Abstract
Pulmonary arterial hypertension (PAH), the first category of pulmonary hypertension, is a chronic and progressive disorder characterised by angioproliferative vasculopathy in the pulmonary arterioles, leading to endothelial and smooth muscle proliferation and dysfunction, inflammation and thrombosis. These changes increase pulmonary vascular resistance and subsequent pulmonary arterial pressure, causing right ventricular failure which leads to eventual death if untreated. The management of PAH has advanced rapidly in recent years due to improved understanding of the condition’s pathophysiology, specifically the nitric oxide, prostacyclin-thromboxane and endothelin-1 pathways. Five classes of drugs targeting these pathways are now available: phosphodiesterase-5 inhibitors, soluble guanylate cyclase stimulators, prostacyclin analogues, prostacyclin receptor agonists and endothelin receptor antagonists. These developments have led to substantial improvements in mortality rate in recent decades. Recently, long-term studies have demonstrated sustained progression-free survival and have created a new paradigm of initial combination therapy. Despite these targeted therapies, PAH is still associated with significant morbidity and mortality. As such, further research into broadening our understanding of PAH pathophysiology is underway with potential of increasing the repertoire of drugs available.
1. Introduction
Pulmonary hypertension (PH) consists of a group of diseases with a resting mean pulmonary artery pressure (mPAP) ≥ 25 mmHg as measured with right heart catheterization [1]. Since 1998, major revisions in the classification of PH have categorised the disease based on the anatomical site and aetiology. The latest revision, in 2013, is shown in Table 1.

Table 1.
Classification of pulmonary hypertension [1].
PH is considered a rare disease, with a population-based study in the Netherlands suggesting a prevalence rate of 2.6% based on echocardiographic findings [2]. According to one Australian cohort study, PH secondary to left heart disease was the subtype with the greatest prevalence but also conferred the highest mortality, followed by PH secondary to respiratory diseases [3].
Group 1 of PH is pulmonary arterial hypertension (PAH), which is defined as mPAP ≥ 25 mmHg, pulmonary artery wedge pressure (PAWP) ≤ 15 mmHg and pulmonary vascular resistance (PVR) > 3 Wood units [1]. PAH is further subcategorised according to its aetiology, with idiopathic PAH (iPAH) comprising the majority of cases, followed by PAH associated with connective tissue diseases (CTD) and congenital heart disease (see Table 1) [4]. In PAH, the pre-capillary arterioles are affected by an angioproliferative vasculopathy that increases the pulmonary vascular resistance, thereby increasing the right ventricular afterload with the resulting right heart failure being the ultimate cause of mortality [5]. When adequately treated, PAH exhibits the best prognosis when compared to other PH categories according to the aforementioned Australian study [3].
According to registries in the United Kingdom, the reported incidence and prevalence rates of PAH are 1.1–2.4 and 6.6–15.0 cases per million per year, respectively [6]. Contemporary data from the 2014 UK National Audit on Pulmonary Hypertension found that the median age of diagnosis of PAH was 60 years in females and 58 years in males, with more than 25% of patients being over 70 years—thereby refuting previous conceptions of PAH being a disease of the young [7]. Data from the United States-based registry to evaluate early and long-term pulmonary arterial hypertension disease management (REVEAL registry) demonstrated certain sex preponderances for specific subtypes of PAH, such as a greater female distribution in iPAH [8]. Males demonstrated a lower survival rate at both two and five years post-enrolment; however, subanalysis showed similar survival rates between women and men <60 years at enrolment but poorer survival rates in men >60 compared to women [8]. Overall median survival rates have improved dramatically over the past two decades (from 2.8 to 7 years in the aforementioned American registry), presumably due to a combination of significant advances in treatment strategies and patient support strategies [9].
2. Risk and Prognostic Factors of PAH
Drugs, toxins, CTD and certain infections (such as HIV and schistosomiasis) have been strongly associated with PAH, and have thus appeared as subcategories in the classification [10,11]. The drugs and toxins considered as definite risk factors include aminorex, fenfluramine, dexfenfluramine and selective serotonin reuptake inhibitors (SSRIs) [10]. In particular, iPAH has been found to be strongly associated with female gender, family history and genetic variants, especially bone morphogenetic protein receptor type 2 (BMPRII) mutations [4,12].
Prognostic stratification of PAH in clinical practice requires extensive assessment and investigation at specialised PH centres. As highlighted in Table 2, the 2015 ESC/ERS (European Society of Cardiology and the European Respiratory Society) guidelines recommend a series of variables to stratify patients into low, intermediate and high-risk categories (corresponding to an estimated one-year mortality rate of <5%, 5–10% and >10% respectively) which subsequently guides management [13]. These variables include an assessment of clinical function, World Health Organisation functional class (WHO-FC), exercise capacity and right ventricular function, with the WHO-FC segregating PAH patients into four categories based on their physical capacity impairment and dyspnea [13,14]. These variables are measured through a combination of imaging (echocardiography, cardiac magnetic resonance imaging), haemodynamics (e.g., right atrial pressure, cardiac index, mixed venous oxygen saturation), exercise testing (e.g., 6-minute walking test, cardiopulmonary exercise testing) and biochemical markers (markers of vascular dysfunction, myocardial stress, low cardiac output and secondary organ damage) [13,14]. Other factors such as age, sex, PAH subtype and symptomatic features of heart failure should be considered in prognostic evaluation, although their importance is largely determined on a case-by-case basis supplemented with clinical expertise [13].

Table 2.
Prognostic risk stratification of pulmonary arterial hypertension. Adapted from 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension [13].
3. Genetics
Heritable PAH (hPAH), a subcategory of PAH, exhibits an autosomal dominant pattern of inheritance, with several associated germline gene mutations having been identified [15]. These mutations primarily occur in the genes encoding the transforming growth factor β (TGF-β) receptor superfamily, namely BMPRII [16], activin receptor-like kinase 1 (ALK1) [17], mothers against decapentaplegic homolog 9 (SMAD9) and endoglin 1 (ENG) [16,17,18]. Approximately 70% of hPAH patients [15], and a minority (10–40%) of patients with apparently sporadic iPAH [19], have mutations in the BMPRII; in comparison to mutations in ALK 1, SMAD9 and ENG, which collectively appear in only 5% of the hPAP population [15,19,20]. Though hPAH was previously considered to exhibit genetic anticipation (i.e., earlier age of onset and death in consecutive generations), recent data has challenged this conclusion [21].
Diagnosis of hPAH is complicated by the incomplete penetrance of BMPRII mutations, with only 20% of individuals possessing disease-associated variants developing the condition [21]. Furthermore, the variable expressivity and female predominance of these gene variants reveal the combination of genetic, genomic and environmental factors in PAH pathogenesis [21,22].
The most commonly studied gene mutation in relation to PAH pathogenesis is with BMPRII. Animal models demonstrate that reduced BMPRII activity in pulmonary vascular endothelial cells increases the incidence of apoptosis, leading to vascular remodelling and ultimately PAH [23,24]. Additionally, improving BMPRII expression in mice models through microRNA inhibition limits endothelial dysfunction and attenuates hypoxia-induced PAH [25].
Though genetic testing for hPAH is available, this service should be offered by trained individuals to those patients with iPAH considered to be sporadic or induced by anorexigens and to patients with a family history of PAH [13]. Ethical principles of genetic testing must include, among others, preserving patient and family autonomy, avoiding harm, and allowing equal access to genetic counselling for all patients. As outlined previously, the variable penetrance and expressivity of the BMPRII mutations may cause genetic testing to identify variants of unknown clinical significance, thereby causing unnecessary anxiety. Nonetheless, genetic testing is available which involves initial testing of only BMPRII variants, with negative results prompting further investigation of rarer pathogenic mutations (e.g., ALK1 and ENG) [13].
4. Pathophysiology
PAH may be idiopathic or secondary to various conditions, but regardless of the underlying aetiology, patients exhibit similar pathological changes which include enhanced pulmonary arteriole contractility, endothelial dysfunction, remodelling and proliferation of both endothelial and smooth muscle cells, and in situ thrombi [5]. The physiological outcome of these disturbances is the partial occlusion of small pulmonary arteries, eventuating in increased PVR, subsequent right ventricular failure and death [5].
