Abstract
Background/Objectives: The prevention of foot ulcers is a priority for the preservation of the integrity of limbs in subjects with Diabetes Mellitus. Footwear is one of the main causes of ulceration regarding this chronic disease. An in-depth study of the influence of footwear is necessary for the establishment of a prevention strategy for foot injuries. This paper aims to identify the type of footwear used by patients with Diabetes Mellitus and to analyse its characteristics and fit to the foot. Methods: The scientific literature was retrieved from the PubMed, Web of Science, and Dialnet databases that covered publications from 2016 to 2025. The inclusion criteria accepted articles that focused on footwear fit and its relationship with ulceration in diabetic patients. Results: A total of 27 articles were selected for study. These articles describe the fitting and features of footwear for a correct adjustment for people with Diabetes. Conclusions: Most of the population with Diabetes Mellitus use poorly adjusted footwear. Incorrect length and width, as well as unsuitable features of the sole and upper, cause patients to become susceptible to the creation of ulcers.
1. Introduction
Diabetes Mellitus (DM) is a chronic, serious metabolic disorder characterised by persistent hyperglycaemia resulting from impaired insulin secretion, insulin action, or both. This dysfunction hinders the cellular uptake of glucose, thereby disrupting normal energy metabolism and storage. Current estimates indicate a global prevalence of DM in approximately 589 million adults aged 20 to 79 years, which represents 11.1% of the worldwide population [1].
Diabetes Mellitus entails a range of health complications, and particularly affects the lower limbs, including Peripheral Neuropathy (PN) and Peripheral Arterial Disease (PAD) [2]. Recently, the International Working Group on the Diabetic Foot (IWGDF) introduced the term Diabetes-Related Foot Disease, which encompasses all diabetes-related complications that affect the foot [3]. Due to sensory, motor, and autonomic neuropathies, patients experience alterations in protective sensation, deformities, and biomechanical abnormalities, as well as viscoelastic disturbances in the skin of the feet [4]. When these changes are compounded by trauma and varying degrees of peripheral vascular disease, they can lead to foot ulceration, with an increased susceptibility to infection, and result in a clinical condition known as Diabetic Foot [4]. It is estimated that up to 34% of diabetic patients develop a foot ulcer at some point in their lifetime [3].
According to the IWGDF, the use of inappropriate footwear (and walking barefoot) is one of the primary causes of trauma, which, in neuropathic feet under the aforementioned conditions and multiple risk factors, significantly increases the predisposition to the development of ulcers [5].
It is estimated that between 33% and 82% of individuals with DM wear improperly fitting footwear [6], which causes microtraumas that lead to excessive mechanical pressure and friction on the foot, potentially triggering stress ulcers of the skin and underlying tissues [7]. If the existing injury is compounded by the patient’s lack of awareness due to peripheral neuropathy and continued use of the same footwear, then the shoe becomes a perpetuating and aggravating factor of the ulcer [5], which carries a potential risk of infection and progression to amputation [7].
The literature provides a vast store of evidence regarding the importance of offloading in the management and healing of diabetic foot ulcers with a neuropathic component, and of the use of therapeutic footwear in the prevention of ulcers in these patients. However, adherence to these methods remains low among patients [8,9].
Prevention of ulceration is essential to reduce patient comorbidities and healthcare costs. It is therefore crucial to ensure proper footwear fit, together with the application of the appropriate materials and design adapted to the morpho-functional conditions of diabetic patients [7].
In this article, a narrative review of studies is conducted that focuses on the footwear fit and features that produce poor foot adjustments in people with Diabetes Mellitus.
2. Materials and Methods
2.1. Search Strategy
The study was initially designed to conduct a systematic review registered in Prospero CRD42024604216, to answer the question: “Is the footwear worn by people with Diabetes appropriate? Due to the lack of literature that met the inclusion criteria, the authors have decided to carry out a narrative review.
An extensive search was carried out between February and June 2025 in several databases, including PubMed, Web of Science, Dialnet, and the FAMA catalogue of the University of Seville.
The Scopus database was not reflected since the PubMed database already encompassed the articles indexed in Scopus.
