Abstract
Background: Metabolic dysfunction-associated steatotic liver disease (MASLD) is defined by the presence of hepatic steatosis and at least one cardiometabolic risk factor. Differences in the incidence of MASLD between men and women are primarily due to distinct metabolic and cardiovascular profiles. The aim of this observational study was to investigate the prevalence and characteristics of MASLD in men and women. Methods: The study included patients from the Polish Gallstone Surgery Registry diagnosed with MASLD according to current criteria. Results: Among 3419 patients, MASLD was diagnosed in 24.2%. Its prevalence was significantly higher in men (29.8%) than in women (21.9%) (p < 0.0001), with the highest incidence observed in men aged 70–79 (32.1%) and women aged 70–79 (33.3%). MASLD was associated with overweight in individuals aged < 50 years (OR 1.87; 95% CI: 1.11–3.14; p < 0.0186) and in those aged ≥ 50 years (OR 1.99; 95% CI: 1.48–2.68; p < 0.001), as well as with obesity in patients aged < 50 years (OR 6.53; 95% CI: 4.08–10.47; p < 0.001) and in those aged ≥ 50 years (OR 3.9; 95% CI: 2.92–5.22; p < 0.0001). Conclusions: In this study, MASLD was diagnosed more frequently in men than in women, and its incidence showed a positive association with increasing BMI. These findings indicate that excess body weight and sex are key predictors of MASLD, highlighting the need for individualized treatment strategies.
1. Introduction
Metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as metabolic dysfunction-associated fatty liver disease (MAFLD) and non-alcoholic fatty liver disease (NAFLD), encompasses a broad spectrum of hepatic and extra-hepatic pathophysiological and clinical manifestations resulting from liver steatosis [1]. According to the current definition, MASLD is diagnosed after excluding causes of steatosis that are not metabolic [2,3].
The prevalence of MASLD is continuously rising, making it the most common liver disease worldwide, affecting approximately 20–30% of adults [4,5]. The risk factors for MASLD are well established; a strong association with obesity, poor nutrition, dyslipidemia, and sedentary lifestyle has been observed. These factors contribute to lipotoxicity, the production of reactive oxygen species, dysbiosis of the intestinal microbiome, genetic predisposition, and the induction of proinflammatory immune mediators [6].
Consequently, patients with MASLD not only present with a worsened cardiometabolic profile [7,8] but are also at a significantly higher risk of death from cardiovascular disease than from liver disease complications [9].
The heterogeneity between females and males in the prevalence, risk factors, and mechanisms of MASLD has long been recognized but remains incompletely understood. Regarding sex-related differences, both the prevalence and severity of MASLD are higher in men than in women of reproductive age. However, after menopause, the condition occurs more frequently in women, suggesting that estrogens have a protective effect [10]. Additionally, estradiol influences fatty acid synthase expression in hepatic and adipose cells, while saturated fatty acids induce endoplasmic reticulum stress and increase mitochondrial free radical generation, leading to cellular injury and liver steatosis [11].
Moreover, sex and age differences are also observed in the prevalence of diabetes mellitus type 2 (T2DM), visceral adipose tissue accumulation, and components of metabolic syndrome—all of these are major risk factors for MASLD [12,13].
There is a lack of evidence exploring sex-related differences in the epidemiological risk factors for MASLD. Therefore, we aimed to investigate the prevalence of MASLD and its characteristics in men and women.
2. Materials and Methods
2.1. Study Design
This prospective, multicenter, and observational study involved patients from the Polish Gallstone Surgery Registry. Patients who underwent cholecystectomy due to gallstone disease were consecutively enrolled across six surgical hospitals, including four academic centers and two regional hospitals, providing a comprehensive overview of surgical approaches in Poland. The data included patients admitted to one of the participating centers between 2019 and 2022, either for elective or emergency procedures. To ensure an unbiased selection process and create a cohort reflective of real-world conditions, no specific exclusion criteria were applied.
