Abstract
The cardiovascular system can be programmed by a diversity of early-life insults, leading to cardiovascular disease (CVD) in adulthood. This notion is now termed developmental origins of health and disease (DOHaD). Emerging evidence indicates hydrogen sulfide (H2S), a crucial regulator of cardiovascular homeostasis, plays a pathogenetic role in CVD of developmental origins. Conversely, early H2S-based interventions have proved beneficial in preventing adult-onset CVD in animal studies via reversing programming processes by so-called reprogramming. The focus of this review will first summarize the current knowledge on H2S implicated in cardiovascular programming. This will be followed by supporting evidence for the links between H2S signaling and underlying mechanisms of cardiovascular programming, such as oxidative stress, nitric oxide deficiency, dysregulated nutrient-sensing signals, activation of the renin–angiotensin system, and gut microbiota dysbiosis. It will also provide an overview from animal models regarding how H2S-based reprogramming interventions, such as precursors of H2S and H2S donors, may prevent CVD of developmental origins. A better understanding of cardiovascular programming and recent advances in H2S-based interventions might provide the answers to bring down the global burden of CVD.
1. Introduction
Cardiovascular disease (CVD) is the leading cause of death worldwide, accounting for almost one third of all global deaths [1]. CVD is a cluster of disorders of the heart and blood vessels and is comprised of coronary heart disease, peripheral vascular disease, cerebrovascular disease and other conditions. Although CVD is most common in older adults, atherosclerosis can begin in childhood and progress slowly across the life span [2]. Therefore, reducing the global burden of CVD by identifying children at risk and providing preventive interventions early are extremely important. Noteworthy, CVD can originate from the early stages of life, not only childhood but tracing back into the fetal life. This theory is now termed the developmental origins of health and disease (DOHaD) by observing how a suboptimal environment in utero has an adverse influence on offspring outcomes in later life [3].
The fetal cardiovascular system is vulnerable to adverse early-life environmental insults [4]. Developmental plasticity accommodates morphological and functional changes during organogenesis, leading to endothelial dysfunction, stiffer vascular tree, small coronary arteries, low nephron endowment, and fewer cardiomyocytes, through a process known as cardiovascular programming [4,5,6]. So far, several mechanisms underlying cardiovascular programming have been proposed, like oxidative stress, nitric oxide (NO) deficiency, activation of the renin–angiotensin system (RAS), dysregulated nutrient-sensing signals, and dysbiosis of gut microbiota [4,5,6].
Hydrogen sulfide (H2S), the third gasotransmitter, has emerged as a crucial regulator of cardiovascular homeostasis [7,8,9]. H2S exerts multifaceted biological functions, including vasodilatation, angiogenesis, antioxidant, anti-inflammation, mitochondria bioenergetics, and antiapoptosis [10,11]. In this regard, H2S-releasing drugs have been considered as potential therapeutics for CVD [7,8]. It is noteworthy that the DOHaD concept provides a strategy termed reprogramming to reverse or postpone the programming processes in early life, accordingly protecting offspring against many adult diseases of developmental origins [12]. Emerging evidence suggests that H2S can be used as a reprogramming strategy in hypertension of developmental origins [13]. Although H2S has been shown to have beneficial effects on CVD [7,8], whether it could serve as a reprogramming intervention for developmental origins of CVD remains largely unclear.
The central aim of this review is to give an overview of H2S implicated in cardiovascular programming. The use of H2S-based interventions as a reprogramming approach to protect offspring against CVD of developmental origins will be summarized.
Our search strategy was designed to retrieve related literature from PubMed/MEDLINE indexed articles. We used different combinations of search terms: “cardiovascular disease”, “developmental programming”, “DOHaD”, “atherosclerosis”, “heart”, “vascular”, “mother”, “endothelial dysfunction”, “hydrogen sulfide”, “cysteine”, “garlic”, “pregnancy”, “offspring”, “progeny”, “reprogramming”, and “hypertension”. We also used the reference lists of identified articles to find other potential studies. The last search was conducted on 30 December 2020.
2. Hydrogen Sulfide in the Cardiovascular System
2.1. H2S Signaling Pathway
H2S, a colorless gas with a characteristic foul odor of rotten eggs, was first identified as an environmental toxin in the 1700s and opened three centuries of research into its biological roles [14]. In the late 1990s, H2S was reclassified as the third gaseous signaling molecule, alongside nitric oxide (NO) and carbon monoxide (CO) [10]. Currently, H2S is known as a ubiquitous second messenger molecule with important functions in cardiovascular physiology [10,15]. Much of the previous work investigating the actions of H2S has been directly focused on incident CVD; however, there is a growing need to better understand the mechanisms and pathways of H2S signaling in CVD of developmental origins.
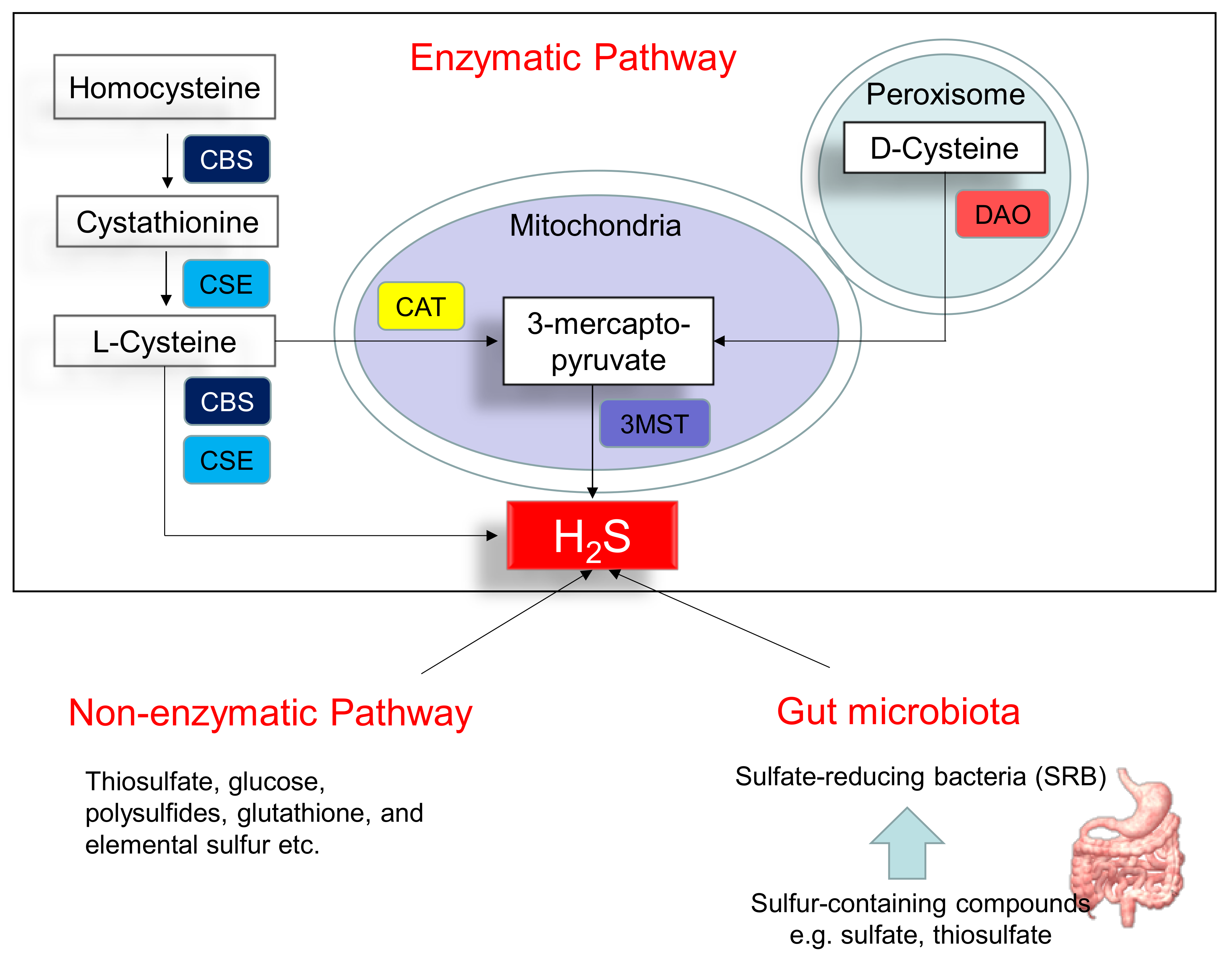
Figure 1 illustrates three major pathways of H2S synthesis, including enzymatic pathway, nonenzymatic pathway, and bacteria origins. Three enzymes have been identified to enzymatically generate H2S, cystathionine β-synthase (CBS), cystathionine γ-lyase (CSE), and 3-mercaptopyruvate sulphurtransferase (3MST) [10]. CBS and CSE are cytosolic enzymes, but 3-MST is mainly existing in the mitochondria. l-cysteine is the principal substrate for both CBS and CSE to generate H2S. CBS and CSE can also produce H2S using other substrates. Homocysteine can be catalyzed by CBS to generate cystathionine, followed by CSE to produce l-cysteine. All of the above-mentioned H2S-generating enzymes are expressed in the heart and blood vessels [10,16]. In an alternative pathway, 3-mercaptopyruvate, the substrate for 3-MST to produce H2S, is provided by cysteine aminotransferase (CAT) and D-amino acid oxidase (DAO). In the peroxisome, d-cysteine can be catabolized by DAO to generate H2S [17]. Besides the enzymatic pathway, H2S can be nonenzymatically produced through thiosulfate, glucose, polysulfides, glutathione, and elemental sulfur.
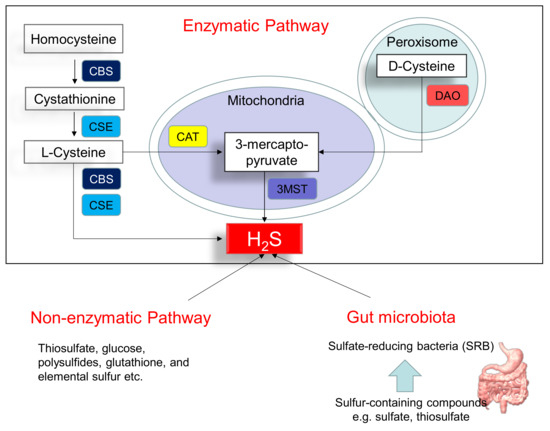
Figure 1.
Schematic representation of three major sources of H2S: enzymatic pathway, nonenzymatic pathway, and bacterial origins. Cystathionine β-synthase (CBS) catalyzes homocysteine to produce Cystathionine. Cystathionine γ-lyase (CSE) catalyzes cystathionine to form l-cysteine or l-cysteine to generate H2S. 3-Mercaptopyruvate sulfurtransferase (3MST) produces H2S from 3-mercaptopyruvate, which is generated by cysteine aminotransferase (CAT) and d-amino acid oxidase (DAO) from l-cysteine and d-cysteine, respectively. Another source of endogenous H2S is coming from nonenzymatic processes. The other source of H2S is derived from gut microbes, mainly by the sulfate-reducing bacteria (SRB).
Another source of H2S is coming from the gut microbiota. Approximately fifty percent of fecal H2S is derived from bacteria. In the gut, sulfate-reducing bacteria (SRB) obtain energy from the oxidation of organic compounds, reducing sulfate to H2S. Desulfovibrio account for 66% of all SRB in the human colon [18]. Other gut bacteria may also produce H2S by sulfite reduction, including species E. coli, Enterobacter, Salmonella, Klebsiella, Bacillus, Corynebacterium, Staphylococcus, and Rhodococcus [19]. Conversely, sulfur-oxidizing bacteria (SOB) reduces H2S via sulfur oxidation. The SOB members include genera Acidithiobacillus, Bacillus, Paracoccus, Pseudomonas, and Xanthobacter. In the gut, a huge quantity of H2S is oxidized by colonocytes to thiosulfate. The existence of thiosulfate in cecal venous blood not only reflects the detoxification of H2S but also the recycling of H2S.
In the circulation and tissues, free H2S can be scavenged and stored in the bound-sulfate and sulfane sulfur pools. Methylation and oxidation are two major mechanisms of H2S metabolism. H2S can be excreted in urine and flatus as free sulfate, free sulfide or thiosulfate.
