Abstract
The case report presents an interdisciplinary treatment of a 65-year-old patient in whom an improper zirconium oxide-based prosthetic crown on tooth 21 resulted in occlusal trauma, causing displacement and extrusion of the tooth as well as its increased mobility to the second degree according to the Miller scale. The change in the position of tooth 21 led to the displacement of the teeth in the lower arch. The traumatic occlusion was eliminated with a short clear aligner treatment of fourteen aligners (seven basic and seven additional) of both arches followed by aligner retention. The treatment lasted 140 days. A clinical improvement in the periodontal condition and long-term increased stabilization of the loose tooth was obtained. After one year of retention, the tooth is still stable, and no sign of periodontal disease or recurrence of the occlusal trauma is noticeable.
1. Introduction
Pathological teeth migration, as well as their increased mobility, widening of the periodontal space, possible bone resorption and pain are some of the most common symptoms and signs of occlusal trauma [1]. In addition to the aesthetic issue, patients report functional problems that make it impossible to perform physiological activities such as biting food and correct articulation [2]. Occlusal injury (traumatic occlusion, occlusal disease) is a set of very small changes, often microscopic or sub-microscopic, manifested by a periodic and reversible increase in tooth (teeth) mobility [3]. These are adaptive or pathological changes in the periodontium resulting from the occlusal forces generated by the masticatory muscles [3]. Occlusal trauma is the damage to periodontal tissues caused by occlusal forces, and the entire occlusion that leads to periodontal damage is called traumatic occlusion [4]. Depending on the duration of the forces, occlusal injury can be classified as chronic or acute. Chronic occlusal trauma results in decreased bone density and widening of the periodontal space near the crown or along the entire length of the root, which causes an increase in teeth mobility and fremitus—i.e., noticeable or palpable small movements of the tooth when traumatic forces are applied to it [5,6,7].
The changes occurring in the periodontium in the case of occlusal trauma are histopathologically identical and independent of the type of traumatic occlusion. The most important difference concerns the resistance of the tooth/teeth and periodontal tissues to occlusal loads occurring in the oral cavity. The most important difference concerns destructive changes in the periodontium [2,8]. Depending on the direction and magnitude of the applied forces, occlusal injury causes tension and pressure. In the pressure zone, bone resorption, root cement resorption or hyalinization, periodontal fibre necrosis, increased vascular permeability, microhaemorrhage and vascular thrombosis occur. In the tension zone, if there is no inflammation, a new alveolar bone develops. Cement apposition and periodontal fibre elongation may sometimes occur [7]. After the cessation of the pathological forces, periodontal repair or regeneration is possible [9]. Physiologically occurring occlusal forces, even small ones, can have a destructive effect on the periodontium if it is reduced as a result of periodontal disease [2,10].
In clinical practice, the effects of traumatic occlusion are much more common in the anterior segment of the upper dental arch, especially in cases of loss of posterior tooth support [2,8]. The most characteristic manifestation of traumatic occlusion includes pathologic tooth migration (PTM), and the maxillary incisors are considered the most vulnerable to it. Depending on the research carried out, the incidence of PTM ranges from 30.3% to 55.8% in patients with periodontitis [11,12]. The specificity of the position of the upper incisors, for example, limited contacts on the proximal surfaces with the adjacent teeth, the absence of contacts or largely limited occlusal contacts with the incisors in the mandible, may cause their increased susceptibility to pathologic migration manifested by the lengthening of the clinical crown of the tooth/teeth [13].
Given the current standards in dental treatment aimed at reducing tooth extraction to the minimum, dentists face the challenge of preserving the patient’s natural teeth for as long as possible [14].
In order to eliminate traumatic occlusion, it is possible to apply orthodontic treatment—e.g., by using conventional fixed appliances or aligners [15]. Orthodontic treatment is aimed at improving the position of the tooth/teeth, for example, by the intrusion of elongated incisors, reduction of diastemas caused by tooth fanning, and removal of premature occlusal contacts and occlusal obstructions [12].
Since orthodontic treatment can be an effective method for treating both primary and secondary occlusal trauma, it should be planned to take into account periodontal condition, adjusting the biomechanics of tooth movement to the current state of supporting tissues. The use of excessive force during orthodontic tooth movement may cause further destruction of the periodontium [16,17,18]. In primary occlusal trauma, in the absence of concomitant inflammation, treatment may lead to the reconstruction of the lost bone tissue [10].
This case report follows the CARE Guidelines.
