Comparison of the Duhamel Procedure and Transanal Endorectal Pull-through Procedure in the Treatment of Children with Hirschsprung’s Disease: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Inclusion/Exclusion Criteria
2.3. Data Extraction
2.4. Quality Assessment
2.5. Data Synthesis and Statistical Analysis
3. Results
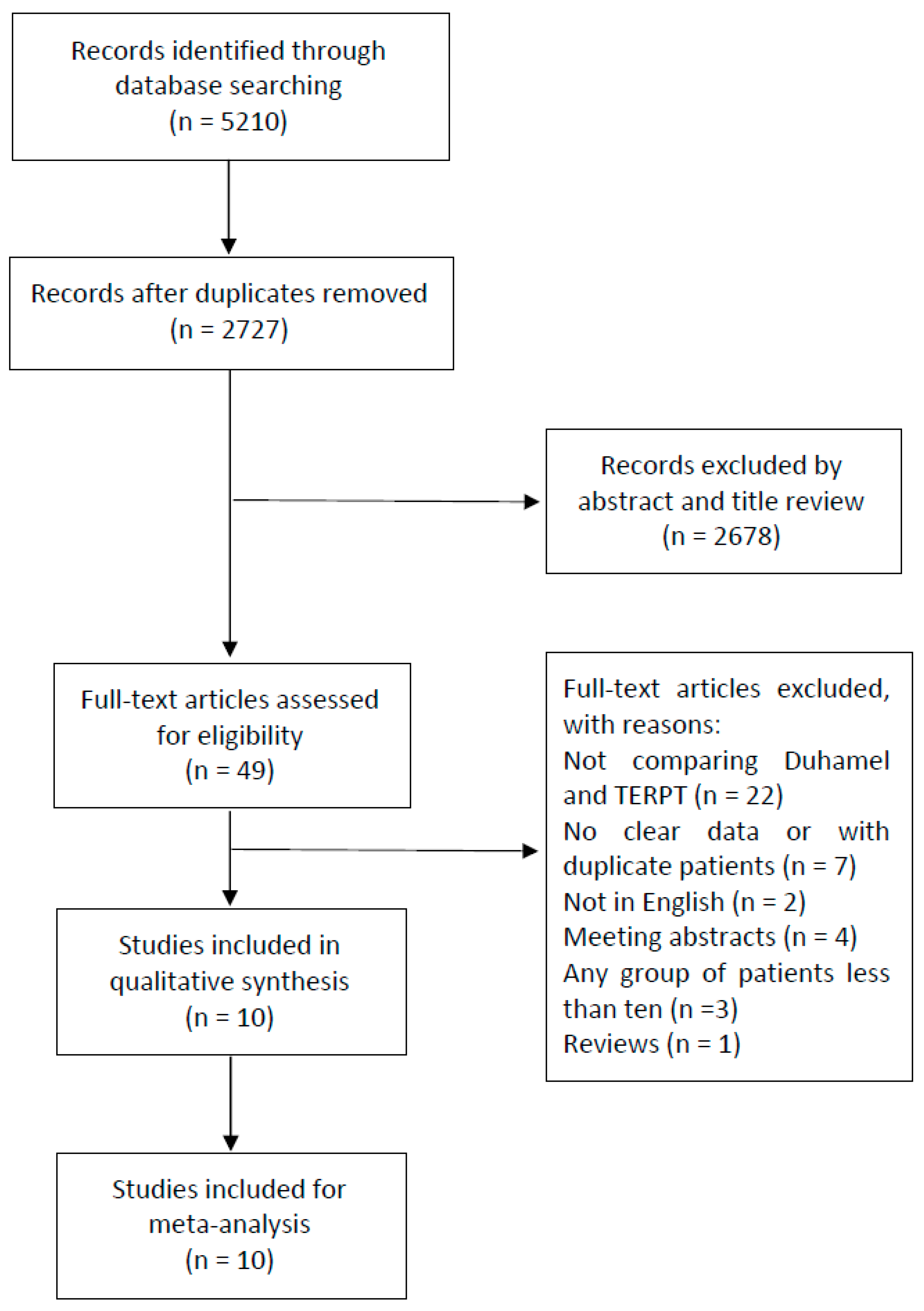
3.1. Search Process and Characteristics of the Included Studies
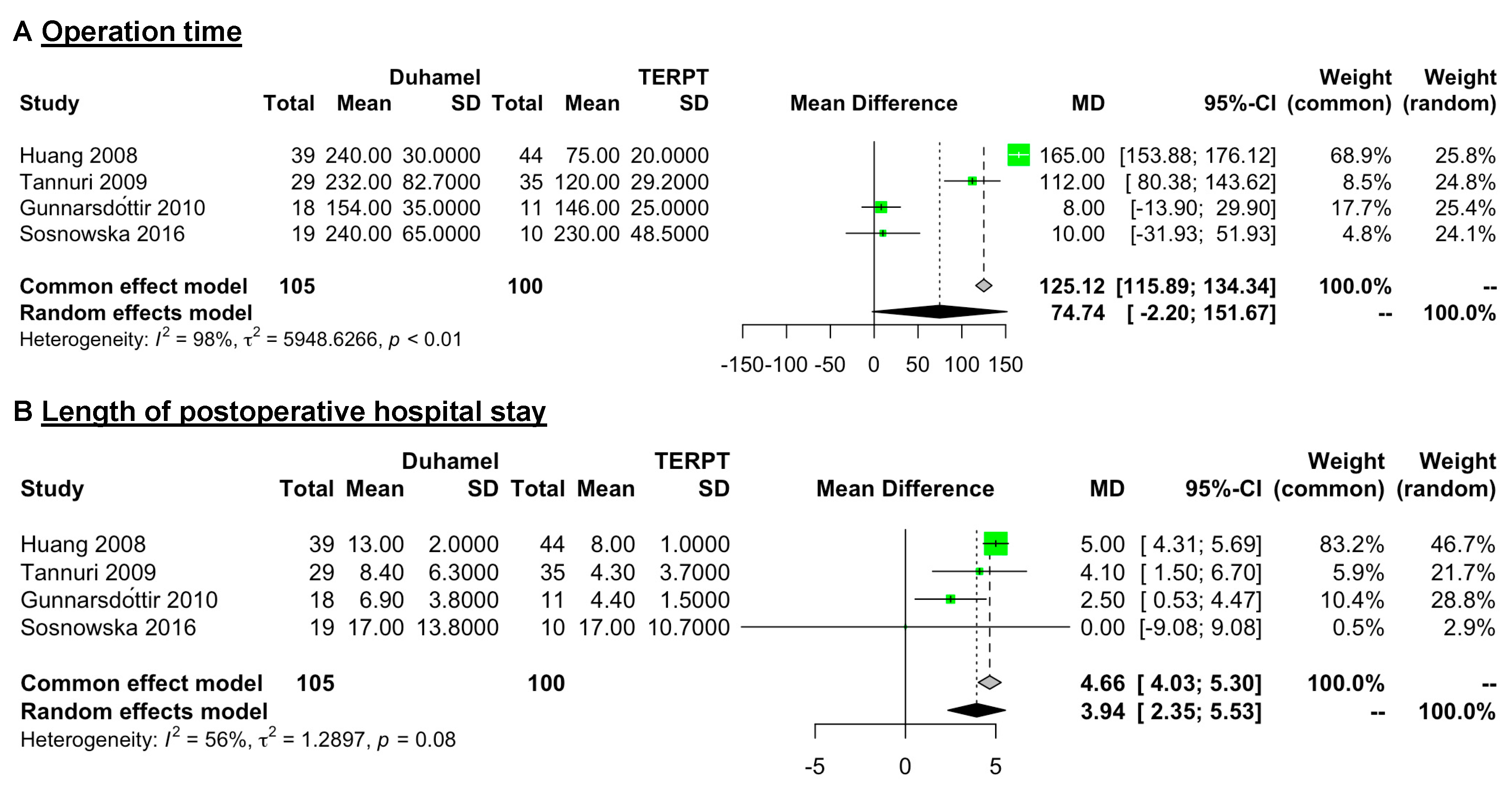
3.2. Operation Time and Length of Postoperative Hospital Stay
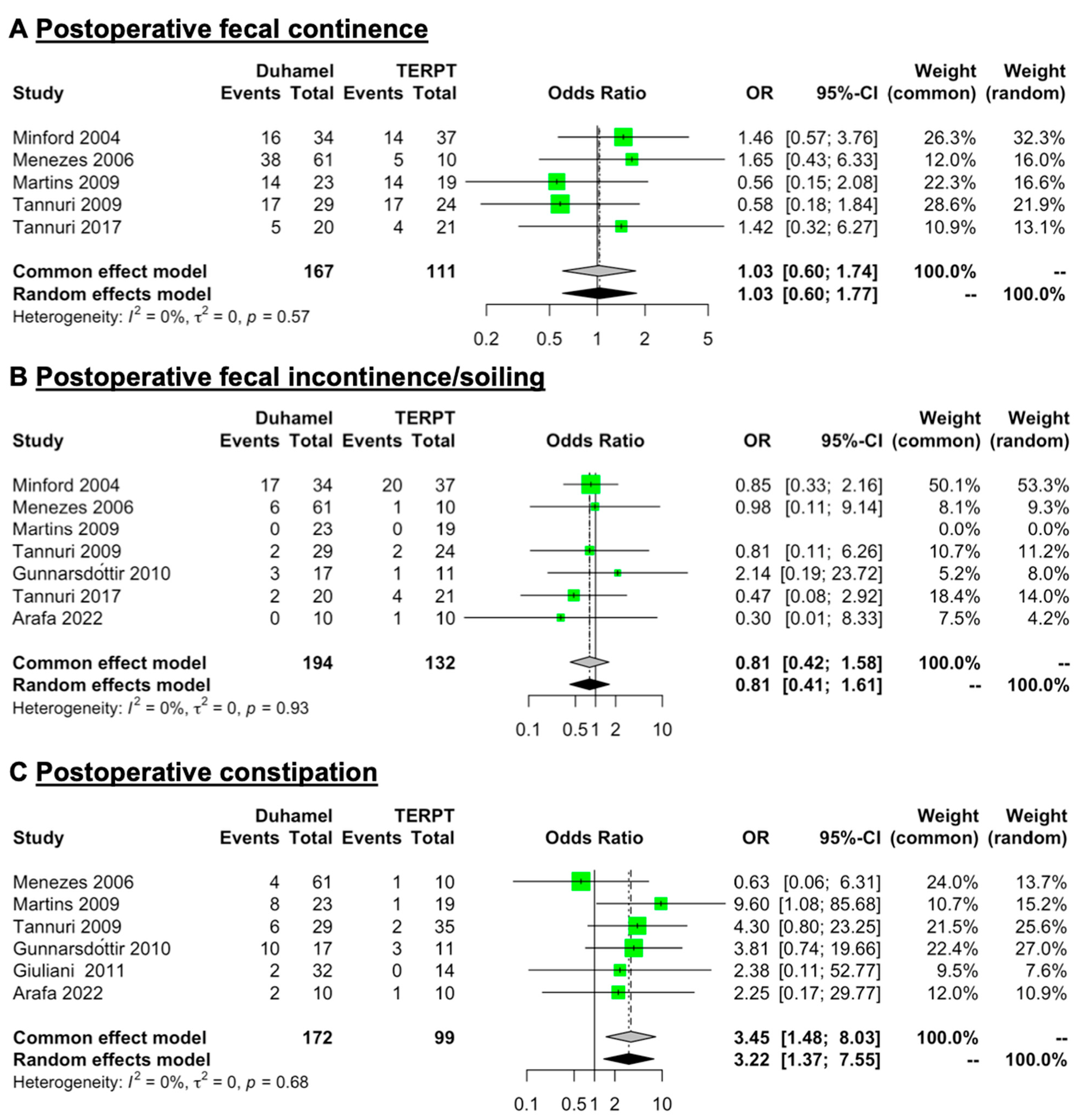
3.3. Postoperative Fecal Continence, Fecal Incontinence/Soiling, and Constipation
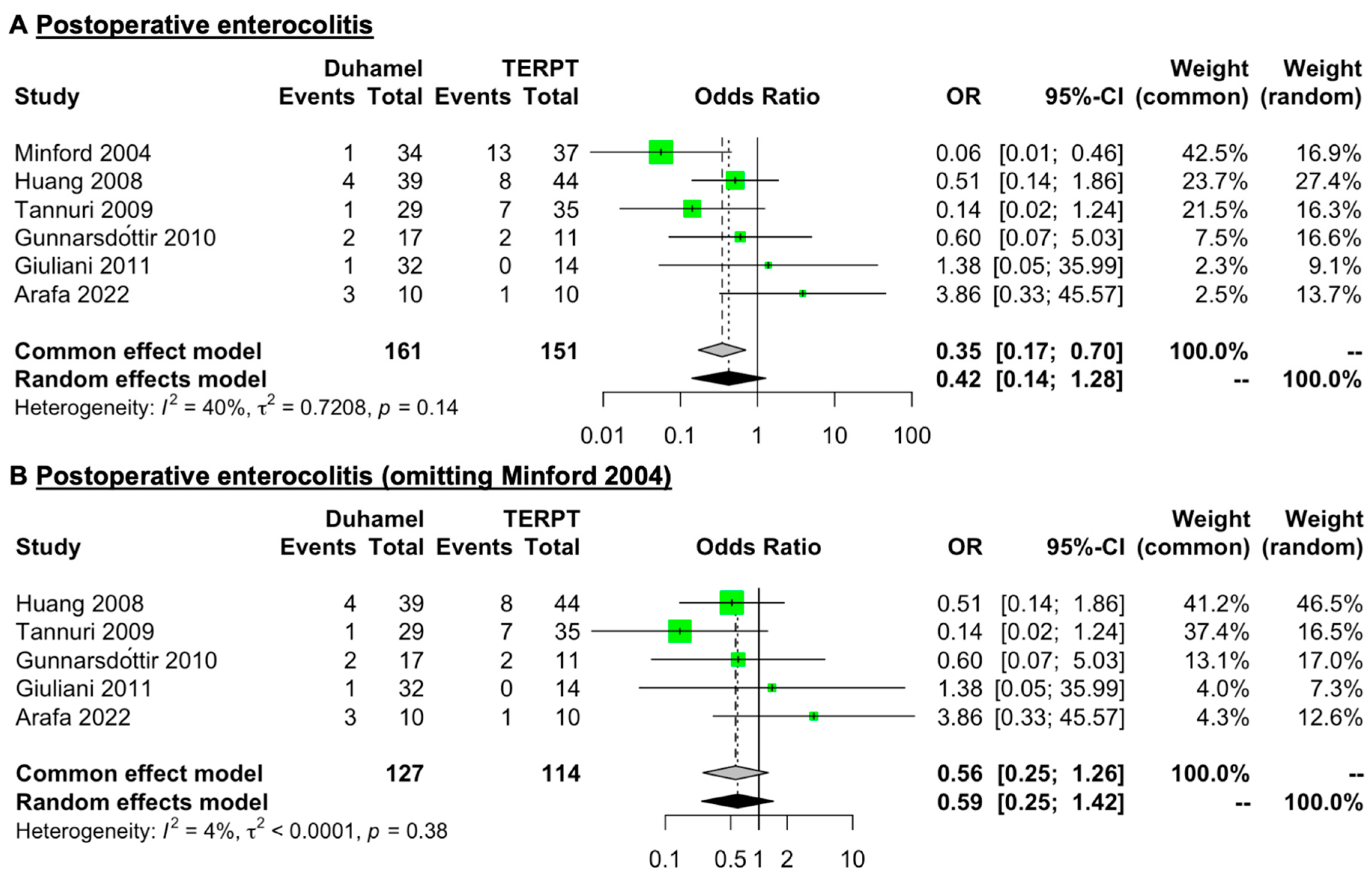
3.4. Postoperative Enterocolitis
3.5. Postoperative Anastomotic Stricture, Anastomotic Leak, and Ileus
3.6. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Parisi, M.A.; Kapur, R.P. Genetics of Hirschsprung disease. Curr. Opin. Pediatr. 2000, 12, 610–617. [Google Scholar] [CrossRef] [PubMed]
- Duhamel, B. A new operation for the treatment of Hirschsprung’s disease. Arch. Dis. Child. 1960, 35, 38–39. [Google Scholar] [CrossRef] [PubMed][Green Version]
- De la Torre-Mondragón, L.; Ortega-Salgado, J.A. Transanal endorectal pull-through for Hirschsprung’s disease. J. Pediatr. Surg. 1998, 33, 1283–1286. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, K. New techniques in the surgical treatment of Hirschsprung’s disease. Surgery 1967, 61, 503–508. [Google Scholar]
- Soave, F. A New Surgical Technique for Treatment of Hirschsprung’s Disease. Surgery 1964, 56, 1007–1014. [Google Scholar]