2.2. The Role of H2S in the Pathophysiology of CVD
Multiple lines of evidence indicate that H2S plays a crucial role in the pathogenesis of CVD. The first are reports on knockout mice lacking genes encoding for CSE, CBS, and 3-MST. CSE is the most relevant H2S-producing enzyme in the cardiovascular system. Mutant mice lacking CSE had decreased H2S levels in the serum, heart, vessels, and other tissues [20]. CSE knockout mice displayed hypertension, endothelial dysfunction, and accelerated atherosclerosis [20,21]. CBS-deficient mice developed endothelial dysfunction [22] and cerebral vascular dysfunction [23]. 3-MST knockout mice developed hypertension and cardiac hypertrophy [17]. Second, are observations that impaired H2S-generating pathways were found in CVDs, including atherosclerosis [24], coronary artery disease [25], stroke [26], and peripheral vascular disease [15].
Third, are studies of protein S-sulfhydration, a vital post-translational modification induced by H2S [9]. S-sulfhydration usually increases the reactivity of target proteins via formation of a cysteine persulfide to target proteins [9]. H2S is able to S-sulfhydrate Kelch-like ECH associated protein 1 (Keap1), specificity protein-1 (SP-1), nuclear factor kappa-B (NF-κB) and interferon regulatory factor-1 (IRF-1) to regulate target gene transcription, which is crucial for the regulation of endothelial phenotypes, myocardial hypertrophy, mitochondrial biogenesis, oxidative stress, apoptosis and inflammation [9].
Fourth, several H2S-releasing drugs have demonstrated considerable promise for beneficial effects against CVDs in various animal models [7,8]. As reviewed elsewhere [7], several cytoprotective actions of H2S have been reported in the heart and vasculature. In the heart, the protective effects of H2S signaling was related to anti-inflammation, antiapoptosis, reduction of oxidative stress, and antifibrosis that leads to cardiac remodeling and functional improvements. In the vessels, H2S signaling can preserve endothelial NO synthase (eNOS)-derived NO production, while reducing oxidative stress, inflammation, fibrosis, and smooth muscle cell proliferation.
2.3. H2S Signaling in Various CVDs
Endothelial dysfunctions are associated with various CVDs, including hypertension, atherosclerosis, myocardial infarction, and the cardiovascular complications of diabetes. H2S can prime endothelial cells toward angiogenesis and contribute to relax vascular smooth muscle cells, and thereby reducing BP [27]. A deficit in H2S homeostasis is involved in the pathogenesis of endothelial dysfunction, while the application of H2S-releasing drugs to increase endogenous H2S level can restore endothelial function and antagonize the progression of CVDs.
Hypertension is a key risk factor for multiple CVDs. Like NO, H2S is a vasodilator. H2S has been reported to relax various blood vessels, such as the rat thoracic aorta, portal vein, and peripheral resistance vessels [28,29,30]. The involvement of H2S deficiency in hypertension has been examined in various animal models of hypertension, including the spontaneously hypertensive rat (SHR) [31], the renovascular hypertensive model [32], Dahl salt-sensitive rats [33], and NO-deficient rats [34]. Conversely, several prior studies have shown the beneficial effects of exogenous and endogenous H2S on hypertension, as reviewed elsewhere [35]. However, little is known about whether these H2S-based therapies could be used as reprogramming interventions perinatally to reduce the vulnerability to developing cardiovascular programming in offspring.
ApoE knockout mice developed advanced atherosclerosis related to a decreased plasma H2S level and vascular CSE expression/activity, suggesting disturbance of the vascular CSE/H2S pathway plays a role in the pathogenesis of atherosclerosis [36]. Additionally, a reduction in circulating H2S has also been noted in diabetic animal models and diabetic patients [37]. Conversely, H2S therapy proved beneficial in diabetes-accelerated atherosclerosis in diabetic mice [38]. In a rat model of myocardial ischemia–reperfusion (I/R), pharmacologic inhibition of CSE resulted in an increase in infarct size, whereas H2S replacement displayed myocardial protection [39]. Likewise, cardiac-specific overexpression of CSE in mice protects against myocardial I/R injury [40]. Summarizing, in clinical and preclinical studies of various CVDs, endogenous H2S production is diminished in these pathological conditions and H2S deficiency contributes to the progression of disease [7].
3. Evidence from Human Studies for Cardiovascular Programming
Important support for cardiovascular programming came from epidemiological reports following birth cohorts in the severe famines (Saint Petersburg 1941–1944; Dutch 1944–1945; Biafra 1967–1971) [41,42,43]. These observations revealed that exposure to undernutrition in early life induced a cluster of metabolic syndrome-related phenotypes such as hypertension, dyslipidemia, obesity, type 2 diabetes, and cardiovascular morbidity, all risks factor for coronary artery disease. Together with undernutrition, other environmental influences that can program later CVD have also been reviewed elsewhere [4,5,6]. These influences include maternal overnutrition, maternal smoking, maternal illness, and exposure to medication or environmental toxins. Fetal overnutrition because of maternal diabetes or obesity is related to offspring’s type 2 diabetes and obesity, both risk factors for CVD [44]. There is a positive association of maternal prenatal smoking with child adiposity and high BP [45]. Another report showed an association between maternal bisphenol A exposure and cardiometabolic traits in childhood [46]. In twins, the association between birth weight and BP is described in infants [47] and the lower bodyweight twins are prone to die from ischemic heart disease [48]. Moreover, several other perinatal risks affecting BP and cardiometabolic outcome in offspring have been identified, like low vitamin D intake [49], gestational hypertension [50], short-term breastfeeding [51], and excessive postnatal weight gain [52].
Although the influence of fetal life for future cardiovascular health has been evidenced by various epidemiologic human studies, it is almost impossible to test prospectively for critical developmental windows in humans. Moreover, nearly all cohort studies involve offspring who have not yet reached middle age and defined cardiovascular endpoints. Therefore, it is difficult to establish direct cause-and-effect relationships between particular environmental insults and later clinical cardiovascular outcomes in these cohort studies. Accordingly, it would be logical to use animal models to test our knowledge, for which a developmental window is decisive for cardiovascular programming, to identify how types of early life insults may program cardiovascular phenotypes, and what reprogramming intervention can be applied.
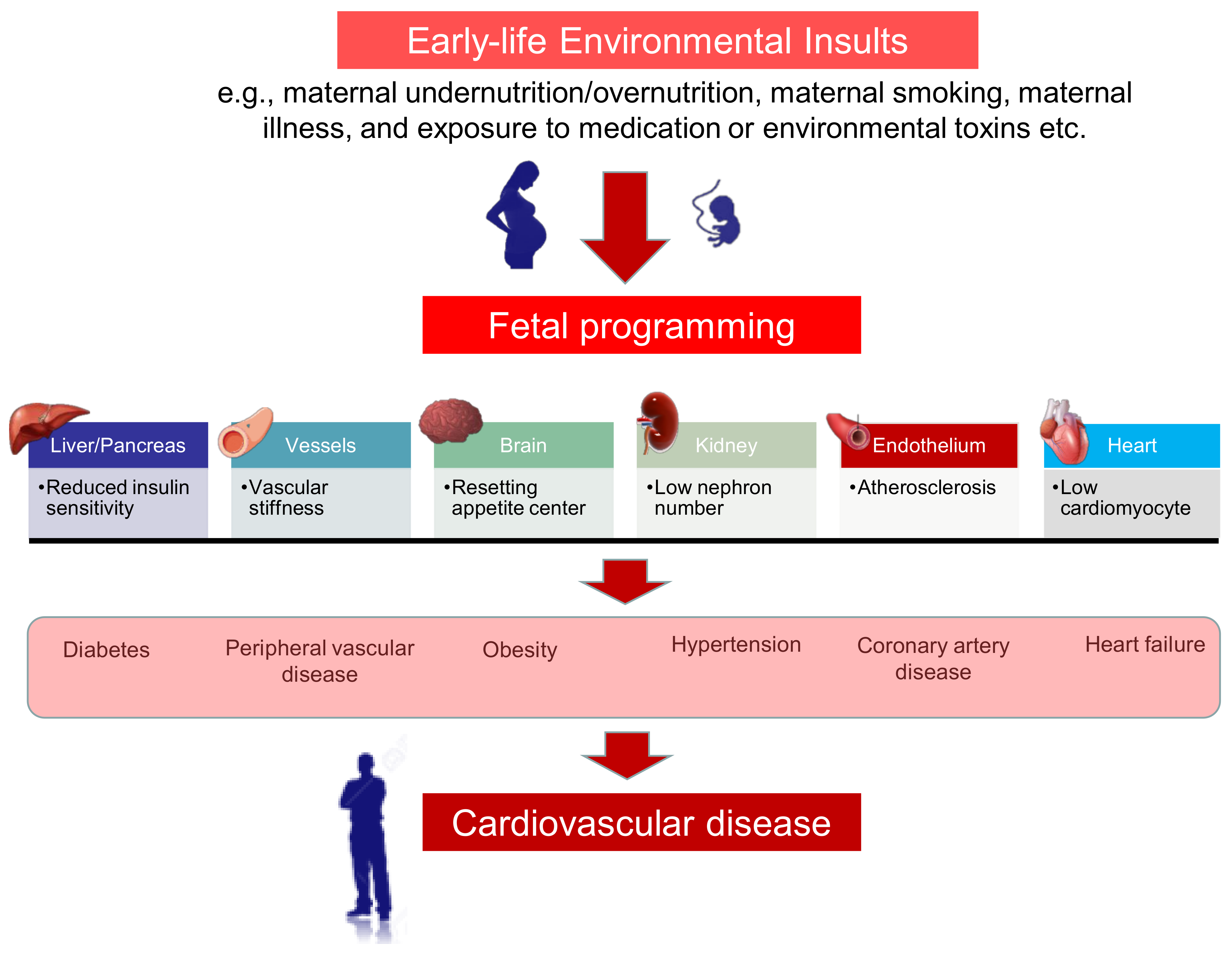
We propose a schema for summarizing the links between early-life insults, fetal programming, and the programming processes in different organ systems that are involved in the developmental programming of CVD, which is presented in Figure 2.
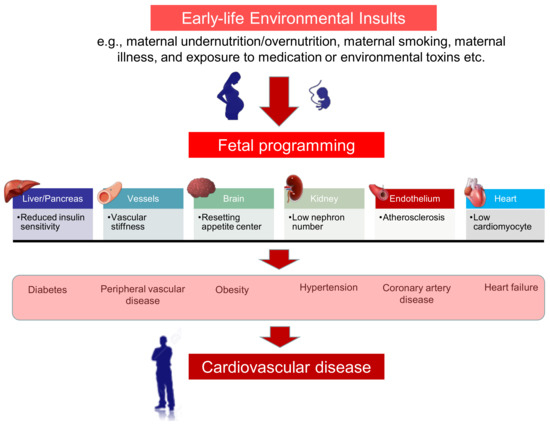
Figure 2.
Schematic illustration of links between maternal insults, fetal programming, and cardiovascular disease of developmental origins. A wide range of early-life environmental factors can influence fetal programming, include maternal undernutrition/overnutrition, maternal smoking, maternal illness, and exposure to medication or environmental toxins. During organogenesis, these maternal insults induce morphological and functional changes in different organ systems, such as liver, pancreas, heart, vessels, brain, kidney, and endothelium. Consequently, cardiovascular programming causes a cluster of phenotypes such as diabetes, hypertension, obesity, dyslipidemia, type 2 diabetes, and cardiovascular morbidity, all risks factor for cardiovascular disease.
4. Common Mechanisms Link H2S to Cardiovascular Programming
Despite a wide range of early-life environmental factors related to CVD in later life, current evidence suggests that there may be common molecular mechanisms underlying cardiovascular programming. Although the complete mechanisms remain inconclusive, animal models have provided important information on particular pathways including oxidative stress, NO, RAS, nutrient-sensing signals, and gut microbiota dysbiosis [4,5,6]. Remarkably, these extensive animal experiments have shown interactions between H2S signaling pathway and the abovementioned mechanisms. We will discuss each of these mechanisms in turn.
4.1. Oxidative Stress
The role of oxidative stress in the onset and progression of atherosclerosis and CVD has been widely studied [53,54]. Oxidative stress reflects an imbalance between oxidants (e.g., reactive oxygen species (ROS)) and antioxidants in favor of the first. Owing to its low antioxidant capacity, the developing fetus is extremely vulnerable to oxidative damage [55]. As we reviewed elsewhere [6], many maternal insults have been described to induce cardiovascular programming associated with oxidative stress, including undernutrition [56], preeclampsia [57], maternal diabetes [58], maternal exposure to nicotine or ethanol [59,60], maternal high-fat intake [61], and prenatal glucocorticoid or hypoxia exposure [62,63]. Oxidative damage in the heart, kidney, and blood vessels is well-known for its contribution to organ dysfunction and CVD. In the prenatal dexamethasone plus postnatal high-fat diet model, high-fat intake caused hypertension in adult offspring coinciding with reduced renal CBS and 3MST protein levels [62].