2. Case Report
A 65-year-old female patient consulted an orthodontist about the possibility of changing the position of the left upper central incisor, which was in a vestibular position in relation to the rest of the teeth. Initial photos of the patient are presented in Figure 1. Tooth 21 was endodontically treated for pulpitis after a childhood injury. Due to the weakening of the tooth’s hard tissues and the aesthetic issue, the crown of the tooth was many times sealed with different adhesive materials that no longer fulfil their function. In 2010, a crown was made of zirconium oxide, but according to the patient, it was not properly modelled on the palatal surface. Damage to the palatal surface of the crown cemented in the patient’s mouth indicated attempts to improve occlusal contacts by grinding porcelain. Examination of the occlusal contacts in maximal intercuspation showed the presence of dominant contacts on the posterior teeth and teeth 31, 32 and 21 (Figure 2).

Figure 1.
Initial photos of the patient.
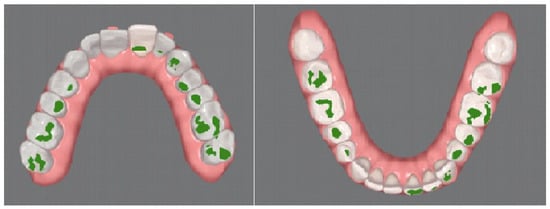
Figure 2.
Occlusal contacts before treatment.
The porcelain crown on tooth 21 was not modelled correctly, which resulted in chronic traumatic occlusion and atrophy of the vestibular lamella of the maxillary alveolar process in the vicinity of this tooth. Based on the history and clinical examination, no other causes were identified that could contribute to the loss of bone tissue in the area of tooth 21. The influence of such local factors as leakage or recontouring of the prosthetic crown in the area of the tooth neck, root caries, the presence of bacterial plaque and inflammation of the gums or periodontium, as well as general factors such as smoking, general diseases, morphology results and vitamin D concentration were taken into account. These parameters were regularly monitored in the patient due to the history of cancer and chemo- and radiotherapy. For this reason, it was decided to reduce the X-ray dose as much as possible and CBCT was abandoned, and the diagnosis was made on the basis of intraoral examination, scan and pantomogram analysis. The schedule of visits is presented in Figure 3.
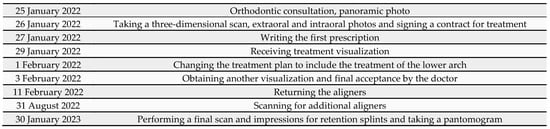
Figure 3.
Timeline.
A three-dimensional iTero scan (iTero Element, Align Technology, San Jose, CA, USA), extraoral and intraoral photos using the dedicated application Invisalign Practice App (Align Technology, San Jose, CA, USA) as well as a pantomogram were taken during the visit.
The intraoral examination showed numerous porcelain restorations, including an implant, which excluded the possibility of orthodontic treatment with a fixed appliance—due to the difficult or sometimes impossible to obtain adhesion of the brackets to the crowns. The mobility of the tooth was a problem, which made eating difficult. The history did not reveal the presence of factors contributing to periodontitis, such as smoking, diabetes, stress and obesity. Current general blood tests presented by the patient were normal (morphology and vitamin D3 level). The periodontal examination showed no pockets deeper than 4 mm (measured with a periodontal probe scaled every 1 mm at six measurement points around each tooth). There was also no omission of the implant during treatment with the continuous arch method and no bleeding on probing (BOP). The modified Sulcus Bleeding Index (mSBI) was also 0. A very good level of oral hygiene was observed during treatment—20% according to the Approximal Plaque Index (API). Tooth 21 showed the second degree of mobility in the three-degree Miller Index scale—that is, vestibule-oral cavity proper mobility not exceeding 1 mm. The dental X-ray showed bone loss along ½ of the length of the root, except for the mesial surface where the bone level was normal. The tooth underwent endodontic treatment in the past—the X-ray image showed a partially filled canal without periapical changes. Clinical attachment loss (CAL) on the labial surface was 3 mm and the periodontal probing depth (PPD) was 4 mm. Tooth 21 and the adjacent tooth 22 were covered with zirconium oxide crowns. The patient also had a perfectly functioning dental implant in position 14. The patient did not consent to the CBCT examination. The diagnosis was based on an intraoral examination, scan, dental and panoramic radiographs as well as intra- and extraoral images.
Based on the diagnosis and analysis of the obtained data, the following treatment plan was proposed:
- Hygienic preparation, short orthodontic treatment with small forces and then stabilization of the effects. Due to horizontal bone atrophy, bone regeneration procedures were not planned.
