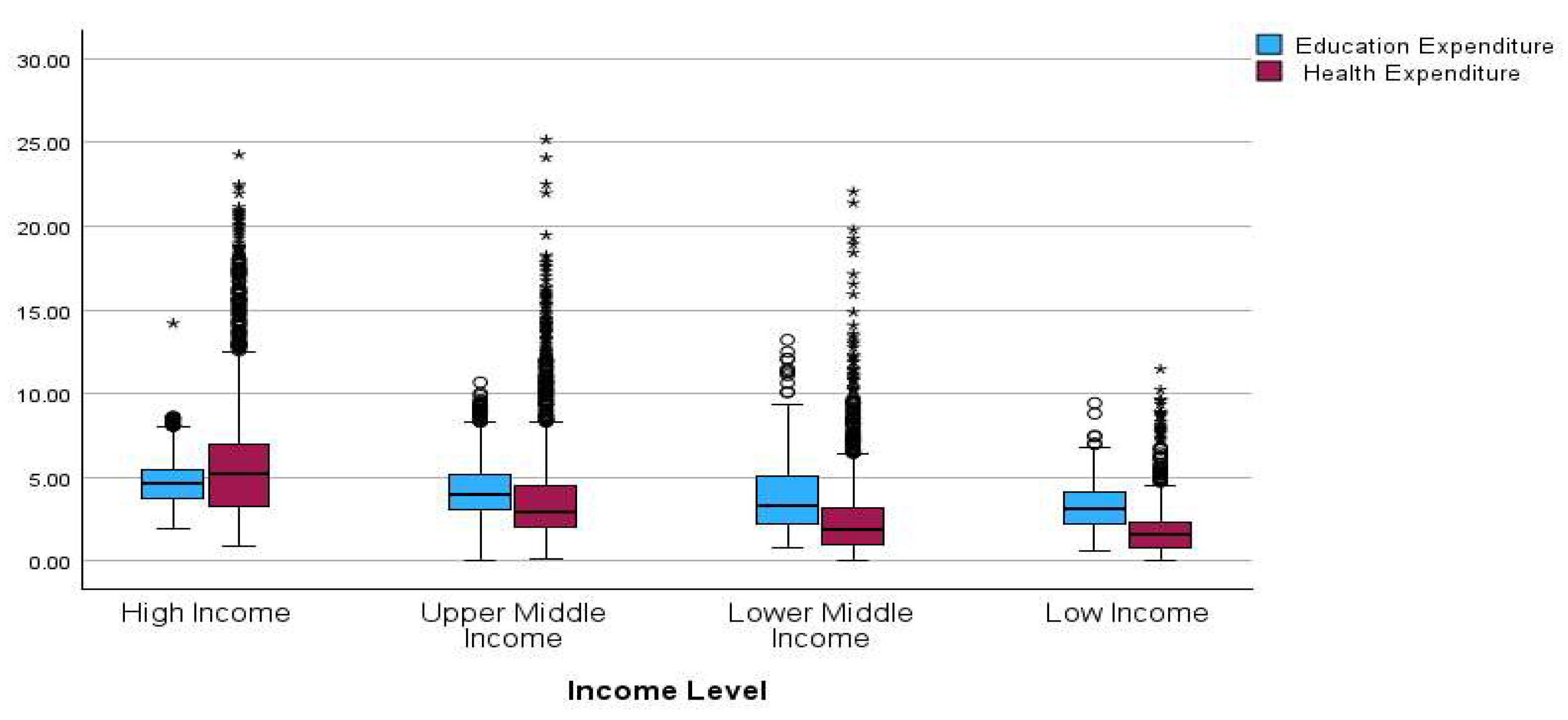
The boxplot (
Figure 2) compares Education Expenditure (blue) and Health Expenditure (purple) across the four income groups (HICs, UMCs, LMCs, and LICs) over the period 1990–2023. This visual approach provides valuable insight into spending patterns and resource allocation disparities. For HICs, the median health expenditure was higher than the median education expenditure, suggesting a more substantial allocation to health. Both types of expenditures showed higher values and more dispersion than the other groups. A high number of outliers (particularly in health) indicates that some countries or years have very high health spending, possibly because of aging populations or advanced healthcare systems.
For UMCs, the median education and health expenditures are relatively close, but health expenditures still slightly exceed those for education. The spread is narrower than that in HICs, although it still includes many outliers. Indicates increased health investment during economic transition, as well as some budget competition with education. For LMCs, both health and education expenditures have declined in median and spread, reflecting a limited fiscal space. Median education spending is now slightly higher than health spending, suggesting a potential crowding-out effect, in which education may be prioritized due to demographic youth bulges or education-driven development agendas. For low-income countries, the lowest medians are for both education and health expenditures. Education expenditure is slightly higher than health expenditure, and is more consistent across countries, with a narrower interquartile range (IQR). Health spending remains low with less variability, suggesting chronic underinvestment. This reflects severe budget constraints and possibly a trade-off in which basic education is prioritized over healthcare.
The inversion in spending patterns, from health > education in HICs to education > health in low-income countries, supports the crowding-out hypothesis. In LIC settings, where resources are limited, increased education expenditure may come at the cost of health expenditure, potentially hindering improvements in life expectancy, as seen in the earlier regression results. The fact that health spending increases significantly with income, while education spending shows much smaller variation, suggests that education may be treated as a fixed priority, while health investment is scaled with fiscal growth.
The chart confirms that resource allocation between education and health varies with income. In poorer countries, education typically receives a greater share. While investing in education is crucial, neglecting health spending can have long-term consequences on life expectancy and human capital. These findings underscore the importance of balanced, synergistic investments in both sectors, particularly LMCs, to prevent unintended crowding-out effects and promote sustainable development.
