Staphylococcus aureus Infections in Malaysia: A Review of Antimicrobial Resistance and Characteristics of the Clinical Isolates, 1990–2017
Abstract
1. Introduction
2. Antibiotic Susceptibility Profiles
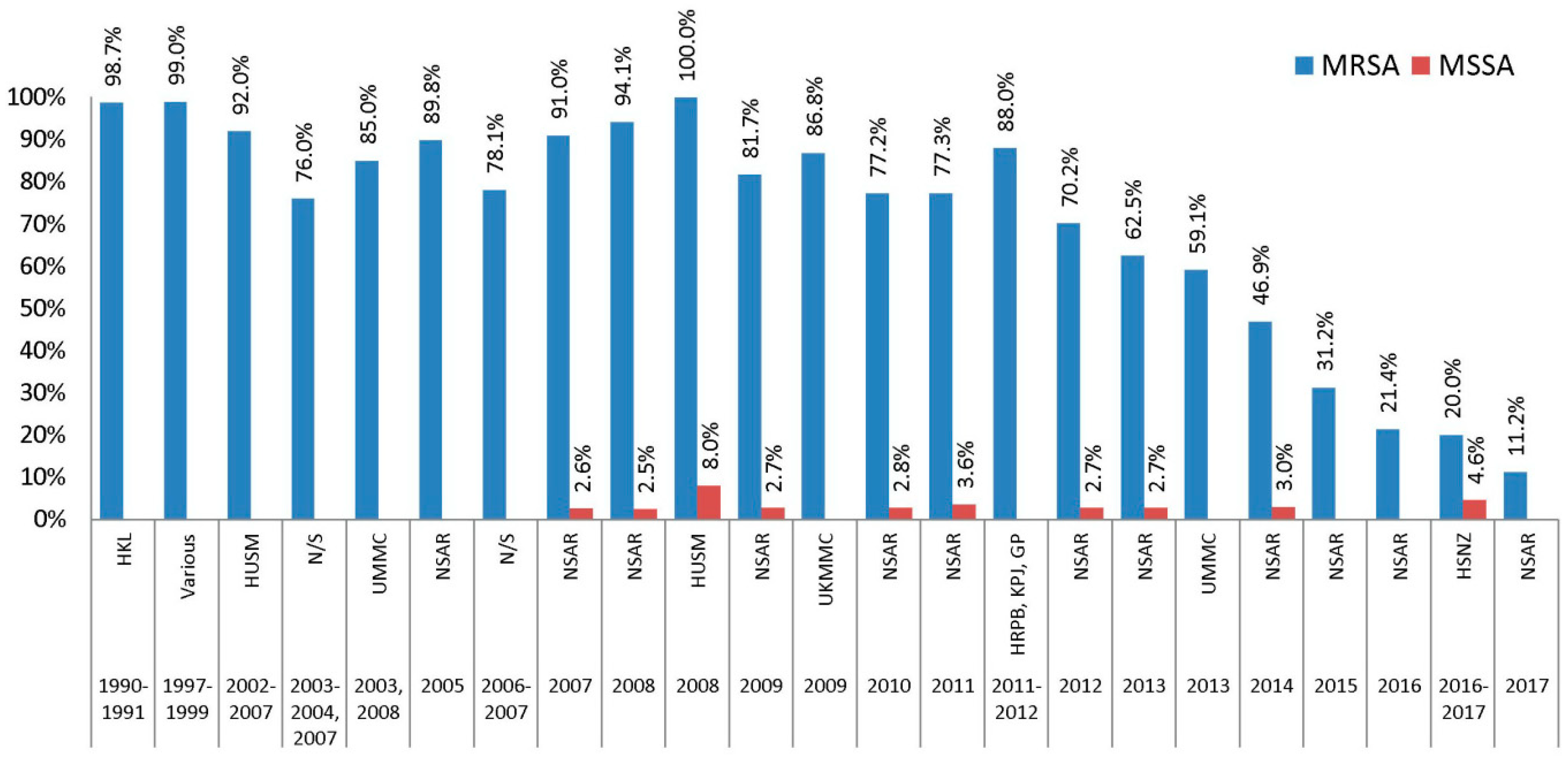
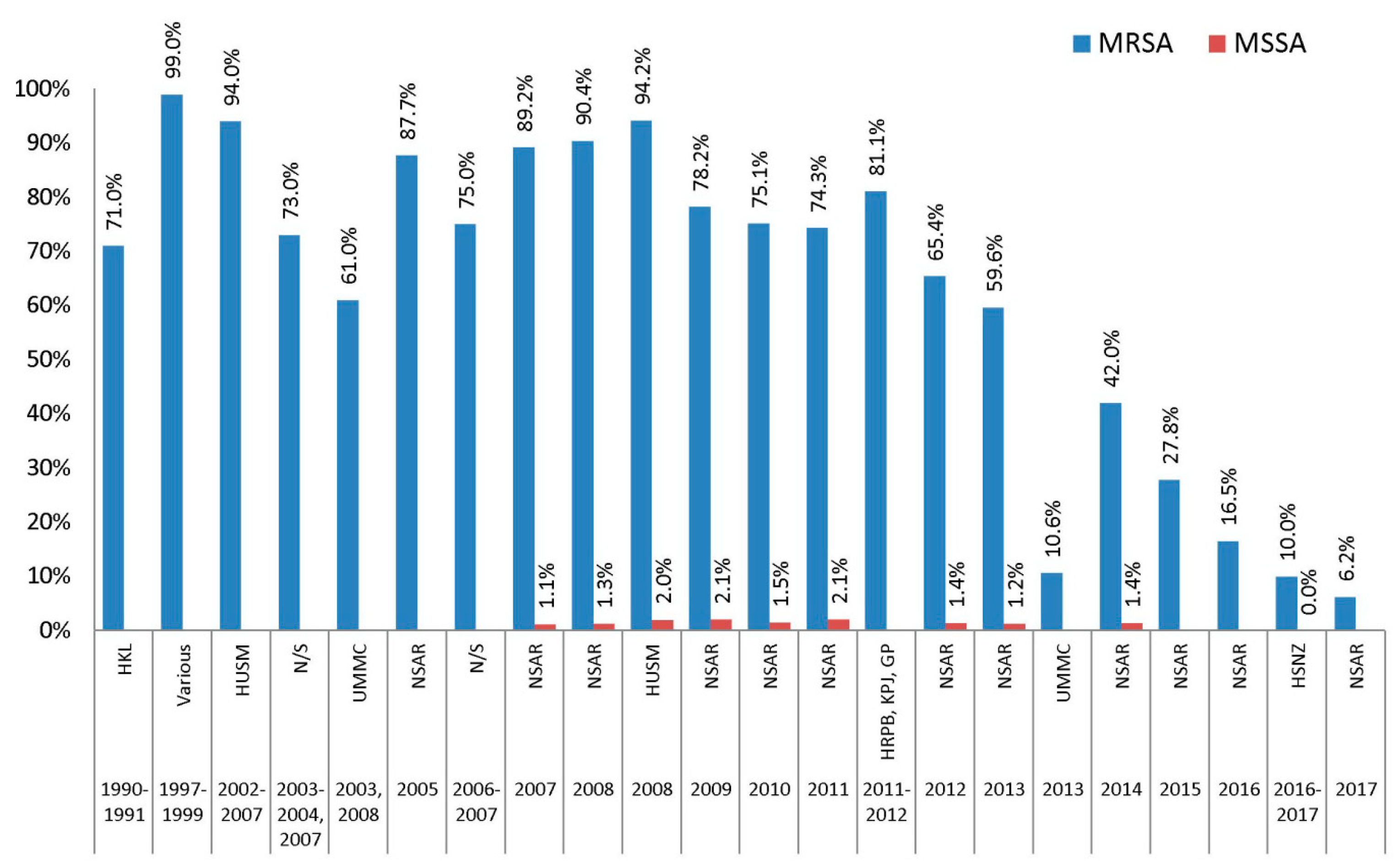
2.1. β-Lactams (Penicillin, Oxacilin, Cefoxitin, and Cefoperazone)
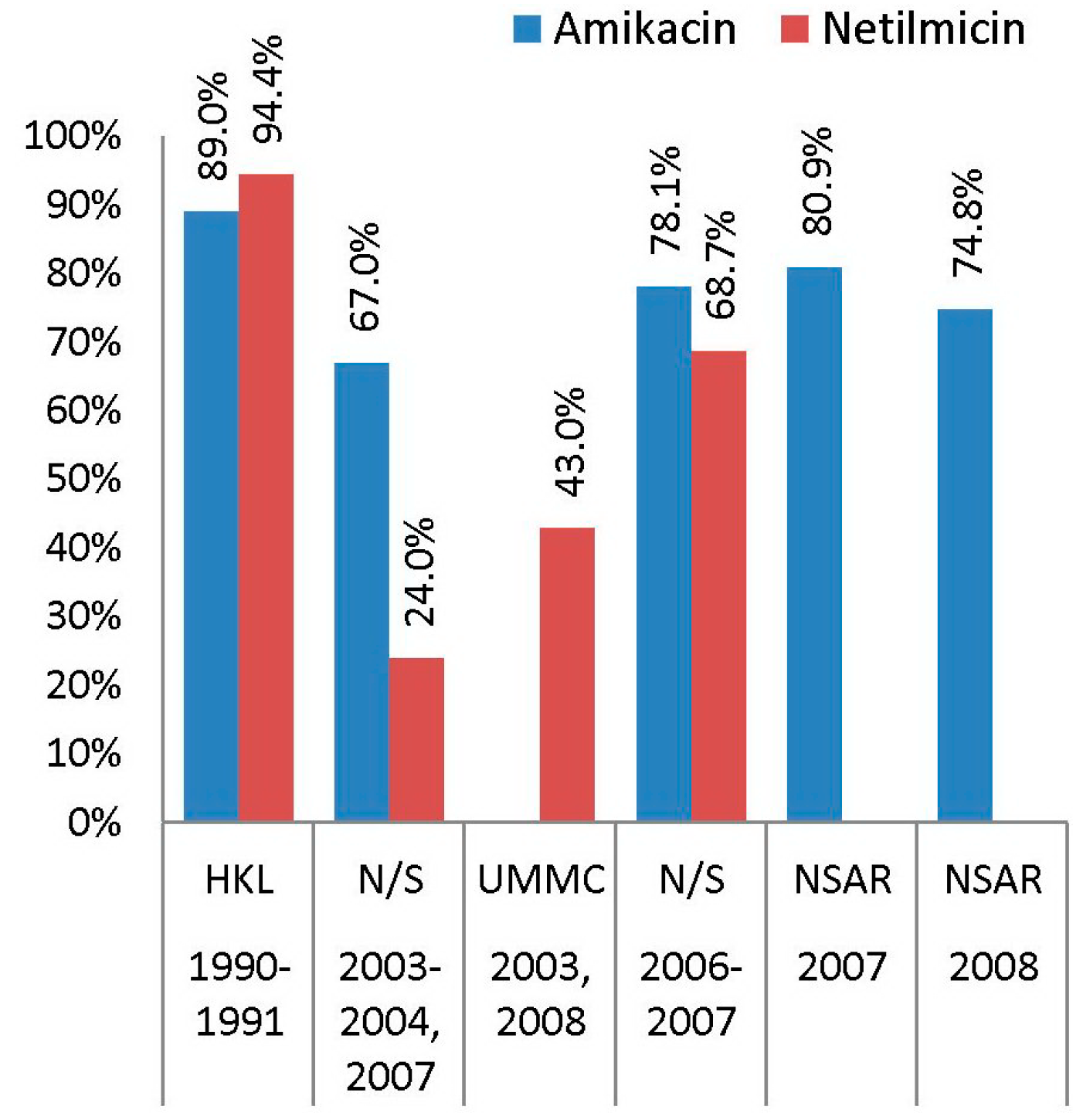
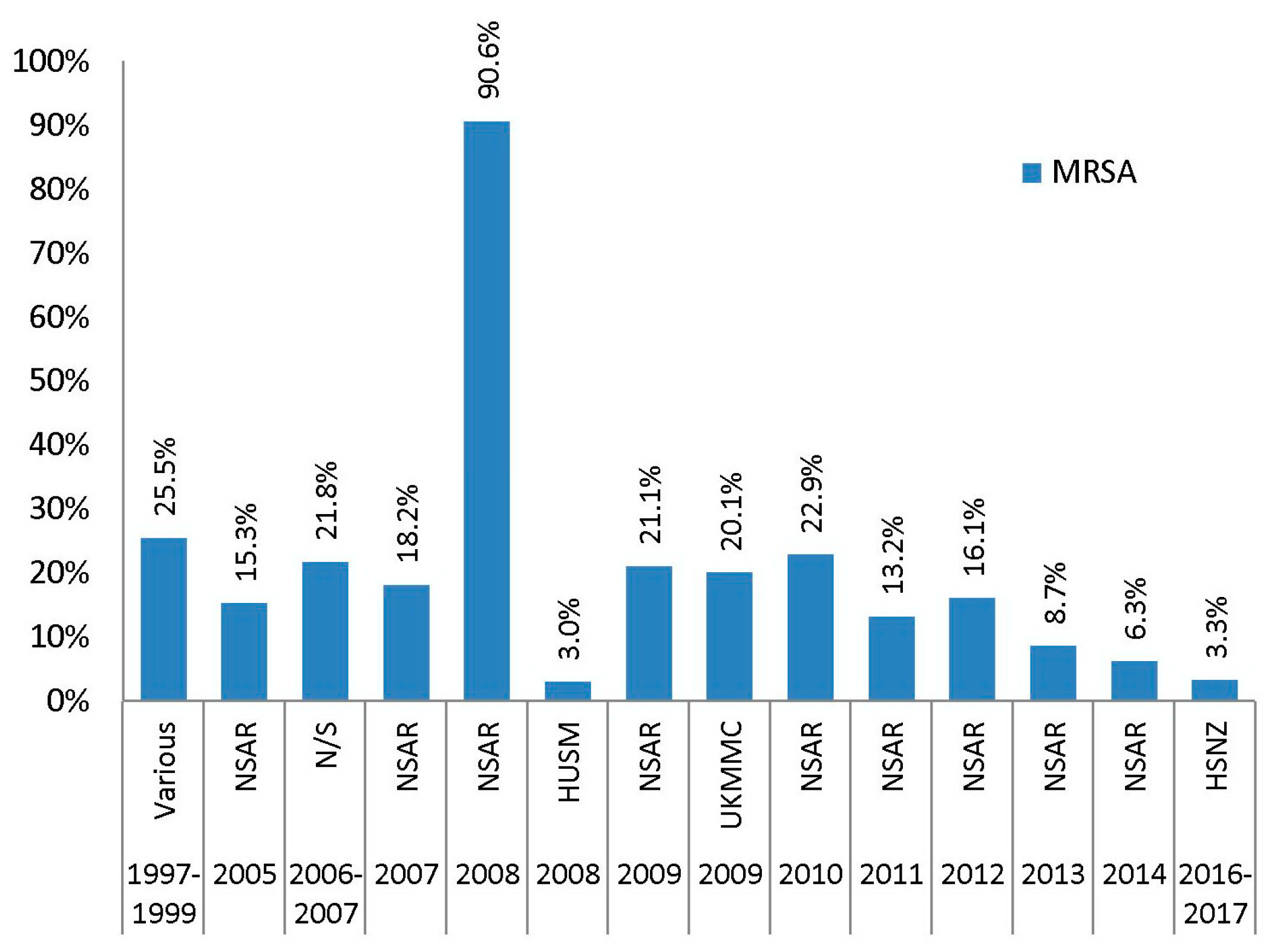
2.2. Aminoglycosides (Gentamicin, Amikacin, Netilmicin, and Kanamycin)
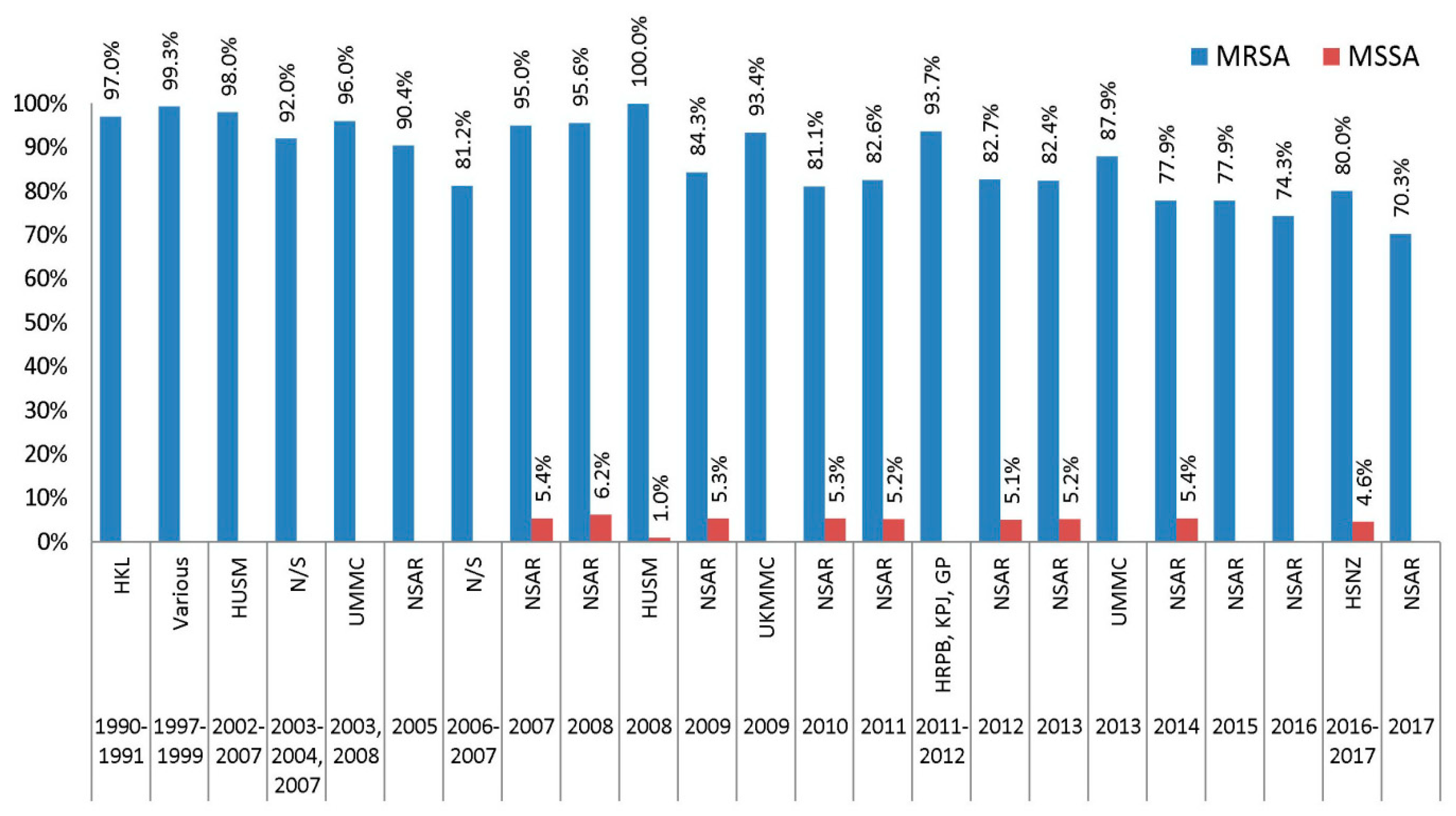
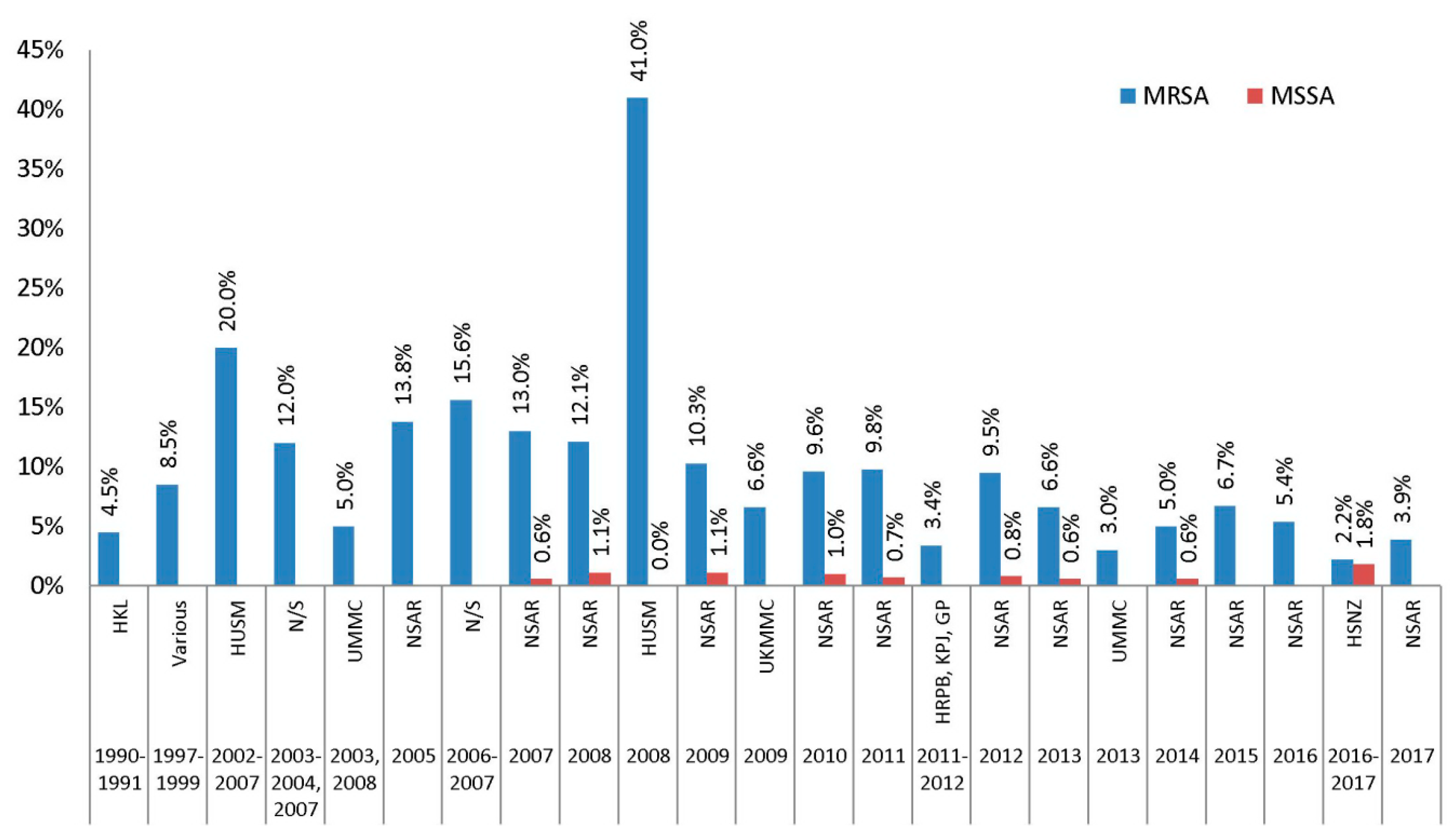
2.3. Macrolides (Erythromycin)
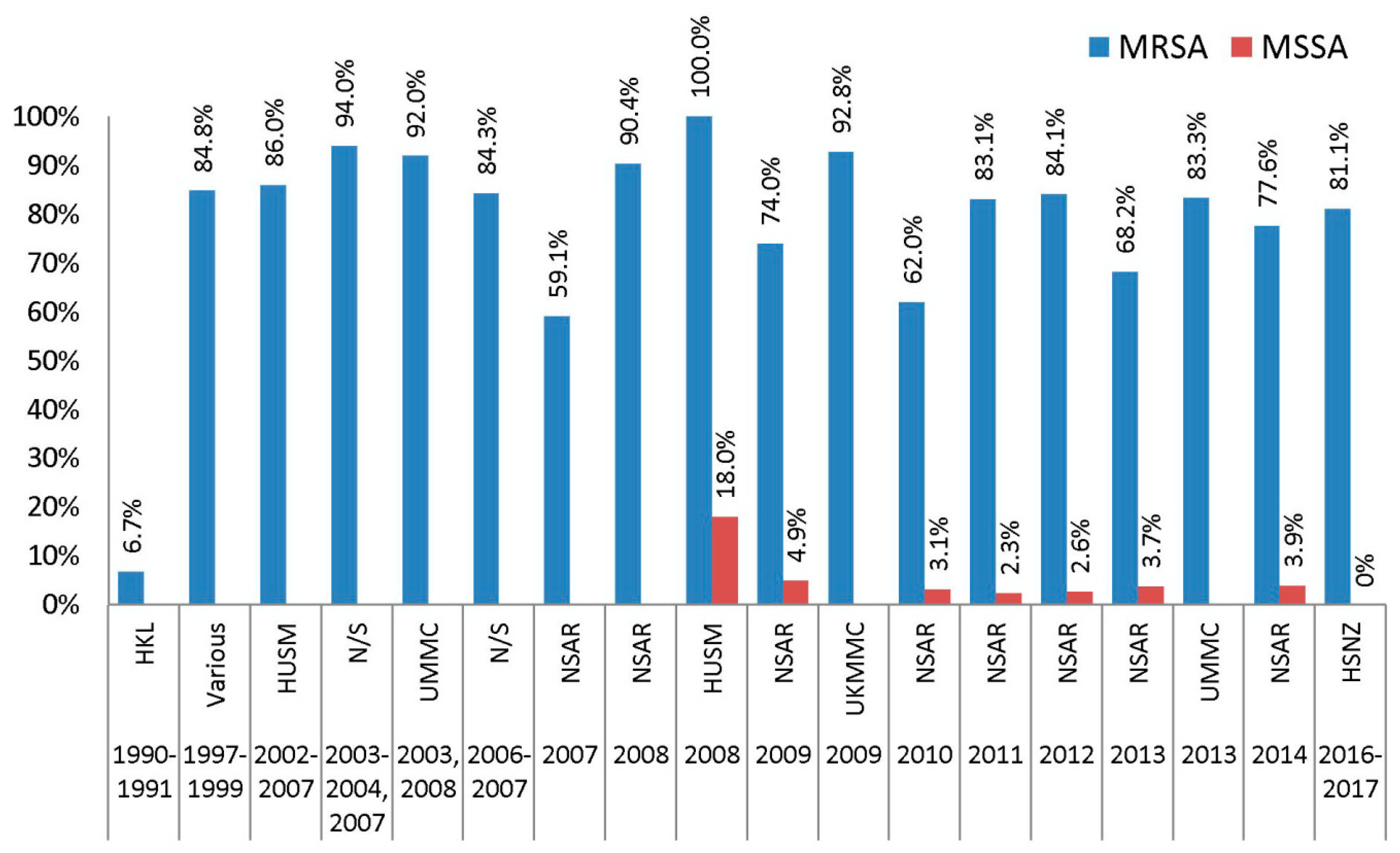
2.4. Lincosamides (Clindamycin)
2.5. Streptogramins (Quinupristin-Dalfopristin)
2.6. Macrolide-Lincosamide-Streptogramin B (MLSB) Phenotypes
2.7. Tetracyclines (Tetracycline, Doxycycline, and Minocycline)
2.8. Fluoroquinolones (Ciprofloxacin, Moxifloxacin, Norfloxacin, and Ofloxacin)
2.9. Folate Pathway Inhibitors (Co-Trimoxazole)
2.10. Phenicols (Chloramphenicol)
2.11. Ansamycins (Rifampin)
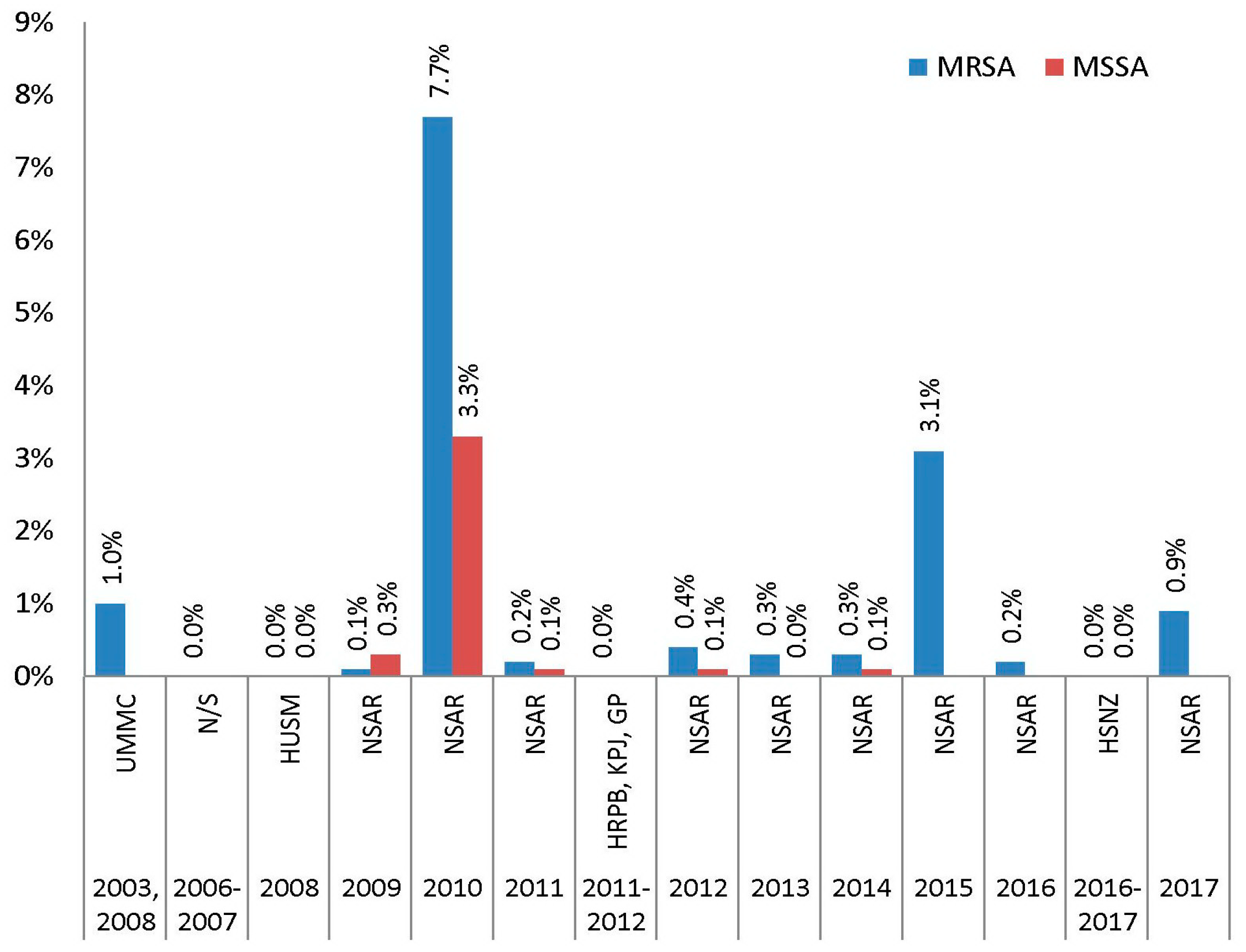
2.12. Glycopeptides (Vancomycin and Teicoplanin)
2.13. Oxazolidinones (Linezolid)
2.14. Fucidanes (Fusidic Acid)
2.15. Glycylcyclines (Tigecycline)
2.16. Lipopeptides (Daptomycin)
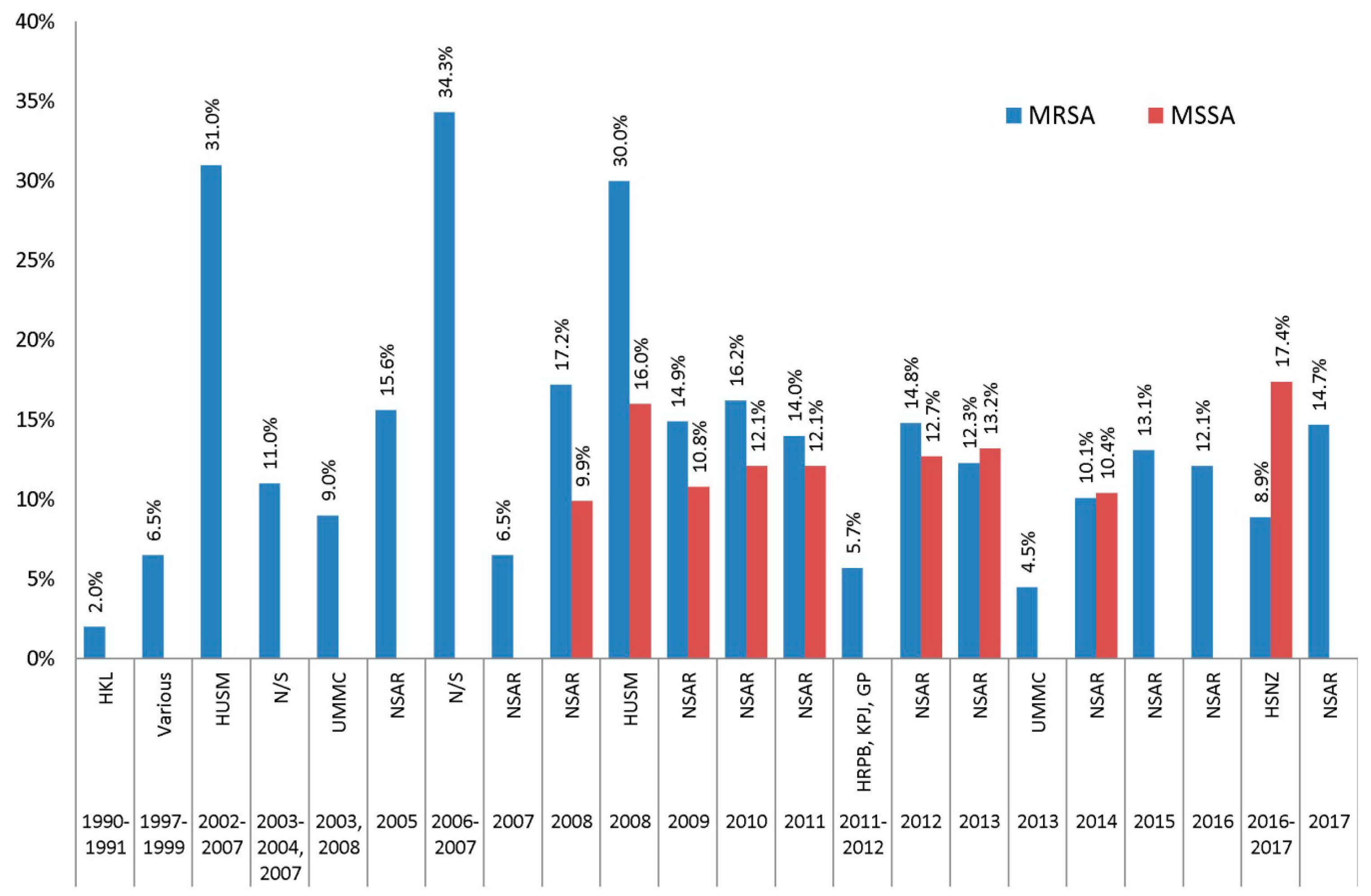
2.17. Overview of Staphylococcus aureus Antimicrobial Resistance Trends in Malaysia