- Boley, S.J. New Modification of the Surgical Treatment of Hirschsprung’s Disease. Surgery 1964, 56, 1015–1017. [Google Scholar]
- Holcomb, G.W.; Murphy, J.P.; Peter, S.D.S. Holcomb and Ashcraft’s Pediatric Surgery, 7th ed.; Elsevier: Philadelphia, PA, USA, 2019. [Google Scholar]
- Langer, J.C.; Minkes, R.K.; Mazziotti, M.V.; Skinner, M.A.; Winthrop, A.L. Transanal one-stage Soave procedure for infants with Hirschsprung’s disease. J. Pediatr. Surg. 1999, 34, 148–151, discussion 152. [Google Scholar] [CrossRef]
- Georgeson, K.E.; Cohen, R.D.; Hebra, A.; Jona, J.Z.; Powell, D.M.; Rothenberg, S.S.; Tagge, E.P. Primary laparoscopic-assisted endorectal colon pull-through for Hirschsprung’s disease: A new gold standard. Ann. Surg. 1999, 229, 678–682, discussion 682–673. [Google Scholar] [CrossRef]
- Mao, Y.Z.; Tang, S.T.; Li, S. Duhamel operation vs. transanal endorectal pull-through procedure for Hirschsprung disease: A systematic review and meta-analysis. J. Pediatr. Surg. 2018, 53, 1710–1715. [Google Scholar] [CrossRef]
- Seo, S.; Miyake, H.; Hock, A.; Koike, Y.; Yong, C.; Lee, C.; Li, B.; Pierro, A. Duhamel and Transanal Endorectal Pull-throughs for Hirschsprung’ Disease: A Systematic Review and Meta-analysis. Eur. J. Pediatr. Surg. 2018, 28, 81–88. [Google Scholar]
- Arts, E.; Botden, S.M.; Lacher, M.; Sloots, P.; Stanton, M.P.; Sugarman, I.; Wester, T.; de Blaauw, I. Duhamel versus transanal endorectal pull through (TERPT) for the surgical treatment of Hirschsprung’s disease. Tech. Coloproctol. 2016, 20, 677–682. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Soper, R.T. Surgery for Hirschsprung’s disease. Aorn J. 1968, 8, 69–81. [Google Scholar] [CrossRef] [PubMed]