2.2. Patient Involvement
Consecutively hospitalized patients who underwent cholecystectomy were included in the study. MASLD was diagnosed based on the current criteria recommended in June 2023 by experts from the following hepatology societies: European Association for the Study of the Liver (EASL), La Asociación Latinoamericana para el Estudio del Hígado (ALEH), and the American Association for the Study of Liver Diseases (AASLD) [10].
The diagnostic criteria for MASLD included the presence of liver steatosis with at least one cardiometabolic factor:
- -
- BMI ≥ 25 kg/m2;
- -
- Fasting serum glucose ≥ 5.6 mmol/L (100 mg/dL) or 2 h post-load glucose level ≥ 7.8 mmol/L (≥140 mg/dL) or HbA1c ≥ 5.7% (39 mmol/L) or diabetes mellitus type 2 (T2DM) or treatment for T2DM;
- -
- Blood pressure ≥ 130/85 mmHg or specific antihypertensive drug treatment;
- -
- Plasma triglycerides ≥ 1.7 mmol/L (150 mg/dL) or lipid lowering treatment;
- -
- Plasma high-density lipoprotein cholesterol (HDL-C) ≤ 1.0 mmol/L (40 mg/dL)—men and ≤ 1.3 mmol/L (50 mg/dL)—women or lipid lowering treatment.
In this study, the two latter factors were collectively referred to as atherogenic dyslipidemia.
All the presented diagnostic criteria were available for all the patients included in the study. Patients with incomplete diagnostic data for MASLD, particularly those lacking BMI information, as well as individuals with liver steatosis due to non-metabolic causes (such as alcohol-related or toxic etiologies), were excluded from the analysis (Figure 1).
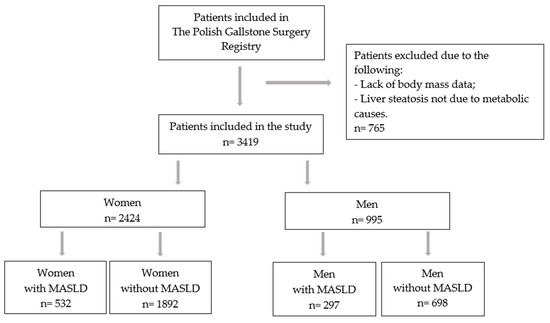
Figure 1.
Flow chart of the study. Abbreviation: MASLD—metabolic dysfunction-associated steatotic liver disease.
MASLD was diagnosed during hospitalization. Clinical data regarding comorbidities were obtained through patient history, while laboratory tests and anthropometric measurements were also performed during hospitalization. Hepatic steatosis was assessed using abdominal ultrasonography.
The study was approved by the Ethics Committee of the Collegium Medicum of Jan Kochanowski University (104/2022). This study adhered to the ethical guidelines outlined in the Declaration of Helsinki and its subsequent amendments. The requirement for patient informed consent was waived, as this was a retrospective study conducted exclusively using de-identified data.
2.3. Statistical Analyses
Continuous data were described using means and standard deviations, while categorical data were summarized as frequencies and percentages. Group comparisons were conducted using the chi-square or Fisher exact test for categorical variables and t-test or Mann–Whitney test for continuous variables. Univariable and multivariable analyses were performed using logistic regression models. Separable multivariable analyses were carried out for younger (<50 years) and older (≥50) patients. For these analyses, odds ratios (OR) with 95% confidence intervals (95% CI) were calculated. A two-tailed p-value < 0.05 was considered statistically significant. All the statistical analyses were conducted using the R software package version 4.0.3.
3. Results
3.1. Patient Characteristics
A total of 3419 participants were analyzed, including 995 men (29.1%) and 2424 women (70.9%). The mean age of the study population was 54.8 years (SD: 15.3). Among the participants, 27 (0.8%) were underweight, 849 (24.8%) had a normal body mass, 1310 (38.3%) were overweight, and 1233 (36.1%) had obesity. Hypertension was diagnosed in 1433 patients (41.9%), T2DM or prediabetes in 519 patients (15.2%), and atherogenic dyslipidemia in 432 patients (12.6%). The baseline characteristics of the study participants categorized by sex are presented in Table 1.

Table 1.
Comparison of patients with and without MASLD categorized by sex.
