Abstract
Aggregatibacter actinomycetemcomitans is implicated in the etiology of periodontitis that affects adolescents. The monitoring and mapping of the geographic dissemination pattern of JP2 and non-JP2 genotypes of A. actinomycetemcomitans are of interest. In Africa, the highly leukotoxic JP2 genotype is known to be prevalent, particularly in north-west Africa. The aims of this study were to determine the prevalence of JP2 and non-JP2 genotypes and investigate the oral hygiene practices among adolescents living in Maasai Mara, Kenya. A total of 284 adolescents (mean age: 15.0 yrs; SD 1.1) were interviewed regarding their age, gender, medical history, and oral hygiene practice, and the number of teeth present was recorded. One subgingival pooled plaque sample from all the first molars of each participant was analyzed by conventional PCR. The mean number of permanent teeth present was 27.9 (SD: 2.0; range: 22–32; 95% CI: 27.7–28.1). Sixteen (5.6%) and two (0.7%) adolescents were positive for non-JP2 and JP2 genotypes, respectively. For the vast majority of the adolescents, the use of a toothbrush (99.3%) and toothpaste (80.1%), as well as some kind of toothpick (>60.2%), were part of their oral hygiene practice, with dental floss (0.4%) and/or mouth rinses (0.4%) rarely being used. We have, for the first time, identified Kenyan adolescents colonized with the JP2 genotype. The prevalence of the JP2 genotype of A. actinomycetemcomitans is low, a possible indicator that spreading through human migration from North and West Africa to East Africa is a rare occasion.
1. Introduction
Periodontitis frequently occurs in humans in African countries [1,2,3,4,5,6]. Among adolescents, much attention has been given to the oral bacterium, Aggregatibacter actinomycetemcomitans, due to its capacity to produce leukotoxin, an exotoxin that is able to kill important cells of the immune system and cause inflammation [7,8,9]. Among the numerous genotypes of A. actinomycetemcomitans, a highly leukotoxic genotype called JP2 has extensively been reported on [10,11,12]. Dahlén and co-workers [13] proposed that the JP2 genotype of A. actinomycetemcomitans is the best-known example of a specific bacterial subtype with implications for periodontal disease. This JP2 genotype is characterized by a 530 base pair (bp) deletion in the promoter region of the leukotoxin gene operon, suggested to be responsible for the enhanced leukotoxin expression [12]. In particular, the highly leukotoxic JP2 genotype of A. actinomycetemcomitans has been strongly associated with the initiation of periodontal attachment loss in adolescents [2,4,14].
Although other genotypes of A. actinomycetemcomitans, other bacterial species, factors related to the host response, and other types of risk factors are associated with increased risk of the development of periodontitis in adolescents [15,16,17,18,19], it is important from a global perspective to understand the pattern of dissemination of the highly leukotoxic JP2 genotype of A. actinomycetemcomitans to be able to ensure infection control and, thereby, prevent the development of severe periodontitis in young individuals [20].
The JP2 genotype, with an estimated origin dating around 2400 years ago [10], is found to be highly conserved based on analyses of JP2 genotype strains collected over more than 20 years from individuals with geographically different origins and living across a wide geographically area. The mapping of the geographic occurrence of the JP2 genotype has revealed that its colonization is greatly connected to individuals of African descent, but has spread to other parts of the world, including Europe and North and South America [2,4,8,21,22,23,24,25]. Today, human migration from one part of the world to another is a frequent event [26].
