Abstract
The use of virtual reality (VR) for therapeutic purposes has expanded rapidly; however, few studies have specifically addressed amaxophobia, or driving-related fear, using immersive exposure techniques. This pilot study evaluated the feasibility and preliminary effectiveness of an immersive VR-based exposure intervention for pre-drivers with elevated driving fear. Five participants completed a five-session exposure program within a technically stable VR environment designed to support perceptual continuity and reduce cybersickness risk. Driving fear was assessed before and after the intervention using the Cuestionario para la Evaluación del Miedo a Conducir en Preconductores (CEMICP). Results showed a statistically significant reduction in fear, supported by both a one-tailed paired-samples t-test and the exact Wilcoxon signed-rank test, each revealing a large effect size. Reliable and clinically significant change analyses indicated that all participants experienced meaningful improvement, with 60% achieving clinically significant reduction in driving-related fear. These findings suggest that immersive VR exposure may offer a promising and acceptable approach to mitigate amaxophobia in young adults. Given the small single-group sample, further research is required to establish long-term effects, explore behavioral performance outcomes, and determine the mediating role of presence and emotional engagement. Future controlled trials with larger and more diverse samples are warranted to validate the clinical utility of this VR intervention.
1. Introduction
Fear is a basic emotion of considerable intensity that arises in response to an immediate and real danger, placing the individual in a state of alert [1]. According to Craske [2], fear triggers physiological responses such as an increase in heart rate and accelerated breathing. When faced with a threat, the body prepares to flee or fight by redistributing blood flow, generating an impulse to act, and producing an intense but short-lived emotional reaction. Fear may arise naturally—for example, when an animal fears a predator—or can be learned through conditioning techniques [3]. Physiologically, the response varies depending on the sensory channel involved. Different subnuclei of the amygdala and hypothalamus are activated depending on how the threat is perceived [4]. At times, fear becomes irrational and overwhelming, significantly influencing a person’s behavior. When this occurs, it is called phobia [5]. According to the World Health Organization (WHO) [6], phobias are classified into three categories: social phobia, agoraphobia (fear of being in situations where escaping or receiving help might be difficult) and specific phobias. The latter involve an irrational fear of particular objects, situations, or activities. As Eaton [7] notes, specific phobias are the most common, affecting approximately 70% of the population to some degree. The origin of phobias is not fully understood. Coelho and Purkis [8] suggest that they may originate from genetic or evolutionary factors, or from repeated negative experiences with the feared stimulus. According to Boyd et al. [9], most phobias start in early childhood and tend to diminish with time. However, this process can be significantly accelerated through the intervention of a mental health professional.
1.1. Amaxophobia
Regarding specific phobias, a prominent example is amaxophobia, or fear of driving a car. This condition often goes unnoticed, despite evidence indicating that 69% of the population experience some level of driving-related anxiety [6], and 33.3% report a specific fear of driving [10]. High levels of amaxophobia are associated with behaviors such as exaggerated safety measures, performance deficits, and hostility to other drivers [11]. Therefore, amaxophobia not only directly affects the driver, but also the road safety. It can influence decision-making, increase driving errors [10], and increase the risk of accidents, thus contributing to higher public health costs [12]. Earlier studies suggested that all people with amaxophobia had previously been involved in traffic accidents. However, more recent findings indicate otherwise. Fort et al. [13] report that driving anxiety is present in individuals both with and without a history of accidents. In a study with 2491 participants, Taylor [14] found that 5.5% experienced moderate or severe anxiety about driving, and among them, 28% had stopped driving altogether. In addition to anxiety, other related psychological conditions—such as depression, anger, substance abuse, personality disorders, or other mental health problems—may also affect driving ability. These comorbidities can lead to unsafe, aggressive, or erratic driving behaviors [15]. The underlying fears associated with amaxophobia are diverse. However, the most commonly reported fear is that of being involved in a car accident. This fear tends to intensify during periods of high life stress or in the presence of disorders such as generalized anxiety, panic disorder, agoraphobia, or claustrophobia. These factors can heighten the fear of losing control or experiencing a panic attack while driving. Although mentioned less frequently, some individuals also fear being judged by other drivers for their perceived lack of driving skill [11].
1.2. Virtual Reality Exposure Therapy
For the treatment of phobias, the WHO recognizes several techniques: psychosocial interventions, exposure therapy, cognitive-behavioral therapy, and pharmacological treatment in severe cases. Among these, exposure therapy is considered the most effective approach [16]. This method consists of gradually exposing the individual to the feared stimulus in a controlled environment, typically in sessions lasting between 20 and 40 minutes. Through repeated exposure, the person can become desensitized and reduce their fear response [17]. In exposure therapy, virtual reality (VR) has been used to treat phobias by creating simulated digital environments. Several studies have demonstrated that Virtual Reality Exposure Therapy (VRET) can achieve results comparable to or even superior to those of traditional in vivo exposure [16]. VR offers additional advantages, such as the ability to simulate environments that are difficult or impractical to reproduce in real life. It also allows precise control over the intensity and timing of exposure to feared stimuli, providing a more immersive and vivid therapeutic experience [18].
Early VRET employed multi-screen environments or Cave Automatic Virtual Environment (CAVE) systems, which offered only moderate levels of immersion and, in general, produced limited effects on the reduction of specific phobia symptoms [19]. Currently, head-mounted displays (HMDs) allow users to feel fully immersed in virtual environments by completely covering their field of view [20]. These devices offer a high degree of freedom, enabling users to look around, move, and interact as they would in real life, thereby enhancing subjective presence [21]. Moreover, modern immersive experiences can replicate physical sensations through haptic systems that transmit information to the user’s sensory channels [22]. Devices that distort the visual field, incorporate controllers with force feedback, or use motion platforms are capable of simulating resistance, speed, acceleration, and other physical aspects of driving [23].
1.3. Immersion, Presence, Fear Activation, and Extinction
When discussing the variable of immersion, it is important to define it as the degree to which a VR system engages the user’s senses and blocks external stimuli, thereby generating an enveloping perceptual experience [24]. From a psychological perspective, this phenomenon is linked to the concept—also previously mentioned—of subjective presence, characterized by the feeling of “being there” or “being inside” the virtual environment. Presence thus functions as a mediating construct between sensory perception and emotion, modulating the user’s affective involvement [25]. In other words, presence is the bridge between technological immersion and emotional immersion. When presence is high due to a high level of immersion, the individual experiences emotions authentically, perceiving virtual stimuli as relevant and coherent with their own body and context. This allows for the re-experiencing of dysfunctional emotions—such as fear or anxiety —within a controlled setting, thereby facilitating emotional self-regulation and corrective learning, processes that are central to VRET. Thus, VRET not only “shows” a phobic stimulus but also reactivates emotional responses in order to modify them effectively. It has been shown that a “sufficiently immersive” VR environment, like traditional in vivo exposure therapy, is associated with the activation of the fear system, involving structures such as the amygdala, hypothalamus, insula, anterior cingulate cortex, and ventromedial prefrontal cortex [26,27]. This activation produces measurable effects such as increased heart rate, skin conductance, sweating, muscle tension, and the release of adrenaline through the hypothalamic–pituitary–adrenal axis [28,29]. In this regard, Slater et al. [30] demonstrated that participants exposed to highly realistic three-dimensional environments exhibited greater skin conductance and heart rate in response to height stimuli, confirming the relationship between immersion and fear response. This evidence generally supports that greater immersion increases the credibility of the phobic stimulus, activating the same emotional mechanisms as in vivo exposure [31,32]. Along these lines, Riva et al. [27] argued that presence functions as a bridge between cognition and emotion in simulated contexts, and Freeman et al. [33] found that subjective presence predicted anxiety reduction following VR-assisted exposure sessions for acrophobia. A strong sense of presence, by facilitating fear activation, also optimizes extinction learning [25,27]. Once the fear response is triggered, the patient experiences the situation without real consequences (e.g., traffic does not cause an accident). This experiential realization—that the feared stimulus does not lead to actual harm—facilitates implicit cognitive restructuring, whereby dysfunctional beliefs (e.g., “If I drive, I will crash”) are weakened through a controlled emotional experience [31]. In general terms, the initial expectation of danger contrasts with the absence of negative outcomes, violating the threat prediction. This process is key to fear extinction because the brain updates its internal models of what is truly dangerous. Accordingly, Maples-Keller et al. [31] emphasize that immersion increases sensory congruence, which reinforces the emotional response and the efficacy of exposure. Repeated exposure in virtual environments leads to a progressive decrease in autonomic activation (physiological habituation), weakening of the stimulus–threat association (extinction of conditioned fear), and formation of new safety associations, thus establishing a durable inhibitory learning process [32,33].
