Abstract
Background/Objectives: Children’s unique physiological and behavioral needs require individualized treatment planning. It seems reasonable to investigate treatment options for recurrent temporomandibular joint (TMJ) dislocation and assess their outcomes. This review was conducted with the purpose of identifying recent therapeutic approaches for TMJ dislocation in pediatric patients and evaluating their effectiveness. Methods: Searches were conducted on 21 September 2025, using BASE, PubMed, and Scopus. The review included studies with measurable outcomes, published between 2000 and 2025, that focused on patients under the age of 18 with recurrent TMJ dislocation. Studies with unclear diagnoses or undefined treatment methods were excluded. Risk of bias was evaluated using the Joanna Briggs Institute’s critical appraisal tool. The results were tabulated. Results: Based on the inclusion criteria, nine studies were included: one case-control study, three case series, and five case reports. Invasive treatment methods applied in pediatric patients were reported in two of those. Minimally invasive and conservative treatment methods were most frequently described, with botulinum toxin injections being the most commonly reported minimally invasive approach. Conclusions: Research revealed that conservative and minimally invasive methods are preferred in pediatric patients’ treatment. Due to the heterogeneity and limited number of available literature, consistent conclusions regarding the effectiveness of different treatment methods for recurrent TMJ dislocation in children could not be drawn. This study received no funding. PROSPERO ID number: CRD420251139493.
1. Introduction
1.1. Background
The temporomandibular joint (TMJ) is a synovial joint formed by the mandible, temporal bone, and articular disc. The articular head is situated on the condylar process of the mandible, while the temporal bone contains the socket of the joint formed by the glenoid fossa [1,2,3]. The articular disc divides the joint cavity into upper and lower compartments, both lined with fibrocartilage. A fibrocartilage coating plays an essential role in maintaining the durability of a joint [2,4,5]. Joint movements are enabled by muscles, supported by ligaments, and limited by the cranial anatomy [2,6].
During jaw opening, rotational movement is followed by inferior and anterior sliding of the head of the mandible, towards the articular eminence, eventually positioning itself over its top. This motion is facilitated by the activity of the suprahyoid muscles, along with the lateral pterygoid muscle [7,8]. Closure and retraction are executed by the masseter and temporalis. Protrusion is achieved by the synergistic action of medial and lateral pterygoid muscles [7,8,9].
Proper motor function of the temporomandibular joint relies on the precise coordination of all components within its highly complex structure; consequently, any even minor anatomical or neuromuscular disturbances can predispose to TMJ dysfunction. Dislocation of the TMJ, most often, is a result of wide mouth opening, such as during yawning or because of prolonged mouth opening during dental procedures, whereby the mandibular condyle moves beyond the glenoid fossa, becomes trapped, and cannot return to its original position without professional help [10,11,12,13]. The mandible can dislocate posteriorly, laterally, medially, or anteriorly, with anterior dislocation being the most common [12]. A distinction is made between acute, chronic, and recurrent luxation, and also between bilateral and unilateral luxation [12,13,14].
Various predisposing factors have been linked to spontaneous TMJ dislocation that may be associated with excessively flexible ligaments, anatomical irregularities, intense muscle activity, underlying neuromuscular dysfunction, connective tissue disorders, and some medications [11,13,14,15,16].
Emergency mandibular dislocation is usually addressed by manual repositioning of the condyle, using either a posterior or anterior approach [11,13,14,16]. However, this is a temporary solution. Patients with recurrent dislocations should be treated preventively [14,16].
Conservative treatment methods for TMJ dislocation include the use of jaw exercises, acrylic blocks, impression compound spacers, intermaxillary fixation (IMF), injection of botulinum toxin, sclerosing or prolotherapy, and occlusal splints [13,14,16,17,18]. Often, several forms of treatment are used simultaneously in therapy. For example, after applying a posterior acrylic bite block combined with the use of elastic traction, exercises will be recommended [17]. IMF, achieved by wiring the patient’s teeth, limits dislocation by ensuring immobilization. Thus, this method cannot be used in children without erupted teeth or in edentulous patients [19,20]. Botulinum toxin administered to the lateral pterygoid muscle inhibits the release of acetylcholine from the presynaptic membrane, weakening muscle contraction [6,21]. Prolotherapy is a technique involving the injection of irritants into a joint to provoke cell proliferation, with the aim of enhancing the mechanical stability of the surrounding ligaments [6,21].
Surgical methods involve approaches such as increasing the height of the eminence (e.g., Dautrey’s procedure), soft tissue surgery to restrict condylar movement, and eminectomy [16,22,23].
1.2. Rationale
In young children, the condylar process of the mandible has a rounded shape, and the glenoid fossa is flatter [24,25,26]. As they grow, the condylar process becomes longer and tilts forward, while the glenoid fossa increases in depth [25,26]. Such changes progress gradually throughout development as a result of mechanical forces generated by jaw movements [27,28].
Treating children can be challenging for doctors, as it requires adaptation to their stage of development. Effective treatment can also be impeded by a lack of cooperation from young patients. Children require a specific approach and a lot of patience. Still, performing certain procedures while keeping the child conscious may prove impossible.
1.3. Objectives
The primary objective of the study was to identify the main treatment approaches applied in patients under 18 years of age with recurrent temporomandibular joint dislocation, by comparing conservative, minimally invasive and invasive treatment methods and to determine the potential advantages associated with each approach.
2. Materials and Methods
This systematic review has been developed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) methodology and registered in PROSPERO under the number CRD420251139493 [29]. The checklists for the report and abstract can be found in Supplementary Documents S1 and S2, respectively.