As a consequence of the geographical dissemination of the highly leukotoxic JP2 genotype of A. actinomycetemcomitans, European and North and South American periodontitis patients are occasionally also found to be carriers [12,16,17,27,28]. Thus, JP2 genotype carriers with severe periodontitis might appear geographically widespread, and therefore this topic is relevant to clinicians all over the world. Despite the finding that the JP2 genotype of A. actinomycetemcomitans is less frequent in continents other than Africa, both individuals and migrants from the African continent as well as individuals not originating from African countries can be carriers of the JP2 genotype of A. actinomycetemcomitans [12,16,27,28,29,30]. Except for clear signs of a high prevalence of the JP2 genotype in North and West African countries, the dissemination of the JP2 genotype of A. actinomycetemcomitans to the remaining parts of the African continent is not known or has been very rarely examined and reported [31]. For example, in the East-African country Kenya, nothing is known concerning the potential presence of the highly leukotoxic JP2 genotype of A. actinomycetemcomitans. Interestingly, a genotype of A. actinomycetemcomitans, characterized by a 640 bp deletion in the promoter region of the leukotoxin gene operon and high leukotoxicity according to results obtained by the use of a leukotoxicity assay [17], has been detected in one individual living in Sweden with Ethiopian origin, yet nothing is known about its overall prevalence or geographic dissemination pattern [17,31]. Concerning the JP2 genotype of A. actinomycetemcomitans, our hypothesis is that it will not be found in the Kenyan adolescent population living in the fairly remote area of Kenya, called Maasai Mara.
The aims of the present study were to report on the prevalence of JP2 and non-JP2 genotypes of A. actinomycetemcomitans and oral hygiene practices among adolescents living in Maasai Mara, Kenya.
2. Results
2.1. Number of Maxillary and Mandibular Teeth Present in the Oral Cavity of Kenyan Adolescents
Among the 284 teenagers participating in the study, the overall mean number of permanent teeth present in the mouth was 27.9 (SD: 2.0; range: 22–32; 95% CI: 27.7–28.1). One teenager had only 11 permanent teeth and multiple primary teeth present (most likely due to delayed eruption) in the oral cavity, and this participant was therefore excluded from the calculation of the mean number of permanent teeth present. In Table 1, the complete distribution of clinically visible teeth as well as the absence of teeth in the upper and lower jaws according to tooth type is given.

Table 1.
The number of permanent and primary maxillary and mandibular teeth according to tooth type in 284 adolescents.
2.2. Prevalence of JP2 and Non-JP2 Genotypes of A. actinomycetemcomitans Among Adolescents Living in Maasai Mara
A total of 16 (5.6%) adolescents among the 284 participants in the present study were found to be positive for the non-JP2 genotype of A. actinomycetemcomitans. Only two (0.7%) participants out of the 284 adolescents were found to be positive for the JP2 genotype of A. actinomycetemcomitans (Figure 1). Clinical photos of one of the cases positive for the JP2 genotype of A. actinomycetemcomitans are shown in Figure 1.

Figure 1.
Clinical photos of an adolescent who tested positive for the JP2 genotype of A.actinomycetemcomitans (right view, frontal view, and left view, respectively). Red and swollen gingiva and irregular dental papillae are seen along the gum line.
Concerning the reproducibility of the A. actinomycetemcomitans findings in the respective samples of dental plaque, 12 out of the 284 (4.2%) individuals were sampled twice, with two of them testing positive for the non-JP2 genotype of A. actinomycetemcomitans at both sampling occasions (one of the non-JP2 genotype positive cases is illustrated in lanes 13–14; see Figure 2B). The other 10 samples were negative for A. actinomycetemcomitans at both sampling occasions, irrespective of genotype.
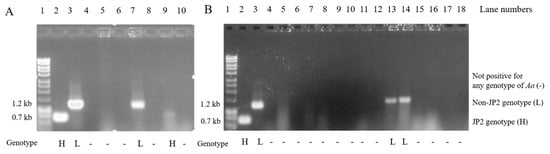
Figure 2.
Agarose gel analysis of DNA fragments amplified by conventional polymerase chain reaction (PCR) directly from subgingival dental plaque samples. (A) Lane 1: a molecular weight marker illustrating sizes of the PCR-amplified DNA fragments; lane 2: a highly leukotoxic (H) reference strains of JP2 genotype of A. actinomycetemcomitans strain, HK921; lane 3: a low leukotoxic (L) reference strains of the non-JP2 genotype of A. actinomycetemcomitans strain, HK1605; lanes 4–10 illustrate findings in dental plaque samples from Kenyan adolescents, among whom the subject in lane 7 was positive for the non-JP2 genotype of A. actinomycetemcomitans and the subject in lane 9 was positive for the JP2 genotype of A. actinomycetemcomitans. The sizes of the fragments can be assessed according to the molecular weight marker in lane 1. The A. actinomycetemcomitans strains were examined for the occurrence of a 530 bp deletion in the promoter region of the leukotoxin gene (H), or not having this 530 bp deletion, being a non-JP2 genotype (L), thus marked by (H) or (L). If there is no band in the lane, the sample was not positive for any A. actinomycetemcomitans strains (-), and (B) illustrates in lanes 13 and 14 two samples from the same patients (reproducibility samples), with both samples from the same patient being positive for the non-JP2 variant of A. actinomycetemcomitans. Lanes 15 and 16 are loaded also with two samples from the same patients (reproducibility samples), with both samples being negative for A. actinomycetemcomitans.