3. Molecular Mechanisms of Antimicrobial Resistance
4. Clonal Types and Characteristics of Malaysian S. aureus Isolates
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ACME | Arginine Catabolic Mobile Element |
| CA | community-associated |
| CC | clonal complex |
| CDC | Centers for Disease Prevention and Control |
| CLSI | Clinical and Laboratories Standard Institute |
| cMLSB | constitutive macrolide-lincosamide-streptogramin B |
| ECDC | European Centre for Disease Prevention and Control |
| EUCAST | European Committee on Antimicrobial Susceptibility Testing |
| GP | Gribbles Pathology Ipoh |
| HA | hospital-associated |
| HKL | Hospital Kuala Lumpur |
| HRPB | Hospital Raja Permaisuri Bainun |
| HSNZ | Hospital Sultanah Nur Zahirah |
| hVISA | heterogeneous vancomycin-intermediate S. aureus |
| HUSM | Hospital Universiti Sains Malaysia |
| iMLSB | inducible macrolide-lincosamide-streptogramin B |
| IMR | Institute for Medical Research |
| KPJ | KPJ Ipoh Specialist Hospital |
| LA | livestock-associated |
| MIC | minimum inhibition concentration |
| MLSB | macrolide-lincosamide-streptogramin B |
| MRSA | methicillin-resistance S. aureus |
| MS | macrolides streptogramin |
| MSSA | methicillin-susceptible S. aureus |
| MLST | multilocus sequence typing |
| MyOHAR | Malaysian One Health Antimicrobial Resistance |
| NSAR | National Surveillance on Antimicrobial Resistance |