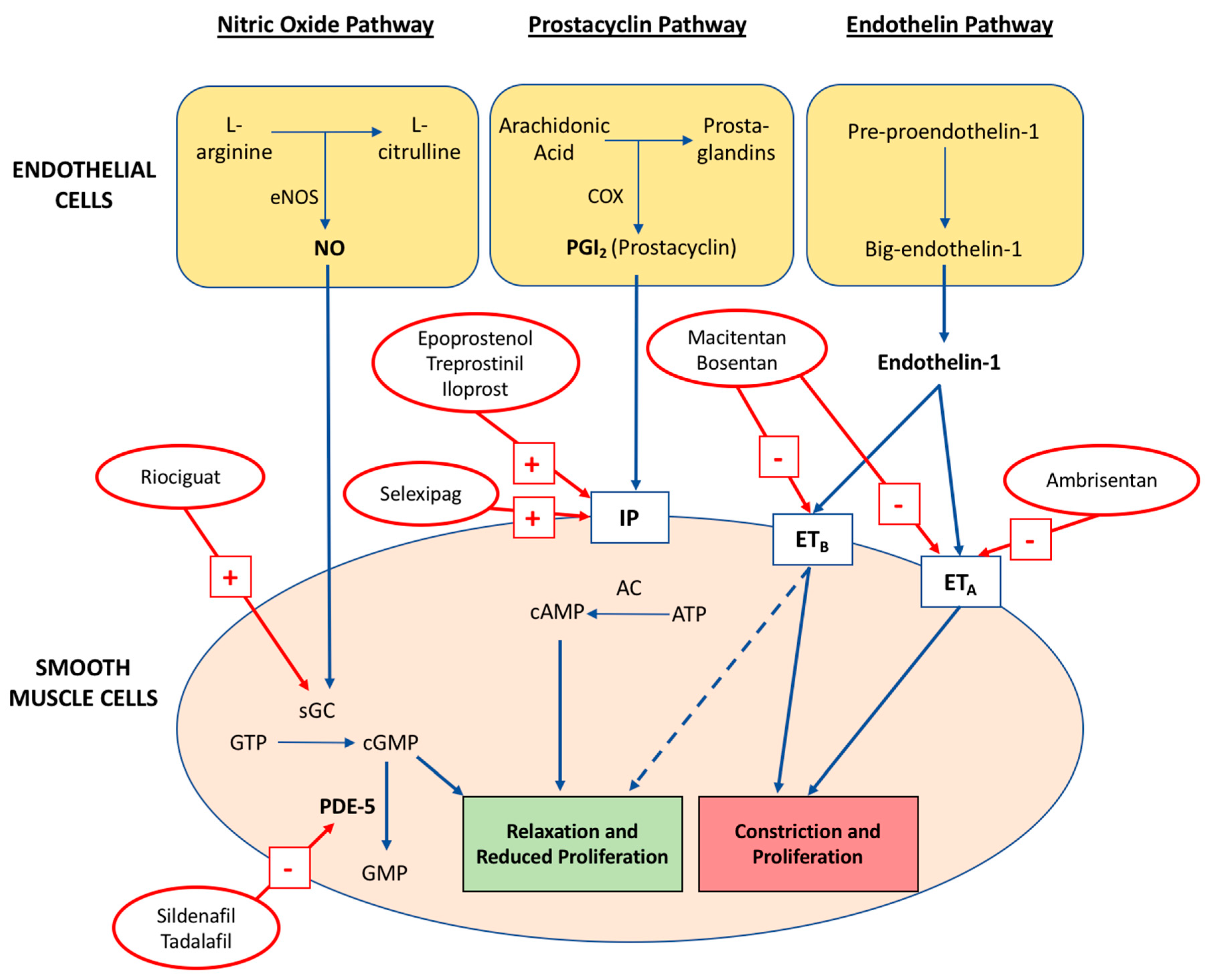
Underpinning these progressive pulmonary vascular defects is the disruption of three key signalling pathways outlined in Figure 1: nitric oxide (NO), prostacyclin (PGI2) and thromboxane A2 (TXA2), and endothelin-1 (ET-1) [26]. Broadly speaking, PAH is caused by impaired vasodilation from reduced PGI2 production (cyclooxygenase-2 dysregulation) and NO synthase (eNOS) function, with concurrent vasoconstrictive and mitogenic effects of an upregulated ET-1 signalling system [26,27]. A mechanistic understanding of these three pathways has prompted rapid development in the quantity and efficacy of targeted pharmacological therapies for PAH.
Figure 1.
The key abnormal pathways targeted in the pharmacological treatment of pulmonary arterial hypertension and the mechanism of action for contemporary drugs. The dashed line from ETB denotes action of endothelial ETB activation via NO and PGI2 production. Adapted from Prior et al. MJA 2016 [28].
4.1. Nitric Oxide Pathway
Nitric oxide is produced in endothelial cells by eNOS, which, in the presence of oxygen, NADPH and other cofactors, catalyses the oxidation of l-arginine to l-citrulline. NO diffuses into the underlying pulmonary vascular smooth muscle cells (PVSMC) and binds to soluble guanylate cyclase (sGC), which in turn, converts guanosine triphosphate (GTP) to cyclic guanosine monophosphate (cGMP). The subsequent activation of downstream cGMP-dependent protein kinases (PKG) results in pulmonary vasodilation. Additionally, NO inhibits PVSMC proliferation, platelet aggregation and thrombosis, collectively maintaining normal healthy pulmonary vasculature.
In PAH, there is decreased bioavailability of NO, causing vasoconstriction and increased smooth muscle cell proliferation, inflammation and thrombosis. Although these pathological changes were initially attributed to observed reductions of eNOS expression amongst PAH patients, more recent studies have demonstrated similar outcomes from persistent eNOS activation in mice and human models [27,29]. A potential explanation for this apparent contradiction is the role of reactive oxygen species (ROS), particularly tetrahydrobiopterin (BH4), in the enzymatic uncoupling of eNOS, thereby accounting for the pathogenesis of endothelial dysfunction, vasoconstriction and vascular remodelling in these models [30].
There are currently two approved drug classes acting on the nitric oxide pathway: phosphodiesterase 5 inhibitors (PDE-5i) and guanylate cyclase (GC) stimulators. PDE-5i prevent the degradation of cGMP, thereby increasing its plasma concentration and promoting the vasodilatory and antiproliferative effects of NO. GC stimulators act directly on sGC, even in the absence of NO, conferring similar increases in cGMP concentration.
4.2. Prostacyclin-Thromboxane A2 Pathway
Prostacyclins are produced in endothelial cells from arachidonic acid via cyclooxygenase and prostacyclin synthase. PGI2 binds to specific I-prostanoid (IP) receptors in smooth muscle cells, thereby activating adenylate cyclase. This enzyme converts adenosine triphosphate (ATP) to cyclic adenosine monophosphate (cAMP), which ultimately causes smooth muscle relaxation and subsequent vasodilation. Prostacyclin inhibits platelet aggregation, attenuates smooth muscle proliferation, and produces anti-inflammatory and antithrombotic effects.
In PAH, the pathway shifts towards an alternative product, thromboxane A2, leading to platelet aggregation, vasoconstriction and proliferation [31]. The aetiological role of prostacyclin is evidenced by animal models, with IP-knockout mice exhibiting severe PAH and subsequent vascular remodeling when subjected to chronic hypoxia [32]. Furthermore, patients with PAH have reduced production of prostacyclins as well as reduced expression of prostacyclin receptor and prostacyclin synthase [33].
The clinical drugs developed for PAH therapy that act on the prostacyclin pathway are the prostacyclin analogues and receptor agonists.
4.3. Endothelin-1 Pathway
Endothelin-1 (ET-1) is a peptide that acts as a potent vasoconstrictor [34]. ET-1 is produced on endothelial cell membranes from the precursor peptide big-endothelin-1 by endothelin-converting enzymes. ET-1 activates ETA and ETB: two G-protein coupled receptors. ETA is found on vascular smooth muscle cells, and promotes vasoconstriction, hypertrophy, proliferation, cell migration and fibrosis when activated. ETB is located on both vascular smooth muscle and endothelial cell surfaces. On smooth muscle, activation of ETB causes vasoconstriction whilst on endothelial surfaces, ETB activates NO and prostacyclin production, causing vasodilation and anti-proliferation [35].
During PAH, there is an increase in expression of ETA and smooth muscle ETB, but reduced expression of endothelial ETB [35]. In addition, PAH patients exhibit increased ET-1 concentrations in their plasma and pulmonary vascular endothelial cells [36,37]. The pathological alterations to this pathway are counteracted by endothelin receptor antagonists (ERAs), which are available as ETA selective or dual-action on ETA and ETB receptors.
5. Management of PAH
Treatment of PAH has progressed significantly over the past few decades in both its complexity and efficacy [38,39]. The aim of therapy is to achieve a low-risk status (maintaining WHO-FC II if possible) to preserve patient function, quality of life and minimise mortality risk [13]. This is generally achieved by optimising the patient’s six-minute walk distance (6MWD); however, current target thresholds rely upon cohort studies and expert consensus [40,41].
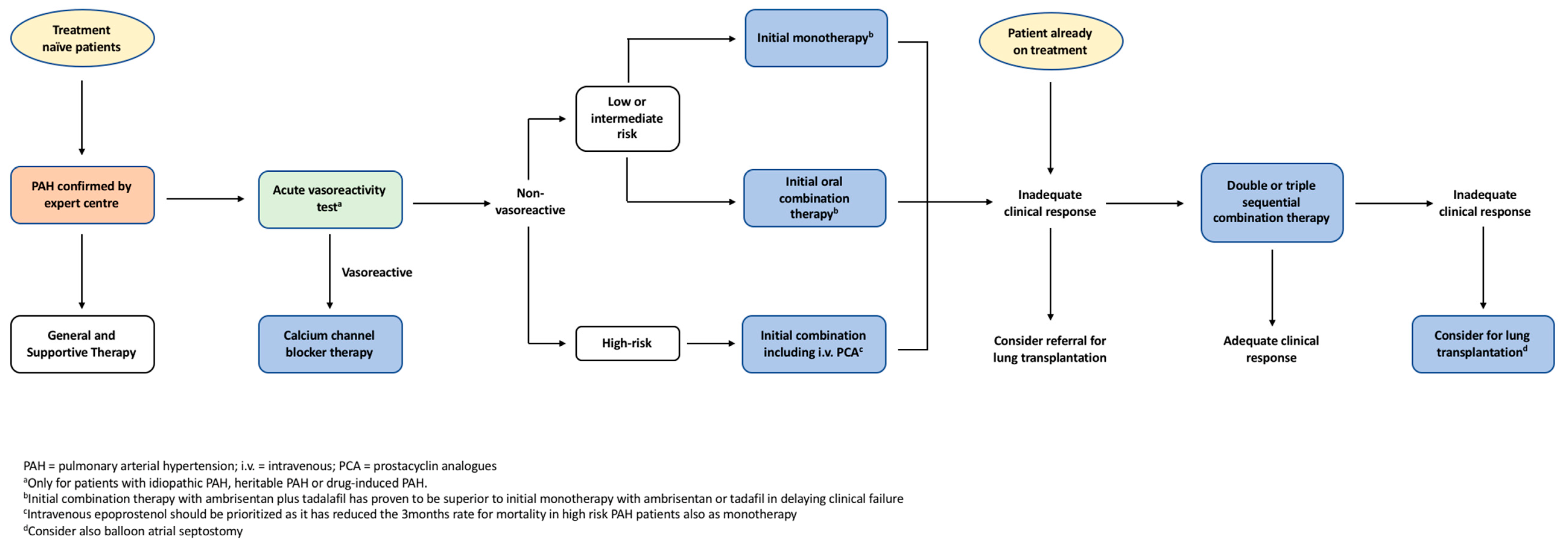
PAH management involves a stepwise pragmatic approach from general supportive treatment up to targeted pharmacological interventions as outlined in Figure 2. Selected patients undergo vasoreactivity testing, with those that exhibit sufficient vasodilation subsequently being commenced on regular high-dose calcium channel blockers (CCB) [13]. Patients who either fail to qualify for vasoreactivity testing or demonstrate inadequate response are then commenced on targeted monotherapy or combination therapies that counteract the pathophysiology of the condition.