Based on the foregoing, it is confirmed that VRET has shown promising results in the treatment of specific phobias and anxiety disorders. However, studies assessing its effectiveness have noted methodological and technological limitations that prevent this approach from consistently outperforming traditional in vivo exposure. In the case of driving phobia (amaxophobia), Elphinston et al. [34] reviewed 14 studies and concluded that interventions were feasible, well-accepted, and associated with significant reductions in self-reported anxiety. Nonetheless, most trials were characterized by small sample sizes, absence of control groups, inconsistent use of validated psychometric instruments, lack of individual-level clinical analyses, limited assessment of immersion and environmental fluidity, and no integration of haptic systems. Similarly, Kaussner et al. [35] conducted a pilot study with 14 patients and documented a 93% reduction in clinical symptoms, though the same methodological issues persisted: small sample size, no controls, and absence of standardized measures of phobia severity or immersion quality. Complementarily, Trappey et al. [36,37] developed a VRET system specifically for amaxophobia, reporting a reduction in fear and high patient acceptance, although design and evaluation shortcomings were noted. For other specific phobias (e.g., animals, heights, claustrophobia), Albakri et al. [38] reviewed 18 studies and confirmed the efficacy of VR in reducing anxiety and avoidance, although not superior to in vivo exposure. They highlighted methodological heterogeneity, short follow-ups, and inconsistent use of validated instruments. Likewise, Freitas et al. [39], in a synthesis of 30 studies, found significant reductions in symptom severity and high clinical response rates but noted the lack of long-term follow-up, individual analyses, and multisensory systems. On a larger scale, Zeng et al. [40] conducted a meta-analysis of 33 trials with 3182 participants, reporting moderate-to-large effect sizes for claustrophobia, acrophobia, fear of flying, and animal phobias, but also emphasized high heterogeneity, risk of bias, and the predominance of general anxiety measures (e.g., HAMA, BAI, STAI) rather than disorder-specific instruments. Similarly, Kuleli et al. [41] compared VRET and in vivo exposure for social anxiety and specific phobias, finding comparable efficacy, though based on only eight studies with heterogeneous protocols and small samples. At a conceptual level, Lindner et al. [42] highlighted that the effectiveness of next-generation VRET will depend on integrating stimulus progression, inhibitory learning, and gamification, elements that could improve therapeutic outcomes beyond those achieved with traditional exposure. From a practical standpoint, Krzystanek et al. [19] reviewed 49 studies and proposed implementation guidelines (e.g., number of sessions, duration, HMD use), reporting anxiety reductions between 40–70%, while also noting persistent issues such as lack of technical detail, absence of validated assessments, and minimal use of multisensory environments. Parallel evidence from the educational field [43] showed that immersive HMD-based environments improved learning outcomes compared to standard monitors, underscoring the importance of high-fidelity audiovisual immersion in therapeutic applications. Taken together, the literature indicates that VRET is effective and comparable to in vivo exposure for various specific phobias (amaxophobia, fear of flying, acrophobia, claustrophobia, animal phobias) and social anxiety, with clinical improvement rates ranging from 40 to 90%. Nevertheless, for VRET to surpass traditional exposure, future research should conduct high-quality controlled trials with larger samples and longer follow-ups; use validated, disorder-specific psychometric instruments consistently; incorporate individual-level analyses of reliable and clinically significant change; standardize the evaluation of immersion and technical fidelity; and integrate multisensory and haptic components along with gamification and inhibitory learning strategies. In particular, the use of reliable psychometric tools will allow for precise measurement of psychological constructs, valid comparisons across individuals and studies, and support for diagnosis, personalized therapy, and research replication [44]. Additionally, when combined with robust inferential analyses (e.g., t-tests, [45]) and standardized effect size reporting such as Cohen’s d, these methods enable variable and context comparisons [46]. The recommendation to include individual analyses—such as the calculation of reliable and clinically significant change—helps determine whether improvements are not only statistically valid but also meaningful at the individual level. These analyses increase study sensitivity, even with small samples, by confirming that observed changes exceed expected measurement error and reflect real improvements in daily functioning [47]. Moreover, optimizing perceptual continuity and controlled immersion through high frame rates helps reduce blur and judder, improving the coherence between user movements and virtual visualization. This enhances subjective presence and, in turn, optimizes fear extinction. Maintaining high FPS also minimizes cybersickness or motion sickness—particularly among users with little VR experience [48]—and improves motor accuracy in VR tasks [49]. Finally, VRET with multisensory tools such as steering wheels, pedals, and gear shifters can create a more realistic driving experience. This helps users stay focused and learn more effectively during sessions designed to treat amaxophobia. As a result, VR simulators can reduce irrational fear, improve driving skills, and facilitate the transfer of learning to real-world driving. Beyond individual benefits, treating driving phobia can also enhance overall road safety, as drivers who avoid panic states can act more rationally and predictably [15], thereby reducing accident risk even under adverse conditions such as rain or low visibility [13]. Fewer accidents also benefit public health and national economies, since traffic incidents account for approximately 3% of the global Gross Domestic Product (GDP) and represent the eighth leading cause of death worldwide [50].
1.4. Immersion: Technical, Perceptual, and Behavioral Parameters
Building on the above, immersion is conceptualized as the integration of perceptual and interactive features designed to enhance subjective presence and emotional engagement during virtual reality exposure interventions. From an operational standpoint, it comprises a set of parameters that directly influence perception, motor control, and multisensory coherence within the environment.
Sensorimotor congruence. In virtual reality, sensorimotor congruence is achieved through six-degree-of-freedom (6-DoF) head tracking, which maintains coherence between physical actions and visual feedback [51,52]. This congruence can be operationally assessed via motion-to-photon latency; several authors recommend keeping it below 20 ms to preserve perceptual stability [51,53]. The Meta Quest Pro headset, featuring inside-out 6-DoF tracking, provides sub-millimeter precision and an average latency of 12–20 ms—within the theoretical optimal range. Under these conditions, it would be expected to reduce unnecessary steering corrections and to support more stable lateral positioning throughout virtual driving.
Frame rate and field of view. A high frame rate (≥72 FPS) and a wide field of view (FOV) between 90° and 110° enhance optic-flow reliability and the sense of motion (vection), promoting comfort, presence, and perceptual continuity [23,31]. Empirical and ergonomic guidelines suggest that an FOV of approximately 100° provides an optimal balance between spatial awareness and visual comfort, whereas values below 80° tend to reduce immersion, and those exceeding 120° may increase distortion or simulator sickness [54,55]. Therapeutic environments therefore typically employ frame rates of 72–90 FPS and FOVs within the 90°–110° range to sustain attentional engagement during exposure tasks [23,31,54]. Under such conditions, more consistent speed regulation and smoother lane keeping would be expected.
Stereoscopic depth. Stereoscopic depth, generated through binocular disparity, enhances spatial realism and distance perception accuracy, facilitating visuomotor integration during virtual driving. Recent studies demonstrate that binocular disparity can influence motor precision and the smoothness of visuomotor coordination [56]. To maintain perceptual fidelity, disparity should remain below Panum’s binocular fusion limit to prevent diplopia or visual fatigue [57,58]. This corresponds roughly to horizontal disparities < 1°, equivalent to moderate relative depths (<40% of viewing distance). The Meta Quest Pro’s native binocular rendering system automatically adjusts interpupillary distance and camera convergence, minimizing visual strain and supporting sustained immersion [56,57]. As a behavioral outcome, more precise lane alignment and trajectory control during turns and lane changes would be expected.
Spatialized audio and ecological cues. Spatialized audio and dynamic sound mixing were incorporated to enhance situational awareness and attentional orientation. Directional auditory cues can improve hazard detection and reduce reaction times [59]. Accordingly, faster braking responses and more adaptive evasive maneuvers would be expected under realistic auditory spatialization.
