Abstract
Although treatment with fixed or mobile appliances has become an important part of modern orthodontics, side effects such as white spot lesions (WSLs) have a negative impact on the aesthetic outcome of orthodontic treatment. The purpose of this article was to review current evidence on the diagnosis, risk assessment, prevention, management and post-orthodontic treatment of these lesions. Data collection was performed electronically, and the initial search using the keywords “white spot lesions”, “orthodontics”, “WSL”, “enamel” and “demineralization” in different combinations resulted in 1032 articles for the two electronic databases used. Ultimately, a total of 47 manuscripts were considered relevant to the aim of this research and included in this review. The results of the review indicate that WSLs remain a significant problem during orthodontic treatment. According to studies in the literature, the severity of WSLs correlates to the duration of treatment. Using toothpaste with more than 1000 ppm fluoride at home reduces the frequency of WSL separation and regular application of varnishes in the office reduces the frequency of the occurrence of WSLs only in the context of maintaining a strict hygiene regime. The old hypothesis that elastomeric ligatures retain more dental plaque than metal ones has been refuted. There are no differences in the appearance of WSLs between conventional brackets and self-ligating brackets. Clear aligner mobile devices develop fewer WSLs but are more extensive as opposed to conventional fixed devices, while lingual orthodontic appliances have a lower incidence of WSLs, and the most effective device for preventing these lesions is WIN, followed by Incognito.
1. Introduction
Orthodontic treatments have enjoyed growing popularity in recent years, and the white chalky spots, also called white spot lesions (WSLs), that appear after treatment are a major problem in dental aesthetics [1]. There are several causes of enamel demineralization, including poor nutrition and hygiene, and the use of incorrect adhesive techniques [2]. Although treatment with fixed or mobile appliances has become an important part of modern orthodontics, side effects such as WSLs have a negative impact on the aesthetic outcome of orthodontic treatment. The reported prevalence varies in each study [2,3,4,5,6], from 97%, as reported by Boersma et al. [5], to 33.8%, as reported by Geiger et al. [6], depending on the method/criteria of analysis chosen and whether the pre-existing enamel lesions are or are not included the reference unit used (surface, tooth or patient). In some cases, these demineralization lesions may be reversible; the chalky appearance may be partially neutralized by salivary proteins that remineralize the enamel surface [7]. However, in the case of orthodontic treatments, these lesions of the enamel evolve progressively and become irreversible, leading to carious processes [8]. Clinically, enamel demineralization initially occurs through white chalky spots, which also occur in dental fluorosis. In contrast, demineralization presents a high risk of developing tooth decay due to the friability of the enamel and the creation of retentive areas for bacterial plaque [9,10]. Demineralization is the process of removing mineral ions from hydroxy-apatite (HA) crystals in hard tissues, such as enamel, dentin, cement and bone. The restoration of these mineral ions in HA crystals is called remineralization. Both processes take place on the surface of the teeth, and a substantial number of mineral ions in HA can be lost without destroying their integrity, but high sensitivity to heat, cold, pressure and chemical stimuli would be expected [11,12]. Demineralization is a reversible process; therefore, partially demineralized HA crystals may increase to their original size if exposed to an oral environment that favors remineralization [13]. Chemical demineralization of teeth is caused by acid attack via two main means: food acid consumed by food or drink and microbial attack by bacteria present in the oral cavity [14].
However, each has its own specific disadvantages. Most importantly, orthodontic appliances, especially brackets, ligatures and arches, create new retentive areas with the undesired effect of plaque buildup [15]. An increase in the amount of dental plaque containing cariogenic bacteria is the main etiological factor in decalcifying the enamel during orthodontic treatment. This demineralization of the dental surfaces results in the appearance of white spots (WSLs) or even caries. However, in the literature, there are contradictory results on the relationship between orthodontic treatment and the development of dental caries [5,16,17]. Many preventive methods have been defined, such as the topical application of fluoride, the use of fluoride-releasing binders, the use of sodium fluoride mouthwashes and the application of chlorhexidine [18,19,20]. Providing adequate oral hygiene has a significant role in preventing demineralization and thus the formation of carious processes during orthodontic treatment [20]. Furthermore, fixed bonded retainers seem to be a good option for preventing tooth relapse after Invisalign and conventional fixed treatments; therefore, there is also an increased risk of developing WSLs after orthodontic treatment [21]. Genetic, prenatal, perinatal and postnatal factors, such as the breastfeeding period (2%), asthma (16%), high-fever episodes (20%), infections/illnesses (20%), chickenpox (12%), antibiotic intake (8%), diarrhea (4%) and pneumonia (4%) are also reported to influence dental demineralization processes [22]. Although WSLs are one of the most frequent and obvious side effects of orthodontic treatment, the effectiveness of WSL interventions has not yet been adequately evaluated in evidence-based medicine [23,24].
Due to the fact that there are many conflicting opinions regarding the etiology of demineralization of enamel after orthodontic treatment, the purpose of this article was to review current evidence on the management of WSLs and post-orthodontic treatment alternatives.
2. Materials and Methods
2.1. Eligibility Criteria
Inclusion criteria:
- Scientific articles published from 1 January 2010 to 31 December 2022;
- Scientific articles published in the English language;
- Clinical studies that mention development of WSLs during or after orthodontic treatment:
- The literature search was not restricted to any age interval, sex, duration of treatment or orthodontic disharmony treated with fixed appliances.
- Only articles related to the development of WSLs in connection with orthodontic treatment were considered relevant to the purpose of this review.
Exclusion criteria:
- Papers with no clear report of clinical study
- Lesions that are not present in the oral cavity or in a well-specified location in title and/or abstract;
- Animal studies;
- In vitro studies, case reports and case series.
2.2. Literature Search Strategy
2.2.1. Data Sources
In order to have a broader view of the subject, with the aid of the PubMed Central electronic library and Cochrane database, a comprehensive manual search was conducted. The main search was performed up to 31 December 2022, using the keywords “white spot lesions”, “orthodontics”, “WSL”, “enamel” and “demineralization” in different combinations (Figure 1). For quantification of the search results, the PRISMA flow chart guidelines [25] was used.
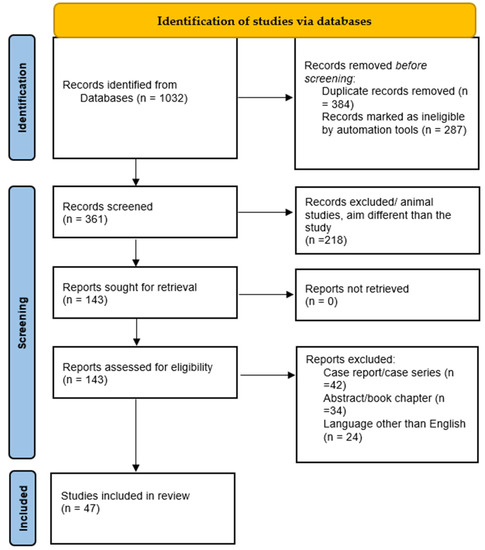
Figure 1.
