Eruption Pattern of Third Molars in Orthodontic Patients Treated with First Permanent Molar Extraction: A Longitudinal Retrospective Evaluation
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kühnisch, J.; Heitmüller, D.; Thiering, E.; Brockow, I.; Hoffmann, U.; Neumann, C.; Heinrich-Weltzien, R.; Bauer, C.P.; von Berg, A.; Koletzko, S.; et al. Proportion and extent of manifestation of molar-incisor-hypomineralizations according to different phenotypes. J. Public Health Dent. 2014, 74, 42–49. [Google Scholar] [CrossRef]
- Jälevik, B. Prevalence and diagnosis of molar-incisor-hypomineralisation (MIH): A systematic review. Eur. Arch. Paediatr. Dent. 2010, 11, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Elhennawy, K.; Schwendicke, F. Managing molar-incisor-hypomineralization: A systematic review. J. Dent. 2016, 55, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Stennett, M.; Tsakos, G. The impact of the COVID-19 pandemic on oral health inequalities and access to oral healthcare in England. Br. Dent. J. 2022, 232, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Bishara, S.E.; Andreasen, G. Third molars: A review. Am. J. Orthod. 1983, 83, 131–137. [Google Scholar] [CrossRef]
- Dachi, S.F.; Howell, F.V. A survey of 3874 routine full-mouth radiographs. I. A study of retained roots and teeth. Oral Surg. Oral Med. Oral Pathol. 1961, 14, 916–924. [Google Scholar] [CrossRef]
- Carter, K.; Worthington, S. Predictors of Third Molar Impaction: A systematic review and meta-analysis. J. Dent. Res. 2016, 95, 267–276. [Google Scholar] [CrossRef]
- Song, F.; O’Meara, S.; Wilson, P.; Golder, S.; Kleijnen, J. The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth. Health Technol. Assess 2000, 4, 1–55. [Google Scholar] [CrossRef]
- Bayram, M.; Özer, M.; Arici, S. Effects of first molar extraction on third molar angulation and eruption space. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, 14–20. [Google Scholar] [CrossRef]
- Richardson, M.E.; Dent, M. Some aspects of lower third molar eruption. Angle Orthod. 1974, 44, 141–145. [Google Scholar] [CrossRef]
- Yavuz, I.; Baydas, B.; Ikbal, A.; Dagsuyu, I.M.; Ceylan, I. Effects of early loss of permanent first molars on the development of third molars. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 634–638. [Google Scholar] [CrossRef] [PubMed]
- Livas, C.; Halazonetis, D.J.; Booij, J.W.; Katsaros, C. Extraction of maxillary first molars improves second and third molar inclinations in class II division 1 malocclusion. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 377–382. [Google Scholar] [CrossRef]
