Abstract
Introduction and objectives: Heart failure (HF) is a major health problem that causes high mortality and hospitalization rates. This study aims to determine the HF prevalence rates in populations aged both ≥18 years and ≥50 years and to assess its association with cardiovascular diseases and chronic kidney disease. Methods: A cross-sectional observational study was conducted in a primary care setting, with a population-based random sample of 6588 people aged 18.0–102.8 years. Crude and adjusted prevalence rates of HF were calculated. The associations of renal and cardiometabolic factors with HF were assessed in both populations using univariate, bivariate and multivariate analysis. Results: The HF crude prevalence rates were 2.8% (95%CI: 2.4–3.2) in adults (≥18 years), and 4.6% (95%CI: 4.0–5.3) in the population aged ≥ 50 years, without significant differences between males and females in both populations. The age- and sex-adjusted prevalence rates were 2.1% (male: 1.9%; female: 2.3%) in the overall adult population, and 4.5% (male: 4.2%; female: 4.8%) in the population aged ≥ 50 years, reaching 10.0% in the population aged ≥ 70 years. Atrial fibrillation, hypertension, low estimated glomerular filtration rate (eGFR), coronary heart disease (CHD), stroke, sedentary lifestyle, and diabetes were independently associated with HF in both populations. A total of 95.7% (95%CI: 92.7–98.6) of the population with HF had an elevated cardiovascular risk. Conclusions: This study reports that HF prevalence increases from 4.5% in the population over 50 years to 10% in the population over 70 years. The main clinical conditions that are HF-related are sedentary lifestyle, atrial fibrillation, hypertension, diabetes, low eGFR, stroke, and CHD.
1. Introduction
Heart failure (HF) is a complex clinical syndrome that results from any structural and/or functional cardiac disturbances. Any cardiac pathology such as myocardial dysfunction (systolic and/or diastolic), heart valve disease, pericarditis, endocarditis, cardiac rhythm and conduction disturbances can cause or contribute to HF [1,2,3].
HF is usually preceded by diseases or conditions which, in turn, may be the cause of other alterations [1,2,3,4] (Figure S1 Supplementary Materials). The most prevalent causes of HF have changed over time [4,5] and are probably different depending on the economic level of different countries [6]. In developed countries, the main causes associated with HF are coronary heart disease (CHD) and arterial hypertension (HTN) [1,2,3,4,5,6].
On the other hand, patients with HF tend to accumulate other comorbidities (CHD, atrial fibrillation [AF], atrial flutter, peripheral arterial disease, stroke, HTN, anemia, obesity, hypercholesterolemia, diabetes mellitus [DM], rheumatoid arthritis, chronic obstructive pulmonary disease and chronic kidney disease [CKD]), either individually or grouped (mean 3.9 comorbidities per patient, with a range of 0 to 9), and this is more frequent in patients with HF with preserved ejection fraction compared to those with reduced ejection fraction [6]. The presence and control of these comorbidities influence the results and quality of life of patients with HF.
HF diagnosis carries an increased risk of morbidity and mortality. HF is a well-recognized public health problem worldwide that causes an increasing health and economic burden due to numerous hospital admissions and high mortality [7,8]. The age-adjusted incidence of HF is decreasing in developed countries, possibly due to better therapeutic management of the disease, although its overall incidence is increasing due to population ageing [7,8,9,10,11,12].
HF prevalence rates range from 1% to 2% of the adult population. Prevalence increases with age, from less than 1% for those younger than 55 years to >10% in those older than 70 years [8,9,10,11,12,13,14,15,16]. It is likely that the true prevalence of HF is higher because patients with HF are not recognized or diagnosed in a primary care setting, especially those with preserved ejection fraction [17].
A SIMETAP-HF study was designed to determine the crude and adjusted prevalence rates of HF both in the adult population (≥18 years) and in the population older than 50 years and to assess its association with other cardiovascular diseases and CKD.
2. Methods
SIIMETAP-HF is a sub-study of the SIMETAP study [18], a multicenter cross-sectional observational study, authorized by the Health Service of the Community of Madrid (SERMAS according to its initials in Spanish), which 121 physicians participated in. The physicians were selected competitively to reach the necessary sample size and belonged to 64 primary care centers (25.6% from de SERMAS healthcare centers). Simple random sampling of 5.45% of the target population aged 18 years and over (194,073 adults) assigned to GPs was performed using random numbers drawn from the Excel function RAND.BETWEEN (bottom, top). Terminally ill patients or those with cognitive impairments, institutionalized persons, and pregnant women were excluded as per protocol. After a response rate of 62.9%, 6588 study subjects were selected with informed consent and with the necessary clinical and laboratory data to be evaluated. The researchers entered study data from January to December 2015, and collected data based on the most recent biochemical parameters determined from blood and urine tests taken during the previous year. For the purposes of this study, registry of HF diagnosis (International Classification of Diseases, Tenth Revision, Clinical Modification [ICD-10-CM] code: I50; International Classification of Primary Care, 2nd edition [ICPC-2] code: K77) in the patient’s medical record was considered HF, without differentiating by phenotypes based on the measurement of the left ventricular ejection fraction or based on the severity of symptoms and physical activity. The concepts and criteria of the assessed clinical conditions and variables are shown in Table S1 (Supplementary Materials). The study was approved by the Research Commission Deputy Management of Planning and Quality Primary Care—Autonomous Community of Madrid Primary Care Management on 8 November 2010 (Approval Code: 05/2010).