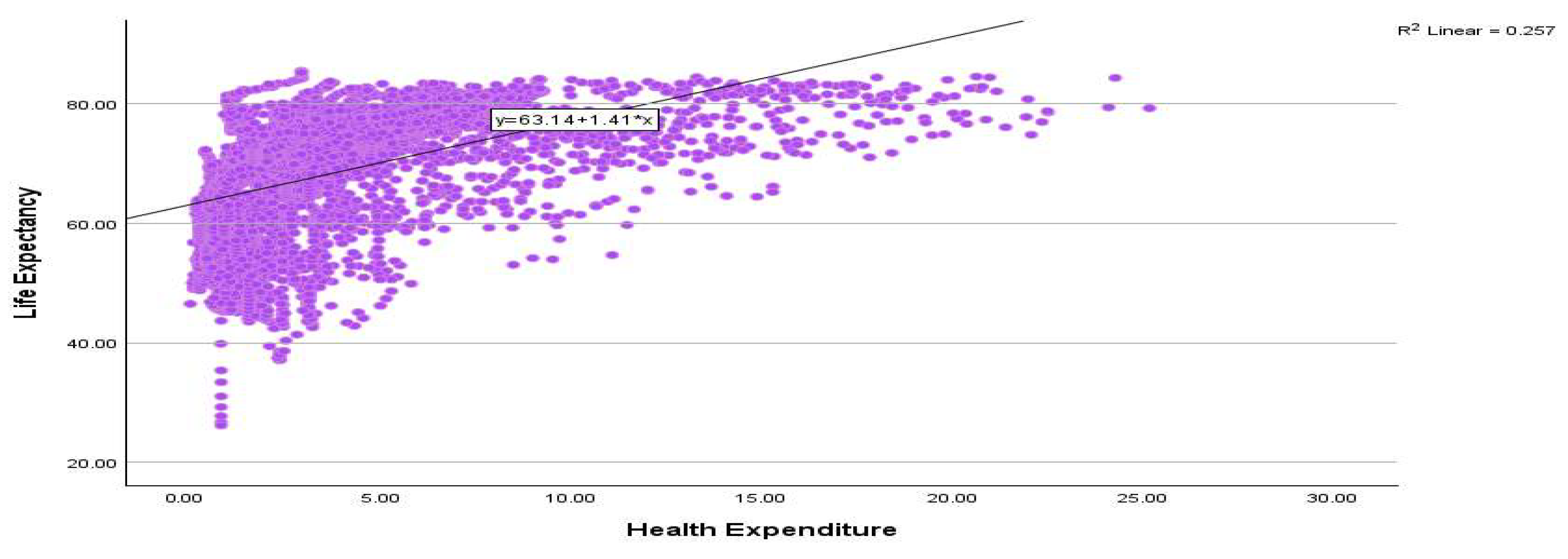
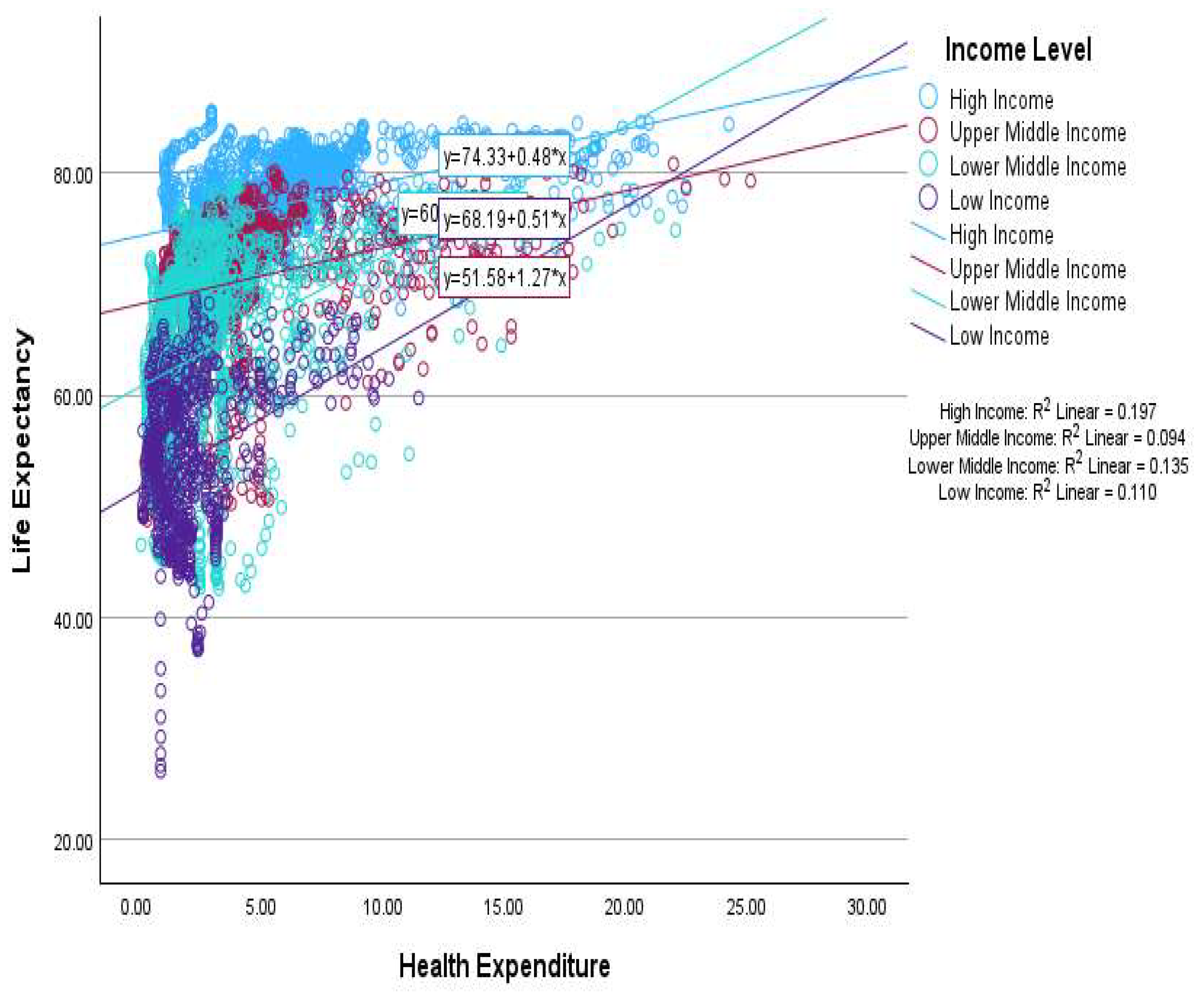
This scatter plot (
Figure 3) shows the relationship between health expenditures and life expectancy across countries or years, with a fitted linear regression line. Densely clustered points between 0 and 10 units of health expenditure indicate that most observations fall within the lower spending range, which is characteristic of low- and middle-income countries. Despite low spending, there is a wide range of life expectancies, indicating that health expenditure alone does not guarantee high life expectancy; efficiency, system quality, and other social determinants also play a role. The scatter shows diminishing returns at higher health expenditure levels; after a certain point (around 10–15 units), increases in spending yield smaller gains in life expectancy. This suggests that in HICs, where health systems are already well established, additional spending has a limited impact on improving life expectancy. The graph confirms that increased health expenditure generally leads to higher life expectancy, but with diminishing marginal returns.
