COVID-19 Vaccine Hesitancy in a Representative Education Sector Population in Qatar
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Instrument
2.3. Statistical Analysis and Sample Size Calculation
3. Results
3.1. Sociodemographic Characteristics
3.2. Vaccine Acceptance
3.3. Knowledge Levels about COVID-19 Disease and Vaccines
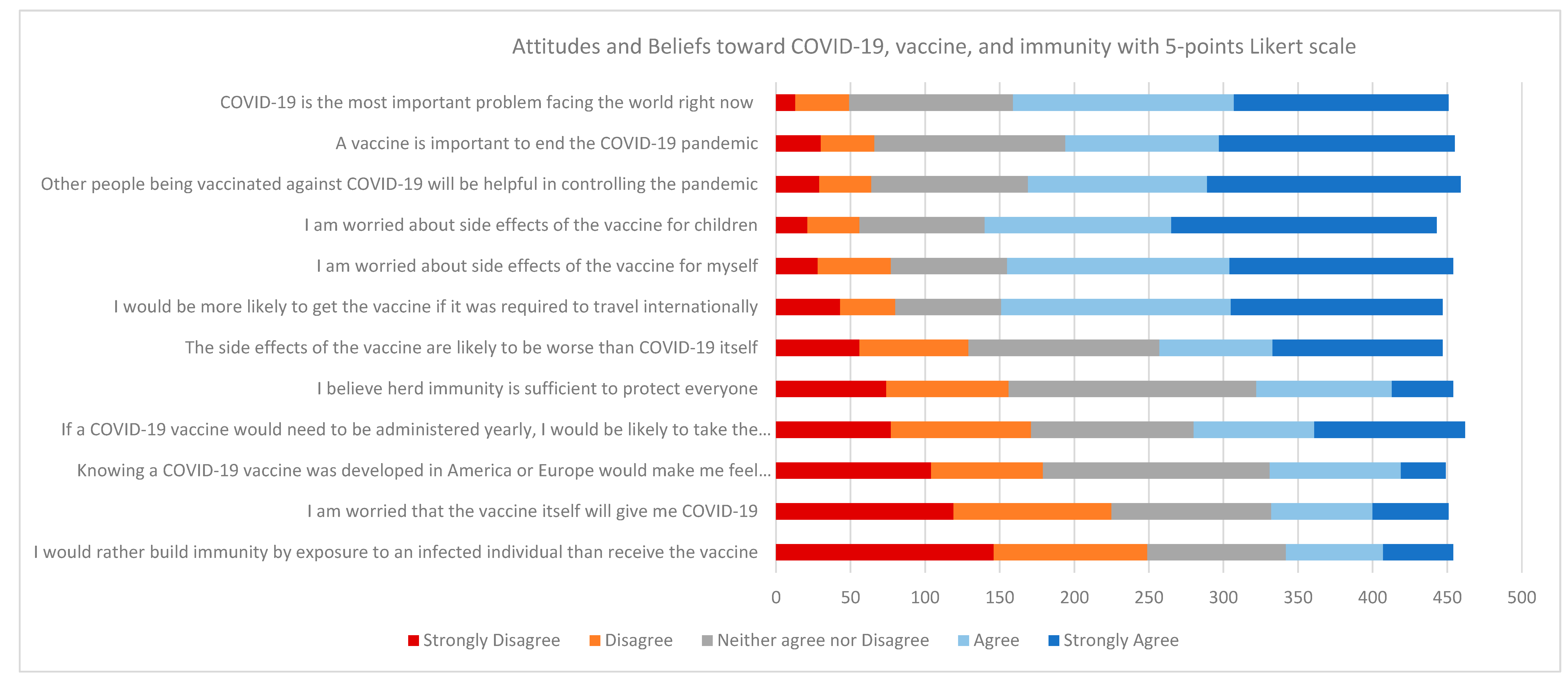
3.4. Attitudes and Beliefs towards COVID-19 Disease and Vaccine
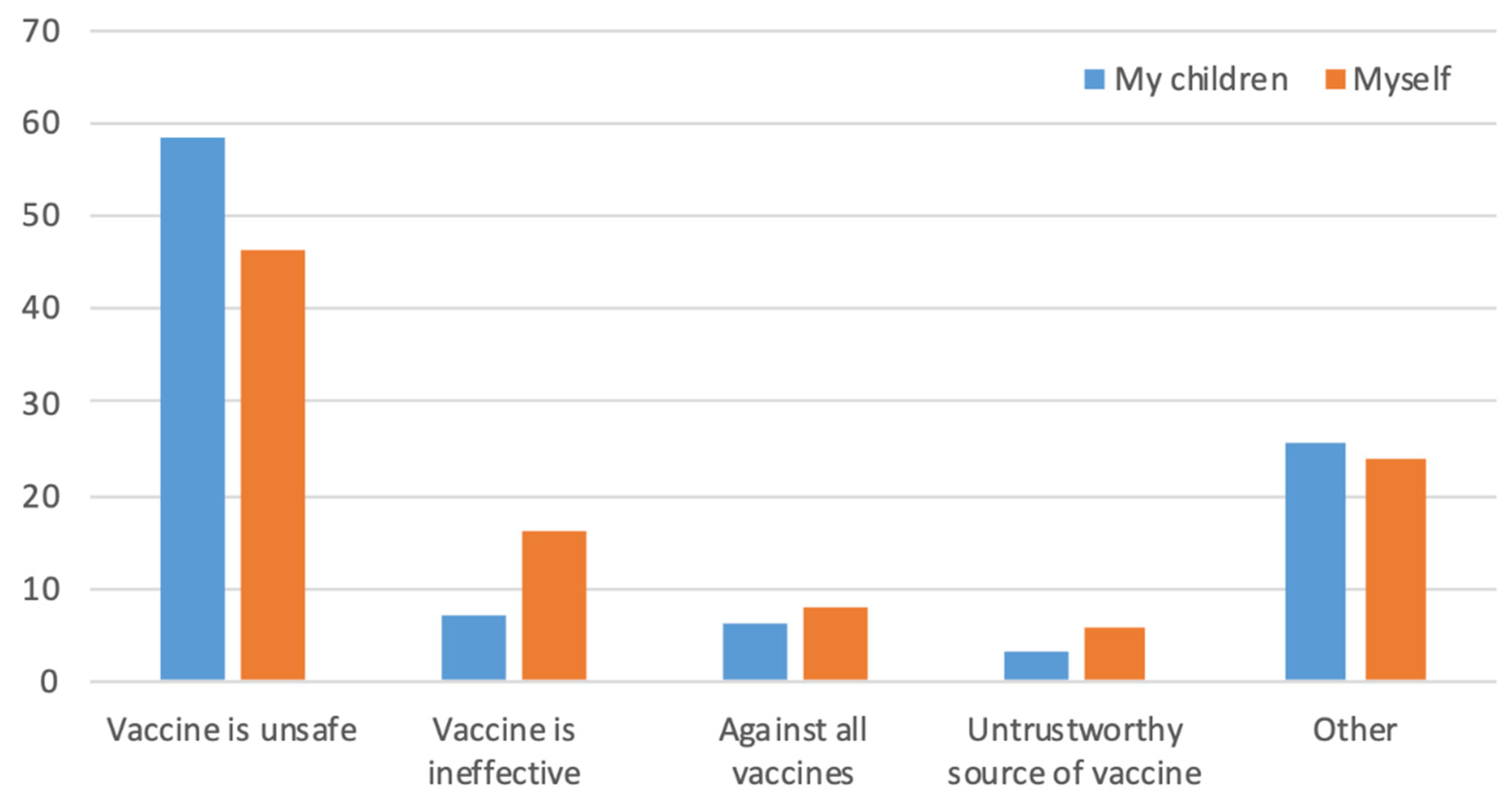
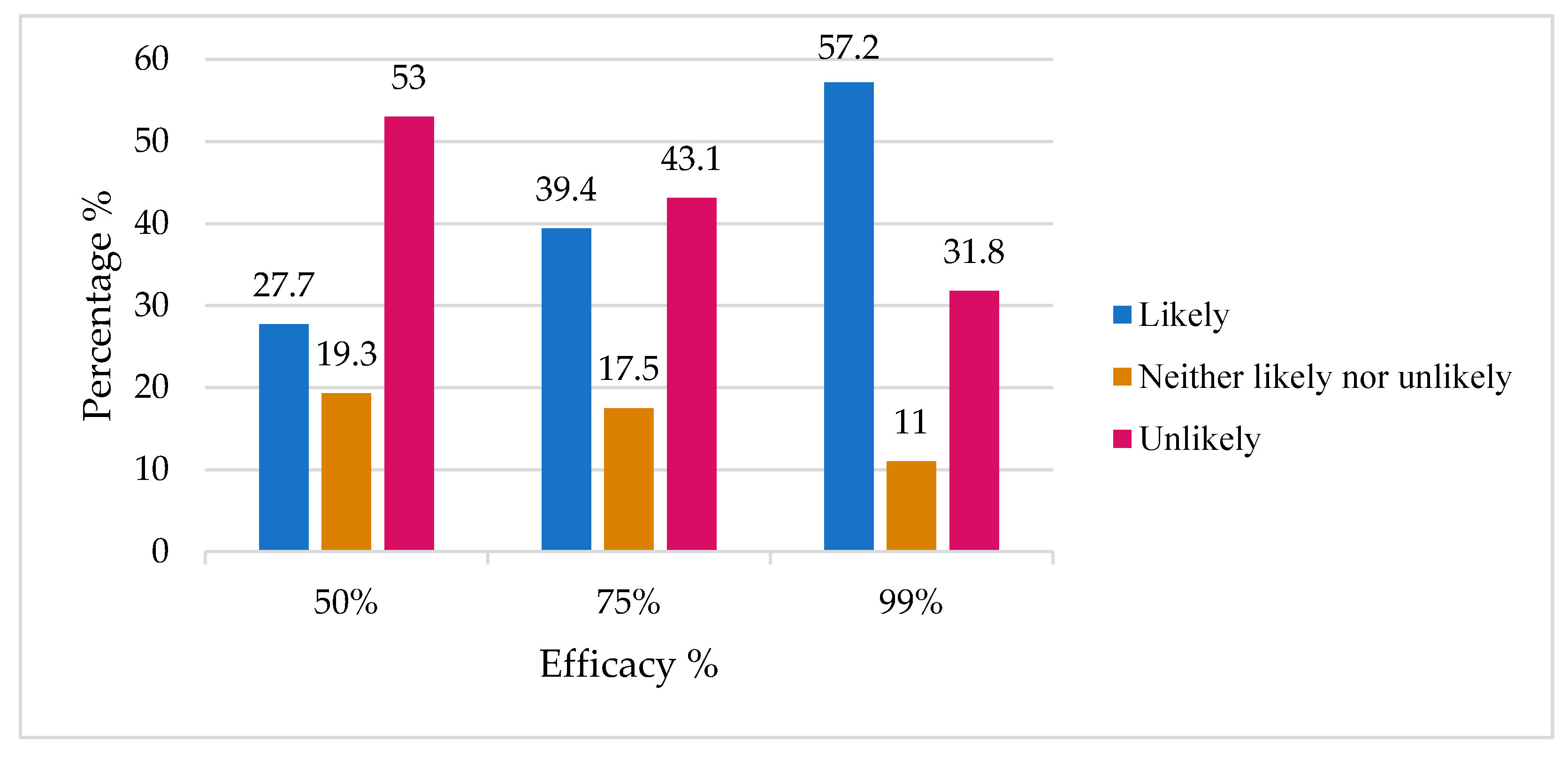
