Abstract
The rapid global ageing population highlights the pressing need for age-friendly housing that supports independent and healthy ageing in place. Indoor environmental quality (IEQ), encompassing thermal comfort, air quality, acoustic environment, lighting, and humidity, is increasingly recognized as a critical determinant of the health and well-being of older adults. Despite this, existing standards and research methodologies often inadequately address the physiological sensitivities and subjective perceptions specific to older populations. This systematic review synthesizes empirical studies published between 2016 and 2025 on IEQ in age-friendly housing. Following PRISMA guidelines, 31 studies were rigorously screened and analyzed using thematic synthesis. Key findings indicate that older adults’ thermal comfort ranges diverge from standard models, indoor air quality and noise levels often fall short of their needs, and their subjective satisfaction remains low. Effective interventions include improved ventilation, enhanced insulation, noise reduction strategies, and the adoption of smart home technologies. Taken together, these findings reveal a significant gap between existing IEQ standards and the needs of older adults and highlight the necessity of both longitudinal, integrated assessments of objective and subjective factors and participatory design strategies to optimize IEQ in age-friendly housing.
1. Introduction
According to the World Health Organization (WHO), by 2030, one in six people worldwide will be aged 60 or over. Additionally, the population aged 60 and over is projected to increase from 1 billion in 2020 to 1.4 billion by 2030. Moreover, by 2050, this population is expected to double. Similarly, between 2020 and 2050, the number of persons aged 80 and over is expected to triple to 426 million. This shift in the distribution of the population towards older persons is known as population ageing []. By international standards, older persons or elders are generally defined as persons aged 60 years and over, with old age specifically defined as 60 to 75 years, 75 to 90 years as the oldest old, and 90 years and over as the longest-lived [].
The ageing population raises the question of how to provide appropriate housing that meets the needs of older persons and facilitates ageing in place without losing their autonomy and independence []. Age-friendly housing refers to residential environments that are designed, adapted, or managed to support the health, safety, autonomy, and social participation of older adults, enabling them to age in place with dignity and independence []. Better age-friendly housing is envisioned to be a solution to help people live longer independently at home, thereby reducing the costs of long-term care and responding to the needs and demands of older persons []. With the deepening of global ageing, indoor environmental quality in the living environments of older people has gradually become a focus of research attention []. Most of the current literature is based on small-sample cross-sectional surveys or single-site monitoring, and there is a lack of long-term follow-up studies across seasons and geographic regions, as well as few studies that integrate objective exposure, subjective perception, and health outcomes into a unified framework [].
Therefore, this study systematically reviewed peer-reviewed empirical English-language studies on indoor environmental quality dimensions such as thermal comfort, air quality, acoustic conditions, lighting, and humidity in age-friendly housing published between 2016 and 2025 and synthesized their objective exposure data, subjective perceptions, and health outcomes into a comprehensive framework. Review articles, conference abstracts, studies of non-residential scenarios, and case reports without raw data were excluded. The current review aims to answer the following questions: (1) What is the current status of key elements of indoor environmental quality (air quality, thermal comfort, acoustic environment, light) in age-friendly housing? (2) How do older people subjectively perceive their living environments, and how do these environmental characteristics affect their physical and psychological health? (3) What design and intervention strategies are effective in improving indoor environmental quality and enhancing the health and satisfaction of older people in age-friendly housing? To address these questions, the remainder of the paper is structured as follows: Section 2 is the literature review, which firstly provides a systematic overview of the main dimensions of indoor environmental quality in ageing homes, including thermal comfort, indoor air quality, acoustic environment, lighting, and humidity; Section 3, Methods, describes in detail the systematic literature review process adopted in this study, including the search strategy, the inclusion and exclusion criteria, the literature screening, the methodology of data extraction and synthesis, and the use of a quality; Section 4 presents the basic characteristics of the included studies, such as year of publication, geographical distribution, and research methodology, and summarizes the core findings around the three main themes of Objective measurement of indoor environmental quality, subjective perceptions and health effects, and intervention and design strategies; Section 5 discusses the impact of the dimensions on the health and quality of life of older adults, analyses the limitations of the studies, and proposes future research. Globally, less than 10% of existing housing stock meets accessibility or adaptability standards suitable for ageing in place, highlighting the urgent need for age-friendly housing design and renovation.
2. Literature Review
2.1. Definition and Evaluation Framework of Age-Friendly Housing
The concept of age-friendly housing can be traced back to the idea of ‘aging in place’ that emerged in the 1970s, which was proposed by Graff and Wiseman (1978) to refer to the phenomenon of older people staying in their original place of residence as they grow older without moving []. Graff and Wiseman (1978) suggested that ‘aging in place’ refers to the phenomenon of older people remaining in their original place of residence as they age without moving []. The concept, which gained popularity in the research literature in the 1970s and 1980s, centres on the desire of older people to remain in their homes and live independently to maintain social connections and independence [].
Since the 2000s, the World Health Organization (WHO) has promoted the development of the Age-Friendly Cities framework, which explicitly includes the residential environment as an important dimension in the assessment of age-friendly communities []. In particular, the WHO’s Decade of Action on Healthy Ageing (DOAH), which will be launched in 2021, proposes a people-centred, cross-sectoral and collaborative global strategy for healthy ageing interventions and assessment systems, making the construction of age-friendly housing an important element of policy practice in all countries []. The practice of age-friendly housing was initially based on the partial modification of barrier-free facilities, and then gradually expanded into a systematic design that comprehensively considers the structural layout of housing, the provision of facilities, and the community environment [].
