Abstract
Background: Dyslipidemia has been suggested to be associated with the occurrence of dry eye disease (DED). However, whether dyslipidemia is responsible for the development of DED remains unclear. In this systematic review, we explored the relationship between DED and dyslipidemia by using quantitative data. Methods: Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, we conducted a comprehensive literature search in several databases, including PubMed, Embase, Cochrane Library, Web of Science, and Google Scholar, and obtained six relevant studies. Results: Our findings indicated that the majority of the selected studies reported a statistically significant association between dyslipidemia and DED, particularly in women. However, our quantitative analysis revealed that only two studies reported statistically significant differences in total cholesterol and high-density lipoprotein cholesterol values. Conclusion: No statistically significant differences exist in the majority of lipid profile parameters between individuals with and without DED, but there is a statistically significant association between dyslipidemia and DED.
1. Introduction
Dry eye disease (DED) is a chronic and multifactorial condition that progressively affects a significant number of individuals worldwide. This condition is also exacerbated by the prolonged and frequent use of visual display terminals and excessive occupational exposure to toxic agents, such as fire, smoke, dust, and airborne particles [1,2,3,4]. With a continuously increasing prevalence of approximately 7% to 33%, DED has been identified as a critical worldwide public health problem [5], placing a substantial burden on public health sectors [6,7].
The primary hallmark of DED is the disruption of the tear film, resulting in reduced aqueous tear flow and excessive evaporation [8]. As shown in Figure 1, the tear film consists of lipid, aqueous, and mucin layers [9,10]. The lipid layer plays a major role in maintaining a smooth corneal surface, preventing rapid evaporation from the eye [11], and protecting the eye against environmental stressors. This layer primarily contains secretions from the meibomian glands [12], with cholesterol and cholesterol esters serving as key components [13]. Because the meibomian glands play a crucial role in regulating lipid secretion within the eyelids, systemic dyslipidemia, characterized by increased levels of total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), and triglycerides (TGs) and decreased levels of high-density lipoprotein cholesterol (HDL-C), may influence the development of DED.
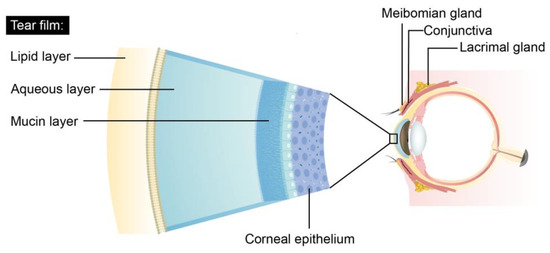
Figure 1.
The three layers of the tear film.
Many epidemiological studies have indicated a correlation between elevated cholesterol levels and meibomian gland dysfunction (MGD), a key factor in the pathogenesis of DED [14]. However, the independent relationship between dyslipidemia and DED still remains under debate and has not been rigorously studied. Given the increasing number of individuals affected by DED, ophthalmologists must investigate the association between dyslipidemia and DED to provide further insights. Because of the inconclusive nature of the relationship between dyslipidemia and DED [15,16,17], we conducted a systematic review to consolidate the existing data and clarify the existing debate. We hope that this systematic review will contribute to future clinical practices associated with the early diagnosis and treatment of DED and will provide valuable guidance in this field.
2. Materials and Methods
2.1. Search Strategy and Data Retrieval Protocol
We conducted a systematic literature review using various electronic databases, including PubMed, Embase, Cochrane Library, Web of Science, and Google Scholar, from their inception until March 2023. We used the following terms to search for publications on DED and dyslipidemia: “dyslipidemia” AND “dry eye”, “hyperlipidemia” AND “dry eye”, “cholesterol” AND “dry eye”. “hypercholesterolemia” AND “dry eye”, “triglyceride” AND “dry eye”, “hypertriglyceridemia” AND “dry eye”, “low-density lipoprotein” AND “dry eye”, and “high-density lipoprotein” AND “dry eye”. We then manually screened the reference lists of the selected articles to identify any potentially relevant publications that we may have missed.