Subsequently, in an additional search of the Web of Science database, two new studies were found that met the inclusion criteria.
To optimise the search, health-related descriptors relevant to the subject were used, along with free terms combined with Boolean operators, and in some cases,
MeSH terms: “Diabetes Mellitus”, “Shoes”, “Ulcers”, “Diabetic foot” and “Prevention”. An advanced search tool was employed in all cases to design the search strategies. A specific strategy was developed for each database, which is given in detail in
Table 1.

Table 1.
Schematic summary of the databases, search strategies, filters, and results obtained from the search.
The aim of this review was to assess the existing evidence on the outcomes of fitting and footwear features that produce a poor adjustment in people with DM.
2.2. Selection Criteria and Study Selection
The selection was not limited to any specific article design, due to the insufficient number of publications for a systematic review to be conducted on the topic, and valuable information could have been lost if a limit had been imposed. This led us to carry out a narrative review, including articles with different levels of scientific evidence, published in English or Spanish, with a filter for the past 10 years.
The inclusion criteria for this review, therefore, encapsulated the following: articles addressing footwear fit and its correlation with the development of ulcers in patients with diabetes.
The exclusion criteria included: documents published before 2016, those written in languages other than English or Spanish, those that do not refer to footwear in adults and/or individuals with Diabetes Mellitus, and those related to therapeutic footwear prescribed for a specific pathological condition.
For the study selection process, two independent reviewers, R.C.-S. and S.B.-B., were appointed. Each reviewer conducted the selection process independently. In the initial stage, they screened the titles and abstracts of the shortlisted articles. Both reviewers then individually assessed whether the studies met the inclusion and exclusion criteria. Moreover, they separately evaluated the key characteristics of the studies to ensure strict adherence to the defined eligibility criteria.
In instances where disagreements arose regarding the inclusion of specific articles, a third reviewer (M.R.-B.) was consulted to carry out the final determination on the suitability of the article in question.
2.3. Data Extraction
In order to facilitate data extraction from the articles included in this review, Zotero 7.0.27 for Windows (Roy Rosenzweig Center for History and New Media, George Mason University, Fairfax, VA, USA) was employed for reference management, identification of duplicate records, and organisation of the bibliographic database. An Excel spreadsheet of Microsoft Windows 365 (Microsoft Corporation, Redmond, WA, USA) was created to systematically extract, categorise, and synthesise the information from each study. The inclusion or exclusion of each study was documented. Each reviewer maintained their own worksheet. Following the final assessment, the results were consolidated, and any discrepancies regarding article inclusion or exclusion were discussed. Initially, these discussions took place between the two primary reviewers, although in certain cases, the involvement of a third reviewer was required to reach a final decision.
Ultimately, two reviewers (R.C.-S. and I.C.P-T.) performed the complete data extraction for the articles selected subsequent to the second assessment. For this task, a Word document was utilised to record the identification and key characteristics of the studies (study type, number of participants, mean age, intervention, outcomes, etc.), thereby ensuring strict adherence to the eligibility criteria established for the review.
3. Results
3.1. Study Selection
A total of 1420 articles were identified through the search. After having screened the titles and abstracts, a further 1275 articles were excluded. Full-text screening of the remaining 145 studies was then conducted, resulting in the 27 final inclusion of relevant articles. In cases where discrepancies arose between the two researchers, they discussed the articles to reach a consensus. Following the full-text review, 2 studies were rejected since they contained irrelevant information. Table 1 shows the search strategies, and Figure 1, the selection process of the studies included in this review.
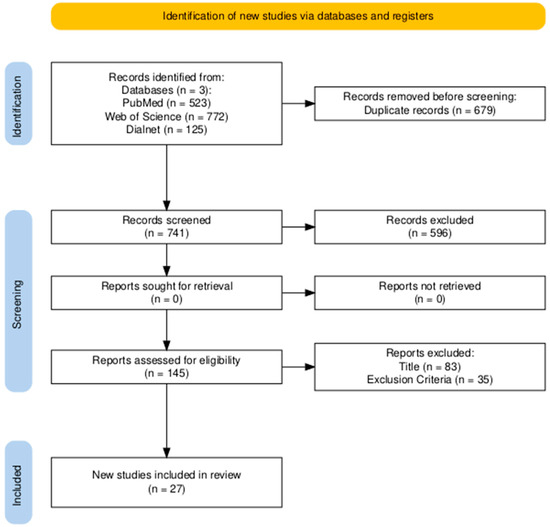
Figure 1.
