Abstract
COVID-19 caused significant morbidity and mortality amongst ethnic minority groups, but vaccine uptake remained lower than non-minoritised groups. Interventions to increase vaccine uptake among ethnic minority communities are crucial. This systematic review synthesises and evaluates behaviour change techniques (BCTs) in interventions to increase vaccination uptake in ethnic minority populations. We searched five databases and grey literature sources. From 7637 records identified, 23 studies were included in the review. Interventions were categorised using the Behaviour Change Wheel (BCW) and Behaviour Change Taxonomy v1. Vaccines included influenza, pertussis, tetanus, diphtheria, meningitis and hepatitis. Interventions were primarily delivered in health centres/clinics and community settings. Six BCW intervention functions and policy categories and 26 BCTs were identified. The main intervention functions used were education, persuasion and enablement. Overall, effective interventions had multi-components and were tailored to specific populations. No strong evidence was observed to recommend specific interventions, but raising awareness and involvement of community organisations was associated with positive effects. Several strategies are used to increase vaccine uptake among ethnic minority communities; however, these do not address all issues related to low vaccine acceptance. There is a strong need for an increased understanding of addressing vaccine hesitancy among ethnic minority groups.
1. Introduction
People from ethnic minorities were disproportionately affected by COVID-19, with an increased risk of severe infection and worse clinical outcomes than White individuals, including disproportionately higher cases and deaths []. However, certain ethnicities and minority populations in the western context have been more reluctant than others to receive the COVID-19 vaccine [,,,]. In the United Kingdom, people from Black, Pakistani and Bangladeshi communities had lower vaccine uptake despite being among the high-risk groups [,,]. In 2021, it was reported that in Great Britain, Black or Black British adults had the highest rates of COVID-19 vaccine hesitancy (18%), followed by those from a South Asian background (17%), compared with White adults (4%) [,]. Similar variability in COVID-19 vaccine acceptance rates has been reported in different countries, with low acceptance rates being more pronounced in the Middle East, Eastern Europe and Russia, and higher acceptance rates in East and South East Asia []. Low vaccine uptake amongst some ethnic minority groups existed before the COVID-19 pandemic and has been associated with lower levels of vaccine confidence, uptake of routine vaccines and trust in vaccine services, all of which have been reflected in the COVID-19 vaccine uptake rates [,,].
Vaccine hesitancy, the delay in acceptance or refusal of vaccination despite the availability of vaccination services, poses a threat to controlling COVID-19 and other vaccine-preventable diseases; hence, the World Health Organization (WHO) considers it one of the top 10 global health threats []. Changing behaviour is complex, and therefore, a systematic approach is required to understand factors influencing vaccine uptake, such as knowledge, beliefs, attitudes and behaviours of the targeted population group []. It is important to address systemic (access to health services and information, the structure and strength of the local healthcare system and service funding), individual (perceived efficacy of vaccines, risk perception, health literacy) and social barriers (social support and networks) to vaccine uptake [,]. Vaccine hesitancy can be reduced, and uptake increased when interventions target emotional, cognitive and social determinants that can either hinder or facilitate this behaviour through culturally appropriate information and messaging, policy and vaccine delivery [,]. Successful immunisation programmes generally result in high vaccine effectiveness and adequate uptake of vaccines.
A key priority in addressing barriers to vaccine uptake is identifying ways to engage with and deliver vaccinations to ethnic minorities and other vulnerable population groups. More targeted vaccination interventions are essential, as this can help understand and address concerns and barriers to uptake among specific groups, and this is beneficial for achieving national vaccination targets []. Identifying the barriers and facilitators to vaccine uptake and existing intervention behavioural strategies that have been effective among ethnic minorities could help address vaccine hesitancy in these groups [,].
Evidence of interventions to increase vaccination uptake exists, but evidence of vaccination interventions by ethnicity and race and the effectiveness of the interventions in increasing vaccine uptake is limited []. Studies that have explored vaccine access and uptake among ethnic minority groups often do not highlight behavioural components within interventions that influence uptake [,,,]. This limits our understanding of the mechanism of change resulting from interventions and the identification of how intervention content can be modified to increase vaccine uptake by drawing on specific behaviour change techniques designed to address barriers and facilitators of vaccine uptake among ethnic minority groups [].
Interventions based on principles drawn from evidence and theories of behaviour and behaviour change have shown to be more effective []. Intervention development guidelines recommend using evidence-based behaviour change strategies [], which requires understanding the behavioural elements of particular interventions that would improve vaccine uptake. Consideration is needed for the targeted population in relation to factors underlying vaccination uptake behaviour []. Behavioural determinants vary for different ethnic and racial minority groups, so it is important to identify and target these influences []. In 2000, the Medical Research Council (MRC) published a framework to help researchers to develop and evaluate complex interventions []. These guidelines outlined the importance of developing a theoretical understanding of causal mechanisms of action within interventions by drawing on existing evidence and theory []. In addition, the Behaviour Change Wheel (BCW) and Behaviour Change Technique Taxonomy v1 (BCTTv1) are comprehensive tools for identifying and describing specific behavioural components useful for intervention content [,]. The BCW is a synthesis of 19 frameworks of behaviour change that can be used to characterise intervention components that contribute to behaviour change; within the BCW is the inner hub (capability, opportunity, and motivation, i.e., COM-B model), which outlines sources of behaviour that could be the target for interventions []. (Figure 1) While the BCTTv1 is a 93-item taxonomy of behaviour change techniques (BCTs) [], (Supplementary Table S1) the two frameworks are complementary and have been used to identify behavioural components in public health interventions, clinical trials and previous systematic reviews [,,,,].
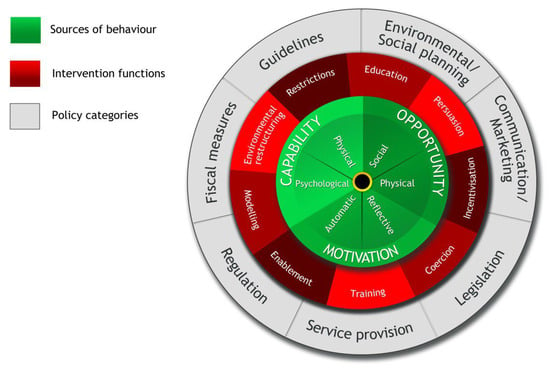
Figure 1.
The Behaviour Change Wheel [].
As some racial and ethnic minority communities have lower vaccine uptake, which was evident during the COVID-19 pandemic, it is essential to identify interventions and strategies that can improve vaccine uptake and reduce hesitancy among diverse populations and how this could inform the development or modification of interventions to support COVID-19 vaccination programmes in ethnic minority communities. Many different types of vaccinations are available, but in the current study, only vaccines that work against similar infections to COVID-19 (excluding COVID-19 vaccines) were reviewed to extrapolate learning from previous interventions to inform future COVID-19 and similar vaccine programme interventions.
Review Questions
This systematic review sought to answer the following questions:
1. What intervention strategies, targeted at people from racial and ethnic minority backgrounds, can increase vaccination uptake?
2. What BCTs are included in interventions designed to increase vaccine uptake in racial and ethnic minority populations?
2. Methodology
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines []. The protocol was pre-registered on the International Prospective Register of Systematic Reviews (PROSPERO ID: CRD42021239010) [].
2.1. Search Strategy and Selection Criteria
Initial scoping review searches of three databases (PubMed, CINAHL and PsycInfo) and registered PROSPERO protocols indicated there were no published reviews or protocols in this area. As a result, a full systematic review of the literature was undertaken with searches for published and unpublished studies.
The search strategy was applied to the following databases: MEDLINE, EMBASE, CINAHL, EBSCOhost, and PsycInfo, hand searching was conducted over the last six years in two key journals (Vaccine and Vaccines). These databases and journals were selected based on their coverage of public health and vaccination topics. For the grey literature, a search was conducted through the first 10 pages of Google Scholar and pre-print databases (SocArXiv, MedRXiv, PsyRXiv, and SSRN). The search terms were based on a combination of keywords for three key concepts: “vaccine hesitancy” AND “minority ethnic groups” AND “intervention”. Within each concept, keywords were combined with Boolean search operators. Table 1 shows the keywords included in the search strategy for each concept. The asterisk * symbol was used as a truncation at the end of root words to broaden the search terms so it captures and includes various word endings and spellings.

Table 1.
Search terms used to identify relevant publications for the review.