In adherence to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria [18] and the International Prospective Register of Systematic Reviews (PROSPERO) guidelines [19], a structured and systematic search strategy was employed. The study selection process and evaluation outcomes are illustrated using a PRISMA flow diagram in Figure 2.
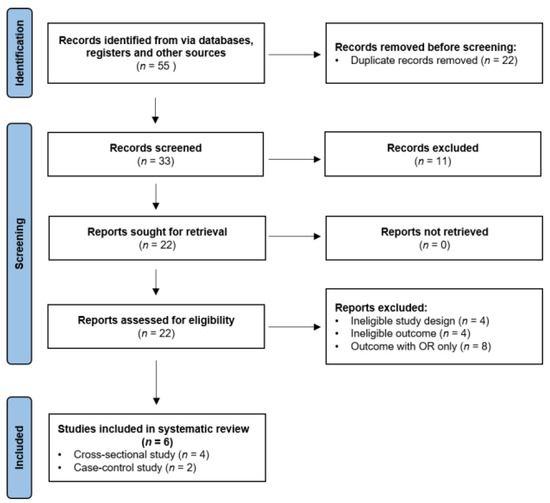
Figure 2.
PRISMA flow diagram of the study selection process and evaluation outcomes.
The initial search yielded 55 articles, 22 duplicates of which were removed. The remaining 33 articles were reviewed in terms of their titles and abstracts. After 11 articles that did not meet the inclusion criteria were excluded, the remaining 22 articles underwent full-text evaluation. Finally, following an eligibility evaluation, 6 articles were included and thoroughly examined.
2.2. Inclusion and Exclusion Criteria
Studies meeting the following criteria were included in this systematic review: (1) studies published in English, (2) studies involving peer-reviewed original research, (3) studies involving human participants, and (4) studies involving quantitative information on lipid profile parameters in individuals with and without DED. By contrast, studies meeting the following criteria were excluded from this systematic review: (1) studies reporting ineligible results, (2) studies focusing exclusively on MGD, and (3) studies possessing characteristics that contradict the aforementioned inclusion criteria. For more details, please refer to Table 1.

Table 1.
Inclusion and exclusion criteria.
3. Results
A total of six studies were included in this systematic review: four cross-sectional studies and two case–control studies. Table 2 provides a summary of the characteristics of the included studies.

Table 2.
Summary of the included studies regarding the relationship between DED and dyslipidemia.
3.1. Highlights of Each Study
In the following text, we discuss the results of each of the aforementioned studies in detail.
Chun et al. [20] conducted a cross-sectional study on 5627 adults aged over 19 years, including 531 with DED. The information of all medication use was collected. They observed no significant gender-related differences in lipid profiles between individuals with and without DED. However, they observed an increased prevalence of high TC and LDL-C levels in older women with DED, particularly in those aged above 65 years. Adjusted analysis revealed that these elevated TC and LDL-C levels were associated with an increased likelihood of DED. Interestingly, they observed that women with DED had a lower prevalence of low HDL-C compared with the controls. They also observed that the mean value of HDL-C was higher in patients with DED, although not significantly, than in the controls. Notably, the authors used a DED questionnaire survey to identify potential patients with DED.
Park et al. [21] examined the relationship between dry eye syndrome (DES) and metabolic syndrome among adults aged 19 years and above. They observed no significant gender-related differences in TG or HDL-C levels between individuals with and without DES. However, they observed a significant association between elevated TG levels and DES in women. After adjustment for confounding variables, they determined that, compared with their counterparts, women with elevated TGs were 1.13 times more likely to have DES. Notably, this study included a total of 15,294 individuals, of whom 2704 received a diagnosis of DES based on signs, symptoms, and comprehensive eye examinations involving a slit lamp. No records of the prescription medication use of the individuals were mentioned.