In contrast, a reprogramming strategy aimed at the reduction of oxidative stress by the use of perinatal antioxidants has been applied in animal models to prevent adult disease of developmental origins [64]. H2S has an antioxidant property, by which it is able to scavenge ROS, increase antioxidant glutathione, and activate nuclear factor E2-related factor 2 (Nrf2), a transcription factor for protection against oxidative stress [9,10,11]. Additionally, N-acetylcysteine (NAC), a precursor for H2S synthesis, has been reported to reprogram hypertension in animal models of developmental hypertension, including suramin-induced preeclampsia [57], and prenatal dexamethasone plus postnatal high-fat diet [62].
All together, these observations reveal that H2S might counterbalance oxidative stress to protect offspring against cardiovascular programming. Nevertheless, whether the anti-oxidative ability of H2S might be interconnected with other mechanisms to prevent CVD of developmental origins remains to be elucidated.
4.2. NO Deficiency
Endothelial dysfunction, mainly characterized by NO deficiency, is the initial event in the development of CVD [65]. NO deficiency in CVD is mainly due to L-arginine deficiency (the substrate for NOS), decreased abundance and/or activity of NOS, inactivation of NO under oxidative stress, and increased asymmetric dimethylarginine (ADMA, an endogenous NOS inhibitor) [66,67].
Abundant evidence indicates that the impaired ADMA/NO pathway contributes to the pathogenesis of cardiovascular programming. First, ADMA competes with L-arginine to inhibit NO production [68] and its increase is involved in coronary artery disease [69], congenital heart disease [70], type 2 diabetes [71], stroke [72], obesity [73], and peripheral arterial occlusive disease [74]. Second, gestational NO depletion induced by NG-nitro-L-arginine-methyl ester (L-NAME, an inhibitor of NOS) causes cardiovascular programming in adult offspring, characterized as endothelial dysfunction, hypertension, defect of carotid artery, and cardiac hypotrophy [75,76]. Third, reprogramming effects of therapeutic strategies targeting the ADMA/NO pathway to prevent the developmental programming of hypertension have been reported in various animal models [76,77,78,79].
On the other hand, growing evidence supports H2S and NO can affect not only the generation of each other but also the further downstream signaling pathway [80]. In the cardiovascular system, H2S and NO display some similar functions like regulation of vascular tone, stimulation of endothelial cell angiogenesis and protection against cardiac injury [80]. H2S has been reported to increase NO bioavailability via activation of eNOS through the Akt pathway or calcium release [81,82], enhancing eNOS activity by S-sulfhydration [9], decreased cGMP degradation by inhibiting phosphodiesterase activity [83], and reduction of nitrite [84]. Although there is plenty of evidence pointing towards their impacts on cardiovascular programming, much work remains still to be done to investigate the cross-talk between H2S and NO.
4.3. Renin–Angiotensin System
The RAS is a major hormone cascade involved in the cardiovascular system [85]. There are two pathways in the RAS system: classical and counter-regulatory pathways. The classical RAS is mainly made up of angiotensin-converting enzyme (ACE), angiotensin (Ang) II, and angiotensin type 1 receptor (AT1R). Under pathophysiological conditions, the classical RAS can be activated to trigger inflammation and structural remodeling, thus promoting cardiac and vascular damage [86]. While the ACE2–angiotensin (1–7)–Mas receptor pathway is termed counter-regulatory RAS to counterbalance the detrimental effects of Ang II signaling.
Both pathways have been implicated in fetal programming [87,88]. The classical RAS expression is reduced at birth, but returns to normal level with age [89]. Under pathophysiological conditions where this normalization overcompensates, consequently fetal programming activates the classical RAS, leading to hypertension in later life [89]. On the other hand, early blockade of the classical RAS can prevent developmental origins of hypertension [90,91]. These findings provide support for the view that RAS plays an important role in cardiovascular programming.
Low levels of H2S and the downregulation of its producing enzymes were reported in hypertensive models with activation of the classical RAS [92,93]. Conversely, the protective role of H2S against hypertension coincided with downregulating RAS-related mRNA expression [94], reducing AT1R protein level [95], and suppressing renin release [93]. Nevertheless, the detailed mechanisms underlying the modulation of RAS components by H2S contributing to the protection of CVD of developmental origins await further investigation.
4.4. Nutrient-Sensing Signals
Maternal nutritional status governs fetal growth and development by means of nutrient-sensing signals. Imbalanced maternal nutrition can disturb nutrient-sensing signals, leading to fetal programming and adverse cardiometabolic outcomes [96]. In the cardiovascular system, peroxisome proliferator-activated receptors (PPARs), cyclic adenosine monophosphate (AMP)-activated protein kinase (AMPK), silent information regulator transcript (SIRT), and PPARγ coactivator-1α (PGC-1α) are known nutrient-sensing signals [97]. These signals are involved in the pathogenesis in CVD, which have been reviewed extensively elsewhere [98,99].
Our prior research revealed that AMPK activation prevents the development of hypertension programmed via regulation of nutrient-sensing signals in various models of developmental hypertension, including high-fat diet [100], high-fructose diet [101], L-NAME plus postweaning high-fructose diet [102], and prenatal dexamethasone exposure plus postweaning high-fat diet [103]. Additionally, PPARs govern the expression of specific sets of target genes involved in hypertension of developmental origins [104], which can be driven by maternal nutritional insults.
Besides, AMPK, SIRT1, and PGC-1α can mediate autophagy, a self-degradative process that promotes proteolytic degradation of cytosolic components at the lysosome [105]. AMPK can induce mitochondrial biogenesis by activating the PGC-1α, either directly or through the SIRT1 [106]. Since autophagy contributes to the homeostasis in most cells of cardiovascular origin (e.g., cardiomyocytes, endothelial cells, and arterial smooth muscle cells) and the development of CVD [107,108], early interventions by AMPK activators or PPAR modulators have been considered as a potential reprogramming strategy against CVD of developmental origins [109].
AMPK and SIRT1 are considered as main mediators of H2S-associated cardiovascular beneficial effects [109]. Activation of AMPK and mediation of autophagy participate in the H2S-induced cytoprotective effect [110]. The cardioprotection of H2S is associated with AMPK phosphorylation and alleviation of autophagy in a myocardial ischemia mice model [111]. In another study, administration of exogenous H2S could inhibit the excessive autophagy of vascular endothelial cells by regulating the AMPK signaling pathway [112]. Moreover, H2S can promote SIRT1 activity to mediate angiogenesis [113]. Another report showed the protective effects of H2S against ischemia/reperfusion (I/R) injury are related to the activation of SIRT1/PGC-1α in a rat I/R model [114]. These observations demonstrate that the interplay between H2S and nutrient-sensing signals are implicated in CVD of developmental origins.
4.5. Gut Microbiota Dysbiosis
The gut bacteria can affect the control of the cardiovascular system via two pathways [115]. First, gut bacteria and/or their metabolites can stimulate the enteric afferent sensory fibers, consequently driving the brainstem cardiovascular centers. Second, gut microbiota-derived metabolites are able to enter into the bloodstream and affect the function of the cardiovascular system.
Adverse environmental conditions occurring early in life can alter the microbial composition of the gut, leading to many adult diseases like CVD [116,117]. So far, the adverse effects of gut microbiota dysbiosis on atherosclerosis, myocardial infarction, arrhythmia, and heart failure have been established, as reviewed elsewhere [103]. Several mechanisms underlying gut microbiota dysbiosis have been linked to CVD, including alterations of short-chain fatty acids (SCFA) and tryptophan-derived metabolites, increases of trimethylamine-N-oxide (TMAO), activation of the RAS, and inhibition of NO as well as H2S [118,119,120].
Conversely, approaches including probiotics, prebiotics, postbiotics (e.g., SCFAs), or microbial inhibitors that target specific pathways (e.g., TMAO), have shown beneficial cardiovascular effects [121]. Our previous research demonstrated that supplementation with prebiotic inulin, probiotics Lactobacillus casei, or postbiotics acetate during pregnancy and lactation can protect adult offspring against hypertension programmed by a variety of maternal insults [122,123,124].
Although gut bacteria-derived H2S has been reported to display BP-lowering effect [125], there is still limited information on the role of microbes-derived H2S on cardiovascular programming. Recently, data obtained from our laboratory demonstrated that maternal NAC therapy that protected male SHR offspring against hypertension was linked to increased fecal concentrations of H2S and thiosulfate, augmentation of H2S-producing pathway in the kidneys, and alterations of gut microbiota [126]. As thiosulfate is a metabolite of H2S and also an index of the sulfide pool [127], our results suggest that targeting microbe-derived H2S might be a potential approach to prevent hypertension and deserves further evaluation. Another study reported that a high-fat diet caused hypertension in adult offspring and was associated with reduced plasma and fetal H2S levels, renal H2S-releasing activity, and a decrease in α-diversity in the gut microbiota [128]. Conversely, garlic oil therapy in pregnancy and lactation protected adult offspring against hypertension, which was related to increased mRNA abundance and activity of H2S-generating enzymes in offspring kidneys as well as increased microbial richness and microbial diversity [128].
Overall, these findings establish a close connection between H2S and other important mechanisms involved in cardiovascular programming. Although there is emerging evidence for crosstalk between H2S and particular mechanisms related to CVD of developmental origins, more research is required to gain insight into how H2S may play an essential role in mediating other mechanisms, to develop a specific strategy to reduce their impact on developmental programming of CVD.
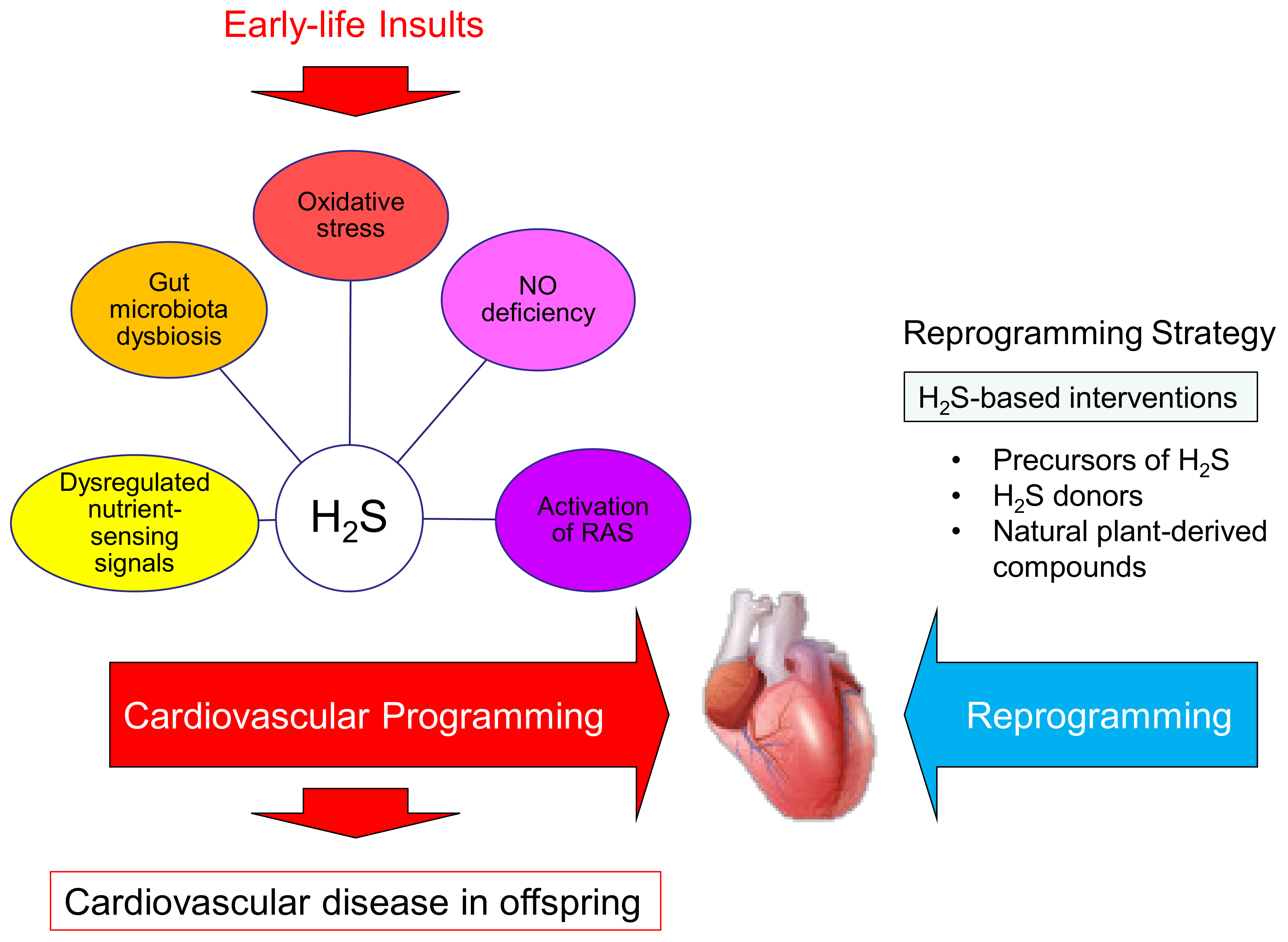
A summary of the links between H2S and other mechanisms implicated in cardiovascular reprogramming by H2S-based interventions to prevent developmental programming of cardiovascular disease is depicted in Figure 3.