2.3. Answers to Questions on Oral Hygiene Tools and Hygiene Practices Used
The answers to the specific question raised on oral hygiene practice to the 284 Kenyan adolescents living in Maasai Mara are summarized in Table 2.

Table 2.
Answers to questions from interviewing the 284 Kenyan adolescents on their oral hygiene practices.
For the vast majority of the adolescents, the use of a toothbrush (99.3%) and toothpaste (80.1%), as well as some kind of toothpick (also called chewing stick or Mswaki) (>60.2%), was a part of their oral hygiene practice, whereas the use of dental floss and/or mouth rinse was extremely rare (0.4% and 0.4%, respectively) (Table 2). The majority of the adolescents brushed their teeth every day (99.3%), the vast majority in the morning (95.4%), and very few (0.7%) answered that they never brushed their teeth. A total of 209 (73.6%) reported brushing their teeth two to three times per day, 67 (23.6%) reported brushing once per day, 6 (2.1%) adolescents reported brushing less than once per day, and only two (0.7%) answered that they never brushed their teeth. In addition, toothpaste with fluoride was very often reported to be used (>80%). About two thirds of them reported using other things while cleaning their teeth—for example, small branches from trees and leaves or chewing sticks (Mswaki) (72.2%).
3. Discussion
In the current study, we report, for the first time, findings on the highly leukotoxic JP2 genotype of A. actinomycetemcomitans in adolescents living in Kenya. The findings are, however, rare in the adolescent population living in Maasai Mara, Kenya (below 1% carriers), but it is now clear that the highly leukotoxic JP2 genotype of A. actinomycetemcomitans is also present in Kenya.
The present research project was carried out in the Mara North Conservancy in Maasai Mara, a rural area of Kenya, where the Maasai Mara National Reserve is situated. In this area, although human–wildlife interaction combined with the interaction with the tourists visiting the National Reserve can be challenging to the indigenous Maasai population living there, this population still maintains their traditional life. It is probable that access to more information through the internet, computers, and television might, over time, increasingly lead to behavioral and lifestyle changes in the population. In addition, changes in the oral microbiome of the Maasai population are likely to occur in the future due to increasing interaction with visitors in the Maasai Mara National Reserve, as well as when some members of the community travel outside Maasai Mara.
Concerning the oral health practices of the adolescents living in Maasai Mara, this is of interest, given the reports from previous studies carried out in African countries which show that unconventional oral hygiene tools may be used, such as branches from trees, leaves from bushes, or chewing sticks [32,33]. The use of important and conventional oral hygiene tools such as toothbrushes, toothpaste, and toothpicks was, however, high. The number using traditional oral hygiene tools, such as twigs from specific trees, was high, despite also using commercial conventional tools. In various populations around the world, people live under different life circumstances, with different resources available to them and with different risks for the development of periodontitis. To be at the forefront of a potential need for the development of new, efficient oral hygiene practices, we need to know about the current oral hygiene practices employed. We then might be able to recommend or even develop new oral hygiene tools and preventive strategies for the future that are acceptable to the focus population. For example, plant materials may contain beneficial plant extracts that exert an anti-leukotoxic potential [32,33,34,35]. Recently, proanthocyanidins and epigallocatechin gallate of plant origin have been found to neutralize the effect of the A. actinomycetemcomitans leukotoxin [35,36,37].