3.2. Prevalence of MASLD in Men and Women
Among the patients included in the study, MASLD was diagnosed in 829 patients (24.2%). Its prevalence was significantly higher in the men (n = 297, 29.8%) than in the women (n = 532, 21.9%), p < 0.0001. Lean MASLD was diagnosed in 94 patients (11.3% of those with MASLD), including 63 women (8.9% of women without overweight/obesity) and 31 men (17.2% of men without overweight/obesity), p = 0.0012. MASLD in the patients with overweight/obesity was diagnosed in 469 women (27.3%) and in 266 men (32.6%), p = 0.0057.
3.3. Prevalence of Cardiometabolic MASLD Diagnostic Criteria in Men and Women According to BMI
Most patients met two diagnostic criteria for MASLD diagnosis. No significant differences were observed in the number of diagnostic criteria between men and women. Table 2 presents the number of diagnostic criteria by sex.

Table 2.
Number of factors included in MASLD diagnosis.
In the normal body mass group, hypertension, T2DM or prediabetes, and atherogenic dyslipidemia were diagnosed more frequently in men than in women (37.7% vs. 23.4%; 11.2% vs. 5.7%; 14.0% vs. 6.7%, respectively). In contrast, no significant differences in the incidence of these conditions were observed between male and female patients in the overweight group (Table 3).

Table 3.
Prevalence of MASLD and cardiometabolic conditions in various BMI groups among women and men.
3.4. Comparison of Men and Women with MASLD
In the present study, women and men with MASLD did not differ significantly in age (59.6 vs. 58.5, p = 0.2383). The proportion of patients with MASLD and obesity was not statistically higher in women than in men (57.3% vs. 50.5%, p = 0.0516). However, gender-related differences were observed across obesity classes. Among the patients with MASLD and obesity, class I obesity was diagnosed in 180 women (58.8%) and 107 men (71.3%)—p = 0.0094; class II obesity was diagnosed in 82 women (26.8%) and 27 men (18%)—p = 0.0385; and class III obesity was observed in 44 women (14.4%) and 16 men (10.7%)—p = 0.2705.
The clinical characteristics of the men and women with MASLD were similar, with no significant differences in the incidence of hypertension, T2DM or prediabetes, atherogenic dyslipidemia, heart failure, or atrial fibrillation (Table 1).
3.5. Prevalence of MASLD and Stratification by Age, BMI, and Metabolic Disorder
The prevalence of MASLD was not linearly associated with age (Figure 2). In the overall population, the prevalence gradually increased with age, peaking at 32.1% in the 70–79 age group. Interestingly, in the men, the prevalence of MASLD rose sharply between the ages of 40–49 and remained stable until age 79, reaching a peak of 33% in the 70–79 age group. In contrast, MASLD prevalence in the women gradually increased in the 50–59 age range, peaking at 33.3% between ages 70 and 79. As expected, the lowest incidence of MASLD in both women and men was observed in the <30 and ≥80 age groups.
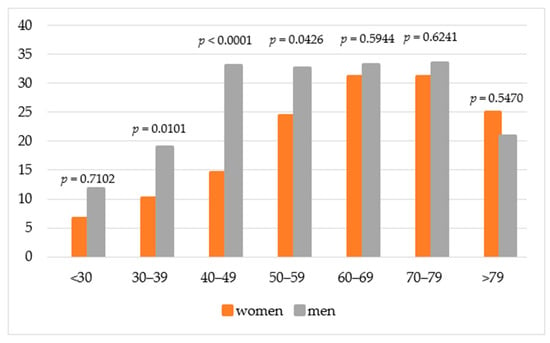
Figure 2.
Prevalence of MASLD in different age groups.
The prevalence rates of MASLD in different cardiometabolic groups by sex differed only in the patients with overweight and obesity, with a higher incidence in men than in women (32.6% vs. 27.2%, p = 0.0057). In the patients with hypertension, those with T2DM or prediabetes, and those with atherogenic dyslipidemia, the prevalence of MASLD did not differ between the women and the men (Table 4).

Table 4.
