Effectiveness of Therapeutic Exercise in Physiotherapy with Blood Flow Restriction in Patients with Knee Pathologies: A Systematic Review
Abstract
1. Introduction
- -
- The stimulus must be individualized, considering the pressure applied according to the characteristics of the subject, the circumference of the limb and the cuff.
- -
- The BFR produces its greatest benefits in terms of muscle development when combined with light loads. Improvements are also observed using only flow restriction during immobilizations or combined with low-intensity aerobic exercise.
- -
- In healthy individuals, the effects of training are maximized if BFR is combined with traditional training with high loads.
1.1. Physiological Effects of Blood Flow Restriction Training
1.1.1. Physiological Mechanisms of Flow Restriction Training
1.1.2. Neuromuscular Responses to Flow Restriction Training
1.1.3. Metabolic Responses to Blood Flow Restriction Training
1.1.4. Hemodynamic Responses to Blood Flow Restriction Training
1.1.5. Endocrine Responses to Blood Flow Restriction Training
1.2. Use of BFR in Knee Pathologies
2. Materials and Methods
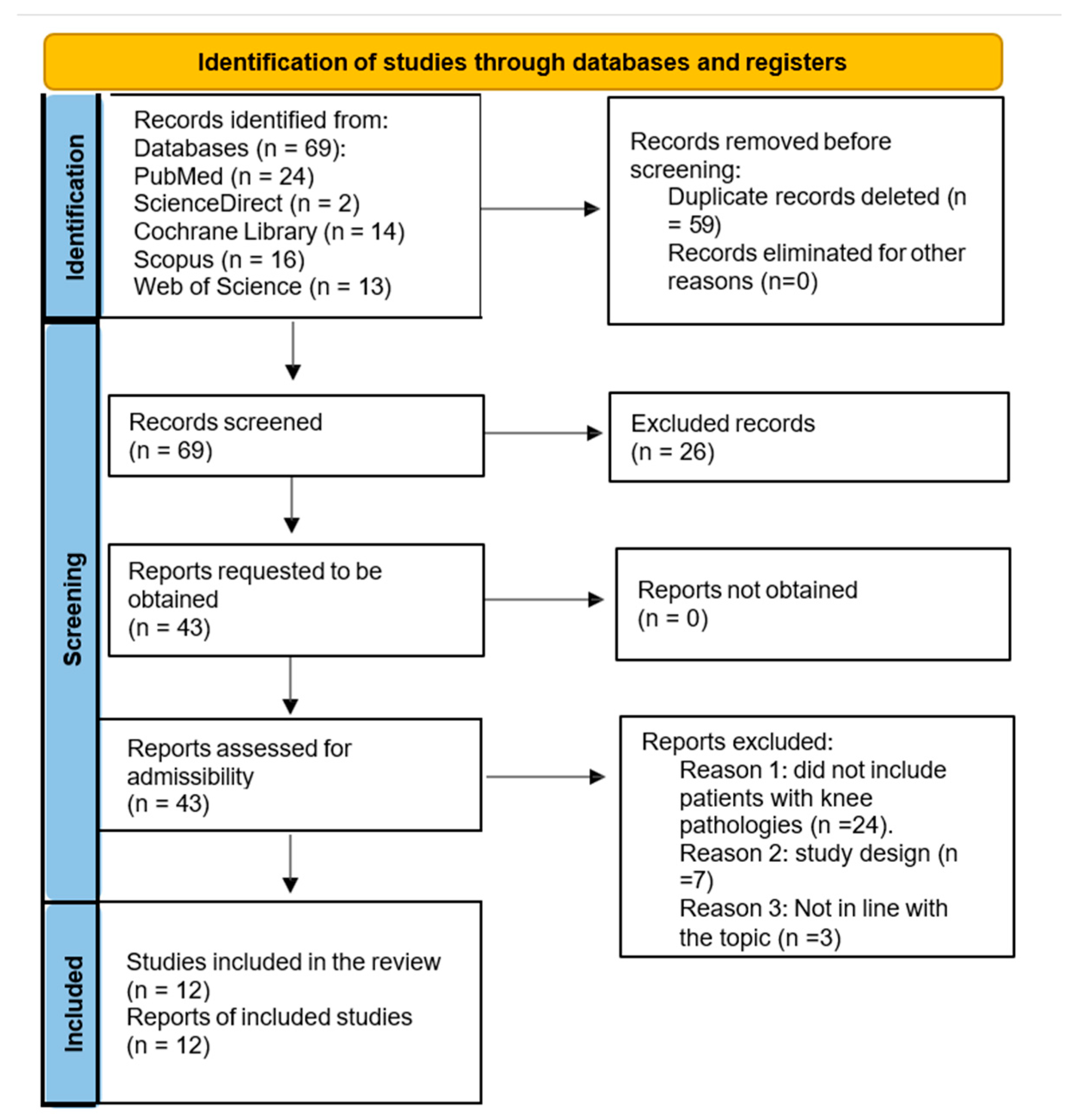
2.1. Search Criteria
2.2. Criteria for Selection
2.3. Search Strategy
2.4. Evaluation of the Methodological Quality
3. Results
3.1. Methodological Quality Assessment
3.2. Description of Studies and Synthesis of Results
3.3. Participant Characteristics
3.4. Main Measurement Variables
3.5. Type and Time of Training