Ecological cockpit cues. Elements such as mirrors, dashboard displays, and road signage provided semantic familiarity, reducing cognitive load and facilitating more intuitive interactions [32]. Such cues would be expected to support automatic action selection and to decrease attention demands during control adjustments.
As shown in Table 1, immersive elements are theoretically associated with improvements in motor-performance indicators.

Table 1.
Expected behavioral indicators associated with immersive mechanisms implemented in the VR system.
Although these indicators were not objectively assessed in this initial phase, each immersive component described above is theoretically linked to specific aspects of driving control. These relationships will guide future validation stages as the system advances toward clinical implementation.
Based on the aforementioned rationale, the objective of this study was to evaluate the effectiveness of an immersive VR-based exposure intervention in reducing driving-related fear among pre-drivers aged 20 to 25 years. Additionally, the study aimed to (a) verify the technical stability of the immersive environment during exposure sessions and (b) examine the consistency of individual improvements across participants, in order to assess the feasibility of the system for subsequent clinical implementation.
1.5. Hypotheses
Based on the literature and the objectives of this work, the following hypotheses were formulated:
- H1.
- Participants will show a significant reduction in driving-related fear after completing the immersive VR exposure intervention.
- H2.
- The proportion of participants demonstrating reliable and clinically significant improvement will exceed what could be attributed to measurement error.
- H3.
- Stable VR performance (optimal frame rate and low latency) will ensure a comfortable and perceptually coherent experience, supporting attentional engagement throughout exposure.
- H4.
- Improvements will be consistent across individuals, even under a small-sample pilot design.
2. Methods
2.1. Participants
A total of five participants (men and women) aged 20 to 25 years took part in the study. All were students from the School of Mechanical and Electrical Engineering (ESIME), Culhuacán Unit, at the Instituto Politécnico Nacional (IPN). Recruitment was carried out through an awareness campaign inviting eligible students to participate voluntarily. Those interested signed an informed consent form, ensuring confidentiality and anonymity. The inclusion criteria were voluntary participation, previous driving experience, and selfreported anxiety related to driving. Additionally, participants were required to score above 26.25 on the Questionnaire for the Evaluation of Fear of Driving in Pre-Drivers (CEMICP), corresponding to a moderate level of amaxophobia. This level was defined for the purposes of the study based on quartiles derived from the scale’s total scoring range. The exclusion criteria included failure to complete any questionnaire item (in either the pretest or posttest) or absence from any intervention session. Although no previous studies have reported amaxophobia levels by age group, research conducted in Mexico indicates that between 2.1 and 2.8% of adults have experienced a phobic disorder [60]. Since specific phobias often emerge during mid-adolescence, young adults may be more prone to exhibiting elevated levels of driving-related fear.
2.2. Design
A pre-experimental design was implemented [61], with a pretest administered before the intervention (including simulator sessions) and a posttest afterward to assess its effectiveness. This approach allowed for a pilot study that can inform future experimental research [62].
2.3. Instruments
The CEMICP [63] was administered in both the pretest and posttest. It consists of 15 items across three factors—anticipatory anxiety, anxiety response, and avoidance responses—that together explain 50.6% of the variance. These dimensions align with the DSM-V criteria for specific phobias [64]. Responses are given on a 4-point Likert scale (1 = low, 4 = high). Since clinical norms for the CEMICP are not yet available, this study applied a distribution-based approach using quartiles, a method commonly employed when normative thresholds are lacking in driving-anxiety research (see instrument development and population distribution reports in [13,65,66]. According to this quartile-based method, total scores were categorized as follows: 15–26.4 = low, 26.5–48.75 = intermediate, and 48.76–60 = high levels of amaxophobia.
Regarding its psychometric properties, internal consistency was assessed using Cronbach’s alpha, which indicated excellent reliability 0.86) [63]. To explore its internal structure, a principal components analysis with varimax rotation was conducted. Although no published empirical validation is currently available for Mexican or Latin American populations, the use of the instrument is considered justified. The construct it measures is conceptually robust, and the questionnaire specifically targets anticipatory fear of driving—a relevant dimension in pre-drivers that is rarely addressed by existing tools. Additionally, expert judgment was employed to assess the semantic and cultural equivalence of the items for the Mexican context [67].
2.4. VR System Design and Technical Validation
From a software engineering perspective, the VR environments were developed with emphasis on perceptual fidelity and operational stability. Physics-based rendering techniques with high-resolution textures and dynamic lighting were implemented to support spatial coherence during exposure. Spatialized audio and synchronized multisensory feedback (visual, auditory, and tactile) were included to facilitate realistic interaction.
To ensure consistency and participant comfort, the HMD was calibrated before each session, and visual settings (FOV 90°–110°; individualized interpupillary distance adjustment) were standardized. Hazard-related spatialized audio cues were verified for directional accuracy.
Overall, technical validation confirmed stable performance throughout all exposure sessions, ensuring perceptual continuity and preventing sensorimotor conflicts that could interfere with the treatment experience.
2.5. Intervention Procedure
The VR environments were designed to create exposure scenarios with increasing levels of driving-related fear. A panel composed of three psychologists with expertise in cognitive-behavioral interventions for anxiety, one specialist in research methodology and data analysis, and one educator with experience in curriculum evaluation reviewed and validated all scenarios. Validation followed the Fuzzy Delphi Method [68], using Item-Level Content Validity Index (I-CVI) scores and fuzzy logic criteria. Elements with ≥75% agreement were retained to ensure cognitive-behavioral consistency and ecological relevance.
The exposure protocol consisted of five levels progressing from low-demand driving contexts to increasingly complex traffic environments, consistent with graded exposure principles [69,70]. This structure aimed to promote gradual emotional adaptation while preventing overwhelming distress.
To support naturalistic motor actions during exposure tasks, the HMD was used in conjunction with a steering wheel and pedal system (see Figure 1), facilitating intuitive control and realistic behavioral engagement throughout the sessions.

Figure 1.
Experimental setup for immersive virtual reality exposure therapy.
Based on this setup, a five-level exposure therapy was designed as follows:
- Basic Driving. In this level, the driver practices in an open field by completing the following tasks:
- -
- Starting and Stopping—Practicing smooth acceleration and braking to maintain vehicle control.
- -
- Steering Control—Learning to make gradual turns, keep a steady grip, and understand how the car responds.
- -
- Straight-Line Driving—Driving in a straight line without excessive steering corrections.
- -
- Basic Turns—Performing controlled left and right turns while adjusting speed appropriately.
- -
- Parking and Low-Speed Maneuvers—Practicing parking skills, including reversing and parallel parking.
- -
- Obstacle Avoidance—Driving around cones or markers to improve reaction time and precision.
- -
- Emergency Braking—Learning how to stop the car quickly while maintaining control.
- -
- Gradual Speed Adjustment—Practicing smooth acceleration and deceleration without abrupt changes.
According to Figure 2, we outline the activities involved in this level as follows. Figure 2. Level 1 overview: route map and virtual environment.Route Description:
Figure 2. Level 1 overview: route map and virtual environment.Route Description:- -
- Begin on a straight path to practice smooth starts and stops.
- -
- Drive in a large oval loop to practice gradual turns and steering control.
- -
- Include a cone slalom section for obstacle avoidance and steering precision.
- -
- Add a parking zone with marked spaces for practicing low-speed maneuvers and reverse parking.
- -
- Designate an area for emergency braking drills with clear stopping points.
- -
- Use a long straight stretch for practicing gradual acceleration and deceleration.
Level 2. Precise Driving. In this level, the driver practices parking smoothly in a tight space, where even small mistakes are not tolerated. The activities include:
- Turn Control—Performing safe and controlled turns with awareness of hazards and pedestrians.
- Precise Parking—Practicing city parking with minimal space between vehicles.
- Low-Speed Management—Maintaining steady speed without sudden acceleration or hard braking.
- Close-Distance Driving—Navigating around vehicles and through narrow spaces without collisions.
- Obstacle Avoidance—Reacting to unexpected obstacles, such as carts or pedestrians.
Figure 3 provides a visual guide to the activities described below.
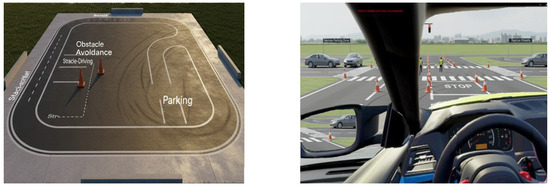
Figure 3.