Figure 2.
The European Society of Cardiology and the European Respiratory Society (ESC/ERS) evidence-based treatment algorithm for pulmonary arterial hypertension patients. Adapted from ECS/ERS guidelines for the diagnosis and treatment of pulmonary hypertension [13].
5.1. General and Supportive Therapies
Supportive care remains the mainstay of PAH management despite insufficient and heterogeneous data supporting these practices [13]. These measures (supervised physical exercise, pregnancy avoidance, appropriate birth control, oxygen supplementation, diuretics, digoxin, oral anticoagulation, psychosocial support, genetic counselling) serve to provide symptomatic relief or minimise the morbidity associated with this condition.
Patients with PAH are recommended to engage in physical activity as permitted by their symptomatic control, with supervised rehabilitation performed at specialist centres for deconditioned patients [13]. The benefit of physical activity is elucidated by a randomised controlled trial (RCT) of 30 patients with optimal medical control, with the exercise group demonstrating improved exercise capacity, 6MWD, quality of life, functional status and oxygen consumption levels compared to non-training controls [42]. Subsequent RCTs have similarly found exercise training to improve fatigue levels, 6MWD and patient quality of life [43,44]. These recommendations are hampered by the limited study sample sizes (the largest having 183 patients), unknown prognostic implications and the lack of direct comparison between different exercise regimes.
Pregnancy, due to its associated high mortality and morbidity in PAH, is not recommended [13,45]. Additionally, pregnancy reduces the range of drugs available for PAH treatment since ERAs are formally contraindicated given their teratogenicity [46,47]. Recent registry data suggest treatment advancements may have partially ameliorated this burden, particularly amongst CCB-managed patients, but there are insufficient extensive, long-term trials to amend current pregnancy recommendations [48].
Appropriate birth control measures are an area of inquiry with less consensus. Barrier methods and progesterone are recommended and often used in combination, while oestrogens are used cautiously due to the risk of venous thromboembolism, pulmonary vascular effects and reduced efficacy due to drug–drug interactions with the ERA bosentan [49]. Should pregnancy continue despite education concerning high maternal and fetal risks, patients should receive disease-specific therapy and elective delivery with support from a PAH specialty team [50].
Hypoxia causes significant pulmonary arterial vasoconstriction and oxygen therapy has been demonstrated to reduce PVR in PAH patients [51]. However, there are no long-term randomised trials that evaluate the effects of oxygen, but expert consensus recommends sufficient supplementation to maintain saturation levels above 90% [52].
Optimising intravascular fluid status through the appropriate administration of diuretics reduces right ventricular (RV) dilatation, hepatic congestion, ascites and oedema. Despite this theoretical rationale, no RCTs have investigated the role of diuretics in PAH, thus the type and dosage of diuretics is largely left to clinical discretion [13].
Digoxin acutely improves cardiac output in iPAH patients, but its long-term use remains controversial since there is no data concerning chronic effects or clinical benefit [53]. Angiotensin converting enzyme-inhibitors, angiotensin receptor blockers, beta-blockers and ivabradine are not routinely recommended in the absence of associated comorbidities [13].
Given observed abnormalities in coagulation and fibrinolytic pathways in PAH patients, oral anticoagulation is currently recommended in patients with iPAH, hPAH or PAH secondary to anorexigens, based primarily upon short-term, single-centre retrospective studies [13,54,55,56,57,58]. However, the limited registry and RCT evidence available is inconclusive, heterogeneous and to-date has not examined the role of the new oral anticoagulant agents [54,57,58]. Anticoagulation is not recommended in other subtypes of PAH [13].
Multidisciplinary teams at specialised PH clinics provide a holistic approach to manage all aspects of patient care. Psychosocial counselling and patient support groups are effective for minimising the psychological, social, financial, spiritual and emotional impact on patients and their families [59,60]. As previously discussed, the option to provide genetic counselling to eligible patients is offered when medically and ethically appropriate [13].
5.2. Calcium Channel Blockers
Calcium channel blockers (CCB) inhibit the inflow of calcium into smooth muscle cells, thereby causing vasodilation. Most PAH patients demonstrate minimal response to acute vasodilatory challenges during right heart catheterisation testing; however, some patients demonstrate vasodilation to normal or near-normal pressures. In some of these patients, ongoing high-dose CCBs can have dramatic improvements with sustained haemodynamics to near physiological values [61]. Long-term response to CCB is most commonly observed in iPAH patients [61]. In contrast, patients with PAH associated with CTD, HIV, Portopulmonary hypertension (porto-pulmonary-HTN) and Pulmonary veno-occlusive disease (PVOD) exhibit poor long-term CCB efficacy, even in the presence of positive vasoreactivity testing [62]. Therefore, the ESC/ERS guidelines recommend pulmonary vasoreactivity testing in iPAH, hPAH and drug induced PAH patients [13]. Patients with insufficient responses to high-dose CCBs should be commenced on additional PAH-specific therapies [13]. CCBs should not be administered in patients with negative vasodilatory results or those who have not undergone vasoreactivity studies, due to potential side effects of RV failure, hypotension and syncope [13].
5.3. Targeted Therapies
Specific therapies which address the underlying pathophysiology of PAH include phosphodiesterase-5 inhibitors (PDE-5i), guanylate cyclase (GC) stimulators, prostacyclin analogues, prostacyclin receptor agonists, and endothelin receptor antagonists (ERA). In comparison to historical treatment regimes, these targeted therapies have revolutionised modern PAH management [38], with several studies having demonstrated improved exercise capacity, WHO-FC and time to clinical worsening (TTCW) as summarised in Table 3. The individual studies were not sufficiently powered to analyse mortality but a subsequent meta-analysis of RCTs demonstrated a 43% reduction in mortality rate [63].

Table 3.
Summary of randomised clinical trials of drugs approved for treatment of pulmonary arterial hypertension.
5.4. Phosphodiesterase-5 Inhibitors
Sildenafil is a selective PDE-5i which is predominantly prescribed orally but can be administered intravenously for long-term patients who are unable to tolerate oral formulations. The SUPER-1 (Sildenafil Use in Pulmonary Arterial Hypertension) trial randomly allocated 278 treatment-naïve PAH patients to either placebo or sildenafil for 12 weeks [82]. Sildenafil conferred significant improvements in 6MWD, WHO-FC and pulmonary artery pressures when compared to placebo, but there was no difference in clinical worsening incidence [82]. When extended to three years in the SUPER-2 trial, 60% and 46% of patients maintained or improved their WHO-FC and 6MWD respectively [84]. Addition of sildenafil to epoprostenol similarly improved 6MWD and TTCW [76]. Some adverse effects of sildenafil included headaches, flushing, epistaxis, dyspepsia and diarrhoea, ranging from mild to moderate in severity [82]. Since PDE-5i cause vasodilation, these drugs should be used cautiously in combination with other vasodilatory agents, particularly nitrates and CCBs.
Tadalafil, an alternative PDE-5i medication, possesses a superior pharmacokinetic profile in that it is dispensed once-daily in comparison to sildenafil which requires thrice-daily administration. In the PHIRST-1 (Pulmonary Arterial Hypertension and Response to Tadalafil) trial, 405 patients who were either treatment-naïve or on existing bosentan therapy, were randomised to receive placebo or tadalafil for 16 weeks [78]. The tadalafil arms of both the treatment-naïve and background therapy groups demonstrated significantly improved exercise capacity, symptomatic control, haemodynamics and reduced TTCW [78]. Tadalafil was well tolerated in the long-term, with sustained improvements in exercise capacity [85].