3.5. Other Determinants Influencing COVID-19 Vaccine Hesitancy and Acceptance
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wilson, S.L.; Wiysonge, C. Social Media and Vaccine Hesitancy. BMJ Glob. Health 2020, 5, e004206. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.M.; Vegvari, C.; Truscott, J.; Collyer, B.S. Challenges in Creating Herd Immunity to SARS-CoV-2 Infection by Mass Vaccination. Lancet 2020, 396, 1614–1616. [Google Scholar] [CrossRef]
- Lin, C.; Tu, P.; Beitsch, L.M. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines 2020, 9, 16. [Google Scholar] [CrossRef] [PubMed]
- Calnan, M.; Douglass, T. Hopes, Hesitancy and the Risky Business of Vaccine Development. Health Risk Soc. 2020, 22, 291–304. [Google Scholar] [CrossRef]
- DeStefano, F.; Shimabukuro, T.T. The MMR Vaccine and Autism. Annu. Rev. Virol. 2019, 6, 585–600. [Google Scholar] [CrossRef]
- Refuting A Lie That Won’t Die: Taking The Fight For Vaccines Beyond The Doctor’s Office|Health Affairs Blog. Available online: https://www.healthaffairs.org/do/10.1377/hblog20190226.742851/full/ (accessed on 1 April 2021).