Searches of databases had no date restriction and included papers from inception to 24 March 2021, and the search was updated 27 June 2022. Searches of pre-print databases were conducted and included papers up to 21 July 2022, after the last searches were conducted. Studies not captured by the database search engines were identified through bibliometric cross-referencing. We included studies reporting interventions for respiratory and routinely recommended vaccine-preventable diseases among ethnic minority groups globally. Vaccine-preventable vector-borne, sexually transmitted infectious diseases and non-routinely recommended vaccines were excluded in the search terms (i.e., NOT “HPV or malaria or typhoid or cholera”) (see Supplementary Figure S2), as these vaccines include different considerations to many routinely recommended vaccines. Studies on COVID-19 vaccines were excluded because the original research scope and search were developed before the widespread availability of the COVID-19 vaccine. In addition, the intervention strategies used for COVID-19 vaccines were rapid, and at the time of conducting these searches, the vaccines were still being developed and tested. If a study included groups of diseases in the included and excluded categories, e.g., influenza and COVID-19, only information related to respiratory non-COVID-19 and routinely recommended vaccines were extracted.
2.2. Eligibility Criteria
Using PICOS (Population, Intervention, Comparator, Outcome, Study Design), the following inclusion criteria were used:
- Population: studies that included patients and the general public from racial and ethnic minority groups and excluded studies with a majority white ethnic population (i.e., studies with ≥50% white ethnic sample size). Ethnic minority groups were defined as groups that are not part of the majority ethnicity in the country of the study;
- Interventions: reported interventions, which included specific strategies designed to improve vaccination services and uptake in racial and ethnic minority groups, focusing on respiratory and routinely recommended vaccine-preventable diseases. Studies were excluded that did not provide details of the interventions;
- Comparator: included any reported comparator such as pre-intervention data, alternative intervention, or control group;
- Outcomes: studies were included if they reported vaccine behaviour-related data (intention, behaviour and uptake) after implementation of the intervention;
- Study Design: all study designs, including quantitative and qualitative, were included, except case studies and case series.
Only peer-reviewed articles in the English language were included. Papers were excluded if there was no empirical data, if they reported only conference proceedings, or were not in English.
3. Screening
Each reference was uploaded to the Rayyan review manager, an app with semi-automation that helped with the initial screening of abstracts and titles based on the eligibility criteria []. After the automatic removal of some duplicates, the remaining studies were manually screened. Two investigators (WE and AC) independently conducted initial screening to determine if the eligibility criteria were met. Discrepancies were resolved by discussion between WE, AC and AK. Studies that met the inclusion criteria underwent full-text screening, and the reference lists of all papers included in the synthesis were reviewed for additional articles.
3.1. Data Extraction
3.1.1. Intervention Study Details
Data were extracted by WE and AC separately, and 10% of the sample from each individual’s extraction was checked for completeness and quality purposes by another reviewer (AK). For each study, the following data were extracted if available: vaccine focus, study information (including country of study and design); participant characteristics (such as sample size, ethnicity and age); intervention details (such as intervention components and outcomes) and vaccine coverage or uptake, hesitancy, barriers and facilitators.
3.1.2. BCT and BCW Intervention Details
Two reviewers (WE and EG) read the intervention descriptions to identify the BCW components, intervention functions and policy categories reflected within each intervention. The BCTTv1 was used to identify components of the 93 BCTs used in each intervention, which were then categorised into 16 groups. Intervention components were also mapped onto the BCW, nine intervention functions, and seven policy categories. This information (BCW and BCT details) was entered onto a standardised data extraction form. All included studies were coded for the BCTs and BCW by one author (WE) and checked by a second author (EG), and discrepancies were resolved by a third author (AK) to reach a consensus.
3.2. Risk of Bias
Risk of bias was measured using the AXIS critical appraisal tool for cross-sectional studies and Critical Appraisals Skills Programme (CASP) guidelines for other study designs [,]. The AXIS critical appraisal tool included 20 questions to address study design, reporting quality, and the risk of bias in cross-sectional studies. CASP guidelines for cohort studies, randomised controlled trials, and qualitative research included questions to assess appropriateness of study design, methodology, and results. Each reviewer (WE and AC) assessed 50% of included studies; 10% of these were reviewed by a second reviewer, with discrepancies resolved by a third reviewer (AK). Studies were rated low, moderate, or high. For each study design, the proportion of positive assessments was used to determine the quality of each study. For example, fewer than 11 positive scores using the AXIS critical appraisal tool was considered low quality, 11–16 = moderate, and a score of 17 or higher was high quality (See Supplementary Table S3).
3.3. Synthesis Method
Findings from the included studies were entered into tables and descriptively synthesised. The analysis explored the variation in the vaccines reported, study design information, and the intervention details and outcomes. Effect sizes of the outcomes were not accessed due to wide variation in the details reported; this included differences in the measure of effects being used, lack of analysis, heterogeneity of the population samples and insufficient data reporting the same outcome across the studies. Due to the vast differences in the types of interventions, components, measurements, and reported outcomes, a meta-analysis could not be conducted.
In addition, the factors that influenced the intervention implementation and outcomes, such as information on hesitancy, barriers and facilitators to uptake, and challenges experienced while implementing the intervention, were extracted and analysed. Finally, the recommendations suggested by the study authors on approaches to improve similar interventions and other areas that need further exploration were summarised and grouped according to the related BCTs.
4. Results
4.1. Search Results
A total of 7637 citations were identified from searching peer-reviewed databases; 7569 from specific database searches and 68 from hand searching. (Figure 2) Of these, 3180 duplicates were removed, leaving 4457 citations to be screened, of which 271 full texts were reviewed. A total of 35 articles reported vaccination interventions targeting ethnic minority groups, of which 12 studies were on interventions targeted at healthcare workers (HCWs) who support ethnic minority communities. These 12 studies were excluded and analysed as a separate review topic focusing on interventions designed to support HCWs. Another eight studies were later removed due to insufficient information and evidence related to the interventions implemented. Finally, 23 articles reported interventions targeting ethnic minority groups and were included in this review, from which two studies reported the same data [,].
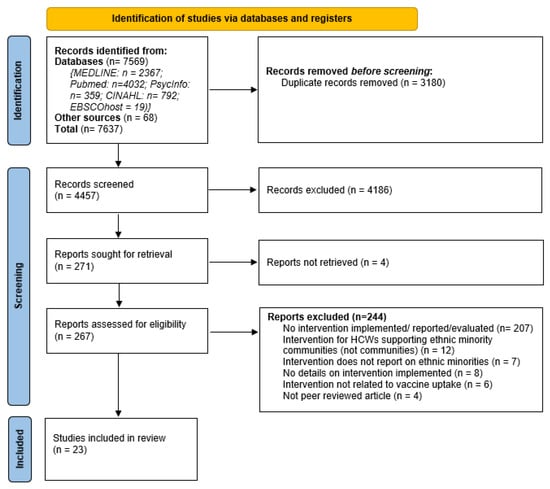
Figure 2.
PRISMA flow chart [].
4.2. Study Characteristics
Table 2 summarises the intervention characteristics and results across the 23 included studies. The selected studies included 166,528 participants from five countries: the United States (n =18 studies), the United Kingdom (n = 2), and one study from Canada, Greece, and Israel. Ethnic minorities represented were Black/African Americans (n = 18), Asians (n = 9), Hispanic/Latinos (n = 8), two studies on Native American/American Indians and Pacific Islanders, and one study on Jewish and Roma populations (n = 1). Study designs used in the included studies were RCT/Quasi-experiments (n = 11), cohort (n = 6), and cross-sectional (n = 6). The vaccines targeted included a wide range of illnesses, including influenza [,,,,,,,,,,,], pneumococcal [,], hepatitis [,,,,,,], polio [,,,], pertussis [,,,,,], diphtheria and tetanus [,,,,], and measles-mumps-rubella []. The interventions were conducted in two broad settings: health centres/clinics (n = 15) and a community setting (n = 8). The interventions were conducted between 2001 and 2021, ranging from two months to five years (min = 5 months, max = 60 months, average = 14.6 months).

Table 2.
Description of vaccine interventions implemented in increased vaccine uptake among EM communities.
4.3. Risk of Bias
The studies were of moderate to high quality and had a moderate risk of bias (high = 10; moderate = 13). (Table 2) The potential risk of bias was primarily related to the intervention component details, reporting (e.g., response rates, follow-up, identification of other influencing factors), and statistical methods (including adjustment of confounding factors).
4.4. Intervention Effects and Outcomes
As shown in Table 2, outcomes of interest mainly focused on vaccine uptake and coverage amongst ethnic minority patients/participants (n = 19 studies). All interventions targeted ethnic minority populations’ behaviour and were designed to access vaccine knowledge and perception [,,,,], intention to vaccinate after the intervention [,,,], adoption of healthy behaviours [], and cost-effectiveness []. Overall, the effects of the different intervention functions and associated BCTs varied. All the studies reported positive changes from the implemented interventions, except the study by Frew et al., 2016 where neither intervention implemented significantly increased influenza immunisation [].
