Abstract
Arrhythmias (ARs) are potential cardiovascular complication of COVID-19 but may also have a prognostic role. The aim of this study was to explore the prevalence and impact of cardiac ARs in hospitalized COVID-19 patients. All-comer patients admitted to the emergency department of Modena University Hospital from 16 March to 31 December 2020 and diagnosed with COVID-19 pneumonia infection were included in the study. The primary endpoint was 30-day mortality. Out of 902 patients, 637 (70.6%) presented a baseline 12-lead ECG registration; of these, 122 (19.2%) were diagnosed with ARs. Atrial fibrillation (AF, 40.2%) was the most frequent AR detected. The primary endpoint (30-day mortality) occurred in 33.6% (p < 0.001). AR-patients presented an almost 3-fold risk of mortality compared to non-AR-patients at 30d (Adj. OR = 2.8, 95%CI: 1.8–4.3, p < 0.001). After adjustment for significant baseline characteristics selected by a stepwise backward selection, AR-patients remained at increased risk of mortality (Adj. HR = 2.0, 95%CI: 1.9–2.3, p < 0.001). Sub-group analysis revealed that among ARs patients, those with AF at admission presented the highest risk of 30-day mortality (Adj. HR = 3.1, 95%CI: 2.0–4.9, p < 0.001). In conclusion, ARs are a quite common manifestation in COVID-19 patients, who are burdened by even worse prognosis. AR patients with AF presented the highest risk of mortality; thus, these patients may benefit from a more aggressive secondary preventive therapy and a closer follow up.
1. Introduction
Coronavirus disease (COVID-19) with severe acute respiratory syndrome (SARS) due to a novel Coronavirus (CoV-2) has rapidly spread worldwide [1]; as of 25 December 2021, over 278 million confirmed cases and nearly 5.3 million deaths were reported globally by the WHO [2]. The COVID-19 pandemic out broke in our regions at the end of February 2020, with a significant impact on cardiovascular hospitalization rate [3]. Arrhythmias (ARs) represent quite common complications of COVID-19 disease, particularly in patients admitted to intensive care units (ICU) [4]. Prevalence and type of ARs in COVID-19 patients vary across different studies [5]. Mechanisms of ARs development in COVID-19 patients are still not completely defined, although they have been already investigated in several papers [6,7,8]. Nevertheless, ARs onset in COVID-19 patients has been associated with increased mortality [9,10]. The aim of the present study was to investigate prevalence and impact on outcome of ARs at admission in hospitalized COVID-19 patients.
2. Materials and Methods
All-comer patients admitted to the Emergency Department of Modena University Hospital from 16 March to 31 December 2020 with confirmed COVID-19 pneumonia by positive nasopharyngeal swab and typical radiological features on chest X-ray were enrolled in the study. Clinical data, including outcome, were extracted from medical records. Venous and arterial blood samples for blood gas analysis were collected at the time of hospitalization and thereafter based on clinical indication. We used 12-lead ECG with 25 mm/s and 1 mV/cm calibration and 0.05–150 Hz filter setting. ECG traces were recorded and analysed offline. The following ECG parameters were considered: heart rate (HR), presence of ST-T abnormalities and corrected QT interval (msec), this latter was measured as the time between the start of the Q wave and the end of the T wave, corrected by HR according to Bazett’s formula. Rhythm and conduction alterations were also considered. The primary endpoint was 30-day mortality.
Statistical Analysis
Continuous variables were expressed as medians and interquartile ranges, while categorical data were expressed as absolute values and proportions. Variables were compared between patient survivors and non-survivors at 30 days by using the Fisher exact test and the t-test, as appropriate. Survival curves were plotted using the Kaplan–Meier method with log-rank test and COX-regression model was applied. Analyses were performed with SPSS (Statistical Package for Social Science) software (v26, SPSS Inc., Chicago, IL, USA). For all the statistical analyses, p < 0.05 was considered significant.
3. Results
Baseline characteristics are summarized in Table 1.

Table 1.