Rathnakumar et al. [22] reported statistically significant differences in all serum lipid profile parameters, except for VLDL-C, between individuals with and without DED. They observed that women exhibited significant differences in each parameter. In particular, they observed a statistically significant difference in TC levels (p < 0.001) among women with DED, with a mean value of 363 ± 19.05 mg/dL. Notably, this study included a total of 60 clinically diagnosed DED cases and age- and sex-matched healthy controls. They only excluded patients using antihypertensive drugs. DED was diagnosed using a questionnaire and clinical examinations, such as the tear breakup time (TBUT) test, Schirmer’s test, and slit-lamp biomicroscopy.
Choi et al. [23] reported a significantly increased prevalence of hypercholesterolemia among patients with DES (p < 0.008). This prevalence increased with the severity of DES (p < 0.002). Only HDL-C exhibited a significant difference between individuals with and without DES, with those with DES exhibiting increased mean levels of HDL-C. After adjustment for confounding variables, the authors observed that, compared with men without dyslipidemia, men with dyslipidemia were 1.40 times more likely to have DES. However, they observed no significant associations between dyslipidemia and DES in women, regardless of their menopausal status. Notably, this study included a total of 2272 individuals, of whom 1117 received a diagnosis of DES based on Ocular Surface Disease Index (OSDI) scores. They excluded 147 individuals who were taking lipid-lowering drugs.
Shokr et al. [25] investigated the presence of microvascular endothelial dysfunction as an indicator of early cardiovascular disease in patients with DED. They observed significant differences in TC and HDL-C levels between individuals with and without DED, with p values of 0.036 and 0.014, respectively. However, they observed no significant differences in the other lipid profile parameters. Notably, this study included a total of 50 individuals, half of whom received a diagnosis of DED based on criteria set by TFOS DEWS II. Patients with the positive diagnosis of dyslipidemia that required medical treatment were excluded from the study.
Choi et al. [26] examined a total of 475 individuals, of whom 230 had DES. Individuals using lipid-lowering medication were included in the study. They defined DES as an OSDI score greater than 13. They observed no statistically significant association between the prevalence of hypercholesterolemia and DES or its severity.
3.2. Quantitative Data Analysis
In our quantitative analysis, we collected lipid profile parameters from each of the aforementioned studies (see Table 3). Among these parameters, only three exhibited a statistically significant difference between individuals with and without DED. Shokr et al. [25] reported a significant difference in the mean values of TC and HDL-C, with p values of 0.036 and 0.014, respectively. Choi et al. [23] reported a significant difference in the mean value of HDL-C, with a p value of 0.050. However, none of the other studies reported a significant difference in the lipid profile parameters between individuals with and without DED.

Table 3.
Comparison of lipid profile parameters between individuals with and without DED.
4. Discussion
In this systematic review, the scope was expanded to emphasize the relationship between DED and systemic dyslipidemia. Our analysis demonstrated a statistically significant association between dyslipidemia and DED, with a prominence in women. We also extracted the quantitative lipid profile parameters from each included study. There were no statistically significant differences in the values of lipid profiles between DED and non-DED patients.
4.1. Higher Prevalence of Dyslipidemia in Female DED Patients
According to the results of the selected studies, dyslipidemia is statistically significantly associated with DED in both men and women. However, compared with men with DED, women with DED tend to exhibit a higher prevalence of dyslipidemia.
Rathnakumar et al. [22] reported that DED was more significantly associated with elevated TC levels in women (p < 0.001) than in men (p < 0.002). They reported significantly higher TG levels and altered lipoprotein profile parameters (TC, increased LDL-C, and decreased HDL-C) in women than in men, indicating the predominance of dyslipidemia in women. Park et al. [21] reported a significantly increased prevalence of elevated TG levels in women with DES. After adjustment for confounding variables, they only observed a significant association between DES and hypertriglyceridemia in women in final multivariate models (p < 0.05). Chun et al. [20] reported statistically significant differences in the prevalence of high TC and LDL-C between the control group and women with DED stratified according to age (20–65 and above 65 years of age), especially among those aged above 65. After adjustment for confounding variables, they observed that the only lipid profile parameter associated with an increased likelihood of DED was elevated TC levels in women. In addition, other studies by Ooi et al. [27] and Mussi et al. [28] documented higher occurrences of DED symptoms and serum cholesterol levels in women compared to men.