Prevalence of MASLD across different cardiometabolic groups in women and men.
3.6. Risk Factors for MASLD
The relationship between MASLD, age, and BMI is presented in Table 5, which shows the incidence of MASLD across the BMI categories and various age groups in both the females and the males.

Table 5.
Multivariable logistic regression analysis including age, sex, and BMI as predictors of MASLD.
Multivariable logistic regression analysis showed that younger age group was associated with MASLD incidence. As expected, the risk increased with an increase in BMI. In patients with BMI ≥ 30 kg/m2, the risk was significantly high in younger and older patients.
4. Discussion
The prevalence of MASLD appears to differ between men and women depending on age and the presence of comorbidities. The major findings of this study are as follows. Firstly, our country-specific registry data revealed that the incidence of MASLD is higher in men than in women. Secondly, the incidence of MASLD increases with age and in both sexes, reaching a peak between 70 and 79 years. Thirdly, higher body weight was identified as a strong risk factor for MASLD, independent of age.
Our findings indicate that MASLD posed a significant burden on the population undergoing cholecystectomy, with an overall prevalence of 24.2%. Although the study population consisted of patients with gallstone disease, the incidence of MASLD was similar to that in the general population. Notably, we observed a sex-specific difference in MASLD prevalence, with men having a higher prevalence (29.8%) than women (21.9%), suggesting that men are more susceptible to MASLD than women. The higher prevalence of MASLD in men may increase their vulnerability to chronic diseases such as hypertension, cardiovascular disease, T2DM, and stroke.
It should be emphasized that currently there is evidence suggesting a potential association between gallstone disease and MASLD. Both gallstone disease and MASLD represent increasingly prevalent global pathologies contributing to a substantial economic and healthcare burden [14,15]. However, the underlying etiology linking these two conditions remains unclear [16,17]. Even among individuals with normal BMI, patients with MASLD have a 1.29-fold higher risk of gallstone disease [18]. Furthermore, gallstone disease incidence is influenced not only by sex and BMI but also by age, waist circumference, and smoking habits, which indicates that the development of gallstone disease and MASLD originate from similar risk factors [19,20].
Crudele et al. [21] reported that MASLD was diagnosed in 59% of patients having metabolic syndrome, with a higher incidence observed in men. A Spanish study found the overall prevalence of NAFLD to be 19.1%, with rates of 27.9% in men and 6.8% in women, increasing across age groups [22]. Data from the National Health and Nutrition Examination Survey III (NHANES III) also indicated that MASLD is more common in men than in women. Similarly, Chang et al. [23] demonstrated a clear male predominance in MASLD prevalence, with a higher rate in men (45.7%) than in women (23.9%). It is important to note that MASLD is more frequently observed in Asian populations [24,25]. However, another study reported a higher prevalence in women (31.7%) compared to men (25.5%), which may be attributed to a smaller sample size and, more significantly, differences in the age distribution of the study population [26]. That study included patients with a mean age of 67 years, whereas the mean age in our study was 55.
The inclusion of a higher proportion of postmenopausal women may have influenced the results, as estrogen has been shown to have a protective effect against MASLD [27,28,29]. Studies on sex differences in MASLD show that MASLD is more prevalent in men than in women of reproductive age. However, after menopause, this difference diminishes, exposing older women to higher rates of MASLD. Analysis of the Polish Gallstone Surgery Registry showed that the incidence of MASLD increased with age, with the highest percentage of patients observed in the 70–79 age group for both women and men. Chang et al. [23] reported the highest prevalence of MASLD in the 50–59 age group, suggesting that it is more common in middle-aged individuals. A high proportion of MASLD diagnoses in men was observed between 40 and 49 years, whereas in women it was most common between 50 and 59 years. This difference may be influenced by hormonal changes in women, making them more susceptible to MASLD at an older age. Conversely, younger men have a higher incidence of metabolic and cardiovascular diseases, which may predispose them to develop MASLD at an earlier age than women.
