High Tibial Osteotomy (HTO), Unicompartmental Knee Arthroplasty (UKA), and Proximal Fibular Osteotomy (PFO) for Medial-Compartment Knee Osteoarthritis: A Narrative Review of Comparative Mechanisms, Clinical Outcomes, and Decision-Making
Abstract
1. Introduction
2. Methods
2.1. Design and Rationale
2.2. Eligibility Criteria
2.3. Information Sources and Search Window
2.4. Search Strategy
- (“high tibial osteotomy” OR HTO OR osteotomy[tiab]) AND (medial[tiab] OR varus[tiab]) AND (knee[tiab])
- (“unicompartmental knee arthroplasty” OR UKA OR “partial knee”) AND (medial[tiab] OR varus[tiab])
- (“proximal fibular osteotomy” OR PFO) AND (knee[tiab] OR osteoarthritis[tiab])
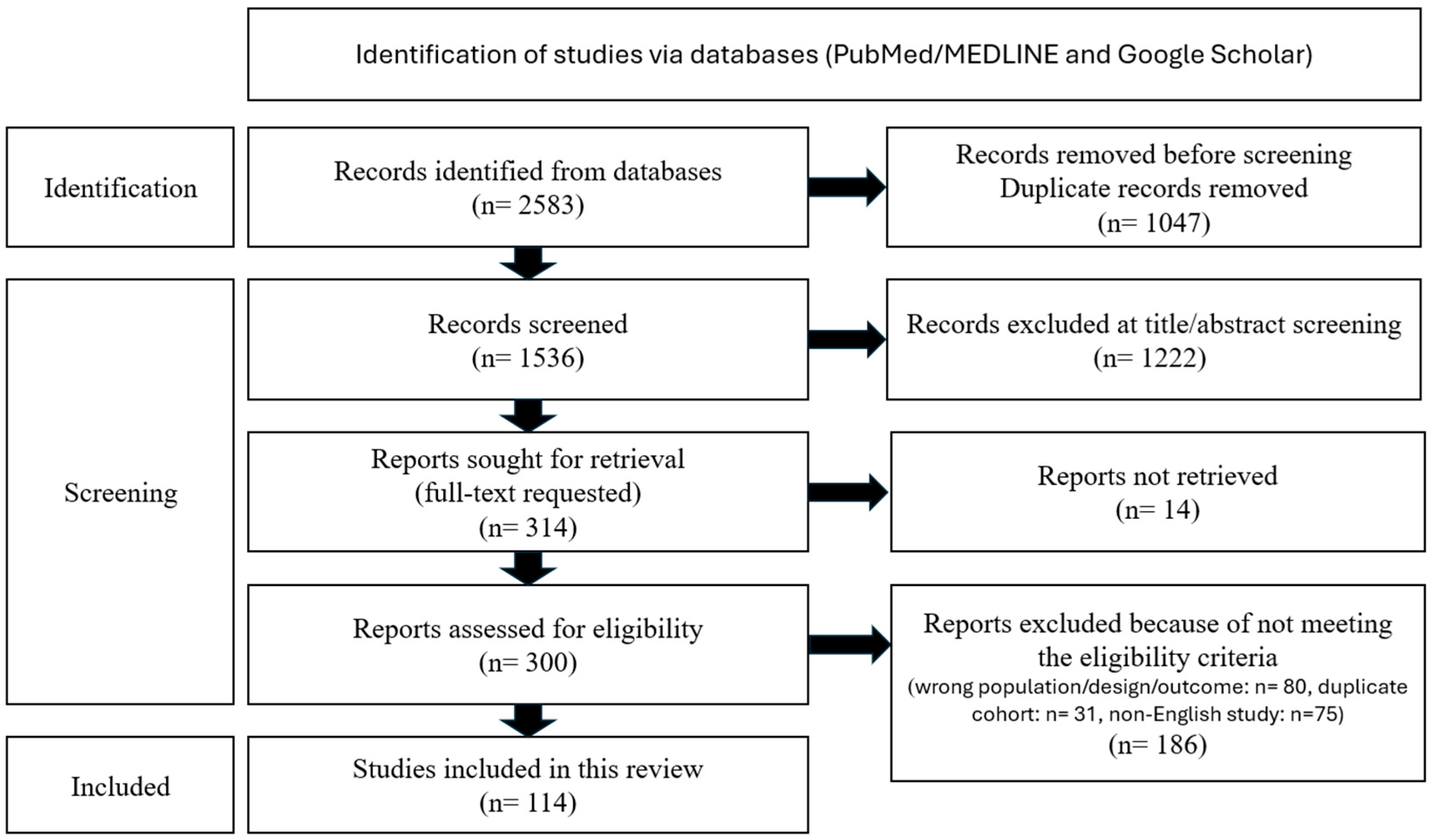
2.5. Study Selection and Data Extraction
2.6. Registration
2.7. Yield
3. Discussion
3.1. Overview of the Evidence Base and Study Designs
3.2. High Tibial Osteotomy (HTO): Durability, Correction Fidelity, and Safety Profile
3.2.1. Durability
3.2.2. Correction Fidelity and Sagittal Control (PTS/Patellofemoral Effects)
3.2.3. Safety Profile
3.3. Unicondylar Knee Arthroplasty (UKA): Early Gains, Revision Modes, and Volume/İmplant Effects
3.3.1. Classic İndications and Contemporary Survivorship
3.3.2. UKA—Early Pain Relief
3.3.3. UKA—Registries and Real-World Revision Burden
3.3.4. UKA—Cost-Effectiveness and Resource Use
3.3.5. Failure Modes, Bearing Design, and Learning Curve
3.3.6. Limitations/Heterogeneity Note
3.4. Proximal Fibular Osteotomy (PFO): Hypothesized Mechanism, Early Clinical Signal, and Heterogeneity
3.5. Head-to-Head Comparative Effectiveness
3.6. Biomechanics and Radiographic Consequences That Shape Outcomes
3.7. Return to Work/Sport, Satisfaction, and Predictors
3.8. Complications, Reoperations, and Survivorship—What the Large Datasets Show
3.9. Practicalities: Peri-Operative Burden, Learning Curve, and Health-System Context
3.10. Patient Selection—Aligning Mechanics with Goals and Comorbidity
3.11. Synthesis and Clinical Guidance
3.12. Gaps and Priorities for Future Research
3.13. Limitations of This Narrative Review
4. Conclusions
Supplementary Materials
Funding
Data Availability Statement
Conflicts of Interest
List of Abbreviations
| ADL | Activities of Daily Living |
| AKSS | American Knee Society Score (often used interchangeably with KSS) |
| BMI | Body Mass Index |
| CAS | Computer-Assisted Surgery |
| CI | Confidence Interval |
| CPN | Common Peroneal Nerve |
| CWHTO | Closing-Wedge High Tibial Osteotomy (also written LCWHTO for “lateral” closing-wedge) |
| DMM | Destabilization of the Medial Meniscus (preclinical mouse OA model) |
| DVT | Deep Vein Thrombosis |
| EQ-5D | EuroQol-5 Dimensions Health Utility Index |
| FE/FEA | Finite-Element (Analysis) |
| FTA | Femorotibial Angle |
| HKA | Hip–Knee–Ankle Angle |
| HSS | Hospital for Special Surgery (knee) Score |
| HTO | High Tibial Osteotomy |
| HR | Hazard Ratio |
| IPTW | Inverse Probability of Treatment Weighting |
| JLCA | Joint Line Convergence Angle |
| JS/JSW | Joint Space/Joint Space Width |
| JSR | Joint Space Ratio (e.g., medial:lateral) |
| KL | Kellgren–Lawrence (radiographic osteoarthritis grading) |
| KOA | Knee Osteoarthritis |
| KOOS | Knee Injury and Osteoarthritis Outcome Score |
| KSS/KSFS | Knee Society Score/Knee Society Function Score |
| LDFA | Lateral Distal Femoral Angle |
| LOE | Level of Evidence |
| MCID | Minimal Clinically Important Difference |
| MD | Mean Difference (effect-size metric) |
| MCL | Medial Collateral Ligament |
| MOWHTO | Medial (Opening-Wedge) High Tibial Osteotomy |
| MPTA | Medial Proximal Tibial Angle |
| OA | Osteoarthritis |
| OKS | Oxford Knee Score |
| OR | Odds Ratio |
| OWHTO | Opening-Wedge High Tibial Osteotomy |
| PF/PFJ | Patellofemoral/Patellofemoral Joint |
| PFO | Proximal Fibular Osteotomy |
| PRO/PROs | Patient-Reported Outcome(s) |
| PSI | Patient-Specific Instrumentation (guides/templates) |
| PTS | Posterior Tibial Slope |
| QoL | Quality of Life |
| RCT | Randomized Controlled Trial |
| ROM | Range of Motion |
| TKA | Total Knee Arthroplasty |
| UCLA | University of California, Los Angeles Activity Score |
| UKA | Unicompartmental Knee Arthroplasty |