PRISMA flow chart representation of the methodology for the conducted study.
2.2.2. The Data Collection Protocol Used in This Review Was as Follows
Data collection was performed electronically, and the initial search using the keywords “white spot lesions”, “orthodontics”, “WSL”, “enamel” and “demineralization” in different combinations resulted in 1032 articles for the two electronic databases used. To narrow down the number of articles and remove articles that were not of interest for our study, the following procedures were performed:
- -
- Selection of items from the Dentistry and Oral Health category;
- -
- The population was not restricted in any way (any race, sex, age, geographical location);
- -
- Selection of studies that included only orthodontically treated abnormalities by fixed or mobile methods;
- -
- Selection of articles only provided as a full text.
A total of 1032 documents in all were found following a thorough search of the online journals. Similar/duplicate publications were removed, leaving 143 distinct papers that were initially available. After reviewing the submissions’ abstracts and titles, 96 more articles were disqualified. The abstracts of the studies to be included were manually analyzed by two authors; the titles and abstracts of retrieved studies were screened and all the studies that contained one or more of the exclusion criteria were excluded. The articles selected for full-text reading were examined by the two authors, and those that were lacking relevant information for the purpose of this review were excluded. Any controversy was resolved with the aid of a third reviewer, selected among the authors. Ultimately, 47 documents that satisfied the necessary inclusion and exclusion criteria were selected.
2.3. Risk of Bias
In order to evaluate the methodological quality of included studies, the articles’ data were independently evaluated by the authors using a special manual form designed according to the following categories: study model design, major outcomes related to WSLs associated with orthodontic appliances, number of subjects and study results.
3. Results
This paper includes scientific articles published in the English language in recent years and clinical studies exploring orthodontic treatment and WSL occurrence and evolution related with different conditions. The results are systematized as follows.
3.1. Results According to the Prevention Method Used
3.1.1. Toothpaste with Fluoride
One of the most common topics in the selected articles was the effectiveness of high-fluoride toothpastes for WSL prevention (Table 1, Figure 2). In general, the concentration of sodium mono-fluorophosphate found in a common brand of toothpaste was 0.76% and the concentration of sodium fluoride was 0.22%. It was shown that the use of toothpaste with a fluoride concentration (in one of these forms) of over 1000 ppm reduces the frequency of enamel lesions by 20% [24].

Table 1.
Effectiveness of high-fluoride toothpastes for WSL prevention. X: not specified; +: positive result; -: negative result.
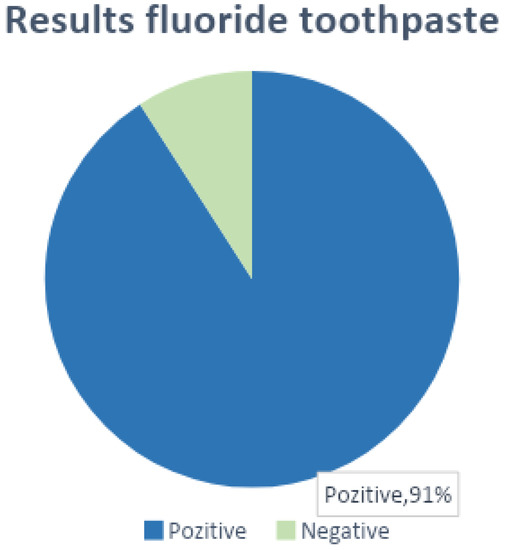
Figure 2.
Results that confirm/refute the effectiveness of fluoride pastes in WSL prevention.
Of the 47 studies analyzed, 10 of them (21.3%) showed that the use of toothpaste with a high fluoride concentration at home or in combination with the use of fluoride toothpastes in the office periodically leads to satisfactory results in preventing the occurrence of WSLs. One study did not find conclusive differences between the studied group and the control group, and 34 of the studies did not specify this aspect. A total of 91% had positive results, demonstrating the usefulness of fluoride toothpaste in the prevention of WSL.
3.1.2. Varnish with Fluoride
Using only standard prophylaxis, the treatment of demineralization around brackets has progressed. Additional prophylactic measures such as fluoride varnishes are needed. Among the analyzed studies that address the use of fluorinated varnishes and gels in the office for the prevention of WSLs and even the treatment of incipient lesions, 14 of the studies demonstrated the effectiveness of varnishes for this purpose (Figure 3).
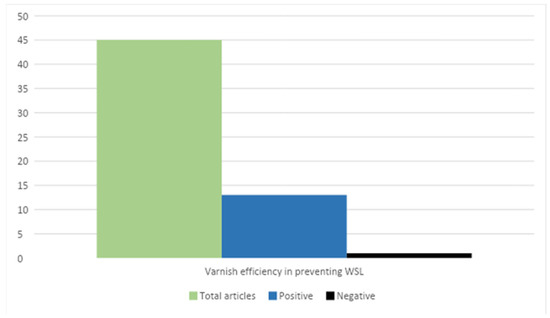
Figure 3.
The effectiveness of varnish-type varnishes in the prevention and treatment of incipient WSL lesions. Positive results: Restrepo M et al. [29], Rechmann P et al. [30], Federico Perrini et al. [35], Ashok Kumar Jena et al. [36], Nicoline CW van der Kaaij et al. [46], Adílis Kalina Alexandria et al. [49], Lídia Lipták et al. [50], Roslyn J Mayne et al. [61], Benson PE et al. [64], Gamze Metin-Gürsoy et al. [70], Marco Aurélio Paschoal et al. [57]. Negative result: Marcela Cristina Damião Andrucioli et al. [55].
Of the 14 articles evaluating the effectiveness of varnishes, only 1 study showed negative results. In their study, Damião Andrucioli et al. [55] compared the levels of Streptococcus mutans (MS) in saliva and the retained bacterial plaque around the brackets. In study group 1, a resin-modified glass ionomer cement (RMGIC) was used for cementing the brackets, and for group 2, a composite resin was utilized. Cementing with the RMGIC did not influence the number of MSs adjacent to the brackets; instead, the composite resin showed a progressive increase in MSs, with the appearance of demineralization signs. Topical applications with fluoride were not clinically relevant in this situation. The MS level was not altered in any of the groups following acid demineralization. Their conclusion suggested that topical application with fluoride has not been shown to be effective in reducing MSs and thus subsequent demineralization.
3.1.3. Differences between Paste and Varnish
Rechmann P, Bekmezian S et al. [30] attempted to demonstrate the difference in efficacy between fluoridated pastes and fluoridated varnish application in a study of 37 patients undergoing orthodontic treatment for 12 months. A paste with a concentration of 1100 ppm fluoride and a varnish were used once every 4 days in their study, for the experimental group and the control group. The same paste, with 1100 ppm fluoride, was used, but the varnish was replaced with mouthwash with a high concentration of fluoride. No statistically significant differences were found in the EDI (Early Development Index) or ICDAS (International Caries Detection and Assessment System). Salivary fluoride levels were significantly higher at 12 months for the experimental group than for the control group (0.20 ± 0.26 vs. 0.04 ± 0.04 ppm), demonstrating the superior efficacy of topical varnish applications used clinically [47].