The phenomenon of a higher prevalence of dyslipidemia in women with DED compared to men was observed in the studies mentioned above. Notably, Chun et al. [20] demonstrated the association of DED and dyslipidemia, especially among women aged above 65. The increased prevalence of dyslipidemia in women with DED aged >65 years can be attributed to the hormonal changes in women above age 60 [29,30,31,32]. Hjortland et al. [33] documented an increase in cholesterol levels that correlates with menopause, indicating a potential causal role of menopause in altering lipid levels. Carr et al. [34] observed that menopause was associated with a shift in LDL particles towards smaller, denser, and more atherogenic particles, in addition to higher LDL-C levels. Matthews et al. [35] also reported decreases in both total HDL-C and HDL2 in postmenopausal women. The increased risk of dyslipidemia in postmenopausal-aged women may be associated with the increased risk of dyslipidemia in older women with DED.
Despite the evidence provided by the majority of studies, Choi et al. [23] reported different results. After fully adjusting for age, body mass index, hypertension, diabetes, occupation, smoking and drinking habits, physical activity, contact lens use, computer use, region, and calendar year of study, they observed an adjusted odds ratio (OR) of 1.40 (1.03–1.90) for DES in men with dyslipidemia and an adjusted OR of 1.10 for DES in women with dyslipidemia, indicating that men with dyslipidemia are at an increased risk of DES compared with women. A stratified analysis of menopausal status revealed that the multiple adjusted ORs for DES were insignificant in both premenopausal and postmenopausal women. Also, another study by Ahn et al. [36] found that interactions between sex and dyslipidemia status among the DED patients showed no significance.
These contradictory results may be attributed to differing methodologies. In contrast to other studies, Choi et al. [23] evaluated the severity of DES through a questionnaire with OSDI scores, unlike other studies that employed more basic questions regarding eye dryness and prior DES diagnoses. It also incorporated multiple statistical models with potential confounders on the basis of previous studies and a larger sample size (n = 2272), enhancing the robustness of their results. Nevertheless, additional studies are still warranted to validate these inconclusive results.
4.2. Abnormal Lipid Profiles Are Not Significantly Associated with DED Patients
According to the data collected and integrated from each study (see Table 3), the majority of studies [20,21,26] revealed no statistically significant differences in lipid profile parameters between individuals with and without DED, despite the current prevalence of a strong association between DED and dyslipidemia.
However, some studies have highlighted a different point of view. For instance, Shokr et al. [25] reported that patients with DED had significantly increased TC and decreased HDL-C levels, albeit at borderline, consistent with previous studies. By contrast, Choi et al. [23] discovered that patients with DED had significantly increased HDL-C levels. Chun et al. [20] reported that women with DED had higher HDL-C levels than those in the control group. They also indicated that, among women, none of the combinations of lipid profile parameters that included low HDL-C exhibited significant differences in prevalence between individuals with and without DED, whereas all combinations without low HDL-C exhibited significant differences. In summary, according to Chun et al. [20], Park et al. [21] and Choi et al. [23], patients with DED have elevated HDL-C levels, although the difference is not statistically significant, which contradicts the current perception of HDL-C as a well-known preventive factor in cardiovascular disease, indicating that HDL-C may have negative effects on the presence of DED.