PRISMA flow diagram adopted for this review.
3.2. Study Characteristics
Among the 27 studies included in the review, 3 were Systematic Reviews and Meta-analyses [10,11,12], 4 were Systematic Reviews [4,13,14,15], 1 was a Randomised Clinical Trial [16], 1 was a Case–Control Study [17], 8 were Observational Studies [7,18,19,20,21,22,23,24], 1 was a Qualitative Study [25], and 9 were Narrative Reviews [5,6,26,27,28,29,30,31,32]. Due to the different types of design, the levels of evidence vary widely. The main outcomes of each article are summarised in Table 2.

Table 2.
Description and main outcomes of the articles studied.
The scientific literature on footwear for patients with Diabetes Mellitus reveals a progressive consensus regarding specific design features that contribute to the prevention and reduction in plantar ulcers. First, rigid soles and rocker sole designs constitute the most frequent recommendation, appearing in approximately 43% of the reviewed studies. Bus et al. [13,29] and Premkumar et al. [17] highlight their capacity to decrease plantar pressure and prevent forefoot ulceration. López-Moral et al. [16,20] demonstrate that rigid soles reduce ulcer recurrence by 64% compared to semi-rigid soles. Collings et al. [10] and Ahmed et al. [14] provide systematic evidence that these soles reduce metatarsal head pressure by 30–50%. Lastly, Van Netten et al. [12] confirm that footwear with rigid soles decreases both the incidence of initial ulcers and their recurrence.
Secondly, toe-box spacing and internal shoe length are identified as critical factors in approximately 29% of the studies. Mohamed et al. [18] recommend an excess length of 1–2 cm beyond the foot, while Bus et al. [29] and Jones et al. [30] suggest an optimal range of 1–1.5 cm, accompanied by a sufficiently high toe box. Chicharro-Luna et al. [7] and Zhang et al. [23] add that the toe box should be rounded and manufactured with elastic materials to accommodate wide or deformed feet. Schaper et al. [5] and Van Netten et al. [12] concur that such spacing is essential to prevent friction and deformities.
Regarding materials, 25% of the studies emphasise the need for footwear to be flexible, breathable, and free of internal seams. Mohamed et al. [18] and Chicharro-Luna et al. [7] recommend natural leather. Bus et al. [29] underline the importance of flexible tongues and durable materials, while Zhang et al. [23] propose elastic materials to accommodate deformities.
The heel height is mentioned in 18% of the studies, with recommendations ranging from 1.5 to 3 cm to ensure stability without increasing forefoot pressure [5,7,14,18,29]. Likewise, the fastening system (laces or Velcro) appears in 21% of the studies, and is considered by Barwick et al. [19], Bus et al. [29], Ahmed et al. [14], and Schaper et al. [5] as fundamental to securing the foot and ensuring stability within the shoe.
The Scale for the Assessment of Narrative Review Articles (SANRA) was completed to rate the quality of this review. See
Appendix A.
4. Discussion
Microtrauma, which may lead to ulceration in subjects with DM, represents a significant clinical concern. According to Armstrong et al. [3], up to 34% of individuals with DM develop foot ulcers, with repetitive microtrauma being a notable contributing factor. Abu-Qamar et al. [31] identified footwear as the second most frequent external cause of foot trauma in those patients, accounting for 16.2% of cases.
Footwear type and its features involve multifaceted parameters that are difficult to analyse. Moreover, the correct adjustment of several specific components, such as length, width, materials, and cushioning, presents a challenge to researchers.