- Livas, C.; Pandis, N.; Booij, J.W.; Halazonetis, D.J.; Katsaros, C.; Ren, Y. Influence of unilateral maxillary first molar extraction treatment on second and third molar inclination in class II subdivision patients. Angle Orthod. 2016, 86, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Ay, S.; Agar, U.; Bicakci, A.A.; Kosger, H.H. Changes in mandibular third molar angle and position after unilateral mandibular first molar extraction. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Türköz, C.; Ulusoy, C. Effect of premolar extraction on mandibular third molar impaction in young adults. Angle Orthod. 2013, 83, 572–577. [Google Scholar] [CrossRef] [PubMed]
- Årtun, J.; Behbehani, F.; Thalib, L. Prediction of maxillary third molar impaction in adolescent orthodontic patients. Angle Orthod. 2005, 75, 904–911. [Google Scholar] [CrossRef]
- Capelli, J., Jr. Mandibular growth and third molar impaction in extraction cases. Angle Orthod. 1991, 61, 223–229. [Google Scholar] [CrossRef]
- Demirel, O.; Akbulut, A. Evaluation of the relationship between gonial angle and impacted mandibular third molar teeth. Anat Sci. Int. 2020, 95, 134–142. [Google Scholar] [CrossRef]
- Breik, O.; Grubor, D. The incidence of mandibular third molar impactions in different skeletal face types. Aust. Dent. J. 2008, 53, 320–324. [Google Scholar] [CrossRef]
- Demirjian, A.; Goldstein, H.; Tanner, J.M. A new system of dental age assessment. Hum. Biol. 1973, 45, 211–227. [Google Scholar]
- Miclotte, A.; Grommen, B.; Cadenas de Llano-Perula, M.; Verdonck, A.; Jacobs, R.; Willems, G. The effect of first and second premolar extractions on third molars: A retrospective longitudinal study. J. Dent. 2017, 61, 55–66. [Google Scholar] [CrossRef]
- Lim, A.A.; Wong, C.W.; Allen, J.C., Jr. Maxillary third molar: Patterns of impaction and their relation to oroantral perforation. J. Oral Maxillofac. Surg. 2012, 70, 1035–1039. [Google Scholar] [CrossRef] [PubMed]
- Archer, W.H. Oral and Maxillofacial Surgery, 5th ed.; Saunders: Philadelphia, PA, USA, 1975; pp. 137–142. [Google Scholar]
- Winter, G.B. Principles of Exodontia as Applied to the Impacted Third Molar; American Medical Book Company: St. Louis, MO, USA, 1926; pp. 42–83. [Google Scholar]
- Pell, G.J.; Gregory, G.T. Impacted mandibular third molars: Classification and modified technique for removal. Dent. Dig. 1933, 39, 330–338. [Google Scholar]