- Eggertson, L. Lancet Retracts 12-Year-Old Article Linking Autism to MMR Vaccines. Can. Med. Assoc. J. 2010, 182, E199–E200. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Vaccine Hesitancy among Healthcare Workers and Their Patients in Europe: A Qualitative Study; European Centre for Disease Prevention and Control, Publications Office, European Union: Solna, Sweden, 2015. [Google Scholar]
- À Propos des Vaccins. Site Officiel du Pr Henri Joyeux. De Blog Pr Henri Joyeux, France. 2015. Available online: https://professeur-joyeux.com/en/ (accessed on 21 May 2021).
- Lucia, V.C.; Kelekar, A.; Afonso, N.M. COVID-19 Vaccine Hesitancy among Medical Students. J. Public Health 2020, fdaa230. [Google Scholar] [CrossRef] [PubMed]
- Pogue, K.; Jensen, J.L.; Stancil, C.K.; Ferguson, D.G.; Hughes, S.J.; Mello, E.J.; Burgess, R.; Berges, B.K.; Quaye, A.; Poole, B.D. Influences on Attitudes Regarding Potential COVID-19 Vaccination in the United States. Vaccines 2020, 8, 582. [Google Scholar] [CrossRef]
- Irwin, A. What It Will Take to Vaccinate the World against COVID-19. Nature 2021. [Google Scholar] [CrossRef] [PubMed]
- Moberly, T. Covid-19: Vaccine Hesitancy Fell after Vaccination Programme Started. BMJ 2021, n837. [Google Scholar] [CrossRef]
- Alabdulla, M.; Reagu, S.M.; Al-Khal, A.; Elzain, M.; Jones, R.M. COVID-19 Vaccine Hesitancy and Attitudes in Qatar: A National Cross-sectional Survey of a Migrant-majority Population. Influenza Other Respi Viruses 2021. irv.12847. [Google Scholar] [CrossRef]
- AlAwadhi, E.; Zein, D.; Mallallah, F.; Bin Haider, N.; Hossain, A. Monitoring COVID-19 Vaccine Acceptance in Kuwait During the Pandemic: Results from a National Serial Study. RMHP 2021, 14, 1413–1429. [Google Scholar] [CrossRef]
- Al-Qerem, W.A.; Jarab, A.S. COVID-19 Vaccination Acceptance and Its Associated Factors Among a Middle Eastern Population. Front. Public Health 2021, 9, 632914. [Google Scholar] [CrossRef]
- Qunaibi, E.; Basheti, I.; Soudy, M.; Sultan, I. Hesitancy of Arab Healthcare Workers towards COVID-19 Vaccination: A Large-Scale Multinational Study. Vaccines 2021, 9, 446. [Google Scholar] [CrossRef]
- Alley, S.J.; Stanton, R.; Browne, M.; To, Q.G.; Khalesi, S.; Williams, S.L.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. As the Pandemic Progresses, How Does Willingness to Vaccinate against COVID-19 Evolve? IJERPH 2021, 18, 797. [Google Scholar] [CrossRef]
- Neumann-Böhme, S.; Varghese, N.E.; Sabat, I.; Barros, P.P.; Brouwer, W.; van Exel, J.; Schreyögg, J.; Stargardt, T. Once We Have It, Will We Use It? A European Survey on Willingness to Be Vaccinated against COVID-19. Eur. J. Health Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef]
- Di Pietrantonj, C.; Rivetti, A.; Marchione, P.; Debalini, M.G.; Demicheli, V. Vaccines for Measles, Mumps, Rubella, and Varicella in Children. Cochrane Database Syst. Rev. 2020. [Google Scholar] [CrossRef]
- Barello, S.; Nania, T.; Dellafiore, F.; Graffigna, G.; Caruso, R. ‘Vaccine Hesitancy’ among University Students in Italy during the COVID-19 Pandemic. Eur. J. Epidemiol. 2020, 35, 781–783. [Google Scholar] [CrossRef] [PubMed]