- Xu, P.P.; Chang, X.P.; Zhang, X.; Chi, S.Q.; Cao, G.Q.; Li, S.; Yang, D.H.; Li, X.Y.; Tang, S.T. Transumbilical enterostomy for Hirschsprung’s disease with a two-stage laparoscopy-assisted pull-through procedure. World J. Gastroenterol. 2019, 25, 6781–6789. [Google Scholar] [CrossRef]
- Minford, J.L.; Ram, A.; Turnock, R.R.; Lamont, G.L.; Kenny, S.E.; Rintala, R.J.; Lloyd, D.A.; Baillie, C.T. Comparison of functional outcomes of Duhamel and transanal endorectal coloanal anastomosis for Hirschsprung’s disease. J. Pediatr. Surg. 2004, 39, 161–165, discussion 161–165. [Google Scholar] [CrossRef]
- Menezes, M.; Corbally, M.; Puri, P. Long-term results of bowel function after treatment for Hirschsprung’s disease: A 29-year review. Pediatr. Surg. Int. 2006, 22, 987–990. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zheng, S.; Xiao, X. A follow-up study on postoperative function after a transanal Soave 1-stage endorectal pull-through procedure for Hirschsprung’s disease. J. Pediatr. Surg. 2008, 43, 1691–1695. [Google Scholar] [CrossRef] [PubMed]
- Martins, E.C.; Peterlini, F.L.; Fagundes, D.J.; Martins, J.L. Clinical, manometric and profilometric evaluation after surgery for Hirschsprung’s disease: Comparison between the modified Duhamel and the transanal rectosigmoidectomy techniques. Acta Cir. Bras. 2009, 24, 416–422. [Google Scholar] [CrossRef]