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BFR | Blood Flow Restriction |
| OCT | Occlusive Training |
| GH | Growth Hormone |
| mTOR | Mammalian Target of Rapamycin |
| HSP-72 | Heat Shock Protein |
| NE | Norepinephrine |
| NO | Nitric Oxide |
| IGF-1 | Growth Factor-1 |
| VEGF | Endothelial Growth Factor |
| ACL | Anterior Cruciate Ligament |
| OA | Osteoarthritis |
| RA | Rheumatoid Arthritis |
| PICO | Patient, Intervention, Comparison, Outcomes |
| PRISMA | Preferred Reporting Items for Systematic Review and Meta-Analysis |
| MESH | Medical Subject Headings |
| Rob2 | Risk of Bias tool |
| CEBM | The Oxford Centre for Evidence-Based Medicine |
References
- Sato, Y. The history and future of KAATSU Training. Int. J. Kaatsu Train. Res. 2005, 1, 1–5. [Google Scholar] [CrossRef]
- Bowman, E.N.; Elshaar, R.; Milligan, H.; Jue, G.; Mohr, K.; Brown, P.; Watanabe, D.M.; Limpisvasti, O. Upper-extremity blood flow restriction: The proximal, distal, and contralateral effects—A randomized controlled trial. J. Shoulder Elb. Surg. 2020, 29, 1267–1274. [Google Scholar] [CrossRef] [PubMed]
- Scott, B.R.; Loenneke, J.P.; Slattery, K.M.; Dascombe, B.J. Exercise with blood flow restriction: An updated evidence-based approach for enhanced muscular development. Sports Med. 2015, 45, 313–325. [Google Scholar] [CrossRef]
- Martínez González, D. Aplicación del Entrenamiento Oclusivo como Prevención y Tratamiento de Lesiones. Universidad de Valladolid. 2017. Available online: https://uvadoc.uva.es/handle/10324/23224 (accessed on 22 March 2025).