In their 2023 publication of the IWGDF Practical Guidelines, Schaper et al. [5] identified ill-fitting footwear as one of the primary causes of foot trauma leading to ulceration. This conclusion is reinforced by Reddie et al. [32], who noted that, in low- and middle-income countries, contrary to the general recommendations for individuals with DM, sandals and flip-flops are the most commonly worn types of footwear.
Populations with lower socio-economic status not only face financial constraints but also tend to have limited health literacy. This is particularly evident among individuals with DM, who generally exhibit lower socio-economic levels compared to non-diabetic populations. Consequently, many are unaware of ulcer prevention strategies, and even when informed, may be unable to afford properly fitted footwear, resorting instead to cheaper alternatives such as sandals and flip-flops.
It should be borne in mind that this phenomenon also occurs in high-income countries with warm climates, such as Spain, where sandals are commonly worn from spring through to autumn due to their breathability, despite being suboptimal for foot protection.
This issue is further supported by Chicharro-Luna et al. [7], who found that most patients with PN did not wear appropriate footwear. Their study revealed that out of 17 subjects with PN, 11 (67.4%) were not using optimal footwear. Although the sample size of PN patients was limited (—only 17 out of 108 participants), the data aligns closely with the findings of Buldt and Menz [6], and offers a valuable insight into the broader reality.
These economic and demographic determinants suggest that international guidelines (largely developed in high-income settings) may not always be feasible or practical in other contexts. Therefore, diabetic foot experts and local healthcare stakeholders should collaborate in order to adapt or redesign preventive recommendations and footwear-related strategies that are both realistic and culturally acceptable.
A positive aspect was highlighted by Malki et al. [25], who found that comfort and fit were the most valued factors among PN patients when selecting footwear. Although their study is limited by its small sample size (24 participants), it is noteworthy that patients prioritise fit and comfort despite their lack of foot sensitivity. This paradox underscores the main challenge in footwear fitting for individuals with DM and PN: their inability to perceive whether the shoe is properly fitted. As described by Malki et al. [25], although patients pay close attention to fit, the reality (as demonstrated by multiple studies) is that the majority wear inadequately fitted footwear.
Buldt and Menz [6] reported that between 10% and 43% of individuals with DM wore shoes that were too short, 23% to 81% wore shoes that were excessively long, and 46% wore shoes that were too narrow. Furthermore, they emphasised that individuals wearing overly tight footwear were five times more likely to develop foot ulcers. These findings are particularly concerning, since they suggest that nearly half of the diabetic population with PN wears shoes that are too narrow, thereby significantly increasing their risk of ulceration.
Abu-Qamar et al. [31] further classified poor fit, incorrect sizing, narrow footwear, and the use of new shoes as sources of microtrauma, and underscored the importance of evaluating all structural elements of footwear.
Regarding shoe length fit, Buldt and Menz [6] recommended a clearance of 10–15 mm between the foot length and the internal length of the shoe. Jones et al. [15] suggested that fit is inadequate if the clearance is less than 2 mm or exceeds 10 mm, although in a subsequent study, they proposed an optimal range of 10–20 mm. The prevailing consensus indicates that deviations outside the 10–15 mm interval may result in improper fit and potential microtrauma.
In terms of width fit, Jones et al. [28] stated that the shoe should match the width of the foot at the metatarsophalangeal joints. Nevertheless, a margin of 2–3 mm on each side is advisable to accommodate dynamic changes in foot volume during gait, as highlighted by Zhang et al. [23], particularly in the presence of deformities such as hallux abductus valgus.
The shoe sole is another critical component. Premkumar et al. [17] noted that cushioning midsoles offer limited stability. Collings et al. [10] emphasised that sole materials should be selected based on offloading requirements. López-Moral et al. [16] and Ahmed et al. [14] concluded that semi-rigid and cushioned soles impair propulsion and increase forefoot plantar pressure, thereby rendering them less suitable for patients with DM and motor neuropathy.
The shoe upper must be flexible, breathable, and free of internal seams. Van Netten et al. [12], Igiri et al. [27], and Chicharro-Luna et al. [7] agreed that it should be made of natural leather or high-quality synthetic textiles. While leather is preferred for its durability and adaptability, synthetic materials may offer similar properties at a lower cost, albeit with reduced longevity. Internal seams should be avoided, as they may cause friction and skin erosion, potentially leading to ulceration.