3.1.4. Use of Probiotics
Numerous studies have shown how probiotics act to limit the proliferation of certain acidogenic bacteria, which motivated an attempt to demonstrate probiotics’ effect on the prevention of WSLs. This acid-neutralizing property was tested on 60 patients with fixed orthodontic appliances by Jose JE et al. [71]. They were divided into three groups of 20: the first group was the control, group 2 followed treatment with oral probiotics, and group 3 used toothpaste with probiotics daily.
The plaque index was analyzed twice: before the start of the study and after 30 days. The presence of Streptococcus mutans was assessed using the real-time PCR technique. The statistical analysis showed that there were significant reductions in the concentration of S mutans in groups 2 and 3 compared to group 1, but there were no statistically significant differences between groups 2 and 3. This study demonstrated the superior efficacy of probiotic toothpaste over oral probiotics in preventing WSLs.
On the other hand, Sotiria Gizani et al. [44] denies the effectiveness of using probiotics for WSL prevention, based on the results of a study of 85 patients. The study period was between 7 and 24 months after the removal of the orthodontic device. They were randomly assigned to the test group or placebo group. Subjects in the test group were instructed to take a probiotic pill containing two strains of Lactobacillus Reuteri once a day. Dental plaque, WSLs and salivary MS and LB levels were recorded at baseline and immediately after orthodontic device removal. This study concluded that the intake of probiotics has no clinical influence on the development of orthodontically induced WSLs with fixed appliances.
3.2. Results According to the Type of Ligatures Used (Elastic/Wire)
To identify the relationship between the amount of plaque and pathogenic bacteria present at the edge of the orthodontic appliance and the type of ligature material used, Tyson Buck, Peter Pellegrini et al. [37] analyzed the formation of white chalky spots via photographic evaluation and a fluorescent laser light (DIAGNOdent™). The study was performed on 13 subjects, including wearers of classic orthodontic appliances with elastic ligatures and wearers of SL (self-ligating) brackets. Bacterial plaque samples collected one year after device adhesion were analyzed via ATP bioluminescence, and WSLs were identified with DIAGNOdent™.
Through this study and with the help of ATP bioluminescence, the theory that elastomeric ligatures retain a richer bacterial colony than metal ones, which is upheld by many authors, was refuted. The amount of plaque and colonized bacteria were not significantly different between the two groups. Based on photographic determinations and DIAGNOdent™, WSLs were found to be equally prevalent in the two groups evaluated.
Fatma Deniz Uzuner, Emine Kaygisiz et al. [72] evaluated the effect of the type of ligatures used (conventional brackets with elastic ligatures versus self-ligating brackets) on the levels of Streptococcus Mutans (SM) and Lactobacillus (LB) in saliva and bacterial plaque. Their study included 40 non-smoking patients aged 14–16 that did not suffer from systemic diseases and were not under any antibiotic or probiotic treatments. They were randomly divided into two groups: conventional treatment (CB) and self-ligating brackets (SLBs). Using the Dentocult™ LB and MS system, no differences were observed in the number of MSs or LBs in the bacterial plaque between groups.
3.3. Results Depending on the Type of Orthodontic Appliance Used
3.3.1. Mobile versus Fixed Device
The emergence of alignment orthodontic appliances is considered revolutionary in orthodontics, mainly due to their aesthetic properties. Ziad Albhaisi et al. [38], aiming to analyze the relationship between orthodontic treatment with an aligner (CA—clear aligner) and the development of WSLs with a comparison with fixed orthodontic treatment (FA), conducted a randomized clinical study on 49 patients. CA treatment was performed for group 1 and FA for group 2. WSLs were analyzed using QLF (quantitative light-induced fluorescence). The mean fluorescence loss was 0.4% for the CA group (p = 0.283) and 1.2% for the FA group (p = 0.013). The average increase in lesion area was 82.2 pixels for the CA group (p < 0.001) and 9.3 pixels for the FA group (p = 0.225). Additionally, the mean value of newly developed lesions per patient was 6 WSLs in the CA group and 8.25 in the FA group (p = 0.039).
Demineralization was present in both groups treated with a mobile or fixed device, with the main difference being that in the CA group, larger but less developed lesions were found, while the FA group developed several new WSLs with a greater depth but a reduced surface size. Additionally, the plaque index (PI) was significantly higher in the group with fixed orthodontic braces.
3.3.2. Incognito versus WIN
Even if the appearance of WSLs on the vestibular surface of the teeth is not noticed by the patients during the treatment, they become a problem after the removal of the appliance, when the aesthetics are affected. The use of the oral surface of the teeth for the placement of brackets does not only present aesthetic advantages but can even be useful for reducing the frequency of enamel demineralization.
In order to make a comparison between the two types of multi-bracket devices (which differ in terms of design, material and manufacturing technology), the incidence of WSLs in subjects treated with lingual orthodontic appliances was analyzed in two studies. Knösel M et al. [59,62] demonstrated that subjects treated with the WIN device were at a lower risk of developing enamel-decalcifying side effects than those treated with the Incognito device. Both types of lingual devices reduced the frequency of WSLs compared to conventional devices.
3.4. Results Depending on the Adhesive Material of the Brackets
3.4.1. Cement
Ahmet Yagci et al. [43] compared three cementing agents’ (glass ionomer cement, compomer and poly-carboxyl cement) influence on the formation of WSLs in patients with circuit breakers. Subsequent white chalky spots were analyzed using the QLF method. Subjects were divided into three groups, including a control group that comprised patients who had never had orthodontic treatment. QLF images taken before and after the rapid maxillary expansion treatment were analyzed with regard to the following parameters: the proportion of fluorescence loss compared to healthy tissue and the maximum loss of fluorescence in the entire lesion. Demineralization was present in all three groups studied, and significantly more so in the treated groups than the control group. Polycarboxylate-cemented teeth developed the most WSLs, followed by glass-ionomer-cemented teeth. Compomers showed the best results, with compomer-cemented teeth developing the fewest WSLs. The benefits of glass ionomers were also presented by Damião Andrucioli et al. [55], who compared the levels of Streptococcus Mutans (SM) in saliva and the biofilm around the cemented resin-modified glass ionomer (RMGIC) and a classical composite resin. Their study showed a significant increase in the level of MS in the biofilm adjacent to the composite resin cast elements, while the RMGIC allowed better control of the number of MSs in the adjacent biofilm [55].