2.1. Eligibility Criteria
The eligibility criteria were established based on the PICOS methodology (Table 1). This review includes publications on patients under 18 years old and those including both children and adults with recurrent TMJ dislocation. However, studies in which TMJ dislocation was treated as part of broader therapy, as well as cadaver and animal studies, were excluded. All treatment methods outlined in research were included if performed during treatment and properly documented. Studies in which the level of evidence could not be determined, along with preprints and conference proceedings, were excluded. Then articles published within the current quarter-century (2000–2025) were selected for full-text screening. For the article to be included in the study, it must contain at least one of the following measures: dislocation frequency (pre-/post-treatment), acoustic symptoms (pre-/post-treatment), mandibular opening path (pre-/post-treatment), pain intensity (pre-/post-treatment) or range of abduction (pre-/post-treatment).

Table 1.
Eligibility criteria.
2.2. Search Strategy
The initial literature searches were undertaken using Bielefeld Academic Search Engine (BASE), PubMed and Scopus. The search was conducted on 21 September 2025. Search queries were formulated based on the eligibility criteria (Table 1), and after adjusting and refining, the final queries presented in Table A1 were used.
2.3. Selection and Data Processing
According to the PICOS criteria, research selection was performed using the Rayyan platform [22]. Duplicated articles were excluded, and the screening of abstracts began.
In the first stage, two authors (K.C. and A.H.) independently assessed the titles and abstracts, selecting articles that met the eligibility criteria for inclusion in the full text assessment. All articles for which discrepancy occurred were included for full-text review. The same authors conducted a full-text assessment. Discrepancies identified at this stage were first addressed through discussion between the two assessing researchers; if consensus could not be achieved, the final decision was made by the third author.
Using a standard form developed in Google Sheets, part of the Google Workspace suite (2025 version, Google LLC, Mountain View, CA, USA), the following data were extracted from the included studies: (1) first author and publication year, (2) type of intervention, (3) patient characteristic (age, sex), (4) dislocation frequency before treatment, (5) dislocation frequency after treatment, (6) acoustic symptoms before treatment, (7) acoustic symptoms after treatment, (8) mandibular opening path before treatment, (9) mandibular opening path after treatment, (10) pain intensity before treatment, (11) pain intensity after treatment, (12) range of abduction before treatment, and (13) range of abduction after treatment. The collected data were organized into tables.
2.4. Study Risk of Bias Assessment
The risk of bias was evaluated using the Joanna Briggs Institute’s critical appraisal tool, which is designed to assess the quality of various research studies, with separate checklists tailored to different study designs [30]. Thus, the JBI checklists for case–control studies, case reports and case series were used, depending on the study type. This assessment was conducted independently by two reviewers, A.H. and M.C. The (1) percentage agreement, (2) Cohen’s kappa, (3) PABAK, (4) AC1 Gweta were calculated to measure the inter-reviewer agreement. Any discrepancies between the reviewers were resolved through discussion until consensus was reached.
2.5. Qualification of Reports
Based on the Oxford Centre of Evidence-Based Medicine 2011 Levels of Evidence scale, the authors assessed the level of evidence for each study. Due to the very limited number of high-quality articles, studies were included regardless of their level of evidence, as long as evaluation was possible.
3. Results
In total, 268 articles were identified through the search: 102 via BASE, 96 from PubMed, and 70 from Scopus. After removing duplicates, 168 records remained for screening, out of which 34 qualified for full-text evaluation. Unfortunately, despite efforts, access to the full text of one article could not be obtained [31]. Ultimately, after excluding 24 reports (Table A2), nine studies were included for the synthesis (Figure 1).
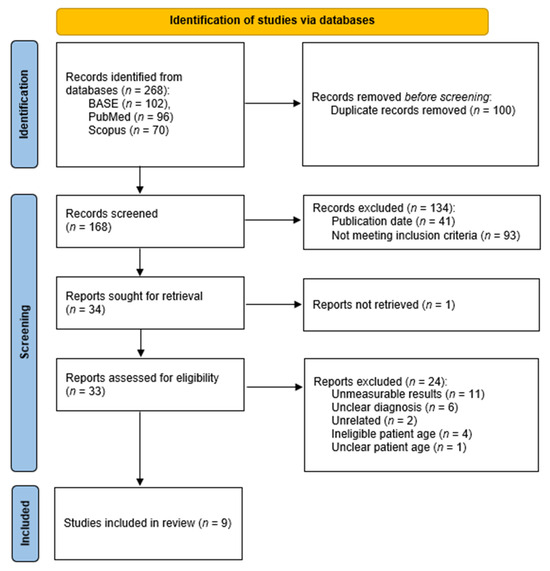
Figure 1.
PRISMA flow diagram.
This study includes 5 case reports, 3 case series, and 1 case–control study. An assessments of level of evidence, along with the methods performed in each study, is presented in Table 2.

Table 2.
Included studies.
Table 3 presents the dislocation frequency before and after treatment as reported in all included studies, along with demographic data such as age and sex. The remaining extracted data, which could be classified under one of the considered measures, are presented in Table 4. Data from two patients across two different studies were excluded: in one case [33], the patient’s data were not classified into one of the measures, and in the other [38], the patient belonged to the control group. Since the mandibular opening path, initially planned as an assessment measure, was not examined in any of the analyzed studies, it was removed from the final data organization.

Table 3.
Research results across groups of pediatric patients and results regarding dislocation frequency before and after treatment.

Table 4.
Research results in groups of pediatric patients, remaining outcome measures.