Interestingly, in the present study, the incidence of MASLD did not differ between men and women in the subgroups of patients having hypertension, T2DM/prediabetes, or atherogenic dyslipidemia. Numerous epidemiological studies have shown that overweight and obesity are significant, independent, and modifiable risk factors for MASLD, as evidenced by the parallel rise in obesity rates and prevalence of MASLD [7,30,31]. Chen et al. [25] also identified a strong, nearly linear relationship between MASLD incidence and increased BMI. Regardless of other metabolic abnormalities, patients with obesity face a higher risk of developing MASLD. Accordingly, the prevention of MASLD requires effective strategies targeting both the prevention and treatment of obesity. The data regarding the role of excess body weight in the development of MASLD is unequivocal and it is well established that obesity most frequently results from insufficient physical activity combined with unhealthy dietary habits. Current clinical guidelines for the management of patients with MASLD highlight the central role of non-pharmacological interventions, which are considered fundamental both in the prevention and in the therapeutic management of this condition [32,33].
However, our subgroup analysis of age and BMI revealed distinct sex differences, showing that men are more prone to MASLD than women, particularly at a younger age. Furthermore, our data demonstrated a significant link between MASLD, BMI, and age, with higher BMI and younger age strongly associated with greater prevalence. These findings suggest that elevated BMI, especially in younger men, may be a key factor in the onset and progression of MASLD.
5. Strengths and Limitations
The present study has several strengths, including the focus on MASLD as a common and highly relevant clinical problem, the use of data obtained from a multicenter study, and the consideration of sex-related differences in the epidemiology of metabolic diseases, which are of particular importance when planning preventive and early diagnostic strategies tailored to women and/or men. It should also be emphasized that in recent years the definition and diagnostic criteria of MASLD have undergone dynamic changes, further highlighting the importance of continuously addressing this condition.
This study has inherent limitations, the primary one being the specific population analyzed—patients who underwent cholecystectomy for gallstone disease. This limitation may be considered from two perspectives. On the one hand, the findings may not be fully generalizable to a broader population, even though the incidence of MASLD observed in this study is consistent with that reported in the general population. On the other hand, it should be noted that the study cohort displayed a prevalence of MASLD, including sex-related distribution between women and men, similar to that observed in the general population. Additionally, it is important to recognize that the study cohort predominantly consisted of women, which may have influenced the results. As with all retrospective studies, the presence of unidentified confounders cannot be excluded. In particular, we were unable to adjust for individual-level socioeconomic status, duration of diabetes mellitus, or hormonal status within the study group. Furthermore, another limitation is the incomplete availability of certain data, as some variables were missing for some patients (e.g., laboratory tests other than those required for the diagnosis of MASLD).
6. Conclusions
Our results suggest a high prevalence of MASLD and other metabolic conditions, particularly obesity, in patients undergoing cholecystectomies. In both men and women, the prevalence of MASLD increased with age and BMI. Prioritizing the prevention and management of metabolic disorders, especially obesity, is crucial for the effective treatment of MASLD. These findings underscore the importance of developing personalized interventions to prevent and manage MASLD in both women and men.
Author Contributions
Conceptualization, I.G.-G., Ł.N., K.R. (Krzysztof Ratnicki), and P.M.; methodology, I.G.-G., Ł.N., R.M., K.R. (Krzysztof Ratnicki), M.C., K.M., M.P. and K.R. (Kamil Rapacz); formal analysis, I.G.-G., Ł.N., M.K., R.M., K.R. (Krzysztof Ratnicki), M.C., P.R., K.R. (Kamil Rapacz), M.S. (Maciej Sroczyński), and M.S. (Mateusz Szmit); investigation, I.G.-G., Ł.N., M.K., R.M., M.N., M.C., S.L., L.K. and P.R.; resources, I.G.-G., R.M., M.N., K.R. (Krzysztof Ratnicki), S.L., K.M., L.K., M.P., P.R., K.R. (Kamil Rapacz), M.S. (Maciej Sroczyński), and M.S. (Mateusz Szmit); data curation, I.G.-G., Ł.N., M.K., R.M., M.N., S.L., K.M., L.K., M.S. (Maciej Sroczyński), and M.S. (Mateusz Szmit); writing—original draft preparation, I.G.-G., Ł.N., M.K., P.M. and M.P.; writing—review and editing, R.M. and K.R. (Krzysztof Ratnicki); project administration, I.G.-G., Ł.N. and P.M. All authors have read and agreed to the published version of the manuscript.