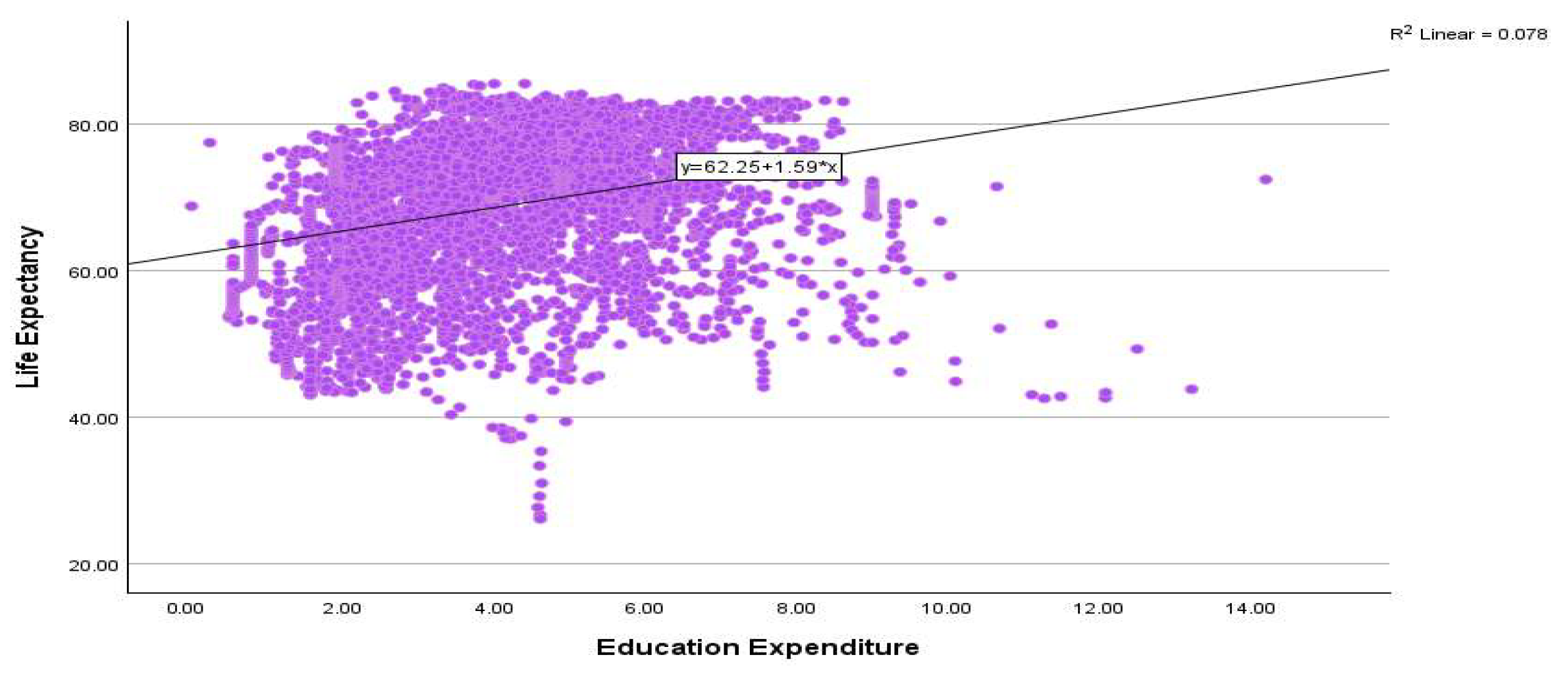
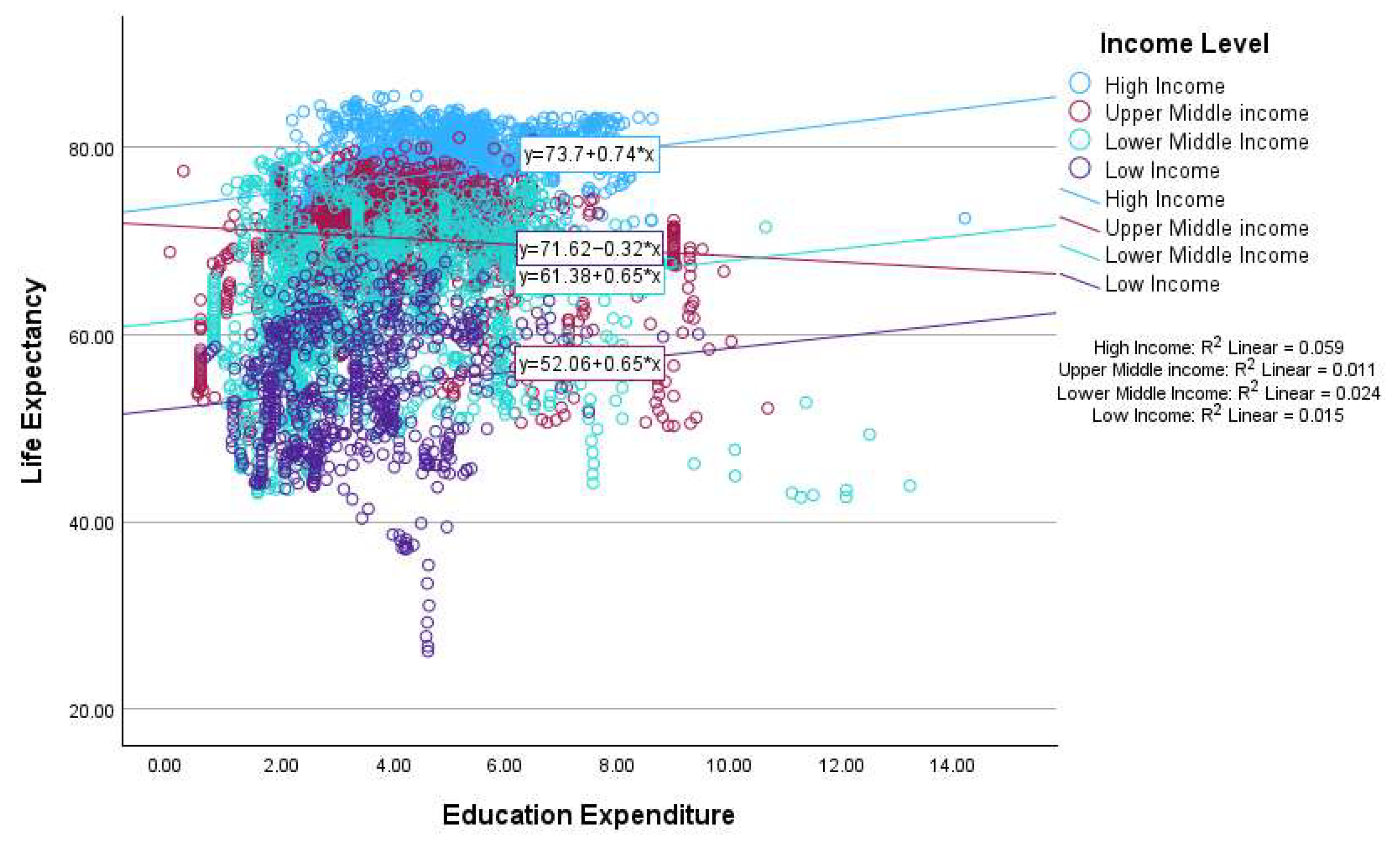
This scatter plot (
Figure 4) visualizes the relationship between Education Expenditure and Life Expectancy across countries or periods with a fitted linear regression line. Most data points are concentrated between 1% and 8% of education expenditure. There is a high degree of vertical spread (variance in life expectancy) for similar levels of educational spending, especially between 2% and 6%. This implies that other factors, such as health spending, income, governance, and inequality, play a significant role in determining life expectancy. Despite the low R
2, the positive slope of the regression line indicates that educational investment has a generally positive, albeit modest, relationship with life expectancy. However, the marginal return is inconsistent across the expenditure range, and there are several outliers with low life expectancy despite higher education spending, possibly due to poor health infrastructure or conflict. While the graph shows a positive correlation between educational expenditure and life expectancy, the relationship is weak and scattered. Education alone does not guarantee improved health outcomes unless complemented by sufficient health investment, economic stability, and social equity. This further supports earlier findings that in resource-constrained settings, prioritizing education may not automatically translate to a longer life, potentially contributing to a crowding-out effect on health-related gains if health spending is sidelined.
This scatter plot (
Figure 5) illustrates the relationship between Health Expenditure (
x-axis) and Life Expectancy (
y-axis) disaggregated by income level: HICs, UMCs, LMCs, and LICs. Each income group is color-coded and fitted with a separate linear regression line, accompanied by its Equation and R
