Diagnostic Value of C-Reactive Protein and Serum White Blood Cell Count during Septic Two-Stage Revision of Total Knee Arthroplasties
Abstract
1. Introduction
- Do CRP and WBC count show a significant response to the first stage surgery of TSR and subsequent antibiotic treatment?
- Do CRP and WBC counts behave differently in cases of later reinfection?
- What is the diagnostic value of CRP and WBC counts, as well as their course over 14 days in the interim phase for predicting later re-infection?
- Is there a threshold value of CRP and WBC counts, as well as for their course over 14 days, with a diagnostic value that would help decision-making for reimplantation?
2. Material and Methods
2.1. Patients
2.2. Treatment Protocol
2.2.1. First Stage of TSR
2.2.2. Interval
2.2.3. Second Stage of TSR
2.3. Laboratory Parameters
2.4. Outcome Measurements
2.5. Statistical Analysis
3. Results
3.1. Collective
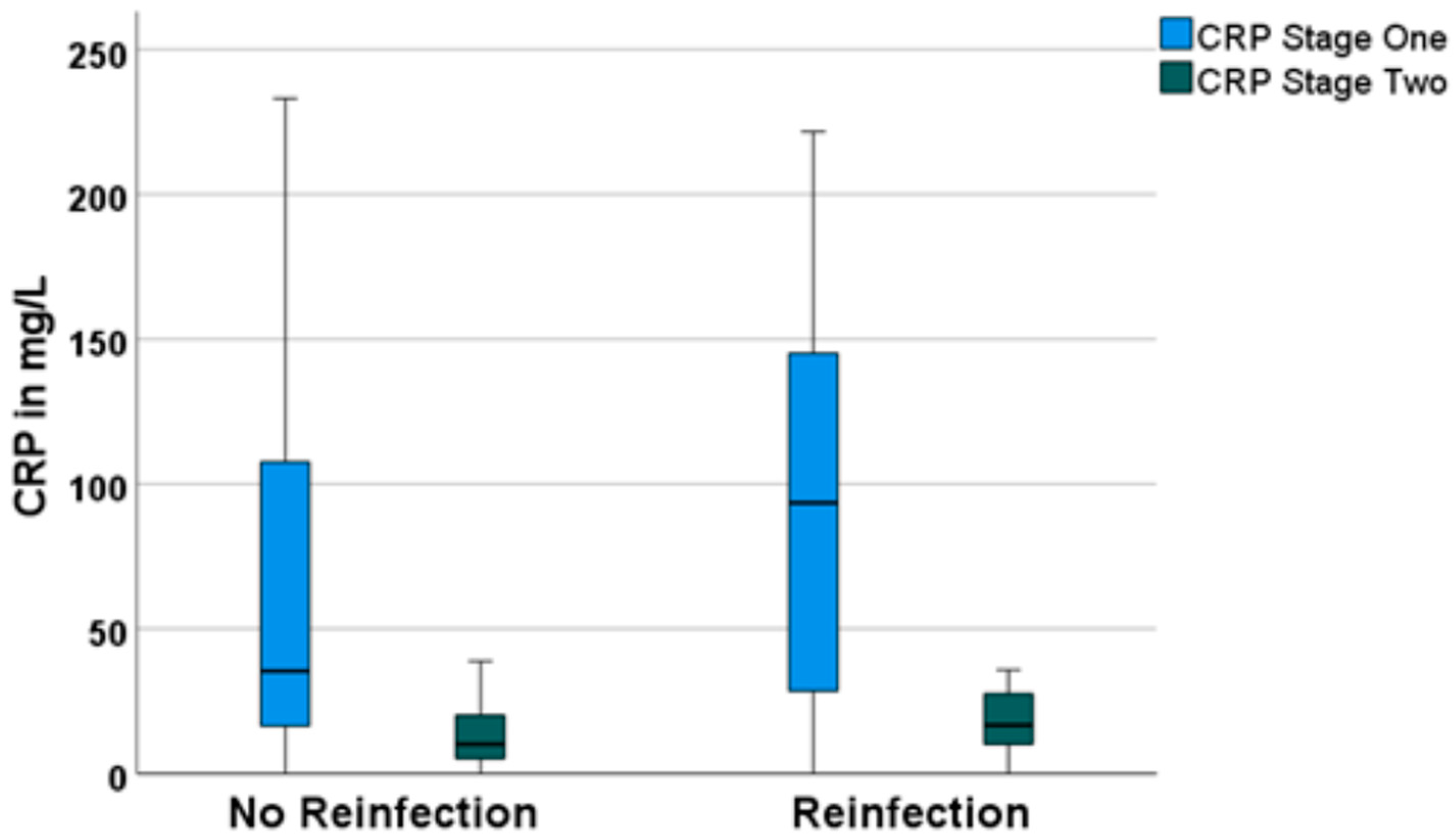
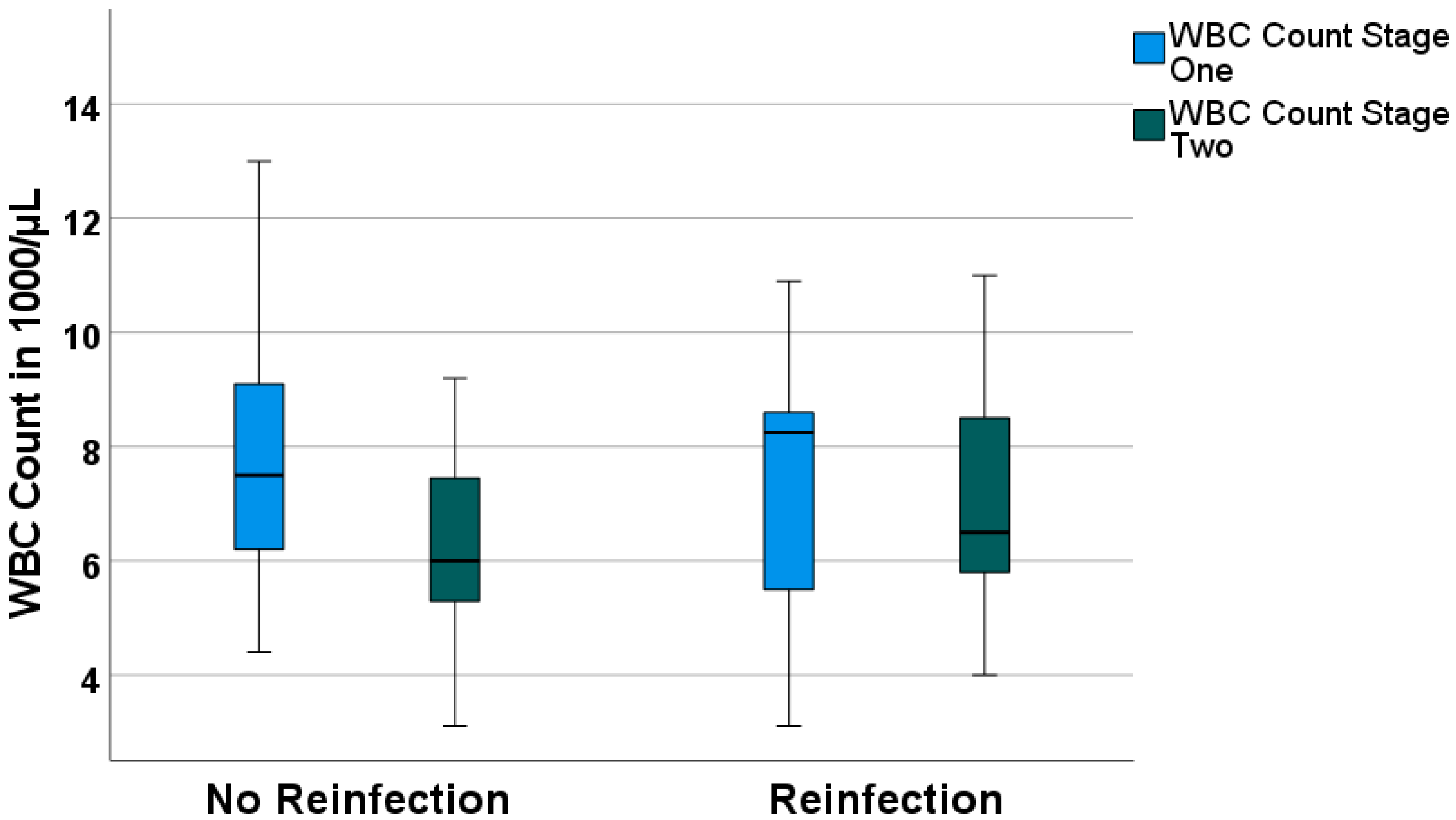
3.2. Treatment Response
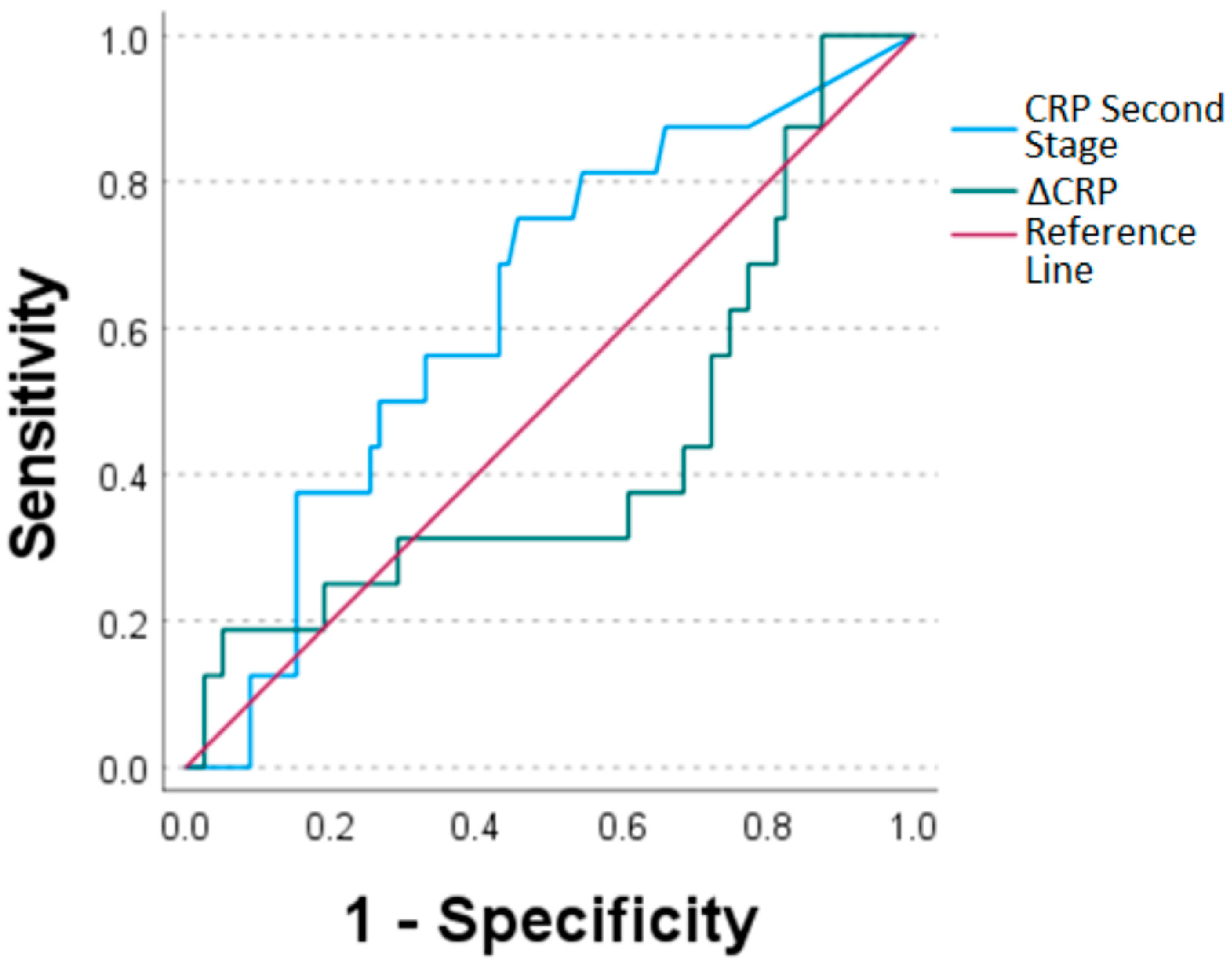
3.3. Diagnostic Value and Determination of Optimal Threshold
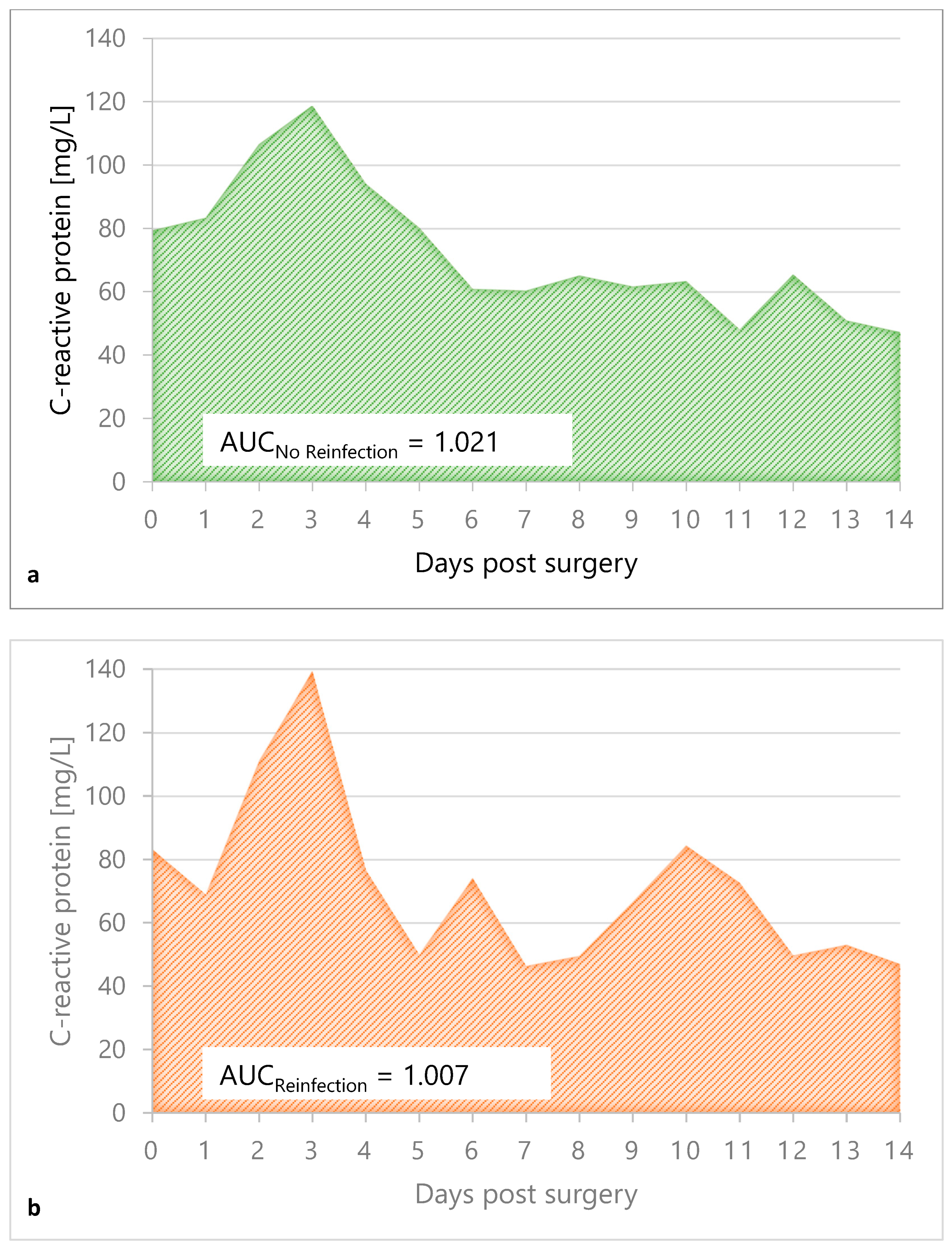
3.4. CRP Value Course in the Interim Phase
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Poultsides, L.A.; Triantafyllopoulos, G.K.; Sakellariou, V.I.; Memtsoudis, S.G.; Sculco, T.P. Infection risk assessment in patients undergoing primary total knee arthroplasty. Int. Orthop. 2018, 42, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Madarevic, T.; Buterin, A.; Jelicic, J.; Sirola, L.; Vuckovic, D. Functional recovery after two-stage short-interval revision of chronic periprosthetic knee joint infection. Int. Orthop. 2021, 45, 985–989. [Google Scholar] [CrossRef] [PubMed]