| PBP 2a | penicillin binding protein 2a |
| PVL | panton-valentine leucocidin |
| SCCmec | staphylococcal cassette chromosome mec |
| ST | sequence type |
| UKMMC | Universiti Kebangsaan Malaysia Medical Centre |
| UMMC | University of Malaya Medical Centre |
| VISA | vancomycin-intermediate S. aureus |
| VRSA | vancomycin-resistant S. aureus |
| WGS | whole genome sequencing |
| WHO | World Health Organization |
References
- World Health Organization. Antimicrobial Resistance: Global Report on Surveillance. 2014. Available online: https://apps.who.int/iris/bitstream/handle/10665/112642/9789241564748_eng.pdf?sequence=1 (accessed on 20 June 2019).
- Lowy, F.D. Staphylococcus Aureus Infections. N. Engl. J. Med. 1998, 339, 520–532. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.J.; Huang, Y.C. New Epidemiology of Staphylococcus Aureus Infection in Asia. Clin. Microbiol. Infect. 2014, 20, 605–623. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Malaysia. National Surveillance of Antimicrobial Resistance; 2016. Available online: https://www.imr.gov.my/images/uploads/NSAR/NSAR_2016/NSAR_report_2016.pdf (accessed on 20 June 2019).
- Ministry of Health Malaysia. National Surveillance of Antimicrobial Resistance; 2017. Available online: https://www.imr.gov.my/images/uploads/NSAR/NSAR_2017/NSAR_report_2017-edited-31.1.2019.pdf (accessed on 20 June 2019).