Risk of Bias in Studies
The detailed risk of bias assessment for each study is summarized in Table A3, Table A4 and Table A5. The study by Triantafillidou et al. demonstrates a low risk of bias, as all criteria from the critical appraisal tool were met [38]. The case series by Coser et al., Yoshida et al., and Gadre et al. present a moderate overall risk of bias [34,36,39]. Although each of these studies fulfilled the majority of the criteria, they consistently lacked appropriate statistical analysis. Additionally, issues related to unclear reporting of participant inclusion and, in some cases, measurement reliability, may further affect the validity and generalizability of their findings. The case reports were assessed as having varying levels of risk of bias [32,33,35,37,40]. Only the report by Stark et al. met all the appraisal criteria, indicating a low risk of bias [37]. The remaining case reports were assessed as having a moderate risk of bias due to incomplete reporting in key areas [32,33,35,40]. The agreement between the two authors independently assessing the risk of bias was high, with approximately 78% overlap in responses. Despite this, Cohen’s kappa coefficient was relatively low (≈0.10). This discrepancy can be explained by the fact that both reviewers frequently selected the “Yes” option, which artificially inflated the expected chance agreement. Therefore, the low kappa value in this case does not indicate substantial discrepancies in the assessment of bias risk, but rather reflects an uneven distribution of responses across the options (“Yes”, “No”, “Unclear”). For comparison, alternative indicators of agreement were calculated, demonstrating moderate to high concordance between the reviewers (PABAK = 0.56; AC1 Gweta = 0.71).
4. Discussion
TMJ dislocations are a part of TMJ disorders (TMDs), a collective term that also includes conditions such as arthralgia, degenerative joint disease, osteoarthritis, and other pathologies associated with TMJ dysfunctions [41]. The latest research showed that TMDs may affect even 31% of adults and 11% of children [42]. Furthermore, Zielinski et al. estimate that by 2050, this prevalence could increase to 44% of the global population and 37% of the European population [43]. Despite this, the available data concerning the incidence of TMJ dislocations in children, particularly recurrent dislocations, is notably limited and primarily derived from case reports. Mandibular dislocations are reported slightly more frequently in women and tend to occur most commonly in the fourth and fifth decades of life. According to Papoutsis et al., the majority of TMJ dislocations are recurrent (62.5%) [44]. Similar results were reported by Tarhio et al. (61.9%) [14].
Current research shows that there is no single factor responsible for TMDs, as their etiology is multifactorial [41]. In addition to the anatomical variations in bone structure observed in pediatric patients, such as a flatter glenoid fossa, various other conditions may predispose to TMJ dislocation, including connective tissue disorders like Ehlers-Danlos Syndrome, which are associated with structural defects in collagen and elastin leads to loss of stability and ligament support [45,46]. Additionally, neuromuscular diseases, such as muscular dystrophies, due to myotonia and weakness of masticatory muscles, result in impaired mandibular movements, thereby increasing the load on the temporomandibular joint, as well as neurological disorders that result in seizures or involuntary movements, can further increase the risk [47,48]. Chronic steroid therapy is another contributing factor, as it may lead to muscle and ligament weakening, thereby promoting the occurrence of recurrent dislocations [49,50]. Another condition that may prove crucial in TMD development is joint hypermobility, a prevalent condition in childhood, affecting between 8% to 39% of school-aged individuals [51]. The benign form most commonly affects individuals between the ages of 3 and 10, with its prevalence diminishing as children age [52]. Notably, hypermobile joints are more vulnerable to mechanical stress and may experience excessive wear over time. Furthermore, patients with joint hypermobility are more likely to develop TMDs in later stages of life [53].
It is worth noting that in children, the majority of TMJ dislocations are associated with trauma [14]. Therefore, recurrent TMJ dislocations in pediatric patients are especially rare. Regardless of age, TMJ dislocations occurring repeatedly during daily activities should be managed starting with the identification and elimination of underlying causes, where feasible. Then, the most appropriate therapeutic strategy should be selected from available methods.
The results of our research highlighted that among pediatric patients with recurrent TMJ dislocation, conservative and minimally invasive treatment methods are most commonly applied. However, the results of such treatment were not documented reliably enough to confirm or deny their effectiveness. Considering the low risk associated with this approach, such methods should be considered as first-line treatment options. Particularly considering the nature of treating pediatric patients, it seems reasonable to avoid needle-based interventions, thereby supporting the preference for conservative treatment methods. Notably, several reports indicated that successful recovery often requires the involvement of various specialists, including psychologists, neurologists, and others. This multidisciplinary approach results from the multifactorial nature of TMJ dislocation and the incomplete understanding of the pathophysiological mechanisms that contribute to its development.
It is worth noting that lack of cooperation and significant distress in pediatric patients can be managed with the administration of nitrous oxide or various forms of sedation (e.g., propofol-induced). Patient discomfort can be alleviated with local anesthesia. Additionally, these medications may be beneficial in cases of unsuccessful jaw repositioning maneuvers, as increased tension of the masticatory muscles impedes completion of the procedure. The use of nitrous oxide prior to the repositioning maneuver was reported by Mohan et al. and Sicard et al., and prior to the botulinum toxin injections by Stark et al. [32,33,37]. Light intravenous sedation before manual reduction was described by French et al., while propofol sedation was reported by Sicard et al. [33,35]. Coser et al. and Stark et al. described injections of local anaesthetic administered before arthrocentesis and prior to carrying out the repositioning maneuver, respectively [36,37]. As the research revealed, sedation alone may in some cases be sufficient, Sicard et al. reported spontaneous reduction, which occurred under propofol-induced sedation [33].