- Clauss, M.; Cadosch, D.; Morgenstern, M. Periprosthetic Joint Infections—An Overview. Ther. Umsch. 2020, 77, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Rajput, V.; Meek, R.M.D.; Haddad, F.S. Periprosthetic joint infection: What next? Bone Jt. J. 2022, 104–b, 1193–1195. [Google Scholar] [CrossRef] [PubMed]
- Serota, D.P.; Chueng, T.A.; Tookes, H.E. Treatment of Knee Periprosthetic Joint Infection Among Patients With Substance Use Disorder. Orthopedics 2021, 44, 262. [Google Scholar] [CrossRef]
- Talsma, D.T.; Ploegmakers, J.J.W.; Jutte, P.C.; Kampinga, G.; Wouthuyzen-Bakker, M. Time to positivity of acute and chronic periprosthetic joint infection cultures. Diagn. Microbiol. Infect. Dis. 2021, 99, 115178. [Google Scholar] [CrossRef]
- Dombrowski, M.E.; Klatt, B.A.; Deirmengian, C.A.; Brause, B.D.; Chen, A.F. Musculoskeletal Infection Society (MSIS) Update on Infection in Arthroplasty. Instr. Course. Lect. 2020, 69, 85–102. [Google Scholar]
- Fink, B.; Rechtenbach, A.; Büchner, H.; Vogt, S.; Hahn, M. Articulating Spacers Used in Two-stage Revision of Infected Hip and Knee Prostheses Abrade with Time. Clin. Orthop. Relat. Res. 2011, 469, 1095–1102. [Google Scholar] [CrossRef]
- Li, C.; Renz, N.; Trampuz, A. Management of Periprosthetic Joint Infection. Hip Pelvis 2018, 30, 138–146. [Google Scholar] [CrossRef]
- Matar, H.E.; Bloch, B.V.; Snape, S.E.; James, P.J. Outcomes of single- and two-stage revision total knee arthroplasty for chronic periprosthetic joint infection: Long-term outcomes of changing clinical practice in a specialist centre. Bone Jt. J. 2021, 103–b, 1373–1379. [Google Scholar] [CrossRef]