| WBL/WBLR | Weight-Bearing Line/Weight-Bearing-Line Ratio |
References
- Hui, C.; Salmon, L.J.; Kok, A.; Williams, H.A.; Hockers, N.; Van Der Tempel, W.M.; Chana, R.; Pinczewski, L.A. Long-term survival of high tibial osteotomy for medial compartment osteoarthritis of the knee. Am. J. Sports Med. 2011, 39, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Flecher, X.; Parratte, S.; Aubaniac, J.-M.; Argenson, J.-N.A. A 12–28-year followup study of closing wedge high tibial osteotomy. Clin. Orthop. Relat. Res. 2006, 452, 91–96. [Google Scholar] [CrossRef]
- Papachristou, G.; Plessas, S.; Sourlas, J.; Levidiotis, C.; Chronopoulos, E.; Papachristou, C. Deterioration of long-term results following high tibial osteotomy in patients under 60 years of age. Int. Orthop. 2006, 30, 403–408. [Google Scholar] [CrossRef]
- Khakha, R.S.; Bin Abd Razak, H.R.; Kley, K.; van Heerwaarden, R.; Wilson, A.J. Role of high tibial osteotomy in medial compartment osteoarthritis of the knee: Indications, surgical technique and outcomes. J. Clin. Orthop. Trauma 2021, 23, 101618. [Google Scholar] [CrossRef]
- Ranjan, P.; Anand, R.; Choudhary, R. Functional Outcome of Proximal Fibular Osteotomy in Medial Compartment Knee Osteoarthritis. J. Orthop. Dis. Traumatol. 2021, 4, 107–110. [Google Scholar] [CrossRef]
- Kakumanu, R.K.; Kunadharaju, R.T.; Ganesh, C. Prospective Study of Functional and Radiological Outcome of Proximal Fibular Osteotomy for Medial Compartment Osteoarthritis in Elderly. J. Orthop. Dis. Traumatol. 2021, 4, 86–91. [Google Scholar] [CrossRef]
- Ahmed, M.; Bux, M.; Kumar, M.; Ahmed, N.; Hussain, G.; Ishtiyaque, M. Proximal Fibular Osteotomy in the Management of Osteoarthritis of Medial Compartment of Knee Joint. Cureus 2020, 12, e8481. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.O.; Wilson, A.J.; Thomas, N.P. Osteotomy around the knee: Evolution, principles and results. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 3–22. [Google Scholar] [CrossRef]
- Hinterwimmer, S.; Beitzel, K.; Paul, J.; Kirchhoff, C.; Sauerschnig, M.; Von Eisenhart-Rothe, R.; Imhoff, A.B. Control of posterior tibial slope and patellar height in open-wedge valgus high tibial osteotomy. Am. J. Sports Med. 2011, 39, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Rodner, C.M.; Adams, D.J.; Diaz-Doran, V.; Tate, J.P.; Santangelo, S.A.; Mazzocca, A.D.; Arciero, R.A. Medial opening wedge tibial osteotomy and the sagittal plane: The effect of increasing tibial slope on tibiofemoral contact pressure. Am. J. Sports Med. 2006, 34, 1431–1441. [Google Scholar] [CrossRef]
- Constantin, H.; Salmon, L.J.; Russell, V.; Sundaraj, K.; Roe, J.P.; Pinczewski, L.A. 20-Year Outcomes of High Tibial Osteotomy: Determinants of Survival and Functional Outcome. Am. J. Sports Med. 2024, 52, 344–351. [Google Scholar] [CrossRef]
- Michaela, G.; Florian, P.; Michael, L.; Christian, B. Long-term outcome after high tibial osteotomy. Arch. Orthop. Trauma. Surg. 2008, 128, 111–115. [Google Scholar] [CrossRef]
- Martin, R.; Birmingham, T.B.; Willits, K.; Litchfield, R.; Lebel, M.E.; Giffin, J.R. Adverse event rates and classifications in medial opening wedge high tibial osteotomy. Am. J. Sports Med. 2014, 42, 1118–1126. [Google Scholar] [CrossRef]
- Miltenberg, B.; Puzzitiello, R.N.; Ruelos, V.C.B.; Masood, R.; Pagani, N.R.; Moverman, M.A.; Menendez, M.E.; Ryan, S.P.; Salzler, M.J.; Drager, J. Incidence of Complications and Revision Surgery After High Tibial Osteotomy: A Systematic Review. Am. J. Sports Med. 2024, 52, 258–268. [Google Scholar] [CrossRef] [PubMed]
- Griffin, T.; Rowden, N.; Morgan, D.; Atkinson, R.; Woodruff, P.; Maddern, G. Unicompartmental knee arthroplasty for the treatment of unicompartmental osteoarthritis: A systematic study. ANZ J. Surg. 2007, 77, 214–221. [Google Scholar] [CrossRef]
- Han, S.-B.; Kyung, H.-S.; Seo, I.-W.; Shin, Y.-S. Better clinical outcomes after unicompartmental knee arthroplasty when comparing with high tibial osteotomy. Medicine 2017, 96, e9268. [Google Scholar] [CrossRef] [PubMed]