Theoretically, the design of age-friendly housing is influenced by the Bronfenbrenner social-ecological system model []. The model suggests that individual health and development are affected by the interaction of multiple levels of environment, including the micro-environment of individuals, the meso-environment of community organizations, and the macro-environment of policy and culture []. Therefore, the design of age-friendly housing needs to take into account multiple dimensions such as individual capabilities, social support, healthcare services, and community accessibility. From the perspective of international practice, Europe has carried out research on age-friendly housing earlier. The UK proposed the ‘Lifetime Homes’ standard in the early 1990s, which emphasizes flexibility and accessibility, while the Nordic countries promote the concept of universal design through universal welfare and regulatory support []. Japan has established a diversified model of ‘service homes for the elderly’ and community care based on long-term care insurance and accessibility laws []. Australia has adopted the Design Guidelines for Livable Homes. It will incorporate basic accessibility requirements into the national building code in 2022, realizing the transformation of age-friendly housing from advocacy to mandatory implementation [].
2.2. Current Research Status of Indoor Environmental Quality in Age-Friendly
2.2.1. Occupants’ Subjective Responses
With the global ageing of the population and the prevalence of home care models, addressing IEQ in the living environment is critical to promoting the health and well-being of older people []. The concept of indoor environmental quality (IEQ) originated in the 1970s, when Danish scholar P.O. Fanger pioneered the assessment of indoor thermal environments by first combining environmental parameters with subjective human perceptions []. Thermal comfort has always been closely related to the housing satisfaction and health status of older people and has therefore been a focus of research on age-friendly housing []. Previous studies have highlighted that older people often prefer warmer indoor environments to standard thermal comfort models, as they are more vulnerable to temperature extremes. For example, a heatwave study in the Netherlands found that more than 40% of older residents experienced heat-related symptoms when indoor temperatures exceeded approximately 25 °C, with their thermal discomfort increasing by 33% for every 1 °C increase in temperature []. In addition, a study of 72 older residents in Sichuan, China, found that the temperature in their homes was higher than that in their homes. In contrast, a field study of 72 senior flats in Sichuan, China, showed that 81.9% of winter indoor temperature measurements were below the comfort range recommended by ASHRAE-55, averaging approximately 13.9 °C []. Given these differences, studies often use a mixed-methods approach that combines physical measurements with subjective assessments to evaluate the comfort of the living environment [].
2.2.2. Objective Sensor Measurements
The majority of indoor air quality studies in age-friendly housing have used cross-sectional and longitudinal designs, with sensors continuously monitoring indoor pollutant concentrations and health outcome indicators, to systematically assess the physiological and psychological impacts on the elderly as a vulnerable group [,]. It has been widely found that chronic exposure to indoor pollutants can lead to cognitive decline when older people spend more than 85% of their time in indoor environments. In the area of respiratory health, CO2 concentrations are both an important indicator of poor ventilation and highly correlated with symptoms such as dyspnea and cough []. It has been noted that the combined effects of pollutants and thermal comfort parameters in the presence of inadequate ventilation make older persons more vulnerable to adverse respiratory outcomes: high ambient temperatures reduce wheezing symptoms, while low temperatures induce colds, which exacerbate airway hyperresponsiveness []. Older people in socio-economically disadvantaged areas are particularly vulnerable to temperature extremes, and even low levels of indoor pollution can seriously impair their respiratory health, a vulnerability that is further exacerbated with age []. Common problems are poor ventilation, high levels of particulate and biological contaminants, often stemming from aging buildings or the habits of residents []. For example, in Portugal, although the national standards for CO2 and other gases were maintained in winter, the fungal spore counts repeatedly exceeded 500 CFU/m3; and in China, many elderly residents in senior flats relied on open windows for ventilation, which subjectively improves freshness, but also leads to new problems, such as cold winds, humidity, and outdoor noise [,].
Based on the above findings, future studies should integrate the quantification of cognitive and respiratory outcomes under the same research framework and explore the interaction of multiple factors such as ventilation, temperature, humidity, and bio-pollution in depth.
2.2.3. Combined Subjective–Objective Assessments
Studies on the acoustic environment of age-friendly homes often combine objective noise measurements with subjective assessments to fully reveal the effects of noise on the hearing and physical and mental health of older people []. Studies agree that the decline in hearing function with age makes older people significantly more sensitive to background noise and that excessive indoor noise levels can impair their quality of life; relatively speaking, they prefer natural sound sources to alleviate noise stress []. Regarding the comfort of the acoustic environment, different studies give different conclusions: some report a decrease in comfort ratings with age, while others point out that older people are more tolerant of noise than younger groups []. Prolonged exposure to noise above 60 dB significantly increases the risk of cardiovascular disease in older people; night-time noise can also disrupt sleep and exacerbate agitated behaviors in people with dementia Cemre []. In summary, age-friendly housing should maintain low background noise, reasonably introduce natural sound sources, and pay attention to night-time sound insulation and acoustic environment design to improve the overall living comfort and health and well-being of the elderly.
Despite the significant impact of Indoor environmental quality on older adults, current evaluation and design criteria are mostly based on assumptions of healthy adults, which make it difficult to adequately reflect differences in physiological tolerance, sensory thresholds, and behavioral patterns among older adults [].
3. Methodology
3.1. Search Strategy
The review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines to ensure transparency and reproducibility []. This study followed the PRISMA process to conduct a literature search, which included Google Scholar, Web of Science, Science Direct, Scopus, PubMed, and ProQuest. The study followed the PRISMA 2020 guidelines (see Supplementary Materials, Table S1: PRISMA checklist). To capture the most recent developments, it includes only studies published in the last ten years, starting on 7 August 2016. The keywords searched included: indoor environmental quality, indoor air quality, acoustic environment, light environment, age-friendly housing, ageing, residential, housing, home. Specific inclusion and exclusion criteria (Table 1) were used in this study to ensure the accuracy of the literature screening process.