- Rodvold, K.A.; McConeghy, K.W. Methicillin-Resistant Staphylococcus Aureus Therapy: Past, Present and Future. Clin. Infect. Dis. 2014, 58, 20–27. [Google Scholar] [CrossRef] [PubMed]
- CDC. Staphylococcus Aureus Resistant to Vancomycin-United States, 2002. MMWR. Morb. Mortal. Wkly. Rep. 2002, 51, 565–567. [Google Scholar]
- Walters, M.S.; Eggers, P.; Albrecht, V.; Travis, T.; Lonsway, D.; Hovan, G.; Taylor, D.; Rasheed, K.; Limbago, B.; Kallen, A. Notes from the Field: Vancomycin-Resistant Staphylococcus Aureus—Delaware, 2015. Morb. Mortal. Wkly. Rep. 2015, 64, 1056. [Google Scholar] [CrossRef]
- Ramazoni, M.; Siregar, M.L.; Jamil, K.F. Vancomycin-Resistant Staphylococcus Aureus (VRSA) in Hepatic Cirrhosis Patient: A Case Report. IOP Conf. Ser. Earth Environ. Sci. 2018, 25, 012096. [Google Scholar] [CrossRef]
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing, 28th ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018. [Google Scholar]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-Resistant, Extensively Drug-Resistant and Pandrug-Resistant Bacteria: An International Expert Proposal for Interim Standard Definitions for Acquired Resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef]
- The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters, Version 8.1; 2018. Available online: http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_8.1_Breakpoint_Tables.pdf (accessed on 20 June 2019).