- Pretreatment occlusion scan using the iTeroTM 5.0 scanner, extracted into OrthoCAD 5.9.1.50 software (Align Technology, San Jose, CA, USA) (Figure 4), extra- and intraoral images taken with the Invisalign Practice App (Align Technology, San Jose, CA, USA) and pantomogram (Figure 5). Based on the iTeroTM 3D scan (Align Technology, San Jose, CA, USA) and occlusal examination, it was decided to use the Invisalign® system (Align Technology, San Jose, CA, USA) with the Express 1 arch subtype—the shortest possible treatment with seven aligners (and seven additional aligners) involving only the upper arch because the aim was to eliminate the occlusal injury of one tooth by its intrusion and a change of the anterior–posterior and mesiodistal inclination. The first treatment plan was performed using the ClinCheck 6.0 software (Align Technology, San Jose, CA, USA), which assumed movements of tooth 21—the main movement was a palatal inclination of the crown by 4.4 degrees, a distortion by 3.3 degrees and an intrusion by 0.4 mm (Figure 6). The analysis of this plan showed that it was impossible to eliminate the traumatic occlusion when changing the position of only one tooth in the arch (Figure 7)—the analysis showed numerous abnormal occlusal contacts.
 Figure 4. Pretreatment occlusion scan performed using the iTeroTM 5.0 scanner, extracted into OrthoCAD 5.9.1.50 software: extraoral and intraoral images.
Figure 4. Pretreatment occlusion scan performed using the iTeroTM 5.0 scanner, extracted into OrthoCAD 5.9.1.50 software: extraoral and intraoral images. Figure 5. Pantomogram—visible porcelain restorations and an implant in area 14.
Figure 5. Pantomogram—visible porcelain restorations and an implant in area 14.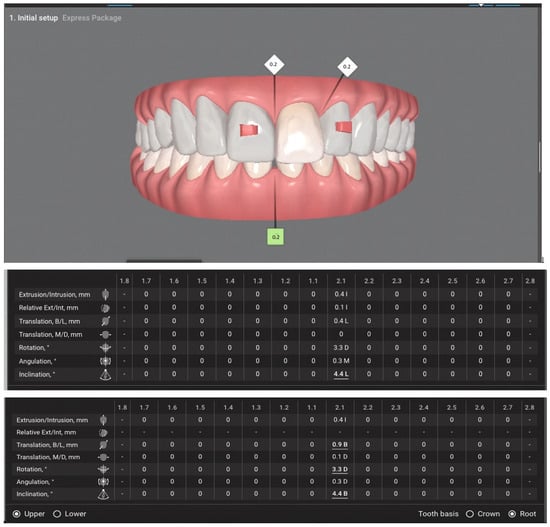 Figure 6. Foreground ClinCheck 6.0—only the upper arch was planned to be treated with clear aligners—insufficient to eliminate occlusal trauma. The numbers in the diamanond are decimals and indicate 0.2 mm. The numbers in the tables are expressed in milimeters (mm) and degrees (°). I—intrusion, L—lingual, D—distal, M—mesial. The underlined numbers are to most extensive movements of the tooth—of all the presented movements.
Figure 6. Foreground ClinCheck 6.0—only the upper arch was planned to be treated with clear aligners—insufficient to eliminate occlusal trauma. The numbers in the diamanond are decimals and indicate 0.2 mm. The numbers in the tables are expressed in milimeters (mm) and degrees (°). I—intrusion, L—lingual, D—distal, M—mesial. The underlined numbers are to most extensive movements of the tooth—of all the presented movements.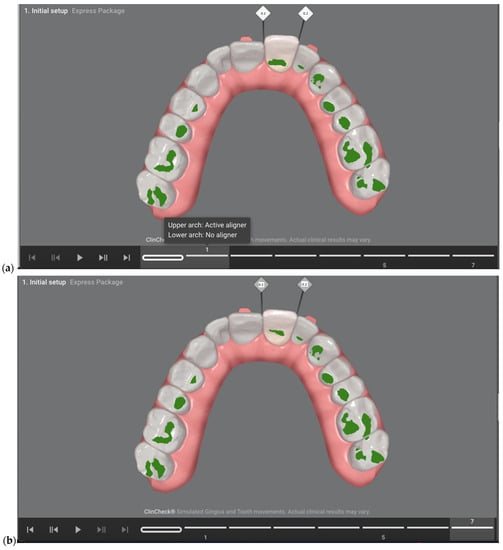 Figure 7. (a) Occlusal contacts in the upper arch before starting treatment—according to the first treatment plan; (b) occlusal contacts in the upper arch after applying 7 aligners—according to the first treatment plan. The numbers in the diamanond are decimals and indicate 0.2 mm.
Figure 7. (a) Occlusal contacts in the upper arch before starting treatment—according to the first treatment plan; (b) occlusal contacts in the upper arch after applying 7 aligners—according to the first treatment plan. The numbers in the diamanond are decimals and indicate 0.2 mm.
For this reason, the plan was changed, extending the orthodontic treatment to include the lower arch—a significant intrusion of the lower incisors and canines from 0.5 mm to 1.4 mm, distorotation up to 9.3 degrees and lingual inclination up to 5.5 degrees were planned. Translational axial movements and isolated root movements were also planned, including even 5-degree lingual torque movements (Figure 8a,b). The main focus was on the movements of the lower teeth due to the need to minimize the inevitable resorption of the root apex of tooth 21 (Figure 8c,d).