The participants in our study came from the Mara North Conservancy from part of the Maasai population. The present study sample represents the Maasai living in Maasai Mara only. The Maasai population with its semi-nomadic lifestyle differs greatly from the Kenyan population in general. Thus, the results obtained in the present study may differ from the potential data and, thereby, research findings based on other parts of the Kenyan population.
The clinical examinations were carried out in classrooms at the participating schools and the lighting was of varying quality. It is not known precisely how this may have affected the results. However, the results are expected to have been minimally affected, if affected at all, by the working conditions and the available natural light sources, given that the recording of teeth present in the oral cavity was not demanding in terms of the requirement of the light source. Hence, these available conditions were judged as sufficient for fulfilling the requirements of the present study.
Concerning the prevalence of the JP2 and non-JP2 genotypes of A. actinomycetemcomitans, the methodology applied in the present study has been used in several previously published studies [2,10,11,33,38]. As previously reported, the prevalence of the JP2 genotype of A. actinomycetemcomitans is high in North and West Africa (up to 13% of the adolescent population is colonized with the highly leukotoxic genotype of A. actinomycetemcomitans) [2]. Further, in a cohort consisting of 180 young African Americans with and without localized aggressive periodontitis (with 60 being localized aggressive periodontitis patients, 60 healthy siblings, and 60 unrelated health controls) in North Florida, the occurrence of JP2 genotype-positive subjects was evident. Altogether, 90 JP2 genotype-positive subjects (50%) were found in that study [14]. In comparison to such findings, the observations of the JP2 genotype in the present Maasai population can still be considered as very rare (0.7%). It is unknown if the low prevalence of the JP2 genotype of A. actinomycetemcomitans in Maasai Mara is unique or a common characteristic of the whole Kenyan population. However, the very low level of dissemination of the JP2 genotype of A. actinomycetemcomitans to the Maasai Mara region in Kenya might be associated with the very limited migration from North and West Africa to Maasai Mara in East Africa.
The present study shows for the first time that a few adolescents from Maasai Mara, Kenya, are colonized with the highly leukotoxic JP2 genotype of A. actinomycetemcomitans. The prevalence of the JP2 genotype of A. actinomycetemcomitans is, however, low. This indicates that the human migration of populations from North and West Africa to Maasai Mara in East Africa and, thereby, the potential risk of transfer of the JP2 genotype of A. actinomycetemcomitans through close interpersonal contacts, is most likely low. Regarding oral hygiene practices, while the majority of the adolescents used commercial toothbrushes and toothpaste, more than 60% reported using small branches from trees, leaves, or the local chewing sticks (Mswaki) as other means of maintaining oral hygiene.
4. Materials and Methods
4.1. Study Population
The study was conducted in Maasai Mara, more specifically in Mara North Conservancy, Kenya. The study population consisted of 284 Kenyan teenagers (mean age: 15.0; SD 1.1; range 14–18 years) recruited from the four primary and one mixed secondary schools in the Mara North Conservancy, Maasai Mara, Narok County of Kenya, as previously reported by Kemoli and coworkers [39]. The study population was representative of the Mara North Conservatory of Maasai Mara and consisted of healthy adolescents present at school on the day of the examination. None of the participants reported having smoked previously nor being an active smoker at the time of the study (one missing answer out of a total of 284 respondents). None of the participants reported having diabetes (missing answers from three out of 284 participants).
The study consisted of a face-to-face interview using structured questionnaires, a clinical examination to record the presence of participants’ teeth in the oral cavity, the collection of dental plaque sample(s) from mesial sites of all permanent first molars, and finally, the intra-oral photographing of the dentition.
4.2. Face-to-Face Interview
Structured questionnaires were used to collect data on age, gender, medical history, and the use of oral hygiene tools according to procedures previously described [39].
4.3. Recording of the Presence of Maxillary and Mandibular Teeth in the Mouth
The recording of the teeth present in the oral cavity was performed, and teeth were recorded as present when either partly or fully erupted. Oral examinations, including inter-rater reliability testing, were conducted as previously reported [39]. A procedure including the recall of the subjects for traditional intra-reliability evaluation was not possible due to the limited working time at the research site. As part of the data collection procedure, intraoral photographs were taken for the right, left, and frontal perspectives of the teeth in occlusion.