The reasons underlying why elevated HDL-C levels may pose a risk for the development of DED, despite the established role of HDL-C in heart protection, remain unclear. Multiple studies have directly investigated this phenomenon by using relevant animal models. However, only a few studies have provided valuable insights, suggesting that the meibomian glands may be the key to unraveling this mystery [37,38]. The meibomian glands are a specialized type of sebaceous glands that are closely associated with the biosynthesis of cholesterol [39]. In a study involving a murine model, Deplewski et al. [40] discovered that both HDL-C and VLDL-C strongly promoted the differentiation of sebaceous epithelial cells, resulting in an increased accumulation of lipid droplets, which are the primary components of sebum. They also discovered that HDL-C induced the accumulation of both TGs and cholesterol. In another study involving a murine model, Yagyu et al. [41] discovered that the lack of acyl-coenzyme A:cholesterol acyltransferase-1 (ACAT-1) resulted in not only reduced atherosclerosis but also in the atrophy of the meibomian glands. ACAT-1 plays a crucial role in catalyzing the esterification of cellular cholesterol, facilitating the formation and release of lipoproteins into the bloodstream. Collectively, these studies indicate that, although HDL-C serves a cardioprotective function by facilitating the removal of endogenous cholesterol from tissues and transporting it to the liver for elimination, HDL-C may contribute to MGD through lipid production. However, further investigation of the precise biochemical mechanisms underlying the involvement of HDL-C in MGD is warranted to provide valuable insights.
4.3. Limitations
This review has several limitations. First, of the six studies reviewed, four had a cross-sectional design and two had a case–control design. These studies confirmed a link between dyslipidemia and DED, but were unable to establish a causal relationship. Therefore, well-designed longitudinal studies are warranted to further clarify the relationship between DED and lipid profile parameters. Secondly, Rathnakumar et al. [22], Choi et al. [26] and Shokr et al. [25] included small samples in their studies, meaning that the statistical power of their studies may have been insufficient to validate their findings and their results may not be representative of the general population. Although the remaining studies included larger samples, they all solely targeted the Korean population, resulting in a lack of genetic and ethnic variability and increasing the difficulty of reproducing the results to in more heterogenous populations.
Thirdly, no standardized diagnosis of DED has yet been established. All of the included studies utilized questionnaires, such as the OSDI, as an evaluation metric of DED, which may have resulted in misclassification and recall bias due to the patients’ subjective responses. Despite the presence of conventional methods such as corneal staining, TBUT test, Schirmer’s test, and tear osmolarity test, no consensus has yet been reached regarding the diagnosis of DED [42,43].
Fourthly, not all potentially crucial confounding factors could be thoroughly controlled for or excluded from evaluations. Not all historical medical records were included and the influence of medical comorbidities was difficult to verify. In addition, potential environmental confounders and other influential factors, like the extent of computer or electronic device use or occupational elements [4], were also overlooked.
5. Conclusions