- Ping, H.; Wen, J.; Liu, Y.; Li, H.; Wang, X.; Kong, X.; Chai, W. Unicompartmental knee arthroplasty is associated with lower pain levels but inferior range of motion, compared with high tibial osteotomy: A systematic overview of meta-analyses. J. Orthop. Surg. Res. 2022, 17, 425. [Google Scholar] [CrossRef]
- Belsey, J.; Yasen, S.K.; Jobson, S.; Faulkner, J.; Wilson, A.J. Return to Physical Activity After High Tibial Osteotomy or Unicompartmental Knee Arthroplasty: A Systematic Review and Pooling Data Analysis. Am. J. Sports Med. 2021, 49, 1372–1380. [Google Scholar] [CrossRef]
- Hoorntje, A.; Pronk, Y.; Brinkman, J.M.; van Geenen, R.C.I.; van Heerwaarden, R.J. High tibial osteotomy versus unicompartmental knee arthroplasty for Kellgren–Lawrence grade 3–4 knee osteoarthritis in younger patients: Comparable improvements in patient-reported outcomes, adjusted for osteoarthritis grade and sex. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4861–4870. [Google Scholar] [CrossRef] [PubMed]
- Santoso, M.B.; Wu, L. Unicompartmental knee arthroplasty, is it superior to high tibial osteotomy in treating unicompartmental osteoarthritis? A meta-analysis and systemic review. J. Orthop. Surg. Res. 2017, 12, 50. [Google Scholar] [CrossRef]
- Shanmugasundaram, S.; Kambhampati, S.B.S.; Saseendar, S. Proximal fibular osteotomy in the treatment of medial osteoarthritis of the knee—A narrative review of literature. Knee Surg. Relat. Res. 2019, 31, 16. [Google Scholar] [CrossRef]
- Qin, D.; Chen, W.; Wang, J.; Lv, H.; Ma, W.; Dong, T.; Zhang, Y. Mechanism and influencing factors of proximal fibular osteotomy for treatment of medial compartment knee osteoarthritis: A prospective study. J. Int. Med. Res. 2018, 46, 3114–3123. [Google Scholar] [CrossRef]
- Wang, X.; Wei, L.; Lv, Z.; Zhao, B.; Duan, Z.; Wu, W.; Zhang, B.; Wei, X. Proximal fibular osteotomy: A new surgery for pain relief and improvement of joint function in patients with knee osteoarthritis. J. Int. Med. Res. 2017, 45, 282–289. [Google Scholar] [CrossRef]
- Yang, Z.Y.; Chen, W.; Li, C.X.; Wang, J.; Shao, D.C.; Hou, Z.Y.; Gao, S.-J.; Wang, F.; Li, J.-D.; Hao, J.-D.; et al. Medial compartment decompression by fibular osteotomy to treat medial compartment knee osteoarthritis: A pilot study. Orthopedics 2015, 38, e1110–e1114. [Google Scholar] [CrossRef]
- Wu, Z.X.; Ren, W.X.; Wang, Z.Q. Proximal fibular osteotomy versus high tibial osteotomy for treating knee osteoarthritis: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2022, 17, 470. [Google Scholar] [CrossRef]
- Bayrak, H.C.; Adiguzel, I.F.; Demir, M.; Karagöz, B.; Ordu, S. Comparative outcomes of proximal fibular osteotomy versus high tibial osteotomy in patients with medial knee osteoarthritis: A retrospective analysis. Acta Orthop. Belg. 2024, 90, 629–638. [Google Scholar] [CrossRef]
- Gavrilovski, A.; Dimovska, A.G.; Spasov, M.; Kostov, H.; Igor, I.M.; Jonoski, K.; Trpeski, S. Alternative Treatment of Gonarthrosis: Proximal Fibular Osteotomy. Prilozi 2024, 45, 13–18. [Google Scholar] [CrossRef]
- Fu, D.; Li, G.; Chen, K.; Zhao, Y.; Hua, Y.; Cai, Z. Comparison of high tibial osteotomy and unicompartmental knee arthroplasty in the treatment of unicompartmental osteoarthritis: A meta-analysis. J. Arthroplast. 2013, 28, 759–765. [Google Scholar] [CrossRef]
- Huang, L.; Xu, Y.; Wei, L.; Yuan, G.; Chen, W.; Gao, S.; Liu, W.; Tan, Z.; Zhao, J. Unicompartmental knee arthroplasty is superior to high tibial osteotomy for the treatment of medial unicompartmental osteoarthritis: A systematic review and meta-analysis. Medicine 2022, 101, e29576. [Google Scholar] [CrossRef]
- Cao, Z.; Mai, X.; Wang, J.; Feng, E.; Huang, Y. Unicompartmental Knee Arthroplasty vs High Tibial Osteotomy for Knee Osteoarthritis: A Systematic Review and Meta-Analysis. J. Arthroplasty 2018, 33, 952–959. [Google Scholar] [CrossRef]
- Jiang, Y.; Li, J.; Zhang, L.; Jia, X.; Wang, T.; Zhao, X.; Chen, J.; Xu, K. Clinical efficacy and radiological changes of proximal fibular osteotomy for medial compartment knee osteoarthritis: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2025, 20, 672. [Google Scholar] [CrossRef]