2 value. For HICs, each 1-unit increase in health expenditure was associated with a 0.48-year increase in life expectancy. The R
2 value (19.7%) indicates a moderate correlation, suggesting that health spending contributes meaningfully, but not exclusively, to longevity. The slope is positive but lower than that in LICs, possibly because of diminishing returns in highly developed systems.
For UMCs,
Figure 5 shows a slope similar to that of HICs, but with a lower explanatory power (9.4%). This suggests that growing health expenditures support longevity, but other factors, such as inequality, governance, or education, remain influential. For LMCs, the slope is consistent with that of UMCs but with a lower intercept, indicating a shorter base life expectancy. R
2 (13.5%) showed a slightly stronger correlation than UMCs, implying that increased health spending yields more visible benefits in this group. Low-income countries have the steepest slope, meaning that every 1-unit increase in health expenditure corresponds to a 1.27-year increase in life expectancy. Although R
2 is still relatively low (11%), the high slope suggests strong marginal returns on health investment in resource-scarce environments. Positive Correlation Across All Groups: Health expenditure consistently correlates positively with life expectancy regardless of income level. LICs show greater gains per unit of spending as their health systems are underdeveloped and more responsive to investment. HICs experience smaller returns, consistent with saturation and a decline in marginal benefits; explanatory power increases with development. R
2 is the highest in HICs, indicating a more stable relationship between spending and outcomes. However, no group had an R
2 above 0.20, reinforcing the idea that health outcomes depend on a complex set of factors beyond just expenditure (e.g., efficiency, access, sanitation, education, and inequality).