3.4.2. Composite Resins
In fixed orthodontic treatments, the most retentive area for bacterial plaque is around the metal bracket, due to the rough surface structure of the adhesive materials. The free surface energy released by them plays an important role in the adhesion of MSs to these materials. The different properties of materials, such as composites, glass ionomers, compomers and other materials, give them a wide range of indications, but none meet the ideal conditions. Alabdullah MM et al. [31] analyzed the effects of a fluoride-releasing composite on enamel and on the appearance of WSLs. Thirty-four patients were followed for twelve months, half of whom underwent orthodontic treatment with the classic composite material and the other half with the fluoride-releasing composite. The percentage of new WSL lesions increased from 6.3% (after 3 months) to 15% (after 12 months) for the control group and from 3% to 16.3% for the study group. No significant differences between the two groups in terms of lesions over time were found in DIAGNOdent™ examinations or photographic analyses. Alabdullah MM et al. [31] concluded that composite resins do not have the desired effect of preventing demineralization and WSL formation during fixed-brace orthodontic treatment.
3.4.3. Sealers
The application of sealants for the protection of enamel is common in patients with fixed orthodontic appliances; however, the data regarding their in vivo durability are quite unclear. Although there are studies showing a decrease in the frequency of WSLs after the application of a sealing agent, very few studies have examined in vivo changes in sealant integrity and the influence of hygiene and observation time on results. We compared data from four studies that analyzed the effectiveness of sealers in the prevention of WSLs, of which 100% showed positive results. In combination with proper oral hygiene, fluoride-releasing sealants help reduce the frequency of WSLs [51,58,68,70].
Although these studies demonstrate the effectiveness of sealers in the prevention of WSLs, we must also consider their action over time. In vivo studies by Michael Knösel et al. [62] have shown that sealers provide enhanced protection against new WSLs, but do not provide protection throughout treatment, requiring reapplication. The durability of the sealing material can be influenced both by the time elapsed between applications and by the brushing technique or the forces applied, which cause the abrasion of the material. The integrity of the material was assessed using a UV lamp with black light, under which the sealant appears. The results of their study indicate that sealers are very effective in preventing WSLs, but their effectiveness decreases over time, and thus they require reapplication at approximately three and a half month intervals.
3.5. Results Depending on the Bonding Agent Used
Direct versus Indirect Technique
Aykan Onur Atilla et al. [51], in order to evaluate the level of enamel demineralization in fixed orthodontic treatment depending on the adhesive method used (direct or indirect), used QLF to compare the results of the two techniques. In their study, the percentage of fluorescence loss (ΔF and ΔF max), the degree of demineralization (ΔQ) and the surface area of the lesion (WS area) were determined and compared according to the adhesive technique. The study conducted on 56 patients demonstrated the low frequency of WSLs in the indirect technique. In addition, the increased efficiency of flowable composites has been demonstrated compared to conventional ones in terms of the occurrence of WSLs.
On the other hand, another study conducted by Kübra Yıldırım et al. [46] comparing the effects of the direct and indirect bond technique found no significant differences in the occurrence of WSLs in the two techniques. The indirect technique was significantly faster than the direct technique, and the marginal closure proved to be superior, but the bacterial plaque accumulation rate and WSL formation were not significantly different between the two groups.
3.6. Results Depending on the Demineralization Technique
3.6.1. Self-Etching Primers versus Conventional Demineralization
For the past 50 years, acid etching has been an important step in the bonding of orthodontic appliances. Obviously, the mineral component of enamel decreases over time, which makes it more prone to possible damage. In order to reduce the risks of acid etching, so-called self-etching primers have appeared on the market. Hu H et al. [67] evaluated the efficiency of SEPs (self-etching primers) compared to the conventional demineralization technique with orthophosphoric acid. Their study did not find any useful evidence suggesting whether SEPs or conventional acid etching lead to the formation of a smaller number of WSLs or a smaller surface area.
3.6.2. Total Etching versus Partial Etching
In determining whether total or partial etching techniques influence the occurrence of demineralization, Michael Knösel et al. [62] demonstrated that total demineralization of the vestibular surface, in combination with poor hygiene, has unfavorable WSL results. Excess etching over the entire surface, as well as prolonged acid etching time, should be avoided for the prevention of iatrogenic WSLs. Ahmet Yagci et al. [43] compared the two demineralization methods using quantitative fluorescent light (QLF) imaging. Photographs were taken at the beginning of treatment and at 3 (T1) and 6 (T2) months after the start of treatment, as well as at the end of treatment, after de-bracketing (T3).
Although partial etching seemed to be more successful in the first 6 months, in the long run, the results started to stabilize, and the differences between total and partial acid etching were demonstrated to be statistically insignificant. However, the authors concluded that PE (partial etching) is more successful than TE (total etching), as WSL formation was lower in the PE group than in the TE group, in all periods except T2 to T3 [60].
3.7. Results by Sex and Age
Michael Knösel et al. [62] also investigated the relevance of different patient selection criteria (age, sex) for the incidence and severity of WSLs or SBLs (under-bracket lesions). The incidence of WSLs in study subjects ≤16 and >16 years of age was analyzed separately, as the hypothesis of increased sensitivity of enamel lesions in pre-adolescents was considered. WSL development has been shown to be significantly increased in pre-adolescents (≤16 years) compared to adolescents (>16 years) and in male subjects, as demonstrated in 630 subjects.
4. Discussions
The results of this review indicate that WSLs remain a significant problem during orthodontic treatment. After analyzing all the included articles and comparing them according to the criteria mentioned above, detection of enamel lesions during orthodontic treatment was determined to be a challenge for the clinician [73]. The entire surface of the tooth should be free of plaque and not covered by the gums, and the tooth should be dried very well in order to detect incipient WSLs. In the absence of QLF or DIAGNOdent™, WSLs could be easily overlooked. These assessment methods are essential for the diagnosis of enamel lesions, being an additional aid for their monitoring [74]. Clinical evaluation using photographs is the simplest and the most commonly used method of diagnosis and monitoring [75]. Due to the subjectivity of this method and the low-quality properties, it should be standardized so that it is reproducible. In the absence of these standard parameters, this assessment should be based on quantitative methodology such as DIAGNOdent™ and QLF [74].
Due to individual differences in patient oral hygiene, eating habits and adherence, which play very important roles in the emergence of WSLs, the conclusions of this review cannot be generalized. Thus, additional studies on large patient populations are needed to validate its clinical relevance. Moreover, the oral hygiene status of patients, as assessed via plaque index scores, should be carefully assessed both before and during orthodontic treatment. Despite these limitations of this review due to different diagnostic and monitoring methods used, the lack of standardization of assessment methods and limited number of patients in some studies, a common finding for all included articles was that fluoride-based remineralization agents reduce the incidence of WSLs. It is very well known that fluoride has been the gold standard for remineralization in clinical practice for a few decades, but in recent years, new remineralizing strategies based on the integration of calcium and phosphates at the level of demineralized dental surfaces have been developed. Hydroxyapatite represents one of the most recently discovered remineralization systems and is used in an innovative biomimetic approach that aims to integrate it completely within the enamel structure and ensure its restoration with the same type of substance from which it is formed [76,77]. Due to its ability to repair dental hard tissue, it can protect teeth from erosions, wear and caries [78], while also being an effective desensitizing agent, even better than fluoride [79]. On the other hand, pre-orthodontic treatment with fluoride lacquer or varnish leads to lower bond strengths, which is likely to result in a higher frequency of premature detachment of the bracket [80]. The hydroxyapatite-based toothpaste tested caused a higher reduction in hypersensitivity/pain values than that found with conventional fluoride toothpaste [81]. So, in the future, hydroxyapatite could be helpful for patients with a high risk of enamel demineralization and carious lesions, such as orthodontic patients, and could perhaps become the new gold standard. Very recent studies suggest that resin infiltration and micro-abrasion techniques are comparably effective in reducing the sizes of WSLs, but resin infiltration enjoys an aesthetic advantage over micro-abrasion [82]. Furthermore, Simon et al. (2002), in their study, suggest that both resin infiltration and casein phospho-peptide-amorphous calcium phosphate have desired and durable aesthetic improvements in terms of a reduction in the area as well as the color of post-orthodontic white spot lesions [83].