- Rivera-Herrera, R.S.; Esparza-Villalpando, V.; Bermeo-Escalona, J.R.; Martinez-Rider, R.; Pozos-Guillen, A. Agreement analysis of three mandibular third molar retention classifications. Gac. Med. Mex. 2020, 156, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Garg, N.; Jain, A.K.; Saha, S.; Singh, J. Essentiality of early diagnosis of molar incisor hypomineralization in children and review of its clinical presentation, etiology and management. Int. J. Clin. Pediatr. Dent. 2012, 5, 190–196. [Google Scholar] [CrossRef]
- de Farias, A.L.; Rojas-Gualdrón, D.F.; Girotto Bussaneli, D.; Santos-Pinto, L.; Mejía, J.D.; Restrepo, M. Does molar-incisor hypomineralization (MIH) affect only permanent first molars and incisors? New observations on permanent second molars. Int. J. Paediatr. Dent. 2022, 32, 1–10. [Google Scholar] [CrossRef]
- Elhennawy, K.; Jost-Brinkmann, P.G.; Manton, D.J.; Paris, S.; Schwendicke, F. Managing molars with severe molar-incisor hypomineralization: A cost-effectiveness analysis within German healthcare. J. Dent. 2017, 63, 65–71. [Google Scholar] [CrossRef]
- Behbehani, F.; Årtun, J.; Thalib, L. Prediction of mandibular third-molar impaction in adolescent orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 47–55. [Google Scholar] [CrossRef]
- Jälevik, B.; Möller, M. Evaluation of spontaneous space closure and development of permanent dentition after extraction of hypomineralized permanent first molars. Int. J. Paediatr. Dent. 2007, 17, 328–335. [Google Scholar] [CrossRef]
- Brusevold, I.J.; Kleivene, K.; Grimsøen, B.; Skaare, A.B. Extraction of first permanent molars severely affected by molar incisor hypomineralisation: A retrospective audit. Eur. Arch. Paediatr. Dent. 2022, 23, 89–95. [Google Scholar] [CrossRef]
- Patel, S.; Ashley, P.; Noar, J. Radiographic prognostic factors determining spontaneous space closure after loss of the permanent first molar. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 718–726. [Google Scholar] [CrossRef]
- Teo, T.K.; Ashley, P.F.; Parekh, S.; Noar, J. The evaluation of spontaneous space closure after the extraction of first permanent molars. Eur. Arch. Paediatr. Dent. 2013, 14, 207–212. [Google Scholar] [CrossRef]
- Eichenberger, M.; Erb, J.; Zwahlen, M.; Schätzle, M. The timing of extraction of non-restorable first permanent molars: A systematic review. Eur. J. Paediatr. Dent. 2015, 16, 272–278. [Google Scholar]
- Liversidge, H.M. Timing of human mandibular third molar formation. Ann. Hum. Biol. 2008, 35, 294–321. [Google Scholar] [CrossRef]
