Modified Clavien–Dindo Classification and Outcome Prediction in Free Flap Reconstruction among Patients with Head and Neck Cancer
Abstract
1. Introduction
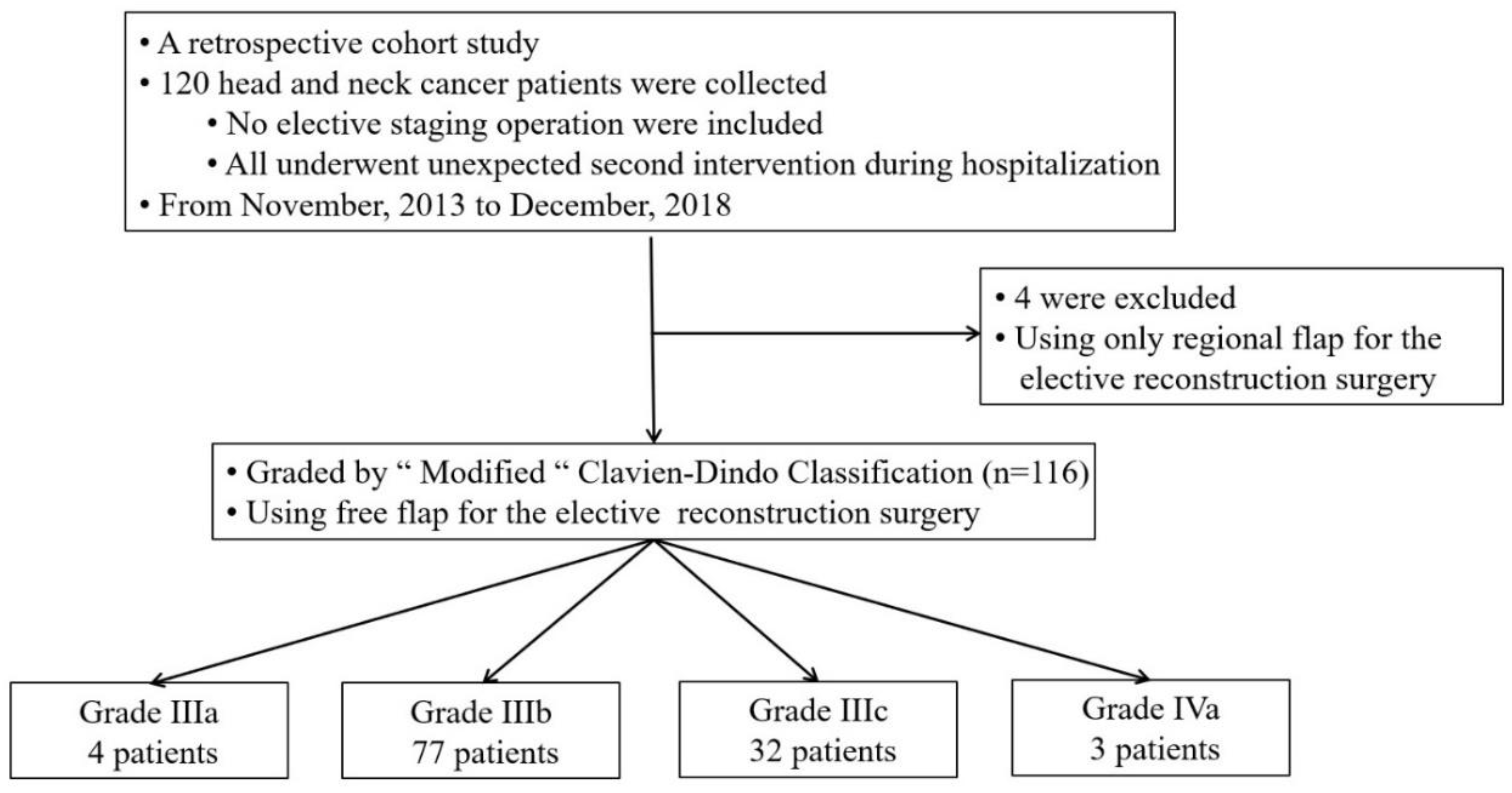
2. Material and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Dindo, D.; Demartines, N.; Clavien, P.-A. Classification of Surgical Complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Clavien, P.-A.; Barkun, J.; De Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; De Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo Classification of Surgical Complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Perisanidis, C.; Herberger, B.; Papadogeorgakis, N.; Seemann, R.; Eder-Czembirek, C.; Tamandl, D.; Heinze, G.; Kyzas, P.A.; Kanatas, A.; Mitchell, D.; et al. Complications after free flap surgery: Do we need a standardized classification of surgical complications? Br. J. Oral Maxillofac. Surg. 2012, 50, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, E.; Sklar, M.C.; Eskander, A.; De Almeida, J.R.; Shrime, M.; Gullane, P.; Irish, J.; Gilbert, R.W.; Brown, D.H.; Higgins, K.M.; et al. Assessment of the Clavien-Dindo classification system for complications in head and neck surgery. Laryngoscope 2014, 124, 2726–2731. [Google Scholar] [CrossRef]
- Chassin, M.R.; Loeb, J.M.; Schmaltz, S.P.; Wachter, R.M. Accountability Measures—Using Measurement to Promote Quality Improvement. N. Engl. J. Med. 2010, 363, 683–688. [Google Scholar] [CrossRef]
- Mitropoulos, D.; Artibani, W.; Biyani, C.S.; Jensen, J.B.; Rouprêt, M.; Truss, M. Validation of the Clavien–Dindo Grading System in Urology by the European Association of Urology Guidelines Ad Hoc Panel. Eur. Urol. Focus 2018, 4, 608–613. [Google Scholar] [CrossRef]
- Sink, E.L.; Academic Network for Conservational Hip Outcomes Research Group; Leunig, M.; Zaltz, I.; Gilbert, J.C.; Clohisy, J. Reliability of a Complication Classification System for Orthopaedic Surgery. Clin. Orthop. Relat. Res. 2012, 470, 2220–2226. [Google Scholar] [CrossRef]
- Ivanovic, J.; Al-Hussaini, A.; Al-Shehab, D.; Threader, J.; Villeneuve, P.J.; Ramsay, T.; Maziak, D.E.; Gilbert, S.; Shamji, F.M.; Sundaresan, R.S.; et al. Evaluating the Reliability and Reproducibility of the Ottawa Thoracic Morbidity and Mortality Classification System. Ann. Thorac. Surg. 2011, 91, 387–393. [Google Scholar] [CrossRef]
- Dwyer, M.E.; Dwyer, J.T.; Cannon, G.M.; Stephany, H.A.; Schneck, F.X.; Ost, M.C. The Clavien-Dindo Classification of Surgical Complications is Not a Statistically Reliable System for Grading Morbidity in Pediatric Urology. J. Urol. 2016, 195, 460–464. [Google Scholar] [CrossRef]
- Zafereo, M.E.; Weber, R.S.; Lewin, J.S.; Roberts, D.B.; Hanasono, M.M. Complications and functional outcomes following complex oropharyngeal reconstruction. Head Neck 2009, 32, 1003–1011. [Google Scholar] [CrossRef]