A total of 7 out of 280 studies on remineralization, micro-abrasion and resin infiltration met the required criteria. WSL treatment generally involves several sessions, and recall intervals should be adjusted for the assessment of preventive interventions and monitoring of initial lesions and possible training in changing the patient’s oral and behavioral hygiene.
According to studies in the literature, the severity of WSLs correlates to the duration of treatment, and the clinical relevance of comparative studies is significant only for those conducted under the same period of orthodontic treatment. Although the number of articles included is quite small, the implication for the field is significant in that it brings a complex systematization of the data present in the literature. Although most patients have received sanitizing instructions, their cooperation and compliance need to be individually considered. Subsequent studies on the occurrence of WSLs after orthodontic treatment would be a real help in supplementing the information found so far in the literature.
Limitations of this Review
The results of this review can be seen to have certain limitations, namely the rather small number of studies analyzed. The present review augments the reference data in the literature, supporting future research in this field.
5. Conclusions
Using toothpaste with more than 1000 ppm fluoride at home reduces the frequency of WSL separation, and regular application of varnishes in the office reduces the frequency of the occurrence of WSLs only in the context where strict hygiene is maintained. The old hypothesis that elastomeric ligatures retain more plaque than metal ones has been refuted. There are no differences in the appearance of WSLs between conventional brackets and self-ligating brackets. Additionally, clear aligner mobile devices develop fewer but more extensive WSLs as opposed to conventional fixed devices, while lingual orthodontic appliances have a lower incidence of WSLs, with the most effective being WIN, followed by Incognito.
Author Contributions
All authors contributed equally to this research. L.L., A.B., L.M. and E.B. designed and performed the data collection phase; A.V., A.P.L., L.B. and L.L. derived the models and analyzed the data; A.V., E.B. and A.P.L. assisted with measurements and helped carry out the statistical analysis; L.L., A.V., L.M. and A.B. produced the manuscript in collaboration with E.B. and L.B.; A.P.L. assisted with the review of the article. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data supporting reported results, including links to publicly archived datasets analyzed can be checked with the corresponding author at alexandru.vlasa@umfst.ro.
Conflicts of Interest
The authors declare that they have no conflict of interests regarding this manuscript, and did not receive any financial support from any organizations or a research grant.
References
- Höchli, D.; Hersberger-Zurfluh, M.; Papageorgiou, S.N.; Eliades, T. Interventions for orthodontically induced white spot lesions: A systematic review and meta-analysis. Eur. J. Orthod. 2017, 39, 122–133. [Google Scholar] [CrossRef]
- Agrawal, A.; Shigli, A. Comparison of six different methods of cleaning and preparing occlusal fissure surface before placement of pit and fissure sealant: An in vitro study. J. Indian Soc. Pedod. Prev. Dent. 2012, 30, 51. [Google Scholar] [CrossRef]
- Srivastava, K.; Tikku, T.; Khanna, R.; Sachan, K. Risk factors and management of white spot lesions in orthodontics. J. Orthod. Sci. 2013, 2, 43–49. [Google Scholar] [CrossRef]
- Sundararaj, D.; Venkatachalapathy, S.; Tandon, A.; Pereira, A. Critical evaluation of incidence and prevalence of white spot lesions during fixed orthodontic appliance treatment: A meta-analysis. J. Int. Soc. Prev. Community Dent. 2015, 5, 433–439. [Google Scholar] [CrossRef]
- Boersma, J.; van der Veen, M.; Lagerweij, M.; Bokhout, B.; Prahl-Andersen, B. Caries Prevalence Measured with QLF after Treatment with Fixed Orthodontic Appliances: Influencing Factors. Caries Res. 2005, 39, 41–47. [Google Scholar] [CrossRef]
- Geiger, A.M.; Gorelick, L.; Gwinnett, A.J.; Griswold, P.G. The effect of a fluoride program on white spot formation during orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 1988, 93, 29–37. [Google Scholar] [CrossRef]
- Farooq, I.; Bugshan, A. The role of salivary contents and modern technologies in the remineralization of dental enamel: A narrative review. F1000 Research 2020, 9, 171. [Google Scholar] [CrossRef]
- Neel, E.A.A.; Aljabo, A.; Strange, A.; Ibrahim, S.; Coathup, M.; Young, A.M.; Bozec, L.; Mudera, V. Demineralization–remineralization dynamics in teeth and bone. Int. J. Nanomed. 2016, 11, 4743–4763. [Google Scholar] [CrossRef]
- Robinson, C.; Connell, S.; Kirkham, J.; Brookes, S.; Shore, R.; Smith, A. The Effect of Fluoride on the Developing Tooth. Caries Res. 2004, 38, 268–276. [Google Scholar] [CrossRef]
- Stavrianos, C.; Papadopoul, C.; Vasiliadis, L.; Dagkalis, P.; Stavrianou, I.; Petalotis, N. Enamel Structure and Forensic Use. Res. J. Biol. Sci. 2010, 5, 650–655. [Google Scholar] [CrossRef]
- Nanci, A. Ten Cate’s Oral Histology: Development, Structure, and Function; Mosby: Maryland Heights, MO, USA, 2008; pp. 22–31. [Google Scholar]
- Hart, S.; Hart, T. Disorders of human dentin. Cells Tissues Organs 2007, 186, 70–77. [Google Scholar] [CrossRef]
- Scaramucci, T.; Carvalho, J.C.; Hara, A.T.; Zero, D.T. Causes of Dental Erosion: Extrinsic Factors; Springer International Publishing: Berlin/Heidelberg, Germany, 2015; pp. 69–96. [Google Scholar]
- Scaramucci, T.; Carvalho, J.C.; Hara, A.T.; Zero, D.T. Causes of Dental Erosion: Intrinsic Factors; Springer International Publishing: Berlin/Heidelberg, Germany, 2015; pp. 35–67. [Google Scholar]
- Miura, K.K.; Ito, I.Y.; Enoki, C.; Elias, A.M.; Matsumoto, M.A.N. Anticariogenic effect of fluoride-releasing elastomers in orthodontic patients. Braz. Oral Res. 2007, 21, 228–233. [Google Scholar] [CrossRef]