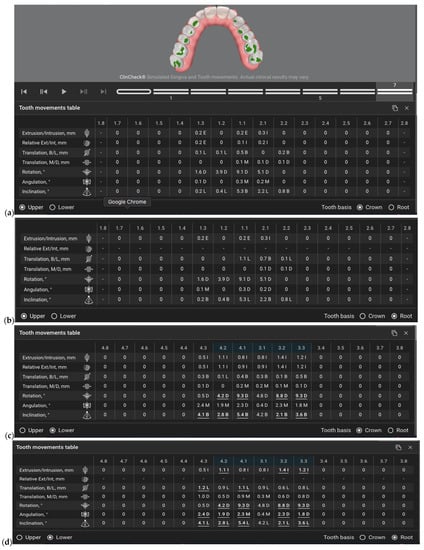
Figure 8.
ClinCheck of the second treatment plan. (a) presents the movements of the crowns in the upper arch, (b) presents the movements of the roots in the upper arch (c) presents the movements of the crowns in the lower arch (d) presents the movements of the roots in the lower arch. The numbers in the tables are expressed in milimeters (mm) and degrees (°). I—intrusion, L—lingual, D—distal, M—mesial. The underlined numbers are to most extensive movements of the tooth—of all the presented movements.
- Movements of tooth crowns in the lower arch. Visible leading moves tooth no. 4.3 lingual inclination, distorotation, lingual translation; 4.2 distorotation, lingual inclination, intrusion; 4.1 lingual inclination, lingual translation; 3.2 lingual inclination and intrusion; 3.3 lingual inclination, distorotation, distal angulation, intrusion.
- Figure 8. (a) Movements of tooth crowns in the upper arch. Visible leading moves, 1.3—distortion, 1.1—distortion and buccal inclination, 2.1 distortion. (b) Movements of tooth roots in the upper arch. Leading movements tooth no. 1.3 distorotation, 1.2 distorotation, 1.1 distorotation and lingual inclination, 2.1 buccal inclination (c).
- Figure 8. Movements of tooth crowns in the lower arch. Visible leading moves tooth no. 43 buccal inclination, 4.2 distorotation and buccal inclination, 3.2 distorotation, buccal inclination, z. 3.3 distorotation and buccal inclination.
- Figure 8. Movements of tooth crowns in the lower arch. Visible leading moves tooth no. 43 buccal inclination, 4.2 distorotation and buccal inclination, 3.2 distorotation, buccal inclination, z. 3.3 distorotation and buccal inclination.
The patient wore the aligners 22 h a day, changing each aligner every 10 days. In the case of patients with a reduced periodontal bone level, tooth movements in the aligners should be halved, i.e., each aligner affects the teeth half as much as during orthodontic treatment in the case of a healthy periodontium.
After using seven aligners, the patient was scanned again to continue treatment with the use of another seven aligners in order to achieve the best possible treatment results. The occlusion after the first part of the treatment (after the first seven aligners) is shown in Figure 9a,b. No occlusal overloads on the upper incisors are visible; thus, therapeutic success was achieved.
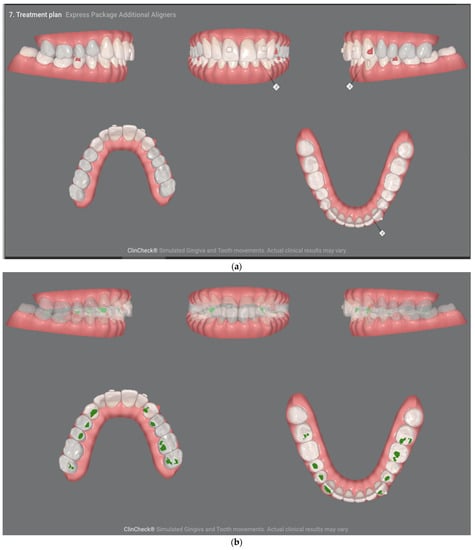
Figure 9.
(a) Occlusal condition before wearing additional aligners. (b) No occlusal overloads on the incisors are visible; thus, therapeutic success was achieved.
Subsequent aligners were used to calibrate the occlusion and obtain the aesthetic effect.
After one year of retention, the tooth is still stable, and no signs of periodontal disease or recurrence of the occlusal trauma are noticeable.
The final treatment effect is shown in Figure 10a,b.