Botulinum toxin injections were the most commonly reported minimally invasive method, with autologous blood injections reported nearly as frequent. Botulinum toxin type A, which is produced by the gram-positive bacterium Clostridium botulinum, exerts a paralytic effect by rapidly binding to presynaptic cholinergic nerve terminals [34]. Typically, injecting into the lateral pterygoid muscle reduces excessive muscular activity, contributing to recurrent dislocation [54]. Autologous blood injections stimulate a localized inflammatory response, contributing to enhanced joint stability and the promotion of fibrosis. Clinical follow-up assessments of patients who have undergone this treatment demonstrate no radiographic or functional evidence of ankylosis [6,55]. Conservative treatment is commonly adopted for children with TMJ dislocation due to its less invasive nature and better psychological tolerance, while ensuring ongoing craniofacial growth is not compromised.
It should also be emphasized that the available literature lacks sufficient long-term evidence to support the choice of surgical interventions in children. There are several important considerations regarding children that make this approach more complex and potentially controversial, which include ongoing growth, joint physiology, and potential complications like joint ankylosis [56]. Immobilization can impair normal growth, reduce the flow of synovial fluid, and impede nutrient exchange. Therefore, early mobilization and physiotherapy are advocated for successful treatment [57,58]. Invasive treatment methods were reported only in two of the included studies [35,39]. Nevertheless, in both cases, surgical procedures were chosen as a last resort and resulted in successful outcomes. Thus, high-quality, reliable further research using valid and comparable measures should be prioritized in the future.
Considering all of the limitations, due to the lack of comparable reviews available in recent years, it is not feasible to draw comparisons with existing literature. The level of evidence of included studies is generally low, with only four publications rated above level 5, introducing a high risk of bias. Over the past quarter-century, only nine articles on this topic have been found, highlighting an unsatisfactory level of scientific attention. As the review revealed a lack of sufficient literature, it seems reasonable to recommend conducting thorough studies of any kind on this topic. However, in order to maintain high-quality data organization and comparability, standardized outcome measures for treatment effectiveness should be developed. Thus, authors intending to conduct future research should consider assessing and reporting at least all of the above: dislocation frequency, occurrence of acoustic symptoms, mandibular opening path, pain intensity, and range of jaw abduction, both before and after the investigated treatment method.
Consequently, although conservative and minimally invasive methods are more frequently chosen for the treatment of pediatric patients, the current literature does not indicate that age alone should be considered a sufficient contraindication to surgical approaches in children, due to a lack of evidence. The significance of an interdisciplinary approach seems to be highlighted, as this treatment strategy appears repeatedly in successfully resolved case reports. However, the available data are limited and lack the consistency needed to draw any definitive conclusions.
The main limitations identified while conducting the study were primarily the small number of eligible studies available in the literature and the particularly small number of participants involved in the included research. In addition, the overall level of evidence was low, as most of the included articles were case reports. Consequently, heterogeneity was observed among study designs, interventions, and outcome measures, which made direct comparisons difficult or impossible. Furthermore, the possibility of reporting bias among the included studies cannot be fully excluded. The limitations mentioned above suggest that the results should be interpreted with caution.
In conclusion, although research indicates that conservative and minimally invasive methods are the most frequently chosen approaches for managing recurrent temporomandibular joint dislocation in children, the limited number of recent studies on this topic prevents drawing definitive conclusions regarding their effectiveness. While some reports suggest that surgical approaches may also be effective, they should be considered a last resort, and further high-quality research is needed to confirm their safety in the paediatric population. Importantly, future studies should employ the outcome measures identified in this review to ensure comparability and consistency of results.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm14217881/s1, Document S1: PRISMA 2020 Checklist; Document S2: PRISMA 2020 for Abstracts Checklist.
Author Contributions
Conceptualization, A.H., M.C. and M.S.; methodology, A.H., N.T. and M.C.; software, A.H., M.C., K.C. and K.K.; validation, N.T., K.C., A.M., B.W., T.W. and M.C.; formal analysis, A.H., N.T., M.C. and K.C.; investigation, A.H., M.C. and K.R.; resources, A.H., M.C. and K.R.; data curation, A.H., N.T., M.C. and K.R.; writing—original draft preparation, A.H., N.T., M.C., K.C., K.K. and K.R.; writing—review and editing, N.T., A.M., B.W., T.W. and M.S.; visualization, A.H. and M.C.; supervision, M.S.; project administration, M.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is contained within the article or Supplementary Materials.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| TMJ | Temporomandibular joint |
| TMDs | Temporomandibular joint disorders |
| IMF | Intermaxillary fixation |
Appendix A

Table A1.
Search queries.
Table A1.
Search queries.
| Database | Search Query |
|---|---|
| BASE | (habitual OR recurrent OR chronic OR repeated OR relapsing OR recurring) AND (dislocation OR luxation OR subluxation OR displacement OR malposition) AND (temporomandibular OR mandible OR TMJ OR jaw) AND (child OR kids OR minor OR adolescent OR toddler OR preteen OR juvenile OR pediatric OR underage OR preadolescent OR youth) AND (treatment OR management OR therapy OR remediation OR remedy OR care OR approach) |
| PubMed | (habitual OR recurrent OR chronic OR repeated OR relapsing OR recurring) AND (dislocation [Title] OR luxation [Title] OR subluxation [Title] OR displacement [Title] OR malposition [Title]) AND (temporomandibular OR mandible OR TMJ OR jaw) AND (child OR kids OR minor OR adolescent OR toddler OR preteen OR juvenile OR pediatric OR underage OR preadolescent OR youth) AND (treatment OR management OR therapy OR remediation OR remedy OR care OR approach) |
| Scopus | TITLE-ABS-KEY ((habitual OR recurrent OR chronic OR repeated OR relapsing OR recurring) AND (temporomandibular OR mandible OR tmj OR jaw) AND (child OR kids OR minor OR adolescent OR toddler OR preteen OR juvenile OR pediatric OR underage OR preadolescent OR youth) AND (treatment OR management OR therapy OR remediation OR remedy OR care OR approach)) AND (TITLE (dislocation OR luxation OR subluxation OR displacement OR malposition)) |

Table A2.