5.5. Guanylate Cyclase Stimulators
Riociguat directly activates sGC, thus promoting vasodilation. In PATENT-1 (Pulmonary Arterial Hypertension Soluble Guanylate Cyclase-Stimulator Trial), 443 patients who were either treatment-naïve or had existing PAH treatment were randomised to placebo or riociguat, with the latter group demonstrating favourable outcomes regarding 6MWD, haemodynamics, WHO-FC and TTCW [77]. On sub-analysis, improved exercise capacity was also observed in patients on existing background therapy [77]. The long-term efficacy and safety profile of riociguat are currently being evaluated in PATENT-2, with interim analysis showing acceptable drug tolerability and continued improvements in 6MWD and WHO-FC compared to the PATENT-1 baseline [86]. The adverse effects of GC stimulators are similar to PDE-5i, including hypotension and syncope [77]. Combination therapy with PDE-5i was found to have a non-positive benefit-risk ratio due to increased hypotension and other drug-related side-effects [87].
5.6. Prostacyclin Analogues
Epoprostenol is a synthetic prostacyclin that can only be administered intravenously due to its short half-life (3–5 min) and limited stability at room temperature. Randomised trials have examined the benefit of continuous epoprostenol infusions in patients with iPAH [68,79] and PAH secondary to the scleroderma spectrum of disease [67], with this regimen producing improved symptomatic control, exercise capacity and haemodynamics [67,68,79]. Crucially, one study found improved survival rates among patients with severe iPAH—making epoprostenol the only therapy to-date to demonstrate a reduced mortality rate within a single RCT [68]. According to the ESC/ERS guidelines, a subsequent meta-analysis of the aforementioned randomised trials found a risk reduction in mortality of about 70% [13,67,68,79].
Treprostinil is a prostanoid analogue with similar properties to epoprostenol, but due to its longer half-life, it can be administered through multiple routes. A RCT comparing subcutaneous treprostinil to placebo demonstrated exercise capacity, symptomatic control and haemodynamics improved significantly, however infusion site pain was a common adverse event causing 8% of the population to withdraw from the study [81]. A RCT intended to investigate intravenous (IV) treprostinil was closed prematurely due to safety considerations [88]. Amongst the enrolled population, in 44 (35%) of the planned 126 participants, there were significant improvements in exercise capacity, symptoms and functional class [88]. Observational studies have found short-term IV treprostinil to be tolerable and produce a similar benefit profile to epoprostenol [89,90]. The TRIUMPH (Treprostinil Sodium Inhalation Used in the Management of Pulmonary Arterial Hypertension) trial investigated the addition of inhaled treprostinil to background therapy of either bosentan or sildenafil [83]. There was a significant improvement in 6MWD and quality of life, but minimal effect on functional class or TTCW [83]. The FREEDOM-C (Multicenter, Double-101 Blind, Randomized, Placebo-Controlled Study of the Efficacy and Safety of Oral Treprostinil Sustained Release Tablets in Subjects With Pulmonary Arterial Hypertension) [73] and FREEDOM-C2 [74] trials studied oral formulations of treprostinil in PAH patients on background bosentan and/or sildenafil therapy. Both studies demonstrated non-significant improvements in 6MWD [73,74] however a subsequent RCT with treatment-naïve patients observed a significant improvement [91].
Iloprost is available in IV, oral or aerosol formulations, although the effects of oral iloprost have not yet been studied. Inhaled iloprost, as demonstrated in the AIR (Aerosolized Iloprost Randomized) study, conferred significant improvements in symptomatic control, haemodynamics, WHO-FC and quality of life, though it was commonly associated with flushing and jaw pain [64]. Data concerning IV iloprost in PAH is scarce, with an observational study demonstrating limited clinical benefits [92].
5.7. Prostacyclin Receptor Agonists
Selexipag is an oral prostacyclin IP receptor agonist which produces vasodilatory and anti-proliferative effects. This agent was studied in the 71-week GRIPHON (Prostacyclin Receptor Agonist in Pulmonary Arterial Hypertension) study, which involved 1156 PAH patients with pre-existing monotherapy or dual therapy [75]. Time to first morbidity or mortality event was significantly reduced by 40%, though mortality rates were not significantly affected [75]. Selexipag significantly improved 6MWD, but was associated with headache, diarrhoea, nausea and jaw pain [75].
5.8. Endothelin Receptor Antagonists (ERA)
Bosentan is a dual-acting ERA, binding to both the ETA and ETB receptors. The BREATHE-1 (Bosentan Randomized Trial of Endothelin Antagonist Therapy) study commenced 213 treatment-naïve PAH patients on a 12-week bosentan regimen which conferred improvements in 6MWD, functional class and time to first worsening [69]. These findings were similarly demonstrated in a subsequent 24-week study, with both studies showing increased hepatic enzymes as the main adverse event [69,72]. COMPASS-2 is a more recent, 38-month trial involving 334 patients on background sildenafil therapy who were randomised to either bosentan or placebo [71]. This study did not meet its primary endpoint (time to first morbidity or mortality) nor its secondary endpoints (functional class and PAH hospital-related admissions) except for a significant improvement in 6MWD [71].
Ambrisentan selectively binds to ETA receptors, with minimal binding to vasodilatory endothelial ETB receptors [66]. ARIES-1 (Ambrisentan in Pulmonary Arterial Hypertension, Randomized, Double-Blind, Placebo-Controlled, Multicentre Efficacy Study) and ARIES-2 involved 202 and 192 treatment-naïve PAH patients respectively [66]. Ambrisentan elicited improvements in 6MWD, functional class and TTCW, but produced adverse effects including peripheral oedema, headache and nasal congestion [66].
Macitentan is a novel drug targeting ETA and ETB receptors. SERAPHIN (Study with an Endothelin Receptor Antagonist in Pulmonary Arterial Hypertension to Improve Clinical Outcome) compared macitentan to placebo in 742 PAH patients (who were either treatment-naïve or on background therapy) over an average of 100 weeks [80]. Macitentan significantly reduced the composite endpoint (morbidity and mortality events, PAH-related hospitalisations, 6MWD and WHO-FC), although the study was insufficiently powered to show significant mortality reduction in sub-analysis [80]. These benefits were observed in both treatment-naïve and background-treated patients [80].
5.9. Combination Therapies
Combination therapies have been increasingly recognised in the treatment of PAH as they allow the targeting of multiple signalling pathways. A meta-analysis performed by Galiè and colleagues showed a reduction in TTCW and improvements in clinical outcomes when sequential combination therapy was added following suboptimal response to monotherapy [13,93]. Although the meta-analysis demonstrated a reduction in mortality, the analysis was not sufficiently powered to achieve statistical significance [93]. A recent meta-analysis similarly demonstrated benefits of combination therapy over monotherapy [39].
BREATHE-2, an extension of BREATHE-1, was the first trial to explore combination therapy and involved 33 patients on existing epoprostenol treatment who were either randomised to placebo or bosentan [70]. BREATHE-2 failed to demonstrate significant differences in haemodynamics or clinical improvement, however these conclusions are limited by the study’s small sample size [70]. This has been investigated in subsequent studies, such as COMPASS-2 [71] and PACES [76], and some results can be inferred from subanalyses of other studies with patients on background therapy from baseline. Based on the findings of these studies, the ESC/ERS pulmonary hypertension guidelines outline several possible combination therapies for PAH [13].
The AMBITION (Ambrisentan and Tadalafil in Patients with Pulmonary Arterial Hypertension) trial was a pivotal study in combination therapy which directly investigated the role of initiating dual therapy in treatment-naïve patients by randomising these participants to either combination therapy or monotherapy of either ambrisentan or tadalafil for 73 weeks [65]. The primary endpoint (time to clinical failure event) was reached with both dual and monotherapy, with the former group exhibiting an additional 50% relative reduction compared to the latter [65]. This was the first study to provide a direct outcome comparison between monotherapy and combination therapy in treatment-naïve patients, thereby creating a new paradigm for the initial management of high-risk PAH.
5.10. Clinical Approach to PAH Treatment
The ESC/ERS guidelines recommend a stepwise pragmatic approach to PAH management as outlined in Figure 2 [13]. Recent long-term trials have revealed that targeted therapies confer significant improvements in clinical outcomes, thereby changing the therapeutic approach to PAH [39,63]. Risk assessment and treatment options should be considered at the time of diagnosis, with the aim of treatment to maintain low risk profiles [13]. Risk assessment, as discussed earlier, stratifies patients into low, intermediate or high risk of clinical worsening or death, although other prognostic factors should also be considered [13]. Patients with low or intermediate risk can be initiated on monotherapy, with regular monitoring of treatment response [13]. Results from the SERAPHIN and GRIPHON trials suggest there is benefit in adding either long-term macitentan or selexipag to background therapies in those patients who require additional treatment [75,80]. Conversely, for high-risk patients, the AMBITION trial highlighted the benefits of immediate combination therapy rather than a graduated, stepwise approach [65]. Often, IV epoprostenol is prioritised in high-risk patients given that this agent has been demonstrated to improve 3-month mortality rate of patients with severe PAH [13,68]. Patients refractory to treatment may be considered for lung transplantation or balloon atrial septostomy, the discussion of which exceeds the scope of this review.
Since bosentan induces cytochrome P450 isoenzymes CYP3A4 and CYP2C9, and sildenafil is metabolised by these same isoenzymes, care should you taken to avoid drug-drug interactions. Furthermore, PAH-targeted medications should be used cautiously in patients taking co-existing antihypertensives to avoid systemic hypotension.