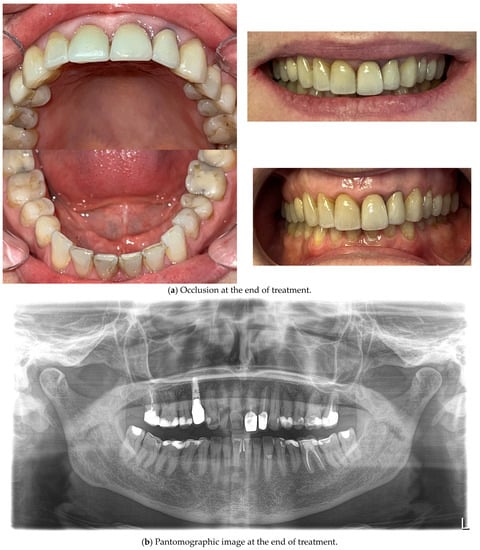
Figure 10.
The outcome of the clear aligner treatment in photos, scans and X-rays.
Periodontal status and oral hygiene were regularly monitored during treatment. Professional teeth cleaning was performed every 3 months. After obtaining the correct position of the teeth, thermoformable splint retention treatment was applied and the occlusion was rechecked for possible traumatic nodes. There were improvements in tooth stabilization (mobility of the first degree on the Miller scale) and the position of the connective tissue attachment on the labial surface—CAL—2 mm and PPD also 2 mm. The patient was not referred for re-endodontic treatment of the tooth since the previous root canal treatment was surely carried out according to the most modern standards at that time—under a microscope, filled with liquid gutta-percha—the gaps in the canal visible on the X-ray are not due to incomplete filling—the canal was obliterated, probably due to tooth trauma in childhood and the slow death of the pulp inside the tooth.
Patient Perspective
The patient reported concern about her upper central incisor, which protruded more and more with every bite of harder food, to such an extent that she was afraid to bite for fear of losing it. In previous years, the patient reported this problem to her dentist. The doctor, wanting to improve the occlusal conditions, ground the palatal surface of the crown and the enamel surface of the opposing tooth in order to eliminate premature contact. The patient did not report any bleeding of the gum or the tooth, she did not feel hypersensitivity to biting, changes in temperature or flavours. She only noticed that the tooth had recently leaned out a lot and was mobile. The patient was surprised and astonished by the proposal of clear aligner treatment—she did not think that in her case and at her age this form of treatment could be effective. She was also afraid that in the case of orthodontic treatment, she would lose the loose tooth. The treatment process itself was perceived by the patient as very comfortable, which she emphasized a lot, evaluating the treatment as painless and comfortable. She wore the aligners very conscientiously and systematically and followed all recommendations. The only thing she noticed was quite frequent damage to the mucous membrane, due to irritation by the edges of aligners—she reported this as a difficulty in regular wearing.
3. Discussion
In the presented case, the patient experienced primary occlusal injury resulting from iatrogenic prosthetic treatment. The crown, which was not adjusted to the occlusion, triggered excessive occlusal forces on the initially healthy periodontium, leading to bone remodelling, partial bone loss and a change in the tooth position. In addition to the aesthetic issue, this condition could consequently lead to tooth loss [5,17]. Occlusal injury requires a complex treatment procedure. Moreover, different but equally effective methods can be proposed for the same diagnosis. Orthodontic treatment is considered to be the basic method for preventing and treating traumatic occlusion [7,17]. Orthodontic treatment in adult patients might be hindered by several problems, such as little time for regular dental visits and periodontal diseases [18]. In the described case, orthodontic treatment was chosen as the least invasive and non-burdensome for the patient. In addition, the choice of clear aligner treatment was dictated by the presence of ceramic-coated crowns on the patient’s own teeth and the implant-supported crown. This condition makes it difficult to apply treatment with a fixed appliance. The lack of periodontal inflammation and the patient’s very good hygiene made it possible to partially reverse the changes that had occurred in the periodontium. According to Shetty et al., perfect hygiene is a prerequisite for reversing the changes that have occurred in the periodontium [17]. The choice of clear aligner treatment in this case is also justified by the need to maintain perfect oral hygiene. Both periodontal status and the level of oral hygiene are better in patients using aligners compared to patients wearing fixed appliances [19]. Furthermore, the amount of periodontal pathogenic bacteria in these patients is lower [20,21]. Clear aligner treatment provides a therapeutic effect in a shorter time than fixed appliances and enables sequential and selective tooth movements [22]. Due to low and constant forces, it also reduces the risk of root resorption [23]. In the treatment of occlusal injury, an individualized approach and prompt treatment are required to prevent further tissue destruction [24]. After completing the treatment, patients with occlusal trauma use retention adapted to their individual needs [5].