Funding
The science project of Jan Kochanowski University in Kielce, Poland (project number, SUPS.RN.25.029; to I.G.-G.).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Collegium Medicum, Jan Kochanowski University (104/2022)—4 November 2022.
Informed Consent Statement
The requirement for patient informed consent was waived as this was a retrospective study conducted exclusively using de-identified data.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Rinella, M.E.; Lazarus, J.V.; Ratziu, V.; Francque, S.M.; Sanyal, A.J.; Kanwal, F.; Romero, D.; Abdelmalek, M.F.; Anstee, Q.M.; Arab, J.P.; et al. NAFLD Nomenclature consensus group. A multi-society Delphi consensus statement on new fatty liver disease nomenclature. J. Hepatol. 2023, 6, 1542–1556. [Google Scholar] [CrossRef] [PubMed]
- Janczura, J.; Brzdęk, M.; Dobrowolska, K.; Flisiak, R.; Martonik, D.; Brzdęk, K.; Pleśniak, R.; Kukla-Woźnica, D.; Wajdowicz, M.; Zarębska-Michaluk, D. Steatotic liver disease in patients treated for chronic hepatitis B. Pol. Arch. Intern. Med. 2025, 135, 16942. [Google Scholar] [CrossRef] [PubMed]
- Dixon, W.; Corey, K.E.; Luther, J.; Goodman, R.P.; Schaefer, E.A. Prevalence and Clinical Correlation of Cardiometabolic Risk Factors in Alcohol-Related Liver Disease and Metabolic Dysfunction and Alcohol Associated Liver Disease (MetALD). J. Clin. Exp. Hepatol. 2025, 15, 102492. [Google Scholar] [CrossRef] [PubMed]
- Pimpin, L.; Cortez-Pinto, H.; Negro, F.; Corbould, E.; Lazarus, J.V.; Webber, L.; Sheron, N. Burden of liver disease in Europe: Epidemiology and analysis of risk factors to identify prevention policies. J. Hepatol. 2018, 69, 718–735. [Google Scholar] [CrossRef]
- Yang, A.H.; Tincopa, M.A.; Tavaglione, F.; Ajmera, V.H.; Richards, L.M.; Amangurbanova, M.; Butcher, C.; Hernandez, C.; Madamba, E.; Singh, S. Prevalence of steatotic liver disease, advanced fibrosis and cirrhosis among community-dwelling overweight and obese individuals in the USA. Gut 2024, 73, 2045–2053. [Google Scholar] [CrossRef]
- Hong, S.; Sun, L.; Hao, Y.; Li, P.; Zhou, Y.; Liang, X.; Hu, J.; Wei, H. From NAFLD to MASLD: When metabolic comorbidity matters. Ann. Hepatol. 2024, 29, 101281. [Google Scholar] [CrossRef]
- Zhao, D.; Zheng, X.; Wang, L.; Xie, Y.; Chen, Y.; Zhang, Y. Overlap prevalence and interaction effect of cardiometabolic risk factors for metabolic dysfunction-associated steatotic liver disease. Nutr. Metab. 2025, 22, 10. [Google Scholar] [CrossRef]
- Stefan, N.; Yki-Järvinen, H.; Neuschwander-Tetri, B.A. Metabolic dysfunction-associated steatotic liver disease: Heterogeneous pathomechanisms and effectiveness of metabolism-based treatment. Lancet Diabetes Endocrinol. 2025, 13, 134–148. [Google Scholar] [CrossRef]
- Mayén, A.L.; Sabra, M.; Aglago, E.K.; Perlemuter, G.; Voican, C.; Ramos, I.; Debras, C.; Blanco, J.; Viallon, V.; Ferrari, P.; et al. Hepatic steatosis, metabolic dysfunction and risk of mortality: Findings from a multinational prospective cohort study. BMC Med. 2024, 22, 221. [Google Scholar] [CrossRef]