5.11. Future Research
The past few decades have seen dramatic changes in the understanding and management of PAH, leading to improved symptomatic control, exercise tolerance and progression free survival [38,39,63]. However, there have been variable definitions in study endpoints—particularly TTCW, complicating its interpretation in meta-analyses [39]. This endpoint includes a collection of outcomes, including symptomatic worsening, lack of improvement, PAH-related hospital admissions, transplantation and mortality [94]. However, PAH-related hospitalisation, mortality and transplantation often follows clinical deterioration and hence TTCW may underestimate the true mortality and morbidity [39]. Further research should have a consistent definition in study endpoints and broader analysis of total PAH-related events [39,94]. Nevertheless, clinical worsening and mortality was still prevalent in these studies despite adequate therapy [39,63] indicating the need for identification of novel therapeutic agents. Research is currently underway to investigate the role of oestrogen [95], tyrosine kinase inhibitors [96] and BMPRII gene activation [97], (amongst many others) in the management of PAH.
6. Conclusions
Substantial advancements in the understanding and management of PAH have been made in the recent decades. The current understanding of PAH aetiology includes the nitric oxide, prostacyclin-thromboxane and endothelin-1 pathways. This has led to five classes of drugs which target these the pathways: namely phosphodiesterase-5 inhibitors, soluble guanylate cyclase inhibitors, prostacyclin analogues, prostacyclin receptor agonists and endothelin receptor antagonists. Recent long-term trials have shown evidence of progression-free survival with initial, or early, addition of these drugs, either in isolation or in combination with other drug classes. In particular, emerging evidence has favoured the use of initial combination therapies in high risk patients. These medications are recommended with general and supportive measures; however, the evidence supporting these practices is heterogeneous and inconclusive. Ongoing study into alternative pathways involved in PAH pathogenesis represent opportunities for future targets in PAH management.
Author Contributions
All authors were involved in the drafting of the manuscript. All authors agreed with the final version of this manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hoeper, M.M.; Bogaard, H.J.; Condliffe, R.; Frantz, R.; Khanna, D.; Kurzyna, M.; Langleben, D.; Manes, A.; Satoh, T.; Torres, F. Definitions and diagnosis of pulmonary hypertension. J. Am. Coll. Cardiol. 2013, 62, D42–D50. [Google Scholar] [CrossRef] [PubMed]
- Moreira, E.M.; Gall, H.; Leening, M.J.; Lahousse, L.; Loth, D.W.; Krijthe, B.P.; Kiefte-de Jong, J.C.; Brusselle, G.G.; Hofman, A.; Stricker, B.H. Prevalence of pulmonary hypertension in the general population: The rotterdam study. PLoS ONE 2015, 10, e0130072. [Google Scholar] [CrossRef] [PubMed]
- Strange, G.; Playford, D.; Stewart, S.; Deague, J.A.; Nelson, H.; Kent, A.; Gabbay, E. Pulmonary hypertension: Prevalence and mortality in the armadale echocardiography cohort. Heart 2012, 98, 1805–1811. [Google Scholar] [CrossRef] [PubMed]
- Badesch, D.B.; Raskob, G.E.; Elliott, C.G.; Krichman, A.M.; Farber, H.W.; Frost, A.E.; Barst, R.J.; Benza, R.L.; Liou, T.G.; Turner, M. Pulmonary arterial hypertension: Baseline characteristics from the reveal registry. Chest 2010, 137, 376–387. [Google Scholar] [CrossRef] [PubMed]
- Tuder, R.M.; Archer, S.L.; Dorfmüller, P.; Erzurum, S.C.; Guignabert, C.; Michelakis, E.; Rabinovitch, M.; Schermuly, R.; Stenmark, K.R.; Morrell, N.W. Relevant issues in the pathology and pathobiology of pulmonary hypertension. J. Am. Coll. Cardiol. 2013, 62, D4–D12. [Google Scholar] [CrossRef] [PubMed]
- Thenappan, T.; Ryan, J.J.; Archer, S.L. Evolving epidemiology of pulmonary arterial hypertension. Am. J. Respir. Crit. Care Med. 2012, 186, 707–709. [Google Scholar] [CrossRef] [PubMed]
- Health and Social Care Information Centre. Fifth Annual Report: Key Findings from the National Audit of Pulmonary Hypertension for the United Kingdom, Channel Islands, Gibraltar and Isle of Man; Health and Social Care Information Centre: Leeds, UK, 2015. [Google Scholar]
- Shapiro, S.; Traiger, G.L.; Turner, M.; McGoon, M.D.; Wason, P.; Barst, R.J. Sex differences in the diagnosis, treatment, and outcome of patients with pulmonary arterial hypertension enrolled in the registry to evaluate early and long-term pulmonary arterial hypertension disease management. Chest 2012, 141, 363–373. [Google Scholar] [CrossRef] [PubMed]
- Benza, R.L.; Miller, D.P.; Barst, R.J.; Badesch, D.B.; Frost, A.E.; McGoon, M.D. An evaluation of long-term survival from time of diagnosis in pulmonary arterial hypertension from the reveal registry. Chest 2012, 142, 448–456. [Google Scholar] [CrossRef] [PubMed]
- Simonneau, G.; Gatzoulis, M.A.; Adatia, I.; Celermajer, D.; Denton, C.; Ghofrani, A.; Sanchez, M.A.G.; Kumar, R.K.; Landzberg, M.; Machado, R.F. Updated clinical classification of pulmonary hypertension. J. Am. Coll. Cardiol. 2013, 62, D34–D41. [Google Scholar] [CrossRef] [PubMed]
- Simonneau, G.; Robbins, I.M.; Beghetti, M.; Channick, R.N.; Delcroix, M.; Denton, C.P.; Elliott, C.G.; Gaine, S.P.; Gladwin, M.T.; Jing, Z.-C. Updated clinical classification of pulmonary hypertension. J. Am. Coll. Cardiol. 2009, 54, S43–S54. [Google Scholar] [CrossRef] [PubMed]
- Austin, E.D.; Loyd, J.E. Genetics and mediators in pulmonary arterial hypertension. Clin. Chest Med. 2007, 28, 43–57. [Google Scholar] [CrossRef] [PubMed]
- Galiè, N.; Humbert, M.; Vachiery, J.-L.; Gibbs, S.; Lang, I.; Torbicki, A.; Simonneau, G.; Peacock, A.; Vonk Noordegraaf, A.; Beghetti, M.; et al. 2015 esc/ers guidelines for the diagnosis and treatment of pulmonary hypertensionthe joint task force for the diagnosis and treatment of pulmonary hypertension of the european society of cardiology (ESC) and the european respiratory society (ERS): Endorsed by: Association for european paediatric and congenital cardiology (AEPC), international society for heart and lung transplantation (ISHLT). Eur. Heart J. 2016, 37, 67–119. [Google Scholar] [CrossRef] [PubMed]
- Houtchens, J.; Martin, D.; Klinger, J.R. Diagnosis and management of pulmonary arterial hypertension. Pulm. Med. 2011, 2011. [Google Scholar] [CrossRef] [PubMed]
- Machado, R.D.; Eickelberg, O.; Elliott, C.G.; Geraci, M.W.; Hanaoka, M.; Loyd, J.E.; Newman, J.H.; Phillips, J.A.; Soubrier, F.; Trembath, R.C. Genetics and genomics of pulmonary arterial hypertension. J. Am. Coll. Cardiol. 2009, 54, S32–S42. [Google Scholar] [CrossRef] [PubMed]
- Lane, K.B.; Machado, R.D.; Pauciulo, M.W.; Thomson, J.R.; Phillips, J.A.; Loyd, J.E.; Nichols, W.C.; Trembath, R.C. Heterozygous germline mutations in bmpr2, encoding a tgf-β receptor, cause familial primary pulmonary hypertension. Nat. Genet. 2000, 26, 81–84. [Google Scholar] [CrossRef] [PubMed]
- Harrison, R.E.; Flanagan, J.A.; Sankelo, M.; Abdalla, S.; Rowell, J.; Machado, R.D.; Elliott, C.; Robbins, I.; Olschewski, H.; McLaughlin, V. Molecular and functional analysis identifies alk-1 as the predominant cause of pulmonary hypertension related to hereditary haemorrhagic telangiectasia. J. Med. Genet. 2003, 40, 865–871. [Google Scholar] [CrossRef] [PubMed]
- Chaouat, A.; Coulet, F.; Favre, C.; Simonneau, G.; Weitzenblum, E.; Soubrier, F.; Humbert, M. Endoglin germline mutation in a patient with hereditary haemorrhagic telangiectasia and dexfenfluramine associated pulmonary arterial hypertension. Thorax 2004, 59, 446–448. [Google Scholar] [CrossRef] [PubMed]