Until recently, fixed appliances were the most commonly used conventional method of treatment in contemporary orthodontics [25]. Recent years have brought a significant increase in cases treated with aligners, which, thanks to continuous development and improvement, enable the treatment of most defects, even gnathic defects prepared for orthognathic treatment. However, as with any other treatment, orthodontic procedures can entail complications. Periodontal problems are one of the most commonly observed side effects associated with orthodontics [26]. These mainly include gingivitis, periodontitis and gingival recession [27]. However, the risks and complications associated with the treatment are significantly lower compared to other surgical or non-surgical interventions [28]. The presence of bacterial plaque is believed to be the most important factor in the onset, progression and recurrence of periodontal disease [29]. It has been established that, when domiciliary oral hygiene procedures are not followed properly, conventional braces retain more plaque, which promotes gingivitis. Actually, orthodontic retainers and ligatures may interfere with the effective removal of plaque, thus increasing the risk of gingivitis, which is especially dangerous in patients with reduced bone levels at the beginning of treatment. Additionally, some recently introduced compounds have been demonstrated to have a significant influence on the oral environment. Probiotics [30], lysates [31] and postbiotics [32] can modify clinical and microbiological parameters in periodontal patients, so these products should be considered in future clinical trials as adjuvants, and also during clear aligner therapy.
Bearing in mind the described case of the patient, attention should also be paid to the prosthetic restorations present in the oral cavity, which, in their iatrogenic preparation, caused irreversible changes in the periodontium. Occlusion recommendations for fixed prosthetic restorations, including crowns and bridges made on dental or implanted abutments, include the concept of mutually protected occlusion. Appropriate contact points on the molars and premolars stabilize the central occlusion, whereas the anterior teeth control protrusive and laterotrusive movements, leading to the disclusion of the side teeth during eccentric movements. Stable occlusal contacts on the posterior teeth allow for the relief of the anterior teeth that are not morphologically adapted to participate in the transmission of masticatory forces. In patients with periodontal diseases, progressive tooth loading is particularly important due to the reduced periodontium of the anterior teeth [33]. The proper position of the front teeth, and especially correct modelling of the crowns made on them, not only protect these teeth from overloading but also allows for the control of mandibular movements, enabling the proper activity of the temporomandibular joints and masticatory muscles and proper functioning of the stomatognathic system. Too steep positioning of the front teeth or incorrect modelling of their palatal surface may contribute not only to occlusal disorders—traumatic occlusion, but also to functional disorders of the masticatory system. Li A, Shao B, Chong DYR and Liu Z conducted research on the distribution of stresses occurring in the temporomandibular joint, taking into account the articular ligaments depending on the position of the incisors. Based on the study of 3D models of the maxilla and mandible positioned on the basis of cone-beam computed tomography and magnetic resonance imaging as well as the analysis of simulations in finite element models, they showed that in the group of patients, in whom the palatal surface of the incisors was excessively tilted towards the palate, there is an abnormal stress distribution, which is harmful to the temporomandibular joints [34].
The presented report is intended to show the possibility of treating a case that may not be qualified by a general dentist for orthodontic treatment in the first reflex and adding a clear aligner treatment might not be the first idea. As it is shown, the treatment has been an effective, long-term approach to the treatment of an elderly patient. The authors’, and at the same time the attending physician’s, main concern was the maintenance of the retention phase. The patient must remember about the retention splint, if she forgets about it for 2–3 days, she feels stress on the tooth that has previously been seriously displaced. This is, of course, a normal process after orthodontic treatment but the effects of the tooth being subjected to jiggling forces are the greatest threat in terms of orthodontic resorption of the already shortened root. As for the case report itself, the reacher X-ray documentation, including CBCT, should be provided. However, taking into account the process of treatment and diagnosis itself, it was sufficient for its use. It is also necessary to continue the check-up visits so that we can still ensure 100 per cent health success, which the authors consider lifelong maintenance of the patient’s tooth.
4. Conclusions
Occlusal trauma caused irreversible changes in the patient’s periodontium, which carried the risk of losing the improperly loaded incisor.
It was not possible to eliminate occlusal trauma locally—by fitting fillings or prosthetic reconstruction, it was necessary to consider orthodontic treatment—regardless of age.
Clear aligner treatment proved to be an effective treatment in the described case. Three-dimensional scans allowed us to precisely assess the occlusion, calculate the exact points of abnormal contact and obtain measurements to the tenth of a millimetre necessary to eliminate it.