- Tannuri, A.C.; Tannuri, U.; Romão, R.L. Transanal endorectal pull-through in children with Hirschsprung’s disease--technical refinements and comparison of results with the Duhamel procedure. J. Pediatr. Surg. 2009, 44, 767–772. [Google Scholar] [CrossRef]
- Gunnarsdóttir, A.; Larsson, L.T.; Arnbjörnsson, E. Transanal endorectal vs. duhamel pull-through for Hirschsprung’s disease. Eur. J. Pediatr. Surg. 2010, 20, 242–246. [Google Scholar] [CrossRef]
- Giuliani, S.; Betalli, P.; Narciso, A.; Midrio, P.; Gamba, P.G. Outcome comparison among laparoscopic, laparotomic-duhamel, and transanal endorectal pull-through: A single-center 18-year experience. J. Laparoendosc. Adv. Surg. Tech. 2011, 21, A4–A5. [Google Scholar] [CrossRef]
- Sosnowska, P.; Błaszczyński, M.; Moryciński, S.; Porzucek, W.; Mańkowski, P. Are there any factors influencing the course of multistage treatment in Hirschsprung’s disease? Prz. Gastroenterol. 2016, 11, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Tannuri, A.C.; Ferreira, M.A.; Mathias, A.L.; Tannuri, U. Long-term results of the Duhamel technique are superior to those of the transanal pullthrough: A study of fecal continence and quality of life. J. Pediatr. Surg. 2017, 52, 449–453. [Google Scholar] [CrossRef] [PubMed]
- Arafa, A.; Ragab, M.; Abdelazim, O.; Khedr, S.; Mohamed, W. Minimally invasive surgery in older children with Hirschsprung’s disease in a North African Country. Front. Surg. 2022, 9, 934289. [Google Scholar] [CrossRef] [PubMed]