Dyslipidemia may be associated with DED, particularly in women with DED, who exhibit a significantly higher prevalence of dyslipidemia than men do. According to the quantitative data of relating to lipid profile parameters in the majority of the included studies, no statistically significant differences exist between individuals with and without DED. These results suggest that an abnormal lipid profile may not be directly linked to the development of DED. Despite this, the observed correlation emphasizes that ophthalmologists must be vigilant of regarding potential DED manifestations in female dyslipidemia patients. Early detection and intervention may prove essential in preventing or slowing the progression of DED.
Author Contributions
Conceptualization, T.-H.W.; methodology, T.-H.W.; software, T.-H.W.; validation, T.-H.W., Y.-J.T. and Y.-H.W.; formal analysis, T.-H.W.; investigation, T.-H.W. and I.-C.L.; resources, T.-H.W. and I.-C.L.; data curation, T.-H.W.; writing—original draft preparation, T.-H.W.; writing—review and editing, Y.-H.W. and C.-L.W.; visualization, C.-L.W. and Y.-J.T.; supervision, Y.-J.T. and I.-C.L.; project administration, I.-C.L.; funding acquisition, Y.-H.W. and I.-C.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors acknowledge the academic and science graphic illustration service provided by Taipei Medical University Office of Research and Development.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Gayton, J.L. Etiology, prevalence, and treatment of dry eye disease. Clin. Ophthalmol. 2009, 3, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Messmer, E.M. The pathophysiology, diagnosis, and treatment of dry eye disease. Dtsch. Arztebl. Int. 2015, 112, 71–81, quiz 82. [Google Scholar] [CrossRef] [PubMed]
- Schaumberg, D.A.; Dana, R.; Buring, J.E.; Sullivan, D.A. Prevalence of dry eye disease among US men: Estimates from the Physicians’ Health Studies. Arch. Ophthalmol. 2009, 127, 763–768. [Google Scholar] [CrossRef] [PubMed]
- Ay, İ.E.; Şenol, Y.; Gobeka, H.H.; Doğan, M. Is a Dry Eye Disorder in Firefighters an Occupational Disease? Med. Lav. 2023, 114, e2023020. [Google Scholar] [PubMed]
- Chia, E.-M.; Mitchell, P.; Rochtchina, E.; Lee, A.J.; Maroun, R.; Wang, J.J. Prevalence and associations of dry eye syndrome in an older population: The Blue Mountains Eye Study. Clin. Exp. Ophthalmol. 2003, 31, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Miljanović, B.; Dana, R.; Sullivan, D.A.; Schaumberg, D.A. Impact of dry eye syndrome on vision-related quality of life. Am. J. Ophthalmol. 2007, 143, 409–415.e2. [Google Scholar] [CrossRef] [PubMed]
- Tong, L.; Waduthantri, S.; Wong, T.Y.; Saw, S.M.; Wang, J.J.; Rosman, M.; Lamoureux, E. Impact of symptomatic dry eye on vision-related daily activities: The Singapore Malay Eye Study. Eye 2010, 24, 1486–1491. [Google Scholar] [CrossRef] [PubMed]
- Lam, S.M.; Tong, L.; Yong, S.S.; Li, B.; Chaurasia, S.S.; Shui, G.; Wenk, M.R. Meibum lipid composition in Asians with dry eye disease. PLoS ONE 2011, 6, e24339. [Google Scholar] [CrossRef]
- Goto, E.; Dogru, M.; Fukagawa, K.; Uchino, M.; Matsumoto, Y.; Saiki, M.; Tsubota, K. Successful tear lipid layer treatment for refractory dry eye in office workers by low-dose lipid application on the full-length eyelid margin. Am. J. Ophthalmol. 2006, 142, 264–270.e1. [Google Scholar] [CrossRef]
- Craig, J.P.; Tomlinson, A. Importance of the lipid layer in human tear film stability and evaporation. Optom. Vis. Sci. 1997, 74, 8–13. [Google Scholar] [CrossRef]
- Bron, A.; Tiffany, J.; Gouveia, S.; Yokoi, N.; Voon, L. Functional aspects of the tear film lipid layer. Exp. Eye Res. 2004, 78, 347–360. [Google Scholar] [CrossRef] [PubMed]