4.4. Procedure for Collecting and Analyzing Dental Plaque Samples
The collection of dental plaque samples for conventional polymerase chain reaction (PCR) analysis was carried out in all participants with the help of sterilized disposable mouth mirrors and tweezers. The subgingival plaque sample of the oral microbiota was collected with paper points (one separate, autoclaved package per participant, including four paper points, size 40; TopDent®, Väsby, Sweden) inserted subgingivally in the gingival crevice for 10–15 s at the mesial aspect of all first permanent molars. If one or more of these permanent first molars were not present, no sample from this/these quadrant(s) was included in the pooled plaque sample. The paper points from each patient were pooled into a tube containing 1 mL of 0.9% (weight/volume) NaCl.
Samples for the PCR detection of A. actinomycetemcomitans were analyzed at the Department of Biomedicine, Aarhus University, Denmark. Samples were processed and analyzed blindly by conventional PCR for the presence of the JP2 and non-JP2 genotypes of A. actinomycetemcomitans, as described previously [40]. Notably, the PCR detected the presence of the bacterium and distinguished between the JP2 and non-JP2 genotypes based on the distinct sizes of the amplicons because the JP2 genotype strains have a characteristic 530 bp deletion in the promoter of the leukotoxin operon.
4.5. Data analysis
The data collected were cleaned, coded, and entered into the computer, then analyzed with the use of SPSS 24 (Statistical Package for the Social Sciences, SPSS Inc., Chicago, IL, USA) and STATA 14.0 (StataCorp LLC, TX, USA).
Author Contributions
Conceptualization, D.H., A.J.; methodology, D.H., A.J.; software, D.H.; validation, D.H., A.K., H.G., A.J.; formal analysis, D.H., H.G., A.J.; investigation, T.M., H.G., M.-L.M.N., M.L., A.J., A.K., D.H.; resources, D.H., A.J., H.G.; data curation, D.H.; writing—original draft preparation, D.H.; writing—review and editing, D.H., T.M., A.K., A.J., M.L., H.G., M.-L.M.N.; visualization, M.L., D.H., H.G.; supervision, D.H., A.J.; project administration, D.H.; funding acquisition, D.H., A.J., H.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by Ingeborg and Leo Dannin Foundation, seed funding from UFFE network grant, entitled ‘Sustainable Heritage Conservation and Development in East Africa in the 21st Century’, Aarhus University, and The Västerbotten County Research Fund (TUA), Sweden. The role of the funding agencies was solely financial support, and the agencies were not involved in the design of the study or collection, analysis, and interpretation of data or the writing of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the KNH–UoN Ethics and Research Committee, Kenya (P711/11/2015, 25 January 2016).
Informed Consent Statement
The parent/guardian and child also provided written informed consent and assent, respectively, after full disclosure of the study had been given to them. Permission to carry out the research at schools in the Mara North Conservancy was sought from the relevant authorities in Kenya.
Acknowledgments
The authors would like to thank the secretary, Gitte Bak Ditlefsen, and clinical assistants at the Department of Dentistry and Oral Health, Section for Paediatric Dentistry, Aarhus University, Denmark for the assistance in practical matters related to the preparation of questionnaires and examinations of the Kenyan adolescents. Also, laboratory assistant Mette L.G. Nikolajsen is acknowledged for taking part in the analysis of the microbiological samples. Furthermore, we are grateful to the staff at Karen Blixen Camp for supporting our activities while doing our field studies in Maasai Mara, Kenya. Our thanks also go to the board of the MMSDI project at Aarhus University, and Chief Joseph Nabala, Maasai Mara for giving advice and various types of information needed to make this project possible. Finally, our thanks go to all the teenagers and their guardians who contributed to and made this study possible.
Conflicts of Interest
The authors declare they have no conflict of interest.