- Davidson, J.R.; Mutanen, A.; Salli, M.; Kyrklund, K.; De Coppi, P.; Curry, J.; Eaton, S.; Pakarinen, M.P. Comparative cohort study of Duhamel and endorectal pull-through for Hirschsprung’s disease. BJS Open 2022, 6, zrab143. [Google Scholar] [CrossRef] [PubMed]
- Langer, J.C. Laparoscopic and transanal pull-through for Hirschsprung disease. Semin. Pediatr. Surg. 2012, 21, 283–290. [Google Scholar] [CrossRef]
- Weidner, B.C.; Waldhausen, J.H. Swenson revisited: A one-stage, transanal pull-through procedure for Hirschsprung’s disease. J. Pediatr. Surg. 2003, 38, 1208–1211. [Google Scholar] [CrossRef]
- Levitt, M.A.; Hamrick, M.C.; Eradi, B.; Bischoff, A.; Hall, J.; Pena, A. Transanal, full-thickness, Swenson-like approach for Hirschsprung disease. J. Pediatr. Surg. 2013, 48, 2289–2295. [Google Scholar] [CrossRef]
- De la Torre, L.; Ortega, A. Transanal versus open endorectal pull-through for Hirschsprung’s disease. J. Pediatr. Surg. 2000, 35, 1630–1632. [Google Scholar] [CrossRef]
- Zhang, S.; Li, J.; Wu, Y.; Hu, Y.; Duan, C.; Wang, M.; Gai, Z. Comparison of Laparoscopic-Assisted Operations and Laparotomy Operations for the Treatment of Hirschsprung Disease: Evidence From a Meta-Analysis. Medicine 2015, 94, e1632. [Google Scholar] [CrossRef]
- The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: https://www.ohri.ca//programs/clinical_epidemiology/oxford.asp (accessed on 10 August 2023).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef]
- Li, T.; Higgins, J.P.T.; Deeks, J.J. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (Updated February 2022). Cochrane. 2022. Available online: fromwww.training.cochrane.org/handbook (accessed on 10 August 2023).