- Cheong, I.; Tan, S.C.; Wong, Y.H.; Zainudin, B.M.; Rahman, M.Z. Methicillin-Resistant Staphylococcus Aureus (MRSA) in a Malaysian Hospital. Med. J. Malays. 1994, 49, 24–28. [Google Scholar]
- Norazah, A.; Koh, Y.T.; Ghani Kamel, A.; Alias, R.; Lim, V.K.E. Mupirocin Resistance among Malaysian Isolates of Methicillin-Resistant Staphylococcus Aureus. Int. J. Antimicrob. Agents 2001, 17, 411–414. [Google Scholar] [CrossRef]
- Al-Talib, H.; Chan, Y.Y.; Al-Jashamy, K.; Hasan, H. Methicillin-Resistant Staphylococcus Aureus Nosocomial Infection Trends in Hospital Universiti Sains Malaysia during 2002–2007. Ann. Saudi Med. 2010, 30, 358–363. [Google Scholar] [CrossRef]
- Thong, K.L.; Junnie, J.; Liew, F.Y.; Yusof, M.Y.; Hanifah, Y.A. Antibiograms and Molecular Subtypes of Methicillin-Resistant Staphylococcus Aureus in Local Teaching Hospital, Malaysia. J. Microbiol. Biotechnol. 2009, 19, 1265–1270. [Google Scholar] [PubMed]
- Neela, V.; Sasikumar, M.; Ghaznavi, G.R.; Zamberi, S.; Mariana, S. In Vitro Activities of 28 Antimicrobial Agents against Methicillin-Resistant Staphylococcus Aureus (MRSA) from a Clinical Setting in Malaysia. Southeast Asian J. Trop. Med. Public Health 2008, 39, 885–892. [Google Scholar]
- Lim, K.T.; Hanifah, Y.A.; Mohd Yusof, M.Y.; Ito, T.; Thong, K.L. Comparison of Methicillin-Resistant Staphylococcus Aureus Strains Isolated in 2003 and 2008 with an Emergence of Multidrug Resistant ST22: SCCmec IV Clone in a Tertiary Hospital, Malaysia. J. Microbiol. Immunol. Infect. 2013, 46, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Al-Talib, H.; Al-Khateeb, A.; Hassan, H. Antimicrobial Resistance of Staphylococcus Aureus Isolates in Malaysian Tertiary Hospital. Int. Med. J. 2015, 22, 1–3. [Google Scholar]
- Noordin, A.; Sapri, H.F.; Mohamad Sani, N.A.; Leong, S.K.; Tan, X.E.; Tan, T.L.; Mohamad Zin, N.; Neoh, H.; Hussin, S. Antimicrobial Resistance Profiling and Molecular Typing of Methicillin-Resistant Staphylococcus Aureus Isolated from a Malaysian Teaching Hospital. J. Med. Microbiol. 2016, 65, 1476–1481. [Google Scholar] [CrossRef]
- Ho, W.Y.; Choo, Q.C.; Chew, C.H. Predominance of Three Closely Related Methicillin-Resistant Staphylococcus Aureus Clones Carrying a Unique CcrC-Positive SCC Mec Type III and the Emergence of Spa T304 and T690 SCC Mec Type IV Pvl + MRSA Isolates in Kinta Valley, Malaysia. Microb. Drug Resist. 2017, 23, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Sit, P.S.; Teh, C.S.J.; Idris, N.; Ponnampalavanar, S. Methicillin-Resistant Staphylococcus Aureus (MRSA) Bacteremia: Correlations between Clinical, Phenotypic, Genotypic Characteristics and Mortality in a Tertiary Teaching Hospital in Malaysia. Infect. Genet. Evol. 2018, 59, 132–141. [Google Scholar] [CrossRef]
- Che Hamzah, A.M.; Yeo, C.C.; Puah, S.M.; Chua, K.H.; Rahman, N.I.; Abdullah, F.H.; Othman, N.; Chew, C.H. Tigecycline and Inducible Clindamycin Resistance in Clinical Isolates of Methicillin-Resistant Staphylococcus Aureus from Terengganu, Malaysia. J. Med. Microbiol. 2019. [Google Scholar] [CrossRef]
- Ministry of Health Malaysia. National Surveillance of Antimicrobial Resistance 2003–2005. Available online: https://www.imr.gov.my/images/uploads/NSAR%20Archives/NSAR%20data%202002-2005.pdf (accessed on 20 June 2019).
- Ministry of Health Malaysia. National Surveillance of Antimicrobial Resistance; 2008. Available online: https://www.imr.gov.my/images/uploads/NSAR%20Archives/Summary%20of%20antibiotic%20resistance%202008.pdf (accessed on 20 June 2019).
- Ministry of Health Malaysia. National Surveillance of Antimicrobial Resistance; 2007. Available online: https://www.imr.gov.my/images/uploads/NSAR%20Archives/Summary%20of%20Antibiotic%20Resistance%202007.pdf (accessed on 20 June 2019).
- Ministry of Health Malaysia. National Surveillance of Antimicrobial Resistance; 2009. Available online: https://www.imr.gov.my/images/uploads/NSAR%20Archives/Summary%20of%20antibiotic%20resistance%202009.pdf (accessed on 20 June 2019).
- Ministry of Health Malaysia. National Surveillance of Antimicrobial Resistance; 2010. Available online: https://www.imr.gov.my/images/uploads/NSAR%20Archives/National%20Surveillance%20of%20Antibiotic%20Resistance%20report%202010.pdf (accessed on 20 June 2019).
- Ministry of Health Malaysia. National Surveillance of Antimicrobial Resistance; 2011. Available online: https://www.imr.gov.my/images/uploads/NSAR%20Archives/Summary%20of%20antibiotic%20resistance%202011.pdf (accessed on 20 June 2019).
- Ministry of Health Malaysia. National Surveillance of Antimicrobial Resistance; 2012. Available online: https://www.imr.gov.my/images/uploads/NSAR/Summary_of_antibiotic_resistance_2012_for_website.pdf (accessed on 20 June 2019).
- Ministry of Health Malaysia. National Surveillance of Antimicrobial Resistance; 2013. Available online: https://www.imr.gov.my/images/uploads/NSAR/NSAR_2013/Summary_of_NSAR_2013_report.pdf (accessed on 20 June 2019).
- Ministry of Health Malaysia. National Surveillance of Antimicrobial Resistance; 2014. Available online: https://www.imr.gov.my/images/uploads/NSAR/NSAR_2014/Summary_of_Antibiotic_Resistance_2014_report.pdf (accessed on 20 June 2019).
- Ministry of Health Malaysia. National Surveillance of Antimicrobial Resistance; 2015. Available online: https://www.imr.gov.my/images/uploads/NSAR/NSAR_2015/edited_251616_NSAR_Antibiotic_Resistance_Surveillance_data_2015.pdf (accessed on 20 June 2019).
- Wielders, C.L.C.; Fluit, A.C.; Brisse, S.; Verhoef, J.; Schmitz, F.J. MecA Gene Is Widely Disseminated in Staphylococcus Aureus Population. J. Clin. Microbiol. 2002, 40, 3970–3975. [Google Scholar] [CrossRef]
- Leclercq, R. Mechanisms of Resistance to Macrolides and Lincosamides: Nature of the Resistance Elements and Their Clinical Implications. Clin. Infect. Dis. 2002, 34, 482–492. [Google Scholar] [CrossRef]
- Drinkovic, D.; Fuller, E.R.; Shore, K.P.; Holland, D.J.; Ellis-Pegler, R. Clindamycin Treatment of Staphylococcus Aureus Expressing Inducible Clindamycin Resistance. J. Antimicrob. Chemother. 2001, 48, 315–316. [Google Scholar] [CrossRef]
- Ong, M.H.L.; Ho, W.Y.; Ng, W.W.; Chew, C.H. High Prevalence of TetM as Compared to TetK amongst Methicillin-Resistant Staphylococcus Aureus (MRSA) Isolates from Hospitals in Perak, Malaysia. Jundishapur J. Microbiol. 2017, 10, e13935. [Google Scholar]
- Norazah, A.; Lim, V.K.E.; Rohani, M.Y.; Kamel, A.G.M. In-Vitro Activity of Quinupristin/Dalfopristin, Levofloxacin and Moxifloxacin against Fusidic Acid and Rifampicin-Resistant Strains of Methicillin-Resistant Staphylococcus Aureus (MRSA) from Malaysian Hospitals. Med. J. Malays. 2005, 60, 411–415. [Google Scholar]
- Hiramatsu, K. Vancomycin-Resistant Staphylococcus Aureus: A New Model of Antibiotic Resistance. Lancet Infect. Dis. 2001, 1, 147–155. [Google Scholar] [CrossRef]
- Ramli, S.R.; Neoh, H.M.; Aziz, M.N.; Hussin, S. Screening and Detection of Heterogenous Vancomycin Intermediate Staphylococcus Aureus in Hospital Kuala Lumpur Malaysia, Using the Glycopeptide Resistance Detection Etest and Population Analysis Profiling. Infect. Dis. Rep. 2012, 4, e20. [Google Scholar] [CrossRef]
- Hashim, R.; Hamzah, H.H.; Dahalan, N.A.; Amran, F.; Ahmad, N.; Hazwani, N.Z.; Baharudin, S.; Zainal, S.; Raj, A.S.S. Vancomycin-Intermediate Staphylococcus Aureus in Malaysia: A Case Study. J. Clin. Case Reports 2018, 8, 1178. [Google Scholar]
- Atshan, S.S.; Nor Shamsudin, M.; Lung, L.T.T.; Sekawi, Z.; Pei Pei, C.; Karunanidhi, A.; Jeevajothi Nathan, J.; Mateg Ali, A.; Ghaznavi-Rad, E.; Abduljaleel, S.A.; et al. Genotypically Different Clones of Staphylococcus Aureus Are Diverse in the Antimicrobial Susceptibility Patterns and Biofilm Formations. Biomed Res. Int. 2013, 2013, 515712. [Google Scholar] [CrossRef]
- Ministry of Health Malaysia. National Antibiotic Guideline; 2014. Available online: https://www.pharmacy.gov.my/v2/sites/default/files/document-upload/national-antibiotic-guideline-2014-full-versionjun2015_1.pdf (accessed on 20 June 2019).
- Ministry of Health Malaysia. Protocol on Antimicrobial Stewardship Program in Healthcare Facilities; 2014. Available online: https://www.pharmacy.gov.my/v2/sites/default/files/document-upload/protocol-antimicrobial-stewardship.pdf (accessed on 20 June 2019).
- Sing, D.Y.F.; Boo, Y.L.; Mukhlis, R.; Chin, P.W.; Hoo, F.K. Antimicrobial Stewardship Program in a Malaysian District Hospital: First Year Experience. Pakistan J. Med. Sci. 2016, 32, 999–1004. [Google Scholar] [CrossRef]
- Gerald, N.M.J. Malaysian Action Plan on Antimicrobial Resistance (MyAP-AMR) 2017–2021; 2018. Available online: http://www.moh.gov.my/moh/resources/Penerbitan/Garis%20Panduan/Garis%20panduan%20Umum%20(Awam)/National_Action_Plan_-_FINAL_29_june.pdf (accessed on 20 June 2019).
- Kanjilal, S.; Sater, M.R.A.; Thayer, M.; Lagoudas, G.K.; Kim, S.; Blainey, P.C.; Grad, Y.H. Trends in Antibiotic Susceptibility in Staphylococcus Aureus in Boston, Massachusetts, from 2000 to 2014. J. Clin. Microbiol. 2018, 56, e01160-17. [Google Scholar] [CrossRef]
- Chen, K.; Huang, Y.; Song, Q.; Wu, C.; Chen, X.; Zeng, L. Drug-Resistance Dynamics of Staphylococcus Aureus between 2008 and 2014 at a Tertiary Teaching Hospital, Jiangxi Province, China. BMC Infect. Dis. 2017, 17, 97. [Google Scholar] [CrossRef]
- Malaysian Society of Intensive Care. Guide to Antimicrobial Therapy in the Adult ICU. 2017. Available online: http://www.msic.org.my/download/AntibioticGuidelines.pdf (accessed on 20 June 2019).