Table 1.
Include and exclude criteria.
3.2. Data Extraction and Quality Assessment
In this systematic review, we defined P (Population) as older adults (aged 60 years and over) living in age-friendly housing; E (Exposure) as key indoor environmental quality factors—air quality, thermal comfort, acoustic environment, and lighting; O (Outcomes) as health and quality-of-life indicators (physical health, psychological well-being, life satisfaction), residents’ subjective perceptions and environmental needs, and the effects of design interventions; S (Setting) as residential, age-friendly housing; and T (Timeframe) as studies published in the last ten years, from 7 August 2016 onward. The study used EndNote 21, a literature manager, for literature management and Rayyan (web-based version, https://www.rayyan.ai) software for the full text screening stage. Data extraction consisted of Study, Country, Setting/context, Participant characteristics, Groups, Outcomes measured, and Main description of results sections. The Joanna Briggs Institute’s Analytical Cross-Sectional Study Critical Appraisal Checklist was used for the quantitative study, and the JBI Qualitative Research Critical Appraisal Checklist for qualitative research; all assessment tools were taken from the JBI Manual []. Disagreements were resolved through discussion until a consensus was reached, ensuring the reliability of the inclusion process and minimizing subjective bias. A standard data extraction template was used to specify literature characteristics, study context, participant information, research methods, measures, and key findings. Meanwhile, the JBI quality assessment tool was used to assess the quality of each piece of literature to confirm the validity and reliability of the research evidence.
3.3. Data Synthesis
A clear analytical structure was developed by thematically synthesizing the 259 free codes extracted from the included literature. Six major descriptive themes were formed, which were further integrated into three higher-level analytical themes to reveal the complex relationship between indoor environmental quality (IEQ) and the health of older adults. The thematic analyses were divided into three core sections: Objective measurement of indoor environmental quality, subjective perceptions and health effects, and intervention and design strategies, with corresponding research limitations and future research directions.
This study used the theme synthesis method proposed by []. Qualitative coding and thematic synthesis were conducted using NVivo 20 []. By using NVivo 20, the thematic synthesis method was divided into three specific stages as follows (Table 2):

Table 2.
Thematic Synthesis Process.
To present the results of the thematic analysis intuitively, the word cloud function in NVivo was used to visualize the analytical themes (Figure 1). The word cloud shows that the frequency of ‘environment’, ‘elderly’, and ‘indoor’ is extremely high, which makes it clear that the core of the study is the ‘environment’, ‘elderly’, and ‘indoor’. extremely high, making clear the focus of the core of the study. In addition, the terms ‘thermal’, ‘health’, ‘lighting’, and ‘Noise’ are also prominent, reflecting the focus of research on each theme and the trend of literature content.
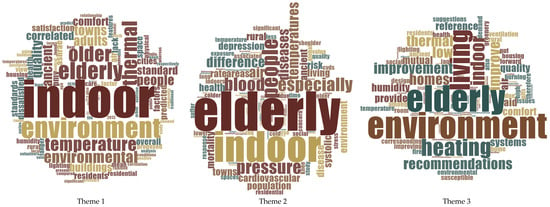
Figure 1.
Thematic Analysis Word Cloud.
4. Results
The literature screening process is illustrated in Figure 2, which follows the PRISMA guidelines. In the identification phase, 2123 records were retrieved from six databases (Google Scholar, Web of Science, ScienceDirect, Scopus, PubMed, and ProQuest), and 767 duplicates were removed. In the screening phase, the remaining 1356 titles and abstracts were assessed, leading to the exclusion of 1249 studies for reasons including non-home-based elderly care settings, age <60 years, lack of primary data, topics unrelated to indoor environmental quality or policy, outdoor or green space focus, and evidence of significant bias.
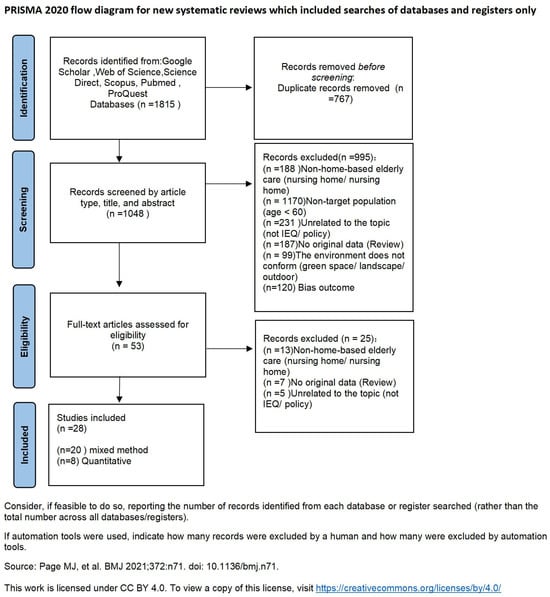
Figure 2.
Literature screening from PRISMA [].
In the eligibility phase, the full text of 107 articles was assessed, of which 76 were excluded, mainly because they did not address home-based care for older people, lacked original empirical data, or were outside the scope of indoor environmental quality research. Finally, at the inclusion stage, 31 studies met all criteria for inclusion in the review, including 22 mixed-methods studies (71%) and 9 purely quantitative studies (29%). This flowchart transparently documents how the review narrowed down the initial set of more than 2000 records to studies that directly informed the analyses.