Author Contributions
Conceptualization, M.M.; methodology, M.M.; software, M.M.; validation, R.S., M.T. and L.S.-S.; formal analysis, K.W.; investigation, M.M.; resources, A.B.-Z.; data curation, M.M.; writing—original draft preparation, M.M., R.S., M.T. and A.B.-Z.; writing—review and editing, M.M.; visualization, K.W.; supervision, K.W. and L.S.-S.; project administration, M.M.; funding acquisition, M.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
All the data of the described case is available online on the dr Monika Machoy Invisalign Doctor Site. If interested please contact.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Campiño, J.I.; Ríos, C.C.; Rodriguez-Medina, C.; Botero, J.E. Association between traumatic occlusal forces and periodontitis: A systematic review. J. Int. Acad. Periodontol. 2019, 21, 148–158. [Google Scholar] [PubMed]
- Thierens, L.A.M.; Van de Velde, T.; De Pauw, G.A.M. Orthodontic Management of a Migrated Maxillary Central Incisor with a Secondary Occlusal Trauma. Clin. Adv. Periodontics 2020, 10, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Sutthiboonyapan, P.; Wang, H.L. Occlusal Splints and Periodontal/Implant Therapy. J. Int. Acad. Periodontol. 2019, 21, 45–50. [Google Scholar] [PubMed]
- Saravanan, R.; Babu, P.J.; Rajakumar, P. Trauma from occlusion—An orthodontist’s perspective. J. Indian Soc. Periodontol. 2010, 14, 144–145. [Google Scholar] [CrossRef] [PubMed]
- Klasyfikacja Chorób Przyzębia Oraz Chorób Wokół Implantów. 2017. Available online: http://webcache.googleusercontent.com/search?q=cache:DiDo9t3zUT0J:perio.org.pl/europerio-9-nowa-klasyfikacja-chorob-przyzebia/&cd=19&hl=pl&ct=clnk&gl=pl (accessed on 15 August 2023).
- Amaral, M.F.; Poi, W.R.; Debortoli, C.V.L.; Panzarini, S.R.; Brandini, D.A. The influence of traumatic occlusion on the repair process for teeth following subluxation. Dent. Traumatol. 2017, 33, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Caton, J.G. Occlusal trauma and excessive occlusal forces: Narrative review, case definitions, and diagnostic considerations. J. Periodontol. 2018, 89 (Suppl. S1), S214–S222. [Google Scholar] [CrossRef]
- Górska, R.; Stawicka-Wychowańska, M.; Nędzi-Góra, M. Nowa klasyfikacja chorób przyzębia: Wrodzone i nabyte czynniki miejscowe oraz deformacje śluzówkowo—Dziąsłowe modyfikujące przebieg choroby przyzębia. Stomat. Współ. 2001, 8, 21–25. [Google Scholar]
- Soi, S.; Bains, V.K.; Srivastava, R.; Madan, R. Comparative evaluation of improvement in periodontal and glycemic health status of type 2 diabetes mellitus patients after scaling and root planing with or without adjunctive use of diode laser. Lasers Med. Sci. 2021, 36, 1307–1315. [Google Scholar] [CrossRef]
- Borges, R.N.; Arantes, B.M.; Vieira, D.F.; Guedes, O.A.; Estrela, C. Occlusal adjustment in the treatment of primary traumatic injury. Stomatos 2011, 17, 71–74. [Google Scholar]
- Zafar, K.; Nazeer, M.R.; Ghafoor, R. Interdisciplinary management of gingival recession and pathologic teeth migration—Revisiting dental aesthetics. J. Pak. Med. Assoc. 2019, 69, 1385–1389. [Google Scholar]
- Zasčiurinskienė, E.; Rastokaitė, L.; Lindsten, R.; Basevičienė, N.; Šidlauskas, A. Malocclusions, pathologic tooth migration, and the need for orthodontic treatment in subjects with stage III-IV periodontitis. A cross-sectional study. Eur. J. Orthod. 2023, 45, 418–429. [Google Scholar] [CrossRef] [PubMed]
- Rzeszut, A.; Kawala, B.; Szulc, M.; Ziętek, M. Patologiczna migracja zębów siecznych szczęki a stan tkanek przyzębia. Dent. Med. Probl. Off. Organ Wroc. Med. Univ. Pol. Stomatol. Assoc. 2006, 43, 245–251. [Google Scholar]
- Sarafidou, K.; Lazaridi, I.; Gotsis, S.; Kirmanidou, Y.; Vasilaki, D.; Hirayama, H.; Michalakis, K. Tooth preservation vs. extraction and implant placement in periodontally compromised patients: A systematic review and analysis of studies. J. Prosthodont. 2022, 31, e87–e99. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Chen, X.; Sun, L.; Zhao, B.; Liu, Y. Sequential soft- and hard-tissue augmentation after clear aligner-mediated adjustment of traumatic occlusion: A case report. J. Am. Dent. Assoc. 2022, 153, 572–581.e1. [Google Scholar] [CrossRef] [PubMed]