The study by DiTosto et al., which evaluated whether guidelines were associated with improved Tdap vaccine uptake during pregnancy, reported improvement in vaccine uptake, as women were approximately five times more like to receive Tdap vaccines during the recommended window compared to the pre-guideline cohort (95% CI 3.54–5.72) []. A similar intervention aimed to assess women’s intentions to receive influenza and Tdap vaccines during pregnancy and their beliefs about the vaccines and the diseases they prevent after reading evidence-based information about the vaccines. Women were more likely to get the vaccine after reading information: Flu (26.0%), Tdap (49.9%; 43.0% of those in the third trimester) []. These findings reflected the positive impact of education, increasing awareness about vaccination, and the personal persuasion felt after receiving and understanding vaccine-related information. Frew et al. described pregnant women’s likelihood of vaccinating their infants against seasonal influenza based on how messages were framed and observed that although a gain-framed message (OR = 2.13, 90% CI = 1.12–4.05) and loss-framed messages (OR = 2.02, 90% CI = 1.08–3.79) were significantly associated with infant influenza vaccination intention compared to control, intention to immunize infants was significantly higher among gain-framed compared to control messages (OR = 2.20, 90% CI = 1.13–4.30), while the loss-framing was not significantly associated with intention to vaccinate infants, compared to gain-framed and control messages []. This shows that considering the benefits from vaccination had more influence on increased uptake than what might be lost. In the study to assess the effectiveness of providing personal support to awareness, Wood et al. showed how empowering communities with their personal vaccine information and including follow-up services optimised the immunisation completion rates []. In the study, groups with both case management and a health passport had a higher completion rate than those who were only given a health passport (63.8% vs. 50.6%, p = 0.01) [].
4.5. Intervention Behaviour Change Components
Behaviour change intervention components targeted Psychological Capability (n = 20 studies), Reflective Motivation (n = 18), Social Opportunity (n = 8), Physical Opportunity (n = 7), Physical Capability (n=2), and Automatic Motivation (n = 1). (Table 3). Only six of the nine intervention functions were used in the studies; these were Education (n = 21), Persuasion (n = 17), Enablement (n = 9), Environmental Restructuring (n = 8), Incentivisation (n = 2), and Modelling (n = 1). The three intervention functions not identified were Coercion, Training, and Restriction. Five of the six policy categories were also identified; these were Guidelines (n = 19), Communication/Marketing (n = 17), Service Provision (n = 11), Environmental/Social Planning (n = 9), Regulation (n = 6), and Fiscal (n = 2). Legislation was the only policy category not identified in any study.

Table 3.
Summary of the BCW components identified in the vaccination interventions.
Twenty-six BCTs were identified across all of the studies, and this represented 12 of the 16 BCTTv1 groups (Table 4). The most commonly used BCTs were Information about health consequences (n = 14 studies); “Information about antecedents” and “Credible source” (n = 12 each); Prompts/cues (n = 9); “Instruction on how to perform the behaviour”, “Restructuring the physical environment”, and “Framing/reframing” (n = 7 each); “Social support (practical)” and “Adding objects to the environment” (n = 6 each). Twenty studies implemented multiple BCTs ranging from two to nine BCTs [,,], compared to three studies that adopted a single BCT [,,]. On average, across all the studies, approximately five BCTs were used per study. Interventions conducted in community settings (n = 8 studies) primarily used an educational approach including coaching [,,,,,,,], case management [], and media-led information and education outreach campaigns []. The coaching intervention delivered two approaches: peer coaching with nurse case management (PC-NCM) and peer coaching alone, and compared these with usual care (which included minimal PC and nurse involvement) []. The case management intervention also provided health passports to parents, which only contained information on the recommended visits for well-child care and the childhood immunisation schedule []. One study after the education intervention provided onsite vaccination []; and another study provided community vaccination []. Some education interventions used community members to deliver the intervention, which included training peer health educators [,] and using religious leaders to enhance recruitment and uptake in vaccination programs [,]. Three studies reported providing culturally specific information and interpretation in the local languages of the ethnic minority groups [,,].

Table 4.
Summary of BCTs identified in the vaccine interventions.
4.6. Intervention Functions and Policy Categories
The effects of the different identified intervention functions and associated BCTs varied.
4.6.1. Education
Of all the included studies, only two [,] did not have the education intervention element. Types of educational resources included brochures and information sheets, video presentations, workshops, community representatives such as church pastors, and public health campaigns. Most of these were aimed at providing information on vaccination and instruction on how to get it. The messages sometimes included the pros and cons of taking vaccination and possible future outcomes.
Armstrong et al. showed that an educational brochure addressing reasons for vaccination refusal was more likely to improve influenza vaccination than only postcard reminders that showed influenza as a leading cause of sickness, hospitalisation, and death in people over 65 years of age, and vaccination timing (66.4% vs. 56.9%, p = 0.04). However, video interventions appeared more effective in improving vaccine knowledge than printed media, as shown in three studies [,,]. The video tutorial provided by Frew et al., and Kriss et al. also included information on existing current guidelines for vaccination during pregnancy as a form of providing information about antecedents; this was particularly important, as the most common reason for not taking Tdap vaccines among unvaccinated women was the lack of recommendations from their health physician [,].
Interventions expanding to family and close contacts appeared as effective as the individual-targeted strategies common in most studies. For instance, the “Cocooning strategy” to prevent influenza transmission from their close contact with susceptible neonates and young infants in the study by Maltezou et al., provided vaccine services to fathers and other household contacts by first educating them about the safety and efficacy of vaccines and the expected effectiveness for the neonate []. From this, higher vaccine uptake during pregnancy was recorded compared to the general US hospital-based post-partum vaccination program (73.7% vs. 44.7% mothers, 55.8% vs. 25.7% fathers, respectively). Similarly, in the UK, Larcher et al. showed that sharing information about health consequences through counselling women positive for hepatitis B (mostly African, Oriental, and Turkish) on the implications for themselves, their partners, and their families, and the need for immunisation of their babies led to a significant increase in baby vaccinations, and a reduction in hepatology referral services during the study []. However, another public-focused intervention in the UK using a communication campaign as a means of prompt/cue informed pregnant women about the need for antenatal pertussis and influenza vaccination showed that only 3.0% of the study population (n = 6/200) used the public health campaign as the primary source of information, but 16.7% received the vaccine []. A similar public campaign in the United States that used a combination of media strategies, including Vietnamese-language versions, emphasising the need for hepatitis B catch-up vaccinations, showed increased awareness of hepatitis B in all study areas, with the significant increase only in the media education area (+21.5% points) vs. control area (+9.0% points) (p = 0.001) []. These findings evidence direct contact with patients after public strategies, and information in local languages were more likely to increase the effectiveness of a national approach.
Another mass media intervention, a nationwide bOPV campaign in Israel, presented evidence of a large-scale and positive use of prompt/cue []. Exposure to media messages was associated with increased vaccine uptake, mostly with 3–5 days delay in all vaccines except for MMRV, which showed a negative effect with 6–8 days delay that diminished afterwards []. These observations imply that after increased awareness, vaccine uptake was also influenced by time, as the duration between receiving the information and taking action had an impact on the corresponding actions and outcomes. The time effect illustrated intention to receive vaccination did not always translate to receiving it; for instance, in the intervention by Stringer et al., where nurses provided pros and cons of vaccination through additional information via pamphlets on HBV and offered the immediate vaccine in hospitals when the patients accepted to receive it []. Despite the option for immediate vaccine provision, although vaccination acceptance was high (91%), actual vaccination receipt was slightly lower (86%).
4.6.2. Persuasion
The 17 studies that included persuasion intervention functions used a variety of approaches, which included outreach and postcard reminders [,], national guidelines [], communication with healthcare professionals [,,,,], support from trained peer health educators and community representatives [,,,], and visual stimulation through evidence-based videos and reading resources [,,,]. These approaches reflected all five policy categories identified in this review. Based on methods of delivery, education through video was more persuasive than written sources of information [].
At a broad scale, implementation of updated guidelines from the Advisory Committee on Immunization Practices (ACIP), which recommended universal Tdap vaccination among pregnant individuals between 27 to 36 weeks gestational age, regardless of prior vaccine status, increased vaccine uptake for Tdap, influenza, and pneumococcal diseases []. While at a smaller scale, the studies by Frew et al. illustrated how visual gain-framed messages increased intention to vaccinate compared to loss-framed messages [,,]. This persuasive approach was slightly contradicted in the study by Armstrong et al., which showed providing information about the effect of being unvaccinated as well as addressing related concerns on the dangers of vaccination motivated the participants to seek vaccination []. Also, between affective messaging (recommendation to obtain influenza immunisation while acknowledging and discussing patients’ concerns) compared to the cognitive messaging intervention approaches (providing detailed, question-and-answer information on influenza vaccines), no significant increase was observed []. Generally, providing some vaccination message, whether gain or loss-focused, encouraged a willingness to get vaccinated compared to no information at all, as illustrated by Frew et al. [,]. This highlighted that any form of awareness could increase the intention and receipt of vaccination.