Level 2 overview: route map and virtual environment.
Route Description:
- Start with narrow lanes to practice close-distance driving and low-speed control.
- Include tight parking spots between cones or mock vehicles for precision parking.
- Add sharp turns and T-intersections to practice turn control and hazard awareness.
- Introduce unexpected obstacles (e.g., moving cones or pedestrian dummies) for reaction training.
- Include a loop with varying widths to simulate real-world tight navigation.
Level 3. Precise Driving and Incorporation into Avenues. This level requires the driver to demonstrate advanced vehicle control, spatial awareness, and adaptability to changing traffic conditions. The activities are divided into two categories:
Precise Driving Activities
- Controlled Acceleration and Braking—Transitioning smoothly between speeds to avoid abrupt movements.
- Exact Lane Positioning—Keeping the vehicle centered within the lane and minimizing drifting.
- Precision Turns—Performing sharp or gradual turns with accurate steering and speed control.
- Mirror and Blind Spot Awareness—Using mirrors properly and checking blind spots before maneuvers.
- Close-Proximity Navigation—Driving near other vehicles while maintaining safe distances.
- Consistent Speed Control—Adjusting speed smoothly to match traffic flow without sudden changes.
Incorporation into Avenues
- Merging Techniques—Entering traffic smoothly while maintaining safe gaps.
- Acceleration Management—Adjusting speed for fluid integration into busy avenues.
- Predictive Driving—Anticipating traffic behavior and responding appropriately.
- Lane Transitions—Changing lanes with proper timing and signaling.
- Defensive Driving—Staying alert to unpredictable drivers and avoiding hazards.
- Exit Strategies—Preparing lane changes early to exit without abrupt maneuvers.
Figure 4 provides a visual guide to the activities described below.

Figure 4.
Level 3 overview: route map and virtual environment.
Route Description:
- Begin with marked lanes for practicing exact lane positioning and consistent speed.
- Include curved roads and roundabouts for precision turns and steering.
- Add mirror check zones where drivers must identify blind spots before lane changes.
- Introduce traffic merging areas with simulated moving vehicles.
- Include multi-lane sections for practicing lane transitions and defensive driving.
Level 4. Incorporation into Avenues and Free Driving in Parking Areas. At this level, the driver must demonstrate precision and situational awareness in traffic and confined spaces. Key activities are divided into two parts:
Incorporation into Avenues
- Traffic Gap Assessment—Identifying safe gaps for merging without disrupting traffic flow.
- Acceleration Control—Adjusting speed to match the avenue’s pace before merging.
- Signaling and Predictive Driving—Using signals early and anticipating the actions of other drivers.
- Mirror and Blind Spot Checks—Ensuring the path is clear before changing lanes.
- Lane Discipline—Maintaining a consistent position within the lane after merging.
- Defensive Positioning—Keeping a safe distance and staying alert to unpredictable behavior.
Free Driving in Parking Areas
- Smooth Navigation Through Tight Spaces—Driving at a steady speed around parked cars and pedestrians.
- Turning and Positioning Efficiency—Making fluid turns and aligning the vehicle correctly within lanes.
- Adapting to Unexpected Obstacles—Reacting promptly to moving vehicles or pedestrians.
- Speed Control in Confined Areas—Applying low-speed techniques to ensure safety.
- Reverse and U-Turn Adjustments—Practicing controlled reversing and repositioning when necessary.
Figure 5 provides a visual guide to the activities described below.

Figure 5.
Level 4 overview: route map and virtual environment.
Route Description:
- Start on a moderate-traffic avenue to practice merging, signaling, and lane discipline.
- Include intersections with traffic lights for predictive and defensive driving.
- Transition into a parking lot with tight spaces and pedestrian activity.
- Practice navigating around parked cars, reversing, and U-turns.
- Add randomized obstacles (e.g., cones, moving objects) to simulate real-world unpredictability.
Level 5. Free Driving in Urban Environments. At this stage, the driver must demonstrate adaptability, precision, and full awareness of complex surroundings. Key activities include:
- Traffic Flow Adaptation—Modifying speed and position in according to congestion and pedestrian movement.
- Intersection Navigation—Managing stoplights, crosswalks, and unprotected turns with accuracy.
- Lane Discipline and Merging—Maintaining lane control and merging smoothly without disrupting other vehicles.
- Predictive Driving—Anticipating the actions of nearby cars, cyclists, and pedestrians.
- Efficient Route Planning—Navigating city streets while optimizing time and fuel consumption.
- Street Parking and Quick Stops—Executing parallel parking, curbside stops, and brief pullovers effectively.
- Adapting to Road Hazards—Responding to potholes, abrupt stops, or unexpected obstacles with control.
- Driving in High-Traffic Areas—Handling narrow spaces, traffic jams, and multi-lane transitions with confidence.
Figure 6 provides a visual guide to the activities described below.

Figure 6.
Level 5 overview: route map and virtual environment.
Route Description:
- Navigate through busy intersections with traffic signals and pedestrian crossings.
- Drive along main roads and side streets.
- Practice parallel parking and quick curbside stops in real traffic.
- Include multi-lane roads for merging and lane changes.
- Navigate construction zones, potholes, and narrow streets to build hazard awareness.
The structure and progression of the driving scenarios were intentionally aligned with both ecological validity and the psychological demands associated with driving-related fear. Each level was designed to activate and progressively reduce specific cognitive, emotional, and behavioral processes known to maintain amaxophobia—such as anticipatory anxiety, fear of making mistakes, and limited tolerance for unpredictability. By adjusting attentional and emotional load step by step, this graded exposure approach follows established cognitive-behavioral principles that facilitate inhibitory learning and mastery acquisition, thereby strengthening perceived control and reducing avoidance across increasingly complex situations:
Level 1—Basic Driving. Conducted in a distraction-free environment. The primary psychological challenge is managing anticipatory anxiety, including catastrophic thoughts (e.g., “I will not be able to do this”) and somatic hyperarousal upon entering the vehicle [71,72]. Expected behavioral outcome: participants initiate and sustain the driving task with reduced physiological distress.
Level 2—Precision Driving. Focuses on low-speed motor tasks (e.g., parking) without traffic. The main challenge involves self-criticism and perfectionism, which may lead to excessive muscle tension and overcontrol [73,74]. Expected behavioral outcome: improved motor fluidity and tolerance of minor errors.
Level 3—Driving in Avenues. Integrates basic navigation demands. This level elicits social evaluative concerns and intrusive thoughts about negative judgment from others [75]. Expected behavioral outcome: maintenance of vehicle control while managing divided attention and social pressure.
Level 4—Avenues with Low Traffic. Introduces mild unpredictability and autonomous decision-making demands. Anxiety may arise from reduced situational control [76]. Expected behavioral outcome: increased confidence handling unexpected events.
Level 5—Urban Free Driving. Involves complex real-world stimuli (traffic, signage, noise). Emotional stability must be maintained despite heightened cognitive load [77,78]. Expected behavioral outcome: successful application of coping strategies under high demand, supporting skill transfer to real driving situations.
2.6. Data Analysis
All analyses were pre-specified to address four hypotheses (H1–H4). Statistical tests used an a priori significance level of . Given the directional nature of the primary clinical hypothesis (H1), one-tailed tests were employed for pre–post reductions in fear; all other inferential procedures were two-tailed. Effect sizes and confidence intervals (CIs) are reported alongside p-values to facilitate interpretation.
H1. Reduction in driving-related fear. To test whether participants showed a significant decrease in driving-related fear after completing the immersive VR exposure intervention, we analyzed total CEMICP scores (pre vs. post). Distributional assumptions were examined with the Shapiro–Wilk test. When normality was tenable (), a one-tailed paired-samples t-test evaluated the directional hypothesis (post < pre), with effect size computed as Cohen’s d for dependent means and 95% CI obtained from the noncentral-t distribution. If normality was not tenable, the exact Wilcoxon signed-rank test (one-tailed) was used, reporting the effect size and its 95% CI via large-sample approximation. Alongside null-hypothesis tests, we provide an estimate of the mean change () with bootstrap 95% CI (10,000 resamples) to quantify the magnitude and precision of improvement.