The 31 studies included in this review were published between 2016 and 2025. Only one study appeared per year from 2016 to 2018, indicating the field was then in its infancy; publication counts fluctuated between one and two during 2019–2021. From 2022 onwards, output rose markedly, with five studies in 2022, six in 2023, and eight in 2024, which reflects a period of rapid scholarly growth; to date, five studies have appeared in 2025. Altogether, 11 studies (35%) were published in 2022–2023, eight (26%) in 2024, five (16%) in 2025, and seven (23%) during 2016–2021 (Figure 3).
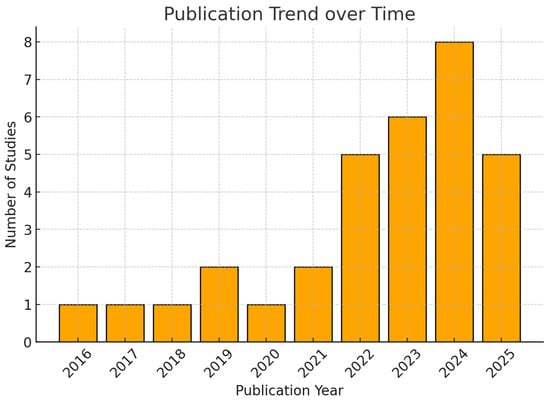
Figure 3.
Histogram of annual trends in the literature.
Figure 4 shows that China (n = 16) contributed six studies in 2022, five in 2023, seven in 2024, five in 2025, and one and two in 2020 and 2021, respectively. Other regions are far less active: Australia (n = 2) published one study each in 2019 and 2022; the USA (n = 2) in 2016 and 2021; Greece (n = 1) in 2019; Uganda (n = 2) in 2025; and Poland (n = 1), Denmark (n = 1), India (n = 1), Italy (n = 1), Hong Kong (n = 1), Japan (n = 1), Korea (n = 1), and the UK (n = 1) each produced a single study.
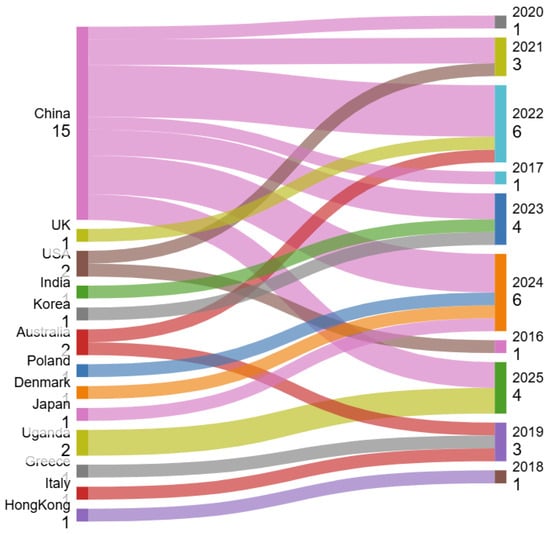
Figure 4.
Geographical distribution of literature.
Regarding intervention levels, the most prevalent type was IA–UI (intervention–no intervention), accounting for 15 studies (48%) and primarily based on observational field surveys. PPₘ–UI (physiological parameters–no intervention) appeared in four studies (13%), employing this approach to measure physiological parameters concurrently with upstream surveys. IA–DI (representing downstream interventions, such as remodeling strategies combined with environmental assessments) appeared in four studies (13%). Other types included MI–DI and DI–PPₘ, both reflecting intervention-oriented approaches, but each reported in only one study (3%). Furthermore, studies combining on-site assessments with mixed-methods frameworks (IA–M and UI–M) were also relatively scarce.
Sample sizes varied considerably, ranging from 10 to 11,614 participants. Median sample sizes for mixed-method studies typically fell between 72 and 152 participants. Overall, the existing literature remains heavily concentrated on upstream surveys and baseline environmental assessments, with comparatively fewer studies undertaking post-intervention retesting and evaluation (Table 3).

Table 3.
Data extraction (n = 31).
Quality Assessment
The quality assessment of the included studies was conducted for 9 quantitative and 22 mixed-methods studies (Table 4 and Table 5). For the quantitative studies (n = 9), methodological appraisal was performed using the Joanna Briggs Institute (JBI) Analytical Cross-Sectional Study Critical Appraisal Checklist [], which is designed to evaluate the methodological quality of quantitative studies reporting associations and correlations (Appendix B). The checklist consists of eight criteria covering sampling, measurement validity, confounder control, and statistical analysis. All nine studies (100%) received the highest rating (“++”) for the use of standardized measurement criteria, while eight (89%) were rated “++” for identifying potential confounders. Seven studies (78%) achieved “++” for clearly defined sampling criteria and for valid, reliable outcome measurement. Six studies (67%) were rated “++” for adequately describing subjects and settings, outlining strategies to address confounding, and applying appropriate statistical analyses. Only five (56%) were rated “++” for the validity and reliability of exposure measurement.

Table 4.
Methodological quality of quantitative studies (n = 9).

Table 5.
Methodological quality of mixed methods studies (n = 22).
For the mixed-methods studies (n = 22), the quantitative components were appraised using the JBI Analytical Cross-Sectional Checklist, while the qualitative components were evaluated with the JBI Qualitative Research Checklist (Appendix A). In line with JBI guidance, results were reported item by item rather than aggregated into a single score, allowing a more nuanced evaluation of methodological quality. Overall, twenty studies (91%) received the highest rating (“++”) for valid exposure measurement and standardized condition measurement, and eighteen (82%) were rated “++” for clearly defined sampling criteria, adequate description of subjects and settings, valid outcome measures, and appropriate statistical analysis. Nineteen studies (86%) demonstrated philosophical congruence, while seventeen (77%) showed consistency between research questions, interpretations, and participant representation. In addition, twenty-one studies (95%) ensured consistency in data analysis and interpretation, and twenty (91%) documented ethical approval and adherence. By contrast, only fifteen studies (68%) identified confounders, implemented confounder-control strategies, and demonstrated researcher reflexivity, while fourteen (64%) explicitly reported researcher positioning. Nevertheless, twenty-one studies (95%) provided coherent conclusions clearly grounded in the data.