- Pope, Z.K.; Willardson, J.M.; Schoenfeld, B.J. Exercise and blood flow restriction. J. Strength Cond. Res. 2013, 27, 2914–2926. [Google Scholar] [CrossRef]
- Brandner, C.R.; Warmington, S.A.; Kidgell, D.J. Corticomotor excitability is increased following an acute bout of blood flow restriction resistance exercise. Front. Hum. Neurosci. 2015, 9, 652. [Google Scholar] [CrossRef]
- Neto, G.R.; Novaes, J.S.; Dias, I.; Brown, A.; Vianna, J.; Cirilo-Sousa, M.S. Effects of resistance training with blood flow restriction on haemodynamics: A systematic review. Clin. Physiol. Funct. Imaging 2017, 37, 567–574. [Google Scholar] [CrossRef]
- Park, S.-Y.; Kwak, Y.S.; Harveson, A.; Weavil, J.C.; Seo, K.E. Low intensity resistance exercise training with blood flow restriction: Insight into cardiovascular function, and skeletal muscle hypertrophy in humans. Korean J. Physiol. Pharmacol. 2015, 19, 191–196. [Google Scholar] [CrossRef]
- Staron, R.S.; Malicky, E.S.; Leonardi, M.J.; Falkel, J.E.; Hagerman, F.C.; Dudley, G.A. Muscle hypertrophy and fast fiber type conversions in heavy resistance-trained women. Europ. J. Appl. Physiol. 1990, 60, 71–79. [Google Scholar] [CrossRef]
- Plotkin, D.L.; Roberts, M.D.; Haun, C.T.; Schoenfeld, B.J. Muscle Fiber Type Transitions with Exercise Training: Shifting Perspectives. Sports 2021, 9, 127. [Google Scholar] [CrossRef]
- Henning, F.; Kohn, T.A. Preservation of shortening velocity and power output in single muscle fibres from patients with idiopathic inflammatory myopathies. J. Muscle Res. Cell Motil. 2023, 44, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Panesso, M.C.; Trillos, M.C.; Guzmán, I.T. Biomecánica Clínica de la Rodilla; Editorial Universidad del Rosario: Bogotá, Colombia, 2009. [Google Scholar] [CrossRef]
- George, M.S.; Dunn, W.R.; Spindler, K.P. Current Concepts Review: Revision Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2006, 34, 2026–2037. [Google Scholar] [CrossRef] [PubMed]
- Márquez Arabia, J.J.; Márquez Arabia, W.H. Lesiones del ligamento cruzado anterior de la rodilla. Iatreia 2009, 22, 256–271. [Google Scholar] [CrossRef]
- Ranalletta, A.; Ranalletta, M.; Rossi, W.; Vieta, R.D.; Paoletta, R.E.; Hamilton, P.G. Ligamento cruzado posterior. Anatomía aplicada a la técnica quirúrgica. Artroscopia 2011, 18, 60–64. [Google Scholar]
- Ayala-Mejías, J.D.; García-Estrada, G.A.; Pérez-España, A. Lesiones del ligamento cruzado anterior. Acta Ortopédica Mex. 2014, 28, 57–67. [Google Scholar]
- Sánchez-Alepuz, E.; Miranda, I.; Miranda, F.J. Evaluación funcional de los pacientes con rotura del ligamento cruzado anterior. Estudio analítico transversal. Rev. Española Cir. Ortop. Traumatol. 2020, 64, 99–107. [Google Scholar] [CrossRef]
- Fineberg, M.S.; Zarins, B.; Sherman, O.H. Practical considerations in anterior cruciate ligament replacement surgery. J. Arthrosc. 2020, 16, 715–724. [Google Scholar] [CrossRef]
- Mayoral Rojals, V. Epidemiología, repercusión clínica y objetivos terapéuticos. Rev. Soc. Esp. Dolor 2021, 28, 4–10. [Google Scholar] [CrossRef]
- Spain, V.V. La Artrosis se Convertirá en la Cuarta Causa de Discapacidad en el Mundo en 2020, Según la OMS. 2013. Available online: https://www.vademecum.es/noticia-131011-la+artrosis+se+convertir+aacute++en+la+cuarta+causa+de+discapacidad+en+el+mundo+en+2020%2C+seg+uacute+n+la+oms_7506 (accessed on 19 December 2024).