Considering a significant predictor of vaccine acceptance included the history of previous vaccinations, as shown in the study by Schwartz et al. (OR = 8.64, 95% CI = 4.17–17.91, p < 0.001), having credible sources like medical assistants and physicians who addressed patients’ concerns and recommended vaccination increased vaccine acceptance (27% agreed to receive influenza vaccination after physicians addressed their concerns) []. Nevertheless, healthcare professionals communicating about vaccination did not always significantly increase vaccine uptake [,]. For instance, in the study by Donaldson et al., while 47.5% of women indicated a willingness to accept pertussis vaccine in their next pregnancy, 24% had engaged in meaningful discussions with a GP for further information (who were considered credible sources), but 26% received vaccines during the current pregnancy []. Observed uptake differed by up to 15.0% between ethnicities, which included Black populations with only 18% uptake []. In the study by Callahan et al., 70.2% of Black women reported they would not get vaccinated during pregnancy, and only 23.1% of Black compared to 46.2% of White women unvaccinated in the first and second trimesters planned on receiving a Tdap vaccination []. However, engaging community representatives showed to have a positive effect on the intervention, as shown by Daniels et al., where in addition to getting information from credible sources through physician reminders and presentations on vaccination benefits and side effects, church pastors supported the recruitment of people, and this successfully encouraged >90% willingness to participate in education about influenza and pneumococcal vaccination []. McPhee et al. also showed that the persuasive approach of using multiple community engagement as practical social support approaches significantly increases the odds of receiving vaccines [community mobilisation (OR: 2.15, 95% CI: 1.16–3.97); media campaign (OR: 3.02, 95% CI: 1.62–5.64)] compared with the control areas for a study on accepting three doses of hepatitis B vaccines []. The intervention also provided rewards to children receiving vaccinations. Higher uptake was noted among children who had previously received at least 1 DTP shot, married parents who knew someone with liver disease, and those who had greater knowledge about hepatitis B. Vaccination was, however, still significantly lower for older children.
4.6.3. Environmental Restructuring
Making environmental changes to improve vaccination mainly included using community-based vaccination centres. When onsite vaccinations were offered in a community church, the intervention group received significantly more influenza (OR = 4.8, 95% CI: 2.5–9.4) and pneumococcal (OR = 3.6, 1.8–7.2) vaccinations []. In contrast, Donaldson et al. reported low vaccine uptake in healthcare settings (pertussis 34.0% and influenza 48%) []. To facilitate attendance immunisations, Larcher et al. added extra components to the existing environment by carrying out weekly vaccine clinics in hospitals at the same time as neonatal follow-up clinics, and also implemented an opportunistic policy for latecomers []. From this, 242 infants (91%) were fully vaccinated, and 217 (82%) had serology; hence, full vaccination in the intervention group was 95%, compared to 78% in the control group who were non-residents of the area and often lost to follow-up. The study also reported high mobility among families (25%), significantly affecting outcomes []. These findings show that national and clinical interventions adapted to the population were more effective.
To efficiently facilitate the community approaches, tailored resources appeared more successful. Findley et al. used a package of bilingual and community-appropriate immunisation-promotion materials, which supported provider immunisation delivery []. The intervention included credible sources, social support, and monitoring elements by using trained peer health educators and personalised immunisation outreach and promotion within social service and educational programs. The intervention resulted in significantly increased immunisation coverage by 11.1% compared to the control, which had none of the intervention services. In addition, 53% of the intervention group were more likely to complete the immunisation series earlier (by 11 days, t = 3.91) compared to the control (AOR = 1.53; 95% CI = 1.33–1.75). The study also stated ethnicity, being Latino, did not significantly influence immunisation coverage (AOR = 1.07; 95% CI = 0.93–1.24). Similarly, the practical social support community mobilisation strategy by McPhee et al. utilised existing health regulation guidelines to establish a Vietnamese-American community-based organisation formed by the coalition that included health workers, local authorities, businesses, and community people and delivered vaccine services []. Outcomes from the intervention showed increased receipt of three hepatitis B vaccinations. These findings suggest that community interventions can be effective for any ethnic group. In addition to this, the location of delivery could also influence participation. The community-based participatory research (CBPR) approach used by Ma et al., which utilised churches to inform people about vaccination and offered church health worker training, in combination with more flexible vaccine open clinic hours with bilingual medical staff in the community, recorded a significant increase in HBV screening in the intervention group but not the control [(intervention, 58.5% to 95.8%), control (38% to 39.8%)], with a group difference of 37.8% vs. 1.8% (p < 0.001), respectively []. Furthermore, there was also an increase in previously non-compliant people’s screening rate in the intervention group (those who never had an HBV test), 93.1%, compared to 2.9% for the control (2 screened/70 never screened) groups. This approach exhibited evidence of the adaptable nature of the environmental/social planning policy category.
4.6.4. Enablement
Strategies used in the nine studies implementing the enablement function included engaging health visitors to meet with families, offering free vaccines, and providing a platform for patients to share their views [,,,,,,,,]. Larcher et al. used hospital-based liaison health visitors as a means of monitoring from credible sources to contact families that did not receive vaccinations and notified their general practitioner, these health visitors attempted to contact the family themselves to reinforce the need for attendance []. The community vaccination clinics in the study by Peterson et al. adopted the National Vaccine Advisory Committee standards for immunisation programs in non-traditional settings and used the fiscal measure of obtaining free vaccines through an entitlement program for uninsured children and adults, thereby removing the cost implication from the patients []. By using this approach, which provided vaccination instruction and material incentive, through credible sources restructuring physical environments, >80,000 free influenza vaccinations were administered to vulnerable populations over 12 years [].
The empowerment of patients also served as a means to enable them to make positive vaccination decisions. For example, health passports containing information on the recommended visits for well-child care and approved childhood immunisation schedule were given to all participants in the study by Wood et al. []. In addition to the case management assessment of client health, other needs with set goals were included in the intervention package. This approach was used as a means of solving barriers to the receipt of well-child care, such as lapses in insurance or problems with transportation. The results showed immunisation completion in the case management group was 13.2% higher than the control group (63.8% vs. 50.6%, p = 0.01), but the high vaccination rate in both groups indicated the benefit of the passport to both groups. Also, Zibrik et al., who conducted 68 socially supportive culturally tailored HBV education workshops over a 12-month period for participants, showed >50% of participants engaged in HBV prevention or management actions, positive behaviour changes to health (62%), and 55% took specific action related to HBV prevention or management []. This showed that providing instructions in a community setting on how to take action, in addition to enabling information, had positive effects.
4.6.5. Incentivisation
Only two studies included incentive function in their intervention [,]. Ma et al. included the option for community members to train and become health workers, and the study reported increased HBV screening in the intervention group, but not the control [(intervention, 58.5% to 95.8%), control (38% to 39.8%)], with a group difference of 37.8% vs. 1.8% (p < 0.001), respectively []. As a form of fiscal measure and material incentive, the study negotiated with health providers to lower the cost of HBV tests and treatments for uninsured individuals with HBV infection towards overcoming financial constraints. In the study by Peterson et al., free influenza vaccinations were offered in non-traditional settings for uninsured and underinsured immigrant and ethnic minority groups []. Using this approach, 5910 vaccines were administered through 99 community-based vaccination clinics in one influenza season, and of this, 43.1% were uninsured, and 6.9% were vaccinated for the first time. When probed for the reasons for choosing the study clinics, the common reasons given were because it was in a convenient location (19.9%) free vaccination (13.5%), and it provided vaccines for those who lacked health insurance to pay for vaccination (12.8%). This emphasises the relationship between enablement, convenience, and fiscal measures in vaccination interventions.
4.6.6. Modelling
The single study that included a modelling function was by Nyamathi et al., who implemented a three-level peer coaching and nurse-delivered intervention for homeless men recently released on parole from prison and jails []. The intervention comprised a series of interactive exercises and role-playing that provided information about vaccination and health consequences, and provided opportunities to practice and rehearse possible scenarios related to vaccination. Each intervention had a research nurse or peer coach who reviewed the vaccine dosing and tracked progress, which was a means of monitoring behaviour without needing direct feedback; however, the nurse involvement varied across the different intervention packages. Peer coaches were former parolees who successfully completed a similar program, and as paraprofessionals, they were positive role models with whom the parolees could identify, therefore, providing social support. All three approaches recorded high rates of HAV and HBV vaccine series completion, 75.4% (PC-NCM), 71.8% (PC), and 71.9% (UC), and the difference in uptake was not statistically significant (p = 0.78). This showed that regardless of how involved nurses were, interactive sessions with peer coaches who served as role models helped increase vaccine uptake and completion.
4.7. Predictors, Barriers and Facilitators That Influence Vaccination Uptake
Several studies reported factors and predictors contributing to vaccination hesitancy (Table 5). The main predictors of vaccine uptake were history of sickness from past vaccination; knowing someone who became sick; fear of side effects; perceptions around importance and efficacy, such as the inability of vaccines to prevent flu; fear of needles; not wanting it; flu not considered a serious disease; and individuals not wanting to get the flu. In the study by Stringer et al., there were no differences between the acceptors and non-acceptors with respect to their behavioural and attitudinal HBV beliefs []. Nyamathi et al. also highlighted a few personal attributes that influenced vaccine uptake, and this included ethnicity (Black and Latinos in the United States), experiencing high levels of hostility, social support, history of injection drug use, ex-prisoners, and people admitted for psychiatric illness []. McPhee et al. listed other attributes that decreased vaccination uptake, which included factors such as having older children, higher number of years since the parent immigrated, and household income above the poverty line [].