Baseline characteristics.
Out of 902 COVID-19 patients enrolled, 637 (70.6%) underwent baseline 12-lead ECG at admission; of these, 122 (19.2%) were diagnosed with ARs. Compared to those without ARs, ARs patients were older (75.5 vs. 72, p < 0.001), with a more complex CV-history (hypertension, CA, CKD, AF (all p < 0.05). Symptoms and vital parameters did not differ between Ars and no-Ars patients. QTc interval prolongation (483 vs. 440 msec, p < 0.001) and conduction abnormalities (27.0% vs. 19.2%, p = 0.039) were more commonly found in Ars patients. These patients presented more frequently with lower levels of total white blood cells count (7.2 vs. 7.9, p = 0.042). AF (40.2%) and sinus bradycardia (29.5%) were the most common AR revealed at baseline 12-lead ECG (Figure 1, Panel a).
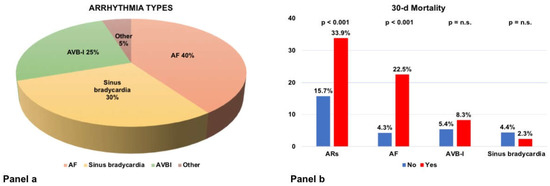
Figure 1.
Panel (a): types of arrhythmias. Panel (b): 30-day mortality across ARs types.
The primary endpoint occurred significantly higher in ARs patients (33.9% vs. 15.7%, p < 0.001, Figure 1, Panel b).
AR patients presented an almost 3-fold risk of mortality compared to non-AR patients at 30d (Adj. OR = 2.8, 95%CI: 1.8–4.3, p < 0.001). After adjustment for significant baseline characteristics selected by a stepwise backward selection (Table 2), AR patients remained at increased risk of mortality (Adj. HR = 2.0, 95%CI: 1.9–2.3, p < 0.001, Figure 2a). Sub-group analysis revealed that among ARs patients, those with AF at admission presented the highest risk of 30-day mortality (Adj. HR = 3.1, 95%CI: 2.0–4.9, p < 0.001, Figure 2b).

Table 2.
Baseline characteristics used for the multivariate analysis. ARs = arrhythmias; CAD = coronary artery disease.
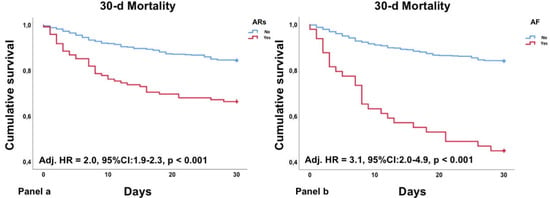
Figure 2.
KM curves describing 30-day mortality for ARs (Panel (a)) and AF (Panel (b)).
4. Discussion
Cardiovascular diseases have been associated with worse prognosis in COVID-19 patients [11,12]. Recent evidence underlined whether arrhythmias may negatively affect outcome in this setting [13]. In this retrospective real-world cohort of COVID-19 patients, we confirmed a high short-term mortality, particularly in patients with baseline Ars, and we obtained the following novel key findings: (1) ARs at admission are quite common in COVID-19 infection and related to a higher risk of mortality; (2) among ARs, AF at admission has been associated with the highest risk of mortality; (3) myocardial biomarkers resulted higher in ARs patients compared to non-ARs patients, as an expression of a more severe disease with multi-organ-failure manifestation.