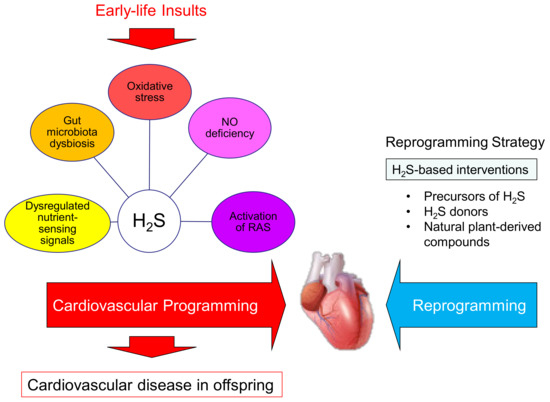
Figure 3.
Schema outlining the cardiovascular programming versus reprogramming interventions. Maternal insults can induce cardiovascular programming, consequently leading to cardiovascular disease in adulthood. Hydrogen sulfide (H2S) interconnects with other mechanisms and plays a key role in the pathogenesis of cardiovascular programming. These mechanisms include oxidative stress, nitric oxide (NO) deficiency, activation of the renin–angiotensin system (RAS), dysregulated nutrient-sensing signals, and gut microbiota dysbiosis. Conversely, early H2S-based interventions may reverse or delay programmed processes to prevent cardiovascular disease of developmental origins by so-called reprogramming.
5. H2S-Based Reprogramming Intervention
In the past decade, there has been heightened enthusiasm for the development H2S-based agents as potential therapeutics [7,8]. Sulfide salts, such as sodium sulfide and sodium hydrosulfide, represent the first class of H2S donors [129]. Sulfide salts provide direct and prompt release of free H2S. Naturally occurring H2S donors derived from garlic and onions generate free H2S at a slower rate than sulfide salts [130]. Earlier on, GYY4137 was developed in 2008 as one of the first slow-releasing H2S donors [131], and its slow H2S-releasing profile better mimics physiological H2S production. However, the poor pharmacological properties of sulfide salts and naturally occurring H2S donors warrant the need for further development of novel, synthetic H2S donors like SG-1002 [132]. Additionally, thiol-activated H2S donors (e.g., acyl perthiol donors) [133], pH-controlled H2S donors (e.g., JK donors) [134], and enzyme-dependent H2S donors [135], have been designed and shown cardiovascular benefits. Although novel H2S-donating agents are designed and tested in preclinical models of CVD, few of them have been examined in CVD of developmental origins.
Here, we show Table 1 that summarizes studies documenting H2S-based reprogramming interventions in animal models of cardiovascular programming, restricting interventions to critical periods during early development [52,57,72,85,114,136,137,138,139,140]. In the current review, we only considered studies reporting offspring outcomes starting from childhood.

Table 1.
Summary of H2S-based modalities used as reprogramming interventions in animal models of cardiovascular programming.
As shown in Table 1, rats have been the dominant animal species used. Various developmental programming models have been studied, including the genetic hypertension model [93,136], suramin-induced preeclampsia model [57], NG-nitro-l-arginine-methyl-ester (L-NAME) induced preeclampsia model [76], prenatal dexamethasone and postnatal high-fat diet [62], maternal hypertension [126], high-fat diet [128], maternal nicotine exposure [137,138], and maternal renovascular hypertension model [139,140]. The major adverse cardiovascular outcome is hypertension [57,62,76,93,126,128,139,140], followed by myocardial ischemia-reperfusion injury [137,138] and sympathetic activation [139,140]. The reprogramming effects of H2S-based therapies have been reported in rats ranging from 12 week to 8 months of age, which is roughly equivalent to human ages from young to middle adulthood. Available H2S-based treatment modalities used as reprogramming interventions include l-cysteine, d-cysteine, NAC, sodium hydrosulfide (NaHS), and garlic.
5.1. Precursors of H2S
l-cysteine is a sulfur-containing amino acid. Besides, l-cysteine is a component of glutathione, a potent antioxidant in our body. As it is the substrate for H2S, l-cysteine supplementation is a way to produce endogenous H2S in experimental studies. Since H2S and glutathione are closely linked to BP regulation [13,141], l-cysteine has shown an antihypertensive effect [142]. NAC, a stable cysteine analog, has shown beneficial effects for hypertension and CVD in human and experimental studies [143,144]. Another H2S precursor, d-cysteine, is nutritionally antagonistic, and, hence, has received less attention [145]. Although one previous report indicating d-cysteine supplementation protects against ischemia/reperfusion injury in the kidney [136], its effect in the heart and vessels remains unknown.
We previously presented that high salt-treated SHRs supplemented with d- or l-cysteine between four and six weeks of age were protected against hypertension and kidney injury at 12 weeks old [136]. Although one study reported that the d-cysteine pathway has an 80-fold greater H2S-releasing activity compared to the l-cysteine pathway [146], our results demonstrated that their beneficial effects on BP are comparable. Similarly, early NAC therapy, starting at four weeks of age, has proved beneficial for hypertension in SHRs [147]. As such, the use of NAC therapy in pregnancy and lactation has been shown to have benefits for hypertension of developmental origins in several animal models, including suramin-induced preeclampsia [57], prenatal dexamethasone and postnatal high-fat diet [62], L-NAME-induced preeclampsia [76], and maternal hypertension [126]. Although several H2S precursors in response to various insults that have been studied displayed protection against hypertension, there remains a lack of data regarding other cardiovascular benefits.
5.2. H2S Donors
Inorganic sulfide salts such as sodium hydrosulfide (NaHS) and sodium sulfide (Na2S) are the most widely used H2S donors to evaluate the therapeutic potential of exogenous H2S [7,8]. NaHS has demonstrated protective effects against hypertension in various animal models, including NO-deficient rats [33], Dahl salt-sensitive rats [32], Ang II-infused mice [91], and SHR [148]. Likewise, Na2S has shown an antihypertensive effect in SHR [149].
Table 1 shows NaHS therapy between four and six weeks of age prevented hypertension in adult SHRs at 12 weeks of age [93]. In NaHS-treated SHR, NaHS-prevented hypertension coincided with increased H2S production and glutathione level [93]. These findings support the notion that H2S prodrug may function not only as a source of H2S but also as precursors of glutathione, a potent antioxidant in the body [10]. Another report showed that maternal NaHS therapy protects adult offspring against hypertension in a renovascular hypertension model [139]. Additionally, using the same model, maternal NaHS therapy benefits on cardiovascular outcome prevented sympathetic activation [140]. The beneficial effect of NaHS on BP may also be attributed to the reduced expression of angiotensin II type 1 receptor (AT1R)/ROS/inflammation pathway in the brain.
As we mentioned earlier, inorganic sulfide salts induce a rapid but short-lived increase of H2S to supraphysiological concentrations. Thus, several organic slow-releasing H2S donors have been synthesized to overcome this limitation [7,8]. Although GYY4137 showed a protective effect against hypertension in a CSE inhibition-induced preeclampsia model as well as a L-NAME-treated SHR model [150,151], none of the organic slow-releasing H2S donors have yet been tested in terms of their reprogramming effects on CVD of developmental origins. Furthermore, thiosulfate may serve as a unique H2S donor. Thiosulfate can produce H2S through a nonenzymatic pathway or by an enzymatic pathway via a glutathione-dependent reduction [152]. On the other hand, H2S can be enzymatically oxidized in mitochondria to thiosulfate. Owing to thiosulfate having therapeutic potential in hypertensive animal models [153,154], there is an ongoing need for additional study to elucidate its reprogramming effects in cardiovascular programming.
5.3. Organosulfur Compounds
Organosulfur compounds derived from garlic or onions have drawn attention as natural precursors of H2S. Garlic-derived organic polysulfides have proved beneficial for attenuating hypertension-related disorders [155,156]. One possible reason is because garlic-derived polysulfides can mediate NO pathway, resulting in NO-mediated vasodilation [157]. Garlic-derived compounds also provide protection in atherosclerosis, diabetes, myocardial infarction, and ischemic stroke [158]. Little information currently exists with regard to their cardiometabolic health benefits in CVD of developmental origins. So far, only one report from our group demonstrated that supplementing garlic oil in pregnancy and lactation prevented hypertension programmed by a high-fat diet, which is associated with increased expression and activity of H2S-producing enzymes in offspring kidneys and reshaping gut microbiota [128].
Natural and synthetic isothiocyanates are also known as H2S donors [159]. Natural isothiocyanates are found in cruciferous vegetables such as broccoli, rocket, cauliflower, etc., [159]. Due to their beneficial biological effects, natural isothiocyanates have been exploited for the design of new synthetic analogs [160]. Broccoli consumption is associated with reduced risk of ischemic reperfusion injury-mediated cardiomyocyte death [161]. Another study demonstrated that 4-carboxyphenyl isothiocyanate processed cardioprotective properties in the ex vivo and in vivo I/R models [161]. Nevertheless, it is currently difficult to link isothiocyanates with cardiovascular programming because of the lack of data on their reprogramming effects.
5.4. Others
Numerous commonly used medications have been reported to increase H2S concentrations, such as metformin, amlodipine, ramipril, carvediol, atorvastatin, digoxin, aspirin, paracetamol, testosterone, vitamin D, and 17β-estradiol [152]. So far very few studies have targeted their potential in reprogramming with a focus on CVD, despite significant progress achieved in recent years on pharmacotherapies in the field of H2S research. Since many available H2S-releasing drugs are still in preclinical experiments, it would be interesting to see whether targeting the H2S downstream signal-related mechanisms would appear to be a practical approach to prevent CVD of developmental origins from further clinical translation.
Moreover, abundant SRB in the gut produce significant amounts of H2S and sulfur compounds. However, scant data have been reported on the effects of gut-derived H2S on cardiovascular programming [161]. More research on gut SRB and their products is required as they may become a potential therapeutic target in CVD of developmental origins.
However, a concern raised by these studies is that some H2S-based interventions have other actions beyond supplementing H2S production. For example, l-cysteine and NAC have antioxidant effects through the glutathione pathway; however, to what extent their reprogramming effects on CVD can be attributed to H2S deserves further elucidation. A better understanding of the H2S-dependent and -independent mechanisms responsible for the protective effects of various H2S-based interventions on CVD of developmental origins is therefore warranted.
6. Conclusions and Perspectives
The evidence supporting the potential therapeutic role of H2S-based therapy in CVD of developmental origins is robust but incomplete. This review has provided a general overview on the various H2S-based interventions that shows cardiovascular benefits, including precursors of H2S, H2S donors, and organosulfur compounds.
It stands to reason that early-life H2S-based interventions are considered as potential reprogramming therapies for CVD of developmental origins. However, it is noteworthy that H2S at supraphysiologic concentrations are toxic. Although some H2S-releasing agents (e.g., SG1002) have shown to be safe and well tolerated in Phase I clinical trials [7], attention will need to be paid to increase efficiency and reduce toxicity, and to be able to accurately monitor levels of H2S in vivo. Currently, various methods have been established for endogenous H2S measurement. Nevertheless, these methods have obvious limitations, especially in the clinical setting [127]. Therefore, future work in developing ideal methodology is needed to better assess H2S measurements in clinical practice and ensure H2S-based therapy would only apply in the case of deficits.
Meanwhile, we are aware that a long road still lies ahead in determining the right dose of H2S-based intervention for the right person, at the right time, for clinical applications. Little reliable information currently exists regarding the reprogramming effects of H2S-releasing drugs in human trials. Much of the preclinical work investigating the cardiovascular reprogramming actions of H2S has mainly studied hypertension. Since children with chronic kidney disease are at high risk for future CVD and they develop hypertension at early stages of CKD [162], and that early H2S-based interventions can prevent the transition of prehypertension to hypertension [93,136], there will be a growing need to examine their reprogramming effects by targeting other animal models of programmed and this specific study population.