Qualitative variables were analyzed using percentages, a chi-square test, and odds ratios, with a 95% confidence interval (CI). The Shapiro–Wilk test was used to check the data fitting to normal distribution for quantitative variables. If the variables showed normal distribution, they were analyzed using the arithmetic mean, standard deviation (SD) and Student’s t-test or analysis of variance. The median and interquartile range (IQR) of age were determined. Prevalence rates were determined in populations aged ≥18, ≥50, ≥60, and ≥70 years of age. The age- and sex-adjusted prevalence rates were calculated by the direct method, using standardized ten-year age groups of the Spanish population as of January 2015 according to the National Institute of Statistics [19].
Bivariate and multivariate analyses were performed in populations aged ≥18 years and ≥50 years. To assess the individual effect of comorbidities and cardiovascular risk factors (CVRFs) on the dependent variable HF, multivariate logistic regression analysis was performed using the backward stepwise method. Initially, all the variables that showed association in the univariate analysis up to a p-value of <0.10 were introduced into the model, except for erectile dysfunction because it affects only men and CUN-BAE-obesity [20] and metabolic syndrome (MetS) [21] because both variables integrate some factors or criteria assessed independently in the analysis (Table S1, Supplementary Materials). Subsequently, the variable that contributed least to the fit of the analysis was eliminated at each step. All tests were considered statistically significant if the two-tailed p-value was <0.05. The Statistical Package for the Social Sciences was used for the statistical analysis.
3. Results
The study population consisted of 6588 adults aged 18.0–102.8, whose mean (SD) age was 55.1 (17.5) years, and median (IQR) was 54.7 (41.7–68.1) years. The difference in percentage between males (44.1% [95%CI: 42.9–45.3%]) and females (55.9% [95%CI: 54.7–57.1%]) was significant (p < 0.001). The median (IQR) ages of the male and female populations were 55.0 (42.4–67.5) years and 54.5 (41.0–68.8) years, respectively, with the difference in mean (SD) age between males (55.3 [16.9] years) and females (55.0 [18.0] years) being non-significant (p = 0.634).
3.1. HF Prevalence Rates
The crude and adjusted prevalence rates of HF in populations aged ≥18, ≥50, ≥60, and ≥70 years are shown in Table 1. The differences in prevalence rates between males and females were non-significant both globally (≥18 years) and by age group (Figure 1). The distribution of HF prevalence rates by ten-year age group increased according to the polynomial function y = 0.0085x2 − 0.046x + 0.0497 (R2 = 0.911). The prevalence rates were anecdotal in the population aged <50 years (Figure 1).

Table 1.
Heart failure prevalence rates.
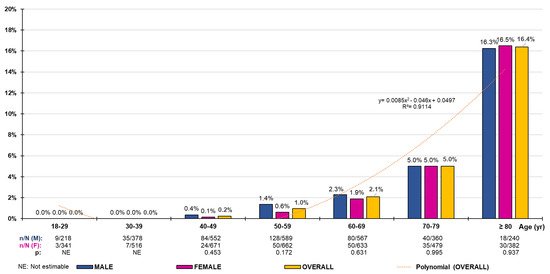
Figure 1.
Heart failure prevalence rates by age group. n: number of cases; N: sample size; M: male; F: female; p: p-value of the difference in percentages (M–F).
3.2. Analysis of Populations ≥18 Years with and without HF
The median (IQR) ages of the populations with and without HF were 80.9 (72.0–88.7) years and 54.3 (41.4–67.2) years, respectively, with the difference in mean (SD) ages (23.9 [95%CI: 21.4–26.4] years) between both populations being significant (p < 0.001) (Table 2). The difference in the female percentage (0.6% [95%CI: −6.7–7.9]) between the populations with and without HF was non-significant (p = 0.868) (Table 3). In the population with HF, the difference in mean (SD) age between males (78.8 [10.2] years) and females (76.4 [12.2] years) was significant (p = 0.040).

Table 2.
Clinical characteristics of populations with and without heart failure.

Table 3.
Risk factors and comorbidities in populations with and without heart failure.
All quantitative clinical variables were significantly higher in the population with HF than in the population without HF, except for diastolic blood pressure, total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), non-HDL-C, low-density lipoprotein cholesterol (LDL-C), non-HDL-C/HDL-C, ALT, and estimated glomerular filtration rate (eGFR), which were significantly higher in the population without HF. The differences in triglycerides (TG), very-low-density lipoprotein cholesterol (VLDL-C), TG/HDL-C, and AST were non-significant (Table 2).
All the ORs of the CVRFs and comorbidities showed a significant association with HF, except for overweight and prediabetes, whose differences were non-significant. The ORs for smoking, alcoholism, and low, moderate, and high cardiovascular risk (CVR) showed a significant association with the population without HF. A total of 95.7% [95%CI: 92.7–98.6]) of the population with HF had a high or very high CVR according to SCORE [22] and SCORE-OP [23] (Table 3). The multivariate analysis showed that AF, HTN, low eGFR, CHD, stroke, low HDL-C, sedentary lifestyle, and DM were independently associated with HF (Table 4).

Table 4.
Clinical conditions and comorbidities independently associated with heart failure.
3.3. Analysis of Populations ≥50 Years with and without HF
The median (IQR) ages of the populations with and without HF were 81.1 (73.3–86.7) years and 65.2 (57.5–74.6) years, respectively, with the difference in mean (SD) ages (12.4 [95%CI: 10.8–14.0] years) between both populations being significant (p < 0.001) (Table 2). The difference in the female percentage (1.9% [95%CI: 5.5–9.3]) between the populations with and without HF was non-significant (p = 0.619) (Table 3). In the population with HF, the difference in mean (SD) age between males (80.2 [9.6] years) and females (77.2 [11.4] years) was close to statistical significance (p = 0.057).