- Libdy, M.R.; Rabello, N.M.; Marques, L.S.; Normando, D. The ability of orthodontists and maxillofacial surgeons in predicting spontaneous eruption of mandibular third molar using panoramic serial radiographs. Dent. Press. J. Orthod. 2020, 25, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Cobourne, M.T.; Williams, A.; Harrison, M. National clinical guidelines for the extraction of first permanent molars in children. Br. Dent. J. 2014, 217, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, C.; Jacobs-Müller, C.; Luley, C.; Erbe, C.; Wehrbein, H. Orthodontic space closure after first molar extraction without skeletal anchorage. J. Orofac. Orthop. 2011, 72, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Janson, G.; Carvalho, P.E.; Cancado, R.H.; de Freitas, M.R.; Henriques, J.F. Cephalometric evaluation of symmetric and asymmetric extraction treatment for patients with class II subdivision malocclusions. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 28–35. [Google Scholar] [CrossRef]
- Sabri, R. Multidisciplinary management of permanent first molar extractions. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 682–692. [Google Scholar] [CrossRef] [PubMed]
- Isomura, E.T.; Kurushima, Y.; Kobashi, H.; Enoki, K.; Yamashita, M.; Ikebe, K. Factors influencing the localization of mandibular third molars in twins. J. Oral Maxillofac. Surg. 2020, 78, 1279–1287. [Google Scholar] [CrossRef] [PubMed]
- Tronje, G.; Welander, U.; McDavid, W.D.; Morris, C.R. Image distortion in rotational panoramic radiography. IV. Object morphology; outer contours. Acta Radiol. Diagn. 1981, 22, 689–696. [Google Scholar] [CrossRef]
- Tronje, G.; Welander, U.; McDavid, W.D.; Morris, C.R. Image distortion in rotational panoramic radiography. III. Inclined objects. Acta Radiol. Diagn. 1981, 22, 585–592. [Google Scholar] [CrossRef]
- Kumar, S.S.; Thailavathy, V.; Srinivasan, D.; Loganathan, D.; Yamini, J. Comparison of orthopantomogram and lateral cephalogram for mandibular measurements. J. Pharm. Bioallied. Sci. 2017, 9, 92–95. [Google Scholar] [CrossRef]
- Larheim, T.A.; Svanaes, D.B. Reproducibility of rotational panoramic radiography: Mandibular linear dimensions and angles. Am. J. Orthod. Dentofac. Orthop. 1986, 90, 45–51. [Google Scholar] [CrossRef]
- Gohilot, A.; Pradhan, T.; Keluskar, K.M. Effects of first premolar extraction on maxillary and mandibular third molar angulation after orthodontic therapy. J. Oral Biol. Craniofac. Res. 2012, 2, 97–104. [Google Scholar] [CrossRef]