Another important aspect is that significant progress has been made over the last few decades in H2S-releasing drugs, while less attention has been paid to gut bacteria-derived H2S. Lacking in the literature is how microbiota-targeted therapies may alter SRB to produce gut-derived H2S and whether it is beneficial or harmful for cardiovascular health.
Cardiovascular programming, apart from the H2S signaling pathway, has been linked to other common molecular mechanisms. What is the exact manner of cross-talk between these pathways? Are early-life interventions targeting other mechanisms (e.g., AMPK activator or RAS blockers) also able to mediate the H2S pathway to prevent CVD of developmental origins?
Finally, H2S is a meaningfully pathogenetic link for the developmental origins of CVD. After all this tremendous growth in H2S-based interventions and greater understanding of cardiovascular programming, we expect that H2S-based reprogramming therapies will be applied in clinics to reduce the global burden of CVD.
Author Contributions
C.-N.H.: contributed to data interpretation, drafting of the manuscript, critical revision of the manuscript, concept generation, and approval of the article; Y.-L.T.: drafting of the manuscript, data interpretation, contributed to concept generation, critical revision of the manuscript and approval of the article. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Chang Gung Memorial Hospital, Kaohsiung, Taiwan, grants CMRPG8J0251, CMRPG8J0252, CMRPG8J0253, CMRPG8J0891, and CMRPG8J0892.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. Cardiovascular Diseases (CVDs). 2017. Available online: https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 27 December 2020).
- McGill, H.C., Jr.; McMahan, C.A.; Herderick, E.E.; Malcom, G.T.; Tracy, R.E.; Strong, J.P. Origin of atherosclerosis in child-hood and adolescence. Am. J. Clin. Nutr. 2000, 72, 1307S–1315S. [Google Scholar]
- Hanson, M. The birth and future health of DOHaD. J. Dev. Orig. Health Dis. 2015, 6, 434–437. [Google Scholar] [CrossRef]
- Thornburg, K.L. The programming of cardiovascular disease. J. Dev. Orig. Health Dis. 2015, 6, 366–376. [Google Scholar] [CrossRef]
- Blackmore, H.L.; Ozanne, S.E. Programming of cardiovascular disease across the life-course. J. Mol. Cell. Cardiol. 2015, 83, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Tain, Y.-L.; Hsu, C.-N. Interplay between Oxidative Stress and Nutrient Sensing Signaling in the Developmental Origins of Cardiovascular Disease. Int. J. Mol. Sci. 2017, 18, 841. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Polhemus, D.J.; Lefer, D.J. Evolution of Hydrogen Sulfide Therapeutics to Treat Cardiovascular Disease. Circ. Res. 2018, 123, 590–600. [Google Scholar] [CrossRef] [PubMed]
- Wen, Y.-D.; Wang, H.; Zhu, Y.Z. The Drug Developments of Hydrogen Sulfide on Cardiovascular Disease. Oxid. Med. Cell. Longev. 2018, 2018, 1–21. [Google Scholar] [CrossRef]
- Meng, G.-L.; Zhao, S.; Xie, L.; Han, Y.; Ji, Y. Protein S-sulfhydration by hydrogen sulfide in cardiovascular system. Br. J. Pharmacol. 2017, 175, 1146–1156. [Google Scholar] [CrossRef]
- Kimura, H. The physiological role of hydrogen sulfide and beyond. Nitric Oxide 2014, 41, 4–10. [Google Scholar] [CrossRef]
- Olas, B. Medical Functions of Hydrogen Sulfide. Adv. Appl. Microbiol. 2016, 74, 195–210. [Google Scholar] [CrossRef]
- Tain, Y.-L.; Joles, J.A. Reprogramming: A Preventive Strategy in Hypertension Focusing on the Kidney. Int. J. Mol. Sci. 2015, 17, 23. [Google Scholar] [CrossRef]
- Hsu, C.-N.; Tain, Y.-L. Hydrogen Sulfide in Hypertension and Kidney Disease of Developmental Origins. Int. J. Mol. Sci. 2018, 19, 1438. [Google Scholar] [CrossRef]
- Szabo, C. A timeline of hydrogen sulfide (H2S) research: From environmental toxin to biological mediator. Biochem. Pharmacol. 2018, 149, 5–19. [Google Scholar] [CrossRef] [PubMed]
- Kanagy, N.L.; Szabo, C.; Papapetropoulos, A. Vascular biology of hydrogen sulfide. Am. J. Physiol. Physiol. 2017, 312, C537–C549. [Google Scholar] [CrossRef] [PubMed]
- Peleli, M.; Bibli, S.-I.; Li, Z.; Chatzianastasiou, A.; Varela, A.; Katsouda, A.; Zukunft, S.; Bucci, M.; Vellecco, V.; Davos, C.H.; et al. Cardiovascular phenotype of mice lacking 3-mercaptopyruvate sulfurtransferase. Biochem. Pharmacol. 2020, 176, 113833. [Google Scholar] [CrossRef]
- Shibuya, N.; Kimura, H. Production of hydrogen sulfide from d-cysteine and its therapeutic potential. Front. Endocrinol. 2013, 4, 87. [Google Scholar] [CrossRef]
- Linden, D.R. Hydrogen Sulfide Signaling in the Gastrointestinal Tract. Antioxid. Redox Signal. 2014, 20, 818–830. [Google Scholar] [CrossRef] [PubMed]
- Blachier, F.; Davila, A.-M.; Mimoun, S.; Benetti, P.-H.; Atanasiu, C.; Andriamihaja, M.; Benamouzig, R.; Bouillaud, F.; Tomé, D. Luminal sulfide and large intestine mucosa: Friend or foe? Amino Acids 2009, 39, 335–347. [Google Scholar] [CrossRef]
- Yang, G.; Wu, L.; Jiang, B.; Yang, W.; Qi, J.; Cao, K.; Meng, Q.; Mustafa, A.K.; Mu, W.; Zhang, S.; et al. H2S as a physiologic vasorelaxant: Hypertension in mice with deletion of cystathionine gamma-lyase. Science 2008, 322, 587–590. [Google Scholar] [CrossRef]
- Mani, S.; Li, H.; Untereiner, A.; Wu, L.; Yang, G.; Austin, R.C.; Dickhout, J.G.; Lhoták, Š.; Meng, Q.H.; Wang, R. Decreased Endogenous Production of Hydrogen Sulfide Accelerates Atherosclerosis. Circulation 2013, 127, 2523–2534. [Google Scholar] [CrossRef] [PubMed]
- Dayal, S.; Bottiglieri, T.; Arning, E.; Maeda, N.; Malinow, M.R.; Sigmund, C.D.; Heistad, D.D.; Faraci, F.M.; Lentz, S.R. Endothelial dysfunction and elevation of S-adenosylhomocysteine in cystathionine beta-synthase-deficient mice. Circ. Res. 2001, 88, 1203–1209. [Google Scholar] [CrossRef] [PubMed]
- Dayal, S.; Arning, E.; Bottiglieri, T.; Böger, R.H.; Sigmund, C.D.; Faraci, F.M.; Lentz, S.R. Cerebral Vascular Dysfunction Mediated by Superoxide in Hyperhomocysteinemic Mice. Stroke 2004, 35, 1957–1962. [Google Scholar] [CrossRef]
- Sun, Y.; Yuan, Y.; Yan, H.; Wan, H.; Li, X.; Chen, S.; Li, H.; Tang, C.-S.; Du, J.; Liu, G.; et al. Plasma H 2 S predicts coronary artery lesions in children with Kawasaki disease. Pediatr. Int. 2015, 57, 840–844. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Wu, X.; Xu, Y.; Guizhen, A.; Yang, J.; Li, J.; Li, Y.; Ao, G.; Cheng, J.; Jiaying, Y. The cystathionine β-synthase/hydrogen sulfide pathway contributes to microglia-mediated neuroinflammation following cerebral ischemia. Brain, Behav. Immun. 2017, 66, 332–346. [Google Scholar] [CrossRef]
- Altaany, Z.; Moccia, F.; Munaron, L.; Mancardi, D.; Wang, R. Hydrogen sulfide and endothelial dysfunction: Relationship with nitric oxide. Curr. Med. Chem. 2014, 21, 3646–3661. [Google Scholar] [CrossRef]
- Zhao, W.; Zhang, J.; Lu, Y.; Wang, R. The vasorelaxant effect of H(2)S as a novel endogenous gaseous K(ATP) channel opener. EMBO J. 2001, 20, 6008–6016. [Google Scholar] [CrossRef]
- Hosoki, R.; Matsuki, N.; Kimura, H. The Possible Role of Hydrogen Sulfide as an Endogenous Smooth Muscle Relaxant in Synergy with Nitric Oxide. Biochem. Biophys. Res. Commun. 1997, 237, 527–531. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Ndisang, J.F.; Tang, G.; Cao, K.; Wang, R. Hydrogen sulfide-induced relaxation of resistance mesenteric artery beds of rats. Am. J. Physiol. Circ. Physiol. 2004, 287, H2316–H2323. [Google Scholar] [CrossRef] [PubMed]
- Yan, H.; Du, J.; Tang, C. The possible role of hydrogen sulfide on the pathogenesis of spontaneous hypertension in rats. Biochem. Biophys. Res. Commun. 2004, 313, 22–27. [Google Scholar] [CrossRef]
- Xiao, L.; Dong, J.-H.; Jing-Hui, D.; Xue, H.-M.; Guo, Q.; Teng, X.; Wu, Y.-M. Hydrogen Sulfide Improves Endothelial Dysfunction via Downregulating BMP4/COX-2 Pathway in Rats with Hypertension. Oxidative Med. Cell. Longev. 2016, 2016, 1–10. [Google Scholar] [CrossRef]
- Huang, P.; Chen, S.; Wang, Y.; Liu, J.; Yao, Q.; Huang, Y.; Li, H.; Zhu, M.; Wang, S.; Li, L.; et al. Down-regulated CBS/H2S pathway is involved in high-salt-induced hypertension in Dahl rats. Nitric Oxide 2015, 46, 192–203. [Google Scholar] [CrossRef] [PubMed]
- Zhong, G.; Chen, F.; Cheng, Y.; Tang, C.-S.; Du, J. The role of hydrogen sulfide generation in the pathogenesis of hypertension in rats induced by inhibition of nitric oxide synthase. J. Hypertens. 2003, 21, 1879–1885. [Google Scholar] [CrossRef] [PubMed]
- Van Goor, H.; Born, J.C.V.D.; Hillebrands, J.-L.; Joles, J.A. Hydrogen sulfide in hypertension. Curr. Opin. Nephrol. Hypertens. 2016, 25, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhao, X.; Jin, H.; Wei, H.; Li, W.; Bu, D.; Tang, X.; Ren, Y.; Tang, C.; Du, J. Role of Hydrogen Sulfide in the Development of Atherosclerotic Lesions in Apolipoprotein E Knockout Mice. Arter. Thromb. Vasc. Biol. 2009, 29, 173–179. [Google Scholar] [CrossRef]
- Durante, W. Hydrogen Sulfide Therapy in Diabetes-Accelerated Atherosclerosis: A Whiff of Success. Diabetes 2016, 65, 2832–2834. [Google Scholar] [CrossRef] [PubMed]
- Xie, L.; Gu, Y.; Wen, M.; Zhao, S.; Wang, W.; Ma, Y.; Meng, G.; Han, Y.; Wang, Y.; Liu, G.; et al. Hydrogen Sulfide Induces Keap1 S-sulfhydration and Suppresses Diabetes-Accelerated Atherosclerosis via Nrf2 Activation. Diabetes 2016, 65, 3171–3184. [Google Scholar] [CrossRef] [PubMed]
- Zhuo, Y.; Chen, P.F.; Zhang, A.Z.; Zhong, H.; Chen, C.Q.; Zhu, Y.Z. Cardioprotective effect of hydrogen sulfide in ischemic reperfusion experimental rats and its influence on expression of surviving gene. Biol. Pharm. Bull. 2009, 32, 1406–1410. [Google Scholar] [CrossRef]
- Calvert, J.W.; Jha, S.; Gundewar, S.; Elrod, J.W.; Ramachandran, A.; Pattillo, C.B.; Kevil, C.G.; Lefer, D.J. Hydrogen sulfide mediates cardioprotection through Nrf2 signaling. Circ. Res. 2009, 105, 365–374. [Google Scholar] [CrossRef]