Collectively, the reviewed studies underscore that improper footwear, whether regarding length, width, sole, or upper, can induce microtrauma and elevate the risk of ulceration in individuals with DM. It is therefore imperative that healthcare professionals, particularly podiatrists, thoroughly assess footwear design and fit in this vulnerable population.
In this context, only a few studies explore footwear selection habits in this population. The factors influencing footwear acquisition and the motivation to change footwear habits when individuals receive specific information regarding its impact on the foot remain unknown. Qualitative research could help towards understanding this issue. Neither do preventive measures appear to be effective, nor is there any common type of footwear that can be considered “protective” for the feet of this population. This term is used by several authors, like Barwick et al. [19], in contrast to so-called “therapeutic footwear,” which tends to be specifically prescribed for particular foot conditions.
We plan to conduct a qualitative study that employs semi-structured interviews, through which people with diabetes can explain the criteria they follow when selecting footwear and the motivations underlying their choices. Moreover, the interview guide will incorporate questions to assess participants’ knowledge of self-care foot practices and their understanding of the types of footwear most appropriate for their condition.
This study has certain limitations, partly due to the variability in the types of designs of the articles included, and also owing to the different levels of evidence. Furthermore, the methodological quality of these articles remains unknown and should be assessed, either through verification guides or by evaluating the risk of bias.
Future studies are needed to establish the ideal type of footwear and the potentially beneficial features for this population in order to guide the prevention strategies that ensure the full collaboration of patients for the preservation of lower-limb health.
5. Conclusions
The use of inappropriate footwear remains a widespread issue among individuals with Diabetes Mellitus, constituting a major contributing factor to the development of repetitive microtrauma and subsequent foot ulceration. The limited number of available studies, together with their methodological heterogeneity, underscores the absence of standardized protocols to assess footwear adequacy in this population.
Recommendations concerning proper shoe length, adequate width, rigid soles, and seamless upper materials have demonstrated efficacy in reducing plantar pressure and lowering the risk of ulceration. Nevertheless, adherence to these recommendations remains insufficient.
From a public health perspective, effective prevention strategies must integrate patient education on foot self-care, routine footwear assessment in primary care settings, and programs that facilitate access to appropriate footwear. Additionally, the lack of studies exploring the personal criteria used by individuals with diabetes when selecting their shoes supports the need for research aimed at designing interventions better aligned with patients’ social and economic realities.
Author Contributions
Conceptualisation, R.C.-S., M.R.-B., M.d.C.V.-B., and S.B.-B.; methodology, R.C.-S., S.B.-B., and M.R.-B.; software, R.C.-S., M.R.-B., and I.C.P.-T.; validation, R.C.-S., M.R.-B., and I.C.P.-T.; formal analysis, R.C.-S.; investigation, R.C.-S.; resources, R.C.-S., M.R.-B., and S.B.-B.; writing—original draft preparation, R.C.-S.; writing—review and editing, M.R.-B., and I.C.P.-T.; visualisation, R.C.-S., S.B.-B., and M.d.C.V.-B.; supervision, M.R.-B., and I.C.P.-T.; project administration, R.C.-S., and M.R.-B.; funding acquisition, not applicable. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare there to be no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| DM | Diabetes Mellitus |
| PN | Peripheral Neuropathy |
| PAD | Peripheral Arterial Disease |
| IWGDF | International Working Group on the Diabetic Foot |
Appendix A
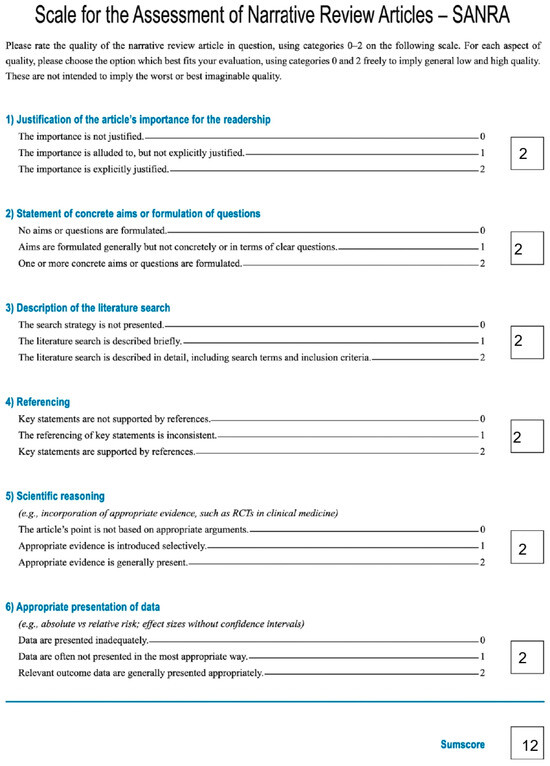
Figure A1.