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef] [PubMed]
- Luo, D.; Wan, X.; Liu, J.; Tong, T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat. Methods Med. Res. 2018, 27, 1785–1805. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Nah, S.A.; Laksmi, N.K.; Ong, C.C.; Chua, J.H.; Jacobsen, A.; Low, Y. Transanal endorectal pull-through versus transabdominal approach for Hirschsprung’s disease: A systematic review and meta-analysis. J. Pediatr. Surg. 2013, 48, 642–651. [Google Scholar] [CrossRef]
- Yan, B.L.; Bi, L.W.; Yang, Q.Y.; Wu, X.S.; Cui, H.L. Transanal endorectal pull-through procedure versus transabdominal surgery for Hirschsprung disease: A systematic review and meta-analysis. Medicine 2019, 98, e16777. [Google Scholar] [CrossRef]
- Yanchar, N.L.; Soucy, P. Long-term outcome after Hirschsprung’s disease: Patients’ perspectives. J. Pediatr. Surg. 1999, 34, 1152–1160. [Google Scholar] [CrossRef]
- Dasgupta, R.; Langer, J.C. Evaluation and management of persistent problems after surgery for Hirschsprung disease in a child. J. Pediatr. Gastroenterol. Nutr. 2008, 46, 13–19. [Google Scholar] [CrossRef]
- Rintala, R.J.; Pakarinen, M.P. Long-term outcomes of Hirschsprung’s disease. Semin. Pediatr. Surg. 2012, 21, 336–343. [Google Scholar] [CrossRef]
- Zhang, S.C.; Bai, Y.Z.; Wang, W.; Wang, W.L. Clinical outcome in children after transanal 1-stage endorectal pull-through operation for Hirschsprung disease. J. Pediatr. Surg. 2005, 40, 1307–1311. [Google Scholar] [CrossRef]
- Rouzrokh, M.; Khaleghnejad, A.T.; Mohejerzadeh, L.; Heydari, A.; Molaei, H. What is the most common complication after one-stage transanal pull-through in infants with Hirschsprung’s disease? Pediatr. Surg. Int. 2010, 26, 967–970. [Google Scholar] [CrossRef]
- Sukarelawanto, A.V.R.; Ritana, A.; Balela, N.; Putri, W.J.K.; Sirait, D.N.; Paramita, V.M.W.; Sasmita, A.P.; Dwihantoro, A.; Makhmudi, A. Postoperative enterocolitis assessment using two different cut-off values in the HAEC score in Hirschsprung patients undergoing Duhamel and Soave pull-through. BMC Pediatrics 2020, 20, 457. [Google Scholar]
- Ruttenstock, E.; Puri, P. Systematic review and meta-analysis of enterocolitis after one-stage transanal pull-through procedure for Hirschsprung’s disease. Pediatr. Surg. Int. 2010, 26, 1101–1105. [Google Scholar] [CrossRef] [PubMed]

| First Author, Publication Year, Country | Journal | Study Design | Surgical Technique (n) | Age at Operation (Month) | Male:Female (n) | Extent of Disease (n) | Length of FolLow Up (Month) | Main Outcome and Complication Measurements | NOS Score | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Short | RS | Long | |||||||||
| Minford [15], (2004), UK | J Pediatr Surg | Prospective | Duhamel (n = 34) | 84 (median) (age at scoring) | 25:9 | 0 | 24 | 10 | NA | Morbidity and mortality, enterocolitis, stricture, rectal spur, myectomy, late stoma formation and operative failure, functional outcome score. | 7 |
| TERPT (n = 37) | 72 (median) (age at scoring) | 27:10 | 0 | 27 | 10 | NA | |||||
| Menezes [16], (2006), Ireland | Pediatr Surg Int | Retrospective | Duhamel (n = 61) | NA | NA | NA | NA | NA | NA | Long-term bowel function, soiling, constipation. | 4 |
| TERPT (n = 10) | NA | NA | NA | NA | NA | NA | |||||