This plot strongly supports the view that health expenditure has a positive influence on life expectancy, especially in low- and middle-income countries where systems are often underfunded. The marginal returns are highest in low-income settings, making it a strong case for prioritizing health spending in development policy. However, the low R2 values across all groups also highlight the need for multi-sectoral investment strategies—in education, infrastructure, and governance—to sustain health gains.
An overall scatter plot of income level (
Figure 6) for HICs reveals that educational expenditure has a positive and moderate effect on life expectancy, with a 1-unit increase associated with a 0.74-year increase in life expectancy. However, R
2 is low (5.9%), meaning that most of the variation in life expectancy is explained by factors other than education, such as health systems, income equality, and aging demographics. For UMCs, the slope is slightly negative, indicating a weak inverse relationship between education expenditure and life expectancy in this group. This may suggest a crowding-out effect, where increased education spending does not translate into immediate health benefits or where resource allocation shifts away from healthcare. The extremely low R
2 value indicates that educational spending has almost no explanatory power for life expectancy in this group. For LMCs, education spending shows a weak positive relationship with life expectancy but with minimal explanatory power (2.4%). This suggests that other developmental and structural factors dominate health outcomes in this income group. For low-income countries, a weak positive slope again indicates a marginal benefit of educational spending, albeit with a very low impact on life expectancy (1.5%). Given the low baseline and limited fiscal space, education expenditure may not be sufficient to produce noticeable improvements in life expectancy, unless accompanied by significant investments in the health sector.
In all income groups, education expenditure had limited explanatory power for life expectancy. Only HICs exhibited a reasonably positive slope, although the effect remained small. The R2 values were low across all groups, confirming that education alone cannot explain the variations in life expectancy. The slightly negative slope in the UMCs suggests a potential crowding-out effect, where education spending may displace health funding, especially in budget-constrained environments.
This graph reinforces the idea that, while education is important for long-term human development, its direct and immediate impact on life expectancy is limited, particularly in lower-income contexts. The crowding-out hypothesis is the most plausible in UMCs, where education may expand faster than complementary health systems, leading to decoupled or even adverse short-term effects on longevity. This suggests the need for balanced investment in both the education and health sectors to achieve sustainable improvements in population well-being.
Across all income groups, Pesaran’s CD test decisively rejects the null hypothesis of cross-sectional independence (Pr = 0.0000 in every case), implying a strong contemporaneous dependence among units within each group. The dependence is particularly pronounced for high- and upper-middle-income panels (statistics ≈84–171 and ≈27–132, respectively), substantial for lower-middle income (≈29–136), and smaller but still highly significant for low-income (≈14–46). Practically, this means that shocks are correlated across countries within each group (common factors/spillovers), so first-generation panel tests that assume independence are inappropriate. We should rely on second-generation methods that account for cross-sectional dependence, such as Pesaran’s CIPS, for unit roots. Most variables were integrated in order I(1) (
Table 2).
The results demonstrate that, across all income groups, health expenditure and life expectancy share a long-run equilibrium relationship, although the strength of the relationship varies. It is the strongest and most stable in high- and UMCs, while it is weaker but still present in low-income countries. This finding supports the idea that policies that increase health expenditure are linked to long-term improvements in life expectancy. However, the impact is more reliable in more developed economies, where health systems and resource allocation are stronger (
Table 3). Overall, the results confirm that the variables under study are cointegrated across all income groups, meaning that, despite being non-stationary in levels, they share a stable long-run relationship. This provides a robust basis for applying long-run estimation techniques, such as fully modified ordinary least squares (FMOLS), to analyze the dynamics between variables.
5. Regression Results
Table 4 presents the estimates of the health expenditure equation across four income groups—high-income (HICs), upper-middle-income (UMCs), lower-middle-income (LMCs), and low-income countries (LICs)—using two econometric approaches: Fully Modified Ordinary Least Squares (FMOLS) and Two-Stage Least Squares (2SLS). The explanatory variables include education expenditure (EEXP), inflation (INFL), urban population (URBP), GDP per capita (GDPC), unemployment (UNEM), and a time trend (TREND). The R-squared values reflect the explanatory power of the 2SLS models.
In HICs, both FMOLS and 2SLS indicate that education expenditure, inflation, and the trend variable have significant positive effects on health expenditure, though the magnitudes differ notably. Under 2SLS, the impact of education expenditure is much stronger (0.707), suggesting that higher education spending contributes substantially to rising health expenditure once endogeneity is accounted for. Urbanization, which is positive and significant in FMOLS, loses its significance in 2SLS, indicating that its apparent impact may be mediated through other economic channels. The sign reversal of GDP per capita from negative under FMOLS to positive under 2SLS underscores the bias correction achieved through instrumental variable estimation. The R-squared value of 0.3218 reflects a good model fit for this income group.
Among UMCs, the results are more variable. Under FMOLS, education expenditure, inflation and GDP per capita are negatively associated with health expenditure, while urbanization, unemployment, and the trend are positive and significant. In contrast, under 2SLS, education expenditure and inflation turn significantly positive, suggesting that once simultaneity is addressed, rising education investment and price levels both stimulate higher health spending. GDP per capita also becomes positive and weakly significant, while urbanization loses significance. Unemployment remains consistently positive and significant, and the trend coefficient increases further, indicating sustained upward pressure on health expenditure over time. The R-squared value of 0.3405 indicates a moderately strong fit.