- Lahtinen, S.L.; Koivunen, P.; Ala-Kokko, T.; Kaarela, O.; Ohtonen, P.; Laurila, P.; Liisanantti, J.H. Complications and outcome after free flap surgery for cancer of the head and neck. Br. J. Oral Maxillofac. Surg. 2018, 56, 684–691. [Google Scholar] [CrossRef] [PubMed]
- Jones, N.F.; Markowitz, B.L.; Jarrahy, R.; Usa, U.L.A.C. Postoperative Medical Complications, Not Microsurgical Complications, Negatively Influence the Morbidity, Mortality, and True Costs after Microsurgical Reconstruction for Head and Neck Cancer. J. Reconstr. Microsurg. 2007, 22, 2053–2060. [Google Scholar] [CrossRef] [PubMed]
- Girod, A.; Brancati, A.; Mosseri, V.; Kriegel, I.; Jouffroy, T.; Rodriguez, J. Study of the length of hospital stay for free flap reconstruction of oral and pharyngeal cancer in the context of the new French casemix-based funding. Oral Oncol. 2010, 46, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.-M.; Sundararajan, V. Updating and Validating the Charlson Comorbidity Index and Score for Risk Adjustment in Hospital Discharge Abstracts Using Data From 6 Countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef]
- Small, L.T.; Lampkin, M.; Vural, E.; Moreno, M.A. American Society of Anesthesiologists Class as Predictor for Perioperative Morbidity in Head and Neck Free Flaps. Otolaryngol. Neck Surg. 2019, 161, 91–97. [Google Scholar] [CrossRef]
- Las, D.E.; De Jong, T.; Zuidam, J.M.; Verweij, N.M.; Hovius, S.; Mureau, M.A.M. Identification of independent risk factors for flap failure: A retrospective analysis of 1530 free flaps for breast, head and neck and extremity reconstruction. J. Plast. Reconstr. Aesthetic Surg. 2016, 69, 894–906. [Google Scholar] [CrossRef]
- Broome, M.; Juilland, N.; Litzistorf, Y.; Monnier, Y.; Sandu, K.; Pasche, P.; Plinkert, P.K.; Federspil, P.A.; Netto, E. Factors Influencing the Incidence of Severe Complications in Head and Neck Free Flap Reconstructions. Plast. Reconstr. Surg. Glob. Open 2016, 4, e1013. [Google Scholar] [CrossRef]
- Choi, N.; Park, S.I.; Kim, H.; Sohn, I.; Jeong, H.-S. The impact of unplanned reoperations in head and neck cancer surgery on survival. Oral Oncol. 2018, 83, 38–45. [Google Scholar] [CrossRef]
- Clark, J.R.; McCluskey, S.A.; Hall, F.; Lipa, J.; Neligan, P.; Brown, D.; Irish, J.; Gullane, P.; Gilbert, R. Predictors of morbidity following free flap reconstruction for cancer of the head and neck. Head Neck 2007, 29, 1090–1101. [Google Scholar] [CrossRef]
- Ebner, J.J.; Mehra, T.; Gander, T.; Schumann, P.; Essig, H.; Zweifel, D.; Rücker, M.; Slankamenac, K.; Lanzer, M. Novel application of the Clavien-Dindo classification system and the comprehensive complications index® in microvascular free tissue transfer to the head and neck. Oral Oncol. 2019, 94, 21–25. [Google Scholar] [CrossRef] [PubMed]