- Lonardo, A.; Nascimbeni, F.; Ballestri, S.; Fairweather, D.; Win, S.; Than, T.A.; Abdelmalek, M.F.; Suzuki, A. Sex differences in nonalcoholic fatty liver disease: State of the art and identification of research gaps. Hepatology. 2019, 70, 1457–1469. [Google Scholar] [CrossRef]
- Chen, K.L.; Madak-Erdogan, Z. Estrogens and female liver health. Steroids. 2018, 133, 38–43. [Google Scholar] [CrossRef]
- Colosimo, S.; Mitra, S.K.; Chaudhury, T.; Marchesini, G. Insulin resistance and metabolic flexibility as drivers of liver and cardiac disease in T2DM. Diabetes Res. Clin. Pract. 2023, 206, 111016. [Google Scholar] [CrossRef]
- Qureshi, K.; Abrams, G.A. Metabolic liver disease of obesity and role of adipose tissue in the pathogenesis of nonalcoholic fatty liver disease. World J. Gastroenterol. 2007, 13, 3540–3553. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Yu, W.; Jiang, G.; Li, H.; Li, S.; Xie, L.; Bai, X.; Cui, P.; Chen, Q.; Lou, Y.; et al. Global Epidemiology of Gallstones in the 21st Century: A Systematic Review and Meta-Analysis. Clin. Gastroenterol. Hepatol. 2024, 22, 1586–1595. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Rydqvist, P.; Ramezani, T.; Haas, J.S.; Bantel, H.; Buggisch, P.; Geier, A.; Hofmann, W.P.; Mauss, S.; Roeb, E.; et al. Metabolic Dysfunction-Associated Steatohepatitis Diagnosis and Management in Germany: Insights From an Expert Consensus Panel. Liver Int. 2025, 45, e70225. [Google Scholar] [CrossRef] [PubMed]
- Roesch-Dietlen, F.; Pérez-Morales, A.G.; Grube-Pagola, P.; González-Santes, M.; Díaz-Roesch, F.; Triana-Romero, A.; Roesch-Ramos, L.; Remes-Troche, J.M.; Cruz-Aguilar, M. Prevalence of metabolic associated fatty liver disease (MAFLD) in patients with gallstone disease. Study on a cohort of cases in South-Southeastern Mexico. Rev. Gastroenterol. Mex. 2023, 88, 225–231. [Google Scholar] [CrossRef]
- Zhao, G.; Shi, R.; Ma, M.; Lin, H.; Zhang, J.; Sheng, B. Elevated LDL-c may warn of the risk of gallbladder stones in the patients with metabolic dysfunction-associated steatotic liver disease: A case-control study. Clin. Res. Hepatol. Gastroenterol. 2024, 48, 102363. [Google Scholar] [CrossRef]
- Kim, N.H.; Kang, J.H.; Kim, H.J. Association between nonalcoholic fatty liver disease and gallstone risk in nonobese and lean individuals. Eur. J. Gastroenterol. Hepatol. 2024, 36, 945–951. [Google Scholar] [CrossRef]
- Shabanzadeh, D.M.; Holmboe, S.A.; Sørensen, L.T.; Linneberg, A.; Andersson, A.M.; Jørgensen, T. Are incident gallstones associated to sex-dependent changes with age? A cohort study. Andrology 2017, 5, 931–938. [Google Scholar] [CrossRef]
- Sogabe, M.; Okahisa, T.; Kagawa, M.; Kashihara, T.; Fujmoto, S.; Kawaguchi, T.; Yokoyama, R.; Kagemoto, K.; Tanaka, H.; Kida, Y.; et al. Association of metabolic dysfunction-associated fatty liver disease with gallstone development: A longitudinal study. J. Gastroenterol. Hepatol. 2024, 39, 754–761. [Google Scholar] [CrossRef]
- Najafi, F.; Pasdar, Y.; Nazar, M.M.; Darbandi, M. Association between obesity phenotypes and non-alcoholic fatty liver: A large population-based study. BMC Endocr. Disord. 2024, 24, 96. [Google Scholar] [CrossRef]