Scale for the Assessment of Narrative Review Articles—SANRA.
References
- IDF Diabetes Atlas 2025, 11th ed.; International Diabetes Federation: Brussels, Belgium, 2021; ISBN 978-2-930229-96-6.
- Røikjer, J.; Ejskjaer, N. Diabetic Peripheral Neuropathy. Handb. Exp. Pharmacol. 2022, 274, 309–328. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Tan, T.-W.; Boulton, A.J.M.; Bus, S.A. Diabetic Foot Ulcers: A Review. JAMA 2023, 330, 62–75. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Panero, A.J.; Ruiz-Muñoz, M.; Cuesta-Vargas, A.I.; Gónzalez-Sánchez, M. Prevention, Assessment, Diagnosis and Management of Diabetic Foot Based on Clinical Practice Guidelines: A Systematic Review. Medicine 2019, 98, e16877. [Google Scholar] [CrossRef] [PubMed]
- Schaper, N.C.; van Netten, J.J.; Apelqvist, J.; Bus, S.A.; Fitridge, R.; Game, F.; Monteiro-Soares, M.; Senneville, E. Practical Guidelines on the Prevention and Management of Diabetes-Related Foot Disease (IWGDF 2023 Update). Diabetes Metab. Res. Rev. 2024, 40, e3657. [Google Scholar] [CrossRef]
- Buldt, A.K.; Menz, H.B. Incorrectly Fitted Footwear, Foot Pain and Foot Disorders: A Systematic Search and Narrative Review of the Literature. J. Foot Ankle Res. 2018, 11, 43. [Google Scholar] [CrossRef]
- Chicharro-Luna, E.; Ortega-Avila, A.B.; Requena-Martínez, A.; Gijon-Nogueron, G. Fit for Purpose? Footwear for Patients with and without Diabetic Peripheral Neuropathy: A Cross-Sectional Study. Prim. Care Diabetes 2021, 15, 145–149. [Google Scholar] [CrossRef]
- Bus, S.A.; Armstrong, D.G.; Crews, R.T.; Gooday, C.; Jarl, G.; Kirketerp-Moller, K.; Viswanathan, V.; Lazzarini, P.A. Guidelines on Offloading Foot Ulcers in Persons with Diabetes (IWGDF 2023 Update). Diabetes Metab. Res. Rev. 2024, 40, e3647. [Google Scholar] [CrossRef]
- Lazzarini, P.A.; Armstrong, D.G.; Crews, R.T.; Gooday, C.; Jarl, G.; Kirketerp-Moller, K.; Viswanathan, V.; Bus, S.A. Effectiveness of Offloading Interventions for People with Diabetes-Related Foot Ulcers: A Systematic Review and Meta-Analysis. Diabetes Metab. Res. Rev. 2024, 40, e3650. [Google Scholar] [CrossRef]
- Collings, R.; Freeman, J.; Latour, J.M.; Paton, J. Footwear and Insole Design Features for Offloading the Diabetic at Risk Foot-A Systematic Review and Meta-Analyses. Endocrinol. Diabetes Metab. 2021, 4, e00132. [Google Scholar] [CrossRef]
- Luo, B.; Cai, Y.; Chen, D.; Wang, C.; Huang, H.; Chen, L.; Gao, Y.; Ran, X. Effects of Special Therapeutic Footwear on the Prevention of Diabetic Foot Ulcers: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Diabetes Res. 2022, 2022, 9742665. [Google Scholar] [CrossRef]
- van Netten, J.J.; Raspovic, A.; Lavery, L.A.; Monteiro-Soares, M.; Paton, J.; Rasmussen, A.; Sacco, I.C.N.; Bus, S.A. Prevention of Foot Ulcers in Persons with Diabetes at Risk of Ulceration: A Systematic Review and Meta-Analysis. Diabetes Metab. Res. Rev. 2024, 40, e3652. [Google Scholar] [CrossRef]