For LMCs, FMOLS results show mixed effects—education expenditure, inflation, urbanization, unemployment, and the trend are all significantly positive, whereas GDP per capita is negative. However, under 2SLS estimation, all key variables, including GDP per capita, become positive and significant, confirming that economic growth and education investment are key drivers of rising health expenditure when endogeneity is properly controlled. The positive trend coefficient further indicates that long-term improvements in access, technology, or policy frameworks continue to push health expenditure upward. The R-squared of 0.3537 represents a relatively strong explanatory capacity for this group.
In LICs, both methods highlight education expenditure and the trend variable as consistently significant determinants of health expenditure. However, inflation and GDP per capita lose significance under 2SLS, while unemployment turns from negative in FMOLS to strongly positive in 2SLS, suggesting a shift once simultaneity and structural factors are accounted for. Urbanization remains statistically insignificant under 2SLS, implying limited urban effects in these economies. The relatively low R-squared (0.2653) points to a weaker fit, likely due to data limitations or greater heterogeneity in health financing systems.
Overall, the comparison across income groups and estimation methods suggests that education expenditure and economic growth are robust long-run drivers of health expenditure once endogeneity is corrected. Inflation and unemployment play secondary but context-dependent roles, often becoming more pronounced in middle- and low-income settings. The transition from FMOLS to 2SLS generally strengthens the explanatory power of the models, reinforcing the importance of accounting for simultaneity and omitted-variable bias in cross-country analyses of health spending.
Table 5 presents the estimates of the life expectancy equation across four income groups—HICs, UMCs, LMCs, and LICs—using two econometric techniques: FMOLS and 2SLS. The explanatory variables include education expenditure (EEXP), government health expenditure (DGGHE), income inequality (GINI), inflation (INFL), GDP per capita (GDPC), unemployment (UNEM), and a time trend representing technological or demographic changes.
In HICs, the FMOLS estimates show that education expenditure, health expenditure, income inequality, GDP per capita, and unemployment are positively and significantly associated with life expectancy. However, inflation and the trend variable are negative, implying that rising prices and potential structural changes may adversely affect longevity. Under 2SLS estimation, which accounts for endogeneity, education and health expenditures, and GDP per capita remain positive and significant, while income inequality and inflation exert significant negative effects. The unemployment effect becomes insignificant, and the trend turns positive, suggesting long-term improvements in living conditions. The 2SLS model exhibits strong explanatory power, with an R-squared of 0.5679.
For UMCs, FMOLS results reveal that education expenditure, inequality, GDP per capita, and unemployment have significant positive impacts on life expectancy, whereas health expenditure and the trend variable have negative effects. Inflation unexpectedly shows a positive relationship. When using 2SLS, the results become more consistent with theory: income inequality and unemployment show a significant negative impact, while government health expenditure and GDP per capita have strong positive influences. Education expenditure becomes weakly negative and insignificant, and the trend variable turns positive, indicating sustained progress in public health over time. The R-squared of 0.3124 indicates a moderate model fit.
In LMCs, FMOLS results show that education expenditure, inequality, GDP per capita, and unemployment are positively and significantly linked with life expectancy, whereas health expenditure and the trend variable are negative. Inflation exerts a mild positive effect. However, under 2SLS estimation, inequality and inflation display significant negative effects, emphasizing the adverse impact of inequality and price instability on population health. Health and education expenditures, as well as GDP per capita, retain positive and significant effects, while unemployment turns negative, suggesting that joblessness is associated with deeper socio-economic vulnerability. The 2SLS R-squared value of 0.4355 indicates reasonably good explanatory power.
In LICs, FMOLS results indicate that education expenditure, inequality, GDP per capita, and the trend variable positively affect life expectancy, while health expenditure and inflation have negative coefficients. Unemployment has a small but negative and significant coefficient. The 2SLS estimates, which better address endogeneity, show that GDP per capita continues to be a strong positive determinant of life expectancy, while income inequality exerts a significant negative influence. Education and health expenditures lose significance, suggesting their effects are indirect or constrained by resource limitations. Inflation turns positive but weakly significant, possibly reflecting nominal effects rather than real welfare improvements. The trend variable remains positive and robust, highlighting long-term progress. The R-squared of 0.5585 indicates a solid model fit for LICs.
Overall, the 2SLS results refine the FMOLS findings by revealing that once endogeneity is controlled, income inequality and inflation tend to reduce life expectancy across all income groups, while government health expenditure and GDP per capita consistently promote longevity. Education expenditure remains a critical but uneven determinant, with its influence diminishing in lower-income contexts where institutional and infrastructural limitations weaken the transmission of educational investment into health outcomes.
The bootstrap regression results (
Table 6) provide important insights into the relationship between public spending and life expectancy across the income groups. A key finding is the substantial and statistically significant impact of governmental health expenditure on life expectancy in all income categories. This effect is particularly pronounced in low-income countries, where a 1% increase in health spending is associated with a 0.035-year increase in life expectancy. The results clearly emphasize that government investment in health is a critical driver of longevity, particularly in settings where access to healthcare is limited and the disease burden is high.
By contrast, the relationship between education expenditure (EEXP) and life expectancy is more nuanced. In LMCs, EEXP shows a statistically significant positive effect with a coefficient of 0.045. This suggests that investments in education in these countries contribute significantly to improvements in public health, likely through mechanisms such as increased health literacy, improved sanitation practices, and enhanced maternal and child health behaviors. Education plays a complementary role in supporting health outcomes, reinforcing the argument that cross-sector investments can yield compounded social benefits.