THEME 1: Objective measurement of indoor environmental quality
Thermal Comfort
Older adults’ thermal tolerance in the home typically exceeds that of younger cohorts, yet extreme seasons expose them to significant health risks. Laboratory and field surveys show that over 60% of seniors report comfort at indoor operative temperatures between 19 °C and 23 °C, and self-rate their health and well-being as “very good” within 18.4–24.3 °C [,]. ISO 28803-2012 concurs, recommending a PMV range of 0 to 0.5 for elderly occupants []. In practice, however, winter measurements in rural homes often fall below 16 °C—well under the 18 °C minimum—and frequently dip beneath 15 °C, a threshold at which systolic blood pressure in older residents rises markedly []. Conversely, many dwellings lack sufficient cooling during heat waves, leaving seniors vulnerable to both cold and heat stress [] (Jiao et al., 2020).
Air Quality
Indoor concentrations of carbon dioxide, particulate matter, volatile organic compounds, and combustion by-products commonly exceed comfort thresholds in senior housing []. Although guidance calls for 25–55% relative humidity, summer monitoring often records values at or above the upper limit, compounding thermal discomfort and pollutant retention []. CO2 levels above 1000 ppm regularly induce sensations of draughtiness and suffocation, and correlate with increased respiratory and cardiovascular symptoms among older occupants []. These patterns underscore inadequate ventilation rates and the urgent need for targeted IAQ interventions in age-friendly design.
Acoustic Environment
The Italian Social Housing Survey showed that 53% of older respondents were satisfied with the indoor acoustic environment (mean 3.43 ± 1.16 points), which was higher than air quality (3.13 ± 1.20), thermal comfort (2.76 ± 1.35) and lighting (2.65 ± 0.96) []; a follow-up study also confirmed that acoustic indicators in multi-unit flats generally met national and international standards [].
Acoustic comfort depends not only on noise source levels but also on room geometry, surface absorption properties, and furniture layout. Studies have shown that using low-reflection wall materials, installing thick carpeting, and strategically placing acoustic panels and upholstered furniture can reduce indoor equivalent continuous noise levels to 40–45 dB, significantly enhancing older adults’ subjective comfort [,].
THEME 2: Elderly Perceptions and Health Outcomes
Subjective Environmental Perceptions
Older adults’ subjective evaluations of their indoor environment are tightly linked to comfort and well-being. Surveys show that over 70% of seniors report their bedrooms feel too cold in winter and too hot in summer, with 42% expressing dissatisfaction with temperature and humidity, and summer dissatisfaction reaching 71% for heat and 42% for humidity [,]. In a study of multigenerational elders in an historic town, 42% were dissatisfied with high midday summer temperatures—far exceeding predictions from standard comfort models—and neutral comfort temperatures clustered at 25–26 °C rather than the typical 22–24 °C [,]. Further demonstrated that seniors’ perceptions of thermal comfort, noise, lighting, and air quality correlate closely with their physical and mental health, as physiological decline amplifies sensitivity to heat extremes, poor lighting, or intrusive noise [].
Physical and Psychological Health Outcomes
Objective health measures confirm perception-driven risks: exposure to cold indoor conditions heightens older adults’ systolic blood pressure and heart rate responses to temperature drops, signaling cardiovascular vulnerability in winter []. The WHO estimates that indoor Objective measurement of indoor environmental quality raises coronary heart-disease risk by 18% and stroke risk by 26% in older populations []. Qualitative interviews with multi-generational residents of traditional Tujia dwellings reveal that inadequate privacy, bathing, and storage facilities undermine elders’ quality of life and psychological well-being []. Individuals reporting fair or poor health place greater importance on IEQ features, underscoring the pronounced needs of health-limited groups []. To generalize these findings, comfort models must be validated on large, multi-season cohorts across diverse climates, incorporating both hot-humid and winter data to fully capture IEQ’s physiological and psychological impacts on older adults [].
THEME 3: Intervention and Design Strategies
Given these exposure issues and perceived impacts, the literature proposes relevant design and behavioral strategies to improve the indoor environment for older people. Thermal comfort interventions in housing for older adults include passive measures [].
Air quality strategies focus on improving ventilation and filtration []. Older people are most comfortable when noise levels are kept below the hazard threshold of 65 dB []. For older people with cognitive impairment and mobility problems, technical aids can provide support. It is vital that interventions are evaluated in terms of actual well-being benefits: as [] have shown, improved lighting, thermal comfort, and air quality may have a positive impact on older people’s health and satisfaction. An integrated approach involving older people in decision-making, guided by ongoing monitoring, offers the best route to healthier, more comfortable homes for an ageing population.
Design Intervention
For thermal comfort, it is recommended to combine intelligent HVAC and air purification equipment, and to strengthen the thermal insulation, shading, and natural ventilation of the envelope to balance thermal comfort and air quality [,]. Meanwhile, passive conditioning measures such as high-performance external windows and thermal quality optimization can also significantly improve winter and summer comfort experiences []. Air quality strategies, on the other hand, focus on strengthening ventilation and filtration systems and introducing affordable air purifiers in low-income or older housing to reduce CO2 and PM2.5 and VOC levels of pollutants []. With regard to the acoustic environment, studies have shown that controlling indoor noise below 65 dB maximizes comfort for older people [].