- Di Martino, G.; Di Giovanni, P.; Di Girolamo, A.; Scampoli, P.; Cedrone, F.; D’Addezio, M.; Meo, F.; Romano, F.; Di Sciascio, M.B.; Staniscia, T. Knowledge and Attitude towards Vaccination among Healthcare Workers: A Multicenter Cross-Sectional Study in a Southern Italian Region. Vaccines 2020, 8, 248. [Google Scholar] [CrossRef] [PubMed]
- Szmyd, B.; Bartoszek, A.; Karuga, F.F.; Staniecka, K.; Błaszczyk, M.; Radek, M. Medical Students and SARS-CoV-2 Vaccination: Attitude and Behaviors. Vaccines 2021, 9, 128. [Google Scholar] [CrossRef]
- Szmyd, B.; Karuga, F.F.; Bartoszek, A.; Staniecka, K.; Siwecka, N.; Bartoszek, A.; Błaszczyk, M.; Radek, M. Attitude and Behaviors towards SARS-CoV-2 Vaccination among Healthcare Workers: A Cross-Sectional Study from Poland. Vaccines 2021, 9, 218. [Google Scholar] [CrossRef] [PubMed]
- Di Gennaro, F.; Murri, R.; Segala, F.V.; Cerruti, L.; Abdulle, A.; Saracino, A.; Bavaro, D.F.; Fantoni, M. Attitudes towards Anti-SARS-CoV2 Vaccination among Healthcare Workers: Results from a National Survey in Italy. Viruses 2021, 13, 371. [Google Scholar] [CrossRef] [PubMed]
- Wood, S.; Schulman, K. Beyond Politics—Promoting Covid-19 Vaccination in the United States. N. Engl. J. Med. 2021, 384, e23. [Google Scholar] [CrossRef] [PubMed]
- Riccò, M.; Gualerzi, G.; Ranzieri, S.; Ferraro, P.; Bragazzi, N.L. Knowledge, Attitudes, Practices (KAP) of Italian Occupational Physicians towards Tick Borne Encephalitis. Trop. Med. 2020, 5, 117. [Google Scholar] [CrossRef] [PubMed]
| Demographic | Variable Category | n | % |
|---|---|---|---|
| Gender | Male | 173 | 37.4 |
| Female | 289 | 62.6 | |
| Age | 18–24 years | 151 | 32.7 |
| 25–34 years | 117 | 25.3 | |
| 35–44 years | 85 | 18.4 | |
| 45+ years | 109 | 23.6 | |
| Nationality | Qatari | 208 | 45 |
| Non-Qatari | 254 | 55 | |
| University Status | Student | 231 | 50 |
| Employee | 231 | 50 | |
| Colleges | Arts and Sciences | 107 | 23.2 |
| Business and Economics | 76 | 16.5 | |
| Engineering | 66 | 14.3 | |
| Education | 40 | 8.7 | |
| Law | 31 | 6.7 | |
| Health Sciences | 20 | 4.3 | |
| Islamic Studies | 17 | 3.7 | |
| Medicine | 9 | 1.2 | |
| Pharmacy | 6 | 1.3 | |
| Dental Medicine | 1 | 0.2 | |
| Others (including general services and presidency) | 82 | 17.7 | |
| Education Level | Diploma/undergraduate | 270 | 58.4 |
| Postgraduate | 192 | 41.6 |
| Demographic | Variable Category | Would Vaccinate n (%) | Would Not Vaccinate n (%) | X2 | p-Value |
|---|---|---|---|---|---|
| Gender Age | Male Female 18–24 years 25–34 years 35–44 years 45+ years | 123 (72.9) 161 (56.7) 77 (51) 61 (53.5) 61 (73.5) 85 (80.2) | 46 (27.1) 124 (43.3) 74 (49) 53 (46.5) 22 (26.5) 21 (19.8) | 12.02 30.91 | <0.001 <0.001 |
| Nationality QU Status | Qatari Non-Qatari Student Employee | 105 (51.2) 179 (71.9) 114 (49.8) 170 (75.6) | 100 (48.8) 70 (28.1) 115 (50.2) 55 (24.4) | 20.50 32.19 | <0.001 <0.001 |
| Education level | Diplomas/Bachelors Masters/PhDs | 136 (50.9) 148 (79.1) | 131 (49.1) 39 (20.9) | 37.39 | <0.001 |
| Health-related discipline | Health colleges | 29 (80.6) | 7 (19.4) | ||
| Non-health colleges | 255 (61) | 163 (39) | 5.40 | 0.02 |
| Knowledge Score | Would Vaccinate n (%) | Would Not Vaccinate n (%) | Statistic | p-Value |
|---|---|---|---|---|
| Low (0–3) | 30 (73.2) | 11 (26.8) | X2 = 2.6 | 0.27 |
| Medium (4–5) | 100 (59.5) | 68 (40.5) | ||
| High (6–7) | 154 (62.9) | 91 (37.1) |