- Amorim, M.L.; Faria, N.A.; Oliveira, D.C.; Vasconcelos, C.; Cabeda, J.C.; Mendes, A.C.; Calado, E.; Castro, A.P.; Ramos, M.H.; Amorim, J.M.; et al. Changes in the Clonal Nature and Antibiotic Resistance Profiles of Methicillin-Resistant Staphylococcus Aureus Isolates Associated with Spread of the EMRSA-15 Clone in a Tertiary Care Portuguese Hospital. J. Clin. Microbiol. 2007, 45, 2881–2888. [Google Scholar] [CrossRef]
- Dai, Y.; Liu, J.; Guo, W.; Meng, H.; Huang, Q.; He, L.; Gao, Q.; Lv, H.; Liu, Y.; Wang, Y.; et al. Decreasing Methicillin-Resistant Staphylococcus Aureus (MRSA) Infections Is Attributable to the Disappearance of Predominant MRSA ST239 Clones, Shanghai, 2008-2017. Emerg. Microbes Infect. 2019, 8, 471–478. [Google Scholar] [CrossRef]
- Lim, K.T.; Hanifah, Y.A.; Yusof, M.Y.M.; Thong, K.L. ErmA, ErmC, TetM and TetK Are Essential for Erythromycin and Tetracycline Resistance among Methicillin-Resistant Staphylococcus Aureus Strains Isolated from a Tertiary Hospital in Malaysia. Indian J. Med. Microbiol. 2012, 30, 203–207. [Google Scholar] [CrossRef]
- Naglich, J.G.; Andrews, R.E. Introduction of the Streptococcus Faecalis Transposon Tn916 into Bacillus Thuringiensis Subsp. Israelensis. Plasmid 1988, 19, 84–93. [Google Scholar] [CrossRef]
- Villedieu, A.; Diaz-Torres, M.L.; Hunt, N.; McNab, R.; Spratt, D.A.; Wilson, M.; Mullany, P. Prevalence of Tetracycline Resistance Genes in Oral Bacteria. Antimicrob. Agents Chemother. 2003, 47, 878–882. [Google Scholar] [CrossRef]
- Suhaili, Z.; Rafee, P.A.; Mat Azis, N.; Yeo, C.C.; Nordin, S.A.; Abdul Rahim, A.R.; Al-Obaidi, M.M.J.; Mohd Desa, M.N. Characterization of Resistance to Selected Antibiotics and Panton-Valentine Leukocidin-Positive Staphylococcus Aureus in a Healthy Student Population at a Malaysian University. Germs 2018, 8, 21–30. [Google Scholar] [CrossRef]
- Costa, S.S.; Viveiros, M.; Amaral, L.; Couto, I. Multidrug Efflux Pumps in Staphylococcus Aureus: An Update. Open Microbiol. J. 2013, 7, 59–71. [Google Scholar] [CrossRef]
- Deng, X.; Sun, F.; Ji, Q.; Liang, H.; Missiakas, D.; Lan, L.; He, C. Expression of Multidrug Resistance Efflux Pump Gene NorA Is Iron Responsive in Staphylococcus Aureus. J. Bacteriol. 2012, 194, 1753–1762. [Google Scholar] [CrossRef]
- Huang, J.; O’Toole, P.W.; Shen, W.; Amrine-Madsen, H.; Jiang, X.; Lobo, N.; Palmer, L.M.; Voelker, L.; Fan, F.; Gwynn, M.N.; et al. Novel Chromosomally Encoded Multidrug Efflux Transporter MdeA in Staphylococcus Aureus. Antimicrob. Agents Chemother. 2004, 48, 909–917. [Google Scholar] [CrossRef]
- Saiful, A.J.; Mastura, M.; Zarizal, S.; Mazurah, M.I.; Shuhaimi, M.; Ali, A.M. Efflux Genes and Active Efflux Activity Detection in Malaysian Clinical Isolates of Methicillin-Resistant Staphylococcus Aureus (MRSA). J. Basic Microbiol. 2008, 48, 245–251. [Google Scholar] [CrossRef]
- CDC. Active Bacterial Core Surveillance Report, Emerging Infections Program Network, Methicillin-Resistant Staphylococcus Aureus; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2015.
- Nathwani, D.; Morgan, M.; Masterton, R.G.; Dryden, M.; Cookson, B.D.; French, G.; Lewis, D. Guidelines for UK Practice for the Diagnosis and Management of Methicillin-Resistant Staphylococcus Aureus (MRSA) Infections Presenting in the Community. J. Antimicrob. Chemother. 2008, 61, 976–994. [Google Scholar] [CrossRef]
- Stryjewski, M.E.; Chambers, H.F. Skin and Soft-tissue Infections Caused by Community-acquired Methicillin-resistant Staphylococcus Aureus. Clin. Infect. Dis. 2008, 46, S368–S377. [Google Scholar] [CrossRef]
- Kilic, A.; Li, H.; Stratton, C.W.; Tang, Y.-W. Antimicrobial Susceptibility Patterns and Staphylococcal Cassette Chromosome Mec Types of, as Well as Panton-Valentine Leukocidin Occurrence among, Methicillin-Resistant Staphylococcus Aureus Isolates from Children and Adults in Middle Tennessee. J. Clin. Microbiol. 2006, 44, 4436–4440. [Google Scholar] [CrossRef]
- Enright, M.C.; Robinson, D.A.; Randle, G.; Feil, E.J.; Grundmann, H.; Spratt, B.G. The Evolutionary History of Methicillin-Resistant Staphylococcus Aureus (MRSA). Proc. Natl. Acad. Sci. USA 2002, 99, 7687–7692. [Google Scholar] [CrossRef]
- Oliveira, D.C.; Tomasz, A.; de Lencastre, H. The Evolution of Pandemic Clones of Methicillin-Resistant Staphylococcus Aureus: Identification of Two Ancestral Genetic Backgrounds and the Associated Mec Elements. Microb. Drug Resist. 2001, 7, 349–361. [Google Scholar] [CrossRef]
- Oliveira, D.C.; Tomasz, A.; de Lencastre, H. Secrets of Success of a Human Pathogen: Molecular Evolution of Pandemic Clones of Meticillin-Resistant Staphylococcus Aureus. Lancet Infect. Dis. 2002, 2, 180–189. [Google Scholar] [CrossRef]
- Ghaznavi-Rad, E.; Shamsudin, M.N.; Sekawi, Z.; Khoon, L.Y.; Aziz, M.N.; Hamat, R.A.; Othman, N.; Chong, P.P.; Van Belkum, A.; Ghasemzadeh-Moghaddam, H.; et al. Predominance and Emergence of Clones of Hospital-Acquired Methicillin-Resistant Staphylococcus Aureus in Malaysia. J. Clin. Microbiol. 2010, 48, 867–872. [Google Scholar] [CrossRef]
- Neela, V.; Ghasemzadeh Moghaddam, H.; Van Belkum, A.; Horst-Kreft, D.; Mariana, N.S.; Ghaznavi Rad, E. First Report on Methicillin-Resistant Staphylococcus Aureus of Spa Type T037, Sequence Type 239, SCCmec Type III/IIIA in Malaysia. Eur. J. Clin. Microbiol. Infect. Dis. 2010, 29, 115–117. [Google Scholar] [CrossRef][Green Version]
- Ahmad, N.; Ruzan, I.N.; Ghani, M.K.A.; Hussin, A.; Nawi, S.; Aziz, M.N.; Maning, N.; Eow, V.L.K. Characteristics of Community- and Hospital-Acquired Meticillin-Resistant Staphylococcus Aureus Strains Carrying SCCmec Type IV Isolated in Malaysia. J. Med. Microbiol. 2009, 58, 1213–1218. [Google Scholar] [CrossRef]
- Suhaili, Z.; Lean, S.S.; Yahya, A.; Mohd Desa, M.N.; Ali, A.M.; Yeo, C.C. Draft Genome Sequence of Methicillin-Resistant Staphylococcus Aureus KT/Y21, a Sequence Type 772 (ST772) Strain Isolated from a Pediatric Blood Sample in Terengganu, Malaysia. Genome Announc. 2014, 2, e00271–e14. [Google Scholar] [CrossRef]
- Suhaili, Z.; Lean, S.S.; Mohamad, N.M.; Abdul Rachman, A.R.; Mohd Desa, M.N.; Yeo, C.C. Draft Genome Sequence of Staphylococcus Aureus KT/312045, an ST1-MSSA PVL Positive Isolated from Pus Sample in East Coast Malaysia. Genom. Data 2016, 9, 111–112. [Google Scholar] [CrossRef][Green Version]
- Hsu, L.Y.; Harris, S.R.; Chlebowicz, M.A.; Lindsay, J.A.; Koh, T.H.; Krishnan, P.; Tan, T.Y.; Hon, P.Y.; Grubb, W.B.; Bentley, S.D.; et al. Evolutionary Dynamics of Methicillin-Resistant Staphylococcus Aureus within a Healthcare System. Genome Biol. 2015, 16, 81. [Google Scholar] [CrossRef]
- Knight, G.M.; Budd, E.L.; Whitney, L.; Thornley, A.; Al-Ghusein, H.; Planche, T.; Lindsay, J.A. Shift in Dominant Hospital-Associated Methicillin-Resistant Staphylococcus Aureus (HA-MRSA) Clones over Time. J. Antimicrob. Chemother. 2012, 67, 2514–2522. [Google Scholar] [CrossRef]
- Sam, I.C.; Kahar-Bador, M.; Chan, Y.F.; Loong, S.K.; Mohd Nor Ghazali, F. Multisensitive Community-Acquired Methicillin-Resistant Staphylococcus Aureus Infections in Malaysia. Diagn. Microbiol. Infect. Dis. 2008, 62, 437–439. [Google Scholar] [CrossRef]
- Lim, K.T.; Hanifah, Y.A.; Mohd Yusof, M.Y.; Goering, R.V.; Thong, K.L. Temporal Changes in the Genotypes of Methicillin-Resistant Staphylococcus Aureus Strains Isolated from a Tertiary Malaysian Hospital Based on MLST, Spa, and Mec-Associated Dru Typing. Diagn. Microbiol. Infect. Dis. 2012, 74, 106–112. [Google Scholar] [CrossRef]