- Re, S.; Corrente, G.; Abundo, R.; Cardaropoli, D. The use of orthodontic intrusive movement to reduce infrabony pockets in adult periodontal patients: A case report. Int. J. Periodontics Restor. Dent. 2002, 22, 365–371. [Google Scholar]
- Shetty, P.; Hegde, S.; Chelkar, S.; Chaturvedi, R.; Pochhi, S.; Shrivastava, A.; Lakshmi, D.; Mukherjee, S.; Bajaj, P.; Raza, S.A. Perspective Chapter: Trauma from Occlusion—Practical Management Guidelines. In Dental Trauma and Adverse Oral Conditions; IntechOpen: Rijeka, Croatia, 2022. [Google Scholar] [CrossRef]
- Meme’, L.; Gallusi, G.; Coli, G.; Strappa, E.; Bambini, F.; Sampalmieri, F. Photobiomodulation to Reduce Orthodontic Treatment Time in Adults: A Historical Prospective Study. Appl. Sci. 2022, 12, 11532. [Google Scholar] [CrossRef]
- Partouche, A.J.D.; Castro, F.; Baptista, A.S.; Costa, L.G.; Fernandes, J.C.H.; Fernandes, G.V.O. Effects of Multibracket Orthodontic Treatment versus Clear Aligners on Periodontal Health: An Integrative Review. Dent. J. 2022, 10, 177. [Google Scholar] [CrossRef] [PubMed]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Periodontal health during clear aligners treatment: A systematic review. Eur. J. Orthod. 2015, 37, 539–543. [Google Scholar] [CrossRef]
- Ke, Y.; Zhu, Y.; Zhu, M. A comparison of treatment effectiveness between clear aligner and fixed appliance therapies. BMC Oral. Health 2019, 19, 24. [Google Scholar] [CrossRef]
- Fang, X.; Qi, R.; Liu, C. Root resorption in orthodontic treatment with clear aligners: A systematic review and meta-analysis. Orthod. Craniofacial Res. 2019, 22, 259–269. [Google Scholar] [CrossRef]
- Kartha, S.; Vellore, K.P.; Challa, S.K.; Vallu, R.; Pusuluri, S. Traumatogenic Occlusion in a Pediatric Dental Patient: A Case Report. Int. J. Clin. Pediatr. Dent. 2022, 15, 222. [Google Scholar] [CrossRef] [PubMed]
- Sandic, M.Z.; Popovic, B.; Carkic, J.; Nikolic, N.; Glisic, B. Changes in subgingival microflora after placement and removal of fixed orthodontic appliances. Srp. Arh. Celok. Lek. 2014, 142, 301–305. [Google Scholar] [CrossRef] [PubMed]
- Dannan, A. An update on periodontic-orthodontic interrelationships. J. Indian Soc. Periodontol. 2010, 14, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Preoteasa, C.T.; Ionescu, E.; Preoteasa, E. Risks and complications associated with orthodontic treatment. In Orthodontics—Basic Aspects and Clinical Considerations, 1st ed.; Bourzgui, F., Ed.; IntechOpen: Rijeka, Crotia, 2012; pp. 403–428. [Google Scholar]
- Genco, R.J.; Borgnakke, W.S. Risk factors for periodontal disease. Periodontology 2000, 62, 59–94. [Google Scholar] [CrossRef] [PubMed]
- Passanezi, E.; Sant’Ana, A.C.; Damante, C.A. Occlusal trauma and mucositis or peri-implantitis? J. Am. Dent. Assoc. 2017, 148, 106–112. [Google Scholar] [CrossRef]
- Meynardi, F.; Lauritano, D.; Pasqualini, M.E.; Rossi, F.; Grivet-Brancot, L.; Comola, G.; Dal Carlo, L.; Moglioni, E.; Zampetti, P. The importance of occlusal trauma in the primary etiology of periodontal disease. J. Biol. Regul. Homeost. Agents 2018, 32 (Suppl. S1), 27–34. [Google Scholar] [PubMed]
- Butera, A.; Pascadopoli, M.; Pellegrini, M.; Gallo, S.; Zampetti, P.; Scribante, A. Oral Microbiota in Patients with Peri-Implant Disease: A Narrative Review. Appl. Sci. 2022, 12, 3250. [Google Scholar] [CrossRef]
- Vale, G.C.; Mayer, M.P.A. Effect of probiotic Lactobacillus rhamnosus by-products on gingival epithelial cells challenged with Porphyromonas gingivalis. Arch. Oral. Biol. 2021, 128, 105174. [Google Scholar] [CrossRef]
- Butera, A.; Pascadopoli, M.; Pellegrini, M.; Gallo, S.; Zampetti, P.; Cuggia, G.; Scribante, A. Domiciliary Use of Chlorhexidine vs. Postbiotic Gels in Patients with Peri-Implant Mucositis: A Split-Mouth Randomized Clinical Trial. Appl. Sci. 2022, 12, 2800. [Google Scholar] [CrossRef]
- Sheridan, R.A.; Decker, A.M.; Plonka, A.B.; Wang, H.L. The Role of Occlusion in Implant Therapy: A Comprehensive Updated Review. Implant. Dent. 2016, 25, 829–838. [Google Scholar] [CrossRef]
- Li, A.; Chong, D.Y.R.; Shao, B.; Liu, Z. An Improved Finite Element Model of Temporomandibular Joint in Maxillofacial System: Experimental Validation. Ann. Biomed. Eng. 2023. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).