All quantitative clinical variables were significantly higher in the population with HF than in the population without HF, except for diastolic blood pressure, TC, HDL-C, non-HDL-C, LDL-C, non-HDL-C/HDL-C, and eGFR, which were significantly higher in the population without HF. The differences for systolic blood pressure, TG, VLDL-C, TG/HDL-C, triglyceride-glucose (TyG) index, and AST were non-significant (Table 2).
All the ORs of the CVRFs and comorbidities showed a significant association with HF, except for overweight, abdominal obesity, increased WHtR, prediabetes, hypercholesterolaemia, hypertriglyceridaemia, and atherogenic dyslipidemia, whose differences were non-significant. The ORs for smoking, alcoholism and low, moderate and high CVR showed a significant association with the population without HF. A total of 97.2% [95%CI: 94.8–99.6] of the population with HF had a high or very high CVR according to SCORE [22] and SCORE-OP [23] (Table 3). The multivariate analysis showed that the same variables independently associated with HF in the overall adult population were also associated in the population aged ≥50 years (Table 4). The main results are summarized in the Graphical Abstract.
4. Discussion
4.1. HF Prevalence Rates
The healthcare burden of HF is increasing worldwide, probably due to population ageing and lower mortality because of better management of the disease and its associated factors [8,9,10,11,12,13]. Consequently, the use of healthcare resources and hospitalizations readmissions, and outpatient visits due to HF have been increasing [16,24,25,26]. Seferovic et al. [26] showed that the incidence of HF in Spain was 2.76 per 1000 person-years and the prevalence was 12.0 per 1000 persons. The adjusted prevalence rates of HF in the present study increased with age (R2 = 0.911), from 2.1% in the population aged ≥18 years to 10.0% in the population aged ≥70 years, and was slightly higher in females in all age groups. HF cases are concentrated in the older age groups and are anecdotal in those under 50 years of age (Figure 1). It should be noted that the mean age of the subjects with HF in the SIMETAP-HF study (78.4 years) is similar to the mean age found in Störk et al.’s study [27] (76.2 years). The prevalence rates in the PRICE study [28] ranged from 1.3% in the 45–54 age group to 16.1% in those older than 74 years. HF prevalence in the population over 50 years was 4.5%, whereas the PRICE study [28] showed a prevalence of 6.8% in the population over 45 years. We observed that women with HF were younger than men, both in the ≥50 years group (mean 77.2 years [female] vs. 80.2 [male]) and in the ≥18 years group (76.4 years [female] vs. 78.8 [male]), which is probably due to gender differences in terms of predominant etiology (CHD in men vs. HTN and DM in women) [29].
4.2. Clinical Conditions and Factors Associated with HF
In a review by Khan et al. [30], although the prevalence of smoking in patients with HF has been decreasing in recent years, hyperlipidemia, CHD, DM, HTN, CKD and AF have increased over time. The SIMETAP-HF study found that 22 comorbidities were more frequent in the population aged ≥18 years with HF than in non-HF, and they were reduced to 15 when the analysis focused on the population aged ≥50 years (Table 3). Loosen et al.’s study [31] showed that 36 previously defined comorbidities were more frequent in HF patients, but regression analysis showed that only 19 of them were significantly associated with it. The multifactorial analysis performed in SIMETAP-HF showed that sedentary lifestyle, HTN, DM AF, CHD, stroke, and low eGFR were the factors independently associated with HF (Table 4).
Physical inactivity has been associated with an increased risk of HF worsening and all-cause mortality in patients with HF [32]. In our study, 64% of patients with HF had a sedentary lifestyle, and this was independently associated with HF (OR 2.0).
There is a correlation between obesity and adiposity, especially abdominal fat, with cardiovascular disease [33]. The obesity and abdominal obesity prevalence rates were higher in patients with HF (41% and 61%, respectively) than in those without HF (27% and 44%, respectively). A study conducted in China showed that the highest WHtR values (≥0.5) constituted an independent risk factor for all-cause mortality, cardiovascular mortality and HF rehospitalization [34]. In patients with HF in the present study, the prevalence of elevated WHtR was 76%. Adiposity was also highly prevalent among HF patients in our study. The Jackson Heart study showed that visceral adiposity was associated with hospitalization for incident HF, pericardial adiposity and mortality [35].
HTN is the clinical condition most frequently associated with HF. A systematic review of HTN trials concluded that 28.9% of hypertensive patients had developed HF [36]. We found that more than 90% of patients with HF had HTN. Pulse pressure has also been linked to CVR [37]. Pulse pressure in the present study was higher in subjects with HF than in those without HF. Hypercholesterolemia and low HDL-C levels were also more common in HF patients. High levels of non-HDL cholesterol or low HDL-C levels are associated with the HF incidence [38].
Abnormal glucose regulation and DM maintain a close and bidirectional relationship with HF, and the presence of DM increases mortality and hospitalizations in patients with HF [39]. Up to 27% and 42% of patients with HF in the SIMETAP-HF study had prediabetes and DM, respectively. Insulin resistance is the link between DM and MetS. In our study, the MetS prevalence in patients with HF (82%) was similar to that shown in other studies [40].