References
- Baelum, V.; Scheutz, F. Periodontal diseases in Africa. Periodontology 2000 2002, 29, 79–103. [Google Scholar] [CrossRef] [PubMed]
- Haubek, D.; Ennibi, O.K.; Poulsen, K.; Vaeth, M.; Poulsen, S.; Kilian, M. Risk of aggressive periodontitis in adolescent carriers of the JP2 clone of Aggregatibacter (Actinobacillus) actinomycetemcomitans in Morocco: A prospective longitudinal cohort study. Lancet 2008, 371, 237–242. [Google Scholar] [CrossRef]
- Baelum, V.; Fejerskov, O.; Manji, F. Periodontal diseases in adult Kenyans. J. Clin. Periodontol. 1988, 15, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Höglund Åberg, C.; Kwamin, F.; Claesson, R.; Dahlen, G.; Johansson, A.; Haubek, D. Progression of attachment loss is strongly associated with presence of the JP2 genotype of Aggregatibacter actinomycetemcomitans: A prospective cohort study of a young adolescent population. J. Clin. Periodontol. 2014, 41, 232–241. [Google Scholar] [CrossRef]
- Bouziane, A.; Hamdoun, R.; Abouqal, R.; Ennibi, O. Global prevalence of aggressive periodontitis: A systematic review and meta-analysis. J. Clin. Periodontol. 2020, 47, 406–428. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, A.; Bouziane, A.; Erraji, S.; Lakhdar, L.; Rhissassi, M.; Miyazaki, H.; Ansai, T.; Iwasaki, M.; Ennibi, O. Etiology of aggressive periodontitis in individuals of African descent. Jpn. Dent. Sci. Rev. 2021, 57, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Brogan, J.M.; Lally, E.T.; Poulsen, K.; Kilian, M.; Demuth, D.R. Regulation of Actinobacillus actinomycetemcomitans leukotoxin expression: Analysis of the promoter regions of leukotoxic and minimally leukotoxic strains. Infect Immun. 1994, 62, 501–508. [Google Scholar] [CrossRef]
- Tsai, C.C.; Ho, Y.P.; Chou, Y.S.; Ho, K.Y.; Wu, Y.M.; Lin, Y.C. Aggregatibacter (Actinobacillus) actimycetemcomitans leukotoxin and human periodontitis—A historic review with emphasis on JP2. Kaohsiung J. Med. Sci. 2018, 34, 186–193. [Google Scholar] [CrossRef]
- Konig, M.F.; Abusleme, L.; Reinholdt, J.; Palmer, R.J.; Teles, R.P.; Sampson, K.; Rosen, A.; Nigrovic, P.A.; Sokolove, J.; Giles, J.T.; et al. Aggregatibacter actinomycetemcomitans-induced hypercitrullination links periodontal infection to autoimmunity in rheumatoid arthritis. Sci. Trans. Med. 2016, 8, 369ra176. [Google Scholar] [CrossRef] [PubMed]
- Haubek, D.; Poulsen, K.; Kilian, M. Microevolution and patterns of dissemination of the JP2 clone of Aggregatibacter (Actinobacillus) actinomycetemcomitans. Infect. Immun. 2007, 75, 3080–3088. [Google Scholar] [CrossRef] [PubMed]
- Haubek, D.; Dirienzo, J.M.; Tinoco, E.M.; Westergaard, J.; López, N.J.; Chung, C.P.; Poulsen, K.; Kilian, M. Racial tropism of a highly toxic clone of Actinobacillus actinomycetemcomitans associated with juvenile periodontitis. J. Clin. Microbiol. 1997, 35, 3037–3042. [Google Scholar] [CrossRef]
- Haubek, D. The highly leukotoxic JP2 clone of Aggregatibacter actinomycetemcomitans: Evolutionary aspects, epidemiology and etiological role in aggressive periodontitis. APMIS 2010, 1–53. [Google Scholar] [CrossRef]