- Aldred, M.A.; Vijayakrishnan, J.; James, V.; Soubrier, F.; Gomez-Sanchez, M.A.; Martensson, G.; Galie, N.; Manes, A.; Corris, P.; Simonneau, G. Bmpr2 gene rearrangements account for a significant proportion of mutations in familial and idiopathic pulmonary arterial hypertension. Hum. Mutat. 2006, 27, 212–213. [Google Scholar] [CrossRef] [PubMed]
- Cogan, J.D.; Pauciulo, M.W.; Batchman, A.P.; Prince, M.A.; Robbins, I.M.; Hedges, L.K.; Stanton, K.C.; Wheeler, L.A.; Phillips, J.A., III; Loyd, J.E. High frequency of bmpr2 exonic deletions/duplications in familial pulmonary arterial hypertension. Am. J. Respir. Crit. Care Med. 2006, 174, 590–598. [Google Scholar] [CrossRef] [PubMed]
- Larkin, E.K.; Newman, J.H.; Austin, E.D.; Hemnes, A.R.; Wheeler, L.; Robbins, I.M.; West, J.D.; Phillips, J.A., III; Hamid, R.; Loyd, J.E. Longitudinal analysis casts doubt on the presence of genetic anticipation in heritable pulmonary arterial hypertension. Am. J. Respir. Crit. Care Med. 2012, 186, 892–896. [Google Scholar] [CrossRef] [PubMed]
- Austin, E.D.; Phillips, J.A.; Cogan, J.D.; Hamid, R.; Yu, C.; Stanton, K.C.; Phillips, C.A.; Wheeler, L.A.; Robbins, I.M.; Newman, J.H. Truncating and missense bmpr2 mutations differentially affect the severity of heritable pulmonary arterial hypertension. Respir. Res. 2009, 10, 87. [Google Scholar] [CrossRef] [PubMed]
- Morrell, N.W.; Adnot, S.; Archer, S.L.; Dupuis, J.; Jones, P.L.; MacLean, M.R.; McMurtry, I.F.; Stenmark, K.R.; Thistlethwaite, P.A.; Weissmann, N. Cellular and molecular basis of pulmonary arterial hypertension. J. Am. Coll. Cardiol. 2009, 54, S20–S31. [Google Scholar] [CrossRef] [PubMed]
- West, J.; Fagan, K.; Steudel, W.; Fouty, B.; Lane, K.; Harral, J.; Hoedt-Miller, M.; Tada, Y.; Ozimek, J.; Tuder, R. Pulmonary hypertension in transgenic mice expressing a dominant-negative bmprii gene in smooth muscle. Circ. Res. 2004, 94, 1109–1114. [Google Scholar] [CrossRef] [PubMed]
- Chun, H.J.; Bonnet, S.; Chan, S.Y. Translational advances in the field of pulmonary hypertension. Translating microrna biology in pulmonary hypertension. It will take more than “miR” words. Am. J. Respir. Crit. Care Med. 2017, 195, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Budhiraja, R.; Tuder, R.M.; Hassoun, P.M. Endothelial dysfunction in pulmonary hypertension. Circulation 2004, 109, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Giaid, A.; Saleh, D. Reduced expression of endothelial nitric oxide synthase in the lungs of patients with pulmonary hypertension. N. Engl. J. Med. 1995, 333, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Prior, D.L.; Adams, H.; Williams, T.J. Update on pharmacotherapy for pulmonary hypertension. Med. J. Aust. 2016, 205, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.-Y.; Zhao, Y.D.; Mirza, M.K.; Huang, J.H.; Potula, H.-H.S.; Vogel, S.M.; Brovkovych, V.; Yuan, J.X.-J.; Wharton, J.; Malik, A.B. Persistent enos activation secondary to caveolin-1 deficiency induces pulmonary hypertension in mice and humans through pkg nitration. J. Clin. Investig. 2009, 119, 2009–2018. [Google Scholar] [CrossRef] [PubMed]
- Alp, N.J.; Channon, K.M. Regulation of endothelial nitric oxide synthase by tetrahydrobiopterin in vascular disease. Arterioscler. Thromb. Vasc. Biol. 2004, 24, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Christman, B.W.; McPherson, C.D.; Newman, J.H.; King, G.A.; Bernard, G.R.; Groves, B.M.; Loyd, J.E. An imbalance between the excretion of thromboxane and prostacyclin metabolites in pulmonary hypertension. N. Engl. J. Med. 1992, 327, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Hoshikawa, Y.; Voelkel, N.F.; Gesell, T.L.; Moore, M.D.; Morris, K.G.; Alger, L.A.; Narumiya, S.; Geraci, M.W. Prostacyclin receptor-dependent modulation of pulmonary vascular remodeling. Am. J. Respir. Crit. Care Med. 2001, 164, 314–318. [Google Scholar] [CrossRef] [PubMed]
- Tuder, R.M.; Cool, C.D.; Geraci, M.W.; Wang, J.; Abman, S.H.; Wright, L.; Badesch, D.; Voelkel, N.F. Prostacyclin synthase expression is decreased in lungs from patients with severe pulmonary hypertension. Am. J. Respir. Crit. Care Med. 1999, 159, 1925–1932. [Google Scholar] [CrossRef] [PubMed]
- Yanagisawa, M.; Kurihara, H.; Kimura, S.; Tomobe, Y.; Kobayashi, M.; Mitsui, Y.; Yazaki, Y.; Goto, K.; Masaki, T. A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 1988, 332, 411–415. [Google Scholar] [CrossRef] [PubMed]
- Tabima, D.M.; Frizzell, S.; Gladwin, M.T. Reactive oxygen and nitrogen species in pulmonary hypertension. Free Radic. Biol. Med. 2012, 52, 1970–1986. [Google Scholar] [CrossRef] [PubMed]
- Giaid, A.; Yanagisawa, M.; Langleben, D.; Michel, R.P.; Levy, R.; Shennib, H.; Kimura, S.; Masaki, T.; Duguid, W.P.; Stewart, D.J. Expression of endothelin-1 in the lungs of patients with pulmonary hypertension. N. Engl. J. Med. 1993, 328, 1732–1739. [Google Scholar] [CrossRef] [PubMed]
- Stewart, D.J.; Levy, R.D.; Cernacek, P.; Langleben, D. Increased plasma endothelin-1 in pulmonary hypertension: Marker or mediator of disease? Ann. Intern. Med. 1991, 114, 464–469. [Google Scholar] [CrossRef] [PubMed]
- Hoeper, M.; Markevych, I.; Spiekerkoetter, E.; Welte, T.; Niedermeyer, J. Goal-oriented treatment and combination therapy for pulmonary arterial hypertension. Eur. Respir. J. 2005, 26, 858–863. [Google Scholar] [CrossRef] [PubMed]
- Lajoie, A.C.; Lauzière, G.; Lega, J.-C.; Lacasse, Y.; Martin, S.; Simard, S.; Bonnet, S.; Provencher, S. Combination therapy versus monotherapy for pulmonary arterial hypertension: A meta-analysis. Lancet Respir. Med. 2016, 4, 291–305. [Google Scholar] [CrossRef]
- Benza, R.L.; Miller, D.P.; Gomberg-Maitland, M.; Frantz, R.P.; Foreman, A.J.; Coffey, C.S.; Frost, A.; Barst, R.J.; Badesch, D.B.; Elliott, C.G. Predicting survival in pulmonary arterial hypertension. Circulation 2010, 122, 164–172. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, V.V.; Gaine, S.P.; Howard, L.S.; Leuchte, H.H.; Mathier, M.A.; Mehta, S.; Palazzini, M.; Park, M.H.; Tapson, V.F.; Sitbon, O. Treatment goals of pulmonary hypertension. J. Am. Coll. Cardiol. 2013, 62, D73–D81. [Google Scholar] [CrossRef] [PubMed]
- Mereles, D.; Ehlken, N.; Kreuscher, S.; Ghofrani, S.; Hoeper, M.M.; Halank, M.; Meyer, F.J.; Karger, G.; Buss, J.; Juenger, J. Exercise and respiratory training improve exercise capacity and quality of life in patients with severe chronic pulmonary hypertension. Circulation 2006, 114, 1482–1489. [Google Scholar] [CrossRef] [PubMed]
- Chan, L.; Chin, L.M.; Kennedy, M.; Woolstenhulme, J.G.; Nathan, S.D.; Weinstein, A.A.; Connors, G.; Weir, N.A.; Drinkard, B.; Lamberti, J. Benefits of intensive treadmill exercise training on cardiorespiratory function and quality of life in patients with pulmonary hypertension. Chest 2013, 143, 333–343. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, A.A.; Chin, L.M.; Keyser, R.E.; Kennedy, M.; Nathan, S.D.; Woolstenhulme, J.G.; Connors, G.; Chan, L. Effect of aerobic exercise training on fatigue and physical activity in patients with pulmonary arterial hypertension. Respir. Med. 2013, 107, 778–784. [Google Scholar] [CrossRef] [PubMed]
- Duarte, A.G.; Thomas, S.; Safdar, Z.; Torres, F.; Pacheco, L.D.; Feldman, J. Management of pulmonary arterial hypertension during pregnancy: A retrospective, multicenter experience. Chest 2013, 143, 1330–1336. [Google Scholar] [CrossRef] [PubMed]
- Ciracì, R.; Tirone, G.; Scaglione, F. The impact of drug–drug interactions on pulmonary arterial hypertension therapy. Pulm. Pharmacol. Ther. 2014, 28, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Weiss, J.; Theile, D.; Rüppell, M.A.; Speck, T.; Spalwisz, A.; Haefeli, W.E. Interaction profile of macitentan, a new non-selective endothelin-1 receptor antagonist, in vitro. Eur. J. Pharmacol. 2013, 701, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Jaïs, X.; Olsson, K.M.; Barbera, J.A.; Blanco, I.; Torbicki, A.; Peacock, A.; Vizza, C.D.; Macdonald, P.; Humbert, M.; Hoeper, M.M. Pregnancy outcomes in pulmonary arterial hypertension in the modern management era. Eur. Respir. J. 2012, 40, 881–885. [Google Scholar] [CrossRef] [PubMed]