- Maale, G.E.; Eager, J.J.; Srinivasaraghavan, A.; Mohammadi, D.K.; Kennard, N. The evolution from the two stage to the one stage procedure for biofilm based periprosthetic joint infections (PJI). Biofilm 2020, 2, 100033. [Google Scholar] [CrossRef] [PubMed]
- Wolf, C.F.; Gu, N.Y.; Doctor, J.N.; Manner, P.A.; Leopold, S.S. Comparison of one and two-stage revision of total hip arthroplasty complicated by infection: A Markov expected-utility decision analysis. J. Bone Jt. Surg. Am. 2011, 93, 631–639. [Google Scholar] [CrossRef] [PubMed]
- Burnett, R.S.J.; Kelly, M.A.; Hanssen, A.D.; Barrack, R.L. Technique and Timing of Two-stage Exchange for Infection in TKA. Clin. Orthop. Relat. Res. 2007, 464, 164–178. [Google Scholar] [CrossRef] [PubMed]
- Fink, B. Revision of late periprosthetic infections of total hip endoprostheses: Pros and cons of different concepts. Int. J. Med Sci. 2009, 6, 287–295. [Google Scholar] [CrossRef]
- Fu, J.; Ni, M.; Li, H.; Li, X.; Chai, W.; Zhou, Y.; Hao, L.; Chen, J. The proper timing of second-stage revision in treating periprosthetic knee infection: Reliable indicators and risk factors. J. Orthop. Surg. Res. 2018, 13, 214. [Google Scholar] [CrossRef]
- Jiang, Q.; Fu, J.; Chai, W.; Hao, L.-B.; Zhou, Y.-G.; Xu, C.; Chen, J.-Y. Changes in serum markers failed to predict persistent infection after two-stage exchange arthroplasty. J. Orthop. Surg. Res. 2020, 15, 382. [Google Scholar] [CrossRef]
- Kusuma, S.K.; Ward, J.; Jacofsky, M.; Sporer, S.M.; Della Valle, C.J. What is the role of serological testing between stages of two-stage reconstruction of the infected prosthetic knee? Clin. Orthop. Relat. Res. 2011, 469, 1002–1008. [Google Scholar] [CrossRef]