However, for HICS and UMCs, the impact of education expenditure on life expectancy was statistically insignificant. In HICs, this may reflect a saturation effect, where additional spending on well-established education systems yields limited marginal returns in terms of health. In UMCs, the small positive but non-significant coefficient could indicate time lags or inefficiencies in how education funds are allocated. Meanwhile, in low-income countries, education expenditure has a negative, although statistically insignificant, relationship with life expectancy. This could be due to factors such as weak institutions, poor education quality, or misallocation of funds, and may also reflect a potential crowding-out of essential health investments when education is prioritized over more immediate health needs.
Overall, these findings underscore the importance of strategic context-sensitive public budgeting. While health spending is a universally effective policy lever for improving life expectancy, education spending requires targeted applications to yield health benefits. In LMCs, educational investment appears to significantly enhance life expectancy, while in low-income settings, improving life expectancy may depend more directly on direct health interventions. Policymakers should ensure that increases in education budgets do not occur at the expense of vital health services, particularly in resource-constrained environments. An integrated fiscal approach that considers both short-term health impacts and long-term educational benefits is essential for sustainable improvement in population well-being.
Sobel’s (
1982) z-test statistics are 9.62, 8.70, 7.68, and 3.07 for HICs, UMCs, LMCs, and LICs, respectively, indicating an indirect (mediated) effect. For every model, the product of the coefficients is positive, implying that higher education spending increases health spending, which in turn raises life expectancy; that is, a crowding-in rather than a crowding-out channel in these data. All four Sobel statistics exceed 1.96, and the corresponding
p-values are below 0.05; therefore, the mediated pathway is statistically significant in every specification (strongly so for Models 1–3 and moderately so for Model 4).
6. Conclusions and Policy Implications
This study examined whether education expenditure crowds out or complements health investment in influencing life expectancy across 158 countries from 1990 to 2023. Using FMOLS, 2SLS, and bootstrap estimation, the findings reveal a predominantly crowding-in relationship, though the magnitude of complementarity varies across income levels. Quantitatively, a 1% rise in education expenditure corresponds to a −0.003%, −0.005%, 0.045%, and −0.01% change in life expectancy in high-, upper-middle-, lower-middle-, and low-income countries, respectively. The Sobel tests (z = 9.62−3.07, p < 0.05) confirm that the indirect pathway operates mainly through increased government health expenditure, particularly in middle-income economies where fiscal and administrative structures allow education gains to translate into stronger health investment.
In interpreting these findings, it is crucial to recognize that education exerts both behavioral and productivity-based effects on health outcomes. Educated individuals are more likely to adopt preventive health behaviors, follow medical advice, and make informed lifestyle choices that reduce morbidity and mortality. At the same time, education enhances labor productivity and household income, enabling greater access to medical services and nutritious food, while improving governments’ fiscal capacity to finance health systems through higher tax revenues. These micro- and macro-level channels jointly explain the complementarity between education spending and health investment, reinforcing life expectancy through both human capital and fiscal pathways.
Descriptive evidence also indicates a nuanced form of the crowding-out effect, particularly in low-income and middle-income countries where fiscal space is limited. The comparative boxplot and scatter analyses reveal that as education expenditure rises relative to health spending, gains in life expectancy tend to diminish or plateau. In several upper- and lower-middle-income and low-income countries, the inversion of spending priorities—where education outpaces health—suggests a substitution mechanism rather than complementarity, reflecting budgetary trade-offs under constrained public finances. This displacement effect underscores that expanding education budgets without proportionate increases in health investment can attenuate the overall returns to human capital formation. In contrast, high-income countries maintain a balanced and mutually reinforcing allocation between the two sectors, minimizing such trade-offs. These findings highlight the importance of integrated fiscal design and coordinated sectoral policies that safeguard health investment while sustaining education-driven development, ensuring that progress in one dimension of human capital does not come at the expense of another.
From a policy perspective, this calls for joint expenditure frameworks that explicitly coordinate the sequencing of education and health investments. Governments should develop multi-sectoral budget planning processes and earmarked cross-sector funds—for example, for school-based immunization, adolescent nutrition, reproductive-health education, and health literacy campaigns—to institutionalize synergy rather than substitution between sectors.
The combined evidence from the health expenditure and life expectancy equations shows that education spending complements health investment, but the strength and direction of its effect depend on structural and macroeconomic contexts. In HICs, both education and public health expenditure positively influence life expectancy, while income inequality and inflation exert negative effects. This suggests that longevity gains at advanced stages of development stem less from new educational inputs and more from efficient health financing, social equality, and technological progress. Consistent with the bootstrap results, government health expenditure exerts a strong and highly significant positive effect on life expectancy in HICs, while the coefficient for education expenditure is negative and statistically insignificant, indicating that additional educational spending yields minimal health gains once a high level of human capital has already been achieved. Education’s direct effect on health expenditure remains positive but moderate, reflecting saturation in basic human-capital returns. Thus, policies should prioritize optimizing health-system performance—through digital health transformation, preventive care, and aging support—over expanding education budgets as a lever for additional life expectancy gains. Further, policy alignment mechanisms such as performance-based budgeting can ensure that incremental spending in one sector is contingent upon measurable gains in the other, promoting accountability and efficient resource allocation.
In UMCs, the results highlight a strong indirect complementarity between education and health. Under 2SLS, government health spending significantly raises life expectancy, while income inequality and unemployment reduce it. At the same time, education positively influences health expenditure once endogeneity is addressed. Consistent with the bootstrap results, government health expenditure exerts a strong and significant positive effect on life expectancy in UMCs, while the coefficient for education expenditure is positive but not statistically significant, suggesting that health outcomes in this group rely more on efficient health financing than on additional educational spending. This underscores governance and fiscal management as the main transmission channels. Policymakers should strengthen institutional linkages between education-driven capacity building and efficient health-sector spending. Establishing joint monitoring frameworks—for example, pairing literacy and maternal-health coverage targets—can ensure that rising educational attainment translates into tangible health improvements. Additionally, targeted inter-ministerial coordination units could be created to align educational and health objectives, harmonizing data collection, budget execution, and outcome evaluation across ministries.