- Fresneda, S.; Abbate, M.; Busquets-Cortés, C.; López-González, A.; Fuster-Parra, P.; Bennasar-Veny, M.; Yáñez, A.M. Sex and age differences in the association of fatty liver index-defined non-alcoholic fatty liver disease with cardiometabolic risk factors: A cross-sectional study. Biol. Sex. Differ. 2022, 13, 64. [Google Scholar] [CrossRef] [PubMed]
- Ji, H.; Cheng, S. Heart-Liver Axis Research Collaboration: Sex differences in prevalence and prognosis of steatotic liver disease phenotypes: Biological sex matters. J. Hepatol. 2024, 80, e68–e69. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.; Shao, Z.; Wei, W.; Shen, P.; Shen, G. Sex-specific prevalence and risk factors of metabolic-associated fatty liver disease among 75,570 individuals in eastern China. Front. Endocrinol. 2023, 14, 1241169. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.L.; Li, H.; Li, S.; Xu, Z.; Tian, S.; Wu, J.; Liang, X.Y.; Li, X.; Liu, Z.L.; Xiao, J.; et al. Prevalence of and risk factors for metabolic associated fatty liver disease in an urban population in China: A cross-sectional comparative study. BMC Gastroenterol. 2021, 21, 212. [Google Scholar] [CrossRef]
- Lei, F.; Qin, J.J.; Song, X.; Liu, Y.M.; Chen, M.M.; Sun, T.; Huang, X.; Deng, K.Q.; Zuo, X.; Yao, D.; et al. The prevalence of MAFLD and its association with atrial fibrillation in a nationwide health check-up population in China. Front. Endocrinol. 2022, 13, 1007171. [Google Scholar] [CrossRef]
- Duan, H.; Gong, M.; Yuan, G.; Wang, Z. Sex Hormone: A Potential Target at Treating Female Metabolic Dysfunction-Associated Steatotic Liver Disease? J. Clin. Exp. Hepatol. 2025, 15, 102459. [Google Scholar] [CrossRef]
- Alves, E.S.; Santos, J.D.M.; Cruz, A.G.; Camargo, F.N.; Talarico, C.H.Z.; Santos, A.R.M.; Silva, C.A.A.; Morgan, H.J.N.; Matos, S.L.; Araujo, L.C.C.; et al. Hepatic Estrogen Receptor Alpha Overexpression Protects Against Hepatic Insulin Resistance and MASLD. Pathophysiology 2025, 32, 1. [Google Scholar] [CrossRef]
- Cherubini, A.; Della Torre, S.; Pelusi, S.; Valenti, L. Sexual dimorphism of metabolic dysfunction-associated steatotic liver disease. Trends. Mol. Med. 2024, 30, 1126–1136. [Google Scholar] [CrossRef]
- Ma, X.M.; Guo, Y.M.; Jiang, S.Y.; Li, K.X.; Zheng, Y.F.; Guo, X.G.; Ren, Z.Y. Potential predictive role of Non-HDL to HDL Cholesterol Ratio (NHHR) in MASLD: Focus on obese and type 2 diabetic populations. BMC Gastroenterol. 2025, 25, 79. [Google Scholar] [CrossRef]
- Shi, S.; Zhou, F.; Shen, J. Trends in the prevalence of cardiometabolic diseases in US adults with newly diagnosed and undiagnosed diabetes, 1988–2020. Public Health 2025, 239, 94–102. [Google Scholar] [CrossRef]
- Romeo, S.; Vidal-Puig, A.; Husain, M.; Ahima, R.; Arca, M.; Bhatt, D.L.; Diehl, A.M.; Fontana, L.; Foo, R.; Frühbeck, G.; et al. Clinical staging to guide management of metabolic disorders and their sequelae: A European Atherosclerosis Society consensus statement. Eur. Heart J. 2025, ehaf314. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines on the management of metabolic dysfunction-associated steatotic liver disease (MASLD). J. Hepatol. 2024, 81, 492–542. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).