- Stambough, J.B.; Curtin, B.M.; Odum, S.M.; Cross, M.B.; Martin, J.R.; Fehring, T.K. Does Change in ESR and CRP Guide the Timing of Two-stage Arthroplasty Reimplantation? Clin. Orthop. Relat. Res. 2019, 477, 364–371. [Google Scholar] [CrossRef]
- Alijanipour, P.; Bakhshi, H.; Parvizi, J. Diagnosis of periprosthetic joint infection: The threshold for serological markers. Clin. Orthop. Relat. Res. 2013, 471, 3186–3195. [Google Scholar] [CrossRef]
- Parvizi, J.; Tan, T.L.; Goswami, K.; Higuera, C.; Della Valle, C.; Chen, A.F.; Shohat, N. The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria. J. Arthroplast. 2018, 33, 1309–1314.e2. [Google Scholar] [CrossRef]
- Parvizi, J.; Zmistowski, B.; Berbari, E.F.; Bauer, T.W.; Springer, B.D.; Della Valle, C.J.; Garvin, K.L.; Mont, M.A.; Wongworawat, M.D.; Zalavras, C.G. New definition for periprosthetic joint infection: From the Workgroup of the Musculoskeletal Infection Society. Clin. Orthop. Relat. Res. 2011, 469, 2992–2994. [Google Scholar] [CrossRef]
- Diaz-Ledezma, C.; Higuera, C.A.; Parvizi, J. Success after treatment of periprosthetic joint infection: A Delphi-based international multidisciplinary consensus. Clin. Orthop. Relat. Res. 2013, 471, 2374–2382. [Google Scholar] [CrossRef]
- Fischer, J.E.; Bachmann, L.M.; Jaeschke, R. A readers’ guide to the interpretation of diagnostic test properties: Clinical example of sepsis. Intensive Care Med. 2003, 29, 1043–1051. [Google Scholar] [CrossRef] [PubMed]
- Ghanem, E.; Azzam, K.; Seeley, M.; Joshi, A.; Parvizi, J. Staged revision for knee arthroplasty infection: What is the role of serologic tests before reimplantation? Clin. Orthop. Relat. Res. 2009, 467, 1699–1705. [Google Scholar] [CrossRef] [PubMed]