In LMCs, both education and health expenditures remain robust and mutually reinforcing drivers of life expectancy. Once endogeneity is controlled, GDP per capita and public health expenditure exert strong positive effects, while inequality and inflation diminish longevity. Consistent with the bootstrap results, both government education and health expenditures show large and highly significant positive coefficients, indicating that increases in either domain yield substantial and complementary improvements in life expectancy in LMCs. The positive and significant influence of education expenditure on both health spending and life expectancy implies a synergistic cycle between knowledge accumulation and health improvement. Policy should therefore encourage co-financing mechanisms, such as school-based health and nutrition programs, integrated community-education initiatives, and joint budget planning between education and health ministries, ensuring that fiscal expansion in one sector amplifies the other rather than competing with it. Governments could also introduce conditional intergovernmental transfers that reward local administrations for achieving joint education–health outcomes, promoting horizontal accountability and effective resource sharing.
Based on the 2SLS estimates, GDP per capita emerges as the principal and most robust determinant of life expectancy in low-income countries. The positive and statistically significant coefficient (0.040, p < 0.01) indicates that higher income levels are closely linked to longer life expectancy, even after accounting for endogeneity. This highlights the critical role of economic growth in enhancing health outcomes through improved access to nutrition, healthcare, and living standards. Consistent with the bootstrap results, government health expenditure exerts a strong and significant positive effect on life expectancy, while education expenditure remains negative and statistically insignificant, suggesting that in LICs, health gains are driven more by direct public health investment than by additional educational spending. Although the direct effect of education expenditure on life expectancy is relatively modest, its positive influence suggests that investment in education can complement income growth by promoting healthier behaviors, better health awareness, and more effective use of healthcare services. Therefore, policies should aim to integrate education and economic strategies—fostering income-generating opportunities while simultaneously expanding access to quality education—to create mutually reinforcing pathways toward higher life expectancy and overall human development.
Synthesizing across income groups, the results confirm that education and health expenditures are fiscal complements rather than rivals, but their interaction is conditioned by fiscal capacity, inequality, and macroeconomic stability. In high- and middle-income settings, education enhances health outcomes through institutional and behavioral pathways—improved literacy, better health awareness, and stronger fiscal capacity. In low-income economies, the same mechanism operates only after a critical threshold of health infrastructure and governance quality is achieved.
Accordingly, governments should adopt integrated budgetary frameworks that align education and health priorities. Medium-term expenditure strategies should include safeguard clauses ensuring that proportional adjustments match increases in education budgets and health spending. Establishing cross-sector funds—for instance, for school-based immunization, reproductive-health education, and sanitation programs—can institutionalize long-run complementarity. Moreover, performance-based budgeting should link disbursements to joint sectoral outcomes, such as improvements in health literacy, disease-prevention coverage, and student well-being. To strengthen implementation, public financial management reforms should embed joint program evaluation criteria and require inter-ministerial consultation before major expenditure reallocations, thus reducing the risk of resource crowding-out between education and health sectors.
The findings directly address the study’s core research questions concerning whether education expenditure crowds out or complements health investment in determining life expectancy. The evidence supports the complementarity hypothesis, showing that education spending generally enhances health investment and longevity rather than displacing healthcare expenditure. Quantitatively, the positive coefficients of education expenditure on life expectancy from 2SLS across all income groups, coupled with significant indirect effects via health expenditure (Sobel z = 3.07–9.62, p < 0.05), confirm that education promotes both behavioral and fiscal pathways to better health outcomes. The results refine the first hypothesis by revealing that the crowding-out effect emerges only in fiscally constrained low-income contexts, while the second and third hypotheses are validated by the strong direct and mediated impacts of education on life expectancy through increased health spending in middle-income countries. Thus, the study concludes that education and health are mutually reinforcing dimensions of human capital, and their integration within coordinated fiscal frameworks is key to maximizing gains in population longevity and sustainable development.
Future research should refine this understanding by exploring nonlinear and threshold dynamics between education and health spending—testing whether the crowding-in effect weakens or reverses beyond certain income or expenditure levels. Advanced econometric techniques such as panel smooth-transition regressions (PSTR) and dynamic stochastic general equilibrium (DSGE) models could help capture these inter-sectoral feedbacks. Additionally, spatial econometric frameworks would allow examination of cross-border spillovers in education–health linkages, especially among developing regions where policy diffusion is common. Further, investigating behavioral micro-foundations—such as how literacy levels influence preventive care uptake or healthcare utilization—would deepen understanding of the mechanisms driving the education–health nexus. Future research could extend this analysis by comparing results using alternative fiscal indicators—such as education expenditure as a percentage of government expenditure or per capita terms. Such extensions would allow a deeper understanding of how government prioritization interacts with overall economic capacity, providing a more comprehensive picture of fiscal commitment to education across countries and over time.
In conclusion, the study demonstrates that while education and health expenditures are mutually reinforcing investments in human capital, their synergy depends on income level, governance quality, and macroeconomic stability. The indirect, fiscal-behavioral effects of education spending on life expectancy are stronger than its direct effects, confirming the pivotal role of health expenditure as the main conduit of longevity gains. Sustainable progress, therefore, requires coordinated fiscal strategies that preserve the integrity of the health sector while leveraging education’s transformative potential to achieve inclusive and long-term improvements in population well-being. Ultimately, an integrated human capital strategy—anchored in balanced financing, joint accountability, and cross-sector policy design—offers the most viable pathway to ensure that education and health together serve as enduring pillars of economic and social resilience.