- Janson, G.; Putrick, L.M.; Henriques, J.F.; de Freitas, M.R.; Henriques, R.P. Maxillary third molar position in class II malocclusions: The effect of treatment with and without maxillary premolar extractions. Eur. J. Orthod. 2006, 28, 573–579. [Google Scholar] [CrossRef]
- Jain, S.; Valiathan, A. Influence of first premolar extraction on mandibular third molar angulation. Angle Orthod. 2009, 79, 1143–1148. [Google Scholar] [CrossRef] [PubMed]
- Nanda, R.S.; Merrill, R.M. Cephalometric assessment of sagittal relationship between maxilla and mandible. Am. J. Orthod. Dentofac. Orthop. 1994, 105, 328–344. [Google Scholar] [CrossRef]
- Li, J.L.; Kau, C.; Wang, M. Changes of occlusal plane inclination after orthodontic treatment in different dentoskeletal frames. Prog. Orthod. 2014, 15, 41. [Google Scholar] [CrossRef] [PubMed]
- Ferrario, V.F.; Sforza, C.; Colombo, A.; Ciusa, V.; Serrao, G. Three-dimensional inclination of the dental axes in healthy permanent dentitions--A cross-sectional study in a normal population. Angle Orthod. 2001, 71, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Tassoker, M.; Kok, H.; Sener, S. Is there a possible association between skeletal face types and third molar impaction? A retrospective radiographic study. Med. Princ. Pr. 2019, 28, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Barone, S.; Antonelli, A.; Averta, F.; Diodati, F.; Muraca, D.; Bennardo, F.; Giudice, A. Does mandibular gonial angle influence the eruption pattern of the lower third molar? A three-dimensional study. J. Clin. Med. 2021, 10, 4057. [Google Scholar] [CrossRef]
- Nguyen, A.; Caplin, J.; Avenetti, D.; Durfee, S.; Kusnoto, B.; Sciote, J.J.; Nicholas, C.L. A longitudinal assessment of sex differences in the growth of the mandibular retromolar space. Arch. Oral Biol. 2022, 143, 105547. [Google Scholar] [CrossRef]
- Chen, K.; Han, X.; Huang, L.; Bai, D. Tooth movement after orthodontic treatment with 4 second premolar extractions. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 770–777. [Google Scholar] [CrossRef]
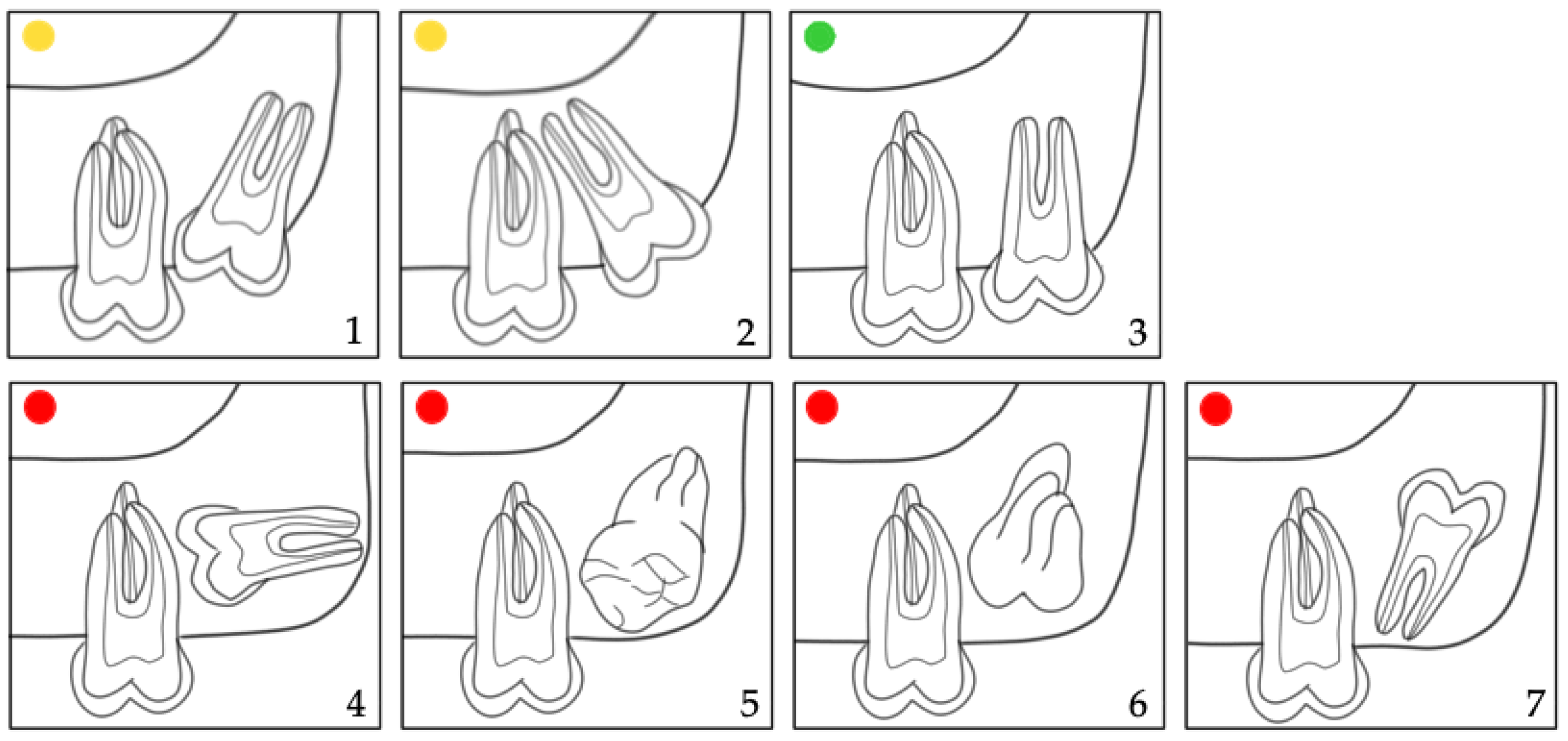
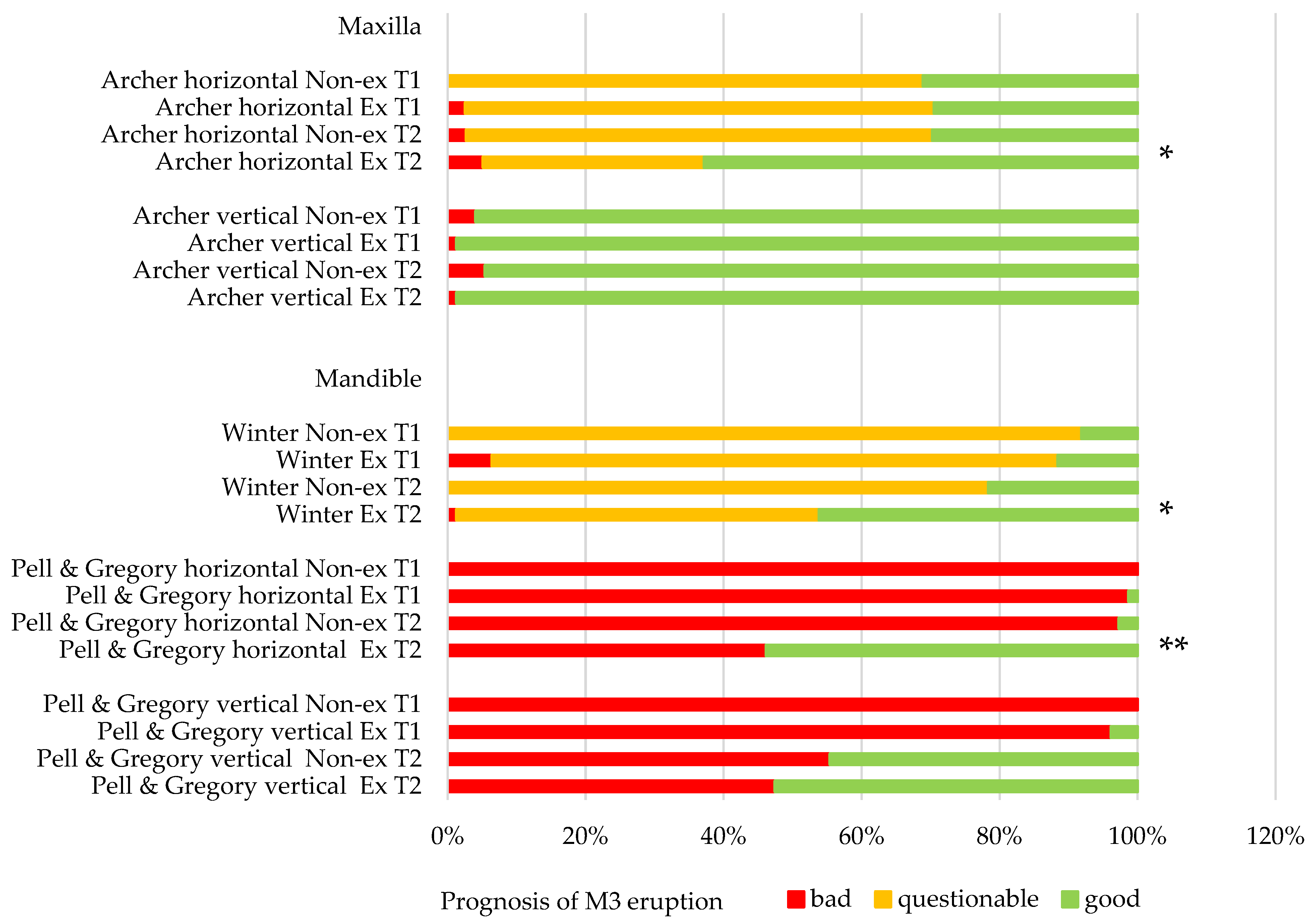
 ); 3: good (
); 3: good ( ); 4–7: bad prognosis (
); 4–7: bad prognosis ( ).
).
 ); 3: good (
); 3: good ( ); 4–7: bad prognosis (
); 4–7: bad prognosis ( ).
).
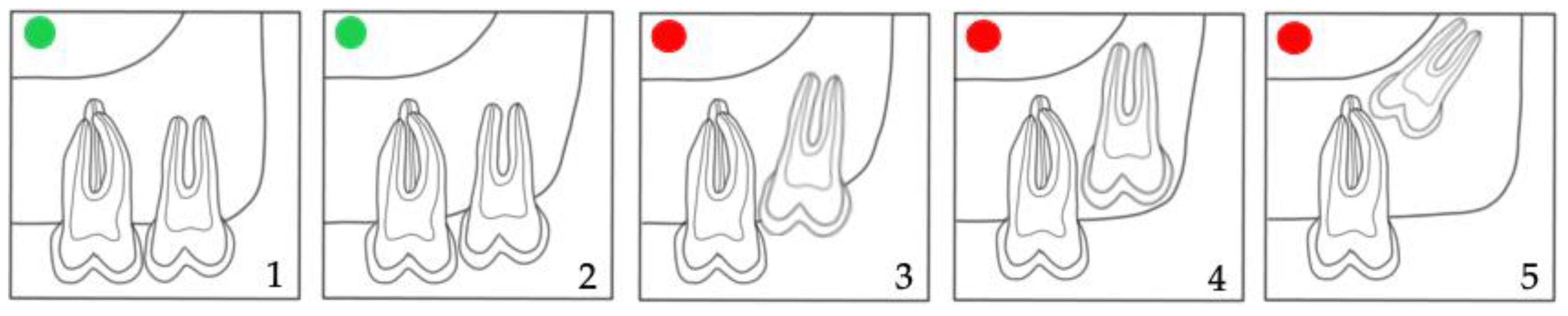
 ); 3–5: bad prognosis (
); 3–5: bad prognosis ( ).
).
 ); 3–5: bad prognosis (
); 3–5: bad prognosis ( ).
).