ARs at admission are frequently revealed in COVID-19 patients, particularly in critical conditions that require ICU admission [14]. ARs represent a common complication of COVID-19 disease with a prevalence as high as almost 50% in COVID-19 patients admitted to ICU [15]. Supraventricular ARs are commonly found in adult population and characterized up to one-fifth of COVID-19 patients [16], while ventricular ARs, such as ventricular tachycardia/fibrillation, are less frequently detected in this population. Bathla and colleagues reported an overall incidence of ARs of 7.5%, which is much higher in ICU patients [6]. The heightened risk of ARs in COVID-19 patients is related to different risk factors, primarily older age as well as comorbidities, the hyperinflammatory response typical of critical conditions, the direct effect of SARS-CoV-2 on myocardial tissue and the administration of pro-arrhythmic drugs. Being elderly is per se a risk factor for Ars development [17], and AF is the most common AR in adult population [18]. Race has been also associated with increased risk of ARs in COVID-19 patients in presence of a sodium channel variant that predispose to ARs [19]. Hypertension, diabetes, coronary artery disease and higher BMI have been also associated with higher risk of ARs development in COVID-19 patients [20,21]. Regardless the underlying mechanism, ARs have been associated with increased mortality in COVID-19 patients [12]. Baseline ECG abnormalities may be useful, in this setting, to predict the risk of cardiac arrest in COVID-19 patients [22]. In our cohort we found an incidence of baseline ARs around 20%, in line with data in the literature; these patients experienced a 2-fold risk of mortality, as reported in the results section. High heart rate, particularly sinus tachycardia, has been associated with higher inflammatory biomarkers and prolonged hospitalization in COVID-19 patients, but not with higher risk of thromboembolic events [23]. Sinus tachycardia resulted the most common ARs in a small cohort of COVID-19 patients, and survivors were less tachycardic than non-survivors [24]. In this context, heart rate variability (HRV) has been investigated and associated with the severity of COVID-19 disease, suggesting a potential role as non-invasive predictor for clinical outcome [25]. Recent evidence showed greater chances of survival in older COVID-19 patients with higher HRV [26].
AF is the most common AR in the adult population, with a global prevalence varying from 2% to 4% according to ESC guidelines [18]. Risk factors for AF include age, hypertension, COPD and other comorbidities. We demonstrated that COVID-19 patients with AF at baseline ECG presented almost a 3-fold risk of death compared to the non-AF-group. This finding is higher compared to previous data [27]. Reasons for this discrepancy may be related to the mean higher CHA2DSVASc of AF patients, which reflects the broad spectrum of comorbidities of this subpopulation. Although AF itself has been associated with being an independent predictor of mortality in COVID-19 patients, the distinction should be made between the role of AF and that of comorbidities on outcome. CHA2DS2VASc score, indeed, has been associated with increased mortality in COVID-19 patients, with an acceptable discriminatory power [28]. Nevertheless, AF seems to be a prognostic risk factor in COVID-19 patients independently from the burden of concomitant comorbidities [29]. Thus, AF may represent a useful clinical marker to identify COVID-19 patients at higher risk of death that should benefit from closer monitoring and more intensive therapy. Our study showed that AF at baseline ECG was characterized by a 3-fold higher risk of death compared to patients with no-AF at baseline ECG, whereas a history of AF had a 2-fold higher risk of death compared to patients without pre-existing AF. This suggests that AF at admission exerts a negative effect on COVID-19 patients’ outcome. The presence of AF in COVID-19 patients may precipitate and be perpetuated by hypoxia, with subsequent hemodynamic compromise and worse outcome, with the most prominent effect on the first 30 days.
Malignant ARs are strictly related to COVID-19 severity, particularly in critical patients with increased levels of cardiac biomarkers [30]. Older COVID-19 patients with tachyarrhythmias had a poorer prognosis compared to those without ARs [31]. Tachyarrhythmias, particularly sustained ventricular tachycardia, are more frequently revealed in COVID-19 patients presenting with acute coronary syndrome (ACS) [32]. TachyARs such as VT/VF are generally revealed in case of severe metabolic stress, while bradyARs could be a primary event contributing to mortality [33], but as reported in the results section, we encountered only few cases of this kind of ARs.
Cardiac biomarkers such as cTnI and NT-pro BNP have been investigated as potential prognostic tools in COVID-19 patients [34]. Patients with increased levels of cTnI reported a higher incidence of ARs, and recent evidence has suggested that the hyperinflammatory response induced by the SARS-CoV2 may precipitate ARs [8,35], and we reported higher levels of cTnI and BNP in ARs-patients.