- Chen, W.; Zhou, Y. Caries outcomes after orthodontic treatment with fixed appliances: A longitudinal prospective study. Int. J. Clin. Exp. Med. 2015, 8, 2815–2822. [Google Scholar]
- Kanthathas, K.; Willmot, D.R.; Benson, P.E. Differentiation of developmental and post-orthodontic white lesions using image analysis. Eur. J. Orthod. 2005, 27, 167–172. [Google Scholar] [CrossRef]
- Örtendahl, T.; Thilander, B.; Svanberg, M. Mutans streptococci and incipient caries adjacent to glass ionomer cement or resin-based composite in orthodontics. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 271–274. [Google Scholar] [CrossRef]
- Jurela, A.; Repic, D.; Pejda, S.; Juric, H.; Vidakovic, R.; Matic, I.; Bosnjak, A. The effect of two different bracket types on the salivary levels of S mutans and S sobrinus in the early phase of orthodontic treatment. Angle Orthod. 2013, 83, 140–145. [Google Scholar] [CrossRef]
- Fukae, M.; Yamamoto, R.; Karakida, T.; Shimoda, S.; Tanabe, T. Micelle structure of amelogenin in porcine secretory enamel. J. Dent. Res. 2007, 86, 758–763. [Google Scholar] [CrossRef]
- Lanteri, V.F.; Lanteri, G.; Caravita, C.; Cossellu, G.R. The efficacy of orthodontic treatments for anterior crowding with Invisalign compared with fixed appliances using the Peer Assessment Rating Index. Quintessence Int. 2018, 49, 581–587. [Google Scholar]
- Butera, A.; Maiorani, C.; Morandini, A.; Simonini, M.; Morittu, S.; Barbieri, S.; Bruni, A.; Sinesi, A.; Ricci, M.; Trombini, J.; et al. Assessment of Genetical, Pre, Peri and Post Natal Risk Factors of Deciduous Molar Hypomineralization (DMH), Hypomineralized Second Primary Molar (HSPM) and Molar Incisor Hypomineralization (MIH): A Narrative Review. Children 2021, 8, 432. [Google Scholar] [CrossRef]
- Quirynen, M.; Bollen, C.M.L. CA Novel Cold Atmospheric Pressure Air Plasma Jet for Peri-Implantitis Treatment: An in Vitro Study. J. Clin. Periodontol. 1995, 22, 1–14. [Google Scholar] [CrossRef]
- Sonesson, M.; Twetman, S.; Bondemark, L. Effectiveness of high-fluoride toothpaste on enamel demineralization during orthodontic treatment—A multicenter randomized controlled trial. Eur. J. Orthod. 2014, 36, 678–682. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef]
- Hoffman, D.A.; Clark, A.E.; Rody, W.J.; McGorray, S.P.; Wheeler, T.T. A prospective randomized clinical trial into the capacity of a toothpaste containing NovaMin to prevent white spot lesions and gingivitis during orthodontic treatment. Prog. Orthod. 2015, 16, 25. [Google Scholar] [CrossRef]
- Restrepo, M.; Bussaneli, D.G.; Jeremias, F.; Cordeiro, R.; Raveli, D.; Magalhães, A.; Candolo, C.; Santos-Pinto, L. Control of White Spot Lesions with Use of Fluoride Varnish or Chlorhexidine Gel During Orthodontic Treatment A Randomized Clinical Trial. J. Clin. Pediatr. Dent. 2016, 40, 274–280. [Google Scholar] [CrossRef]
- Sonesson, M.; Bergstrand, F.; Gizani, S.; Twetman, S. Management of post-orthodontic white spot lesions: An updated systematic review. Eur. J. Orthod. 2017, 39, 116–121. [Google Scholar] [CrossRef]
- Knösel, M.; Bojes, M.; Jung, K.; Ziebolz, D. Increased susceptibility for white spot lesions by surplus orthodontic etching exceeding bracket base area. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 574–582. [Google Scholar] [CrossRef]
- Rechmann, P.; Bekmezian, S.; Rechmann, B.M.T.; Chaffee, B.W.; Featherstone, J.D.B. MI Varnish and MI Paste Plus in a caries prevention and remineralization study: A randomized controlled trial. Clin. Oral Investig. 2018, 22, 2229–2239. [Google Scholar] [CrossRef]
- Alabdullah, M.M.; Nabawia, A.; Ajaj, M.A.; Saltaji, H. Effect of fluoride-releasing resin composite in white spot lesions prevention: A single-centre, split-mouth, randomized controlled trial. Eur. J. Orthod. 2017, 39, 634–640. [Google Scholar] [CrossRef]
- Gómez, C.; Abellán, R.; Palma, J.C. Efficacy of photodynamic therapy vs ultrasonic scaler for preventing gingival inflammation and white spot lesions during orthodontic treatment. Photodiagnosis Photodyn. Ther. 2018, 24, 377–383. [Google Scholar] [CrossRef]
- Yagci, A.; Korkmaz, Y.N.; Yagci, F.; Atilla, A.O.; Buyuk, S.K. Effect of 3 cements on white spot lesion formation after full-coverage rapid maxillary expander: A comparative in-vivo study. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 1005–1013. [Google Scholar] [CrossRef]
- Hammad, S.M.; Knösel, M. Efficacy of a new sealant to prevent white spot lesions during fixed orthodontic treatment: A 12-month, single-center, randomized controlled clinical trial. J. Orofac. Orthopedics. 2016, 77, 439–445. [Google Scholar] [CrossRef]
- Perrini, F.; Lombardo, L.; Arreghini, A.; Medori, S.; Siciliani, G. Caries prevention during orthodontic treatment: In-vivo assessment of high-fluoride varnish to prevent white spot lesions. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 238–243. [Google Scholar] [CrossRef]
- Jena, A.K.; Singh, S.P.; Utreja, A.K. Efficacy of resin-modified glass ionomer cement varnish in the prevention of white spot lesions during comprehensive orthodontic treatment: A split-mouth study. J. Orthod. 2015, 42, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Buck, T.; Pellegrini, P.; Sauerwein, R.; Leo, M.C.; Covell, D.A., Jr.; Maier, T.; Machida, C.A. Elastomeric-ligated vs self-ligating appliances: A pilot study examining microbial colonization and white spot lesion formation after 1 year of orthodontic treatment. Orthod. Art Pract. Dentofac. Enhanc. 2011, 12, 108–121. [Google Scholar]
- Albhaisi, Z.; Al-Khateeb, S.N.; Abu Alhaija, E.S. Enamel demineralization during clear aligner orthodontic treatment compared with fixed appliance therapy, evaluated with quantitative light-induced fluorescence: A randomized clinical trial. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Esenlik, E.; Çelik, E.U.; Bolat, E. Efficacy of a casein phosphopeptide amorphous calcium phosphate (CPP-ACP) paste in preventing white spot lesions in patients with fixed orthodontic appliances: A prospective clinical trial. Eur. J. Paediatr. Dent. 2016, 17, 274–280. [Google Scholar]