- Dahlen, G.; Basic, A.; Bylund, J. Importance of Virulence Factors for the Persistence of Oral Bacteria in the Inflamed Gingival Crevice and in the Pathogenesis of Periodontal Disease. J. Clin. Med. 2019, 8, 1339. [Google Scholar] [CrossRef]
- Burgess, D.; Huang, H.; Harrison, P.; Aukhil, I.; Shaddox, L. Aggregatibacter actinomycetemcomitans in African Americans with Localized Aggressive Periodontitis. JDR Clin. Trans. Res. 2017, 2, 249–257. [Google Scholar] [CrossRef]
- Albandar, J.M.; Rams, T.E. Risk factors for periodontitis in children and young persons. Periodontology 2000 2002, 29, 207–222. [Google Scholar] [CrossRef]
- Susin, C.; Haas, A.N.; Albandar, J.M. Epidemiology and demographics of aggressive periodontitis. Periodontology 2000 2014, 65, 27–45. [Google Scholar] [CrossRef]
- Claesson, R.; Gudmundson, J.; Aberg, C.H.; Haubek, D.; Johansson, A. Detection of a 640-bp deletion in the Aggregatibacter actinomycetemcomitans leukotoxin promoter region in isolates from an adolescent of Ethiopian origin. J. Oral Microbiol. 2015, 7, 26974. [Google Scholar] [CrossRef] [PubMed]
- Fine, D.H.; Markowitz, K.; Furgang, D.; Fairlie, K.; Ferrandiz, J.; Nasri, C.; McKiernan, M.; Gunsolley, J. Aggregatibacter actinomycetemcomitans and its relationship to initiation of localized aggressive periodontitis: Longitudinal cohort study of initially healthy adolescents. J. Clin. Microbiol. 2007, 45, 3859–3869. [Google Scholar] [CrossRef] [PubMed]
- Fine, D.H.; Patil, A.G.; Velusamy, S.K. Aggregatibacter actinomycetemcomitans (Aa) Under the Radar: Myths and Misunderstandings of Aa and Its Role in Aggressive Periodontitis. Front. Immunol. 2019, 10, 728. [Google Scholar] [CrossRef]
- Rylev, M.; Kilian, M. Prevalence and distribution of principal periodontal pathogens worldwide. J. Clin. Periodontol. 2008, 35, 346–361. [Google Scholar] [CrossRef] [PubMed]
- Orrù, G.; Marini, M.F.; Ciusa, M.L.; Isola, D.; Cotti, M.; Baldoni, M.; Piras, V.; Pisano, E.; Montaldo, C. Usefulness of real time PCR for the differentiation and quantification of 652 and JP2 Actinobacillus actinomycetemcomitans genotypes in dental plaque and saliva. BMC Infect. Dis. 2006, 6, 98. [Google Scholar] [CrossRef] [PubMed]
- Kissa, J.; Chemlali, S.; El Houari, B.; Amine, K.; Khlil, N.; Mikou, S.; Nadifi, S.; Albandar, J.M. Aggressive and chronic periodontitis in a population of Moroccan school students. J. Clin. Periodontol. 2016, 43, 934–939. [Google Scholar] [CrossRef]
- Claesson, R.; Hoglund-Aberg, C.; Haubek, D.; Johansson, A. Age-related prevalence and characteristics of Aggregatibacter actinomycetemcomitans in periodontitis patients living in Sweden. J. Oral Microbiol. 2017, 9, 1334504. [Google Scholar] [CrossRef] [PubMed]
- Childers, N.K.; Grenett, H.; Morrow, C.; Kumar, R.; Jezewski, P.A. Potential Risk for Localized Aggressive Periodontitis in African American Preadolescent Children. Pediatr. Dent. 2017, 39, 294–298. [Google Scholar] [PubMed]
- Stähli, A.; Sculean, A.; Eick, S. JP2 Genotype of Aggregatibacter actinomycetemcomitans in Caucasian Patients: A Presentation of Two Cases. Pathogens 2020, 9, 178. [Google Scholar] [CrossRef]
- World Migration Report. 2018. Available online: https://www.iom.int/wmr/world-migration-report-2018 (accessed on 8 December 2017).