- Sugianto, J.A.; Hadipranata, T.; Lazarus, G.; Amrullah, A.H. Proximal fibular osteotomy for the management of medial compartment knee osteoarthritis: A systematic review and meta-analysis. Knee 2021, 28, 169–185. [Google Scholar] [CrossRef]
- Brouwer, R.W.; Van Raaij, T.M.; Bierma-Zeinstra, S.M.A.; Verhagen, A.P.; Jakma, T.S.C.; Verhaar, J.A.N. Osteotomy for treating knee osteoarthritis. Cochrane Database Syst. Rev. 2014, 2014, CD004019. [Google Scholar] [CrossRef]
- Gandhi, R.; Ayeni, O.; Davey, J.R.; Mahomed, N.N. High tibial osteotomy compared with unicompartmental arthroplasty for the treatment of medial compartment osteoarthritis: A meta-analysis. Curr. Orthop. Pract. 2009, 20, 164–169. [Google Scholar] [CrossRef]
- Loia, M.C.; Vanni, S.; Rosso, F.; Bonasia, D.E.; Bruzzone, M.; Dettoni, F.; Rossi, R. High tibial osteotomy in varus knees: Indications and limits. Joints 2016, 4, 98–110. [Google Scholar] [CrossRef]
- Rodriguez-Merchan, E.C. Unicompartmental Knee Osteoarthritis (UKOA): Unicompartmental Knee Arthroplasty (UKA) or High. Tibial Osteotomy (HTO)? Arch. Bone Jt. Surg. 2016, 4, 307–313. [Google Scholar]
- Broughton, N.S.; Newman, J.H.; Baily, R.A.J. Unicompartmental replacement and high tibial osteotomy for osteoarthritis of the knee. A comparative study after 5-10 years’ follow-up. J. Bone Jt. Surg. Br. 1986, 68, 447–452. [Google Scholar] [CrossRef]
- Weale, A.E.; Newman, J.H. Unicompartmental arthroplasty and high tibial osteotomy for osteoarthrosis of the knee. A comparative study with a 12- to 17-year follow-up period. Clin. Orthop. Relat. Res. 1994, 302, 134–137. [Google Scholar]
- LaPrade, R.F.; Spiridonov, S.I.; Nystrom, L.M.; Jansson, K.S. Prospective Outcomes of Young and Middle-Aged Adults with Medial Compartment Osteoarthritis Treated with a Proximal Tibial Opening Wedge Osteotomy. Arthrosc. J. Arthrosc. Relat. Surg. 2012, 28, 354–364. [Google Scholar] [CrossRef]
- Coventry, M.B.; Ilstrup, D.M.; Wallrichs, S.L. Proximal tibial osteotomy. A critical long-term study of eighty-seven cases. J. Bone Jt. Surg. Am. 1993, 75, 196–201. [Google Scholar] [CrossRef]
- Naudie, D.; Bourne, R.B.; Rorabeck, C.H.; Bourne, T.J. The Install Award. Survivorship of the high tibial valgus osteotomy. A 10- to -22-year followup study. Clin. Orthop. Relat. Res. 1999, 367, 18–27. [Google Scholar] [CrossRef]
- Berman, A.T.; Bosacco, S.J.; Kirshner, S.; Avolio, A. Factors influencing long-term results in high tibial osteotomy. Clin. Orthop. Relat. Res. 1991, 272, 192–198. [Google Scholar] [CrossRef]
- Billings, A.; Scott, D.F.; Camargo, M.P.; Hofmann, A.A. High tibial osteotomy with a calibrated osteotomy guide, rigid internal fixation, and early motion. Long-term follow-up. J. Bone Jt. Surg. Am. 2000, 82, 70–79. [Google Scholar] [CrossRef]
- Bonasia, D.E.; Dettoni, F.; Sito, G.; Blonna, D.; Marmotti, A.; Bruzzone, M.; Castoldi, F.; Rossi, R. Medial opening wedge high tibial osteotomy for medial compartment overload/arthritis in the varus knee: Prognostic factors. Am. J. Sports Med. 2014, 42, 690–698. [Google Scholar] [CrossRef]
- Yapici, F.; Aykut, U.S.; Coskun, M.; Arslan, M.C.; Merder-Coskun, D.; Kocabiyik, A.; Ulu, E.; Bayhan, A.I.; Kaygusuz, M.A. Complications, Additional Surgery, and Joint Survival Analysis After Medial Open-Wedge High Tibial Osteotomy. Orthopedics 2020, 43, 303–314. [Google Scholar] [CrossRef]
- Noyes, F.R.; Goebel, S.X.; West, J. Opening wedge tibial osteotomy: The 3-triangle method to correct axial alignment and tibial slope. Am. J. Sports Med. 2005, 33, 378–387. [Google Scholar] [CrossRef]
- Pullen, W.M.; Slone, H.; Abrams, G.; Sherman, S.L. High Tibial Osteotomy in Knee Reconstruction and Joint Preservation. J. Am. Acad. Orthop. Surg. 2024, 32, 577–586. [Google Scholar] [CrossRef]
- Bae, D.K.; Song, S.J.; Kim, K.I.; Hur, D.; Jeong, H.Y. Mid-term survival analysis of closed wedge high tibial osteotomy: A comparative study of computer-assisted and conventional techniques. Knee 2016, 23, 283–288. [Google Scholar] [CrossRef]
- Cseg, T.A.; Gebhard, F.; Krettek, C.; Hüfner, T.; Grützner, P.A.; Stöckle, U.; Imhoff, A.B.; Lorenz, S.; Ljungqvist, J.; Keppler, P. Reliability of computer-assisted surgery as an intraoperative ruler in navigated high tibial osteotomy. Arch. Orthop. Trauma. Surg. 2011, 131, 297–302. [Google Scholar] [CrossRef]