- McMahon, J.; Maciver, C.; Smith, M.; Stathopoulos, P.; Wales, C.; McNulty, R.; Handley, T.P.; Devine, J.C. Postoperative complications after major head and neck surgery with free flap repair—prevalence, patterns, and determinants: A prospective cohort study. Br. J. Oral Maxillofac. Surg. 2013, 51, 689–695. [Google Scholar] [CrossRef] [PubMed]
- Herle, P.; Shukla, L.; Morrison, W.A.; Shayan, R. Preoperative radiation and free flap outcomes for head and neck reconstruction: A systematic review and meta-analysis. ANZ J. Surg. 2015, 85, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, S.; Nakao, J.; Higashino, T.; Yoshimoto, S.; Hayashi, R.; Sakuraba, M. Clavien–Dindo classification for grading complications after total pharyngolaryngectomy and free jejunum transfer. PLoS ONE 2019, 14, e0222570. [Google Scholar] [CrossRef] [PubMed]
- Tan, N.C.; Lin, P.-Y.; Chiang, Y.-C.; Chew, K.-Y.; Chen, C.-C.; Fujiwara, T.; Kuo, Y.-R. Influence of neck dissection and preoperative irradiation on microvascular head and neck reconstruction-Analysis of 853 cases. Microsurgery 2014, 34, 602–607. [Google Scholar] [CrossRef]
- Tsai, M.-H.; Chuang, H.-C.; Lin, Y.-T.; Lü, H.; Chen, W.-C.; Fang, F.-M.; Chien, C.-Y. Clinical impact of albumin in advanced head and neck cancer patients with free flap reconstruction—A retrospective study. PeerJ 2018, 6, e4490. [Google Scholar] [CrossRef]
- Caburet, C.; Farigon, N.; Mulliez, A.; Mom, T.; Boirie, Y.; Gilain, L.; Saroul, N. Impact of nutritional status at the outset of assessment on postoperative complications in head and neck cancer. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2019, S1879-7296(19), 30208. [Google Scholar] [CrossRef]
- Takase, S.; Takada, A.; Tsutsumi, M.; Matsuda, Y. Biochemical markers of chronic alcoholism. Alcohol 1985, 2, 405–410. [Google Scholar] [CrossRef]
- Teppo, A.-M.; Maury, C. Serum prealbumin, transferrm and immunoglobulins in fatty liver, alcoholic cirrhosis and primary biliary cirrhosis. Clin. Chim. Acta 1983, 129, 279–286. [Google Scholar] [CrossRef]
- Shum, J.; Markiewicz, M.R.; Park, E.; Bui, T.; Lubek, J.; Bell, R.B.; Dierks, E.J. Low Prealbumin Level Is a Risk Factor for Microvascular Free Flap Failure. J. Oral Maxillofac. Surg. 2014, 72, 169–177. [Google Scholar] [CrossRef]
- Chiu, Y.-H.; Chang, D.-H.; Perng, C.-K. Vascular Complications and Free Flap Salvage in Head and Neck Reconstructive Surgery. Ann. Plast. Surg. 2017, 78, S83–S88. [Google Scholar] [CrossRef] [PubMed]
- Kucur, C.; Durmus, K.; Uysal, I.O.; Old, M.; Agrawal, A.; Arshad, H.; Teknos, T.N.; Ozer, E. Management of complications and compromised free flaps following major head and neck surgery: Analysis of 150 Cases of Reexploration. Eur. Arch. Oto-Rhino-Laryngol. 2016, 273, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Kao, H.-K.; Chang, K.-P.; Ching, W.-C.; Tsao, C.-K.; Cheng, M.-H.; Wei, F.-C. The impacts of liver cirrhosis on head and neck cancer patients undergoing microsurgical free tissue transfer: An evaluation of flap outcome and flap-related complications. Oral Oncol. 2009, 45, 1058–1062. [Google Scholar] [CrossRef] [PubMed]