AF is strongly associated with an increased risk of HF as these closely related pathologies that often coexist predispose to each other and share risk factors such as HTN, DM, CHD, and valve disease [41,42,43]. The present study shows a strong association of AF with HF (OR 11.5) due to the higher prevalence of AF in patients with HF (46.4%) than the Loosen et al., study [31] (18.6%). In order to better differentiate between the associations of the main clinical conditions or comorbidities with HF, Figure 2A,B show the results of multivariate analysis, including or not including AF, respectively. AF prevalence in the subjects with HF in our study (46%) is intermediate compared to that of other studies [32,42,43]. The differences are probably related to the study design, the age groups analyzed, the control of CVRFs associated with HF, and the greater or lesser availability of echocardiography or natriuretic peptides to diagnose HF in suspected cases.
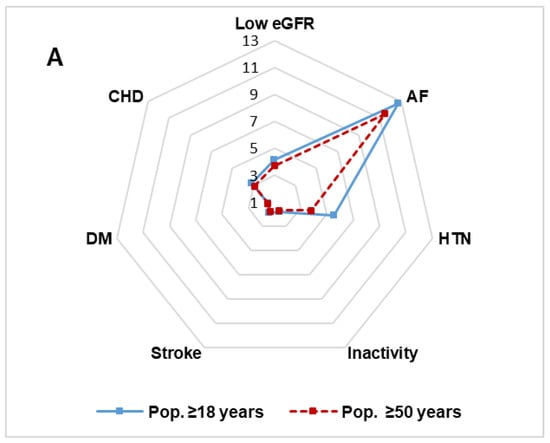
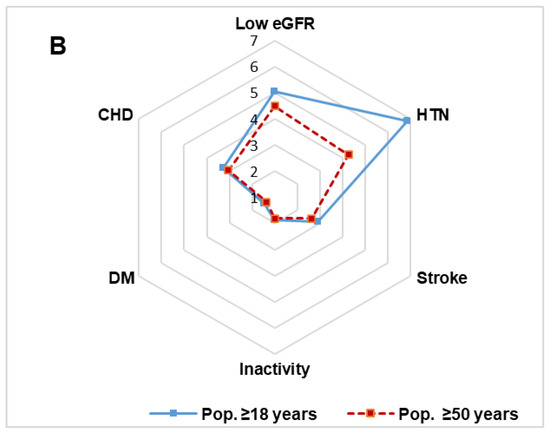
Figure 2.
Radar chart of clinical conditions and comorbidities independently associated with heart failure. (A). Multivariate analysis of factors associated with HF. (B). Multivariate analysis of factors associated with HF excluding AF. Numbers: odds ratio; AF: atrial fibrillation; CHD: coronary heart disease. DM: diabetes mellitus; HTN: hypertension; Inactivity: sedentary lifestyle; Low eGFR: estimated glomerular filtration rate <60 mL/min/1.73 m2.
Erectile dysfunction is an early predictor of cardiovascular events and HF, and HF itself can worsen sexual health due to its comorbidities. In our study, 71% of patients with HF had erectile dysfunction, similar to the other studies [44] (80%). The heart and kidneys act synergistically to maintain blood pressure and homeostasis such that any alteration of one of them leads to the deterioration of the other [45,46]. In the present study, the presence of low eGFR (48%) and CKD (55%) in patients with HF is in line with findings in the Löfman et al., study [47], in which 51% of FH patients had a low eGFR.
CHD is the main etiological factor in patients with HF [46,48]. The German EuroAspire IV cohort study [49] showed that 44.2% of patients with CHD had HF. Our study reports that about 30% of patients with HF had CHD, which is similar to the Swedish population and higher than the Chinese population [50]. The study by Loosen et al. [31] reported a lower association with HF (HR 1.5) probably because the median age of the population without HF (76 years) was much higher than that of our study (54.3 years).
The high prevalence of all these conditions, the metabolic, renal and cardiovascular factors suffered by patients with HF, and the mean age (78.4 years) justifies that more than 85% of the subjects have a very high CVR.
4.3. Strengths and Limitations
The main limitations of this study were the inability to determine causality or to estimate incidence rates, inter-interviewer variability, possible under-reporting in the medical records of the HF diagnosis, possible heterogeneity of the measurement and laboratory equipment, and HF underdiagnoses due to the per protocol exclusion of pregnant women, the terminally ill, and institutionalized or cognitively impaired patients. The main strengths include the population-based random selection, a large sample with people aged 18.0–102.8 years, the determination of both crude and adjusted prevalence rates of HF, and the assessment of the possible association of HF with numerous cardiometabolic and renal variables.
4.4. Clinical Implications
The high prevalence of HF in the population over 50 years of age entails serious socioeconomic and health consequences due to the increase in hospitalizations due to HF and cardiovascular mortality. Assessing the epidemiological magnitude of HF is essential to better plan prevention policies aimed at reducing the high healthcare and economic burden that it causes, both in primary care and in a hospital setting, to optimize available health resources and to improve medical care and quality of life for patients. HF is strongly influenced by age after 50 years, so its prevalence rates should always be age-adjusted to compare them with other populations. We hope that this study improves knowledge of HF prevalence and that it contributes to understanding the importance and magnitude of CVRFs and comorbidities associated with HF.
5. Conclusions
HF is a complex syndrome that constitutes a serious health problem worldwide, closely related to the aging of the population, which accumulates a constellation of comorbidities that accelerate its progression and increase the risk of mortality and hospitalization.
The assessment of the current prevalence of HF among the adult population and its association with ASCVD and CKD is crucial because it can help in the rational management of patients with HF. This study investigated the crude and adjusted prevalence rates of HF and its comorbid conditions. It confirmed the close relationship between age and the prevalence of HF, without differences by sex, being 2.1% in the adult population, 4.6% in those ≥50 years, and reaching 10% in those ≥70 years. The confluence of all the comorbidities independently associated with HF and the patients’ ageing determined that their CVR was very high.