- Choi, H.G.; Kim, J.S.; Jung, Y.S.; Yoo, H.J.; Lee, Y.S. Prediction and Development of Preventive Strategies for Lateral Hinge Fracture During Opening Wedge High Tibial Osteotomy Based on Osteotomy Configurations. Am. J. Sports Med. 2021, 49, 2942–2954. [Google Scholar] [CrossRef]
- Kozinn, S.C.; Scott, R. Current Unicondylar Concepts Knee Review Arthroplasty. J. Bone Jt. Surg. 1989, 71, 145–150. [Google Scholar] [CrossRef]
- Riff, A.J.; Sah, A.P.; Della Valle, C.J. Outcomes and Complications of Unicondylar Arthroplasty. Clin. Sports Med. 2014, 33, 149–160. [Google Scholar] [CrossRef]
- Yoo, J.D.; Huh, M.H.; Shin, Y.S. Risk of revision in UKA versus HTO: A nationwide propensity score-matched study. Arch. Orthop. Trauma Surg. 2023, 143, 3457–3469. [Google Scholar] [CrossRef]
- Serbin, P.A.; Do, D.H.; Hinkle, A.; Wukich, D.; Huo, M.; Sambandam, S. Comparative Analysis of Unicompartmental Total Knee Arthroplasty and High Tibial Osteotomy: Time to Total Knee Arthroplasty and Other Outcome Measures. Arthroplast. Today 2023, 20, 101107. [Google Scholar] [CrossRef]
- Debopadhaya, S.; Acosta, E.; Ortiz, D. Trends and outcomes in the surgical management of young adults with knee osteoarthritis using high tibial osteotomy and unicompartmental knee arthroplasty. Arch. Orthop. Trauma Surg. 2024, 144, 3995–4002. [Google Scholar] [CrossRef]
- Cody, J.P.; Pfefferle, K.J.; Ammeen, D.J.; Fricka, K.B. Is Outpatient Unicompartmental Knee Arthroplasty Safe to Perform at an Ambulatory Surgery Center? A Comparative Study of Early Post-Operative Complications. J. Arthroplast. 2018, 33, 673–676. [Google Scholar] [CrossRef]
- Kim, K.T.; Lee, S.; Lee, J.I.; Kim, J.W. Analysis and treatment of complications after unicompartmental knee arthroplasty. Knee Surg. Relat. Res. 2016, 28, 46–54. [Google Scholar] [CrossRef]
- Ji, J.H.; Park, S.E.; Song, I.S.; Kang, H.; Ha, J.Y.; Jeong, J.J. Complications of medial unicompartmental knee arthroplasty. Clin. Orthop. Surg. 2014, 6, 365–372. [Google Scholar] [CrossRef]
- Song, M.H.; Kim, B.H.; Ahn, S.J.; Yoo, S.H.; Lee, M.S. Early Complications After Minimally Invasive Mobile-Bearing Medial Unicompartmental Knee Arthroplasty. J. Arthroplast. 2009, 24, 1281–1284. [Google Scholar] [CrossRef]
- Ko, Y.-B.; Gujarathi, M.R.; Oh, K.-J. Outcome of Unicompartmental Knee Arthroplasty: A Systematic Review of Comparative Studies between Fixed and Mobile Bearings Focusing on Complications. Knee Surg. Relat. Res. 2015, 27, 141–148. [Google Scholar] [CrossRef]
- Morris, M.J.; Molli, R.G.; Berend, K.R.; Lombardi, A.V. Mortality and perioperative complications after unicompartmental knee arthroplasty. Knee 2013, 20, 218–220. [Google Scholar] [CrossRef]
- Ode, Q.; Gaillard, R.; Batailler, C.; Herry, Y.; Neyret, P.; Servien, E.; Lustig, S. Fewer complications after UKA than TKA in patients over 85 years of age: A case-control study. Orthop. Traumatol. Surg. Res. 2018, 104, 955–959. [Google Scholar] [CrossRef]
- Unal, O.K.; Dagtas, M.Z.; Demir, C.; Najafov, T.; Ugutmen, E. The Effects of Proximal Fibular Osteotomy on the Knee and Ankle Joints: A Finite Element Analysis. Acta Chir. Orthop. Traumatol. Cech. 2021, 88, 313–320. [Google Scholar] [CrossRef]
- Kang, Y.; Kim, J.; Sim, J.A.; Moon, M.; Park, J.C.; Cho, S.H.; Lee, B.H. Stress Effect in the Knee Joint Based on the Fibular Osteotomy Level and Varus Deformity: A Finite Element Analysis Study. Bioengineering 2023, 10, 1003. [Google Scholar] [CrossRef]
- Wang, T.-R.; Wang, H.-D.; Chen, W.; Yu, T.-B.; Qin, Y.; Zhang, Y.-Z. Proximal fibular osteotomy alleviates medial compartment knee osteoarthritis in a mouse model. Int. Orthop. 2020, 44, 1107–1113. [Google Scholar] [CrossRef]
- Aydın, A.; Baydar, M.; Ünkar, E.A.; Erbaş, A.; Üçpunar, H.; Yapıcı, F.; Gür, V.; Öztürk, K. Evaluation of the effect of vascularized fibula graft harvesting on coronal plane alignment and functional outcomes of the lower limb. Sci. Rep. 2024, 14, 15820. [Google Scholar] [CrossRef]