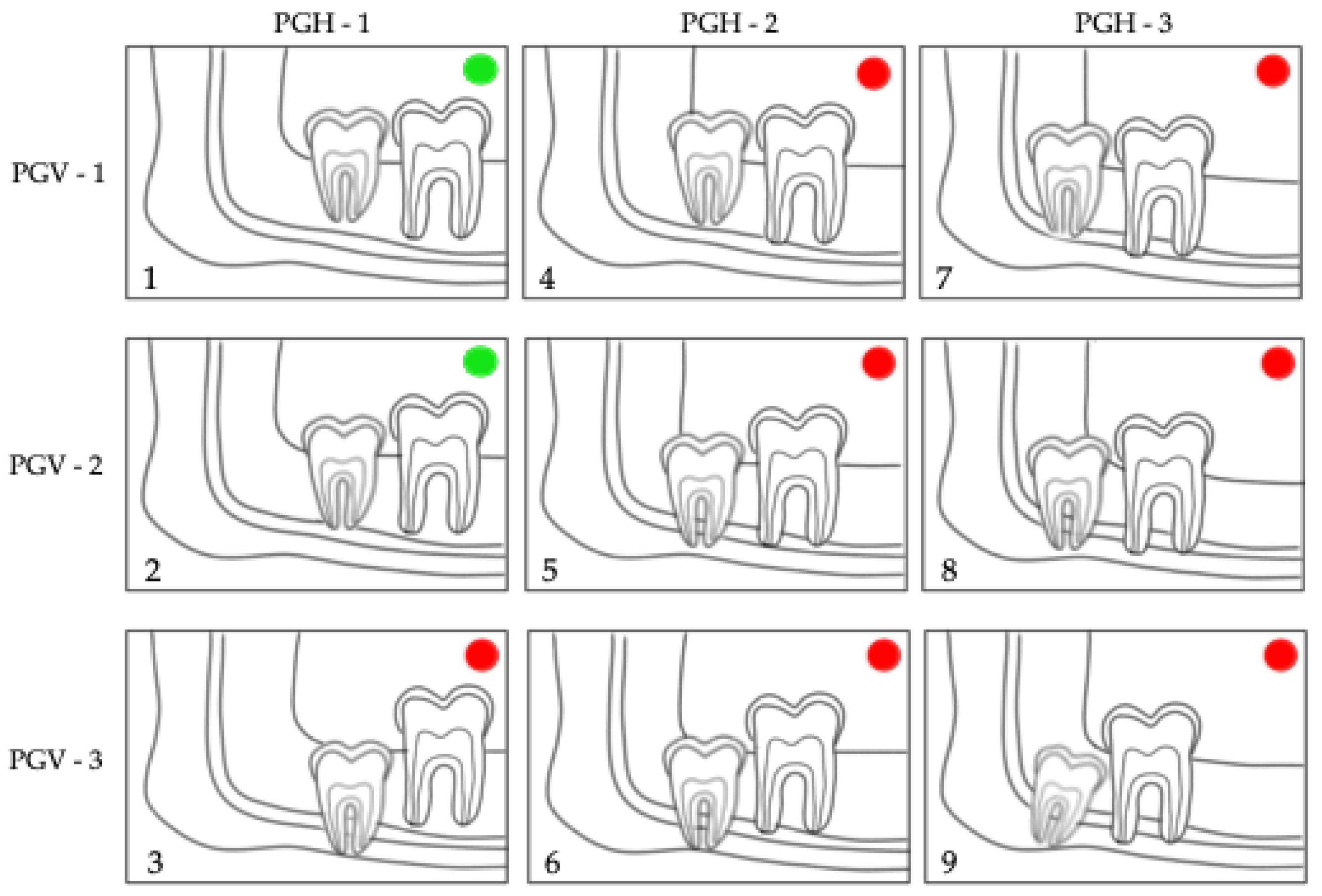
 ); 3,4: questionable (
); 3,4: questionable ( ); 2,5,6: bad prognosis (
); 2,5,6: bad prognosis ( ).
).
 ); 3,4: questionable (
); 3,4: questionable ( ); 2,5,6: bad prognosis (
); 2,5,6: bad prognosis ( ).
).
 ); 3–9: bad prognosis (
); 3–9: bad prognosis ( ).
).
 ); 3–9: bad prognosis (
); 3–9: bad prognosis ( ).
).
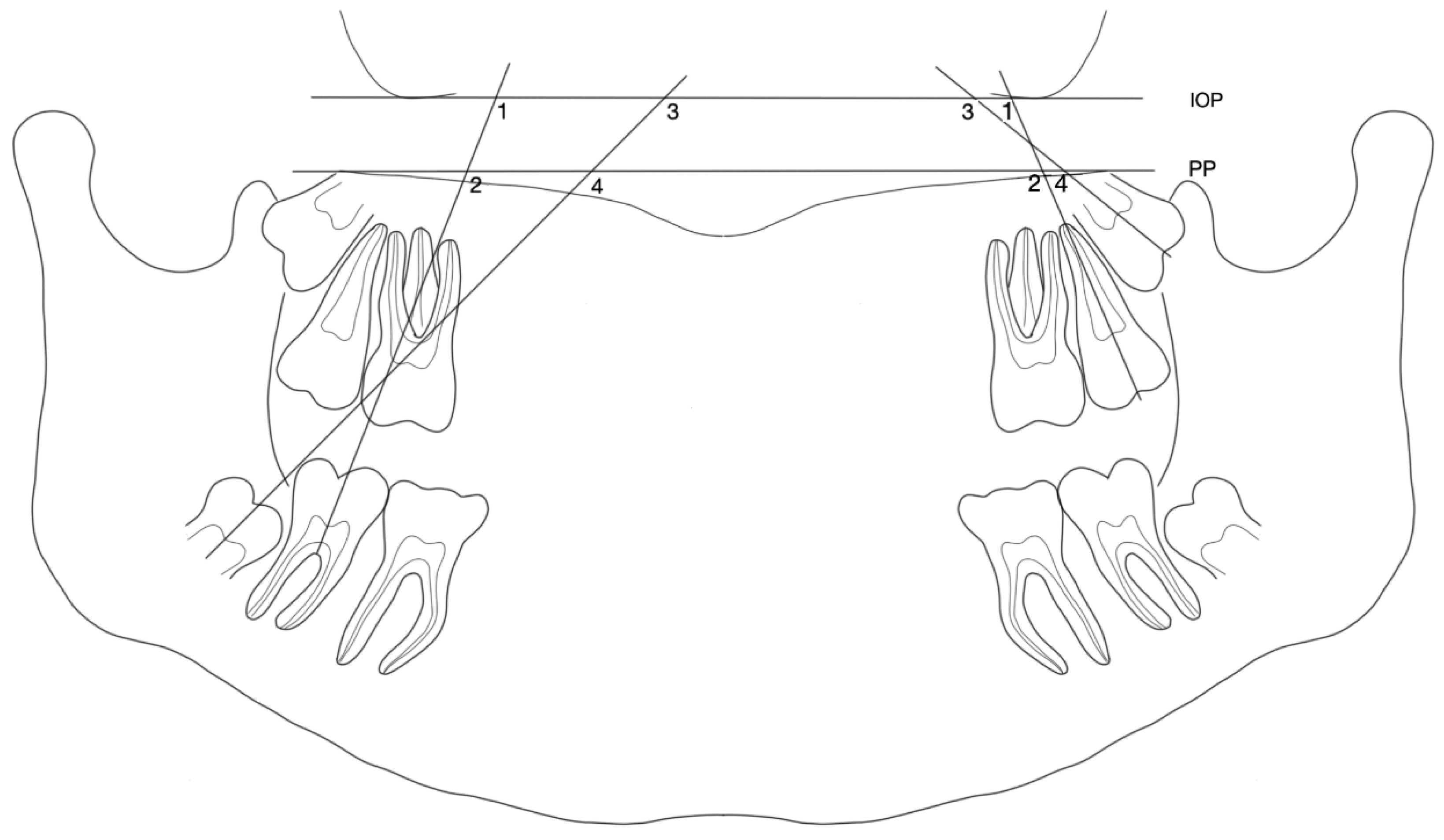
 , M3:
, M3:  ) and extraction (Ex): (M2:
) and extraction (Ex): (M2:  , M3:
, M3:  ) groups. (a) maxillary M2/PP and M3/PP; (b) maxillary M3/IOP and M3/IOP; (c) mandibular M2/PP and M3/PP; (d) mandibular M2/IOP and M3/IOP.
) groups. (a) maxillary M2/PP and M3/PP; (b) maxillary M3/IOP and M3/IOP; (c) mandibular M2/PP and M3/PP; (d) mandibular M2/IOP and M3/IOP.
 , M3:
, M3:  ) and extraction (Ex): (M2:
) and extraction (Ex): (M2:  , M3:
, M3:  ) groups. (a) maxillary M2/PP and M3/PP; (b) maxillary M3/IOP and M3/IOP; (c) mandibular M2/PP and M3/PP; (d) mandibular M2/IOP and M3/IOP.
) groups. (a) maxillary M2/PP and M3/PP; (b) maxillary M3/IOP and M3/IOP; (c) mandibular M2/PP and M3/PP; (d) mandibular M2/IOP and M3/IOP.
| Non-Extraction (n = 37) | Extraction (n = 39) | ||
|---|---|---|---|
| Sex (n (%)) | female | 23 (62.16) | 24 (61.54) |
| male | 14 (37.84) | 15 (38.46) | |
| Age pretreatment (years) | mean | 14.5 | 13.5 |
| range | 9.6–19.4 | 11.8–15.3 | |
| Age post-treatment (years) | mean | 16.2 | 16.2 |
| range | 11.2–21.1 | 14.4–18.0 | |
| Treatment duration (years) | mean | 1.65 | 2.99 |
| Angle classification (n (%)) | Class I | 11 (29.73) | 18 (46.15) |
| Class II | 22 (59.46) | 13 (33.33) | |
| Class III | 4 (10.81) | 8 (20.52) | |
| Skeletal classification (n (%)) | Class I | 10 (27.03) | 15 (38.46) |
| Class II | 20 (54.05) | 15 (38.46) | |
| Class III | 7 (18.92) | 9 (23.08) | |
| Growth pattern (n (%)) | neutral | 18 (48.65) | 14 (35.90) |