Limitations
Our results must be read considering some limitations. First, this is a retrospective single-centre cohort study, which limited the statistical power of our analyses. Moreover, given the logistical limitations at the onset of the pandemic infection, some laboratory data and ECG at admission were not collected in all patients. Echocardiography was not routinely performed in these patients. This study was designed considering COVID-19 patients at admission; thus, data regarding drugs’ administration or modality of data are lacking.
5. Conclusions
ARs are quite common at admission in COVID-19 infection, and have been associated with worse prognosis. In particular, AF at baseline ECG determined a significantly higher risk of mortality compared to other rhythms and even to the history of AF. Thus, baseline ARs should represent a simple clinical tool to stratify risk in COVID-19 patients and identify those subjects that may benefit from a closer follow-up and more aggressive therapies.
Author Contributions
A.D. Conceptualization, methodology, validation, formal analysis, data curation, writing—original draft preparation, writing—review and editing, visualization, supervision. M.S., M.M., F.F., A.T., M.D. and F.S. investigation, data curation, writing—review and editing; G.S.P. and G.B. conceptualization, writing—review and editing; L.S. and G.M. validation, writing—review and editing, visualization, supervision. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the local Ethics Committee (AVEN) of Modena University Hospital (approval code 0017624/20).
Informed Consent Statement
Not applicable.
Data Availability Statement
Data files are available upon request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Dzieciatkowski, T.; Szarpak, L.; Filipiak, K.J.; Jaguszewski, M.; Ladny, J.R.; Smereka, J. COVID-19 challenge for modern medicine. Cardiol. J. 2020, 27, 175–183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- SARS-CoV2 Epidemiology. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---1-march-2022 (accessed on 25 December 2021).
- De Filippo, O.; D’Ascenzo, F.; Angelini, F.; Bocchino, P.P.; Conrotto, F.; Saglietto, A.; Secco, G.G.; Campo, G.; Gallone, G.; Verardi, R.; et al. Reduced Rate of Hospital Admissions for ACS during COVID-19 Outbreak in Northern Italy. N. Engl. J. Med. 2020, 383, 88–89. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Pellicori, P.; Doolub, G.; Wong, C.M.; Lee, K.S.; Mangion, K.; Ahmad, M.; Berry, C.; Squire, I.; Lambiase, P.D.; Lyon, A.; et al. COVID-19 and its cardiovascular effects: A systematic review of prevalence studies. Cochrane Database Syst. Rev. 2021, 3, CD013879. [Google Scholar] [PubMed]
- Bhatla, A.; Mayer, M.M.; Adusumalli, S.; Hyman, M.C.; Oh, E.; Tierney, A.; Moss, J.; Chahal, A.A.; Anesi, G.; Denduluri, S.; et al. COVID-19 and cardiac arrhythmias. Heart Rhythm 2020, 17, 1439–1444. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.; Qin, M.; Shen, B.; Cai, Y.; Liu, T.; Yang, F.; Gong, W.; Liu, X.; Liang, J.; Zhao, Q.; et al. Association of Cardiac Injury with Mortality in Hospitalized Patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020, 5, 802–810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chorin, E.; Dai, M.; Shulman, E.; Wadhwani, L.; Bar-Cohen, R.; Barbhaiya, C.; Aizer, A.; Holmes, D.; Bernstein, S.; Spinelli, M.; et al. The QT interval in patients with COVID-19 treated with hydroxychloroquine