- Hemnes, A.R.; Kiely, D.G.; Cockrill, B.A.; Safdar, Z.; Wilson, V.J.; Al Hazmi, M.; Preston, I.R.; MacLean, M.R.; Lahm, T. Statement on pregnancy in pulmonary hypertension from the pulmonary vascular research institute. Pulm. Circ. 2015, 5, 435–465. [Google Scholar] [CrossRef] [PubMed]
- Bonnin, M.; Mercier, F.J.; Sitbon, O.; Roger-Christoph, S.; Jaïs, X.; Humbert, M.; Audibert, F.; Frydman, R.; Simonneau, G.; Benhamou, D. Severe pulmonary hypertension during pregnancymode of delivery and anesthetic management of 15 consecutive cases. Anesthesiology 2005, 102, 1133–1137. [Google Scholar] [CrossRef] [PubMed]
- Roberts, D.H.; Lepore, J.J.; Maroo, A.; Semigran, M.J.; Ginns, L.C. Oxygen therapy improves cardiac index and pulmonary vascular resistance in patients with pulmonary hypertension. Chest 2001, 120, 1547–1555. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McLaughlin, V.V.; Archer, S.L.; Badesch, D.B.; Barst, R.J.; Farber, H.W.; Lindner, J.R.; Mathier, M.A.; McGoon, M.D.; Park, M.H.; Rosenson, R.S. ACCF/AHA 2009 expert consensus document on pulmonary hypertension: A report of the american college of cardiology foundation task force on expert consensus documents and the american heart association developed in collaboration with the american college of chest physicians; american thoracic society, inc.; and the pulmonary hypertension association. J. Am. Coll. Cardiol. 2009, 53, 1573–1619. [Google Scholar] [CrossRef] [PubMed]
- Rich, S.; Seidlitz, M.; Dodin, E.; Osimani, D.; Judd, D.; Genthner, D.; McLaughlin, V.; Francis, G. The short-term effects of digoxin in patients with right ventricular dysfunction from pulmonary hypertension. Chest 1998, 114, 787–792. [Google Scholar] [CrossRef] [PubMed]
- Galiè, N.; Delcroix, M.; Ghofrani, H.-A.; Jansa, P.; Minai, O.; Perchenet, L.; Rubin, L.; Sastry, B.; Torbicki, A.; Simonneau, G. Anticoagulant therapy does not influence long-term outcomes in patients with pulmonary arterial hypertension (PAH): Insights from the randomised controlled SERAPHIN trial of macitentan. Eur. Heart J. 2014, 35, 10. [Google Scholar]
- Herve, P.; Humbert, M.; Sitbon, O.; Parent, F.; Nunes, H.; Legal, C.; Garcia, G.; Simonneau, G. Pathobiology of pulmonary hypertension: The role of platelets and thrombosis. Clin. Chest. Med. 2001, 22, 451–458. [Google Scholar] [CrossRef]
- Huber, K.; Beckmann, R.; Frank, H.; Kneussl, M.; Mlczoch, J.; Binder, B.R. Fibrinogen, t-pa, and pai-1 plasma levels in patients with pulmonary hypertension. Am. J. Respir. Crit. Care Med. 1994, 150, 929–933. [Google Scholar] [CrossRef] [PubMed]
- Olsson, K.M.; Delcroix, M.; Ghofrani, H.A.; Tiede, H.; Huscher, D.; Speich, R.; Grünig, E.; Staehler, G.; Rosenkranz, S.; Halank, M. Anticoagulation and survival in pulmonary arterial hypertension: Results from the comperative, prospective registry of newly initiated therapies for pulmonary hypertension (COMPERA). Circulation 2013. [Google Scholar] [CrossRef]
- Preston, I.R.; Roberts, K.E.; Miller, D.P.; Sen, G.P.; Selej, M.; Benton, W.W.; Hill, N.S.; Farber, H.W. Effect of warfarin treatment on survival of patients with pulmonary arterial hypertension (PAH) in the registry to evaluate early and long-term PAH disease management (REVEAL). Circulation 2015. [Google Scholar] [CrossRef] [PubMed]
- Guillevin, L.; Armstrong, I.; Aldrighetti, R.; Howard, L.S.; Ryftenius, H.; Fischer, A.; Lombardi, S.; Studer, S.; Ferrari, P. Understanding the impact of pulmonary arterial hypertension on patients’ and carers’ lives. Eur. Respir. Rev. 2013, 22, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Gräfe, K.; Ufer, C.; Kroenke, K.; Grünig, E.; Herzog, W.; Borst, M.M. Anxiety and depression in patients with pulmonary hypertension. Psychosom. Med. 2004, 66, 831–836. [Google Scholar] [CrossRef] [PubMed]
- Sitbon, O.; Humbert, M.; Jaïs, X.; Ioos, V.; Hamid, A.M.; Provencher, S.; Garcia, G.; Parent, F.; Hervé, P.; Simonneau, G. Long-term response to calcium channel blockers in idiopathic pulmonary arterial hypertension. Circulation 2005, 111, 3105–3111. [Google Scholar] [CrossRef] [PubMed]
- Montani, D.; Savale, L.; Natali, D.; Jaïs, X.; Herve, P.; Garcia, G.; Humbert, M.; Simonneau, G.; Sitbon, O. Long-term response to calcium-channel blockers in non-idiopathic pulmonary arterial hypertension. Eur. Heart J. 2010, 31, 1898–1907. [Google Scholar] [CrossRef] [PubMed]
- Galiè, N.; Manes, A.; Negro, L.; Palazzini, M.; Bacchi-Reggiani, M.L.; Branzi, A. A meta-analysis of randomized controlled trials in pulmonary arterial hypertension. Eur. Heart J. 2009, 30, 394–403. [Google Scholar] [CrossRef] [PubMed]
- Olschewski, H.; Simonneau, G.; Galiè, N.; Higenbottam, T.; Naeije, R.; Rubin, L.J.; Nikkho, S.; Speich, R.; Hoeper, M.M.; Behr, J. Inhaled iloprost for severe pulmonary hypertension. N. Engl. J. Med. 2002, 347, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Galiè, N.; Barberà, J.A.; Frost, A.E.; Ghofrani, H.-A.; Hoeper, M.M.; McLaughlin, V.V.; Peacock, A.J.; Simonneau, G.; Vachiery, J.-L.; Grünig, E. Initial use of ambrisentan plus tadalafil in pulmonary arterial hypertension. N. Engl. J. Med. 2015, 373, 834–844. [Google Scholar] [CrossRef] [PubMed]
- Galiè, N.; Olschewski, H.; Oudiz, R.J.; Torres, F.; Frost, A.; Ghofrani, H.A.; Badesch, D.B.; McGoon, M.D.; McLaughlin, V.V.; Roecker, E.B. Ambrisentan for the treatment of pulmonary arterial hypertension. Circulation 2008, 117, 3010–3019. [Google Scholar] [CrossRef] [PubMed]
- Badesch, D.B.; Tapson, V.F.; McGoon, M.D.; Brundage, B.H.; Rubin, L.J.; Wigley, F.M.; Rich, S.; Barst, R.J.; Barrett, P.S.; Kral, K.M. Continuous intravenous epoprostenol for pulmonary hypertension due to the scleroderma spectrum of diseasea randomized, controlled trial. Ann. Intern. Med. 2000, 132, 425–434. [Google Scholar] [CrossRef] [PubMed]
- Barst, R.J.; Rubin, L.J.; Long, W.A.; McGoon, M.D.; Rich, S.; Badesch, D.B.; Groves, B.M.; Tapson, V.F.; Bourge, R.C.; Brundage, B.H. A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension. N. Engl. J. Med. 1996, 334, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Rubin, L.J.; Badesch, D.B.; Barst, R.J.; Galiè, N.; Black, C.M.; Keogh, A.; Pulido, T.; Frost, A.; Roux, S.; Leconte, I. Bosentan therapy for pulmonary arterial hypertension. N. Engl. J. Med. 2002, 346, 896–903. [Google Scholar] [CrossRef] [PubMed]
- Humbert, M.; Barst, R.; Robbins, I.; Channick, R.; Galie, N.; Boonstra, A.; Rubin, L.; Horn, E.; Manes, A.; Simonneau, G. Combination of bosentan with epoprostenol in pulmonary arterial hypertension: BREATHE-2. Eur. Respir. J. 2004, 24, 353–359. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, V.; Channick, R.N.; Ghofrani, H.-A.; Lemarié, J.-C.; Naeije, R.; Packer, M.; Souza, R.; Tapson, V.F.; Tolson, J.; Al Hiti, H. Bosentan added to sildenafil therapy in patients with pulmonary arterial hypertension. Eur. Respir. J. 2015. [Google Scholar] [CrossRef] [PubMed]
- Galiè, N.; Rubin, L.; Hoeper, M.; Jansa, P.; Al-Hiti, H.; Meyer, G.; Chiossi, E.; Kusic-Pajic, A.; Simonneau, G. Treatment of patients with mildly symptomatic pulmonary arterial hypertension with bosentan (EARLY study): A double-blind, randomised controlled trial. Lancet 2008, 371, 2093–2100. [Google Scholar] [CrossRef]