- Stanner, S.A.; Yudkin, J.S. Fetal programming and the Leningrad Siege study. Twin Res. 2001, 4, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Hult, M.; Tornhammar, P.; Ueda, P.; Chima, C.; Bonamy, A.-K.E.; Ozumba, B.; Norman, M. Hypertension, Diabetes and Overweight: Looming Legacies of the Biafran Famine. PLoS ONE 2010, 5, e13582. [Google Scholar] [CrossRef] [PubMed]
- Dabelea, D.; Hanson, R.L.; Lindsay, R.S.; Pettitt, D.J.; Imperatore, G.; Gabir, M.M.; Roumain, J.; Bennett, P.H.; Knowler, W.C. Intrauterine exposure to diabetes conveys risks for type 2 diabetes and obesity: A study of discordant sibships. Diabetes 2000, 49, 2208–2211. [Google Scholar] [CrossRef] [PubMed]
- Oken, E.; Huh, S.Y.; Taveras, E.M.; Rich-Edwards, J.W.; Gillman, M.W. Associations of Maternal Prenatal Smoking with Child Adiposity and Blood Pressure. Obes. Res. 2005, 13, 2021–2028. [Google Scholar] [CrossRef]
- Vafeiadi, M.; Roumeliotaki, T.; Myridakis, A.; Chalkiadaki, G.; Fthenou, E.; Dermitzaki, E.; Karachaliou, M.; Sarri, K.; Vassilaki, M.; Stephanou, E.G.; et al. Association of early life exposure to bisphenol A with obesity and cardiometabolic traits in childhood. Environ. Res. 2016, 146, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Levine, R.S.; Hennekens, C.H.; Jesse, M.J. Blood pressure in prospective population based cohort of newborn and infant twins. BMJ 1994, 308, 298–302. [Google Scholar] [CrossRef] [PubMed]
- Vågerö, D.; Leon, D.A. Ischaemic heart disease and low birth weight: A test of the fetal-origins hypothesis from the Swedish Twin Registry. Lancet 1994, 343, 260–263. [Google Scholar] [CrossRef]
- Hrudey, E.J.; Reynolds, R.M.; Oostvogels, A.J.J.M.; Brouwerv, I.A.; Vrijkotte, T. The Association between Maternal 25-Hydroxyvitamin D Concentration during Gestation and Early Childhood Cardio-metabolic Outcomes: Is There Interaction with Pre-Pregnancy BMI? PLoS ONE 2015, 10, e0133313. [Google Scholar] [CrossRef] [PubMed]
- Fraser, A.; Nelson, S.M.; Macdonald-Wallis, C.; Sattar, N.; Lawlor, D. Hypertensive Disorders of Pregnancy and Cardiometabolic Health in Adolescent Offspring. Hypertension 2013, 62, 614–620. [Google Scholar] [CrossRef] [PubMed]
- Hosaka, M.; Asayama, K.; Staessen, J.A.; Ohkubo, T.; Hayashi, K.; Tatsuta, N.; Kurokawa, N.; Satoh, M.; Hashimoto, T.; Hirose, T.; et al. Breastfeeding leads to lower blood pressure in 7-year-old Japanese children: Tohoku Study of Child Development. Hypertens. Res. 2012, 36, 117–122. [Google Scholar] [CrossRef]
- Keijzer-Veen, M.G.; Finken, M.J.J.; Nauta, J.; Dekker, F.W.; Hille, E.T.; Frölich, M.; Wit, J.M.; Van Der Heijden, A. Is Blood Pressure Increased 19 Years After Intrauterine Growth Restriction and Preterm Birth? A Prospective Follow-up Study in the Netherlands. Pediatrics 2005, 116, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.; Margaritis, M.; Channon, K.M.; Antoniades, C. Evaluating Oxidative Stress in Human Cardiovascular Disease: Methodological Aspects and Considerations. Curr. Med. Chem. 2012, 19, 2504–2520. [Google Scholar] [CrossRef] [PubMed]
- Ho, E.; Galougahi, K.K.; Liu, C.-C.; Bhindi, R.; Figtree, G.A. Biological markers of oxidative stress: Applications to cardiovascular research and practice. Redox Biol. 2013, 1, 483–491. [Google Scholar] [CrossRef]
- Fearon, I.M.; Faux, S.P. Oxidative stress and cardiovascular disease: Novel tools give (free) radical insight. J. Mol. Cell. Cardiol. 2009, 47, 372–381. [Google Scholar] [CrossRef] [PubMed]
- Thompson, L.P.; Al-Hasan, Y. Impact of Oxidative Stress in Fetal Programming. J. Pregnancy 2012, 2012, 1–8. [Google Scholar] [CrossRef]
- Do, M.C.F.; Ponzio, B.F.; Gomes, G.N.; Gil, F.Z.; Tostes, R.; Carvalho, M.H.C.; Fortes, Z.B. Micronutrient prenatal supplementation prevents the development of hypertension and vascular endothelial damage induced by intrauterine malnutrition. Life Sci. 2009, 85, 327–333. [Google Scholar] [CrossRef]
- Tain, Y.-L.; Hsu, C.-N.; Lee, C.-T.; Lin, Y.-J.; Tsai, C.-C. N-Acetylcysteine Prevents Programmed Hypertension in Male Rat Offspring Born to Suramin-Treated Mothers. Biol. Reprod. 2016, 95, 8. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Zhao, Y.-C.; Liang, Y.; Lin, X.-H.; Tan, Y.-J.; Wu, D.-D.; Li, X.-Z.; Ye, B.-Z.; Kong, F.-Q.; Sheng, J.-Z.; et al. The impaired myocardial ischemic tolerance in adult offspring of diabetic pregnancy is restored by maternal melatonin treatment. J. Pineal Res. 2016, 61, 340–352. [Google Scholar] [CrossRef]
- Shirpoor, A.; Nemati, S.; Ansari, M.H.K.; Ilkhanizadeh, B. The protective effect of vitamin E against prenatal and early postnatal ethanol treatment-induced heart abnormality in rats: A 3-month follow-up study. Int. Immunopharmacol. 2015, 26, 72–79. [Google Scholar] [CrossRef]
- Resende, A.C.; Emiliano, A.F.; Cordeiro, V.S.; De Bem, G.F.; De Cavalho, L.C.; De Oliveira, P.R.B.; Neto, M.L.; Costa, C.A.; Boaventura, G.T.; De Moura, R.S. Grape skin extract protects against programmed changes in the adult rat offspring caused by maternal high-fat diet during lactation. J. Nutr. Biochem. 2013, 24, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Tai, I.-H.; Sheen, J.-M.; Lin, Y.-J.; Yu, H.-R.; Tiao, M.-M.; Chen, C.-C.; Huang, L.-T.; Tain, Y.-L. Maternal N-acetylcysteine therapy regulates hydrogen sulfide-generating pathway and prevents programmed hypertension in male offspring exposed to prenatal dexamethasone and postnatal high-fat diet. Nitric Oxide 2016, 53, 6–12. [Google Scholar] [CrossRef]
- Giussani, D.A.; Camm, E.J.; Niu, Y.; Richter, H.G.; Blanco, C.E.; Gottschalk, R.; Blake, E.Z.; Horder, K.A.; Thakor, A.S.; Hansell, J.A.; et al. Developmental Programming of Cardiovascular Dysfunction by Prenatal Hypoxia and Oxidative Stress. PLoS ONE 2012, 7, e31017. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.-N.; Tain, Y.-L. Early Origins of Hypertension: Should Prevention Start Before Birth Using Natural Antioxidants? Antioxidants 2020, 9, 1034. [Google Scholar] [CrossRef] [PubMed]
- Bonetti, P.O.; Lerman, L.O.; Lerman, A. Endothelial dysfunction: A marker of atherosclerotic risk. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 168–175. [Google Scholar] [CrossRef]
- Shaul, P.W. Endothelial nitric oxide synthase, caveolae and the development of atherosclerosis. J. Physiol. 2003, 547, 21–33. [Google Scholar] [CrossRef]
- Boger, R.H. The emerging role of asymmetric dimethylarginine as a novel cardiovascular risk factor. Cardiovasc. Res. 2003, 59, 824–833. [Google Scholar] [CrossRef]
- Tain, Y.-L.; Hsu, C.-N. Toxic Dimethylarginines: Asymmetric Dimethylarginine (ADMA) and Symmetric Dimethylarginine (SDMA). Toxins 2017, 9, 92. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Sim, A.S.; Wang, X.L.; Salonikas, C.; Naidoo, D.; Wilcken, D.E. Relations between plasma asymmetric dimethylarginine (ADMA) and risk factors for coronary disease. Atherosclerosis 2006, 184, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Gorenflo, M.; Zheng, C.; Werle, E.; Fiehn, W.; Ulmer, H.E. Plasma levels of asymmetrical dimethylarginine in patients with congenital heart disease and pulmonary hypertension. J. Cardiovasc. Pharmacol. 2001, 37, 489–492. [Google Scholar] [CrossRef] [PubMed]
- Fard, A.; Tuck, C.H.; Donis, J.A.; Sciacca, R.; Di Tullio, M.R.; Wu, H.D.; Bryant, T.A.; Chen, N.-T.; Torres-Tamayo, M.; Ramasamy, R.; et al. Acute elevations of plasma asymmetric dimethylarginine and impaired endothelial function in response to a high-fat meal in patients with type 2 diabetes. Arter. Thromb. Vasc. Biol. 2000, 20, 2039–2044. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.H.; Lee, S.C. Elevated levels of plasma homocyst(e)ine and asymmetric dimethylarginine in elderly patients with stroke. Atherosclerosis 2001, 158, 425–430. [Google Scholar] [CrossRef]
- Eid, H.M.; Arnesen, H.; Hjerkinn, E.M.; Lyberg, T.; Seljeflot, I. Relationship between obesity, smoking, and the endogenous nitric oxide synthase inhibitor, asymmetric dimethylarginine. Metabolism 2004, 53, 1574–1579. [Google Scholar] [CrossRef]
- Böger, R.H.; Bode-Böger, S.M.; Thiele, W.; Junker, W.; Alexander, K.; Frölich, J.C. Biochemical Evidence for Impaired Nitric Oxide Synthesis in Patients with Peripheral Arterial Occlusive Disease. Circulation 1997, 95, 2068–2074. [Google Scholar] [CrossRef]
- Hsu, C.-N.; Tain, Y.-L. Regulation of Nitric Oxide Production in the Developmental Programming of Hypertension and Kidney Disease. Int. J. Mol. Sci. 2019, 20, 681. [Google Scholar] [CrossRef] [PubMed]
- Tain, Y.L.; Lee, C.T.; Chan, J.Y.; Hsu, C.N. Maternal melatonin or N-acetylcysteine therapy regulates hydrogen sulfide-generating pathway and renal transcriptome to prevent prenatal N(G)-Nitro-L-argininemethyl ester (L-NAME)-induced fetal programming of hypertension in adult male offspring. Am. J. Obstet. Gynecol. 2016, 215, 636. [Google Scholar] [CrossRef]
- Abuiessa, S.A.; Wedn, A.M.; El-Gowilly, S.M.; Helmy, M.M.; El-Mas, M.M. Pre-eclamptic Fetal Programming Alters Neuroinflammatory and Cardiovascular Consequences of Endotoxemia in Sex-Specific Manners. J. Pharmacol. Exp. Ther. 2020, 373, 325–336. [Google Scholar] [CrossRef] [PubMed]
- Kristek, F.; Gerová, M. Hypotrophy of conduit artery walls of the offspring of nitric oxide-defective rats. Braz. J. Med Biol. Res. 2004, 37, 601–606. [Google Scholar] [CrossRef]
- Gerová, M.; Bernátová, I.; Török, J.; Juráni, M. Cardiovascular system of offsprings of hypertensive rats with defective nitric oxide production. Physiol. Res. 2002, 51, 465–474. [Google Scholar]
- Wu, D.; Hu, Q.; Zhu, D. An Update on Hydrogen Sulfide and Nitric Oxide Interactions in the Cardiovascular System. Oxidative Med. Cell. Longev. 2018, 2018, 1–16. [Google Scholar] [CrossRef]
- Predmore, B.L.; Julian, D.; Cardounel, A.J. Hydrogen Sulfide Increases Nitric Oxide Production from Endothelial Cells by an Akt-Dependent Mechanism. Front. Physiol. 2011, 2, 104. [Google Scholar] [CrossRef]