Table 5.
Factors influencing vaccination uptake and intervention implementations.
4.7.1. Barriers to Vaccine Uptake That Affect Ethnic Minority Communities
The most significant barrier to vaccination was limited knowledge and awareness of vaccination transmission, susceptibility, prevention ability, and the opportunity presented to avoid treatment [,,,,]. Other identified barriers included poor accessibility to transportation and inconvenient vaccine appointments, low trust in the healthcare system, lack of culturally relevant and easy-to-understand information, and immigration-related barriers, such as fear of lack of legal status [,,,]. Also, lack of professional encouragement and uncertainties about the risk and benefits of vaccines acted as barriers to the uptake [,].
Behavioural patterns that negatively influence vaccine uptake were based on a perception that a holistic lifestyle, such as a healthy personal lifestyle and breastfeeding, was sufficient for providing needed immunity, so there was a lower risk of contracting the disease [], and having a previous history of not taking vaccines generally [,]. High mobility of families related to address changes significantly affected the effectiveness of hospital-based immunisation programmes [,].
4.7.2. Facilitators of Vaccine Uptake in Ethnic Minority Communities
The most significant facilitators identified were awareness of vaccination importance and schedule [,] and encouragement or recommendation from healthcare professionals, which was more effective because the HCWs were people they had an existing relationship with [,]. Other facilitators included individuals, especially mothers, wanting to take action in the best interests of babies and families by protecting themselves and reducing the risk of a baby developing a disease, knowing someone who had experienced the disease before, having a past personal experience of vaccine-preventable illness, accepting previous vaccines and believing vaccines are effective [,,,]. The protection of families was a particular motivation for large households [].
The perception of how serious a vaccine-preventable illness is, and an awareness of how susceptible people are to getting infected, for instance, influenza during pregnancy, also encouraged more vaccination intentions of mothers for their babies [,]. Furthermore, normative support from family, friends, healthcare providers, and the community surrounding immunisations increased intention to obtain seasonal influenza vaccine [,]. Migration status also influenced uptake, as some migrants had higher vaccine uptake, for example, being of Roma origin or an immigrant []. Other positive influencing individual factors included the marital status of parents (married parents had higher vaccination rates), [] health service accessibility, and affordability [].
4.7.3. Challenges of Intervention Implementation
Participants with a history of previous vaccination adverse outcomes generally had lower than average vaccination uptake and varied presumptions of the information provided, which was not always in line with recommendations [,]. Also, insufficient time to engage in every aspect of the intervention was a challenge, often related to family commitments competing with time for the intervention [,]. Hence, some participants relied on HCWs to keep them informed []. In addition, Frew et al. [,] observed that using a single message exposure was insufficient to persuade or act as a significant factor for determining intention to get immunisations. Less engagement with specific intervention components was also due to low levels of interest; for instance, in the study by Kriss et al., fewer people used the iBook, which was considered less relatable and more challenging to understand than the video [].
Some operational and financial issues were identified at both hospital and community levels. In hospitals, involving HCWs with different expertise, who are traditionally unfamiliar with the specific vaccinations that were offered, such as neonatologists, paediatricians, nurses, and obstetricians was a challenge []. Obtaining health provider reports was also time-consuming and required repeated follow-ups and documentation processes []. While at the community level, limited community representative time availability [] and the qualitative nature of the study did not allow extrapolation of the exact proportion of community members infected with HBV, difficulty in accessing HBV care, or burden from lack of HBV knowledge []. In the study by McPhee et al., it was not possible to determine the eligibility of some participants who were unreachable or refused to be interviewed []. Loss for follow-up due to difficulty in contacting non-attenders with name changes also affected the Larcher et al. study []. This was similar to the limited information available to HCWs to allow accurate identification of patients, and very few could find records reporting vaccination dates []. Stringer et al. also noted that there was no data on the completion of the entire vaccine series; therefore, the study population cohort may not be substantively protected. However, acceptance rates were likely to be higher when the vaccination was offered as part of the usual care, for instance, pregnant adolescents []. Also, there was a need to offer several vaccination opportunities, including during evening hours or weekends [].
A few intervention components were stopped before the end of the study. For instance, the insurance pilot program where insurance payment would be accepted only for people with vaccination insurance showed that accounting outweighed the benefits, and was discontinued in the study by Peterson et al. []. Also, Schwartz et al. reported that vaccine supplies were exhausted before the expected study end date []. Financial constraints to sustain the interventions were challenging [,,]. For example, Wood et al. reported that the overall cost-effectiveness of the intervention (case managers for infants < 6 weeks and home visits two weeks prior to scheduled immunisations) compared unfavourably with other medical interventions []. Also, Nyamathi et al. were concerned that the policies enacted in the California state prison system, particularly realignment (or reducing the state prison population by transferring inmates to county jails), would affect vaccination completion [].
5. Discussion
This systematic review identified 23 studies across five countries that reported interventions aimed at increasing vaccination uptake among ethnic minority populations. All the studies reported that the interventions were somewhat effective, with varying improvements in vaccine uptake and/or reduction in hesitancy. Twenty-six BCTs, six BCW intervention functions, and seven policy categories were identified to promote vaccine delivery and uptake. The most common BCTs used in at least six studies were Information about health consequences (to increase risk awareness and vaccine knowledge), Information about antecedents (to advise patients about vaccination impacts), Credible source (to provide guidelines and health workers’ collaboration with community organisations), Prompts/cues (to provide reminders and motivation), Instruction on how to perform the behaviour (to present guidance on how to get vaccinated), Restructuring the physical environment (to provide ease of access to vaccine service), and Framing/reframing (to present information in formats that can motivate change).
Some intervention functions appeared more effective in improving vaccination rates; however, the most effective were those with a community-based component, which included community clinics and the offer of free vaccination. Predictors of vaccine uptake often acted as both barriers and facilitators. The main predictors included the experience of sickness after previous vaccination and fear of side effects, which were related to barriers and linked to limited knowledge of vaccination transmission, low perceived susceptibility, and low vaccine efficacy. Behavioural patterns linked to positive attributes sometimes negatively influenced vaccine uptake. For instance, a holistic lifestyle (such as healthy eating and breastfeeding) was perceived to be sufficient for providing immunity against vaccine-preventable diseases. These barriers were largely overcome through interaction, encouragement or recommendations from healthcare professionals, which was a key facilitator for increased vaccination uptake. Hence, despite intervention challenges, such as the high resource cost (financial cost and vaccine supply) needed to deliver some interventions, recommendations for future interventions in these studies included the need for additional resources to enhance social support, in addition to providing vaccine education that was locally and culturally relevant to the target community [,,].
Previous studies have reported psychological predictors of vaccination, including vaccination history, perception of disease severity, and vaccine safety and effectiveness [,,,]. To address these challenges, as identified from this review, positive changes in beliefs about vaccinations can be achieved through increased awareness by targeting individuals or groups directly, compared to public campaigns, and where public campaigns are used, it is important to follow-up with direct contact with individuals and groups in a timely manner []. The most effective way of sharing information was visual modes of delivery, which were more effective than written communication; sharing information in this way enabled participants to identify with the characters in the resource []. Also, although most messages can facilitate increased vaccine uptake, positively framed messages have more influence in increasing vaccination [,]. Previous studies have shown that negatively framed messages aimed to elicit feelings of anticipated regret for not getting vaccinated were generally perceived as patronising and unprofessional []. Hence, it is important that messages are factual and emphasise the costs and benefits of vaccination, thereby showing that two-sided messages are viewed more credibly []. Furthermore, having messages from credible sources like physicians did not always significantly increase vaccine awareness and intention to receive a vaccine, but in combination with a trusted community representative, such as a church pastor, more community members can be motivated to consider taking vaccines [].
Although mass media campaigns can reach a broad spectrum of any population, their effects remain modest, primarily because of the effect gaps between intention-to-action [,]. This can be addressed through the use of personalised reminders and prompts []. Furthermore, mass vaccine clinic venues often do not suit some ethnic, cultural or faith-based minority groups, especially where privacy and time are required for meaningful dialogue []. Poor understanding of the health system, language, cultural barriers, and poor doctor-patient relationships compound access issues in minority groups []. Some barriers may stem from longstanding structural inequities and the fact that some racial and ethnic minority communities live in areas of higher deprivation with large family sizes, low-income levels, and a higher burden of diseases, which was identified as a risk factor during the COVID-19 pandemic [,,]. Adapting existing services and guidelines to match community preferences, for instance, offering free services through community-based clinics compared to hospitals to deliver vaccines, emphasises the interrelationship between different intervention functions (incentivisation, environmental restructuring, enablement and fiscal measures) and how using multi-intervention functions for vaccination services can improve the effectiveness of services provided.