Studies excluded at full-text assessment stage.
Table A2.
Studies excluded at full-text assessment stage.
| First Author, Publication Year | Digital Object Identifier (DOI) or Alternative | Reason for Exclusion |
|---|---|---|
| Souza, 2025 | 10.1080/08869634.2022.2110190 | Impossible to determine which patients were under the age of 18. |
| Lee, 2024 | 10.21203/rs.3.rs-5223475/v1 | No treatment methods described. |
| Wang, 2021 | 10.1097/MD.0000000000024012 | Dislocation was a one-time occurrence; there was no recurrence. |
| Aamir, 2020 | - | Impossible to determine which method was performed on the pediatric patient. |
| Bukhari, 2020 | 10.5455/JPMA.5002 | Impossible to determine if the study contained patients under 18 and which method was performed. |
| Papoutsis, 2018 | 10.2147/OAEM.S174116 | Impossible to determine which method was performed on the pediatric patient. |
| Gorchynski, 2014 | 10.1016/j.jemermed.2014.06.050 | Patients aged 18 years or older. |
| Oshiro, 2014 | 10.1016/j.jcms.2014.04.018 | None of the required measures. |
| Ungor, 2013 | 10.1097/SCS.0b013e31827ff14f | Impossible to determine which results describe pediatric patients. |
| Ybema, 2013 | 10.1016/j.ijom.2012.09.017 | Impossible to recognize any of the required measures in a pediatric patient. |
| Zhou, 2013 | 10.1016/j.bjoms.2013.08.018 | Impossible to determine which results describe pediatric patients. |
| Bekreev, 2012 | PMID: 23268183 | Unrelated topic. |
| Torres, 2012 | 10.1016/j.ijom.2012.03.008 | Impossible to determine which method was performed on the pediatric patient. |
| Zakariaei, 2012 | PMID: 22418992 | Dislocation was a one-time occurrence; there was no recurrence. |
| Chhabra, 2011 | 10.4103/0970-4388.90758 | Dislocation was a one-time occurrence; there was no recurrence. |
| Kummoona, 2010 | 10.1097/SCS.0b013e3181f3c682 | Patients aged 18 years or older. |
| Papadopoulos, 2010 | 10.1016/j.ijom.2009.12.011 | Dislocation was a one-time occurrence, there was no recurrence. |
| Sang, 2010 | 10.4314/eamj.v87i1.59949 | Unclear if the patient has recurrent TMJ dislocation; impossible to determine which method was performed on the pediatric patient. |
| Machon, 2009 | 10.1016/j.joms.2008.08.044 | Impossible to recognize any of the required measures in a pediatric patient. |
| Medra, 2008 | 10.1016/j.bjoms.2007.08.004 | Patients aged 18 years or older. |
| Willemsen, 2008 | PMID: 18188830 | Unrelated topic. |
| Cardoso, 2005 | 10.1016/s1808-8694(15)31282-9 | Patients aged 18 years or older. |
| Ugboko, 2005 | 10.1016/j.ijom.2004.10.025 | Impossible to determine if the pediatric patient has recurrent TMJ dislocation; impossible to determine which method was performed on the pediatric patient. |
| Nitzan, 2002 | 10.1053/joms.2002.31846 | Impossible to recognize any of the required measures in a pediatric patient. |

Table A3.
Critical appraisals/case–control studies.
Table A3.
Critical appraisals/case–control studies.
| First Author, Publication Year | Were the Groups Comparable Other than the Presence of Disease in Cases or the Absence of Disease in Controls? | Were Cases and Controls Matched Appropriately? | Were the Same Criteria Used for Identification of Cases and Controls? | Was Exposure Measured in a Standard, Valid and Reliable Way? | Was Exposure Measured in the Same Way for Cases and Controls? | Were Confounding Factors Identified? | Were Strategies to Deal with Confounding Factors Stated? | Were Outcomes Assessed in a Standard, Valid and Reliable Way for Cases and Controls? | Was the Exposure Period of Interest Long Enough to Be Meaningful? | Was Appropriate Statistical Analysis Used? |
|---|---|---|---|---|---|---|---|---|---|---|
| Triantafillidou, 2012 [38] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |

Table A4.
Critical appraisal, case series.
Table A4.
Critical appraisal, case series.
| First Author, Publication Year | Were There Clear Criteria for Inclusion in the Case Series? | Was the Condition Measured in a Standard, Reliable Way for All Participants Included in the Case Series? | Were Valid Methods Used for Identification of the Condition for All Participants Included in the Case Series? | Did the Case Series Have Consecutive Inclusion of Participants? | Did the Case Series Have Complete Inclusion of Participants? | Was There Clear Reporting of the Demographics of the Participants in the Study? | Was There Clear Reporting of Clinical Information of the Participants? | Were the Outcomes or Follow-Up Results of Cases Clearly Reported? | Was There Clear Reporting of the Presenting Site(s)/Clinic(s) Demographic Information? | Was Statistical Analysis Appropriate? |
|---|---|---|---|---|---|---|---|---|---|---|
| Yoshida, 2018 [34] | Yes | Unclear | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | No |
| Coser, 2015 [36] | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | No |
| Gadre, 2010 [39] | Yes | Yes | Unclear | Yes | Unclear | Yes | Yes | Yes | Yes | No |

Table A5.