- Bus, S.A.; van Deursen, R.W.; Armstrong, D.G.; Lewis, J.E.A.; Caravaggi, C.F.; Cavanagh, P.R. Footwear and Offloading Interventions to Prevent and Heal Foot Ulcers and Reduce Plantar Pressure in Patients with Diabetes: A Systematic Review. Diabetes Metab. Res. Rev. 2016, 32 (Suppl. S1), 99–118. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Barwick, A.; Butterworth, P.; Nancarrow, S. Footwear and Insole Design Features That Reduce Neuropathic Plantar Forefoot Ulcer Risk in People with Diabetes: A Systematic Literature Review. J. Foot Ankle Res. 2020, 13, 30. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.; Davies, M.J.; Khunti, K.; Fong, D.T.P.; Webb, D. In-Shoe Pressure Thresholds for People with Diabetes and Neuropathy at Risk of Ulceration: A Systematic Review. J. Diabetes Complicat. 2021, 35, 107815. [Google Scholar] [CrossRef] [PubMed]
- López-Moral, M.; Lázaro-Martínez, J.L.; García-Morales, E.; García-Álvarez, Y.; Álvaro-Afonso, F.J.; Molines-Barroso, R.J. Clinical Efficacy of Therapeutic Footwear with a Rigid Rocker Sole in the Prevention of Recurrence in Patients with Diabetes Mellitus and Diabetic Polineuropathy: A Randomized Clinical Trial. PLoS ONE 2019, 14, e0219537. [Google Scholar] [CrossRef]
- Premkumar, R.; Rajan, P.; Rima, J.; Richard, J. Footwear in the Causation and Prevention of Foot Ulcers in Diabetes Mellitus. Natl. Med. J. India 2017, 30, 255–261. [Google Scholar] [CrossRef]
- Mohamed, O.; Ofiaeli, N.; Syeed, A.; Elhassan, A.; Al Tunaiji, M.; Al Hammadi, K.; Al Ali, M. Assessment of Behaviors, Risk Factors of Diabetic Foot Ulcer and Footwear Safety among Diabetic Patients in Primary Care Setting, Abu Dhabi, UAE. World Fam. Med. 2017, 15, 12–24. [Google Scholar] [CrossRef]
- Barwick, A.; Hurn, S.; van Netten, J.; Reed, L.; Lazzarini, P. Factors Associated with Wearing Inadequate Outdoor Footwear in Populations at Risk of Foot Ulceration: A Cross-Sectional Study. PLoS ONE 2019, 14, e0211140. [Google Scholar] [CrossRef]
- López-Moral, M.; Molines-Barroso, R.J.; Álvaro-Afonso, F.J.; Uccioli, L.; Senneville, E.; Lázaro-Martínez, J.L. Importance of Footwear Outsole Rigidity in Improving Spatiotemporal Parameters in Patients with Diabetes and Previous Forefoot Ulcerations. J. Clin. Med. 2020, 9, 907. [Google Scholar] [CrossRef]
- Zwaferink, J.B.J.; Custers, W.; Paardekooper, I.; Berendsen, H.A.; Bus, S.A. Optimizing Footwear for the Diabetic Foot: Data-Driven Custom-Made Footwear Concepts and Their Effect on Pressure Relief to Prevent Diabetic Foot Ulceration. PLoS ONE 2020, 15, e0224010. [Google Scholar] [CrossRef]
- Chatzistergos, P.E.; Gatt, A.; Formosa, C.; Farrugia, K.; Chockalingam, N. Optimised Cushioning in Diabetic Footwear Can Significantly Enhance Their Capacity to Reduce Plantar Pressure. Gait Posture 2020, 79, 244–250. [Google Scholar] [CrossRef]