5.1. Limitations of the Review
This review may be subject to publication and selection bias, as unsuccessful interventions may be less likely to be documented in peer-reviewed literature. The review is also limited in its focus on only respiratory and routinely recommended vaccines, which means the findings should be interpreted with caution for non-respiratory and routinely recommended vaccines. Study inclusion is likely to have been restricted due to use of PICO questions, which emphasise specific, single-component strategies, whereas many intervention strategies are neither designed nor evaluated in this way. Multi-component interventions were identified, but only overall impact data were presented. Therefore, outcome data for individual strategies to address vaccine hesitancy were not separately available.
There is evidence of vaccine hesitancy in all populations in different countries, but this is greater evidence among some ethnic minority populations [,]. Yet, only five countries were represented in this review, with most studies from the United States. No relevant study reporting interventions to support ethnic minority groups in Asia and Africa was identified. This indicates an evidence gap, on a global scale, about vaccinations for racial and ethnic minority groups. More research which includes racial and ethnic minority populations is required to ensure evidence-based vaccine interventions are developed that reflect the needs of all communities, including diverse groups. In addition, studies on COVID-19 vaccines were excluded as the aim of the study was designed, in part, to inform strategies to support the existing and future COVID-19 vaccination programme. However, inclusion of several non-COVID-19 respiratory vaccination interventions includes sufficient parallels and considerations for the COVID-19 vaccination programme.
5.2. Recommendations
The present review findings suggest that increased awareness and knowledge sharing from credible sources have the potential to encourage the general public to get vaccinated, but this needs to be community focused. It is also essential to strengthen engagement and build trust with ethnic minority communities, and acquire a better understanding of how to support diverse groups by ensuring more meaningful inclusion through more culturally competent health systems. This approach, especially for addressing COVID-19 hesitancy, would require co-producing solutions based on the principles of inclusion and engagement. This can be guided using three core elements as suggested by Chevallier et al., which are by testing a communication campaign addressing vaccine hesitancy, using behavioural insights to make vaccination more accessible, and leveraging the power of social norms []. To effectively design a community-based intervention, members of the community also need to be included. For instance, Frew et al. showed that engaging with potential participants in the formative stage of research provided additional insights into the content of the framed message, and this contributed to a high level of engagement in the final intervention []. Table 6 provides an overview of recommendations to develop vaccine interventions for racial and ethnic minority groups based on the findings of this review. The use of behavioural science frameworks such as the COM-B model, BCW, and BCT can guide the development of interventions which are tailored to the motivational drivers, educational needs, and which reflect the socio-cultural context of diverse communities. Table 6 outlines recommendations based on BCTs identified in this review that can be used to promote vaccine uptake in racial and ethnic minority communities.

Table 6.
Recommendations to develop vaccine interventions for racial and ethnic minority populations.
6. Conclusions
The relevance and effectiveness of vaccination strategies are critical for successful public health protection against infectious diseases. To optimise outcomes, all members of the population need to be engaged, and this includes racial and ethnic minority populations. Identifying the intervention components and behaviours that make effective and efficient services are essential for proper planning and implementation. This systematic review has shown which vaccine strategies work well and the factors that encourage vaccine uptake. The most common approach used is related to education and providing vaccine information to targeted populations, and this is most effective when provided in a visual format, delivered through credible sources which include healthcare professionals and respected community representatives, repeated exposure and providing follow-up opportunities for dialogue in a timely manner. To design effective interventions related to the approach identified in this review, strong support from government and healthcare organisations would be needed to institute tailored, culturally appropriate approaches, as there is no one-size-fits-all solution and vaccine strategies have to be adapted according to the different needs of the ethnic minority population.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines11071259/s1, Supplementary Table S1: BCT Taxonomy (v1): 93 hierarchically-clustered techniques; Supplementary Figure S2: OVID Medline Search Terms; and Supplementary Table S3: EM Vaccine Strategy Studies – Quality Assessment.
Author Contributions
Conceptualization, A.K., W.E. and A.C.; Methodology, A.K., W.E. and A.C.; Validation, A.K., W.E. and A.C.; Data Curation, W.E. and A.C.; Formal Analysis, W.E., E.G. and A.K.; Investigation, W.E.; Resources, K.K. and A.K.; Writing—Original Draft Preparation, W.E.; Writing—Review & Editing, W.E., A.K. and A.C.; Supervision, A.K.; Project Administration, W.E. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data generated.
Conflicts of Interest
KK and WE are supported by the National Institute for Health Research (NIHR) Applied Research Collaboration East Midlands (ARC EM) and the NIHR Leicester Biomedical Research Centre (BRC). KK is Director of the University of Leicester Centre for Ethnic Health Research. All other authors declare no conflicts of interest.
References
- Sze, S.; Pan, D.; Nevill, C.R.; Gray, L.J.; Martin, C.A.; Nazareth, J.; Minhas, J.S.; Divall, P.; Khunti, K.; Abrams, K.R.; et al. Ethnicity and clinical outcomes in COVID-19: A systematic review and meta-analysis. EClinicalMedicine 2020, 29, 100630. [Google Scholar] [CrossRef] [PubMed]
- Robertson, E.; Reeve, K.S.; Niedzwiedz, C.L.; Moore, J.; Blake, M.; Green, M.; Katikireddi, S.V.; Benzeval, M.J. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav. Immun. 2021, 94, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Paul, E.; Steptoe, A.; Fancourt, D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg. Health Eur. 2021, 1, 100012. [Google Scholar] [CrossRef] [PubMed]
- Ekezie, W.; Czyznikowska, B.M.; Rohit, S.; Harrison, J.; Miah, N.; Campbell-Morris, P.; Khunti, K. The views of ethnic minority and vulnerable communities towards participation in COVID-19 vaccine trials. J. Public Health 2020, 43, e258–e260. [Google Scholar] [CrossRef]
- Gaughan, C.H.; Razieh, C.; Khunti, K.; Banerjee, A.; Chudasama, Y.V.; Davies, M.J.; Dolby, T.; Gillies, C.L.; Lawson, C.; Mirkes, E.M.; et al. COVID-19 vaccination uptake amongst ethnic minority communities in England: A linked study exploring the drivers of differential vaccination rates. J. Public Health 2023, 45, e65–e74. [Google Scholar] [CrossRef]
- Public Health England. Disparities in the Risk and Outcomes of COVID-19; Public Health England: London, UK, 2021. [Google Scholar]
- OpenSAFELY Collaborative; MacKenna, B.; Curtis, H.J.; Morton, C.E.; Inglesby, P.; Walker, A.J.; Morley, J.; Mehrkar, A.; Bacon, S.; Hickman, G.; et al. Trends, regional variation, and clinical characteristics of COVID-19 vaccine recipients: A retrospective cohort study in 23.4 million patients using OpenSAFELY. MedRxiv 2021. [Google Scholar] [CrossRef]
- ONS. Coronavirus and Vaccine Hesitancy, Great Britain: 26 May to 20 June 2021; Office of National Statistics: London, UK, 2021. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/bulletins/coronavirusandvaccinehesitancygreatbritain/26mayto20june2021 (accessed on 27 April 2023).