Critical appraisal, case reports.
Table A5.
Critical appraisal, case reports.
| First Author, Publication Year | Were the Patient’s Demographic Characteristics Clearly Described? | Was the Patient’s History Clearly Described and Presented as a Timeline? | Was the Current Clinical Condition of the Patient on Presentation Clearly Described? | Were Diagnostic Tests or Assessment Methods and the Results Clearly Described? | Was the Intervention(s) or Treatment Procedure(s) Clearly Described? | Was the Post-Intervention Clinical Condition Clearly Described? | Were Adverse Events (Harms) or Unanticipated Events Identified and Described? | Does the Case Report Provide Takeaway Lessons? |
|---|---|---|---|---|---|---|---|---|
| Mohan, 2022 [32] | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Sicard, 2018 [33] | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| French, 2017 [35] | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Yes |
| Stark, 2015 [37] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Martínez-Pérez, 2004 [40] | Yes | Unclear | Yes | Unclear | Yes | Yes | No | Yes |
References
- Lomas, J.; Gurgenci, T.; Jackson, C.; Campbell, D. Temporomandibular Dysfunction. Aust. J. Gen. Pract. 2018, 47, 212–215. [Google Scholar] [CrossRef]
- Beaumont, S.; Garg, K.; Gokhale, A.; Heaphy, N. Temporomandibular Disorder: A Practical Guide for Dental Practitioners in Diagnosis and Management. Aust. Dent. J. 2020, 65, 172–180. [Google Scholar] [CrossRef]
- Polat, S.; Öksüzler, F.Y.; Öksüzler, M.; Çoban, Ö.; Tunç, M.; Yüksel, H.D.; Özşahin, E.; Göker, P. Temporomandibular Joint and Masticatory Muscles Morphometry and Morphology in Healthy Subjects and Individuals with Temporomandibular Dysfunction: An Anatomical, Radiological, and Machine Learning Application Study. Medicine 2024, 103, e40846. [Google Scholar] [CrossRef]
- Ghasemzadeh, F.; Mortazavi, N.; Mallahi, M.; Gharib, M.H.; Behnampour, N.; Badeleh, M.T.; Asgari, N. Association between Psychological Stress and Mandibular Condyle Structure: An Analytical Cross-Sectional Study. BMC Musculoskelet. Disord. 2024, 25, 563. [Google Scholar] [CrossRef]
- Chęciński, M.; Chęcińska, K.; Turosz, N.; Brzozowska, A.; Chlubek, D.; Sikora, M. Current Clinical Research Directions on Temporomandibular Joint Intra-Articular Injections: A Mapping Review. JCM 2023, 12, 4655. [Google Scholar] [CrossRef]
- Chęciński, M.; Chęcińska, K.; Rąpalska, I.; Turosz, N.; Chlubek, D.; Sikora, M. Autologous Blood Injections in Temporomandibular Hypermobility: A Systematic Review. J. Clin. Med. 2023, 12, 5590. [Google Scholar] [CrossRef]
- Khan, Y.S.; Fakoya, A.O.; Bordoni, B. Anatomy, Head and Neck: Suprahyoid Muscle. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Mansfield, P.J.; Neumann, D.A. Kinesiology of Mastication and Ventilation. In Essentials of Kinesiology for the Physical Therapist Assistant; Elsevier: Amsterdam, The Netherlands, 2019; pp. 368–385. ISBN 978-0-323-54498-6. [Google Scholar]
- Jain, P.; Rathee, M. Anatomy, Head and Neck, Medial Pterygoid Muscle. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Tuijt, M.; Parsa, A.; Koutris, M.; Berkhout, E.; Koolstra, J.H.; Lobbezoo, F. Human Jaw Joint Hypermobility: Diagnosis and Biomechanical Modelling. J. Oral Rehabil. 2018, 45, 783–789. [Google Scholar] [CrossRef]
- Govind, A.; Onuegbu, S.; Rafati, S.; Harrison, P.; Duong, D.K. Landmarks for Positioning and Local Anesthesia to Improve Success and Experience in Reduction of the Dislocated Temporomandibular Joint. J. Emerg. Med. 2025, 70, 117–126. [Google Scholar] [CrossRef] [PubMed]
- White, T.; Hedderick, V.; Ramponi, D.R. Dislocation of the Temporomandibular Joint and Relocation Procedures. Adv. Emerg. Nurs. J. 2016, 38, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Akinbami, B.O. Evaluation of the Mechanism and Principles of Management of Temporomandibular Joint Dislocation. Systematic Review of Literature and a Proposed New Classification of Temporomandibular Joint Dislocation. Head Face Med. 2011, 7, 10. [Google Scholar] [CrossRef] [PubMed]
- Tarhio, R.; Toivari, M.; Snäll, J.; Uittamo, J. Causes and Treatment of Temporomandibular Luxation—A Retrospective Analysis of 260 Patients. Clin. Oral Investig. 2023, 27, 3991–3997. [Google Scholar] [CrossRef] [PubMed]
- Ey-Chmielewska, H.; Rogowska, R.; Kozak, M.; Dalewski, B. Leczenie zachowawcze nawykowego podwichnięcia w zaburzeniach czynnościowych stawu skroniowo-żuchwowego—opis przypadku. Prosthodontics 2016, 66, 41–47. [Google Scholar] [CrossRef]