- Tornero Crespo, M.M.; Montero Matamala, A. Review of the pharmacological treatment of osteoarthritis pain with paracetamol, nonsteroid anti-inflammatory (NSAIDSS) and selective cyclooxygenase-2 inhibitors (COXIB). Rev. Soc. Española Dolor 2021, 28, 43–48. [Google Scholar] [CrossRef]
- Fernández, G.A. Fisioterapia y Artrosis de Rodilla. RCA Grupo Editor. 2023, Volume 6. Available online: https://www.npunto.es/revista/64/fisioterapia-y-artrosis-de-rodilla (accessed on 1 April 2025).
- McInnes, I.B.; Schett, G. The pathogenesis of rheumatoid arthritis. N. Engl. J. Med. 2011, 365, 2205–2219. [Google Scholar] [CrossRef] [PubMed]
- Turrión Nieves, A.; Martín Holguera, R.; Pérez Gómez, A.; Álvarez De Mon-Soto, M. Artritis reumatoide. Med. Programa Form. Méd. Contin. Acreditado 2017, 12, 1615–1625. [Google Scholar] [CrossRef]
- Tornero Molina, J.; Sanmartí Sala, R.; Rodríguez Valverde, V.; Martín Mola, E.; Marenco De La Fuente, J.L.; González Álvaro, I.; Muñoz Fernández, S.; Gómez-Reino Carnota, J.; Carreño Pérez, L.; Batlle Gualda, E.; et al. Actualización del Documento de Consenso de la Sociedad Española de Reumatología sobre el uso de terapias biológicas en la artritis reumatoide. Reum. Clin. 2010, 6, 23–36. [Google Scholar] [CrossRef]
- Butt, J.; Ahmed, Z. Blood Flow Restriction Training and Its Use in Rehabilitation After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 6265. [Google Scholar] [CrossRef] [PubMed]
- Xie, S.Y.; Jiang, X.; Yuan, J.B.; Luo, J.; Song, S.; Hu, H.Y. Mechanisms of blood flow restriction training for knee pain: A mini review. Front. Physiol. 2025, 16, 1542322. [Google Scholar] [CrossRef]
- Ma, F.; He, J.; Wang, Y. Blood flow restriction combined with resistance training on muscle strength and thickness improvement in young adults: A systematic review, meta-analysis, and meta-regression. Front. Physiol. 2024, 15, 1379605. [Google Scholar] [CrossRef]
- Kwon, S.; Bae, K.C.; Yon, C.J.; Kim, D.H. Current Narrative Review-Application of Blood Flow Restriction Exercise in Clinical Knee Problems. Medicina 2025, 61, 1377. [Google Scholar] [CrossRef]
- Martínez Díaz, J.D.; Ortega Chacón, V.; Muñoz Ronda, F.J. El Diseño de Preguntas Clínicas en la Práctica Basada en la Evidencia: Modelos de Formulación. Enferm. Global. 2016, 15, 431–438. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef]
- Letts, L.; Wilkins, S.; Law, M.; Stewart, D.; Bosch, J.; Westmorland, M. Guidelines for Critical Review Form—Qualitative Studies (Version 2.0), Mcmaster University Occupational Therapy Evidence-Based Practice Research Group. 2007. Available online: https://www.semanticscholar.org/paper/Guidelines-for-critical-review-form-Qualitative-Letts-Wilkins/74513fac0424cd8210f9fc9577d3e9bc721bd06c (accessed on 21 December 2024).