- Handschel, P.D.D.J.; Burghardt, S.; Naujoks, C.; Kübler, N.R.; Giers, G. Parameters predicting complications in flap surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 115, 589–594. [Google Scholar] [CrossRef]
- Lahtinen, S.L.; Koivunen, P.; Ala-Kokko, T.; Laurila, P.; Kaarela, O.; Liisanantti, J.H. Quality of life after free flap surgery for cancer of the head and neck in patients with or without postoperative complications. Eur. Arch. Oto-Rhino-Laryngol. 2018, 275, 2575–2584. [Google Scholar] [CrossRef]
- Clavien, P.A.; Sanabria, J.R.; Strasberg, S.M. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery 1992, 111, 518–526. [Google Scholar]

| Complications | Grade IIIa | Grade IIIb | Grade IIIc | Grade IVa | Total |
|---|---|---|---|---|---|
| Hematoma evacuation | 0 | 29 (37.7%) * | 5 (15.6%) | 0 | 34 (29.3%) |
| Wound dehiscence | 3 (75%) * | 12 (15.6%) | 8 (25%) | 1 (33.3%) | 24 (20.7%) |
| Vascular complication | 1 (25%) | 57 (74%) * | 32 (100%) | 3 (100%) | 93 (80.2%) |
| Lymph leakage | 0 | 2 (2.6%) * | 0 | 0 | 2 (1.7%) |
| Fistula formation | 0 | 3 (3.9%) | 2 (6.3%) | 1 (33.3%) | 6 (5.2%) |
| Grade IIIb | Grade IIIc | p | |
|---|---|---|---|
| Characteristics | |||
| Patient number | 77 | 32 | - |
| Age (years) | 56.3 ± 10.6 | 56.0 ± 11.1 | 0.901 |
| Male | 72 (93.5) | 27 (84.4) | 0.154 |
| Body mass index (kg/m2) | 23.7 ± 4.6 | 24.8 ± 3.3 | 0.263 |
| Current or former smoker | 62 (80.5) | 24 (75.0) | 0.608 |
| Alcoholism | 56 (72.7) | 16 (50.0) | 0.028 * |
| Comorbidity | |||
| Diabetes mellitus | 23 (29.9) | 10 (31.3) | 1.000 |
| Hypertension | 37 (48.1) | 14 (43.8) | 0.833 |
| ASA classification | 1.000 | ||
| 1–2 | 40 (51.9) | 17 (53.1) | |
| 3–4 | 37 (48.1) | 15 (46.9) | |
| Charlson Comorbidity Index score | 4.2 ± 1.7 | 3.8 ± 1.5 | 0.219 |
| Previous operation | 29 (37.7) | 19 (59.4) | 0.056 |
| Previous C/T | 22 (28.6) | 11 (34.4) | 0.648 |
| Previous R/T | 26 (33.8) | 12 (37.5) | 0.826 |
| Surgical etiology | |||
| Primary malignancy | 49 (63.6) | 14 (43.8) | 0.088 |
| Recurrent/Residual cancer | 20 (26.0) | 14 (43.8) | 0.075 |
| Previous free flap reconstruction | 10 (13.0) | 5 (15.6) | 0.763 |
| Cancer status | |||
| T stage | 0.520 | ||
| 1–2 | 32 (42.7) | 11 (34.4) | |
| 3–4 | 43 (57.3) | 21 (65.6) | |
| N stage | 0.667 | ||
| 0–1 | 40 (55.6) | 19 (61.3) | |
| >1 | 32 (44.4) | 12 (38.7) | |
| Overall cancer stage | 0.321 | ||
| Early | 19 (25.3) | 5 (15.6) | |
| Advanced | 56 (74.7) | 27 (84.4) | |
| Associated surgical procedures | |||