H2. Reliable and clinically significant improvement. To determine whether improvements exceeded measurement error and reached clinical relevance, we computed (a) the Reliable Change Index (RCI) and (b) Clinically Significant Change (CSC) at the individual level [47]. Reliable change was defined as
where is the pretest standard deviation and denotes internal consistency. Values indicate change unlikely due to measurement error. Clinically significant change followed Method A (shift in the adaptive direction), treated here as an exploratory benchmark given the absence of population norms for pre-drivers. We summarize the proportion of participants meeting RCI and CSC criteria with exact (Clopper–Pearson) 95% CIs, and, optionally, evaluate whether the observed proportion exceeds a minimal benchmark via an exact binomial test (exploratory).
H3. Stability of VR performance during exposure. System performance was continuously monitored with fpsVR to verify that immersion quality met predefined operational thresholds throughout exposure. Metrics included frame rate (FPS), motion-to-photon latency, GPU/CPU frame time, and dropped frames. Session-level summaries (mean, range) were compared to target criteria (e.g., FPS , latency ms, dropped frames ), and compliance was expressed as the proportion of session time within-spec with 95% CIs. These analyses assess whether the technical context remained perceptually coherent (i.e., stable visual flow and low latency) so as not to confound exposure-based learning.
H4. Consistency of improvements across individuals. To examine whether improvements were consistent at the individual level in this small-sample pilot, we (a) inspected within-subject change trajectories, (b) quantified the directional consistency of change using the exact sign test (post < pre), and (c) summarized heterogeneity with the distribution of individual change scores (; median, IQR) and the coefficient of variation of . As an additional robustness check, we report the proportion of participants showing improvement greater than a small, a priori minimal important change (MIC; exploratory) and its exact 95% CI. Taken together with H2 (RCI/CSC), these indicators characterize both the direction and the consistency of pre–post improvement across individuals.
Visualization and reporting. Descriptive graphics (individual pre–post plots and group means with error bars) are presented as complementary evidence to illustrate distributional features and person-level trajectories; they are not used for confirmatory inference. All analyses follow best-practice recommendations for small-n pilots, emphasizing effect sizes, CIs, and individual-level indices in addition to significance testing.
3. Results
3.1. Test of Hypothesis 1: Reduction in Driving-Related Fear
As shown in Table 2, the use of the immersive VR environment during the exposure sessions led to a decrease in amaxophobia levels, as measured by CEMICP scores. Figure 7 and Figure 8 illustrate these improvements at the individual and group levels.

Table 2.
Scores obtained in the CEMICP before and after the intervention.
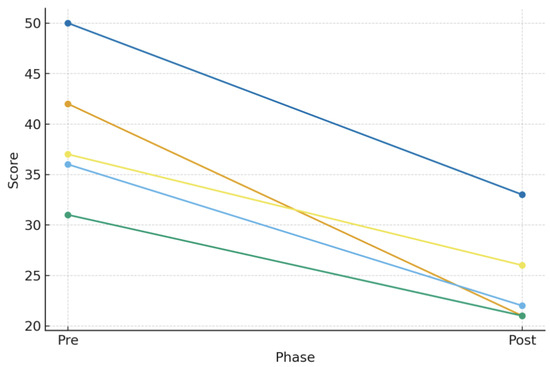
Figure 7.
Individual pre–post scores for each participant on the CEMICP, showing a consistent reduction in driving-related fear following the exposure sessions.
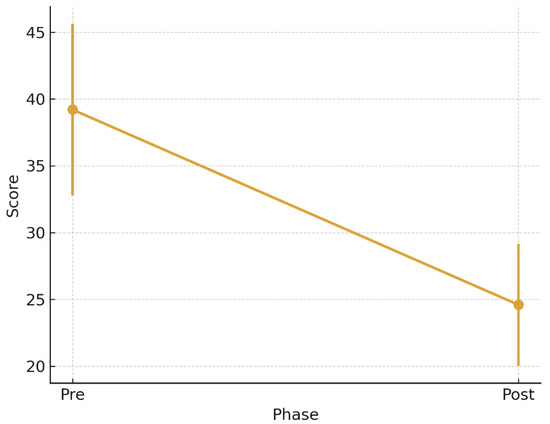
Figure 8.
Mean CEMICP scores before and after the intervention, with error bars representing standard deviations (39.2 ± 6.43 and 24.6 ± 4.58), indicating a significant overall reduction in amaxophobia levels.
The Shapiro–Wilk test confirmed normality of the pre–post difference (, ), supporting the use of parametric testing. Accordingly, a one-tailed paired-samples t-test revealed a statistically significant reduction in driving fear from pretest (, ) to posttest (, ), , , 95% CI [8.67, 20.53], corresponding to a large effect size (). A robustness check using the exact Wilcoxon signed-rank test confirmed this pattern (, ; , ). Together, these results support Hypothesis 1.
3.2. Test of Hypotheses 2 & 4: Reliable Improvement and Consistency Across Participants
To complement the group findings and assess individual improvements, Reliable Change Index (RCI) and Clinically Significant Change (CSC) criteria [47] were applied. A reduction of at least 6.67 points was required for reliable improvement. All participants (100%) exceeded this threshold. Additionally, 60% achieved clinically significant change, while 40% demonstrated reliable but not yet clinically significant improvement (Table 3; Figure 9). These results support Hypotheses 2 and 4.

Table 3.
Type of improvement observed in each participant.
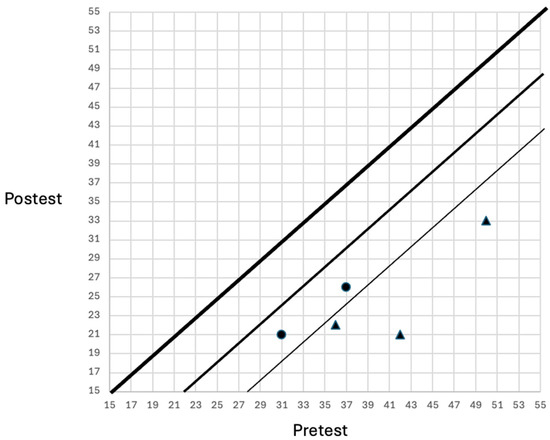
Figure 9.
Participants showing reliable change (circles) and clinically significant change (triangles).
3.3. Test of Hypothesis 3: Stability of VR Performance
Analysis using fpsVR software (2.1.8789) indicated that the immersive environment maintained a stable performance close to 72 FPS, consistent with Meta Quest Pro standards. Frame rate variability was minimal, meeting platform guidelines to minimize dizziness and visual fatigue. Average frame time was 2.6 ms on GPU and 3.1 ms on CPU, with no dropped frames (0%). Collectively, these results indicate that the immersive VR system met both technical and therapeutic expectations, enabling a meaningful evaluation of the exposure protocol.
4. Discussion
This pilot study provides preliminary but compelling evidence that VRET may reduce amaxophobia in young pre-drivers. Statistically significant and clinically relevant decreases in fear following the intervention confirmed the main hypothesis (H1), consistent with previous findings in VR-based treatment of specific phobias [16,39,79]. The consistency of improvements across all participants further supported Hypothesis 4.
A key contribution of this work is the demonstration that the immersive system maintained stable operational performance during exposure (H3), including high frame rates, low latency, and no dropped frames. These factors are critical to maintaining perceptual coherence and attentional engagement, which in turn facilitate therapeutic processing [24,80]. Although presence and emotional engagement were not directly evaluated, maintaining technical fidelity represents a precondition for their development.
The hierarchical five-level exposure structure addressed clinically meaningful mechanisms associated with driving anxiety, including anticipatory fear, performance concerns, social evaluation, uncertainty tolerance, and emotional regulation during increased cognitive load. These properties are consistent with systematic desensitization and inhibitory learning principles [71,81,82], and may have contributed to fear extinction and cognitive reappraisal processes [32]. Moreover, the expert validation process supported ecological and cognitive relevance of the designed scenarios [83,84].
However, several limitations temper the strength of these conclusions. The very small and homogeneous sample increases uncertainty in effect sizes and raises the possibility of overestimation [85,86]. The absence of a control group prevents exclusion of expectancy or novelty effects. Improvements were assessed only immediately after the intervention, making medium- or long-term durability unknown. Additionally, although the system incorporated immersive elements such as binocular disparity, spatialized audio, and ecological cockpit cues, behavioral metrics theoretically linked to these mechanisms (e.g., steering precision, hazard response time) were not collected. Likewise, key mediators—including presence, emotional engagement, and cybersickness—were not measured, which limits interpretation about how and why fear was reduced [24,80].