The early detection of HF-related comorbidities will allow the comprehensive management of HF, which would include healthy lifestyle modifications, and an approach to obesity, HTN, and DM, which would delay the worsening of HF and the development of AF, CKD, and ASCVD.
6. Key Points
6.1. What Is Known about the Topic?
- Heart failure prevalence rates vary according to the income and development of countries.
- Although heart failure mortality is stabilizing over time, heart failure hospitalization is increasing due to population ageing, which carries a high economic and healthcare burden.
- There are many cardiometabolic and renal factors associated with heart failure.
6.2. What Does This Study Add?
- Heart failure is strongly influenced by age after 50 years.
- Heart failure prevalence rates increase from 2.1% in the overall adult population to 10% in people over 70 years.
- Physicians should be aware that atrial fibrillation, hypertension, diabetes, coronary heart disease, stroke, low estimated glomerular filtration rate and sedentary lifestyle are clinical conditions independently associated with heart failure.
- Knowing the cardiometabolic and renal factors associated with heart failure would facilitate its early detection and management to reduce its severity and hospitalization rates.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm12154924/s1, Figure S1: Causes, comorbidities and complications of heart failure; Table S1: Variables or clinical conditions criteria.
Author Contributions
Conceptualization, A.S.-C., C.E.-C., E.A.-M., M.T.-Y. and V.P.-C.; Methodology, A.R.-G., A.S.-C., C.E.-C., E.A.-M., M.T.-Y. and V.P.-C.; Validation, A.R.-G., C.E.-C., E.A.-M., M.T.-Y. and V.P.-C.; Formal analysis, A.R.-G., A.S.-C., C.E.-C. and V.P.-C.; Investigation, A.R.-G., A.S.-C., E.A.-M., M.T.-Y. and V.P.-C.; Resources, A.R.-G., V.P.-C. and V.P.-C.; Data curation, A.R.-G., C.E.-C., M.T.-Y. and V.P.-C.; Writing—original draft, A.R.-G.; Writing—review & editing, A.R.-G., A.S.-C., C.E.-C., E.A.-M., M.T.-Y. and V.P.-C. All authors have read and agreed to the published version of the manuscript.
Funding
The “Pedro Laín Entralgo” Agency for Training, Research and Health Studies of the Community of Madrid (number: RS05/2010) provided economic funding for carrying out this study. The Investigation Commission of the Deputy Management of Planning and Quality of the Primary Care Management of the Community of Madrid issued the favorable report for its realization.
Institutional Review Board Statement
The study was approved by the Research Commission Deputy Management of Planning and Quality Primary Care—Autonomous Community of Madrid Primary Care Management on 8 November 2010 (Approval Code: 05/2010).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Research data is available upon reasonable request.
Acknowledgments
We are grateful for the effort, dedication, and collaboration provided by of the following physicians who have participated in the SIMETAP Study Research Group: Abad Schilling C., Adrián Sanz M., Aguilera Reija P., Alcaraz Bethencourt A., Alonso Roca R., Álvarez Benedicto R., Arranz Martínez E., Arribas Álvaro P., Baltuille Aller M.C., Barrios Rueda E., Benito Alonso E., Berbil Bautista M.L., Blanco Canseco J.M., Caballero Ramírez N., Cabello Igual P., Cabrera Vélez R., Calderín Morales M.P., Capitán Caldas M., Casaseca Calvo T.F., Cique Herráinz J.A., Ciria de Pablo C., Chao Escuer P., Dávila Blázquez G., de la Peña Antón N., de Prado Prieto L., del Villar Redondo M.J., Delgado Rodríguez S., Díez Pérez M.C., Durán Tejada M.R., Escamilla Guijarro N., Escrivá Ferrairó R.A., Fernández Vicente T., Fernández-Pacheco Vila D., Frías Vargas M.J., García Álvarez J.C., García Fernández M.E., García García Alcañiz M.P., García Granado M.D., García Pliego R.A., García Redondo M.R., García Villasur M.P., Gómez Díaz E., Gómez Fernández O., González Escobar P., González-Posada Delgado J.A., Gutiérrez Sánchez I., Hernández Beltrán M.I., Hernández de Luna M.C., Hernández López R.M., Hidalgo Calleja Y., Holgado Catalán M.S., Hombrados Gonzalo M.P., Hueso Quesada R., Ibarra Sánchez A.M., Iglesias Quintana J.R., Íscar Valenzuela I., Iturmendi Martínez N., Javierre Miranda A.P., López Uriarte B., Lorenzo Borda M.S., Luna Ramírez S., Macho del Barrio A.I., Magán Tapia P., Marañón Henrich N., Mariño Suárez J.E., Martín Calle M.C., Martín Fernández A.I., Martínez Cid de Rivera E., Martínez Irazusta J., Migueláñez Valero A., Minguela Puras M.E., Montero Costa A., Mora Casado C., Morales Cobos L.E., Morales Chico M.R., Moreno Fernández J.C., Moreno Muñoz M.S., Palacios Martínez D., Pascual Val T., Pérez Fernández M., Pérez Muñoz R., Plata Barajas M.T., Pleite Raposo R., Prieto Marcos M., Quintana Gómez J.L., Redondo de Pedro S., Redondo Sánchez M., Reguillo Díaz J., Remón Pérez B., Revilla Pascual E., Rey López A.M., Ribot Catalá C., Rico Pérez M.R., Rivera Teijido M., Rodríguez Cabanillas R., Rodríguez de Cossío A., Rodríguez De Mingo E., Rodríguez Rodríguez A.O., Rosillo González A., Rubio Villar M., Ruiz Díaz L., Ruiz García A., Sánchez Calso A., Sánchez Herráiz M., Sánchez Ramos M.C., Sanchidrián Fernández P.L., Sandín de Vega E., Sanz Pozo B., Sanz Velasco C., Sarriá Sánchez M.T., Simonaggio Stancampiano P., Tello Meco I., Vargas-Machuca Cabañero C., Velazco Zumarrán J.L., Vieira Pascual M.C., Zafra Urango C., Zamora Gómez M.M., Zarzuelo Martín N.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| AF | atrial fibrillation |