| Question | Answers | Would Vaccinate n (%) | Would Not Vaccinate n (%) | Multinomial Logistic Regression Analysis | ||
|---|---|---|---|---|---|---|
| Odd ratio * | 95% CI | p | ||||
| How important is it for you to get the flu vaccine every year? | Important | 93 (86.9) | 14 (13.1) | 8.51 | 4.37–16.5 | <0.0001 |
| Somewhat important | 75 (75.8) | 24 (24.2) | 3.38 | 1.94–5.88 | <0.0001 | |
| Not important | 116 (46.8) | 132 (53.2) | Reference | |||
| What is your primary source of information regarding COVID-19? | Professional source | 139 (65.3) | 74 (34.7) | 2.39 | 0.28–20.1 | 0.43 |
| Unprofessional source | 141 (60) | 94 (40) | 1.81 | 0.21–15.5 | 0.59 | |
| Leaders | 2 (50) | 2 (50) | Reference | |||
| How severe were the symptoms of COVID-19 infection for yourself? | Severe | 1 (16.7) | 5 (9.5) | 0.21 | 0.02–2.01 | 0.17 |
| Moderate | 16 (57.1) | 12 (42.9) | 1.12 | 0.44–2.9 | 0.79 | |
| Not at all | 54 (58.7) | 38 (41.3) | Reference | |||
| How severe were the symptoms of COVID-19 infection for your family member? | Severe | 21 (51.2) | 20 (48.8) | 0.75 | 0.33–1.7 | 0.49 |
| Moderate | 71 (62.3) | 43 (37.7) | 1.21 | 0.65–2.3 | 0.53 | |
| Not at all | 50 (58.8) | 35 (41.2) | Reference | |||
| How severe were the symptoms of COVID-19 infection for your friend? | Severe | 20 (69%) | 9 (31) | 1.39 | 0.54–3.61 | 0.49 |
| Moderate | 77 (57.5) | 57 (42.5) | 0.92 | 0.52–1.62 | 0.77 | |
| Not at all | 57 (58.8) | 40 (41.2) | Reference | |||
| How severe were the symptoms of COVID-19 infection for coworker? | Severe | 6 (50) | 6 50) | 0.10 | 0.08–1.26 | 0.10 |
| Moderate | 54 (62.8) | 32 (37.2) | 0.57 | 0.29–1.16 | 0.12 | |
| Not at all | 64 (66) | 33 (34) | Reference | |||
| What is the minimum length of time a testing process would take to make you feel comfortable with COVID-19 vaccine? | 3 months–1 year | 139 (89.1) | 17 (10.9) | 13.1 | 7.01–24.0 | <0.0001 |
| 1–2 years | 68 (63) | 40 (37) | 2.91 | 1.71–4.91 | <0.0001 | |
| 3+ years | 77 (40.5) | 113 (59.5) | Reference | |||
| I worry that the rushed pace of testing for a COVID-19 vaccine will fail to detect potential side effects. | Agree | 155 (52.9) | 138 (47.1) | 0.26 | 0.12–0.54 | <0.0001 |
| Neither agree nor disagree | 80 (78.4) | 22 (21.6) | 0.75 | 0.32–1.76 | 0.50 | |
| Disagree | 49 (83.1) | 10 (16.9) | Reference | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Mulla, R.; Abu-Madi, M.; Talafha, Q.M.; Tayyem, R.F.; Abdallah, A.M. COVID-19 Vaccine Hesitancy in a Representative Education Sector Population in Qatar. Vaccines 2021, 9, 665. https://doi.org/10.3390/vaccines9060665
Al-Mulla R, Abu-Madi M, Talafha QM, Tayyem RF, Abdallah AM. COVID-19 Vaccine Hesitancy in a Representative Education Sector Population in Qatar. Vaccines. 2021; 9(6):665. https://doi.org/10.3390/vaccines9060665
Chicago/Turabian StyleAl-Mulla, Reem, Marawan Abu-Madi, Qusai M. Talafha, Reema F. Tayyem, and Atiyeh M. Abdallah. 2021. "COVID-19 Vaccine Hesitancy in a Representative Education Sector Population in Qatar" Vaccines 9, no. 6: 665. https://doi.org/10.3390/vaccines9060665
APA StyleAl-Mulla, R., Abu-Madi, M., Talafha, Q. M., Tayyem, R. F., & Abdallah, A. M. (2021). COVID-19 Vaccine Hesitancy in a Representative Education Sector Population in Qatar. Vaccines, 9(6), 665. https://doi.org/10.3390/vaccines9060665