- Abrahamsson, H.; Eriksson, L.; Abrahamsson, P.; Häggman-Henrikson, B. Treatment of Temporomandibular Joint Luxation: A Systematic Literature Review. Clin. Oral Investig. 2020, 24, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, L.; Jaisani, M.R.; Sagtani, A.; Win, A. Conservative Management of Chronic TMJ Dislocation: An Old Technique Revived. J. Maxillofac. Oral Surg. 2015, 14, 267–270. [Google Scholar] [CrossRef]
- Lubecka, K.; Chęcińska, K.; Bliźniak, F.; Chęciński, M.; Turosz, N.; Rąpalska, I.; Michcik, A.; Chlubek, D.; Sikora, M. Update on Evidence and Directions in Temporomandibular Joint Injection Techniques: A Rapid Review of Primary Research. J. Clin. Med. 2024, 13, 4022. [Google Scholar] [CrossRef]
- Hegab, A.F. Treatment of Chronic Recurrent Dislocation of the Temporomandibular Joint with Injection of Autologous Blood Alone, Intermaxillary Fixation Alone, or Both Together: A Prospective, Randomised, Controlled Clinical Trial. Br. J. Oral Maxillofac. Surg. 2013, 51, 813–817. [Google Scholar] [CrossRef]
- Prechel, U.; Ottl, P.; Ahlers, O.M.; Neff, A. The Treatment of Temporomandibular Joint Dislocation. Dtsch. Ärzteblatt Int. 2018, 115, 59. [Google Scholar] [CrossRef] [PubMed]
- Dasukil, S.; Shetty, S.K.; Arora, G.; Degala, S. Efficacy of Prolotherapy in Temporomandibular Joint Disorders: An Exploratory Study. J. Maxillofac. Oral Surg. 2021, 20, 115–120. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Sikora, M.; Chęciński, M.; Nowak, Z.; Chlubek, D. Variants and Modifications of the Retroauricular Approach Using in Temporomandibular Joint Surgery: A Systematic Review. JCM 2021, 10, 2049. [Google Scholar] [CrossRef]
- Meng, F.; Liu, Y.; Hu, K.; Zhao, Y.; Kong, L.; Zhou, S. A Comparative Study of the Skeletal Morphology of the Temporo-Mandibular Joint of Children and Adults. J. Postgrad. Med. 2008, 54, 191–194. [Google Scholar] [CrossRef]
- Karlo, C.A.; Stolzmann, P.; Habernig, S.; Müller, L.; Saurenmann, T.; Kellenberger, C.J. Size, Shape and Age-Related Changes of the Mandibular Condyle During Childhood. Eur. Radiol. 2010, 20, 2512–2517. [Google Scholar] [CrossRef] [PubMed]
- Buschang, P.H.; Santos-Pinto, A. Condylar Growth and Glenoid Fossa Displacement during Childhood and Adolescence. Am. J. Orthod. Dentofac. Orthop. 1998, 113, 437–442. [Google Scholar] [CrossRef]
- Inarejos Clemente, E.J.; Tolend, M.; Navallas, M.; Doria, A.S.; Meyers, A.B. MRI of the Temporomandibular Joint in Children with Juvenile Idiopathic Arthritis: Protocol and Findings. Pediatr. Radiol. 2023, 53, 1498–1512. [Google Scholar] [CrossRef] [PubMed]
- Bordoni, B.; Varacallo, M. Anatomy, Head and Neck, Temporomandibular Joint. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- JBI Critical Appraisal Tools|JBI. Available online: https://jbi.global/critical-appraisal-tools (accessed on 14 June 2025).
- Lee, K.H.; Chou, H.J. An Interesting Case of Recurrent Temporomandibular Joint Dislocation. N. Z. Dent. J. 2009, 105, 128–130. [Google Scholar]
- Mohan, A.; Zakai, D.; Savani, J.; Pigadas, N. Recurrent TMJ Dislocations in Children: A Case Report and Protocol for Management. Adv. Oral Maxillofac. Surg. 2022, 5, 100216. [Google Scholar] [CrossRef]
- Sicard, L.; O’Hana, D.; Khonsari, R.H.; Kaddour Brahim, A. Bilateral Dislocation of the Temporomandibular Joint in Children. J. Oral Maxillofac. Surg. 2018, 76, 2307–2315. [Google Scholar] [CrossRef]
- Yoshida, K. Botulinum Neurotoxin Injection for the Treatment of Recurrent Temporomandibular Joint Dislocation with and without Neurogenic Muscular Hyperactivity. Toxins 2018, 10, 174. [Google Scholar] [CrossRef]
- French, K.E.; Wilson, M.H.; Revington, P.J. Chronic Recurrent Dislocation of the Temporomandibular Joint Secondary to a Complex Facial Tic Disorder. Br. J. Oral Maxillofac. Surg. 2017, 55, 1045–1046. [Google Scholar] [CrossRef]
- Coser, R.; Da Silveira, H.; Medeiros, P.; Ritto, F.G. Autologous Blood Injection for the Treatment of Recurrent Mandibular Dislocation. Int. J. Oral Maxillofac. Surg. 2015, 44, 1034–1037. [Google Scholar] [CrossRef] [PubMed]
- Stark, T.R.; Perez, C.V.; Okeson, J.P. Recurrent TMJ Dislocation Managed with Botulinum Toxin Type A Injections in a Pediatric Patient. Pediatr. Dent. 2015, 37, 65–69. [Google Scholar]
- Triantafillidou, K.; Venetis, G.; Markos, A. Short-Term Results of Autologous Blood Injection for Treatment of Habitual TMJ Luxation. J. Craniofacial Surg. 2012, 23, 689–692. [Google Scholar] [CrossRef]