| ASCVD | atherosclerotic cardiovascular disease |
| CHD | coronary heart disease |
| CKD | chronic kidney disease |
| CVR | cardiovascular risk |
| CVRFs | cardiovascular risk factors |
| DM | diabetes mellitus |
| eGFR | estimated glomerular filtration rate |
| HF | heart failure |
| HTN | arterial hypertension |
References
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef] [PubMed]
- Bozkurt, B.; Coats, A.J.S.; Tsutsui, H.; Abdelhamid, C.M.; Adamopoulos, S.; Albert, N.; Anker, S.D.; Atherton, J.; Böhm, M.; Butler, J.; et al. Universal definition and classification of heart failure: A report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: Endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. Eur. J. Heart Fail. 2021, 23, 352–380. [Google Scholar] [PubMed]
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA Guideline for the management of heart failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2022, 79, e263–e421. [Google Scholar]
- McMurray, J.J.; Stewart, S. Epidemiology, aetiology, and prognosis of heart failure. Heart 2000, 83, 596–602. [Google Scholar] [CrossRef]
- Screever, E.M.; van der Wal, M.H.L.; van Veldhuisen, D.J.; Jaarsma, T.; Koops, A.; van Dijk, K.S.; Warink-Riemersma, J.; Coster, J.E.; Westenbrink, B.D.; van der Meer, P.; et al. Comorbidities complicating heart failure: Changes over the last 15 years. Clin. Res. Cardiol. 2023, 112, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, S.; Rangarajan, S.; Teo, K.; Islam, S.; Li, W.; Liu, L.; Bo, J.; Lou, Q.; Lu, F.; Liu, T.; et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N. Engl. J. Med. 2014, 371, 818–827. [Google Scholar] [CrossRef] [PubMed]
- Savarese, G.; Lund, L.H. Global public health burden of heart failure. Card. Fail. Rev. 2017, 3, 7–11. [Google Scholar] [CrossRef]
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef] [PubMed]
- Conrad, N.; Judge, A.; Tran, J.; Mohseni, H.; Hedgecott, D.; Crespillo, A.P.; Allison, M.; Hemingway, H.; Cleland, J.G.; McMurray, J.J.V.; et al. Temporal trends and patterns in heart failure incidence: A population-based study of 4 million individuals. Lancet 2018, 391, 572–580. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Sanchis-Gomar, F. Global epidemiology and future trends of heart failure. AME Med. J. 2020, 5, 15. [Google Scholar] [CrossRef]
- Siontis, G.C.; Bhatt, D.L.; Patel, C.J. Secular trends in prevalence of heart failure diagnosis over 20 years (from the US NHANES). Am. J. Cardiol. 2022, 172, 161–164. [Google Scholar] [CrossRef]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Beaton, A.Z.; Boehme, A.K.; Buxton, A.E.; et al. Heart disease and stroke statistics-2023 update: A report from the American Heart Association. Circulation 2023, 147, e93–e621. [Google Scholar] [CrossRef] [PubMed]
- Ceia, F.; Fonseca, C.; Mota, T.; Morais, H.; Matias, F.; de Sousa, A.; Oliveira, A.; EPICA Investigators. Prevalence of chronic heart failure in Southwestern Europe: The EPICA study. Eur. J. Heart Fail. 2002, 4, 531–539. [Google Scholar] [CrossRef]
- Bibbins-Domingo, K.; Pletcher, M.J.; Lin, F.; Vittinghoff, E.; Gardin, J.M.; Arynchyn, A.; Lewis, C.E.; Williams, O.D.; Hulley, S.B. Racial differences in incident heart failure among young adults. N. Engl. J. Med. 2009, 360, 1179–1190. [Google Scholar] [CrossRef]
- Van Riet, E.E.; Hoes, A.W.; Wagenaar, K.P.; Limburg, A.; Landman, M.A.; Rutten, F.H. Epidemiology of heart failure: The prevalence of heart failure and ventricular dysfunction in older adults over time. A systematic review. Eur. J. Heart Fail. 2016, 18, 242–252. [Google Scholar] [CrossRef]
- Smeets, M.; Vaes, B.; Mamouris, P.; van den Akker, M.; van Pottelbergh, G.; Goderis, G.; Janssens, S.; Aertgeerts, B.; Henrard, S. Burden of heart failure in Flemish general practices: A registry-based study in the Intego database. BMJ Open 2019, 9, e022972. [Google Scholar] [CrossRef]
- Van Riet, E.E.; Hoes, A.W.; Limburg, A.; Landman, M.A.; van der Hoeven, H.; Rutten, F.H. Prevalence of unrecognized heart failure in older persons with shortness of breath on exertion. Eur. J. Heart Fail. 2014, 16, 772–777. [Google Scholar] [CrossRef]
- Ruiz-García, A.; Arranz-Martínez, E.; García-Álvarez, J.C.; Morales-Cobos, L.E.; García-Fernández, M.E.; de la Peña-Antón, N.; Martín Calle, M.C.; Díez Pérez, M.C.; Montero Costa, A.; Palacios Martínez, D.; et al. Population and methodology of the SIMETAP study: Prevalence of cardiovascular risk factors, cardiovascular diseases, and related metabolic diseases. Clin. Investig. Arterioscler. 2018, 30, 197–208. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística. INEbase. Demografía y Población. Cifras de Población y Censos Demográficos. Cifras de Población. Available online: http://www.ine.es/dynt3/inebase/es/index.htm?padre=1894&capsel=1895 (accessed on 30 June 2023).