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Mella Sousa, M.; Zamora Navas, P.; Mella Laborde, M.; Ballester Alfaro, J.J.; Uceda Carrascosa, P.; Mella Sousa, M.; Zamora Navas, P.; Mella Laborde, M.; Ballester Alfaro, J.J.; Uceda Carrascosa, P. Niveles de Evidencia Clínica y Grados de Recomendación. Rev. Soc. Andal. Traumatol. Ortop. 2012, 29, 59–72. [Google Scholar]
- Segal, N.A.; Williams, G.N.; Davis, M.C.; Wallace, R.B.; Mikesky, A.E. Efficacy of blood flow–restricted, low-load resistance training in women with risk factors for symptomatic knee osteoarthritis. PM&R 2015, 7, 376–384. [Google Scholar] [CrossRef]
- Jønsson, A.; Johansen, C.; Rolving, N.; Pfeiffer-Jensen, M. Feasibility and estimated efficacy of blood flow restricted training in female patients with rheumatoid arthritis: A randomized controlled pilot study. Scand. J. Rheumatol. 2021, 50, 169–177. [Google Scholar] [CrossRef]
- Jørgensen, S.L.; Bohn, M.B.; Aagaard, P.; Mechlenburg, I. Efficacy of low-load blood flow restricted resistance EXercise in patients with Knee osteoarthritis scheduled for total knee replacement (Exknee): Protocol for a multicentre randomised controlled trial. BMJ Open. 2020, 10, e034376. [Google Scholar] [CrossRef]
- Jørgensen, S.L.; Mechlenburg, I. Effects of low-load blood-flow restricted resistance training on functional capacity and patient-reported outcome in a young male suffering from reactive arthritis. Front. Sports Act. Living 2021, 3, 798902. [Google Scholar] [CrossRef]
- Curran, M.; Bedi, A.; Mendias, C.; Wojtys, E.M.; Kujawa, M.; Palmieri-Smith, R. Blood flow restriction training does not improve quadriceps strength after anterior cruciate ligament reconstruction. Orthop. J. Sports Med. 2019, 7 (Suppl. S5), 2325967119S00293. [Google Scholar] [CrossRef]
- Petersson, N.; Langgård Jørgensen, S.; Kjeldsen, T.; Mechlenburg, I.; Aagaard, P. Blood flow restricted walking in elderly individuals with knee osteoarthritis: A feasibility study. J. Rehabil. Med. 2022, 54, jrm00282. [Google Scholar] [CrossRef] [PubMed]
- Kacin, A.; Drobnič, M.; Marš, T.; Miš, K.; Petrič, M.; Weber, D.; Tomc Žargi, T.; Martinčič, D.; Pirkmajer, S. Functional and molecular adaptations of quadriceps and hamstring muscles to blood flow restricted training in patients with ACL rupture. Scand. J. Med. Sci. Sports 2021, 31, 1636–1646. [Google Scholar] [CrossRef]
- Jacobs, E.; Stroobant, L.; Victor, J.; Elewaut, D.; Tampere, T.; Wallaert, S.; Witvrouw, E.; Schuermans, J.; Wezenbeek, E. Vascular occlusion for optimising the functional improvement in patients with knee osteoarthritis: A randomised controlled trial. Ann. Rheum. Dis. 2025, 84, 341–350. [Google Scholar] [CrossRef] [PubMed]
- Johannsen, M.D. Effects of Blood-flow Restricted Exercise Compared to Standard Rehabilitation in Patients with Knee Osteoarthritis. ClinicalTrials.gov ID NCT05437770. Ins. Sports Med. 2025, 35, e70069. [Google Scholar]
- Gopinatth, V.; Garcia, J.R.; Reid, I.K.; Knapik, D.M.; Verma, N.N.; Chahla, J. Blood Flow Restriction Enhances Recovery After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Arthroscopy 2025, 41, 1048–1060. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Rothrauff, B.; Chen, L.; Jin, S.; He, S.; He, J. Comparison of blood flow restriction training rehabilitation and general rehabilitation exerciseafter anterior cruciate ligament reconstruction: A meta-analysis of randomized controlled trials. Knee Surg Sports Traumatol Arthrosc. 2025, 33, 2713–2728. [Google Scholar] [CrossRef]
- He, J.; Zhang, L.; Wu, Q.; Zhang, J. Credibility of Blood Flow Restriction Training in Patients with Knee Osteoarthritis: A Meta-analysis. Orthop. J. Sports Med. 2025, 13, 23259671241300145. [Google Scholar] [CrossRef] [PubMed]