- Bian, T.; Shao, H.; Zhou, Y.; Huang, Y.; Song, Y. Tests for predicting reimplantation success of two-stage revision for periprosthetic joint infection: A systematic review and meta-analysis. Orthop. Traumatol. Surg. Res. 2018, 104, 1115–1123. [Google Scholar] [CrossRef] [PubMed]
- Hoell, S.; Borgers, L.; Gosheger, G.; Dieckmann, R.; Schulz, D.; Gerss, J.; Hardes, J. Interleukin-6 in two-stage revision arthroplasty: What is the threshold value to exclude persistent infection before re-implanatation? Bone Jt. J. 2015, 97–b, 71–75. [Google Scholar] [CrossRef]
- Khury, F.; Oltmanns, M.; Fuchs, M.; Leiprecht, J.; Reichel, H.; Faschingbauer, M. Against the Norm: Do Not Rely on Serum C-Reactive Protein and White Blood Cell Count Only When Assessing Eradication of Periprosthetic Joint Infection. Antibiotics 2022, 11, 1174. [Google Scholar] [CrossRef]
- Shukla, S.K.; Ward, J.P.; Jacofsky, M.C.; Sporer, S.M.; Paprosky, W.G.; Della Valle, C.J. Perioperative testing for persistent sepsis following resection arthroplasty of the hip for periprosthetic infection. J. Arthroplast. 2010, 25, 87–91. [Google Scholar] [CrossRef]
- Li, Z.Y.; Lin, Y.C.; Chang, C.H.; Chen, S.Y.; Lu, T.W.; Lee, S.H. Trend of serum C-reactive protein is associated with treatment outcome of hip Periprosthetic joint infection undergoing two-stage exchange arthroplasty: A case control study. BMC Musculoskelet. Disord. 2021, 22, 1007. [Google Scholar] [CrossRef]