Another methodological consideration is that the CEMICP, while reliable, would benefit from broader validation among Mexican pre-driver populations to strengthen clinical interpretability. Future studies should integrate standardized presence scales, physiological indicators, and behavioral driving measures to clarify therapeutic pathways and support real-world transfer.
Despite these constraints, the results converge with broader evidence demonstrating that VR can be an accessible, scalable modality for exposure therapy [16,80]. Implementing preventive interventions among pre-drivers may reduce avoidance and enhance road safety by improving confidence and coping under natural driving demands [87].
Future work should employ larger randomized controlled trials, incorporate longitudinal follow-ups, and evaluate stronger mechanisms of change through adaptive stimulus progression, inhibitory learning strategies, and gamification elements designed to enhance motivation and retention [42].
5. Conclusions
This study supports the feasibility and potential therapeutic value of VRET for reducing driving-related fear in young adults. Large, statistically significant effects were obtained despite the reduced sample size, and consistent improvements were observed across all participants. Additionally, the high technical stability of the system supports its suitability for clinical implementation.
Nevertheless, interpretations must remain cautious given the lack of a comparison group, the exclusive reliance on self-report outcomes, and the absence of behavioral or physiological measures. Long-term maintenance of therapeutic gains remains to be established. Moreover, the mediating role of presence and emotional engagement should be directly evaluated in future research.
Further development should include larger, more diverse samples, integration of driving performance metrics, standardized presence measurement, and factorial designs testing specific immersive mechanisms. Optimizing the exposure structure through gamification and inhibitory learning principles may enhance both treatment adherence and transfer to real-world situations.
Overall, this prototype demonstrates that immersive VR represents a promising avenue for addressing driving fear during early driver development, but additional rigorous research is required before clinical adoption.
Author Contributions
Conceptualization, G.S.; Data curation, R.P.F.E. and A.G.G.C.; Formal analysis, G.S. and R.P.F.E.; Funding acquisition, R.P.F.E. and G.S.; Investigation, G.E.O.C. and J.G.A.; Methodology, J.G.A. and G.S.; Resources, R.A.A. and L.S.B.; Software, G.S.; Supervision, L.S.B. and G.S.; Validation, J.G.A. and A.G.G.C.; Writing—original draft, R.P.F.E. and G.S.; Writing—review & editing, R.P.F.E. and G.S. All authors have read and agreed to the published version of the manuscript.
Funding
The authors would like to thank the Instituto Politécnico Nacional for the financial support.
Institutional Review Board Statement
This study was conducted in accordance with the ethical standards and considerations for human research in force in Mexico (Sociedad Mexicana de Psicología, 2010) and the APA (American Psychological Association, 2017). It is a study with minimal risk for participants according to the Reglamento de la Ley General de Salud en Materia de Investigación para la Salud (Art. 3 Frac. I, Art. 4, Art. 6, Title II Chap. I, Art. 17, frac. II) and its update published in the Diario Oficial de la Federación (2 April 2014) and based on the Norma Oficial Mexicana NOM-012-SSA3-2012 (Article 5 numbers 5.3 to 5.13 and 5.15), which establishes the criteria for the execution of health research projects in human beings.
Informed Consent Statement
Based on Articles 21 and 22 of the Reglamento de la Ley General de Salud en Materia de Investigación para la Salud, participants signed an informed consent form after being provided with a clear and complete explanation of the research objectives, the procedures to be followed, the benefits of conducting the study, and the opportunity to request information about the results obtained after the study was completed.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors under a reasonable request.
Acknowledgments
The authors thank the IPN for the financial support for this work.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kazdin, A.E. Encyclopedia of Psychology; American Psychological Association: Washington, DC, USA, 2000; Volume 8. [Google Scholar]
- Craske, M.G.; Rauch, S.L.; Ursano, R.; Prenoveau, J.; Pine, D.S.; Zinbarg, R.E. What is an anxiety disorder? Focus 2011, 9, 369–388. [Google Scholar] [CrossRef]
- Hartley, C.A.; Phelps, E.A. Anxiety and decision-making. Biol. Psychiatry 2012, 72, 113–118. [Google Scholar] [CrossRef]
- Adolphs, R. The biology of fear. Curr. Biol. 2013, 23, R79–R93. [Google Scholar] [CrossRef]
- Medina, M.M.; Peláez, E.P. Estudio Amaxofobia: Miedo a Conducir; Technical Report; Fundación MAPFRE, Instituto de Seguridad Vial: Madrid, Spain, 2005. [Google Scholar]
- WHO. Phobias; Technical Report; World Health Organization, Regional Office for the Eastern Mediterranean: Geneva, Switzerland, 2025. [Google Scholar]
- Eaton, W.W.; Bienvenu, O.J.; Miloyan, B. Specific phobias. Lancet Psychiatry 2018, 5, 678–686. [Google Scholar] [CrossRef]
- Coelho, C.M.; Purkis, H. The origins of specific phobias: Influential theories and current perspectives. Rev. Gen. Psychol. 2009, 13, 335–348. [Google Scholar] [CrossRef]
- Boyd, J.; Rae, D.; Thompson, J.; Burns, B.; Bourdon, K.; Locke, B.; Regier, D. Phobia: Prevalence and risk factors. Soc. Psychiatry Psychiatr. Epidemiol. 1990, 25, 314–323. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.E. The extent and characteristics of driving anxiety. Transp. Res. Part F Traffic Psychol. Behav. 2018, 58, 70–79. [Google Scholar] [CrossRef]
- Clapp, J.D.; Olsen, S.A.; Danoff-Burg, S.; Hagewood, J.H.; Hickling, E.J.; Hwang, V.S.; Beck, J.G. Factors contributing to anxious driving behavior: The role of stress history and accident severity. J. Anxiety Disord. 2011, 25, 592–598. [Google Scholar] [CrossRef] [PubMed]
- Măirean, C. The relation between driving cognitions and driving phobia: The moderating role of emotional regulation strategies. Rom. J. Appl. Psychol. 2018, 20, 37–44. [Google Scholar]
- Fort, A.; Evennou, M.; Jallais, C.; Charbotel, B.; Hidalgo-Muñoz, A. A prevalence study of driving anxiety in France. J. Transp. Health 2023, 32, 101657. [Google Scholar] [CrossRef]
- Taylor, J.E.; Alpass, F.; Stephens, C.; Towers, A. Driving anxiety and fear in young older adults in New Zealand. Age Ageing 2011, 40, 62–66. [Google Scholar] [CrossRef]
- Taylor, J.E. Mental health and driving. In Handbook of Traffic Psychology; Elsevier: Amsterdam, The Netherlands, 2011; pp. 165–178. [Google Scholar]
- Botella, C.; Fernández-Álvarez, J.; Guillén, V.; García-Palacios, A.; Baños, R. Recent progress in virtual reality exposure therapy for phobias: A systematic review. Curr. Psychiatry Rep. 2017, 19, 1–13. [Google Scholar] [CrossRef]
- Gutiérrez-Maldonado, J.; Magallón-Neri, E.; Rus-Calafell, M.; Peñaloza-Salazar, C. Virtual reality exposure therapy for school phobia. Anuario de Psicología 2009, 40, 223–236. [Google Scholar]