- Vaish, A.; Kumar Kathiriya, Y.; Vaishya, R. A Critical Review of Proximal Fibular Osteotomy for Knee Osteoarthritis. Arch. Bone Jt. Surg. 2019, 7, 453–462. [Google Scholar]
- Liang, Z.J.; Koh, D.T.S.; Soong, J.; Lee, K.H.; Bin Abd Razak, H.R. Severity of knee osteoarthritis does not affect clinical outcomes following proximal fibular osteotomy – A systematic review and pooled analysis. J. Clin. Orthop. Trauma 2024, 54, 102473. [Google Scholar] [CrossRef]
- Narang, A.; Shekhawat, M.S.; Singh, A. Functional and Radiological Outcome of Medial Compartment Osteoarthritis of the Knee Treated Byproximal Fibular Osteotomy. Int. J. Med. Biomed. Stud. 2022, 6, 58–61. [Google Scholar] [CrossRef]
- Utomo, D.N.; Mahyudin, F.; Wijaya, A.M.; Widhiyanto, L. Proximal fibula osteotomy as an alternative to TKA and HTO in late-stage varus type of knee osteoarthritis. J. Orthop. 2018, 15, 858–861. [Google Scholar] [CrossRef]
- Huda, N.; Islam, M.S.U.; Kumar, H.; Pant, A.; Bishnoi, S. Proximal Fibular Osteotomy for Medial Compartment Knee Osteoarthritis: Is. It Worth? Indian. J. Orthop. 2020, 54, 47–51. [Google Scholar] [CrossRef]
- Khalil, T.; Nassar, W.; Sakr, H.; Zakaria, Z.; El Seddawy, A.; Morsy, A. Proxımal Fıbular Osteotomy Versus Medıal Openıng Wedge Hıgh Tıbıal Osteotomy to Treat Medıal Compartment Knee Osteoarthrıtıs: A Randomızed Clınıcal Trıal. Ain Shams Med. J. 2021, 72, 217–226. [Google Scholar] [CrossRef]
- Vashisht, A.; Menwal, G.; Bhatnagar, R. A clinico-radiological evaluation of functional outcome of proximal fibular osteotomy for medial compartment knee osteoarthritis: A new emerging technique. Int. J. Res. Orthop. 2020, 6, 515. [Google Scholar] [CrossRef]
- Subash, Y.; Naidu, G.K. The role of proximal fibular osteotomy in the management of medial compartment osteoarthritis of the knee. Int. J. Orthop. Sci. 2018, 4, 369–372. [Google Scholar] [CrossRef]
- Reddy, V.; Raghav, T.S.; Panapana, S.R.; Burma, S.M.; Koduru, S.K. Proximal fibular osteotomy for medial compartment osteoarthrosis of knee. Indian J. Orthop. Surg. 2020, 5, 263–266. [Google Scholar] [CrossRef]
- Yadav, R.; Patkar, D.; Gaur, S. A Nobel procedure for symptomatic pain relief in medial compartment knee osteoarthritis in countries of low socioeconomic status. Int. J. Orthop. Sci. 2020, 6, 541–545. [Google Scholar] [CrossRef]
- Bansal, M. Proximal fibular osteotomy for medical compartment OA knee. Int. J. Orthop. Traumatol. Surg. Sci. 2020, 6, 46–50. [Google Scholar] [CrossRef]
- Gupta, A.; Bhat, B.; Singh, A. Assessment of functional outcomes of Proximal Fibular Osteotomy in Osteoarthritis Knee. J. Adv. Med. Dent. Sci. Res. 2020, 2, 84–86. [Google Scholar] [CrossRef]
- Zuber, M.; Yadav, R.; Gaur, S. Proximal fibular osteotomy with Arthroscopic debridement for symptomatic pain relief in medial compartment knee osteoarthritis. Int. J. Orthop. Sci. 2020, 6, 291–295. [Google Scholar] [CrossRef]
- Elsebaiy, A.; Safwat, H.; Abdel, A.; Ashiry, R. Early Results of Fibular Osteotomy for Treatment of Medial Compartment Osteoarthritis. Egypt. J. Hosp. Med. 2019, 76, 4588–4590. [Google Scholar] [CrossRef]
- Bhushan, A.; Goel, R.; Aloria, J.K. A study on assessment of proximal fibular osteotomy as a treatment of medial compartment knee osteoarthritis. Int. J. Orthop. Sci. 2022, 8, 392–395. [Google Scholar] [CrossRef]
- Monreal, R.; Osinaga, G. Proximal Fibular Osteotomy (PFO) for Medial Compartment Osteoarthritis of Knee with Varus Deformity-Preliminary Report Orthopedics and Rheumatology. Ortho Rheum. Open Access J. 2022, 20, 556027. [Google Scholar]
- Hüttner, F.; Schuster, P.; Ferner, F.; Harrer, J. Fibularesektion bei Varusgonarthrose—Hot oder Schrott? Knie J. 2024, 6, 107–109. [Google Scholar] [CrossRef]
- Łuczkiewicz, P.; Daszkiewicz, K.; Dzierżanowski, J.; Witkowski, W. Proximal fibular osteotomy as a treatment for degenerative meniscal extrusion. Med. Hypotheses 2023, 178, 111119. [Google Scholar] [CrossRef]
- Demirkiran, N.; Husemoglu, R. Finite Element Analysis of Unicondylar Knee Arthroplasty Combined with Proximal Fibular Osteotomy. J. Med. Innov. Technol. 2020, 2, 121–126. [Google Scholar]