- Mederake, M.; Hofmann, U.K.; Benda, S.; Schuster, P.; Fink, B. Diagnostic Value of CRP and Serum WBC Count during Septic Two-Stage Revision of Total Hip Arthroplasties. Antibiotics 2022, 11, 1098. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, P.; Pandey, A.; Sompura, S.; Pursnani, M.L. Role of blood C-reactive protein levels in upper urinary tract infection and lower urinary tract infection in adult patients (>16 years). J. Assoc. Physicians India 2013, 61, 462–463. [Google Scholar] [PubMed]
- Aronson, D.; Bartha, P.; Zinder, O.; Kerner, A.; Markiewicz, W.; Avizohar, O.; Brook, G.J.; Levy, Y. Obesity is the major determinant of elevated C-reactive protein in subjects with the metabolic syndrome. Int. J. Obes. Relat. Metab. Disord. 2004, 28, 674–679. [Google Scholar] [CrossRef] [PubMed]
- Kasapis, C.; Thompson, P.D. The effects of physical activity on serum C-reactive protein and inflammatory markers: A systematic review. J. Am. Coll. Cardiol. 2005, 45, 1563–1569. [Google Scholar] [CrossRef]
- Meisner, M.; Adina, H.; Schmidt, J. Correlation of procalcitonin and C-reactive protein to inflammation, complications, and outcome during the intensive care unit course of multiple-trauma patients. Crit. Care 2006, 10, R1. [Google Scholar] [CrossRef] [PubMed]
- Melbye, H.; Hvidsten, D.; Holm, A.; Nordbø, S.A.; Brox, J. The course of C-reactive protein response in untreated upper respiratory tract infection. Br. J. Gen. Pract. 2004, 54, 653–658. [Google Scholar]
- Della Valle, C.J.; Sporer, S.M.; Jacobs, J.J.; Berger, R.A.; Rosenberg, A.G.; Paprosky, W.G. Preoperative testing for sepsis before revision total knee arthroplasty. J. Arthroplast. 2007, 22, 90–93. [Google Scholar] [CrossRef]
- Trampuz, A.; Hanssen, A.D.; Osmon, D.R.; Mandrekar, J.; Steckelberg, J.M.; Patel, R. Synovial fluid leukocyte count and differential for the diagnosis of prosthetic knee infection. Am. J. Med. 2004, 117, 556–562. [Google Scholar] [CrossRef]