- Kida, M.; Sugiyama, T.; Yoshimoto, T.; Ogawa, Y. Hydrogen sulfide increases nitric oxide production with calcium-dependent activation of endothelial nitric oxide synthase in endothelial cells. Eur. J. Pharm. Sci. 2013, 48, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Bucci, M.; Papapetropoulos, A.; Vellecco, V.; Zhou, Z.; Pyriochou, A.; Roussos, C.; Roviezzo, F.; Brancaleone, V.; Cirino, G. Hydrogen Sulfide Is an Endogenous Inhibitor of Phosphodiesterase Activity. Arter. Thromb. Vasc. Biol. 2010, 30, 1998–2004. [Google Scholar] [CrossRef]
- Pardue, S.; Kolluru, G.K.; Shen, X.; Lewis, S.E.; Saffle, C.B.; Kelley, E.E.; Kevil, C.G. Hydrogen sulfide stimulates xanthine oxidoreductase conversion to nitrite reductase and formation of NO. Redox Biol. 2020, 34, 101447. [Google Scholar] [CrossRef]
- Forrester, S.J.; Booz, G.W.; Sigmund, C.D.; Coffman, T.M.; Kawai, T.; Rizzo, V.; Scalia, R.; Eguchi, S. Angiotensin II Signal Transduction: An Update on Mechanisms of Physiology and Pathophysiology. Physiol. Rev. 2018, 98, 1627–1738. [Google Scholar] [CrossRef] [PubMed]
- Bogdarina, I.; Welham, S.; King, P.J.; Burns, S.P.; Clark, A.J.L. Epigenetic Modification of the Renin-Angiotensin System in the Fetal Programming of Hypertension. Circ. Res. 2007, 100, 520–526. [Google Scholar] [CrossRef] [PubMed]
- Chappell, M.C.; Marshall, A.C.; Alzayadneh, E.M.; Shaltout, H.A.; Diz, D.I. Update on the Angiotensin Converting Enzyme 2-Angiotensin (1–7)-Mas Receptor Axis: Fetal Programing, Sex Differences, and Intracellular Pathways. Front. Endocrinol. 2014, 4, 201. [Google Scholar] [CrossRef] [PubMed]
- Kett, M.M.; Denton, K.M. Renal programming: Cause for concern? Am. J. Physiol. Integr. Comp. Physiol. 2011, 300, R791–R803. [Google Scholar] [CrossRef] [PubMed]
- Manning, J.; Vehaskari, V.M. Postnatal modulation of prenatally programmed hypertension by dietary Na and ACE inhibition. Am. J. Physiol. Integr. Comp. Physiol. 2005, 288, R80–R84. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.-N.; Wu, K.L.H.; Lee, W.-C.; Leu, S.; Chan, J.Y.-H.; Tain, Y.-L. Aliskiren Administration during Early Postnatal Life Sex-Specifically Alleviates Hypertension Programmed by Maternal High Fructose Consumption. Front. Physiol. 2016, 7, 299. [Google Scholar] [CrossRef] [PubMed]
- Al-Magableh, M.R.; Kemp-Harper, B.K.; Hart, J.L. Hydrogen sulfide treatment reduces blood pressure and oxidative stress in angiotensin II-induced hypertensive mice. Hypertens. Res. 2015, 38, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.; Liu, Y.-H.; Goh, H.S.; Wang, J.J.X.; Yong, Q.-C.; Wang, R.; Bian, J.-S. Hydrogen Sulfide Inhibits Plasma Renin Activity. J. Am. Soc. Nephrol. 2010, 21, 993–1002. [Google Scholar] [CrossRef] [PubMed]
- Tain, Y.-L.; Hsu, C.-N.; Lu, P.-C. Early short-term treatment with exogenous hydrogen sulfide postpones the transition from prehypertension to hypertension in spontaneously hypertensive rat. Clin. Exp. Hypertens. 2017, 40, 58–64. [Google Scholar] [CrossRef]
- Guo, Q.; Feng, X.; Xue, H.; Teng, X.; Jin, S.; Duan, X.; Xiao, L.; Wu, Y. Maternal Renovascular Hypertensive Rats Treatment With Hydrogen Sulfide Increased the Methylation of AT1b Gene in Offspring. Am. J. Hypertens. 2017, 30, 1220–1227. [Google Scholar] [CrossRef]
- Jansson, T.; Powell, T.L. Role of Placental Nutrient Sensing in Developmental Programming. Clin. Obstet. Gynecol. 2013, 56, 591–601. [Google Scholar] [CrossRef] [PubMed]
- Efeyan, A.; Comb, W.C.; Sabatini, D.M. Nutrient-sensing mechanisms and pathways. Nat. Cell Biol. 2015, 517, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Ajith, T.A.; Jayakumar, T.G. Peroxisome proliferator-activated receptors in cardiac energy metabolism and cardiovascular disease. Clin. Exp. Pharmacol. Physiol. 2016, 43, 649–658. [Google Scholar] [CrossRef]
- Daskalopoulos, E.P.; Dufeys, C.; Beauloye, C.; Bertrand, L.; Horman, S. AMPK in Cardiovascular Diseases. Exp. Suppl. 2016, 107, 179–201. [Google Scholar] [CrossRef] [PubMed]
- Tain, Y.-L.; Lin, Y.-J.; Sheen, J.-M.; Lin, I.-C.; Yu, H.-R.; Huang, L.-T.; Hsu, C.-N. Resveratrol prevents the combined maternal plus postweaning high-fat-diets-induced hypertension in male offspring. J. Nutr. Biochem. 2017, 48, 120–127. [Google Scholar] [CrossRef]
- Tain, Y.-L.; Lee, W.-C.; Wu, K.L.H.; Leu, S.; Chan, J.Y.H. Resveratrol Prevents the Development of Hypertension Programmed by Maternal Plus Post-Weaning High-Fructose Consumption through Modulation of Oxidative Stress, Nutrient-Sensing Signals, and Gut Microbiota. Mol. Nutr. Food Res. 2018, 62, e1800066. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.E.; Lin, Y.J.; Lin, I.C.; Yu, H.R.; Sheen, J.M.; Tsai, C.C.; Huang, L.T.; Tain, Y.L. Resveratrol prevents combined prenatal NG-nitro-L-arginine-methyl ester (L-NAME) treatment plus postnatal high-fat diet induced programmed hypertension in adult rat offspring: Interplay between nutrient-sensing signals, oxidative stress and gut microbiota. J. Nutr. Biochem. 2019, 70, 28–37. [Google Scholar] [CrossRef]
- Hsu, C.-N.; Lin, Y.-J.; Yu, H.-R.; Lin, I.-C.; Sheen, J.-M.; Huang, L.-T.; Tain, Y.-L. Protection of Male Rat Offspring against Hypertension Programmed by Prenatal Dexamethasone Administration and Postnatal High-Fat Diet with the Nrf2 Activator Dimethyl Fumarate during Pregnancy. Int. J. Mol. Sci. 2019, 20, 3957. [Google Scholar] [CrossRef] [PubMed]
- Tain, Y.-L.; Hsu, C.-N.; Chan, J.Y.H. PPARs Link Early Life Nutritional Insults to Later Programmed Hypertension and Metabolic Syndrome. Int. J. Mol. Sci. 2015, 17, 20. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Giordano, S.; Zhang, J. Autophagy, mitochondria and oxidative stress: Cross-talk and redox signalling. Biochem. J. 2011, 441, 523–540. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Chen, H.; Gao, J.; Liu, Y.; Li, J.; Wang, J. Molecular machinery and interplay of apoptosis and autophagy in coronary heart disease. J. Mol. Cell. Cardiol. 2019, 136, 27–41. [Google Scholar] [CrossRef]
- Sugden, M.C.; Caton, P.W.; Holness, M.J. PPAR control: It’s SIRTainly as easy as PGC. J. Endocrinol. 2010, 204, 93–104. [Google Scholar] [CrossRef]
- Pedro, J.M.B.-S.; Kroemer, G.; Galluzzi, L. Autophagy and Mitophagy in Cardiovascular Disease. Circ. Res. 2017, 120, 1812–1824. [Google Scholar] [CrossRef] [PubMed]
- Tain, Y.-L.; Hsu, C.-N. AMP-Activated Protein Kinase as a Reprogramming Strategy for Hypertension and Kidney Disease of Developmental Origin. Int. J. Mol. Sci. 2018, 19, 1744. [Google Scholar] [CrossRef]
- Wang, M.; Tang, W.; Zhu, Y.Z. An Update on AMPK in Hydrogen Sulfide Pharmacology. Front. Pharmacol. 2017, 8, 810. [Google Scholar] [CrossRef] [PubMed]
- Testai, L.; Citi, V.; Martelli, A.; Brogi, S.; Calderone, V. Role of hydrogen sulfide in cardiovascular ageing. Pharmacol. Res. 2020, 160, 105125. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.-D.; Yang, Y.-R.; Mu, X.-P.; Lin, G.; Wang, Y.-P.; Jin, S.; Chen, Y.; Wang, M.-J.; Zhu, Y.-Z. Hydrogen Sulfide Alleviates Acute Myocardial Ischemia Injury by Modulating Autophagy and Inflammation Response under Oxidative Stress. Oxidative Med. Cell. Longev. 2018, 2018, 1–17. [Google Scholar] [CrossRef]
- Liu, J.; Wu, J.; Sun, A.; Sun, Y.; Yu, X.; Liu, N.; Dong, S.; Yang, F.; Zhang, L.; Zhong, X.; et al. Hydrogen sulfide decreases high glucose/palmitate-induced autophagy in endothelial cells by the Nrf2-ROS-AMPK signaling pathway. Cell Biosci. 2016, 6, 33. [Google Scholar] [CrossRef]
- Das, A.; Huang, G.X.; Bonkowski, M.S.; Longchamp, A.; Li, C.; Schultz, M.B.; Kim, L.-J.; Osborne, B.; Joshi, S.; Lu, Y.; et al. Impairment of an Endothelial NAD+-H2S Signaling Network Is a Reversible Cause of Vascular Aging. Cell 2018, 173, 74–89. [Google Scholar] [CrossRef]
- Hu, M.Z.; Zhou, B.; Mao, H.Y.; Sheng, Q.; Du, B.; Chen, J.L.; Pang, Q.F.; Ji, Y. Exogenous Hydrogen Sulfide Postconditioning Protects Isolated Rat Hearts from Ischemia/Reperfusion Injury Through Sirt1/PGC-1α Signaling Pathway. Int. Heart J. 2016, 57, 477–482. [Google Scholar] [CrossRef]
- Zhou, W.; Cheng, Y.; Zhu, P.; Nasser, M.I.; Zhang, X.; Zhao, M.-Y. Implication of Gut Microbiota in Cardiovascular Diseases. Oxidative Med. Cell. Longev. 2020, 2020, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Chu, D.M.; Meyer, K.M.; Prince, A.L.; Aagaard, K.M. Impact of maternal nutrition in pregnancy and lactation on offspring gut microbial composition and function. Gut Microbes 2016, 7, 459–470. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Li, H. The Role of Gut Microbiota in Atherosclerosis and Hypertension. Front. Pharmacol. 2018, 9, 1082. [Google Scholar] [CrossRef] [PubMed]
- Khodor, S.A.; Reichert, B.; Shatat, I.F. The Microbiome and Blood Pressure: Can Microbes Regulate Our Blood Pressure? Front. Pediatr. 2017, 5, 138. [Google Scholar] [CrossRef]
- Tang, W.W.; Kitai, T.; Hazen, S.L. Gut Microbiota in Cardiovascular Health and Disease. Circ. Res. 2017, 120, 1183–1196. [Google Scholar] [CrossRef]
- Battson, M.L.; Lee, D.M.; Weir, T.L.; Gentile, C.L. The gut microbiota as a novel regulator of cardiovascular function and disease. J. Nutr. Biochem. 2018, 56, 1–15. [Google Scholar] [CrossRef]
- Tang, W.H.W.; Bäckhed, F.; Landmesser, U.; Hazen, S.L. Intestinal Microbiota in Cardiovascular Health and Disease. J. Am. Coll. Cardiol. 2019, 73, 2089–2105. [Google Scholar] [CrossRef]
- Hsu, C.-N.; Hou, C.; Chan, J.Y.H.; Lee, C.-T.; Tain, Y.-L. Hypertension Programmed by Perinatal High-Fat Diet: Effect of Maternal Gut Microbiota-Targeted Therapy. Nutrients 2019, 11, 2908. [Google Scholar] [CrossRef]
- Hsu, C.-N.; Lin, Y.-J.; Hou, C.-Y.; Tain, Y.-L. Maternal Administration of Probiotic or Prebiotic Prevents Male Adult Rat Offspring against Developmental Programming of Hypertension Induced by High Fructose Consumption in Pregnancy and Lactation. Nutrients 2018, 10, 1229. [Google Scholar] [CrossRef]