Considering that 87% of older people prefer to open windows rather than use air conditioning, low-income households should be provided with convenient, low-cost localized heating and ventilation (HVAC) solutions, with accessibility monitoring and emergency response systems in multigenerational or shared community spaces, to ensure standard environments of 18.4 °C to 24.3 °C and 55% relative humidity []. For older people with cognitive or mobility impairments, technical aids such as adjustable toilet seats, smart lighting, and audible alert systems can be introduced to support daily mobility and safety [].
The spatial layout
Emphasizes the design of barrier-free access, functional zoning, and shared activity areas, which not only ensures the safety and autonomy of the elderly living alone but also promotes family companionship and community interactions, thereby enhancing the overall quality of life of the elderly living at home. In addition, improving the low-humidity environment through the transpiration of green plants and providing central heating subsidies or neighborhood-assisted warming design for low-income elderly in rural areas can help alleviate winter fuel poverty and reduce the risk of cardiovascular diseases [].
5. Discussion
From the perspective of evidence structure, research in the IEQ field has seen significant growth in recent years, but still exhibits notable geographical and methodological biases. This review included a total of 28 studies, with only one study published annually from 2016 to 2018. However, output has rapidly increased since 2022, with five studies in 2022, six in 2023, and seven in 2024, as well as two in the first half of 2025. Geographically, China accounted for the highest proportion (n = 18), followed by Australia with 3 studies, the United States and Greece with 2 each, and the remaining countries with 1 each, indicating insufficient broad representation across cultural and climatic zones.
In terms of research design, 75% were mixed-method studies, and 25% were purely quantitative studies; the most common “indoor environment assessment—upstream investigation” accounted for 54%, while studies involving energy-saving renovations or other downstream interventions, followed by reassessment only, accounted for 15%. Sample sizes vary greatly, but true longitudinal field studies with interventions followed by follow-up measurements remain scarce, making it difficult to quantify the causal effects and sustainability of interventions.
In cross-dimensional integration, current research on indoor environmental quality (IEQ) in age-friendly residential buildings generally suffers from issues such as insufficient temporal scope, assessment criteria that neglect the physiological characteristics of older adults, and research methods that overlook the subjective experiences of older adults. This means that while existing studies have preliminarily confirmed the importance of IEQ for older adults’ health, they have not fully revealed the impacts of seasonal changes and individual differences on older adults, nor have they adequately considered older adults’ perceptions and experiences [,,]. Existing building envelope structure studies are primarily short-term monitoring studies conducted under single-season or single-climate conditions, lacking long-term field intervention studies across seasons and multiple climate zones []. However, indoor air quality (IAQ) studies often rely on sensor-based continuous monitoring, but quantitative assessments of the interactions between ventilation, temperature, humidity, and biological pollutants, as well as the unified quantification of the associations between these factors and respiratory health, remain insufficient. Additionally, acoustic environment studies require stronger evidence to establish causal relationships between natural soundscapes, nighttime noise, and sleep, as well as cardiovascular risks.
Research indicates that relying solely on a single technology is insufficient to meet the multi-dimensional indoor environmental quality needs of the elderly. It is essential to integrate passive building envelope design, active temperature control, air purification, acoustic treatment, and behavioral interventions cohesively. First, by enhancing the thermal insulation performance of walls and roofs, and adopting high-performance windows and shading devices, passive technologies can reduce average indoor temperatures by 2.2 °C and save 29% of energy consumption []. Combined with optimized natural ventilation pathways, these measures provide stable boundary conditions for smart HVAC systems, maintaining indoor operating temperatures within the ASHRAE Standard 55-recommended comfort range of 18.4 °C to 24.3 °C (ASHRAE (Peachtree Corners, GA, USA), 2019). Secondly, mechanical ventilation combined with high-efficiency filtration and CO2-triggered demand-controlled ventilation not only significantly reduces CO2, PM2.5, and VOC concentrations but also controls relative humidity between 40% and 55%, effectively alleviating stuffiness and reducing respiratory and cardiovascular symptoms [,]. Optimizing the acoustic environment is equally critical: by installing large-area sound-absorbing wall panels, thick carpets, and soft furniture, the equivalent continuous noise level can be reduced from the daily background value to 40–45 dB, well below the 65 dB cardiovascular stress threshold, thereby significantly improving sleep quality and subjective comfort for the elderly [,].
5.1. Limitations
The literature included in this study exhibits a high degree of geographical concentration, with the overwhelming majority originating from China. This imbalance not only reflects the rapid growth in China’s policy-driven research on ageing and housing but also reveals limitations in methodological approaches and publication standards. Specifically, this review only incorporates empirical studies published in English between 2016 and 2025. Consequently, relevant studies from Japan, Nordic countries, and other European regions were excluded if published in their native languages or prior to 2016. Furthermore, while Chinese research frequently employs mixed-method designs combining quantitative monitoring of indoor environmental parameters with questionnaires or interviews, its focus remains disproportionately concentrated on thermal comfort and indoor air quality, with relatively insufficient attention to acoustic and lighting conditions. Moreover, existing studies are largely confined to short-term cross-sectional surveys, lacking multi-seasonal validation, longitudinal monitoring, or integration with building performance simulations. In contrast, research traditions in Japan and Nordic countries emphasise policy frameworks, universal design, and long-term care models, yet often lack the direct empirical measurement data required for this review.
5.2. Recommendations
A comprehensive analysis of the disproportionate focus on China reveals two key findings: firstly, research on China’s “home-based care” model is flourishing; secondly, studies from other regions, predominantly policy- and design-oriented, face methodological exclusion. To establish a more balanced evidence base, future systematic reviews should broaden their scope: retrieving data from multilingual databases, integrating non-English literature, and incorporating grey literature such as government reports and technical guidelines. Methodologically, combining objective monitoring, subjective surveys, and advanced simulation tools can yield more actionable evidence for adaptation strategies. Complementary qualitative research would further enrich empirical findings, elucidating how cultural and contextual factors shape older adults’ residential experiences. Finally, cross-national comparative studies, particularly drawing on experiences from Japan, Nordic countries, and other European regions, remain crucial for establishing a comprehensive and representative global framework to assess indoor environmental quality in age-friendly housing.