| Causative Bacterium | Quantity |
|---|---|
| Staphylococcusepidermidis | 19 |
| Staphylococcusaureus | 17 |
| Enterococcus faecalis | 5 |
| Staphylococcuscapitis | 4 |
| Streptococcus mitis | 3 |
| Staphylococcuscaprae | 2 |
| Streptococcus anginosus | 2 |
| Cutibacterium acnes | 2 |
| Streptococcus oralis | 2 |
| Pseudomonas aeruginosa | 2 |
| Staphylococcus hominis ssp hominis | 2 |
| Streptococcus dysgalacticae | 1 |
| Streptococcus parasanguis | 1 |
| Corynebacteriumjeikeium | 1 |
| Escherichiacoli | 1 |
| Staphylococcusagalacticae | 1 |
| Finegoldia magna | 1 |
| Streptococcus gordonii | 1 |
| Staphylococcuslugdunensis | 1 |
| Actinomyces odontolyticus | 1 |
| Staphylococcuswarneri | 1 |
| Corynebacterium species | 1 |
| Streptococcus agalacticae | 1 |
| culture negative | 32 |
| total | 104 |
| Area under the ROC Curve | |||||
|---|---|---|---|---|---|
| Test Result Variable (s) | Area | Std. Error | Asymptotic Sig. | Asymptotic 95% Confidence Interval | |
| Lower Limit | Upper Limit | ||||
| CRP count, second stage of TSR | 0.631 | 0.073 | 0.072 | 0.488 | 0.774 |
| ΔCRP | 0.435 | 0.085 | 0.446 | 0.268 | 0.602 |
| WBC count, second stage of TSR | 0.585 | 0.077 | 0.270 | 0.434 | 0.737 |
| ΔWBC count | 0.527 | 0.086 | 0.750 | 0.360 | 0.695 |
| Calculated Threshold Value | Sensitivity | Specificity | |
|---|---|---|---|
| CRP second stage of TSR (in mg/L) | 11.35 | 0.75 | 0.544 |
| ΔCRP (in mg/L) | 11.00 | 0.188 | 0.949 |
| WBC Count second stage of TSR (in/µL) | 6.25 × 103 | 0.688 | 0.557 |
| ΔWBC Count (in/µL) | 0.45 × 103 | 0.313 | 0.873 |
| No Reinfection | Reinfection | p-Value | |
|---|---|---|---|