- Hsu, C.N.; Chang-Chien, G.P.; Lin, S.; Hou, C.Y.; Tain, Y.L. Targeting on Gut Microbial Metabolite Trimethylamine-N-Oxide and Short-Chain Fatty Acid to Prevent Maternal High-Fructose-Diet-Induced Developmental Programming of Hypertension in Adult Male Offspring. Mol. Nutr. Food Res. 2019, 63, e1900073. [Google Scholar] [CrossRef]
- Tomasova, L.; Dobrowolski, L.; Jurkowska, H.; Wróbel, M.; Huc, T.; Ondrias, K.; Ostaszewski, R.; Ufnal, M. Intracolonic hydrogen sulfide lowers blood pressure in rats. Nitric Oxide 2016, 60, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.-N.; Hou, C.-Y.; Chang-Chien, G.-P.; Lin, S.; Tain, Y.-L. Maternal N-Acetylcysteine Therapy Prevents Hypertension in Spontaneously Hypertensive Rat Offspring: Implications of Hydrogen Sulfide-Generating Pathway and Gut Microbiota. Antioxidants 2020, 9, 856. [Google Scholar] [CrossRef] [PubMed]
- Nagy, P.; Pálinkás, Z.; Nagy, A.; Budai, B.; Tóth, I.; Vasas, A. Chemical aspects of hydrogen sulfide measurements in physiological samples. Biochim. Biophys. Acta 2014, 1840, 876–891. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.N.; Hou, C.Y.; Chang-Chien, G.P.; Lin, S.; Tain, Y.L. Maternal garlic oil supplementation prevents high-fat diet-induced hypertension in adult rat offspring: Implications of h2s-generating pathway in the gut and kidneys. Mol. Nutr. Food Res. 2021, in press. [Google Scholar] [CrossRef]
- Yang, G.; Wu, L. Trend in H2S Biology and Medicine Research—A Bibliometric Analysis. Molecules 2017, 22, 2087. [Google Scholar] [CrossRef]
- Benavides, G.A.; Squadrito, G.L.; Mills, R.W.; Patel, H.D.; Isbell, T.S.; Patel, R.P.; Darley-Usmar, V.M.; Doeller, J.E.; Kraus, D.W. Hydrogen sulfide mediates the vasoactivity of garlic. Proc. Natl. Acad. Sci. USA 2007, 104, 17977–17982. [Google Scholar] [CrossRef] [PubMed]
- Rose, P.; Dymock, B.W.; Moore, P.K. GYY4137, a Novel Water-Soluble, H2S-Releasing Molecule. Methods Enzymol. 2015, 554, 143–167. [Google Scholar] [CrossRef] [PubMed]
- Donnarumma, E.; Rushing, A.M.; Boisvert, S.F.; Scarborough, A.L.; Polhemus, D.J.; Trivedi, R.K.; Lefer, D.J.; Goodchild, T.T. The novel H2S pro-drug, SG1002, preserves coronary artery vascular reactivity in the setting of critical limb ischemia in swine. Circulation 2016, 134, A19028. [Google Scholar]
- Roger, T.; Raynaud, F.; Bouillaud, F.; Ransy, C.; Simonet, S.; Crespo, C.; Bourguignon, M.-P.; Villeneuve, N.; Vilaine, J.-P.; Artaud, I.; et al. New Biologically Active Hydrogen Sulfide Donors. ChemBioChem 2013, 14, 2268–2271. [Google Scholar] [CrossRef]
- Kang, J.; Li, Z.; Organ, C.L.; Park, C.M.; Yang, C.T.; Pacheco, A.; Wang, D.; Lefer, D.J.; Xian, M. pH-controlled hydrogen sulfide release for myocardial ischemia-reperfusion injury. J. Am. Chem. Soc. 2016, 138, 6336–6339. [Google Scholar] [CrossRef]
- Zheng, Y.; Yueqin, Z.; Ji, K.; Pan, Z.; Chittavong, V.; Wang, B. Esterase-Sensitive Prodrugs with Tunable Release Rates and Direct Generation of Hydrogen Sulfide. Angew. Chem. Int. Ed. 2016, 55, 4514–4518. [Google Scholar] [CrossRef]
- Hsu, C.N.; Lin, Y.J.; Lu, P.C.; Tain, Y.L. Early supplementation of d-cysteine or l-cysteine prevents hypertension and kidney damage in spontaneously hypertensive rats exposed to high-salt intake. Mol. Nutr. Food Res. 2018, 62, 2. [Google Scholar] [CrossRef]
- Xiao, D.; Huang, X.; Li, Y.; Dasgupta, C.; Wang, L.; Zhang, L. Antenatal Antioxidant Prevents Nicotine-Mediated Hypertensive Response in Rat Adult Offspring1. Biol. Reprod. 2015, 93, 66. [Google Scholar] [CrossRef] [PubMed]
- Xiao, D.; Wang, L.; Huang, X.; Li, Y.; Dasgupta, C.; Zhang, L. Protective Effect of Antenatal Antioxidant on Nicotine-Induced Heart Ischemia-Sensitive Phenotype in Rat Offspring. PLoS ONE 2016, 11, e0150557. [Google Scholar] [CrossRef]
- Guo, Q.; Feng, X.; Xue, H.; Jin, S.; Teng, X.; Duan, X.; Xiao, L.; Wu, Y. Parental Renovascular Hypertension-Induced Autonomic Dysfunction in Male Offspring Is Improved by Prenatal or Postnatal Treatment With Hydrogen Sulfide. Front. Physiol. 2019, 10, 1184. [Google Scholar] [CrossRef]
- Feng, X.; Guo, Q.; Xue, H.; Duan, X.; Jin, S.; Wu, Y. Hydrogen Sulfide Attenuated Angiotensin II-Induced Sympathetic Excitation in Offspring of Renovascular Hypertensive Rats. Front. Pharmacol. 2020, 11, 565726. [Google Scholar] [CrossRef] [PubMed]
- Rybka, J.; Kedziora-Kornatowska, K.; Kozakiewicz, M.; Zary-Sikorska, E.; Pawluk, H.; Pawliszak, W.; Kedziora, J. Role of glutathione metabolism and glutathione-related antioxidant defense systems in hypertension. J. Physiol. Pharmacol. Off. J. Pol. Physiol. Soc. 2016, 67, 331–337. [Google Scholar]
- Vasdev, S.; Singal, P.; Gill, V. The antihypertensive effect of cysteine. Int. J. Angiol. 2009, 18, 07–21. [Google Scholar] [CrossRef] [PubMed]
- Khaledifar, A.; Mobasheri, M.; Kheiri, S.; Zamani, Z. Comparison of N-acetylcysteine and angiotensin converting enzyme inhibitors in blood pressure regulation in hypertensive patients. ARYA Atheroscler. 2015, 11, 5–13. [Google Scholar]
- Dludla, P.V.; Dias, S.C.; Obonye, N.; Johnson, R.; Louw, J.; Nkambule, B.B. A Systematic Review on the Protective Effect of N-Acetyl Cysteine Against Diabetes-Associated Cardiovascular Complications. Am. J. Cardiovasc. Drugs 2018, 18, 283–298. [Google Scholar] [CrossRef] [PubMed]
- Friedman, M.; Levin, C.E. Nutritional and medicinal aspects of d-amino acids. Amino Acids 2011, 42, 1553–1582. [Google Scholar] [CrossRef]
- Shibuya, N.; Koike, S.; Tanaka, M.; Ishigami-Yuasa, M.; Kimura, Y.; Ogasawara, Y.; Fukui, K.; Nagahara, N.; Kimura, H. A novel pathway for the production of hydrogen sulfide from d-cysteine in mammalian cells. Nat. Commun. 2013, 4, 1366. [Google Scholar] [CrossRef] [PubMed]
- Fan, N.-C.; Tsai, C.-M.; Hsu, C.-N.; Huang, L.-T.; Tain, Y.-L. N-Acetylcysteine Prevents Hypertension via Regulation of the ADMA-DDAH Pathway in Young Spontaneously Hypertensive Rats. BioMed Res. Int. 2013, 2013, 1–9. [Google Scholar] [CrossRef]
- Ahmad, F.U.D.; Sattar, M.A.; Rathore, H.A.; Tan, Y.C.; Akhtar, S.; Jin, O.H.; Pei, Y.P.; Abdullah, N.A.; Johns, E.J. Hydrogen sulphide and tempol treatments improve the blood pressure and renal excretory responses in spontaneously hypertensive rats. Ren. Fail. 2014, 36, 598–605. [Google Scholar] [CrossRef]
- Tomasova, L.; Drapala, A.; Jurkowska, H.; Wróbel, M.; Ufnal, M. Na 2 S, a fast-releasing H 2 S donor, given as suppository lowers blood pressure in rats. Pharmacol. Rep. 2017, 69, 971–977. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Ahmad, S.; Cai, M.; Rennie, J.; Fujisawa, T.; Crispi, F.; Baily, J.; Miller, M.R.; Cudmore, M.; Hadoke, P.W.F.; et al. Dysregulation of Hydrogen Sulfide Producing Enzyme Cystathionine γ-lyase Contributes to Maternal Hypertension and Placental Abnormalities in Preeclampsia. Circulation 2013, 127, 2514–2522. [Google Scholar] [CrossRef] [PubMed]
- Sharma, D.K.; Manral, A.; Saini, V.; Singh, A.; Srinivasan, B.; Tiwari, M. Novel diallyldisulfide analogs ameliorate cardiovascular remodeling in rats with L-NAME-induced hypertension. Eur. J. Pharmacol. 2012, 691, 198–208. [Google Scholar] [CrossRef]
- Bełtowski, J. Hydrogen sulfide in pharmacology and medicine—An update. Pharmacol. Rep. 2015, 67, 647–658. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, I.T.; Klooster, A.; Minnion, M.; Feelisch, M.; Verhaar, M.C.; Van Goor, H.; Joles, J.A. Sodium thiosulfate improves renal function and oxygenation in L-NNA–induced hypertension in rats. Kidney Int. 2020, 98, 366–377. [Google Scholar] [CrossRef] [PubMed]
- Snijder, P.M.; Frenay, A.-R.S.; Koning, A.M.; Bachtler, M.; Pasch, A.; Kwakernaak, A.J.; Berg, E.V.D.; Bos, E.M.; Hillebrands, J.-L.; Navis, G.; et al. Sodium thiosulfate attenuates angiotensin II-induced hypertension, proteinuria and renal damage11These authors contributed equally to this manuscript. Nitric Oxide 2014, 42, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Shouk, R.; Abdou, A.; Shetty, K.; Sarkar, D.; Eid, A.H. Mechanisms underlying the antihypertensive effects of garlic bioactives. Nutr. Res. 2014, 34, 106–115. [Google Scholar] [CrossRef]
- Ried, K.; Fakler, P. Potential of garlic (Allium sativum) in lowering high blood pressure: Mechanisms of action and clinical relevance. Integr. Blood Press. Control. 2014, 7, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Şener, G.; Sakarcan, A.; Yeǧen, B.Ç. Role of garlic in the prevention of ischemia-reperfusion injury. Mol. Nutr. Food Res. 2007, 51, 1345–1352. [Google Scholar] [CrossRef]
- Zhu, Y.; Anand, R.; Geng, X.; Ding, Y. A mini review: Garlic extract and vascular diseases. Neurol. Res. 2018, 40, 421–425. [Google Scholar] [CrossRef] [PubMed]
- Martelli, A.; Citi, V.; Testai, L.; Brogi, S.; Calderone, V. Organic Isothiocyanates as Hydrogen Sulfide Donors. Antioxid. Redox Signal. 2020, 32, 110–144. [Google Scholar] [CrossRef] [PubMed]
- Milelli, A.; Fimognari, C.; Ticchi, N.; Neviani, P.; Minarini, A.; Tumiatti, V. Isothiocyanate synthetic analogs: Biological activities, structure-activity relationships and synthetic strategies. Mini-Reviews Med. Chem. 2014, 14, 963–977. [Google Scholar] [CrossRef] [PubMed]
- Owis, A.I. Broccoli; the green beauty: A review. J. Pharm. Sci. Res. 2015, 7, 696703. [Google Scholar]
- Testai, L.; Marino, A.; Tomita, K.; Citi, V.; Martelli, A.; Breschi, M.; Levi, R.; Calderone, V. 4-Carboxyphenyl isothiocyanate (4-CPI), a novel hydrogen sulfide-donor endowed with cardioprotective property. Nitric Oxide 2015, 47, S31. [Google Scholar] [CrossRef]
- Tomasova, L.; Konopelski, P.; Ufnal, M. Gut Bacteria and Hydrogen Sulfide: The New Old Players in Circulatory System Homeostasis. Molecules 2016, 21, 1558. [Google Scholar] [CrossRef]
- Weaver, D.J.; Mitsnefes, M. Cardiovascular Disease in Children and Adolescents with Chronic Kidney Disease. Semin. Nephrol. 2018, 38, 559–569. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).