- Butovich, I.A. Lipidomics of human Meibomian gland secretions: Chemistry, biophysics, and physiological role of Meibomian lipids. Prog. Lipid Res. 2011, 50, 278–301. [Google Scholar] [CrossRef]
- Nicolaides, N. Skin Lipids. II. Lipid Class Composition of Samples from Various Species and Anatomical Sites. J. Am. Oil Chem. Soc. 1965, 42, 691–702. [Google Scholar] [CrossRef] [PubMed]
- Braich, P.S.; Howard, M.K.; Singh, J.S. Dyslipidemia and its association with meibomian gland dysfunction. Int. Ophthalmol. 2016, 36, 469–476. [Google Scholar] [CrossRef]
- Wang, T.-J.; Wang, I.-J.; Hu, C.-C.; Lin, H.-C. Comorbidities of dry eye disease: A nationwide population-based study. Acta Ophthalmol. 2012, 90, 663–668. [Google Scholar] [CrossRef] [PubMed]
- Roh, H.C.; Lee, J.K.; Kim, M.; Oh, J.H.; Chang, M.W.; Chuck, R.S.; Park, C.Y. Systemic Comorbidities of Dry Eye Syndrome: The Korean National Health and Nutrition Examination Survey V, 2010 to 2012. Cornea 2016, 35, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Vehof, J.; Snieder, H.; Jansonius, N.; Hammond, C.J. Prevalence and risk factors of dry eye in 79,866 participants of the population-based Lifelines cohort study in the Netherlands. Ocul. Surf. 2021, 19, 83–93. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Rev. Esp. Cardiol. Engl. Ed. 2021, 74, 790–799. [Google Scholar] [CrossRef]
- Schiavo, J.H. PROSPERO: An International Register of Systematic Review Protocols. Med. Ref. Serv. Q. 2019, 38, 171–180. [Google Scholar] [CrossRef]
- Chun, Y.H.; Kim, H.R.; Han, K.; Park, Y.-G.; Song, H.J.; Na, K.-S. Total cholesterol and lipoprotein composition are associated with dry eye disease in Korean women. Lipids Health Dis. 2013, 12, 84. [Google Scholar] [CrossRef]
- Park, H.W.; Park, J.W. The Association between Symptoms of Dry Eye Syndrome and Metabolic Outcome in a General Population in Korea. J. Korean Med. Sci. 2016, 31, 1121–1126. [Google Scholar] [CrossRef] [PubMed]
- Rathnakumar, K.; Ramachandran, K.; Baba, D.; Ramesh, V.; Anebaracy, V.; Vidhya, R.; Vinothkumar, R.; Poovitha, R.; Geetha, R. Prevalence of dry eye disease and its association with dyslipidemia. J. Basic Clin. Physiol. Pharmacol. 2018, 29, 195–199. [Google Scholar] [CrossRef]
- Choi, H.R.; Lee, J.H.; Lee, H.K.; Song, J.S.; Kim, H.C. Association Between Dyslipidemia and Dry Eye Syndrome Among the Korean Middle-Aged Population. Cornea 2020, 39, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Wolffsohn, J.S.; Arita, R.; Chalmers, R.; Djalilian, A.; Dogru, M.; Dumbleton, K.; Gupta, P.K.; Karpecki, P.; Lazreg, S.; Pult, H.; et al. TFOS DEWS II Diagnostic Methodology report. Ocul. Surf. 2017, 15, 539–574. [Google Scholar] [CrossRef] [PubMed]
- Shokr, H.; Wolffsohn, J.S.; Huarte, S.T.; Scarpello, E.; Gherghel, D. Dry eye disease is associated with retinal microvascular dysfunction and possible risk for cardiovascular disease. Acta Ophthalmol. 2021, 99, e1236–e1242. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.R.; Kim, N.H.; Lee, J.-M.; Choi, D.P.; Seo, Y.; Cho, W.K.; Song, J.S.; Lee, H.K.; Kim, H.C. Risk Factors Influencing the Occurrence and Severity of Symptomatic Dry Eye Syndrome: A Cross-sectional Study. Ophthalmic Epidemiol. 2021, 28, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Ooi, K.G.; Lee, M.H.; Burlutsky, G.; Gopinath, B.; Mitchell, P.; Watson, S. Association of dyslipidaemia and oral statin use, and dry eye disease symptoms in the Blue Mountains Eye Study. Clin. Exp. Ophthalmol. 2019, 47, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Mussi, N.; Haque, W.; Robertson, D.M. The Association Between Risk Factors for Metabolic Syndrome and Meibomian Gland Disease in a Dry Eye Cohort. Clin. Ophthalmol. 2021, 15, 3821–3832. [Google Scholar] [CrossRef] [PubMed]