- Robertson, M.A.; Kau, C.H.; English, J.D.; Lee, R.P.; Powers, J.; Nguyen, J.T. MI Paste Plus to prevent demineralization in orthodontic patients: A prospective randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 660–668. [Google Scholar] [CrossRef]
- O’Reilly, M.T.; Viñas, J.D.J.; Hatch, J.P. Effectiveness of a sealant compared with no sealant in preventing enamel demineralization in patients with fixed orthodontic appliances: A prospective clinical trial. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.-C.; Hu, H.-T.; Chang, Y.-C. Effectiveness of Enzyme Dentifrices on Oral Health in Orthodontic Patients: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 16, 2243. [Google Scholar] [CrossRef] [PubMed]
- Yagci, A.; Seker, E.D.; Demirsoy, K.K.; Ramoglu, S.I. Do total or partial etching procedures effect the rate of white spot lesion formation? A single-center, randomized, controlled clinical trial. Angle Orthod. 2019, 89, 16–24. [Google Scholar] [CrossRef]
- Gizani, S.; Petsi, G.; Twetman, S.; Caroni, C.; Makou, M.; Papagianoulis, L. Effect of the probiotic bacteriumLactobacillus reuterion white spot lesion development in orthodontic patients. Eur. J. Orthod. 2016, 38, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Van Der Kaaij, N.C.W.; Van Der Veen, M.H.; Van Der Kaaij, M.A.E.; Cate, J.M.T. A prospective, randomized placebo-controlled clinical trial on the effects of a fluoride rinse on white spot lesion development and bleeding in orthodontic patients. Eur. J. Oral Sci. 2015, 123, 186–193. [Google Scholar] [CrossRef]
- Yıldırım, K.; Saglam-Aydinatay, B. Comparative assessment of treatment efficacy and adverse effects during nonextraction orthodontic treatment of Class I malocclusion patients with direct and indirect bonding: A parallel randomized clinical trial. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 26–34.e1. [Google Scholar] [CrossRef]
- Guram, G.; Kumar, G.S.; Kashyap, A.; Raghav, S.; Bhardwaj, R.; Singh, A. Role of Text Message Reminder on Oral Hygiene Maintenance of Orthodontic Patients. J. Contemp. Dent. Pract. 2018, 19, 98–101. [Google Scholar] [CrossRef] [PubMed]
- Alexandria, A.K.; Nassur, C.; Nóbrega, C.B.C.; Branco-De-Almeida, L.S.; dos Santos, K.R.N.; Vieira, A.R.; Neves, A.A.; Rosalen, P.L.; Valença, A.M.G.; Maia, L.C. Effect of TiF4 varnish on microbiological changes and caries prevention: In situ and in vivo models. Clin. Oral Investig. 2019, 23, 2583–2591. [Google Scholar] [CrossRef] [PubMed]
- Quaranta, A.; Marchisio, O.; D’isidoro, O.; Genovesi, A.M.; Covani, U. Single-blind randomized clinical trial on the efficacy of an interdental cleaning device in orthodontic patients. Minerva Dent. Oral Sci. 2018, 67, 141–147. [Google Scholar] [CrossRef]
- Lipták, L.; Szabó, K.; Nagy, G.; Marton, S.; Madléna, M. Microbiological Changes and Caries-Preventive Effect of an Innovative Varnish Containing Chlorhexidine in Orthodontic Patients. Caries Res. 2018, 52, 272–278. [Google Scholar] [CrossRef]
- Atilla, A.O.; Öztürk, T.; Eruz, M.M.; Yagci, A. A comparative assessment of orthodontic treatment outcomes using the quantitative light-induced fluorescence (QLF) method between direct bonding and indirect bonding techniques in adolescents: A single-centre, single-blind randomized controlled trial. Eur. J. Orthod. 2020, 42, 441–453. [Google Scholar] [CrossRef]
- Tüfekçi, E.; Pennella, D.R.; Mitchell, J.C.; Best, A.; Lindauer, S.J. Efficacy of a fluoride-releasing orthodontic primer in reducing demineralization around brackets: An in-vivo study. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 207–214. [Google Scholar] [CrossRef]
- Eppright, M.; Shroff, B.; Best, A.M.; Barcoma, E.; Lindauer, S.J. Influence of active reminders on oral hygiene compliance in orthodontic patients. Angle Orthod. 2014, 84, 208–213. [Google Scholar] [CrossRef]
- Danaei, S.M.; Safavi, A.; Roeinpeikar, S.M.; Oshagh, M.; Iranpour, S.; Omidekhoda, M. Ion release from orthodontic brackets in 3 mouthwashes: An in-vitro study. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 730–734. [Google Scholar] [CrossRef] [PubMed]
- Andrucioli, M.C.D.; Faria, G.; Nelson-Filho, P.; Romano, F.; Matsumoto, M.A.N. Influence of resin-modified glass ionomer and topical fluoride on levels of Streptococcus mutans in saliva and biofilm adjacent to metallic brackets. J. Appl. Oral Sci. 2017, 25, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Benson, P.E.; Alexander-Abt, J.; Cotter, S.; Dyer, F.M.V.; Fenesha, F.; Patel, A. Resin-modified glass ionomer cement vs composite for orthodontic bonding: A multicenter, single-blind, randomized controlled trial. Am. J. Orthod. Dentofac. Orthopedics. 2019, 155, 10–18. [Google Scholar] [CrossRef]
- Paschoal, M.A.B.; Gurgel, C.V.; Rios, D.; Magalhães, A.C.; Buzalaf, M.A.R.; Machado, M.A.D.A.M. Fluoride release profile of a nanofilled resin-modified glass ionomer cement. Braz. Dent. J. 2011, 22, 275–279. [Google Scholar] [CrossRef]
- Kantovitz, K.R.; Pascon, F.M.; Nociti, F.H.; Tabchoury, C.P.M.; Puppin-Rontani, R.M. Inhibition of enamel mineral loss by fissure sealant: An in situ study. J. Dent. 2013, 41, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Knösel, M.; Klang, E.; Helms, H.-J.; Wiechmann, D. Lingual orthodontic treatment duration: Performance of two different completely customized multi-bracket appliances (Incognito and WIN) in groups with different treatment complexities. Head Face Med. 2014, 10, 46. [Google Scholar] [CrossRef]
- Oosterkamp, B.C.M.; Wafae, A.; Schols, J.G.J.H.; Van Der Sanden, W.J.M.; Wensing, M. Effectiveness of a clinical guideline to improve dental health among orthodontically treated patients: Study protocol for a cluster randomized controlled trial. Trials 2016, 17, 201. [Google Scholar] [CrossRef]