and azithromycin. Nat. Med. 2020, 26, 808–809. [Google Scholar] [CrossRef]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular Implications of Fatal Outcomes of Patients with Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 811–818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shao, F.; Xu, S.; Ma, X.; Xu, Z.; Lyu, J.; Ng, M.; Cui, H.; Yu, C.; Zhang, Q.; Sun, P.; et al. In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan, China. Resuscitation 2020, 151, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Inciardi, R.M.; Adamo, M.; Lupi, L.; Cani, D.S.; Di Pasquale, M.; Tomasoni, D.; Italia, L.; Zaccone, G.; Tedino, C.; Fabbricatore, D.; et al. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur. Heart J. 2020, 41, 1821–1829. [Google Scholar] [CrossRef] [PubMed]
- Szarpak, L.; Filipiak, K.J.; Skwarek, A.; Pruc, M.; Rahnama, M.; Denegri, A.; Jachowicz, M.; Dawidowska, M.; Gasecka, A.; Jaguszewski, M.J.; et al. Outcomes and mortality associated with atrial arrhythmias among patients hospitalized with COVID-19: A systematic review and meta-analysis. Cardiol. J. 2021, 29, 33–43. [Google Scholar] [CrossRef]
- Kochav, S.M.; Coromilas, E.; Nalbandian, A.; Ranard, L.S.; Gupta, A.; Chung, M.K.; Gopinathannair, R.; Biviano, A.B.; Garan, H.; Wan, E.Y. Cardiac Arrhythmias in COVID-19 Infection. Circ. Arrhythm. Electrophysiol. 2020, 13, e008719. [Google Scholar] [CrossRef] [PubMed]
- Karamchandani, K.; Quintili, A.; Landis, T.; Bose, S. Cardiac Arrhythmias in Critically Ill Patients with COVID-19: A Brief Review. J. Cardiothorac. Vasc. Anesth. 2021, 35, 3789–3796. [Google Scholar] [CrossRef]
- Driggin, E.; Madhavan, M.V.; Bikdeli, B.; Chuich, T.; Laracy, J.; Biondi-Zoccai, G.; Brown, T.S.; Der Nigoghossian, C.; Zidar, D.A.; Haythe, J.; et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J. Am. Coll. Cardiol. 2020, 75, 2352–2371. [Google Scholar] [CrossRef]
- Goyal, P.; Choi, J.J.; Pinheiro, L.C.; Schenck, E.J.; Chen, R.; Jabri, A.; Satlin, M.J.; Campion, T.R., Jr.; Nahid, M.; Ringel, J.B.; et al. Clinical characteristics of COVID-19 in New York City. N. Engl. J. Med. 2020, 382, 2372–2374. [Google Scholar] [CrossRef]
- Tasdemir, G.; Kelebek Girgin, N.; Aydin Kaderli, A.; Cizmeci, E.; Iscimen, R.; Kahveci, F.; Aydinlar, A. Arrhythmia incidence and risk factors in critically ill patients. Crit. Care 2015, 19, P156. [Google Scholar] [CrossRef] [Green Version]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [PubMed]
- Giudicessi, J.R.; Roden, D.M.; Wilde, A.A.M.; Ackerman, M.J. Classification and reporting of potentially proarrhythmic common genetic variation in long QT syndrome genetic testing. Circulation 2018, 137, 619–630. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Wang, T.J.; Parise, H.; Levy, D.; D’Agostino, R.B., Sr.; Wolf, P.A.; Vasan, R.S.; Benjamin, E.J. Obesity and the risk of new-onset atrial fibrillation. JAMA 2004, 292, 2471–2477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaghee, F.; Nafakhi, H.; Alareedh, M.; Nafakhi, A.; Al-Buthabhak, K. ECG markers of malignant arrhythmias and in-hospital outcome of COVID-19 pneumonia. J. Arrhythm. 2021, 37, 426–431. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, J.Y.C.; Kan, J.Y.L.; Mattar, S.A.M.; Qin, Y. The clinical implications of sinus tachycardia in mild COVID-19 infection: A retrospective cohort study. SAGE Open Med. 2021, 9, 20503121211054973. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.H.; Namazi, A.; Shelton, R.; Ramireddy, A.; Ehdaie, A.; Shehata, M.; Wang, X.; Marbán, E.; Chugh, S.S.; Cingolani, E. Cardiac arrhythmias in hospitalized patients with COVID-19: A prospective observational study in the western United States. PLoS ONE 2020, 15, e0244533. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Yu, Z.; Yuan, Y.; Han, J.; Wang, Z.; Chen, H.; Wang, S.; Wang, Z.; Hu, H.; Zhou, L.; et al. Alteration of Autonomic Nervous System Is Associated with Severity and Outcomes in Patients with COVID-19. Front. Physiol. 2021, 12, 630038. [Google Scholar] [CrossRef] [PubMed]
- Mol, M.B.A.; Strous, M.T.A.; van Osch, F.H.M.; Vogelaar, F.J.; Barten, D.G.; Farchi, M.; Foudraine, N.A.; Gidron, Y. Heart-rate-variability (HRV), predicts outcomes in COVID-19. PLoS ONE 2021, 16, e0258841. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Liang, X.; Xu, J.; Hou, H.; Wang, Y. Meta-analysis of atrial fibrillation in patients with COVID-19. Am. J. Cardiol. 2021, 144, 152–156. [Google Scholar] [CrossRef]
- Uribarri, A.; Núñez-Gil, I.J.; Aparisi, Á.; Arroyo-Espliguero, R.; Maroun Eid, C.; Romero, R.; Becerra-Muñoz, V.M.; Feltes, G.; Molina, M.; García-Aguado, M.; et al. Atrial fibrillation in patients with COVID-19. Usefulness of the CHA2DS2-VASc score: An analysis of the international HOPE COVID-19 registry. Rev. Esp. Cardiol. Engl. Ed. 2021, 74, 608–615. [Google Scholar] [CrossRef] [PubMed]
- Sanchis-Gomar, F.; Perez-Quilis, C.; Lavie, C.J. Should atrial fibrillation be considered a cardiovascular risk factor for a worse prognosis in COVID-19 patients? Eur. Heart J. 2020, 41, 3092–3093. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.; Chen, S.; Fu, Y.; Gao, Z.; Long, H.; Ren, H.W.; Zuo, Y.; Wang, J.; Li, H.; Xu, Q.B.; et al. Risk factors associated with clinical outcomes in 323 COVID-19 patients in Wuhan, China. Clin. Infect. Dis. 2020, 71, 2089–2098. [Google Scholar] [CrossRef] [PubMed]
- Gao, P.; Wu, W.; Tian, R.; Yan, X.; Qian, H.; Guo, F.; Li, T.; Liu, Z.; Wang, J.; Zhou, X.; et al. Association between tachyarrhythmia and mortality in a cohort of critically ill patients with coronavirus disease 2019 (COVID-19). Ann. Transl. Med. 2021, 9, 883. [Google Scholar] [CrossRef] [PubMed]
- D’Ascenzo, F.; De Filippo, O.; Borin, A.; Barbieri, L.; Adamo, M.; Morici, N.; Truffa Giachet, A.; Iannaccone, M.; Crimi, G.; Gaido, L.; et al. Impact of COVID-19 pandemic and infection on in hospital survival for patients presenting with acute coronary syndromes: A multicenter registry. Int. J. Cardiol. 2021, 332, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Turagam, M.K.; Musikantow, D.; Goldman, M.E.; Bassily-Marcus, A.; Chu, E.; Shivamurthy, P.; Lampert, J.; Kawamura, I.; Bokhari, M.; Whang, W.; et al. Malignant Arrhythmias in Patients with COVID-19: Incidence, Mechanisms, and Outcomes. Circ. Arrhythm. Electrophysiol. 2020, 13, e008920. [Google Scholar] [CrossRef] [PubMed]
- Weng, H.; Yang, F.; Zhang, L.; Jin, H.; Liu, S.; Fan, F.; Liu, Z.; Zheng, X.; Yang, H.; Li, Y.; et al. Joint Predictive Value of cTnI and NT-proBNP on Mortality in Patients with Coronavirus Disease 2019: A Retrospective Research in Wuhan, China. J. Transl. Int. Med. 2021, 9, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Lazzerini, P.E.; Boutjdir, M.; Capecchi, P.L. COVID-19, arrhythmic risk, and inflammation: Mind the gap! Circulation 2020, 142, 7–9. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).