- Ghasemzadeh-Moghaddam, H.; Ghaznavi-Rad, E.; Sekawi, Z.; Yun-Khoon, L.; Aziz, M.N.; Hamat, R.A.; Melles, D.C.; van Belkum, A.; Shamsudin, M.N.; Neela, V. Methicillin-Susceptible Staphylococcus Aureus from Clinical and Community Sources Are Genetically Diverse. Int. J. Med. Microbiol. 2011, 301, 347–353. [Google Scholar] [CrossRef]
- Lim, K.T.; Yeo, C.C.; Suhaili, Z.; Thong, K.L. Comparison of Methicillin-Resistant and Methicillin-Sensitive Staphylococcus Aureus Strains Isolated from a Tertiary Hospital in Terengganu, Malaysia. Jpn. J. Infect. Dis. 2012, 65, 502–509. [Google Scholar] [CrossRef]
- Samat Muttaqillah, N.A.; Hussin, S.; Neoh, H.M.; Noordin, A.; Ding, C.H.; Wahab, A.A.; Rahman, M.M. Clonal Diversity of Methicillin-Resistant Staphylococcus Aureus in UKM Medical Centre: Characterisation by Multilocus Sequence Typing of Different SCCmec Type Representatives. Sains Malays. 2015, 44, 1315–1323. [Google Scholar] [CrossRef]
- Mustafa, M.I.; Alarosi, N.A.; Amjad, N. Staphylococcal Cassette Chroromosome Mec (SCCmec) Typing of Methicillin-Resistant Staphylococcus Aureus (MRSA) Isolates from Patients Attending Tengku Ampuan Afzan Hospital (HTAA) in Kuantan, Pahang, Malaysia. Int. J. Infect. Dis. 2012, 16, e426. [Google Scholar] [CrossRef][Green Version]
- Sit, P.S.; Teh, C.S.J.; Idris, N.; Sam, I.C.; Syed Omar, S.F.; Sulaiman, H.; Thong, K.L.; Kamarulzaman, A.; Ponnampalavanar, S. Prevalence of Methicillin-Resistant Staphylococcus Aureus (MRSA) Infection and the Molecular Characteristics of MRSA Bacteraemia over a Two-Year Period in a Tertiary Teaching Hospital in Malaysia. BMC Infect. Dis. 2017, 17, 274. [Google Scholar] [CrossRef]
- Amit, L.N.; Yung, C.V.L.; Moy, F.S.; John, D.V. Molecular Characteristics of Infection and Colonization Isolates of Community-Acquired Methicillin-Resistant Staphylococcus Aureus (CA-MRSA). Trop. Biomed. 2018, 35, 442–452. [Google Scholar]
- Aklilu, E.; Ab Manah, H.A.; Abu Daud, N. Presence of Antimicrobial Resistant Staphylococcus Aureus in Chicken Meat and Its Potential Public Health Implications. Malays. J. Microbiol. 2016, 12, 418–422. [Google Scholar]
- Saleha, A.A.; Shamzarina, M.; Fauziah, O.; Zunita, Z. Methicillin-Resistant Staphylococcus Aureus (MRSA) Isolated from Pet Animals and Pet and Non-Pet Owners. J. Vet. Malays. 2006, 18, 13–16. [Google Scholar]
- Ng, W.S.J.; Zunita, Z.; Goh, Y.M.; Raha, A.R. Occurrence of Methicillin-Resistant Staphylococcus Aureus (MRSA) in Cats and Dogs. In Proceedings of the 17th Veterinary Association Malaysia Congress, Kuala Lumpur, Malaysia, 27–30 July 2005; pp. 43–45. [Google Scholar]
- Abdulkadir, M.M.; Zunita, Z.; Goh, Y.M.; Saleha, A.A.; Son, R. Occurrence of Methicillin-Resistant Staphylococcus Aureus (MRSA) in Chickens. In Proceedings of the 19th Veterinary Association Malaysia Congress, Kuala Lumpur, Malaysia, 3–5 August 2007; pp. 182–185. [Google Scholar]
- Khairina, A.K.; Zunita, Z.; Ooi, P.T. Methicillin-Resistant Staphylococcus in Pigs. Emerg. Infect. Dis. 2005, 11, 1965. [Google Scholar]
- Aklilu, E.; Zunita, Z.; Hassan, L.; Chen, H.C. Phenotypic and Genotypic Characterization of Methicillin-Resistant Staphylococcus Aureus (MRSA) Isolated from Dogs and Cats at University Veterinary Hospital, Universiti Putra Malaysia. Trop. Biomed. 2010, 27, 483–492. [Google Scholar]
- Zunita, Z.; Bashir, A.; Hafizal, A. Occurrence of Multidrug Resistant Staphylococcus Aureus in Horses in Malaysia. Vet. World 2008, 1, 165–167. [Google Scholar]
- Neela, V.; Ghaznavi-Rad, E.; Ghasemzadeh-Moghaddama, H.; Nor Shamsudin, M.; van Belkum, A.; Karunanidhi, A. Frequency of Methicillin Resistant Staphylococcus Aureus in the Noses of Malaysian Chicken Farmers and Their Chicken. Iran. J. Vet. Res. 2013, 14, 226–231. [Google Scholar]
- Kanagarajah, R.R.; Lee, D.C.W.; Lee, D.Z.F.; Yusoff, K.; Paramasivam, S.J.; Low, W.Y.; Jeevaratnam, K.; Lim, S.H.E. Antibiotic Profiling of Methicillin Resistant Staphylococcus Aureus (MRSA) Isolates in Stray Canines and Felines. Cogent Biol. 2017, 3. [Google Scholar] [CrossRef]
- Neela, V.; Mohd Zafrul, A.; Mariana, N.S.; van Belkum, A.; Liew, Y.K.; Rad, E.G. Prevalence of ST9 Methicillin-Resistant Staphylococcus Aureus among Pigs and Pig Handlers in Malaysia. J. Clin. Microbiol. 2009, 47, 4138–4140. [Google Scholar] [CrossRef]
- Khalid, K.A.; Zakaria, Z.; Toung, O.P.; McOrist, S. Low Levels of Meticillin-Resistant Staphylococcus Aureus in Pigs in Malaysia. Vet. Rec. 2009, 164, 626–627. [Google Scholar] [CrossRef]
- Chongtrakool, P.; Ito, T.; Ma, X.X.; Kondo, Y.; Trakulsomboon, S.; Tiensasitorn, C.; Jamklang, M.; Chavalit, T.; Song, J.H.; Hiramatsu, K. Staphylococcal Cassette Chromosome mec (SCCmec) Typing of Methicillin-Resistant Staphylococcus aureus Strains Isolated in 11 Asian Countries: A Proposal for a New Nomenclature for SCCmec Elements. Antimicrob. Agents Chemother. 2006, 50, 1001–1012. [Google Scholar] [CrossRef]
- Nor Shamsudin, M.; Sekawi, Z.; van Belkum, A.; Neela, V. First Community-Acquired Methicillin-Resistant Staphylococcus Aureus in Malaysia. J. Med. Microbiol. 2008, 57, 1180–1181. [Google Scholar] [CrossRef]
- Rashid, Z.Z.; Bahari, N.; Othman, A.; Jaafar, R.; Mohamed, N.A.; Jabbari, I.; Sulong, A.; Hashim, R.; Ahmad, N. Community-Acquired Methicillin-Resistant Staphylococcus Aureus in a Malaysian Tertiary Centre. Southeast Asian J. Trop. Med. Public Health 2013, 44, 104–108. [Google Scholar]
- Chan, C.; Merican, A.; Nawar, A.; Hanifah, Y.A.; Thong, K.L. Necrotising Fasciitis of the Lower Limb Caused by Community-Acquired Methicillin-Resistant Staphylococcus Aureus. Malaysian Orthop. J. 2010, 4, 36–38. [Google Scholar] [CrossRef]
- Cunningham, S.A.; Chia, N.; Jeraldo, P.R.; Quest, D.J.; Johnson, J.A.; Boxrud, D.J.; Taylor, A.J.; Chen, J.; Jenkins, G.D.; Drucker, T.M.; et al. Comparison of Whole-Genome Sequencing Methods for Analysis of Three Methicillin-Resistant Staphylococcus Aureus Outbreaks. J. Clin. Microbiol. 2017, 55, 1946–1953. [Google Scholar] [CrossRef]
- Toleman, M.S.; Watkins, E.R.; Williams, T.; Blane, B.; Sadler, B.; Harrison, E.M.; Coll, F.; Parkhill, J.; Nazareth, B.; Brown, N.M.; et al. Investigation of a Cluster of Sequence Type 22 Methicillin-Resistant Staphylococcus Aureus Transmission in a Community Setting. Clin. Infect. Dis. 2017, 65, 2069–2077. [Google Scholar] [CrossRef]
- Lee, L.; Teh, L.; Zainuddin, Z.; Salleh, M. The Genome Sequence of a Type ST239 Methicillin-Resistant Staphylococcus Aureus Isolate from a Malaysian Hospital. Stand. Genomic. Sci. 2014, 9, 933–939. [Google Scholar] [CrossRef][Green Version]
- Neoh, H.M.; Mohamed-Hussein, Z.A.; Tan, X.E.; B Raja Abd Rahman, R.M.F.; Hussin, S.; Mohamad Zin, N.; Jamal, R. Draft Genome Sequences of Four Nosocomial Methicillin-Resistant Staphylococcus Aureus (MRSA) Strains (PPUKM-261-2009, PPUKM-332-2009, PPUKM-377-2009, and PPUKM-775-2009) Representative of Dominant MRSA Pulsotypes Circulating in a Malaysian University Teaching Hospital. Genome Announc. 2013, 1, e00103-12. [Google Scholar]
- World Health Organization. Global Action Plan on Antimicrobial Resistance. 2015. Available online: http://www.wpro.who.int/entity/drug_resistance/resources/global_action_plan_eng.pdf (accessed on 20 June 2019).