6. Conclusions
This systematic review highlights the significant impact of indoor environmental quality on the health and satisfaction of older people in age-appropriate housing. Findings show that existing environmental standards, which are largely based on healthy adult populations, have significant gaps with the physiological and perceived needs of older people. Improving thermal comfort, enhancing ventilation, controlling indoor pollutants, and maintaining low background noise levels are all key elements in creating age-friendly environments. Future research should prioritize longitudinal follow-up studies, combining objective measurements, subjective perceptions, and health outcomes in different geographical and climatic contexts. In terms of practical implications, inclusive design principles should be adopted, and the effectiveness of interventions should be systematically evaluated. In conclusion, the creation of age-friendly indoor environments requires an evidence-based, integrated approach that specifically responds to and meets the nuanced needs of ageing populations.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/buildings15224148/s1, Table S1: PRISMA checklist.
Author Contributions
Conceptualization, P.L. and N.D.D.; Methodology, P.L.; Software, P.L.; Validation, P.L., N.D.D., J.M.J. and N.Z.; Formal Analysis, P.L.; Investigation, P.L.; Resources, P.L.; Data Curation, P.L.; Writing—Original Draft Preparation, P.L.; Writing—Review and Editing, P.L.; Visualization, P.L.; Supervision, P.L.; Project Administration, P.L.; Funding Acquisition, N.D.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
No new data were created or analyzed in this study.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
JBI CRITICAL APPRAISAL CHECKLIST FOR QUALITATIVE RESEARCH
Reviewer______________________________________Date_______________
Author__________________________Year________Record Number_________
Yes No Unclear Not applicable
1. Is there congruity between the stated philosophical
perspective and the research methodology? □ □ □ □
2. Is there congruity between the research methodology
and the research question or objectives? □ □ □ □
3. Is there congruity between the research methodology
and the methods used to collect data? □ □ □ □
4. Is there congruity between the research methodology
and the representation and analysis of data? □ □ □ □
5. Is there congruity between the research methodology
and the interpretation of results? □ □ □ □
6. Is there a statement locating the researcher culturally
or theoretically? □ □ □ □
7. Is the influence of the researcher on the research,
and vice- versa, addressed? □ □ □ □
8. Are participants, and their voices, adequately
represented? □ □ □ □
9. Is the research ethical according to current criteria or,
for recent studies, and is there evidence of ethical approval
by an appropriate body? □ □ □ □
10. Do the conclusions drawn in the research report flow from the analysis, or
interpretation, of the data? □ □ □ □
Overall appraisal: Include □ Exclude □ Seek further info □
Comments (Including reason for exclusion) __________________________________________________________________________________________________________________________________________
Appendix B
JBI Critical Appraisal Checklist for Analytical Cross Sectional Studies
Reviewer______________________________________Date___ ____________
Author__________________________Year________Record Number_________
Yes No Unclear Not applicable
1. Were the criteria for inclusion in the sample clearly
defined? □ □ □ □
2. Were the study subjects and the setting described
in detail? □ □ □ □
3. Was the exposure measured in a valid and reliable
way? □ □ □ □
4. Were objective, standard criteria used for measurement
of the condition? □ □ □ □
5. Were confounding factors identified? □ □ □ □
6. Were strategies to deal with confounding
factors stated? □ □ □ □
7. Were the outcomes measured in a valid and
reliable way? □ □ □ □
8. Was appropriate statistical analysis used? □ □ □ □
Overall appraisal: Include □ Exclude □ Seek further info □
Comments (Including reason for exclusion)
__________________________________________________________________________
References
- Keating, N. A research framework for the United Nations Decade of Healthy Ageing (2021–2030). Eur. J. Ageing 2022, 19, 775–787. [Google Scholar] [CrossRef]
- Dyussenbayev, A. Age periods of human life. Adv. Soc. Sci. Res. J. 2017, 4, 258–263. [Google Scholar] [CrossRef]
- Luciano, A.; Pascale, F.; Polverino, F.; Pooley, A. Measuring Age-Friendly Housing: A Framework. Sustainability 2020, 12, 848. [Google Scholar] [CrossRef]
- Kumar, S.; Underwood, S.H.; Masters, J.L.; Manley, N.A.; Konstantzos, I.; Lau, J.; Haller, R.; Wang, L.M. Ten questions concerning smart and healthy built environments for older adults. Build. Environ. 2023, 244, 110720. [Google Scholar] [CrossRef]
- Yang, S.; Bai, T.; Feng, L.; Zhang, J.; Jiang, W. Indoor Environmental Quality in Aged Housing and Its Impact on Residential Satisfaction Among Older Adults: A Case Study of Five Clusters in Sichuan, China. Sustainability 2025, 17, 5064. [Google Scholar] [CrossRef]
- Graff, T.O.; Wiseman, R.F. Changing Concentrations of Older Americans. Geogr. Rev. 1978, 68, 379. [Google Scholar] [CrossRef]
- Barati, F.; Khoddam, H.; Modanloo, M. Concept development of “Aging in place”: Application of hybrid model. J. Fam. Med. Prim. Care 2022, 11, 6646–6653. [Google Scholar] [CrossRef]
- Rudnicka, E.; Napierała, P.; Podfigurna, A.; Męczekalski, B.; Smolarczyk, R.; Grymowicz, M. The World Health Organization (WHO) approach to healthy ageing. Maturitas 2020, 139, 6–11. [Google Scholar] [CrossRef]
- Black, K.; Jester, D.J. Examining Older Adults’ Perspectives on the Built Environment and Correlates of Healthy Aging in an American Age-Friendly Community. Int. J. Environ. Res. Public Health 2020, 17, 7056. [Google Scholar] [CrossRef] [PubMed]
- CORDIS. cordis.europa.eu. Certified Smart and Integrated Living Environments for Ageing Well. CORDIS European Commission. 22 August 2022. Available online: https://cordis.europa.eu/project/id/826295/reporting (accessed on 13 September 2025).