- Costa, R.T.d.; Carvalho, M.R.d.; Ribeiro, P.; Nardi, A.E. Virtual reality exposure therapy for fear of driving: Analysis of clinical characteristics, physiological response, and sense of presence. Braz. J. Psychiatry 2018, 40, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Krzystanek, M.; Surma, S.; Stokrocka, M.; Romańczyk, M.; Przybyło, J.; Krzystanek, N.; Borkowski, M. Tips for effective implementation of virtual reality exposure therapy in phobias—A systematic review. Front. Psychiatry 2021, 12, 737351. [Google Scholar] [CrossRef] [PubMed]
- Shu, Y.; Huang, Y.Z.; Chang, S.H.; Chen, M.Y. Do virtual reality head-mounted displays make a difference? A comparison of presence and self-efficacy between head-mounted displays and desktop computer-facilitated virtual environments. Virtual Real. 2019, 23, 437–446. [Google Scholar] [CrossRef]
- Chandrasekera, T.; Fernando, K.; Puig, L. Effect of degrees of freedom on the sense of presence generated by virtual reality (VR) head-mounted display systems: A case study on the use of VR in early design studios. J. Educ. Technol. Syst. 2019, 47, 513–522. [Google Scholar] [CrossRef]
- Podobnik, J.; Mihelj, M. Haptics for Virtual Reality and Teleoperation; Springer: Berlin/Heidelberg, Germany, 2012. [Google Scholar]
- Kemeny, A. From driving simulation to virtual reality. In Proceedings of the 2014 Virtual Reality International Conference, Shenyang, China, 30–31 August 2014; pp. 1–5. [Google Scholar]
- Slater, M.; Wilbur, S. A framework for immersive virtual environments (FIVE): Speculations on the role of presence in virtual environments. Presence Teleoperators Virtual Environ. 1997, 6, 603–616. [Google Scholar] [CrossRef]
- Slater, M. Place illusion and plausibility can lead to realistic behaviour in immersive virtual environments. Philos. Trans. R. Soc. B Biol. Sci. 2009, 364, 3549–3557. [Google Scholar] [CrossRef]
- LeDoux, J.E. Coming to terms with fear. Proc. Natl. Acad. Sci. USA 2014, 111, 2871–2878. [Google Scholar] [CrossRef]
- Riva, G.; Mantovani, F.; Capideville, C.S.; Preziosa, A.; Morganti, F.; Villani, D.; Gaggioli, A.; Botella, C.; Alcañiz, M. Affective interactions using virtual reality: The link between presence and emotions. Cyberpsychol. Behav. 2007, 10, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Wiederhold, B.K.; Wiederhold, M.D. Virtual Reality Therapy for Anxiety Disorders; American Psychological Association: Washington, DC, USA, 2005; Volume 10, p. 10858. [Google Scholar]
- Parsons, T.D.; Rizzo, A.A. Affective outcomes of virtual reality exposure therapy for anxiety and specific phobias: A meta-analysis. J. Behav. Ther. Exp. Psychiatry 2008, 39, 250–261. [Google Scholar] [CrossRef] [PubMed]
- Slater, M.; Khanna, P.; Mortensen, J.; Yu, I. Visual realism enhances realistic response in an immersive virtual environment. IEEE Comput. Graph. Appl. 2009, 29, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Maples-Keller, J.L.; Bunnell, B.E.; Kim, S.J.; Rothbaum, B.O. The use of virtual reality technology in the treatment of anxiety and other psychiatric disorders. Harv. Rev. Psychiatry 2017, 25, 103–113. [Google Scholar] [CrossRef]
- Carl, E.; Stein, A.T.; Levihn-Coon, A.; Pogue, J.R.; Rothbaum, B.; Emmelkamp, P.; Asmundson, G.J.; Carlbring, P.; Powers, M.B. Virtual reality exposure therapy for anxiety and related disorders: A meta-analysis of randomized controlled trials. J. Anxiety Disord. 2019, 61, 27–36. [Google Scholar] [CrossRef]
- Freeman, D.; Haselton, P.; Freeman, J.; Spanlang, B.; Kishore, S.; Albery, E.; Denne, M.; Brown, P.; Slater, M.; Nickless, A. Automated psychological therapy using immersive virtual reality for treatment of fear of heights: A single-blind, parallel-group, randomised controlled trial. Lancet Psychiatry 2018, 5, 625–632. [Google Scholar] [CrossRef]
- Elphinston, R.A.; Vaezipour, A.; Fowler, J.A.; Russell, T.G.; Sterling, M. Psychological therapy using virtual reality for treatment of driving phobia: A systematic review. Disabil. Rehabil. 2023, 45, 1582–1594. [Google Scholar] [CrossRef]
- Kaussner, Y.; Kuraszkiewicz, A.; Schoch, S.; Markel, P.; Hoffmann, S.; Baur-Streubel, R.; Kenntner-Mabiala, R.; Pauli, P. Treating patients with driving phobia by virtual reality exposure therapy—A pilot study. PLoS ONE 2020, 15, e0226937. [Google Scholar] [CrossRef]
- Trappey, A.; Trappey, C.V.; Chang, C.M.; Kuo, R.R.; Lin, A.P.; Nieh, C. Virtual reality exposure therapy for driving phobia disorder: System design and development. Appl. Sci. 2020, 10, 4860. [Google Scholar] [CrossRef]
- Trappey, A.; Trappey, C.V.; Chang, C.M.; Tsai, M.C.; Kuo, R.R.; Lin, A.P. Virtual reality exposure therapy for driving phobia disorder (2): System refinement and verification. Appl. Sci. 2020, 11, 347. [Google Scholar] [CrossRef]
- Albakri, G.; Bouaziz, R.; Alharthi, W.; Kammoun, S.; Al-Sarem, M.; Saeed, F.; Hadwan, M. Phobia exposure therapy using virtual and augmented reality: A systematic review. Appl. Sci. 2022, 12, 1672. [Google Scholar] [CrossRef]
- Freitas, J.R.S.; Velosa, V.H.S.; Abreu, L.T.N.; Jardim, R.L.; Santos, J.A.V.; Peres, B.; Campos, P.F. Virtual reality exposure treatment in phobias: A systematic review. Psychiatr. Q. 2021, 92, 1685–1710. [Google Scholar] [CrossRef] [PubMed]
- Zeng, W.; Xu, J.; Yu, J.; Chu, X. Effectiveness of virtual reality therapy in the treatment of anxiety disorders in adolescents and adults: A systematic review and meta-analysis of randomized controlled trials. Front. Psychiatry 2025, 16, 1553290. [Google Scholar] [CrossRef]
- Kuleli, D.; Tyson, P.; Davies, N.H.; Zeng, B. Examining the comparative effectiveness of virtual reality and in-vivo exposure therapy on social anxiety and specific phobia: A systematic review & meta-analysis. J. Behav. Cogn. Ther. 2025, 35, 100524. [Google Scholar] [CrossRef]
- Lindner, P.; Miloff, A.; Hamilton, W.; Reuterskiöld, L.; Andersson, G.; Powers, M.B.; Carlbring, P. Creating state of the art, next-generation Virtual Reality exposure therapies for anxiety disorders using consumer hardware platforms: Design considerations and future directions. Cogn. Behav. Ther. 2017, 46, 404–420. [Google Scholar] [CrossRef] [PubMed]
- Coulter, R.; Saland, L.; Caudell, T.; Goldsmith, T.E.; Alverson, D. The effect of degree of immersion upon learning performance in virtual reality simulations for medical education. Inmedicine Meets Virtual Real. 2007, 15, 155. [Google Scholar]
- Sakata, M.; Toyomoto, R.; Yoshida, K.; Luo, Y.; Nakagami, Y.; Aoki, S.; Irie, T.; Sakano, Y.; Suga, H.; Sumi, M.; et al. Development and validation of the cognitive behavioural therapy skills scale among college students. BMJ Ment. Health 2021, 24, 70–76. [Google Scholar] [CrossRef]
- De Winter, J.C. Using the Student’s t-Test with Extremely Small Sample Sizes. Pract. Assess. Res. Eval. 2013, 18, n10. [Google Scholar]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef]
- Jacobson, N.S.; Truax, P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 1991, 59, 12–19. [Google Scholar] [CrossRef]
- Goedicke, D.; Li, J.; Evers, V.; Ju, W. Vr-oom: Virtual reality on-road driving simulation. In Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems, Montreal, QC, Canada, 21–27 April 2018; pp. 1–11. [Google Scholar]
- Watson, B.; Spaulding, V.; Walker, N.; Ribarsky, W. Evaluation of the effects of frame time variation on VR task performance. In Proceedings of the IEEE 1997 Annual International Symposium on Virtual Reality, Albuquerque, NM, USA, 1–5 March 1997; IEEE: New York, NY, USA, 1997; pp. 38–44. [Google Scholar]