| Tracheostomy | 64 (83.1) | 27 (84.4) | 1.000 |
| Neck dissection | 55 (71.4) | 18 (56.3) | 0.179 |
| Outcome | Grade IIIb | Grade IIIc | p | B or Odds Ratio (95% CI) | p |
|---|---|---|---|---|---|
| Categorical variable | |||||
| Wound infection (%) | 23 (29.9) | 20 (62.5) | 0.002 * | 3.91 (1.65–9.30) | 0.002 * |
| Continuous variable | |||||
| Reoperation times during the current hospitalization | 1.4 ± 0.8 | 2.0 ± 1.0 | <0.001 * | 2.21 (1.45, 2.97) | <0.001 * |
| ICU stay (day) | 6.0 ± 3.4 | 8.7 ± 4.3 | 0.001 * | 2.71 (1.17, 4.24) | 0.001 * |
| Hospital stay (day) | 23.1 ± 10.1 | 28.6 ± 11.9 | 0.015 * | 0.20 (0.15, 0.25) | <0.001 * |
| Grade | Definition |
|---|---|
| I | Any deviation from the normal postoperative course without the need for pharmacological treatment or surgical, endoscopic, or radiological interventions |
| II | Requiring pharmacological treatment with drugs other than those permitted for grade I complication (would include blood transfusions and total parenteral nutrition) |
| III | Requiring surgical, endoscopic, or radiological intervention |
| IIIa | Intervention not under general anesthesia |
| IIIb | Intervention under general anesthesia |
| IIIc | “Partial or total free flap failure after intervention” needing further surgery under general anesthesia |
| IV | Life-threatening complication (including complications of the central nervous system) that requires management in a high dependency or intensive therapy unit |
| IVa | Single organ dysfunction (including dialysis) |
| IVb | Multiorgan dysfunction |
| V | Death |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jan, W.-L.; Chen, H.-C.; Chang, C.-C.; Chen, H.-H.; Shih, P.-K.; Huang, T.-C. Modified Clavien–Dindo Classification and Outcome Prediction in Free Flap Reconstruction among Patients with Head and Neck Cancer. J. Clin. Med. 2020, 9, 3770. https://doi.org/10.3390/jcm9113770
Jan W-L, Chen H-C, Chang C-C, Chen H-H, Shih P-K, Huang T-C. Modified Clavien–Dindo Classification and Outcome Prediction in Free Flap Reconstruction among Patients with Head and Neck Cancer. Journal of Clinical Medicine. 2020; 9(11):3770. https://doi.org/10.3390/jcm9113770
Chicago/Turabian StyleJan, Wei-Ling, Hung-Chi Chen, Chang-Cheng Chang, Hsin-Han Chen, Pin-Keng Shih, and Tsung-Chun Huang. 2020. "Modified Clavien–Dindo Classification and Outcome Prediction in Free Flap Reconstruction among Patients with Head and Neck Cancer" Journal of Clinical Medicine 9, no. 11: 3770. https://doi.org/10.3390/jcm9113770
APA StyleJan, W.-L., Chen, H.-C., Chang, C.-C., Chen, H.-H., Shih, P.-K., & Huang, T.-C. (2020). Modified Clavien–Dindo Classification and Outcome Prediction in Free Flap Reconstruction among Patients with Head and Neck Cancer. Journal of Clinical Medicine, 9(11), 3770. https://doi.org/10.3390/jcm9113770