- Weinstein, N.D.; Kwitel, A.; McCaul, K.D.; Magnan, R.E.; Gerrard, M.; Gibbons, F.X. Risk perceptions: Assessment and relationship to influenza vaccination. Health Psychol. 2007, 26, 146–151. [Google Scholar] [CrossRef]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- SAGE. Factors Influencing COVID-19 Vaccine Uptake among Minority Ethnic Groups; Executive Summary; Scientific Advisory Group for Emergencies: London, UK, 2020. [Google Scholar]
- Curtis, H.J.; Inglesby, P.; Morton, C.E.; MacKenna, B.; Green, A.; Hulme, W.; Walker, A.J.; Morley, J.; Mehrkar, A.; Bacon, S.; et al. Trends and clinical characteristics of COVID-19 vaccine recipients: A federated analysis of 57.9 million patients’ primary care records in situ using OpenSAFELY. Br. J. Gen. Pract. 2021, 72, e51–e62. [Google Scholar] [CrossRef]
- Reid, J.A.; Mabhala, M.A. Ethnic and minority group differences in engagement with COVID-19 vaccination programmes-at Pandemic Pace; when vaccine confidence in mass rollout meets local vaccine hesitancy. Isreal J. Health Policy Res. 2021, 10, 33. [Google Scholar] [CrossRef]
- WHO. Ten Threats to Global Health in 2019; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Marshall, S.; Fleming, A.; Sahm, L.J.; Moore, A.C. Identifying intervention strategies to improve HPV vaccine decision-making using behaviour change theory. Vaccine 2023, 41, 1368–1377. [Google Scholar] [CrossRef] [PubMed]
- Sabnis, S.S.; Conway, J.H. Overcoming Challenges to Childhood Immunizations Status. Pediatr. Clin. N. Am. 2015, 62, 1093–1109. [Google Scholar] [CrossRef] [PubMed]
- Hardt, K.; Bonanni, P.; King, S.; Santos, J.I.; El-Hodhod, M.; Zimet, G.D.; Preiss, S. Vaccine strategies: Optimising outcomes. Vaccine 2016, 34, 6691–6699. [Google Scholar] [CrossRef] [PubMed]
- Witteman, H.O. Addressing Vaccine Hesitancy with Values. Pediatrics 2015, 136, 215–217. [Google Scholar] [CrossRef] [PubMed]
- Ala, A.; Edge, C.; Zumla, A.; Shafi, S. Specific COVID-19 messaging targeting ethnic minority communities. EClinicalMedicine 2021, 35, 100862. [Google Scholar] [CrossRef]
- Control ECfDPa. Guidance on Infection Prevention and Control of Coronavirus Disease (COVID-19) in Migrant and Refugee Reception and Detention Centres in the EU/EEA and the United Kingdom—June 2020; ECDC: Stockholm, Sweden, 2020. [Google Scholar]
- Corker, E.; Marques, M.; Johnston, M.; West, R.; Hastings, J.; Michie, S. Behaviour change techniques taxonomy v1: Feedback to inform the development of an ontology. Wellcome Open Res. 2023, 7, 211. [Google Scholar] [CrossRef]
- Howlett, N.; García-Iglesias, J.; Bontoft, C.; Breslin, G.; Bartington, S.; Freethy, I.; Huerga-Malillos, M.; Jones, J.; Lloyd, N.; Marshall, T.; et al. A systematic review and behaviour change technique analysis of remotely delivered alcohol and/or substance misuse interventions for adults. Drug Alcohol Depend. 2022, 239, 109597. [Google Scholar] [CrossRef]
- WHO. Strategies for Addressing Vaccine Hesitancy-A Systematic Review; WHO SAGE Working Group Dealing with Vaccine Hesitancy; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Bazargan, M.; Wisseh, C.; Adinkrah, E.; Ameli, H.; Santana, D.; Cobb, S.; Assari, S. Influenza Vaccination among Underserved African-American Older Adults. BioMed Res. Int. 2020, 2020, 2160894. [Google Scholar] [CrossRef]
- Hoppe, K.K.; Eckert, L.O. Achieving high coverage of H1N1 influenza vaccine in an ethnically diverse obstetric population: Success of a multifaceted approach. Infect. Dis. Obstet. Gynecol. 2011, 2011, 746214. [Google Scholar] [CrossRef]
- Pritchard, E.N.; Jutel, A.; Tollafield, S. Positive provider interventions for enhancing influenza vaccination uptake among Pacific peoples in New Zealand. N. Z. Med. J. 2011, 124, 75–82. [Google Scholar]
- NICE. Behaviour Change: Individual Approaches; National Institute for Health and Care Excellence: London, UK, 2014. [Google Scholar]
- Epton, T.; Lawes-Wickwar, S.; Ghio, D.; Shorter, G.W.; Whittaker, E.; Arden, M.A.; Armitage, C.; Byrne-Davis, L.; Chadwick, P.; Drury, J.; et al. Optimising Vaccination Uptake for COVID-19; British Psychological Society: London, UK, 2021. [Google Scholar]
- Wooten, K.G.; Wortley, P.M.; Singleton, J.A.; Euler, G.L. Perceptions matter: Beliefs about influenza vaccine and vaccination behavior among elderly white, black and Hispanic Americans. Vaccine 2012, 30, 6927–6934. [Google Scholar] [CrossRef]
- MRC. A Framework for the Development and Evaluation of RCTs for Complex Interventions to Improve Health; Medical Research Council: London, UK, 2000. [Google Scholar]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new Medical Research Council guidance. Int. J. Nurs. Stud. 2013, 50, 587–592. [Google Scholar] [CrossRef]
- Michie, S.; Van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef]
- Sallis, A.; Bunten, A.; Bonus, A.; James, A.; Chadborn, T.; Berry, D. The effectiveness of an enhanced invitation letter on uptake of National Health Service Health Checks in primary care: A pragmatic quasi-randomised controlled trial. BMC Fam. Pract. 2016, 17, 35. [Google Scholar] [CrossRef]
- Garnett, C.V.; Crane, D.; Brown, J.; Kaner, E.F.S.; Beyer, F.R.; Muirhead, C.R.; Hickman, M.; Beard, E.; Redmore, J.; de Vocht, F.; et al. Behavior Change Techniques Used in Digital Behavior Change Interventions to Reduce Excessive Alcohol Consumption: A Meta-regression. Ann. Behav. Med. 2018, 52, 530–5433. [Google Scholar] [CrossRef]
- Alageel, S.; Gulliford, M.C.; McDermott, L.; Wright, A.J. Multiple health behaviour change interventions for primary prevention of cardiovascular disease in primary care: Systematic review and meta-analysis. BMJ Open 2017, 7, e015375. [Google Scholar] [CrossRef]
- Heron, N.; Kee, F.; Donnelly, M.; Cardwell, C.; Tully, M.A.; Cupples, M.E. Behaviour change techniques in home-based cardiac rehabilitation: A systematic review. Br. J. Gen. Pract. J. R. Coll. Gen. Pract. 2016, 66, e747–e757. [Google Scholar] [CrossRef]
- Laba, T.-L.; Bleasel, J.; Brien, J.-A.; Cass, A.; Howard, K.; Peiris, D.; Redfern, J.; Salam, M.A.; Usherwood, T.; Jan, S. Strategies to improve adherence to medications for cardiovascular diseases in socioeconomically disadvantaged populations: A systematic review. Int. J. Cardiol. 2013, 167, 2430–2440. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Kamal, A.; Ekezie, W.; Farooqi, A.; Khunti, K. A Systematic Review of Drivers of Vaccine Hesitancy and Strategies to Reduce Vaccine Hesitancy in Ethnic Minority Populations. PROSPERO 2021 CRD42021239010 2021. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021239010 (accessed on 23 February 2021).
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Downes, M.J.; Brennan, M.L.; Williams, H.C.; Dean, R.S. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open 2016, 6, e011458. [Google Scholar] [CrossRef] [PubMed]
- CASP. Critical Appraisal Skills Programme Checklists 2018: Critical Appraisal Skills Programme. Available online: https://casp-uk.net/casp-tools-checklists/ (accessed on 18 April 2021).