| vertical | 2 (5.40) | 12 (30.77) | |
| horizontal | 17 (45.95) | 13 (33.33) |
| T1 Mean (sd) | T2 Mean (sd) | Coefficient (95% CI) | p-Value | ||
|---|---|---|---|---|---|
| Maxilla | |||||
| M2/IOP | Non-ex | 111.2° (8.9) | 102.8° (7.5) | Reference | |
| Ex | 109.6° (9.4) | 93.6° (7.6) | −8.72 (−11.38, −6.07) | <0.001 ** | |
| M2/PP | Non-ex | 111.4° (8.9) | 102.9° (7.6) | Reference | |
| Ex | 109.8° (9.4) | 93.6° (7.6) | −8.83 (−11.51, 6.15) | <0.001 ** | |
| M3/IOP | Non-ex | 122.6° (11.6) | 111.0° (12.8) | Reference | |
| Ex | 124.0° (16.3) | 101.3° (10.1) | −10.17 (−14.21, 6.13) | <0.001 ** | |
| M3/PP | Non-ex | 122.6° (11.6) | 110.9° (12.8) | Reference | |
| Ex | 124.0° (16.3) | 101.3° (10.2) | −10.04 (−14.14, 5.95) | <0.001 ** | |
| Mandible | |||||
| M2/IOP | Non-ex | 112.5° (8.2) | 106.2° (6.0) | Reference | |
| Ex | 117.7° (10.4) | 108.5° (8.0) | 0.73 (−1.65, 3.11) | 0.55 | |
| M2/PP | Non-ex | 112.7° (8.4) | 106.4° (6.0) | Reference | |
| Ex | 117.9° (10.5) | 108.1 (8.2) | 0.72 (−2.17, 2.72) | 0.83 | |
| M3/IOP | Non-ex | 138.9° (11.2) | 129.2° (12.4) | Reference | |
| Ex | 144.6° (13.6) | 127.8° (13.0) | −4.03 (−8.23, 0.17) | 0.06 | |
| M3/PP | Non-ex | 139.0° (11.1) | 129.3° (12.2) | Reference | |
| Ex | 144.5° (13.5) | 127.7° (13.2) | −4.20 (−8.38, −0.02) | 0.05 |
| Archer Horizontal | Archer Vertical | Winter | Pell & Gregory Horizontal | Pell & Gregory Vertical | ||
|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| Group | Non-ex (Reference) | |||||
| Ex | 1.96 * | 21.79 | 1.92 | 2234.22 * | 2.35 | |
| (1.04, 3.72) | (0.17, 2786.99) | (0.40, 9.15) | (11.35, 439,962.1) | (0.62, 8.94) | ||
| Time | T1 (Reference) | |||||
| T2 | 1.71 | 0.28 | 23.93 ** | 5459.58 * | 509.77 ** | |
| (0.91, 3.23) | (0.01, 10.21) | (3.56, 152.23) | (16.53, 1,802,824) | (39.66, 6522.06) | ||
| Sex | Female (Reference) | |||||
| Male | 0.66 | 0.55 | 4.16 | 6.55 | 2.54 | |