- Gómez-Ambrosi, J.; Silva, C.; Catalán, V.; Rodríguez, A.; Galofré, J.C.; Escalada, J.; Valentí, V.; Rotellar, F.; Romero, S.; Ramírez, B.; et al. Clinical usefulness of a new equation for estimating body fat. Diabetes Care 2012, 35, 383–388. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr.; et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation task force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice. The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar]
- Cooney, M.T.; Selmer, R.; Lindman, A.; Tverdal, A.; Menotti, A.; Thomsen, T.; DeBacker, G.; de Bacquer, D.; Tell, G.S.; Njolstad, I.; et al. Cardiovascular disease risk estimation in older persons: SCORE O. P. Eur. J. Prev. Cardiol. 2016, 23, 1093–1103. [Google Scholar] [CrossRef]
- Bonilla-Palomas, J.L.; Anguita-Sánchez, M.P.; Elola-Somoza, F.J.; Bernal-Sobrino, J.L.; Fernández-Pérez, C.; Ruiz-Ortiz, M.; Jiménez-Navarro, M.; Bueno-Zamora, H.; Cequier-Fillat, Á.; Marín-Ortuño, F. Thirteen-year trends in hospitalization and outcomes of patients with heart failure in Spain. Eur. J. Clin. Investig. 2021, 51, e13606. [Google Scholar] [CrossRef]
- Escobar, C.; Palacios, B.; Varela, L.; Gutiérrez, M.; Duong, M.; Chen, H.; Justo, N.; Cid-Ruzafa, J.; Hernández, I.; Hunt, P.R.; et al. Healthcare resource utilization and costs among patients with heart failure with preserved, mildly reduced, and reduced ejection fraction in Spain. BMC Health Serv. Res. 2022, 22, 1241. [Google Scholar] [CrossRef]
- Seferović, P.M.; Vardas, P.; Jankowska, E.A.; Maggioni, A.P.; Timmis, A.; Milinković, I.; Polovina, M.; Gale, C.P.; Lund, L.H.; Lopatin, Y.; et al. The Heart Failure Association Atlas: Heart failure epidemiology and management statistics 2019. Eur. J. Heart Fail. 2021, 23, 906–914. [Google Scholar] [CrossRef]
- Störk, S.; Handrock, R.; Jacob, J.; Walker, J.; Calado, F.; Lahoz, R.; Hupfer, S.; Klebs, S. Epidemiology of heart failure in Germany: A retrospective database study. Clin. Res. Cardiol. 2017, 106, 913–922. [Google Scholar] [CrossRef]
- Anguita Sánchez, M.; Crespo Leiro, M.; de Teresa, G.E.; Jiménez Navarro, M.; Alonso-Pulpón, L.; Muñiz, G.J.; PRICE Study Investigators. Prevalence of heart failure in the Spanish general population aged over 45 years. The PRICE Study. Rev. Esp. Cardiol. 2008, 61, 1041–1049. [Google Scholar] [CrossRef]
- Regitz-Zagrosek, V. Sex and gender differences in heart failure. Int. J. Heart Fail. 2020, 2, 157–181. [Google Scholar] [CrossRef]
- Khan, M.S.; Tahhan, A.S.; Vaduganathan, M.; Greene, S.J.; Alrohaibani, A.; Anker, S.D.; Vardeny, O.; Fonarow, G.C.; Butler, J. Trends in prevalence of comorbidities in heart failure clinical trials. Eur. J. Heart Fail. 2020, 22, 1032–1042. [Google Scholar] [CrossRef]
- Loosen, S.H.; Roderburg, C.; Curth, O.; Gaensbacher, J.; Joerdens, M.; Luedde, T.; Konrad, M.; Kostev, K.; Luedde, M. The spectrum of comorbidities at the initial diagnosis of heart failure a case control study. Sci. Rep. 2022, 12, 2670. [Google Scholar] [CrossRef]
- Park, L.G.; Dracup, K.; Whooley, M.A.; McCulloch, C.; Lai, S.; Howie-Esquivel, J. Sedentary lifestyle associated with mortality in rural patients with heart failure. Eur. J. Cardiovasc. Nurs. 2019, 18, 318–324. [Google Scholar] [CrossRef]
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Després, J.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and cardiovascular disease. a scientific statement from the American Heart Association. Circulation 2021, 143, e984–e1010. [Google Scholar] [CrossRef]
- Chen, J.; Li, M.; Hao, B.; Cai, Y.; Li, H.; Zhou, W.; Song, Y.; Wang, S.; Liu, H. Waist to height ratio is associated with an increased risk of mortality in Chinese patients with heart failure with preserved ejection fraction. BMC Cardiovasc. Disord. 2021, 21, 263. [Google Scholar] [CrossRef]
- Rao, V.N.; Bush, C.G.; Mongraw-Chaffin, M.; Hall, M.E.; Clark, D.; Fudim, M.; Correa, A.; Hammill, B.G.; O’Brien, E.; Min, Y.I.; et al. Regional adiposity and risk of heart failure and mortality: The Jackson Heart Study. J. Am. Heart Assoc. 2021, 10, e020920. [Google Scholar] [CrossRef]