- Mattar, C.; Ore, A.S.; Fagerberg, S.K.; Ramachandran, R.; Tun, W.; Wiley, E.; Chapman, H.J. One Health and Antimicrobial Resistance. World Med. J. 2016, 62, 108–111. [Google Scholar]
- Cuny, C.; Wieler, L.H.; Witte, W. Livestock-Associated MRSA: The Impact on Humans. Antibiotics 2015, 4, 521–543. [Google Scholar] [CrossRef]
- Butaye, P.; Argudín, M.A.; Smith, T.C. Livestock-Associated MRSA and Its Current Evolution. Curr. Clin. Microbiol. Rep. 2016, 3, 19–31. [Google Scholar] [CrossRef]


| Antimicrobial Category | Antimicrobial Agent | CLSI Breakpoint | EUCAST Breakpoint | Reported by Malaysian NSAR |
|---|---|---|---|---|
| Aminoglycosides | Gentamicin | Yes | Yes | 2005–2017 |
| Ansamycins | Rifampin/rifampicin | Yes | Yes | 2005–2017 |
| Anti-MRSA cephalosporins | Ceftaroline | Yes | Yes | No |
| Anti-staphylococcal β-lactams (or cephamycins) | Oxacillin (or cefoxitin) | Yes | Yes | 2003–2005 |
| Fluoroquinolones | Ciprofloxacin | Yes | Yes | 2007–2014 |
| Moxifloxacin | Yes | Yes | No | |
| Folate pathway inhibitors | Trimethoprim-sulfamethoxazole | Yes | Yes | 2005–2017 |
| Fucidanes | Fusidic acid | No | Yes | 2005–2017 |
| Glycopeptides | Vancomycin | Yes | Yes | 2003–2017 |
| Teicoplanin | Yes | Yes | 2007–2008 | |
| Telavancin | Yes | Yes | No | |
| Glycylcyclines | Tigecycline | No | Yes | No |
| Lincosamides | Clindamycin | Yes | Yes | 2005–2017 |
| Lipopeptides | Daptomycin | Yes | Yes | No |
| Macrolides | Erythromycin | Yes | Yes | 2005–2017 |
| Oxazolidinones | Linezolid | Yes | Yes | 2009–2017 |
| Phenicols | Chloramphenicol | Yes | Yes | 2005–2014 |
| Phosphonic acids | Fosfomycin | No | Yes | No |
| Streptogramins | Quinupristin-dalfopristin | Yes | Yes | 2011 |
| Tetracyclines | Tetracycline | Yes | Yes | 2009–2014 |
| Doxycycline | Yes | Yes | No | |
| Minocycline | Yes | Yes | No |
| Study (Period) | No. of S. aureus (n) or Percentage (%) of MRSA | Study Site(s) or No. of Study Site(s) (n) | Reference |
|---|---|---|---|
| Cheong et al., 1994 (1990–1991) | 2586 35.5% (905) MRSA 539 MRSA included in study | HKL | [13] |
| Norazah et al., 2001 (1997–1999) | 400 MRSA | Various, collected from ten hospitals throughout Malaysia | [14] |
| Al-Talib et al., 2010 (2002–2007) | 8200 1979 MRSA | HUSM | [15] |
| Thong et al., 2009 (2003–2004 and 2007) | 66 MRSA | N/A | [16] |
| Neela et al., 2008 (2006–2007) | 32 MRSA | N/A | [17] |
| Lim et al., 2013 (2003 and 2008) | 162 MRSA | UMMC | [18] |
| Al-Talib et al., 2015 (2008) | 34 MRSA, 124 MSSA | HUSM | [19] |
| Noordin et al., 2016 (2009) | 318 MRSA | UKMMC | [20] |
| Ho et al., 2017 (2011–2012) | 175 MRSA | HRPB, KPJ and GP | [21] |
| Sit et al., 2018 (2013) | 67 MRSA | UMMC | [22] |
| Che Hamzah et al., 2019 (2016–2017) | 90 MRSA, 109 MSSA | HSNZ | [23] |
| NSAR (2003–2005) | N/A | N/A | [24] |
| NSAR (2006) ** | 12,370 [25] 31.5% MRSA [26] | 10 GH [25] | [25,26] |
| NSAR (2007) | 13,548 [25] 28% MRSA | 12 GH [25,26] | [25,26] |
| NSAR (2008) | 23,176 26% MRSA | 13 GH | [25] |
| NSAR (2009) | 20,053 21% MRSA | 16 GH | [27] |
| NSAR (2010) | 20,007 22.2% MRSA | 16 GH | [28] |
| NSAR (2011) | 31,140 19.2% MRSA | 36 hospitals* (35 GH and 1 UH) | [29] |
| NSAR (2012) | 32,611 17.3% MRSA | 37 hospitals* (35 GH and 2 UH) | [30] |
| NSAR (2013) | 34,492 17.7% MRSA | 38 hospitals* (36 GH and 2 UH) | [31] |
| NSAR (2014) | 37,341 17.2% MRSA | 39 hospitals* (37 GH and 2 UH) | [32] |
| NSAR (2015) | 37,416 19.3% MRSA | 39 hospitals* (37 GH and 2 UH) | [33] |
| NSAR (2016) | 37,207 18% MRSA | 39 hospitals* (37 GH and 2 UH) | [4] |
| NSAR (2017) | 39,447 19% MRSA | 39 hospitals* (37 GH and 2 UH) | [5] |
| A. Community- and Hospital-Associated Staphylococcus aureus Isolates in Malaysia | |||||
| Year | MRSA/MSSA | SCCmec (%) | Sequence Type (ST) | Origin | Reference |
| 2003, 2004 | MRSA | III (78.8) IV (18.2) Untypable (3.0) | N/A | N/A | [16] |
| 2003, 2006, 2007 | MRSA | IV IVE | ST6, ST30 ST22, ST1178, ST1179 | HA, CA | [74] |
| 2003, 2008 | MRSA | III (90.0) IV (9.0) V (1.0) | (ST239, ST772, ST6, ST22, ST1178) * | HA, CA | [18] |
| 2003, 2004, 2007, 2008 | MRSA | NA | ST5, ST6, ST20, ST22, ST80, ST239 | NA | [75] |
| 2006–2007 | MRSA | III (41.7) IIIA (52.8) V (5.5) | ST239 ST239 ST1, ST772 | HA, CA | [68] |
| 2006–2008 | MRSA | III (96.8) IV (3.2) | NA ST30, ST22, ST45, ST80, ST101, ST188, ST1284, ST1285, ST1286, ST1287, ST1288 | HA, CA | [69] |
| 2007–2008 | MRSA | III (20.0) IIIA (72.8) V (5.7) IVh (1.5) | (ST239, ST1, ST7, ST22, ST188, ST1283) * | NA | [67] |
| 2008 | MSSA | - | ST1, ST3, ST5, ST8, ST9, ST12, ST15, ST18, ST20, ST25, ST45, ST80, ST88, ST97, ST121, ST152, ST188, ST231, ST239, ST427, ST508, ST769, ST833, ST1050, ST1153 | HA, CA | [76] |
| 2008–2010 | MRSA | III (91.4) IV (2.9) V (5.7) | (ST239, ST772) * | N/A | [77] |
| MSSA | - | ST1, ST7, ST30, ST239, ST508, ST779, ST1179, ST1659 | |||
| 2009 | MRSA | II (0.4) III (94.5) IV (3.4) V (1.7) | ST239 ST239 ST30, ST1178 ST772 | N/A | [78] |
| 2009 | MRSA | III (72.0) IV (2.5) V (1.3) II (0.3) Untypable (9.7) Novel (14.2) | N/A | NA | [20] |
| 2010 | MRSA | III (78.5) IV (21.5) | N/A | NA | [79] |
| 2011–2012 | MRSA | III (81.1) IV (12.6) II (0.6) V (5.7%) | N/A | NA | [21] |
| 2011–2012 | MRSA | II (0.9) III (66.5) IV (28.2) V (3.3) Untypable (0.9) | NA ST239 ST1, ST6, ST22, ST1137 ST5, ST772 ST239, ST508 | HA, CA | [80] |
| 2013 | MRSA | III (55.2) I (1.5) IV (29.9) V (11.9) Untypable (1.5) | ST239 ST152 ST6, ST22, ST30, ST1179 ST1, ST45, ST772, ST951 ST5 | HA, CA | [22] |
| 2015–2017 | MRSA | IVa (35.0) IVc (2.7) V (2.7) II (2.7) Untypable (57.0) | N/A | CA | [81] |
| B. Livestock-Associated Staphylococcus aureus Isolates in Malaysia | |||||
| Year | Livestock | Prevalence (%) | SCCmec (%)/Sequence Type (ST) | Origin | Reference |
| N/A | Raw chicken meat | S. aureus (24.0) | N/A | LA | [82] |
| N/A | Cat and dog | MRSA (11.7) | N/A | LA | [83] |
| N/A | Cat and dog | MRSA (1.9) | N/A | LA | [84] |
| N/A | Chicken | MRSA (18.0) | N/A | LA | [85] |
| N/A | Piglet | MRSA (2.4) | N/A | LA | [86] |
| 2007–2008 | Cat and dog | MRSA (8.0) | N/A | LA | [87] |
| N/A | Horse | S. aureus (44.0) | N/A | LA | [88] |
| 2010 | Chicken | S. aureus (1.0) | ST692 | LA | [89] |
| 2014 | Cat and dog | MRSA in cat (7.7) MRSA in dog (11.7) | N/A | LA | [90] |
| N/A | Pig | MRSA (1.4) | V (100.0)/ST9 | LA | [91] |
| N/A | Pig | S. aureus (24.6) MRSA (0.8) | N/A | LA | [92] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Che Hamzah, A.M.; Yeo, C.C.; Puah, S.M.; Chua, K.H.; Chew, C.H. Staphylococcus aureus Infections in Malaysia: A Review of Antimicrobial Resistance and Characteristics of the Clinical Isolates, 1990–2017. Antibiotics 2019, 8, 128. https://doi.org/10.3390/antibiotics8030128
Che Hamzah AM, Yeo CC, Puah SM, Chua KH, Chew CH. Staphylococcus aureus Infections in Malaysia: A Review of Antimicrobial Resistance and Characteristics of the Clinical Isolates, 1990–2017. Antibiotics. 2019; 8(3):128. https://doi.org/10.3390/antibiotics8030128
Chicago/Turabian StyleChe Hamzah, Ainal Mardziah, Chew Chieng Yeo, Suat Moi Puah, Kek Heng Chua, and Ching Hoong Chew. 2019. "Staphylococcus aureus Infections in Malaysia: A Review of Antimicrobial Resistance and Characteristics of the Clinical Isolates, 1990–2017" Antibiotics 8, no. 3: 128. https://doi.org/10.3390/antibiotics8030128
APA StyleChe Hamzah, A. M., Yeo, C. C., Puah, S. M., Chua, K. H., & Chew, C. H. (2019). Staphylococcus aureus Infections in Malaysia: A Review of Antimicrobial Resistance and Characteristics of the Clinical Isolates, 1990–2017. Antibiotics, 8(3), 128. https://doi.org/10.3390/antibiotics8030128