- Mayne, R.J.; Cochrane, N.J.; Cai, F.; Woods, M.G.; Reynolds, E.C. In-vitro study of the effect of casein phosphopeptide amorphous calcium fluoride phosphate on iatrogenic damage to enamel during orthodontic adhesive removal. Am. J. Orthod. Dentofac. Orthop. 2011, 139, e543–e551. [Google Scholar] [CrossRef]
- Knösel, M.; Klang, E.; Helms, H.-J.; Wiechmann, D. Occurrence and severity of enamel decalcification adjacent to bracket bases and sub-bracket lesions during orthodontic treatment with two different lingual appliances. Eur. J. Orthod. 2016, 38, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Davari, A.; Yassaei, S.; Karandish, M.; Zarghami, F. In vitro Evaluation of Microleakage under Ceramic and Metal Brackets Bonded with LED and Plasma Arc Curing. J. Contemp. Dent. Pract. 2012, 13, 644–649. [Google Scholar] [CrossRef] [PubMed]
- Benson, P.E.; Parkin, N.; Dyer, F.; Millett, D.T.; Germain, P. Fluorides for preventing early tooth decay (demineralised lesions) during fixed brace treatment. Cochrane Database Syst. Rev. 2019, 2019, CD003809. [Google Scholar] [CrossRef]
- Millett, D.T.; Glenny, A.-M.; Mattick, R.C.; Hickman, J.; Mandall, N.A. Adhesives for fixed orthodontic bands. Cochrane Database Syst. Rev. 2016, 2016, CD004485. [Google Scholar] [CrossRef]
- Mandall, N.A.; Hickman, J.; Macfarlane, T.V.; Mattick, R.C.; Millett, D.T.; Worthington, H.V. Adhesives for fixed orthodontic brackets. Cochrane Database Syst. Rev. 2018, 2018, CD002282. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Li, C.; Li, F.; Chen, J.; Sun, J.; Zou, S.; Sandham, A.; Xu, Q.; Riley, P.; Ye, Q. Enamel etching for bonding fixed orthodontic braces. Cochrane Database Syst. Rev. 2013, 2018, CD005516. [Google Scholar] [CrossRef] [PubMed]
- Millett, D.T.; Mandall, N.A.; Mattick, R.C.; Hickman, J.; Glenny, A.-M. Adhesives for bonded molar tubes during fixed brace treatment. Cochrane Database Syst. Rev. 2017, 2017, CD008236. [Google Scholar] [CrossRef] [PubMed]
- Pereira-Cenci, T.; Cenci, M.S.; Fedorowicz, Z.; Azevedo, M. Antibacterial agents in composite restorations for the prevention of dental caries. Cochrane Database Syst. Rev. 2013, 2014, CD007819. [Google Scholar] [CrossRef]
- Metin-Gürsoy, G.; Uzuner, F.D. The Relationship between Orthodontic Treatment and Dental Caries. In Dental Caries-Diagnosis, Prevention and Management; Zühre Akarslan, IntechOpen: London, UK, 2018; pp. 41–52. [Google Scholar] [CrossRef]
- Jose, J.E.; Padmanabhan, S.; Chitharanjan, A.B. Systemic consumption of probiotic curd and use of probiotic toothpaste to reduce Streptococcus mutans in plaque around orthodontic brackets. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 67–72. [Google Scholar] [CrossRef]
- Uzuner, F.D.; Kaygısız, E.; Çankaya, Z.T. Effect of the bracket types on microbial colonization and periodontal status. Angle Orthod. 2014, 84, 1062–1067. [Google Scholar] [CrossRef]
- Munjal, D. Assessment of White Spot Lesions and In-Vivo Evaluation of the Effect of CPP-ACP on White Spot Lesions in Permanent Molars of Children. J. Clin. Diagn. Res. 2016, 10, 149–154. [Google Scholar] [CrossRef]
- Aljehani, A.; Tranæus, S.; Forsberg, C.-M.; Angmar-Mansson, B.; Shi, X.-O. In vitro quantification of white spot enamel lesions adjacent to fixed orthodontic appliances using quantitative light-induced fluorescence and diagnodent. Acta Odontol. Scand. 2004, 62, 313–318. [Google Scholar] [CrossRef]
- Livas, C.; Kuijpers-Jagtman, A.M.; Bronkhorst, E.; Derks, A.; Katsaros, C. Quantification of White Spot Lesions around Orthodontic Brackets with Image Analysis. Angle Orthod. 2008, 78, 585–590. [Google Scholar] [CrossRef]
- Butera, A.; Pascadopoli, M.; Gallo, S.; Lelli, M.; Tarterini, F.; Giglia, F.; Scribante, A. SEM/EDS Evaluation of the Mineral Deposition on a Polymeric Composite Resin of a Toothpaste Containing Biomimetic Zn-Carbonate Hydroxyapatite (microRepair®) in Oral Environment: A Randomized Clinical Trial. Polymers 2021, 13, 2740. [Google Scholar] [CrossRef]
- Scribante, A.; Farahani, M.R.D.; Marino, G.; Matera, C.; Baena, R.R.Y.; Lanteri, V.; Butera, A. Biomimetic Effect of Nano-Hydroxyapatite in Demineralized Enamel before Orthodontic Bonding of Brackets and Attachments: Visual, Adhesion Strength, and Hardness in In Vitro Tests. BioMed Res. Int. 2020, 2020, 6747498. [Google Scholar] [CrossRef] [PubMed]
- Roveri, N.; Marco, L.; Marchisio, O.; Ismaela, F.; Genovesi, A.; Montebugnoli, G.; Massimo, M.; Ugo, C. Different corrosive effects on hydroxyapatite nanocrystals and amine fluoride-based mouthwashes on dental titanium brackets: A comparative in vitro study. Int. J. Nanomed. 2013, 8, 307–314. [Google Scholar] [CrossRef]
- Vano, M.; Derchi, G.; Barone, A.; Pinna, R.; Usai, P.; Covani, U. Reducing dentine hypersensitivity with nano-hydroxyapatite toothpaste: A double-blind randomized controlled trial. Clin. Oral Investig. 2018, 55, 261–320. [Google Scholar] [CrossRef] [PubMed]
- Lanteri, V.; Segu, M.; Doldi, J.; Butera, A. Pre-bonding prophylaxis and brackets detachment: An experimental comparison of different methods. Int. J. Clin. Dent. 2014, 7, 191–197. [Google Scholar]
- Butera, A.; Gallo, S.; Pascadopoli, M.; Montasser, M.A.; Abd El Latief, M.H.; Modica, G.G.; Scribante, A. Home Oral Care with Biomimetic Hydroxyapatite vs. Conventional Fluoridated Toothpaste for the Remineralization and Desensitizing of White Spot Lesions: Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2022, 19, 8676. [Google Scholar] [CrossRef]
- Shan, D.; He, Y.; Gao, M.; Liu, H.; Zhu, Y.; Liao, L.; Hadaegh, F.; Long, H.; Lai, W. A comparison of resin infiltration and microabrasion for postorthodontic white spot lesion. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 516–522. [Google Scholar] [CrossRef] [PubMed]
- Simon, L.S.; Dash, J.K.; Deepika, U.; Philip, S.; Sarangi, S. Management of Post Orthodontic White Spot Lesions Using Resin Infiltration and CPP-ACP Materials- A Clinical Study. J. Clin. Pediatr. Dent. 2022, 46, 70–74. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).