| Pre-operatively | 79 ± 97 | 83 ± 75 | 0.750 |
| Day 1 | 83 ± 92 | 69 ± 58 | 0.879 |
| Day 2 | 107 ± 80 | 111 ± 85 | 0.828 |
| Day 3 | 119 ± 82 | 139 ± 49 | 0.160 |
| Day 4 | 94 ± 52 | 77 ± 61 | 0.837 |
| Day 5 | 80 ± 47 | 50 ± 42 | 0.207 |
| Day 6 | 61 ± 30 | 74 ± 57 | 0.666 |
| Day 7 | 60 ± 43 | 46 ± 7 | 0.690 |
| Day 8 | 65 ± 37 | 50 ± 42 | 0.509 |
| Day 9 | 62 ± 42 | 67 ± 80 | 0.622 |
| Day 10 | 63 ± 45 | 84 ± 57 | 0.399 |
| Day 11 | 48 ± 32 | 73 ± 49 | 0.240 |
| Day 12 | 65 ± 42 | 50 ± 34 | 0.556 |
| Day 13 | 51 ± 37 | 53 ± 50 | 0.768 |
| Day 14 | 47 ± 38 | 47 ± 30 | 0.754 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benda, S.; Mederake, M.; Schuster, P.; Fink, B. Diagnostic Value of C-Reactive Protein and Serum White Blood Cell Count during Septic Two-Stage Revision of Total Knee Arthroplasties. Antibiotics 2023, 12, 14. https://doi.org/10.3390/antibiotics12010014
Benda S, Mederake M, Schuster P, Fink B. Diagnostic Value of C-Reactive Protein and Serum White Blood Cell Count during Septic Two-Stage Revision of Total Knee Arthroplasties. Antibiotics. 2023; 12(1):14. https://doi.org/10.3390/antibiotics12010014
Chicago/Turabian StyleBenda, Sebastian, Moritz Mederake, Philipp Schuster, and Bernd Fink. 2023. "Diagnostic Value of C-Reactive Protein and Serum White Blood Cell Count during Septic Two-Stage Revision of Total Knee Arthroplasties" Antibiotics 12, no. 1: 14. https://doi.org/10.3390/antibiotics12010014
APA StyleBenda, S., Mederake, M., Schuster, P., & Fink, B. (2023). Diagnostic Value of C-Reactive Protein and Serum White Blood Cell Count during Septic Two-Stage Revision of Total Knee Arthroplasties. Antibiotics, 12(1), 14. https://doi.org/10.3390/antibiotics12010014