- Tocci, G.; Sciarretta, S.; Volpe, M. Development of heart failure in recent hypertension trials. J. Hypertens. 2008, 26, 1477–1486. [Google Scholar] [CrossRef]
- Moyá-Amengual, A.; Ruiz-García, A.; Pallarés-Carratalá, V.; Serrano-Cumplido, A.; Prieto-Díaz, M.Á.; Segura-Fragoso, A.; Cinza-Sanjurjo, S.; IBERICAN Study. Elevated pulse pressure and cardiovascular risk associated in Spanish population attended in primary care: IBERICAN study. Front. Cardiovasc. Med. 2023, 10, 1090458. [Google Scholar] [CrossRef]
- Velagaleti, R.S.; Massaro, J.; Vasan, R.S.; Robins, S.J.; Kannel, W.B.; Levy, D. Relations of lipid concentrations to heart failure incidence: The Framingham Heart Study. Circulation 2009, 120, 2345–2351. [Google Scholar] [CrossRef]
- Pop-Busui, R.; Januzzi, J.L.; Bruemmer, D.; Butalia, S.; Green, J.B.; Horton, W.B.; Knight, C.; Levi, M.; Rasouli, N.; Richardson, C.R.; et al. Heart failure: An underappreciated complication of diabetes. a consensus report of the American Diabetes Association. Diabetes Care 2022, 45, 1670–1690. [Google Scholar] [CrossRef]
- Miura, Y.; Fukumoto, Y.; Shiba, N.; Miura, T.; Shimada, K.; Iwama, Y.; Takagi, A.; Matsusaka, H.; Tsutsumi, T.; Yamada, A.; et al. Prevalence and clinical implication of metabolic syndrome in chronic heart failure—Report from MetS-CHF Study. Circ. J. 2010, 74, 2612–2621. [Google Scholar] [CrossRef]
- Bizhanov, K.A.; Abzaliyev, K.B.; Baimbetov, A.K.; Sarsenbayeva, A.B.; Lyan, E. Atrial fibrillation: Epidemiology, pathophysiology, and clinical complications (literature review). J. Cardiovasc. Electrophysiol. 2023, 34, 153–165. [Google Scholar] [CrossRef]
- Ruddox, V.; Sandven, I.; Munkhaugen, J.; Skattebu, J.; Edvardsen, T.; Otterstad, J.E. Atrial fibrillation and the risk for myocardial infarction, all-cause mortality and heart failure: A systematic review and meta-analysis. Eur J Prev Cardiol 2017, 24, 1555–1566. [Google Scholar] [CrossRef]
- Krisai, P.; Johnson, L.S.B.; Moschovitis, G.; Benz, A.; Ramasundarahettige, C.; McIntyre, W.F.; Wong, J.A.; Conen, D.; Sticherling, C.; Connolly, S.J.; et al. Incidence and predictors of heart failure in patients with atrial fibrillation. CJC Open 2021, 3, 1482–1489. [Google Scholar] [CrossRef]
- Zeighami-Mohammadi, S.; Shahparian, M.; Fahidy, F.; Fallah, E. Sexual dysfunction in males with systolic heart failure and associated factors. ARYA Atheroscler. 2012, 8, 63–69. [Google Scholar]
- Szlagor, M.; Dybiec, J.; Młynarska, E.; Rysz, J.; Franczyk, B. Chronic kidney disease as a comorbidity in heart failure. Int. J. Mol. Sci. 2023, 24, 2988. [Google Scholar] [CrossRef]
- Rehm, M.; Rothenbacher, D.; Iacoviello, L.; Costanzo, S.; Tunstall-Pedoe, S.; Fitton, C.A.; Söderberg, S.; Hultdin, J.; Salomaa, V.; Jousilahti, P.; et al. Chronic kidney disease and risk of atrial fibrillation and heart failure in general population-based cohorts: The BiomarCaRE Project. ESC Heart Fail. 2022, 9, 57–65. [Google Scholar] [CrossRef]
- Löfman, I.; Szummer, K.; Hagerman, I.; Dahlström, U.; Lund, L.H.; Jernberg, T. Prevalence and prognostic impact of kidney disease on heart failure patients. Open Heart 2016, 3, e000324. [Google Scholar] [CrossRef]
- Pagliaro, B.R.; Cannata, F.; Stefanini, G.G.; Bolognese, L. Myocardial ischemia and coronary disease in heart failure. Heart Fail. Rev. 2020, 25, 53–65. [Google Scholar] [CrossRef]
- Morbach, C.; Wagner, M.; Güntner, S.; Malsch, C.; Oezkur, M.; Wood, D.; Kotseva, K.; Leyh, R.; Ertl, G.; Karmann, W.; et al. Heart failure in patients with coronary heart disease: Prevalence, characteristics and guideline implementation—Results from the German EuroAspire IV cohort. BMC Cardiovasc. Disord. 2017, 17, 108. [Google Scholar] [CrossRef]
- Feng, Y.; Chen, X.; Schaufelberger, M.; Zhang, Q.; Fu, M. Patient-level comparison of heart failure patients in clinical phenotype and prognosis from China and Sweden. BMC Cardiovasc. Disord. 2022, 22, 91. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).