- Singh, H.; Kathuria, A. Analyzing driver behavior under naturalistic driving conditions: A review. Accid. Anal. Prev. 2021, 150, 105908. [Google Scholar] [CrossRef]
- Jerald, J. The VR Book: Human-Centered Design for Virtual Reality; Morgan & Claypool: San Rafael, CA, USA, 2015. [Google Scholar]
- Slater, M.; Sanchez-Vives, M.V. Enhancing our lives with immersive virtual reality. Front. Robot. AI 2016, 3, 74. [Google Scholar] [CrossRef]
- Diels, C.; Howarth, P.A. Frequency characteristics of visually induced motion sickness. Hum. Factors 2013, 55, 595–604. [Google Scholar] [CrossRef]
- Riva, G. Virtual reality in clinical psychology. Compr. Clin. Psychol. 2022, 91–105. [Google Scholar] [CrossRef]
- Stanney, K.; Lawson, B.D.; Rokers, B.; Dennison, M.; Fidopiastis, C.; Stoffregen, T.; Weech, S.; Fulvio, J.M. Identifying causes of and solutions for cybersickness in immersive technology: Reformulation of a research and development agenda. Int. J. Hum. Comput. Interact. 2020, 36, 1783–1803. [Google Scholar] [CrossRef]
- Kim, H.; Kim, Y.; Lee, J.; Kim, J. Stereoscopic objects affect reaching performance in virtual reality environments: Influence of age on motor control. Front. Virtual Real. 2024, 5, 1475482. [Google Scholar] [CrossRef]
- Hibbard, P.B.; Haines, A.E.; Hornsey, R.L. Magnitude, precision, and realism of depth perception in stereoscopic vision. Cogn. Res. Princ. Implic. 2017, 2, 25. [Google Scholar] [CrossRef]
- Holliman, N.S.; Dodgson, N.A.; Favalora, G.E.; Pockett, L. Three-dimensional displays: A review and applications analysis. IEEE Trans. Broadcast. 2011, 57, 362–371. [Google Scholar] [CrossRef]
- Hoeg, E.R.; Gerry, L.J.; Thomsen, L.; Nilsson, N.C.; Serafin, S. Binaural sound reduces reaction time in a virtual reality search task. In Proceedings of the 2017 IEEE 3rd VR Workshop on Sonic Interactions for Virtual Environments (SIVE), Los Angeles, CA, USA, 19 March 2017; IEEE: New York, NY, USA, 2017; pp. 1–4. [Google Scholar]
- Caraveo-Anduaga, J.J.; Colmenares, E. Prevalencia de los trastornos de ansiedad fóbica en la población adulta de la ciudad de México. Salud Ment. 2000, 23, 10–19. [Google Scholar]
- Campbell, D.T.; Stanley, J.C. Experimental and Quasi-Experimental Designs for Research; Ravenio Books: Ann Arbor, MI, USA, 2015. [Google Scholar]
- Martin, D.W. Psicología Experimental: Cómo Hacer Experimentos en Psicología; Cengage Learning Editores: Ciudad de México, Mexico, 2008. [Google Scholar]
- Marín, S.S. Validation of a short questionnaire to assess the fear driving would-be drivers. Secur. Vialis 2012, 1, 17–22. [Google Scholar] [CrossRef]
- Morrison, J. DSM-5® Guía para el Diagnóstico Clínico; Editorial El Manual Moderno: Ciudad de México, Mexico, 2015. [Google Scholar]
- Ehlers, A.; Taylor, J.E.; Ehring, T.; Hofmann, S.G.; Deane, F.P.; Roth, W.T.; Podd, J.V. The driving cognitions questionnaire: Development and preliminary psychometric properties. J. Anxiety Disord. 2007, 21, 493–509. [Google Scholar] [CrossRef] [PubMed]
- Clapp, J.D.; Olsen, S.A.; Beck, J.G.; Palyo, S.A.; Grant, D.M.; Gudmundsdottir, B.; Marques, L. The driving behavior survey: Scale construction and validation. J. Anxiety Disord. 2011, 25, 96–105. [Google Scholar] [CrossRef]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Ahmad Basri, M.A.F.; Wan Ismail, W.S.; Kamal Nor, N.; Mohd Tohit, N.; Ahmad, M.N.; Mohamad Aun, N.S.; Mohd Daud, T.I. Validation of key components in designing a social skills training content using virtual reality for high functioning autism youth—A Fuzzy Delphi method. PLoS ONE 2024, 19, e0301517. [Google Scholar] [CrossRef]
- Mühlberger, A.; Bülthoff, H.H.; Wiedemann, G.; Pauli, P. Virtual reality for the psychophysiological assessment of phobic fear: Responses during virtual tunnel driving. Psychol. Assess. 2007, 19, 340. [Google Scholar] [CrossRef]
- Wald, J.; Taylor, S. Efficacy of virtual reality exposure therapy to treat driving phobia: A case report. J. Behav. Ther. Exp. Psychiatry 2000, 31, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Emery, G.; Greenberg, R.L. Anxiety Disorders and Phobias: A Cognitive Perspective; Basic Books/Hachette Book Group: New York, NY, USA, 2005. [Google Scholar]
- Bados López, A. Trastorno de Ansiedad Generalizada: Naturaleza, Evaluación y Tratamiento; Universitat de Barcelona, Facultad de Psicología: Barcelona, Spain, 2006. [Google Scholar]
- Shafran, R.; Cooper, Z.; Fairburn, C.G. Clinical perfectionism: A cognitive–behavioural analysis. Behav. Res. Ther. 2002, 40, 773–791. [Google Scholar] [CrossRef]
- Alden, L.E.; Taylor, C.T. Interpersonal processes in social phobia. Clin. Psychol. Rev. 2004, 24, 857–882. [Google Scholar] [CrossRef] [PubMed]
- Bögels, S.; Lamers, C. The causal role of self-awareness in blushing-anxious, socially-anxious and social phobics individuals. Behav. Res. Ther. 2002, 40, 1367–1384. [Google Scholar] [CrossRef]
- Robichaud, M.; Koerner, N.; Dugas, M.J. Cognitive Behavioral Treatment for Generalized Anxiety Disorder: From Science to Practice; Routledge: Oxfordshire, UK, 2019. [Google Scholar]
- Linehan, M. Cognitive-Behavioral Treatment of Borderline Personality Disorder; Guilford Press: New York, NY, USA, 1993. [Google Scholar]
- Foa, E.B.; Kozak, M.J. Emotional processing of fear: Exposure to corrective information. Psychol. Bull. 1986, 99, 20. [Google Scholar] [CrossRef]
- Cummings, J.J.; Bailenson, J.N. How immersive is enough? A meta-analysis of the effect of immersive technology on user presence. Media Psychol. 2016, 19, 272–309. [Google Scholar] [CrossRef]
- Emmelkamp, P.M.; Meyerbröker, K. Virtual reality therapy in mental health. Annu. Rev. Clin. Psychol. 2021, 17, 495–519. [Google Scholar] [CrossRef]
- Wolpe, J. The Practice of Behavior Therapy; Pergamon Press: Oxford, UK, 1990. [Google Scholar]
- Taylor, J.E.; Deane, F.P. Acquisition and severity of driving-related fears. Behav. Res. Ther. 1999, 37, 435–449. [Google Scholar] [CrossRef]
- Wiederhold, B.K.; Wiederhold, M.D. Virtual reality therapy combined with physiological monitoring provides effective treatment, with objective metrics, for post-traumatic stress disorder. Expert Rev. Med. Devices 2025, 22, 117–119. [Google Scholar] [CrossRef]
- Triberti, S.; Sapone, C.; Riva, G. Being there but where? Sense of presence theory for virtual reality applications. Humanit. Soc. Sci. Commun. 2025, 12, 1–6. [Google Scholar] [CrossRef]
- Serdar, C.C.; Cihan, M.; Yücel, D.; Serdar, M.A. Sample size, power and effect size revisited: Simplified and practical approaches in pre-clinical, clinical and laboratory studies. Biochem. Medica 2021, 31, 27–53. [Google Scholar] [CrossRef] [PubMed]
- Albers, C.; Lakens, D. When power analyses based on pilot data are biased: Inaccurate effect size estimators and follow-up bias. J. Exp. Soc. Psychol. 2018, 74, 187–195. [Google Scholar] [CrossRef]
- van Loenen, I.; Scholten, W.; Muntingh, A.; Smit, J.; Batelaan, N. The effectiveness of virtual reality exposure–based cognitive behavioral therapy for severe anxiety disorders, obsessive-compulsive disorder, and posttraumatic stress disorder: Meta-analysis. J. Med. Internet Res. 2022, 24, e26736. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).