- Zhang, B.; Qian, H.; Wu, H.; Yang, X. Unicompartmental knee arthroplasty versus high tibial osteotomy for medial knee osteoarthritis: A systematic review and meta-analysis. J. Orthop. Surg. 2023, 31, 10225536231162829. [Google Scholar] [CrossRef]
- Spahn, G.; Hofmann, G.O.; von Engelhardt, L.V.; Li, M.; Neubauer, H.; Klinger, H.M. The impact of a high tibial valgus osteotomy and unicondylar medial arthroplasty on the treatment for knee osteoarthritis: A meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 96–112. [Google Scholar] [CrossRef] [PubMed]
- Stukenborg-Colsman, C.; Wirth, C.J.; Lazovic, D.; Wefer, A. High tibial osteotomy versus unicompartmental joint replacement in unicompartmental knee joint osteoarthritis: 7-10-Year follow-up prospective randomised study. Knee 2001, 8, 187–194. [Google Scholar] [CrossRef]
- Petersen, W.; Metzlaff, S. Open wedge high tibial osteotomy (HTO) versus mobile bearing unicondylar medial joint replacement: Five years results. Arch. Orthop. Trauma. Surg. 2016, 136, 983–989. [Google Scholar] [CrossRef]
- Gultac, E.; Can, F.İ.; Aydoğan, N.H. Proximal partial fibular resection versus high tibial osteotomy: Comparative outcomes in early-stage knee osteoarthritis. Jt. Dis. Relat. Surg. 2025, 36, 266–271. [Google Scholar] [CrossRef]
- Ashraf, M.; Purudappa, P.P.; Sakthivelnathan, V.; Sambandam, S.; Mounsamy, V. Proximal fibular osteotomy: Systematic review on its outcomes. World J. Orthop. 2020, 11, 499–506. [Google Scholar] [CrossRef] [PubMed]
- Feeley, B.T.; Gallo, R.A.; Sherman, S.; Williams, R.J. Management of osteoarthritis of the knee in the active patient. J. Am. Acad. Orthop. Surg. 2010, 18, 406–416. [Google Scholar] [CrossRef]
- Dettoni, F.; Bonasia, D.E.; Castoldi, F.; Bruzzone, M.; Blonna, D.; Rossi, R. High tibial osteotomy versus unicompartmental knee arthroplasty for medial compartment arthrosis of the knee: A review of the literature. Iowa Orthop. J. 2010, 30, 131–140. [Google Scholar]
- Brown, G.A.; Amendola, A. Radiographic Evaluation and Preoperative Planning for High Tibial Osteotomies. Oper. Tech. Sports Med. 2012, 20, 93–102. [Google Scholar] [CrossRef]
- Noyes, F.R.; Mayfield, W.; Barber-Westin, S.D.; Albright, J.C.; Heckmann, T.P. Opening wedge high tibial osteotomy: An operative technique and rehabilitation program to decrease complications and promote early union and function. Am. J. Sports Med. 2006, 34, 1262–1273. [Google Scholar] [CrossRef]
- Yoon, T.H.; Choi, C.H.; Kim, S.J.; Kim, S.H.; Kim, N.H.; Jung, M. Effect of Medial Open-Wedge High Tibial Osteotomy on the Patellofemoral Joint According to Postoperative Realignment. Am. J. Sports Med. 2019, 47, 1863–1873. [Google Scholar] [CrossRef]
- Park, J.G.; Han, S.B.; Jang, K.M.; Shin, S.M. Differential effects of tibia varus deformity on clinical outcomes following high tibial osteotomy and unicompartmental knee arthroplasty for moderate medial compartment osteoarthritis with moderate varus alignment. Arch. Orthop. Trauma Surg. 2025, 145, 10225536231162829. [Google Scholar] [CrossRef]
- Giffin, J.R.; Stabile, K.J.; Zantop, T.; Vogrin, T.M.; Woo, S.L.Y.; Harner, C.D. Importance of tibial slope for stability of the posterior cruciate ligament-deficient knee. Am. J. Sports Med. 2007, 35, 1443–1449. [Google Scholar] [CrossRef]
- Mancuso, F.; Hamilton, T.W.; Kumar, V.; Murray, D.W.; Pandit, H. Clinical outcome after UKA and HTO in ACL deficiency: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 112–122. [Google Scholar] [CrossRef] [PubMed]
- Noyes, F.R.; Barber-Westin, S.D.; Hewett, T.E. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am. J. Sports Med. 2000, 28, 282–296. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.M.; Crockett, H.C.; Slawski, D.P.; Madsen, M.W.; Windsor, R.E. High tibial osteotomy. J. Am. Acad. Orthop. Surg. 2005, 13, 279–289. [Google Scholar] [CrossRef] [PubMed]
- Coventry, M.B. Osteotomy about the knee for degenerative and rheumatoid arthritis. J. Bone Joint Surg. Am. 1973, 55, 23–48. [Google Scholar] [CrossRef]
- Bae, D.K.; Song, S.J.; Yoon, K.H. Closed-wedge high tibial osteotomy using computer-assisted surgery compared to the conventional technique. J. Bone Joint Surg. Br. 2009, 91, 1164–1171. [Google Scholar] [CrossRef] [PubMed]