- Frew, P.M.; Kriss, J.L.; Chamberlain, A.T.; Malik, F.; Chung, Y.; Cortés, M.; Omer, S.B. A randomized trial of maternal influenza immunization decision-making: A test of persuasive messaging models. Hum. Vaccines Immunother. 2016, 12, 1989–1996. [Google Scholar] [CrossRef] [PubMed]
- Kriss, J.L.; Frew, P.M.; Cortes, M.; Malik, F.A.; Chamberlain, A.T.; Seib, K.; Flowers, L.; Ault, K.A.; Howards, P.; Orenstein, W.A.; et al. Evaluation of two vaccine education interventions to improve pertussis vaccination among pregnant African American women: A randomized controlled trial. Vaccine 2017, 35, 1551–1558. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, K.; Berlin, M.; Schwartz, J.S.; Propert, K.; Ubel, P.A. Educational content and the effectiveness of influenza vaccination reminders. J. Gen. Intern. Med. 1999, 14, 695–698. [Google Scholar] [CrossRef]
- Daniels, N.A.; Juarbe, T.; Moreno-John, G.; Pérez-Stable, E.J. Effectiveness of adult vaccination programs in faith-based organizations. Ethn. Dis. 2007, 17, 15–22. [Google Scholar]
- Findley, S.E.; Irigoyen, M.; Sanchez, M.; Stockwell, M.S.; Mejia, M.; Guzman, L.; Ferreira, R.; Pena, O.; Chen, S.; Andres-Martinez, R. Effectiveness of a Community Coalition for Improving Child Vaccination Rates in New York City. Am. J. Public Health 2008, 98, 1959–1962. [Google Scholar] [CrossRef]
- Frew, P.M.; Zhang, S.; Saint-Victor, D.S.; Schade, A.C.; Benedict, S.; Banan, M.; Ren, X.; Omer, S.B. Influenza vaccination acceptance among diverse pregnant women and its impact on infant immunization. Hum. Vaccines Immunother. 2013, 9, 2591–2602. [Google Scholar] [CrossRef]
- Frew, P.M.; Owens, L.E.; Saint-Victor, D.S.; Benedict, S.; Zhang, S.; Omer, S.B. Factors associated with maternal influenza immunization decision-making: Evidence of immunization history and message framing effects. Hum. Vaccines Immunother. 2014, 10, 2576–2583. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Kalogriopoulou, K.; Pergialiotis, V.; Siahanidou, T.; Skiathitou, A.V.; Katerelos, P.; Goumalatsos, N.; Kostis, E.; Antsaklis, A.; Theodoridou, M. Acceptance of a post-partum influenza vaccination (cocooning) strategy for neonates in Greece. Vaccine 2012, 30, 5871–5874. [Google Scholar] [CrossRef]
- Nicoleau, A.; Nicoleau, C.A.; Balzora, J.D.; Oboh, A.; Siddiqui, N.; Rosenberg, C. Elderly African-Americans and the influenza vaccine: The impact of the primary care physician. J. Am. Med. Dir. Assoc. 2001, 2, 56–59. [Google Scholar] [CrossRef]
- Schwartz, K.L.; Neale, A.V.; Northrup, J.; Monsur, J.; Patel, D.A.; Tobar, R., Jr.; Wortley, P.M. Racial Similarities in Response to Standardized Offer of Influenza Vaccination A MetroNet Study. J. Gen. Intern. Med. 2006, 21, 346–351. [Google Scholar] [CrossRef]
- Wood, D.; Halfon, N.; Donald-Sherbourne, C.; Mazel, R.M.; Schuster, M.; Hamlin, J.S.; Pereyra, M.; Camp, P.; Grabowsky, M.; Duan, N. Increasing immunization rates among inner-city, African American children: A randomized trial of case management. J. Am. Med. Assoc. 1998, 279, 29–34. [Google Scholar] [CrossRef]
- Callahan, A.G.; Strassberg, E.R.; Rhoades, C.P.; Varghese, L.; Schulkin, J.; Power, M.L. Pregnant Women’s Opinions and Acceptance of Influenza and Tdap Vaccines. J. Women’s Health 2022, 31, 656–664. [Google Scholar] [CrossRef]
- DiTosto, J.D.; Weiss, R.E.; Yee, L.M.; Badreldin, N. Association of Tdap vaccine guidelines with vaccine uptake during pregnancy. PLoS ONE 2021, 16, e0254863. [Google Scholar] [CrossRef]
- Larcher, V.F.; Bourne, J.; Aitken, C.; Jeffries, D.; Hodes, D. Overcoming barriers to hepatitis B immunisation by a dedicated hepatitis B immunisation service. Arch. Dis. Child. 2001, 84, 114–119. [Google Scholar] [CrossRef]
- Ma, G.X.; Gao, W.; Tan, Y.; Chae, W.G.; Rhee, J. A Community-Based Participatory Approach to a Hepatitis B Intervention for Korean Americans. Prog. Community Health Partnersh. Res. Educ. Action 2012, 6, 7–16. [Google Scholar] [CrossRef]
- McPhee, S.J.; Nguyen, T.; Euler, G.L.; Mock, J.; Wong, C.; Lam, T.; Nguyen, W.; Nguyen, S.; Ha, M.Q.H.; Do, S.T.; et al. Successful Promotion of Hepatitis B Vaccinations among Vietnamese-American Children Ages 3 to 18: Results of a Controlled Trial. Pediatrics 2003, 111, 1278–1288. [Google Scholar] [CrossRef]
- Nyamathi, A.; Salem, B.E.; Zhang, S.; Farabee, D.; Hall, B.; Khalilifard, F.; Leake, B. Nursing Case Management, Peer Coaching, and Hepatitis A and B Vaccine Completion among Homeless Men Recently Released on Parole: Randomized Clinical Trial. Nurs. Res. 2015, 64, 177–189. [Google Scholar] [CrossRef]
- Stringer, M.; Ratcliffe, S.; Gross, R. Acceptance of hepatitis B vaccination by pregnant adolescents. MCN Am. J. Matern. Nurs. 2006, 31, 54–60. [Google Scholar] [CrossRef]
- Zibrik, L.; Huang, A.; Wong, V.; Lauscher, H.N.; Choo, Q.; Yoshida, E.M.; Ho, K. Let’s Talk About B: Barriers to Hepatitis B Screening and Vaccination among Asian and South Asian Immigrants in British Columbia. J. Racial Ethn. Health Disparities 2018, 5, 1337–1345. [Google Scholar] [CrossRef]
- Dunn, R.A.; Shenouda, P.E.; Martin, D.R.; Schultz, A.J. Videotape Increases Parent Knowledge About Poliovirus Vaccines and Choices of Polio Vaccination Schedules. Pediatrics 1998, 102, e26. [Google Scholar] [CrossRef] [PubMed]
- Sagy, I.; Novack, V.; Gdalevich, M.; Greenberg, D. Mass media effect on vaccines uptake during silent polio outbreak. Vaccine 2018, 36, 1556–1560. [Google Scholar] [CrossRef] [PubMed]
- Donaldson, B.; Jain, P.; Holder, B.S.; Lindsey, B.; Regan, L.; Kampmann, B. What determines uptake of pertussis vaccine in pregnancy? A cross sectional survey in an ethnically diverse population of pregnant women in London. Vaccine 2015, 33, 5822–5828. [Google Scholar] [CrossRef] [PubMed]
- Peterson, P.; McNabb, P.; Maddali, S.R.; Heath, J.; Santibañez, S. Engaging Communities to Reach Immigrant and Minority Populations: The Minnesota Immunization Networking Initiative (MINI), 2006–2017. Public Health Rep. 2019, 134, 241–248. [Google Scholar] [CrossRef]
- Daniels, N.A.; Gouveia, S.; Null, D.; Gildengorin, G.L.; Winston, C.A. Acceptance of pneumococcal vaccine under standing orders by race and ethnicity. J. Natl. Med. Assoc. 2006, 98, 1089–1094. [Google Scholar]
- Bish, A.; Yardley, L.; Nicoll, A.; Michie, S. Factors associated with uptake of vaccination against pandemic influenza: A systematic review. Vaccine 2011, 29, 6472–6484. [Google Scholar] [CrossRef]
- Brien, S.; Kwong, J.C.; Buckeridge, D.L. The determinants of 2009 pandemic A/H1N1 influenza vaccination: A systematic review. Vaccine 2012, 30, 1255–1264. [Google Scholar] [CrossRef]
- Ekezie, W.; Maxwell, A.; Byron, M.; Czyznikowska, B.; Osman, I.; Moylan, K.; Gong, S.; Pareek, M. Health Communication and Inequalities in Primary Care Access during the COVID-19 Pandemic among Ethnic Minorities in the United Kingdom: Lived Experiences and Recommendations. Int. J. Environ. Res. Public Health 2022, 19, 15166. [Google Scholar] [CrossRef]
- Mowbray, F.; Marcu, A.; Godinho, C.A.; Michie, S.; Yardley, L. Communicating to increase public uptake of pandemic flu vaccination in the UK: Which messages work? Vaccine 2016, 34, 3268–3274. [Google Scholar] [CrossRef]
- O’Keefe, D.J.; Jensen, J.D. The relative persuasiveness of gain-framed and loss-framed messages for encouraging disease prevention behaviors: A meta-analytic review. J. Health Commun. 2007, 12, 623–644. [Google Scholar] [CrossRef]
- Chevallier, C.; Hacquin, A.-S.; Mercier, H. COVID-19 Vaccine Hesitancy: Shortening the Last Mile. Trends Cogn. Sci. 2021, 25, 331–333. [Google Scholar] [CrossRef]
- Mercier, H. Not Born Yesterday: The Science of Who We Trust and What We Believe; Princeton University Press: Princeton, NJ, USA, 2020. [Google Scholar]
- Vann, J.C.J.; Jacobson, R.M.; Coyne-Beasley, T.; Asafu-Adjei, J.K.; Szilagyi, P.G. Patient reminder and recall interventions to improve immunization rates (Review). Cochrane Database Syst. Rev. 2018, 1, CD003941. [Google Scholar] [CrossRef]
- Ekezie, W.; Awwad, S.; Krauchenberg, A.; Karara, N.; Dembiński, Ł.; Grossman, Z.; del Torso, S.; Dornbusch, H.J.; Neves, A.; Copley, S.; et al. Access to Vaccination among Disadvantaged, Isolated and Difficult-to-Reach Communities in the WHO European Region: A Systematic Review. Vaccines 2022, 10, 1038. [Google Scholar] [CrossRef]
- Crawshaw, A.F.; Deal, A.; Rustage, K.; Forster, A.S.; Campos-Matos, I.; Vandrevala, T.; Würz, A.; Pharris, A.; Suk, J.E.; Kinsman, J.; et al. What must be done to tackle vaccine hesitancy and barriers to COVID-19 vaccination in migrants? J. Travel Med. 2021, 28, taab048. [Google Scholar] [CrossRef]
- Caspi, G.; Dayan, A.; Eshal, Y.; Liverant-Taub, S.; Twig, G.; Shalit, U.; Lewis, Y.; Shina, A.; Caspi, O. Socioeconomic disparities and COVID-19 vaccination acceptance: A nationwide ecologic study. Clin. Microbiol. Infect. 2021, 27, 1502–1506. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).