- Tapson, V.F.; Torres, F.; Kermeen, F.; Keogh, A.M.; Allen, R.P.; Frantz, R.P.; Badesch, D.B.; Frost, A.E.; Shapiro, S.M.; Laliberte, K. Oral treprostinil for the treatment of pulmonary arterial hypertension in patients on background endothelin receptor antagonist and/or phosphodiesterase type 5 inhibitor therapy (the FREEDOM-C study): A randomized controlled trial. Chest 2012, 142, 1383–1390. [Google Scholar] [CrossRef] [PubMed]
- Tapson, V.F.; Jing, Z.-C.; Xu, K.-F.; Pan, L.; Feldman, J.; Kiely, D.G.; Kotlyar, E.; McSwain, C.S.; Laliberte, K.; Arneson, C. Oral treprostinil for the treatment of pulmonary arterial hypertension in patients receiving background endothelin receptor antagonist and phosphodiesterase type 5 inhibitor therapy (the FREEDOM-C2 study): A randomized controlled trial. Chest 2013, 144, 952–958. [Google Scholar] [CrossRef] [PubMed]
- Sitbon, O.; Channick, R.; Chin, K.M.; Frey, A.; Gaine, S.; Galiè, N.; Ghofrani, H.-A.; Hoeper, M.M.; Lang, I.M.; Preiss, R. Selexipag for the treatment of pulmonary arterial hypertension. N. Engl. J. Med. 2015, 373, 2522–2533. [Google Scholar] [CrossRef] [PubMed]
- Simonneau, G.; Rubin, L.J.; Galie, N.; Barst, R.J.; Fleming, T.R.; Frost, A.E.; Engel, P.J.; Kramer, M.R.; Burgess, G.; Collings, L. Addition of sildenafil to long-term intravenous epoprostenol therapy in patients with pulmonary arterial hypertension: A randomized trial. Ann. Intern. Med. 2008, 149, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Ghofrani, H.-A.; Galiè, N.; Grimminger, F.; Grünig, E.; Humbert, M.; Jing, Z.-C.; Keogh, A.M.; Langleben, D.; Kilama, M.O.; Fritsch, A. Riociguat for the treatment of pulmonary arterial hypertension. N. Engl. J. Med. 2013, 369, 330–340. [Google Scholar] [CrossRef] [PubMed]
- Galiè, N.; Brundage, B.H.; Ghofrani, H.A.; Oudiz, R.J.; Simonneau, G.; Safdar, Z.; Shapiro, S.; White, R.J.; Chan, M.; Beardsworth, A. Tadalafil therapy for pulmonary arterial hypertension. Circulation 2009, 119, 2894–2903. [Google Scholar] [CrossRef] [PubMed]
- Rubin, L.J.; Mendoza, J.; Hood, M.; McGoon, M.; Barst, R.; Williams, W.B.; Diehl, J.H.; Crow, J.; Long, W. Treatment of primary pulmonary hypertension with continuous intravenous prostacyclin (epoprostenol). Ann. Intern. Med. 1990, 112, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Pulido, T.; Adzerikho, I.; Channick, R.N.; Delcroix, M.; Galiè, N.; Ghofrani, H.-A.; Jansa, P.; Jing, Z.-C.; Le Brun, F.-O.; Mehta, S. Macitentan and morbidity and mortality in pulmonary arterial hypertension. N. Engl. J. Med. 2013, 369, 809–818. [Google Scholar] [CrossRef] [PubMed]
- Simonneau, G.; Barst, R.J.; Galie, N.; Naeije, R.; Rich, S.; Bourge, R.C.; Keogh, A.; Oudiz, R.; Frost, A.; Blackburn, S.D. Continuous subcutaneous infusion of treprostinil, a prostacyclin analogue, in patients with pulmonary arterial hypertension: A double-blind, randomized, placebo-controlled trial. Am. J. Respir. Crit. Care Med. 2002, 165, 800–804. [Google Scholar] [CrossRef] [PubMed]
- Galiè, N.; Ghofrani, H.A.; Torbicki, A.; Barst, R.J.; Rubin, L.J.; Badesch, D.; Fleming, T.; Parpia, T.; Burgess, G.; Branzi, A. Sildenafil citrate therapy for pulmonary arterial hypertension. N. Engl. J. Med. 2005, 353, 2148–2157. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, V.V.; Benza, R.L.; Rubin, L.J.; Channick, R.N.; Voswinckel, R.; Tapson, V.F.; Robbins, I.M.; Olschewski, H.; Rubenfire, M.; Seeger, W. Addition of inhaled treprostinil to oral therapy for pulmonary arterial hypertension: A randomized controlled clinical trial. J. Am. Coll. Cardiol. 2010, 55, 1915–1922. [Google Scholar] [CrossRef] [PubMed]
- Rubin, L.J.; Badesch, D.B.; Fleming, T.R.; Galiè, N.; Simonneau, G.; Ghofrani, H.A.; Oakes, M.; Layton, G.; Serdarevic-Pehar, M.; McLaughlin, V.V. Long-term treatment with sildenafil citrate in pulmonary arterial hypertension: The super-2 study. Chest 2011, 140, 1274–1283. [Google Scholar] [CrossRef] [PubMed]
- Oudiz, R.J.; Brundage, B.H.; Galiè, N.; Ghofrani, H.A.; Simonneau, G.; Botros, F.T.; Chan, M.; Beardsworth, A.; Barst, R.J.; Group, P.S. Tadalafil for the treatment of pulmonary arterial hypertension: A double-blind 52-week uncontrolled extension study. J. Am. Coll. Cardiol. 2012, 60, 768–774. [Google Scholar] [CrossRef] [PubMed]
- Rubin, L.J.; Galiè, N.; Grimminger, F.; Grünig, E.; Humbert, M.; Jing, Z.-C.; Keogh, A.; Langleben, D.; Fritsch, A.; Menezes, F. Riociguat for the treatment of pulmonary arterial hypertension: A long-term extension study (PATENT-2). Eur. Respir. J. 2015. [Google Scholar] [CrossRef] [PubMed]
- Galiè, N.; Müller, K.; Scalise, A.-V.; Grünig, E. Patent plus: A blinded, randomised and extension study of riociguat plus sildenafil in pulmonary arterial hypertension. Eur. Respir. J. 2015, 45, 1314–1322. [Google Scholar] [CrossRef] [PubMed]
- Hiremath, J.; Thanikachalam, S.; Parikh, K.; Shanmugasundaram, S.; Bangera, S.; Shapiro, L.; Pott, G.B.; Vnencak-Jones, C.L.; Arneson, C.; Wade, M. Exercise improvement and plasma biomarker changes with intravenous treprostinil therapy for pulmonary arterial hypertension: A placebo-controlled trial. J. Heart Lung Transplant. 2010, 29, 137–149. [Google Scholar] [CrossRef] [PubMed]
- Sitbon, O.; Manes, A.; Jais, X.; Pallazini, M.; Humbert, M.; Presotto, L.; de Paillette, L.; Zaccardelli, D.; Davis, G.; Jeffs, R. Rapid switch from intravenous epoprostenol to intravenous treprostinil in patients with pulmonary arterial hypertension. J. Cardiovasc. Pharmacol. Ther. 2007, 49, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Tapson, V.F.; Gomberg-Maitland, M.; McLaughlin, V.V.; Benza, R.L.; Widlitz, A.C.; Krichman, A.; Barst, R.J. Safety and efficacy of iv treprostinil for pulmonary arterial hypertension: A prospective, multicenter, open-label, 12-week trial. Chest 2006, 129, 683–688. [Google Scholar] [CrossRef] [PubMed]
- Jing, Z.-C.; Parikh, K.; Pulido, T.; Jerjes-Sanchez, C.; White, R.J.; Allen, R.; Torbicki, A.; Xu, K.-F.; Yehle, D.; Laliberte, K. Efficacy and safety of oral treprostinil monotherapy for the treatment of pulmonary arterial hypertension: A randomized controlled trial. Circulation 2013. [Google Scholar] [CrossRef] [PubMed]
- Hoeper, M.; Gall, H.; Seyfarth, H.; Halank, M.; Ghofrani, H.; Winkler, J.; Golpon, H.; Olsson, K.; Nickel, N.; Opitz, C. Long-term outcome with intravenous iloprost in pulmonary arterial hypertension. Eur. Respir. J. 2009, 34, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Galiè, N.; Palazzini, M.; Manes, A. Pulmonary arterial hypertension: From the kingdom of the near-dead to multiple clinical trial meta-analyses. Eur. Heart J. 2010, 31, 2080–2086. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, V.V.; Badesch, D.B.; Delcroix, M.; Fleming, T.R.; Gaine, S.P.; Galiè, N.; Gibbs, J.S.R.; Kim, N.H.; Oudiz, R.J.; Peacock, A. End points and clinical trial design in pulmonary arterial hypertension. J. Am. Coll. Cardiol. 2009, 54, S97–S107. [Google Scholar] [CrossRef] [PubMed]
- Kawut, S.M.; Archer-Chicko, C.L.; DeMichele, A.; Fritz, J.S.; Klinger, J.R.; Ky, B.; Palevsky, H.I.; Palmisciano, A.J.; Patel, M.; Pinder, D. Anastrozole in pulmonary arterial hypertension. A randomized, double-blind, placebo-controlled trial. Am. J. Respir. Crit. Care Med. 2017, 195, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Hoeper, M.M.; Barst, R.J.; Bourge, R.C.; Feldman, J.; Frost, A.E.; Galié, N.; Gómez-Sánchez, M.A.; Grimminger, F.; Grünig, E.; Hassoun, P.M. Imatinib mesylate as add-on therapy for pulmonary arterial hypertension: Results of the randomized impres study. Circulation 2013. [Google Scholar] [CrossRef] [PubMed]
- Spiekerkoetter, E.; Sung, Y.K.; Sudheendra, D.; Scott, V.; Del Rosario, P.; Bill, M.; Haddad, F.; Long-Boyle, J.; Hedlin, H.; Zamanian, R.T. Randomised placebo-controlled safety and tolerability trial of fk506 (tacrolimus) for pulmonary arterial hypertension. Eur. Respir. J. 2017, 50, 1602449. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).