| (0.34, 1.29) | (0.02, 15.94) | (0.78, 23.32) | (0.41, 105.77) | (0.65, 10.02) | ||
| Crowding | No crowding (Reference) | |||||
| <3 mm | 0.93 | 1.67 | 1.10 | 14.46 | 3.44 | |
| (0.46, 1.85) | (0.04, 69.99) | (0.20, 6.14) | (0.61, 343.72) | (0.78, 15.26) | ||
| 3–5 mm | 0.46 | 0.49 | 0.68 | 77.98 | 5.53 | |
| (0.16, 1.32) | (0.01, 42.03) | (0.05, 8.95) | (0.78, 8482.21) | (0.68, 44.92) | ||
| >5 mm | 0.98 | 1.50 × 1013 | 0.004 * | 0.24 | 24.32 | |
| (0.14, 6.78) | (0, non-estimable) | (0.0002, 0.95) | (0.47, 186,379.3) | (0.40, 1475.36) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Langer, L.J.; Pandis, N.; Mang de la Rosa, M.R.; Jost-Brinkmann, P.-G.; Bartzela, T.N. Eruption Pattern of Third Molars in Orthodontic Patients Treated with First Permanent Molar Extraction: A Longitudinal Retrospective Evaluation. J. Clin. Med. 2023, 12, 1060. https://doi.org/10.3390/jcm12031060
Langer LJ, Pandis N, Mang de la Rosa MR, Jost-Brinkmann P-G, Bartzela TN. Eruption Pattern of Third Molars in Orthodontic Patients Treated with First Permanent Molar Extraction: A Longitudinal Retrospective Evaluation. Journal of Clinical Medicine. 2023; 12(3):1060. https://doi.org/10.3390/jcm12031060
Chicago/Turabian StyleLanger, Lisa J., Nikolaos Pandis, Maria R. Mang de la Rosa, Paul-Georg Jost-Brinkmann, and Theodosia N. Bartzela. 2023. "Eruption Pattern of Third Molars in Orthodontic Patients Treated with First Permanent Molar Extraction: A Longitudinal Retrospective Evaluation" Journal of Clinical Medicine 12, no. 3: 1060. https://doi.org/10.3390/jcm12031060
APA StyleLanger, L. J., Pandis, N., Mang de la Rosa, M. R., Jost-Brinkmann, P.-G., & Bartzela, T. N. (2023). Eruption Pattern of Third Molars in Orthodontic Patients Treated with First Permanent Molar Extraction: A Longitudinal Retrospective Evaluation. Journal of Clinical Medicine, 12(3), 1060. https://doi.org/10.3390/jcm12031060