- Mros, S.T.; Berglundh, T. Aggressive periodontitis in children: A 14–19-year follow-up. J. Clin. Periodontol. 2010, 37, 283–287. [Google Scholar] [CrossRef]
- Claesson, R.; Lagervall, M.; Höglund-Aberg, C.; Johansson, A.; Haubek, D. Detection of the highly leucotoxic JP2 clone of Aggregatibacter actinomycetemcomitans in members of a Caucasian family living in Sweden. J. Clin. Periodontol. 2011, 38, 115–121. [Google Scholar] [CrossRef]
- Burgess, D.K.; Huang, H.; Harrison, P.; Kompotiati, T.; Aukhil, I.; Shaddox, L.M. Non-Surgical Therapy Reduces Presence of JP2 Clone in Localized Aggressive Periodontitis. J. Periodontol. 2017, 88, 1263–1270. [Google Scholar] [CrossRef] [PubMed]
- Pahumunto, N.; Ruangsri, P.; Wongsuwanlert, M.; Piwat, S.; Dahlen, G.; Teanpaisan, R. Virulence of Aggregatibacter actinomycetemcomitans serotypes and DGGE subtypes isolated from chronic adult periodontitis in Thailand. Anaerobe 2015, 36, 60–64. [Google Scholar] [CrossRef]
- Elamin, A.; Albandar, J.M.; Poulsen, K.; Ali, R.W.; Bakken, V. Prevalence of Aggregatibacter actinomycetemcomitans in Sudanese patients with aggressive periodontitis: A case-control study. J. Periodontal. Res. 2011, 46, 285–291. [Google Scholar] [CrossRef]
- Kwamin, F.; Gref, R.; Haubek, D.; Johansson, A. Interactions of extracts from selected chewing stick sources with Aggregatibacter actinomycetemcomitans. BMC Res. Notes 2012, 5, 203. [Google Scholar] [CrossRef]
- Ennibi, O.K.; Claesson, R.; Akkaoui, S.; Reddahi, S.; Kwamin, F.; Haubek, D.; Johansson, A. High salivary levels of JP2 genotype of Aggregatibacter actinomycetemcomitans is associated with clinical attachment loss in Moroccan adolescents. Clin. Exp. Dent. Res. 2019, 5, 44–51. [Google Scholar] [CrossRef]
- Krueger, E.; Brown, A.C. Aggregatibacter actinomycetemcomitans leukotoxin: From mechanism to targeted anti-toxin therapeutics. Mol. Oral Microbiol. 2020, 35, 85–105. [Google Scholar] [CrossRef] [PubMed]
- Ben Lagha, A.; Howell, A.; Grenier, D. Cranberry Proanthocyanidins Neutralize the Effects of Aggregatibacter actinomycetemcomitans Leukotoxin. Toxins 2019, 11, 662. [Google Scholar] [CrossRef]
- Ben Lagha, A.; LeBel, G.; Grenier, D. Dual action of highbush blueberry proanthocyanidins on Aggregatibacter actinomycetemcomitans and the host inflammatory response. BMC Complement. Altern. Med. 2018, 18, 10. [Google Scholar] [CrossRef]
- Chang, E.H.; Giaquinto, P.; Huang, J.; Balashova, N.V.; Brown, A.C. Epigallocatechin gallate inhibits leukotoxin release by Aggregatibacter actinomycetemcomitans by promoting association with the bacterial membrane. Mol. Oral Microbiol. 2020, 35, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Åberg, C.H.; Kwamin, F.; Claesson, R.; Johansson, A.; Haubek, D. Presence of JP2 and Non-JP2 Genotypes of Aggregatibacter actinomycetemcomitans and attachment loss in adolescents in Ghana. J. Periodontol. 2012, 83, 1520–1528. [Google Scholar] [CrossRef]
- Kemoli, A.; Gjorup, H.; Norregaard, M.M.; Lindholm, M.; Mulli, T.; Johansson, A.; Haubek, D. Prevalence and impact of infant oral mutilation on dental occlusion and oral health-related quality of life among Kenyan adolescents from Maasai Mara. BMC Oral Health 2018, 18, 173. [Google Scholar] [CrossRef] [PubMed]
- Poulsen, K.; Ennibi, O.K.; Haubek, D. Improved PCR for detection of the highly leukotoxic JP2 clone of Actinobacillus actinomycetemcomitans in subgingival plaque samples. J. Clin. Microbiol. 2003, 41, 4829–4832. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).