- Zhang, L.; Yick, K.-L.; Li, P.-L.; Yip, J.; Ng, S.-P. Foot Deformation Analysis with Different Load-Bearing Conditions to Enhance Diabetic Footwear Designs. PLoS ONE 2022, 17, e0264233. [Google Scholar] [CrossRef] [PubMed]
- Sousa, L.B.; Almeida, I.; Bernardes, R.A.; Leite, T.R.; Negrão, R.; Apóstolo, J.; Salgueiro-Oliveira, A.; Parreira, P. A Three Step Protocol for the Development of an Innovative Footwear (Shoe and Sensor Based Insole) to Prevent Diabetic Foot Ulceration. Front. Public Health 2023, 11, 1061383. [Google Scholar] [CrossRef]
- Malki, A.; Verkerke, G.J.; Dekker, R.; Hijmans, J.M. Factors Influencing the Use of Therapeutic Footwear in Persons with Diabetes Mellitus and Loss of Protective Sensation: A Focus Group Study. PLoS ONE 2023, 18, e0280264. [Google Scholar] [CrossRef]
- van Netten, J.J.; Lazzarini, P.A.; Armstrong, D.G.; Bus, S.A.; Fitridge, R.; Harding, K.; Kinnear, E.; Malone, M.; Menz, H.B.; Perrin, B.M.; et al. Diabetic Foot Australia Guideline on Footwear for People with Diabetes. J. Foot Ankle Res. 2018, 11, 2. [Google Scholar] [CrossRef]
- Igiri, B.E.; Tagang, J.I.; Okoduwa, S.I.R.; Adeyi, A.O.; Okeh, A. An Integrative Review of Therapeutic Footwear for Neuropathic Foot Due to Diabetes Mellitus. Diabetes Metab. Syndr. 2019, 13, 913–923. [Google Scholar] [CrossRef]
- Jones, P.J.; Bibb, R.J.; Davies, M.J.; Khunti, K.; McCarthy, M.; Fong, D.T.P.; Webb, D. A Fitting Problem: Standardising Shoe Fit Standards to Reduce Related Diabetic Foot Ulcers. Diabetes Res. Clin. Pract. 2019, 154, 66–74. [Google Scholar] [CrossRef]
- Bus, S.A.; Zwaferink, J.B.; Dahmen, R.; Busch-Westbroek, T. State of the Art Design Protocol for Custom Made Footwear for People with Diabetes and Peripheral Neuropathy. Diabetes Metab. Res. Rev. 2020, 36 (Suppl. S1), e3237. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.; Bus, S.A.; Davies, M.J.; Khunti, K.; Webb, D. Toe Gaps and Their Assessment in Footwear for People with Diabetes: A Narrative Review. J. Foot Ankle Res. 2020, 13, 70. [Google Scholar] [CrossRef] [PubMed]
- Abu-Qamar, M.Z.; Kemp, V.; Whitehead, L. Foot Ulcers Associated with External Trauma among People with Diabetes: An Integrative Review of the Origin of Trauma and Outcomes. Int. J. Nurs. Stud. 2021, 114, 103822. [Google Scholar] [CrossRef]
- Reddie, M.; Shallal, C.; Frey, D. A Scoping Review of Footwear Worn by People With Diabetes in Low- and Middle-Income Countries: Implications for Ulcer Prevention Programs. Glob. Health Sci. Pract. 2023, 11, e2200392. [Google Scholar] [CrossRef] [PubMed]
- Manterola, C.; Zavando, D. Cómo interpretar los “Niveles de Evidencia” en los diferentes escenarios clínicos∗ Evidence-based clinical practice, levels of evidence. Rev. Chil. Cir. 2009, 61, 582–595. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).