- Zeitlin, C.; Shepherd, M.; Lack, S.; Neal, B. Blood Flow Restriction Training Compared to Conventional Training in People with Knee Pain: A Systematic Review with Meta-analysis. Phys. Ther. Sport. 2025, 74, 65–74. [Google Scholar] [CrossRef] [PubMed]
| Patient | Patients with Knee Pathologies |
|---|---|
| Intervention | Blood flow restriction training |
| Comparison | Blood flow restriction training vs. conventional physiotherapy |
| Outcomes, results | How effective blood flow restriction is in knee patients |
| Title | Author(s) | Year | Type of Study |
|---|---|---|---|
| “Efficacy of Blood Flow Restricted Low-Load Resistance Training in Women with Risk Factors for Symptomatic Knee Osteoarthritis”. | Segall et al. [35] | 2015 | Double-blind, randomized, controlled clinical trial. |
| “Feasibility and estimated efficacy of blood flow restricted training in female patients with rheumatoid arthritis: a randomized controlled pilot study “ | Jønsson et al. [36] | 2021 | Non-blinded, randomized, controlled pilot trial |
| “Efficacy of low-load blood flow restricted resistance EXercise in patients with Knee osteoarthritis scheduled for total knee replacement (EXKnee): protocol for a multicentre randomised controlled trial”. | Jørgensen et al. [37] | 2020 | Controlled, multicenter (two sites), randomized, assessor-blinded trial. |
| “Effects of Low-Load Blood- Flow Restricted Resistance Training on Functional Capacity and Patient- Reported Outcome in a Young Male Suffering From Reactive Arthritis”. | Jørgensen and Mechlenbur [38] | 2021 | Case study |
| “Blood Flow Restriction Training Does Not Improve Quadriceps Strength After Anterior Cruciate Ligament Reconstruction”. | Curran et al. [39] | 2019 | Randomized, controlled trial |
| “Blood flow restricted walking in elderly individuals with knee osteoarthritis: a feasibility study” | Petersson et al. [40] | 2022 | Feasibility study |
| “Functional and molecular adaptations of quadriceps and hamstring muscles to blood flow restricted training in patients with ACL rupture”. | Kacín et al. [41] | 2021 | Prospective, single-center, single-blind, quasi-randomized, controlled trial. |
| “Vascular Occlusion for Optimizing Functional Improvement in Patients With Knee Osteoarthritis (VOFIKO)”. | Jacobs et al. [42] | 2025 | Randomized clinical trial |
| “Effects of Blood-flow Restricted Exercise Compared to Standard Rehabilitation in Patients With Knee Osteoarthritis”. | Johannsen, M.D. [43] | 2022 | Randomized clinical trial |
| Items to be Assessed | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | Total Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author(s) | ||||||||||||||||
| Segal et al. [35] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 12/15 |
| Jønsson et al. [36] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 11/15 |
| Jørgensen et al. [37] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 11/15 |
| Jørgensen and Mechlenbur [38] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 10/15 |
| Curran et al. [39] | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 7/15 |
| Petersson et al. [40] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 13/15 |
| Kacín et al. [41] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 12/15 |
| Jacobs et al. [42] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8/15 |
| Johannsen [43] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8/15 |
| Article | Bias due to Randomization Process | Bias due to Deviations from Intended Interventions | Bias in Measurement of Outcomes | Bias due to Missing Outcome Data | Bias in Selection of Reported Results | Overall Risk of Bias |