| Huang [17], (2008), China | J Pediatr Surg | Retrospective | Duhamel (n = 39) | 27.6 (mean) (range: 3 to 120) | 34:5 | 21 | 18 | 0 | 12 to 60 | Perioperative therapeutic effect, rating of bowel movements, anastomotic leak, incision infection, adhesive ileus, enterocolitis, death, anorectal manometry. | 6 |
| TERPT (n = 44) | NA | NA | 14 | 30 | 0 | 12 to 60 | |||||
| Martins [18], (2009), Brazil | Acta Cir Bras | Prospective | Duhamel (n = 23) | 104.4 (mean) (range: 24 to 180) | NA | NA | NA | NA | NA | Constipation, continence, anorectal manometry | 5 |
| TERPT (n = 19) | 60 (mean) (range: 12 to 108) | NA | NA | NA | NA | NA | |||||
| Tannuri [19], (2009), Brazil | J Pediatr Surg | Retrospective | Duhamel (n = 29) | 42 (mean) (range: 6 to 110) | NA | 0 | 29 | 0 | 2 to 168 | Operating time, post operative hospital stay, enterocolitis, wound infection, mortality, stooling patterns, postoperative continence, perineal dermatitis. | 5 |
| TERPT (n = 35) | 11 (mean) (range: 0.3 to 72) | NA | 0 | 35 | 0 | 2 to 72 | |||||
| Gunnarsdóttir [20], (2010), Sweden | Eur J Pediatr Surg | Retrospective | Duhamel (n = 18) | 5.6 (mean) (range: 1 to 23) | 15:3 | 0 | 18 | 0 | 25 to 45 | Operative time, perioperative bleeding, time of oral feeding and bowel movement postoperatively, the length of hospital stay, enterocolitis. | 7 |
| TERPT (n = 11) | 4.8 (mean) (range: 1 to 24) | 7:4 | 0 | 11 | 0 | 25 to 48 | |||||
| Giuliani [21], (2011), Italy | J Laparoendosc Adv S | Retrospective | Duhamel (n = 32) | 14.61 (mean) | 9:1 | 3 | 28 | 1 | ≥12 | Operative time, length of hospital stay, postoperative start of oral feeding, postoperative enterocolitis, incidence of severe constipation or incontinence. | 6 |
| TERPT (n = 14) | 4.67 (mean) | 8:1 | 2 | 10 | 2 | 26 (mean) | |||||
| Sosnowska [22], (2016), Poland | Prz Gastroenterol | Retrospective | Duhamel (n = 19) | 49 (mean) | NA | NA | NA | NA | NA | Operative time of radical surgery, length of hospitalisation after radical surgeryl, number and cause of complications. | 6 |
| TERPT (n = 10) | 16 (mean) | NA | NA | NA | NA | NA | |||||
| Tannuri [23] , (2017), Brazil | J Pediatr Surg | Retrospective | Duhamel (n = 20) | 41 (median) (range: 6 to 110) | 3:1 | NA | NA | NA | 6 to 60 | The Fecal Continence Index (FCI) questionnaire and the Assessment of Quality of Life in Children and Adolescents with Fecal Incontinence (AQLCAFI) questionnaire | 4 |
| TERPT (n = 21) | 10 (median) (range: 0.3 to 72) | 16:5 | NA | NA | NA | 6 to 55 | |||||
| Arafa [24], (2022), Egypt | Front Surg | Prospective | Duhamel (n = 10) | 36 (mean) | NA | NA | NA | NA | 12 | Operative time, length of hospital stay, leakage, perianal excoriation, postoperative enterocolitis, constipation, anal stenosis, spur formation and fecal incontinence. | 4 |
| TERPT (n = 10) | 36 (mean) | NA | NA | NA | NA | 12 | |||||
| First Author, Publication Year, Country | Journal | Surgical Technique (n) | Operation Time (Minute) a | Length of Postoperative Hospital Stay (Day) a | Fecal Continence (n) | Fecal Incontinence/ Soiling (n) | Constipation (n) | Postoperative Enterocolitis (n) | Anastomotic Stricture (n) | Anastomotic Leak (n) | Post Operative Ileus (n) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Minford [15], (2004), UK | J Pediatr Surg | Duhamel (n = 34) | NA | NA | 16 | 17 | NA | 1 | 0 | NA | NA |