- Gadre, K.S.; Kaul, D.; Ramanojam, S.; Shah, S. Dautrey’s Procedure in Treatment of Recurrent Dislocation of the Mandible. J. Oral Maxillofac. Surg. 2010, 68, 2021–2024. [Google Scholar] [CrossRef]
- Martínez-Pérez, D.; Ruiz-Espiga, P.G. Recurrent Temporomandibular Joint Dislocation Treated with Botulinum Toxin: Report of 3 Cases. J. Oral Maxillofac. Surg. 2004, 62, 244–246. [Google Scholar] [CrossRef]
- Kapos, F.P.; Exposto, F.G.; Oyarzo, J.F.; Durham, J. Temporomandibular Disorders: A Review of Current Concepts in Aetiology, Diagnosis and Management. Oral Surg. 2020, 13, 321–334. [Google Scholar] [CrossRef]
- Valesan, L.F.; Da-Cas, C.D.; Réus, J.C.; Denardin, A.C.S.; Garanhani, R.R.; Bonotto, D.; Januzzi, E.; de Souza, B.D.M. Prevalence of Temporomandibular Joint Disorders: A Systematic Review and Meta-Analysis. Clin. Oral Investig. 2021, 25, 441–453. [Google Scholar] [CrossRef] [PubMed]
- Zieliński, G. Quo Vadis Temporomandibular Disorders? By 2050, the Global Prevalence of TMD May Approach 44%. J. Clin. Med. 2025, 14, 4414. [Google Scholar] [CrossRef]
- Papoutsis, G.; Papoutsi, S.; Klukowska-Rötzler, J.; Schaller, B.; Exadaktylos, A. Temporomandibular Joint Dislocation: A Retrospective Study from a Swiss Urban Emergency Department. OAEM 2018, 10, 171–176. [Google Scholar] [CrossRef]
- De Coster, P.J.; Van den Berghe, L.I.; Martens, L.C. Generalized Joint Hypermobility and Temporomandibular Disorders: Inherited Connective Tissue Disease as a Model with Maximum Expression. J. Orofac. Pain. 2005, 19, 47–57. [Google Scholar] [PubMed]
- Oelerich, O.; Daume, L.; Yekkalam, N.; Hanisch, M.; Menne, M.C. Temporomandibular Disorders among Ehlers-Danlos Syndromes: A Narrative Review. J. Int. Med. Res. 2024, 52, 3000605241242582. [Google Scholar] [CrossRef]
- Zanoteli, E.; Yamashita, H.K.; Suzuki, H.; Oliveira, A.S.B.; Gabbai, A.A. Temporomandibular Joint and Masticatory Muscle Involvement in Myotonic Dystrophy: A Study by Magnetic Resonance Imaging. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002, 94, 262–271. [Google Scholar] [CrossRef]
- Mejersjö, C.; Kiliaridis, S. Temporomandibular Dysfunction in Adult Patients with Myotonic Dystrophy (DM1). J. Oral Rehabil. 2017, 44, 749–755. [Google Scholar] [CrossRef]
- Fry, C.S.; Nayeem, S.Z.; Dillon, E.L.; Sarkar, P.S.; Tumurbaatar, B.; Urban, R.J.; Wright, T.J.; Sheffield-Moore, M.; Tilton, R.G.; Choudhary, S. Glucocorticoids Increase Skeletal Muscle NF-κB Inducing Kinase (NIK): Links to Muscle Atrophy. Physiol. Rep. 2016, 4, e13014. [Google Scholar] [CrossRef]
- Kamel, S.I.; Rosas, H.G.; Gorbachova, T. Local and Systemic Side Effects of Corticosteroid Injections for Musculoskeletal Indications. Am. J. Roentgenol. 2024, 222, e2330458. [Google Scholar] [CrossRef] [PubMed]
- Tofts, L.J.; Elliott, E.J.; Munns, C.; Pacey, V.; Sillence, D.O. The Differential Diagnosis of Children with Joint Hypermobility: A Review of the Literature. Pediatr. Rheumatol. Online J. 2009, 7, 1. [Google Scholar] [CrossRef]
- Wahezi, D.M.; Ilowite, N. Joint Problems and Hypermobility. Pediatr. Rev. 2009, 30, 187–189. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ulmner, M.; Sugars, R.; Naimi-Akbar, A.; Reseland, J.E.; Lund, B. General Joint Hypermobility in Temporomandibular Joint Disease; Clinical Characteristics, Biomarkers, and Surgical Aspects. Heliyon 2023, 9, e23051. [Google Scholar] [CrossRef]
- Ziegler, C.M.; Haag, C.; Mühling, J. Treatment of Recurrent Temporomandibular Joint Dislocation with Intramuscular Botulinum Toxin Injection. Clin. Oral Investig. 2003, 7, 52–55. [Google Scholar] [CrossRef] [PubMed]
- Daif, E. Autologous Blood Injection As A New Treatment Modality for Chronic Recurrent Temporomandibular Joint Dislocation. Hell. Arch. Oral Maxillofac. Surg. 2024, 109, 31–36. [Google Scholar] [CrossRef]
- Ukwas, A.; Elshik, M.; Elbialy, M. TMJ Ankylosis in Children: A Case Report and Literature Review. Case Rep. Dent. 2023, 2023, 6474478. [Google Scholar] [CrossRef] [PubMed]
- Yew, C.C.; Rahman, S.A.; Alam, M.K. Temporomandibular Joint Ankylosis in a Child: An Unusual Case with Delayed Surgical Intervention. BMC Pediatr. 2015, 15, 169. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, F.U. The Immobilization of Joints. In The Immobilized Patient: Functional Pathology and Management; Steinberg, F.U., Ed.; Springer: Boston, MA, USA, 1980; pp. 99–110. ISBN 978-1-4684-3653-2. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).