- Vince, K.G.; Cyran, L.T. Unicompartmental knee arthroplasty: New indications, more complications? J. Arthroplast. 2004, 19, 9–16. [Google Scholar] [CrossRef]
- Screpis, D.; Piovan, G.; Baldini, M.; Amarossi, A.; Natali, S.; Iacono, V.; Gigante, A.; Zorzi, C. Higher activity level after opening wedge high tibial osteotomy compared to medial unicompartimental knee arthroplasty in a selected cohort of advanced age: A propensity score-matched analysis. Knee 2023, 40, 183–191. [Google Scholar] [CrossRef]
- Koh, I.J.; Kim, M.S.; Sohn, S.; Song, K.Y.; Choi, N.Y.; Jung, H.; In, Y. Predictive factors for satisfaction after contemporary unicompartmental knee arthroplasty and high tibial osteotomy in isolated medial femorotibial osteoarthritis. Orthop. Traumatol. Surg. Res. 2019, 105, 77–83. [Google Scholar] [CrossRef]
- Nagel, A.; Insall, J.; Scuderi, G. Proximal tibial osteotomy: A subjective outcome study. J. Bone Jt. Surg. 1996, 78, 1353–1358. [Google Scholar] [CrossRef]
- Li, P.; Qiao, Y.; Zhou, Y.; Li, J.; Lin, Z.; Cao, Y.; Tan, F.; Zeng, J.; Song, X.; Liu, P.; et al. Comparative outcomes of revision total knee arthroplasty: A systematic review and meta-Analysis of high tibial osteotomy vs. unicompartmental knee arthroplasty. BMC Musculoskelet. Disord. 2025, 26, 780. [Google Scholar] [CrossRef]
- Nwachukwu, B.U.; McCormick, F.M.; Schairer, W.W.; Frank, R.M.; Provencher, M.T.; Roche, M.W. Unicompartmental Knee Arthroplasty Versus High Tibial Osteotomy: United States Practice Patterns for the Surgical Treatment of Unicompartmental Arthritis. J. Arthroplast. 2014, 29, 1586–1589. [Google Scholar] [CrossRef]
- Coventry, M.B. Current Concepts Review: Upper Tibial Osteotomy for Osteoarthritis. J. Bone Jt. Surg. 1985, 67-A, 1136–1140. [Google Scholar] [CrossRef]
- Mattei, L.; Lea, S.; Nicolaci, G.; Ferrero, G.; Marmotti, A.; Castoldi, F. Closing wedge tibial osteotomy: Is it an actual procedure nowadays? Ann. Jt. 2017, 2, 30. [Google Scholar] [CrossRef]
- Trieb, K.; Grohs, J.; Hanslik-Schnabel, B.; Stulnig, T.; Panotopoulos, J.; Wanivenhaus, A. Age predicts outcome of high-tibial osteotomy. Knee Surgery, Sports Traumatology, Arthroscopy 2006, 14, 149–152. [Google Scholar] [CrossRef]
- Irismetov, M.E.; Fozilov, K.T.; Khakimov, S.K.; Safarov, N.B. Associated applicance of artroscopic debridement and proximal fibular osteotomy at the treatment of patients with deformic artritis of knee. Genij Ortop. 2022, 28, 768–773. [Google Scholar] [CrossRef]
- Karapınar, S.E.; Bayindir, A.; Dinçer, R.; Atay, T.; Baykal, Y.B.; Kırdemir, V.; Baydar, M.L. The middle-term results of proximal fibular osteotomy and percutaneous drilling in the treatment of gonarthrosis. J. Exp. Clin. Med. 2025, 42, 296–302. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yapıcı, F. High Tibial Osteotomy (HTO), Unicompartmental Knee Arthroplasty (UKA), and Proximal Fibular Osteotomy (PFO) for Medial-Compartment Knee Osteoarthritis: A Narrative Review of Comparative Mechanisms, Clinical Outcomes, and Decision-Making. J. Clin. Med. 2025, 14, 7882. https://doi.org/10.3390/jcm14217882
Yapıcı F. High Tibial Osteotomy (HTO), Unicompartmental Knee Arthroplasty (UKA), and Proximal Fibular Osteotomy (PFO) for Medial-Compartment Knee Osteoarthritis: A Narrative Review of Comparative Mechanisms, Clinical Outcomes, and Decision-Making. Journal of Clinical Medicine. 2025; 14(21):7882. https://doi.org/10.3390/jcm14217882
Chicago/Turabian StyleYapıcı, Furkan. 2025. "High Tibial Osteotomy (HTO), Unicompartmental Knee Arthroplasty (UKA), and Proximal Fibular Osteotomy (PFO) for Medial-Compartment Knee Osteoarthritis: A Narrative Review of Comparative Mechanisms, Clinical Outcomes, and Decision-Making" Journal of Clinical Medicine 14, no. 21: 7882. https://doi.org/10.3390/jcm14217882
APA StyleYapıcı, F. (2025). High Tibial Osteotomy (HTO), Unicompartmental Knee Arthroplasty (UKA), and Proximal Fibular Osteotomy (PFO) for Medial-Compartment Knee Osteoarthritis: A Narrative Review of Comparative Mechanisms, Clinical Outcomes, and Decision-Making. Journal of Clinical Medicine, 14(21), 7882. https://doi.org/10.3390/jcm14217882