|---|---|---|---|---|---|---|
| Segal et al. [35] | Low (–) | Low (–) | Low (–) | Low (–) | Low (–) | Low (–) |
| Jønsson et al. [36] | Low (–) | High (+) | Low (–) | Some concerns (~) | Low (–) | Some concerns (~) |
| Jørgensen et al. [37] | Some concerns (~) | Some concerns (~) | Some concerns (~) | Low (–) | Low (–) | Some concerns (~) |
| Jørgensen and Mechlenbur [38] | High (+) | Some concerns (~) | Low (–) | Some concerns (~) | Some concerns (~) | High (+) |
| Curran et al. [39] | Some concerns (~) | Some concerns (~) | Low (–) | Low (–) | Some concerns (~) | Some concerns (~) |
| Petersson et al. [40] | Some concerns (~) | Some concerns (~) | High (+) | Some concerns (~) | Low (–) | Some concerns (~) |
| Kacín et al. [41] | High (+) | Some concerns (~) | Low (–) | Low (–) | Low (–) | Low (–) |
| Jacobs et al. [42] | Low (–) | Some concerns (~) | Low (–) | Low (–) | Low (–) | Low (–) |
| Johannsen [43] | Some concerns (~) | Some concerns (~) | Some concerns (~) | Some concerns (~) | Low (–) | Some concerns (~) |
| Article | Time (Weeks) | Pressure | Load | Repetitions | Series | Occlusion Time |
|---|---|---|---|---|---|---|
| Segal et al. [35] | 4 | Progressive weekly pressure | 30% (1 RM) | Not specified | Not specified | 12 sessions 3 for week |
| Jønsson et al. [36] | 4 | Individual participant | 20–30% (1 RM) | Not specified | Not specified | 12 sessions 3 for week |
| Jørgensen et al. [37] | 8 | 40–80% LOP | 30% (1 RM) | Not specified | Not specified | Not specified |
| Jørgensen and Mechlenbur [38] | 12 | Not specified | 20% (1 RM) | Not specified | Not specified | Not specified |
| Curran et al. [39] | 8 | 80% Limb occlusion pressure (LOP) | 70% (1 RM) | 10 | 4 | 16 sessions 2 for week |
| Petersson et al. [40] | 8–10 | Partial pressure %LOP | Walking (4 km/h) | Not applied | Not applied | 32–40 sessions 4 for week |
| Kacín et al. [41] | 3 | Not specified | ≤30% (1 RM) | Not specified | Not specified | 9 sessions 3 for week |
| Jacobs et al. [42] | 12 | 60% (LOP) | <50% (1 RM) | Variable | Variable | 24 sessions 2 for week |
| Johannsen [43] | 12 | Partial pressure %LOP | <30% (1 RM) | Not reported | Not reported | 24 sessions 2 for week |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Santana, J.d.C.; Medina-Ramírez, R.; Marrero-Morales, M.S.; Álamo-Arce, D.D.; García-Quintana, M. Effectiveness of Therapeutic Exercise in Physiotherapy with Blood Flow Restriction in Patients with Knee Pathologies: A Systematic Review. Appl. Sci. 2025, 15, 11739. https://doi.org/10.3390/app152111739
López-Santana JdC, Medina-Ramírez R, Marrero-Morales MS, Álamo-Arce DD, García-Quintana M. Effectiveness of Therapeutic Exercise in Physiotherapy with Blood Flow Restriction in Patients with Knee Pathologies: A Systematic Review. Applied Sciences. 2025; 15(21):11739. https://doi.org/10.3390/app152111739
Chicago/Turabian StyleLópez-Santana, Joel del Cristo, Raquel Medina-Ramírez, María Sandra Marrero-Morales, Daniel David Álamo-Arce, and Marlene García-Quintana. 2025. "Effectiveness of Therapeutic Exercise in Physiotherapy with Blood Flow Restriction in Patients with Knee Pathologies: A Systematic Review" Applied Sciences 15, no. 21: 11739. https://doi.org/10.3390/app152111739
APA StyleLópez-Santana, J. d. C., Medina-Ramírez, R., Marrero-Morales, M. S., Álamo-Arce, D. D., & García-Quintana, M. (2025). Effectiveness of Therapeutic Exercise in Physiotherapy with Blood Flow Restriction in Patients with Knee Pathologies: A Systematic Review. Applied Sciences, 15(21), 11739. https://doi.org/10.3390/app152111739