- Schaumberg, D.A.; Sullivan, D.A.; Buring, J.E.; Dana, M. Prevalence of dry eye syndrome among US women. Am. J. Ophthalmol. 2003, 136, 318–326. [Google Scholar] [CrossRef] [PubMed]
- Tankó, L.B.; Bagger, Y.Z.; Qin, G.; Alexandersen, P.; Larsen, P.J.; Christiansen, C. Enlarged waist combined with elevated triglycerides is a strong predictor of accelerated atherogenesis and related cardiovascular mortality in postmenopausal women. Circulation 2005, 111, 1883–1890. [Google Scholar] [CrossRef] [PubMed]
- Hulley, S.; Grady, D.; Bush, T.; Furberg, C.; Herrington, D.; Riggs, B.; Vittinghoff, E.; Heart and Estrogen/Progestin Replacement Study (HERS) Research Group. Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. JAMA 1998, 280, 605–613. [Google Scholar] [CrossRef] [PubMed]
- Talbott, E.; Guzick, D.; Clerici, A.; Berga, S.; Detre, K.; Weimer, K.; Kuller, L. Coronary heart disease risk factors in women with polycystic ovary syndrome. Arter. Thromb. Vasc. Biol. 1995, 15, 821–826. [Google Scholar] [CrossRef] [PubMed]
- Hjortland, M.C.; Mcnamara, P.M.; Kannel, W.B. Some atherogenic concomitants of menopause: The Framingham Study. Am. J. Epidemiol. 1976, 103, 304–311. [Google Scholar] [CrossRef]
- Carr, M.C.; Kim, K.H.; Zambon, A.; Mitchell, E.S.; Woods, N.F.; Casazza, C.P.; Purnell, J.Q.; Hokanson, J.E.; Brunzell, J.D.; Schwartz, R.S. Changes in LDL density across the menopausal transition. J. Investig. Med. 2000, 48, 245–250. [Google Scholar] [PubMed]
- Matthews, K.A.; Meilahn, E.; Kuller, L.H.; Kelsey, S.F.; Caggiula, A.W.; Wing, R.R. Menopause and risk factors for coronary heart disease. N. Engl. J. Med. 1989, 321, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.H.; Choi, Y.-H.; Paik, H.J.; Kim, M.K.; Wee, W.R.; Kim, D.H. Sex differences in the effect of aging on dry eye disease. Clin. Interv. Aging 2017, 12, 1331–1338. [Google Scholar] [CrossRef] [PubMed]
- Dao, A.H.; Spindle, J.D.; Harp, B.A.; Jacob, A.; Chuang, A.Z.; Yee, R.W. Association of dyslipidemia in moderate to severe meibomian gland dysfunction. Am. J. Ophthalmol. 2010, 150, 371–375.e1. [Google Scholar] [CrossRef] [PubMed]
- Kuriakose, R.K.; Braich, P.S. Dyslipidemia and its Association with Meibomian Gland Dysfunction: A Systematic Review. Int. Ophthalmol. 2018, 38, 1809–1816. [Google Scholar] [CrossRef]
- Yoo, Y.-S.; Park, S.-K.; Hwang, H.-S.; Kim, H.-S.; Arita, R.; Na, K.-S. Association of Serum Lipid Level with Meibum Biosynthesis and Meibomian Gland Dysfunction: A Review. J. Clin. Med. 2022, 11, 4010. [Google Scholar] [CrossRef] [PubMed]
- Deplewski, D.; Qin, K.; Ciletti, N.; Rosenfield, R.L. Unique mode of lipogenic activation in rat preputial sebocytes. J. Nutr. Metab. 2011, 2011, 163631. [Google Scholar] [CrossRef] [PubMed]
- Yagyu, H.; Kitamine, T.; Osuga, J.-I.; Tozawa, R.-I.; Chen, Z.; Kaji, Y.; Oka, T.; Perrey, S.; Tamura, Y.; Ohashi, K.; et al. Absence of ACAT-1 attenuates atherosclerosis but causes dry eye and cutaneous xanthomatosis in mice with congenital hyperlipidemia. J. Biol. Chem. 2000, 275, 21324–21330. [Google Scholar] [CrossRef] [PubMed]
- Tsubota, K.; Yokoi, N.; Shimazaki, J.; Watanabe, H.; Dogru, M.; Yamada, M.; Kinoshita, S.; Kim, H.-M.; Tchah, H.-W.; Hyon, J.Y.; et al. New Perspectives on Dry Eye Definition and Diagnosis: A Consensus Report by the Asia Dry Eye Society. Ocul. Surf. 2017, 15, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Shimazaki, J. Definition and Diagnostic Criteria of Dry Eye Disease: Historical Overview and Future Directions. Investig. Opthalmol. Vis. Sci. 2018, 59, DES7–DES12. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).