| TERPT (n = 37) | NA | NA | 14 | 20 | NA | 13 | 7 | NA | NA | ||
| Menezes [16], (2006), Ireland | Pediatr Surg Int | Duhamel (n = 61) | NA | NA | 38 | 6 | 4 | NA | NA | NA | NA |
| TERPT (n = 10) | NA | NA | 5 | 1 | 1 | NA | NA | NA | NA | ||
| Huang [17], (2008), China | J Pediatr Surg | Duhamel (n = 39) | 240 ± 30 | 13 ± 2 | NA | NA | NA | 4 | NA | 1 | 1 |
| TERPT (n = 44) | 75 ± 20 | 8 ± 1 | NA | NA | NA | 8 | NA | 0 | 0 | ||
| Martins [18], (2009), Brazil | Acta Cir Bras | Duhamel (n = 23) | NA | NA | 14 | 0 | 8 | NA | NA | NA | NA |
| TERPT (n =19) | NA | NA | 14 | 0 | 1 | NA | NA | NA | NA | ||
| Tannuri [19], (2009), Brazil | J Pediatr Surg | Duhamel (n = 29) | 232 ± 82.7 | 8.4 ± 6.3 | 17 | 2 | 6 | 1 | 0 | NA | 1 |
| TERPT (n =35) | 120 ± 29.2 | 4.3 ± 3.69 | 17 (among 24 patients) | 2 (among 24 patients) | 2 | 7 | 3 | NA | 0 | ||
| Gunnarsdóttir [20], (2010), Sweden | Eur J Pediatr Surg | Duhamel (n = 18) | 154 ± 35 | 6.9 ± 3.8 | NA | 3 (among 17 patients) | 10 (among 17 patients) | 2 (among 17 patients) | 0 | 1 | 1 |
| TERPT (n = 11) | 146 ± 25 | 4.4 ± 1.5 | NA | 1 | 3 | 2 | 2 | 0 | 0 | ||
| Giuliani [21], (2011), Italy | J Laparoendosc Adv S | Duhamel (n = 32) | 257 (mean) | 6.8 (mean) | NA | NA | 2 | 1 | 0 | 1 | 1 |
| TERPT (n = 14) | 195 (mean) | 4.4 (mean) | NA | NA | 0 | 0 | 1 | 0 | 0 | ||
| Sosnowska [22], (2016), Poland | Prz Gastroenterol | Duhamel (n = 19) | 240 (mean) | 17 (mean) | NA | NA | NA | NA | NA | NA | NA |
| TERPT (n = 10) | 230 (mean) | 17 (mean) | NA | NA | NA | NA | NA | NA | NA | ||
| Tannuri [23], (2017), Brazil | J Pediatr Surg | Duhamel (n = 20) | NA | NA | 5 | 2 | NA | NA | NA | NA | NA |
| TERPT (n = 21) | NA | NA | 4 | 4 | NA | NA | NA | NA | NA | ||
| Arafa [24], (2022), Egypt | Front Surg | Duhamel (n = 10) | NA | NA | NA | 0 | 2 | 3 | 0 | 0 | NA |
| TERPT (n = 10) | NA | NA | NA | 1 | 1 | 1 | 2 | 0 | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Q.; Liang, Y.; Luo, M.; Feng, L.; Xiang, B. Comparison of the Duhamel Procedure and Transanal Endorectal Pull-through Procedure in the Treatment of Children with Hirschsprung’s Disease: A Systematic Review. J. Clin. Med. 2023, 12, 6632. https://doi.org/10.3390/jcm12206632
Wang Q, Liang Y, Luo M, Feng L, Xiang B. Comparison of the Duhamel Procedure and Transanal Endorectal Pull-through Procedure in the Treatment of Children with Hirschsprung’s Disease: A Systematic Review. Journal of Clinical Medicine. 2023; 12(20):6632. https://doi.org/10.3390/jcm12206632
Chicago/Turabian StyleWang, Qi, Yuanyuan Liang, Mengqi Luo, Liwei Feng, and Bo Xiang. 2023. "Comparison of the Duhamel Procedure and Transanal Endorectal Pull-through Procedure in the Treatment of Children with Hirschsprung’s Disease: A Systematic Review" Journal of Clinical Medicine 12, no. 20: 6632. https://doi.org/10.3390/jcm12206632
APA StyleWang, Q., Liang, Y., Luo, M., Feng, L., & Xiang, B. (2023). Comparison of the Duhamel Procedure and Transanal Endorectal Pull-through Procedure in the Treatment of Children with Hirschsprung’s Disease: A Systematic Review. Journal of Clinical Medicine, 12(20), 6632. https://doi.org/10.3390/jcm12206632