- Kawaguchi, K.; Ueno, T.; Ide, K.; Kondo, K. Social participation among residents of serviced housing for older people versus community-dwelling older people in Japan: A propensity score matching analysis. J. Public Health 2024, 1–11. [Google Scholar] [CrossRef]
- Armstrong, A.; Wright, C.; Ashe, B.; Nielsen, H. Enabling Innovation in Building Sustainability: Australia’s National Construction Code. Procedia Eng. 2017, 180, 320–330. [Google Scholar] [CrossRef]
- Zhang, Y.; Liu, X.; Meng, Q.; Li, B.; Caneparo, L. Physical environment research of the family ward for a healthy residential environment. Front. Public Health 2022, 10, 1015718. [Google Scholar] [CrossRef]
- Fanger, P.O. Assessment of man’s thermal comfort in practice. Occup. Environ. Med. 1973, 30, 313–324. [Google Scholar] [CrossRef]
- Kenny, G.P.; Flouris, A.D.; Yagouti, A.; Notley, S.R. Towards establishing evidence-based guidelines on maximum indoor temperatures during hot weather in temperate continental climates. Temperature 2018, 6, 11–36. [Google Scholar] [CrossRef]
- Chen, Y.; Wulff, F.; Clark, S.; Huang, J. Indoor comfort domains and well-being of older adults in residential settings: A scoping review. Build. Environ. 2024, 267, 112268. [Google Scholar] [CrossRef]
- Shahzad, S.; Torres, S.G.; Rijal, H.B.; Nicol, F. Lack of Thermal Comfort Is a Matter of Life and Death: A Systematic Review for Older People. Buildings 2025, 15, 1141. [Google Scholar] [CrossRef]
- Chen, Y.; Cui, P.Y.; Pan, Y.Y.; Li, Y.X.; Waili, N.; Li, Y. Association between housing environment and depressive symptoms among older people: A multidimensional assessment. BMC Geriatr. 2021, 21, 259. [Google Scholar] [CrossRef] [PubMed]
- Niza, I.L.; Gomes, G.C.C.; Broday, E.E. Indoor environmental quality models: A bibliometric, mapping and clustering review. Renew. Sustain. Energy Rev. 2024, 203, 114791. [Google Scholar] [CrossRef]
- Tsoulou, I.; He, R.; Senick, J.; Mainelis, G.; Andrews, C.J. Monitoring summertime indoor overheating and pollutant risks and natural ventilation patterns of seniors in public housing. Indoor Built Environ. 2023, 32, 992–1019. [Google Scholar] [CrossRef]
- Zhang, F.; Shi, L.; Liu, S.; Shi, J.; Cheng, M.; Xiang, T. The Ancient Town Residential Environment of the Elderly in Xiangxi Tujia: Survey, Questions, and Recommendations. Int. J. Environ. Res. Public Health 2022, 19, 10820. [Google Scholar] [CrossRef]
- Ackley, A.; Olanrewaju, O.I.; Oyefusi, O.N.; Enegbuma, W.I.; Olaoye, T.S.; Ehimatie, A.E.; Ukpong, E.; Akpan-Idiok, P. Indoor environmental quality (IEQ) in healthcare facilities: A systematic literature review and gap analysis. J. Build. Eng. 2024, 86, 108787. [Google Scholar] [CrossRef]
- Chen, Y.; Li, M.; Lu, J.; Chen, B. Influence of residential indoor environment on quality of life in China. Build. Environ. 2023, 232, 110068. [Google Scholar] [CrossRef]
- Baudet, A.; Baurès, E.; Blanchard, O.; Le Cann, P.; Gangneux, J.-P.; Florentin, A. Indoor Carbon Dioxide, Fine Particulate Matter and Total Volatile Organic Compounds in Private Healthcare and Elderly Care Facilities. Toxics 2022, 10, 136. [Google Scholar] [CrossRef]
- Cui, P.; Zhang, J.; Li, T.T. Research on Acoustic Environment in the Building of Nursing Homes Based on Sound Preference of the Elderly People: A Case Study in Harbin, China. Front. Psychol. 2021, 12, 707457. [Google Scholar] [CrossRef] [PubMed]
- Mu, J.; Kang, J. Indoor Environmental Quality of Residential Elderly Care Facilities in Northeast China. Front. Public Health 2022, 10, 860976. [Google Scholar] [CrossRef]
- Cubukcuoglu, C.; Kunduraci, A.C.; Zarkhah, S.A.A. Indoor Environmental Quality Optimisation Model for Institutional Care Rooms of Elderly People. Buildings 2023, 13, 2625. [Google Scholar] [CrossRef]
- Hansen, A.; Williamson, T.; Pisaniello, D.; Bennetts, H.; van Hoof, J.; Martins, L.A.; Visvanathan, R.; Zuo, J.; Soebarto, V. The Thermal Environment of Housing and Its Implications for the Health of Older People in South Australia: A Mixed-Methods Study. Atmosphere 2022, 13, 96. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef] [PubMed]
- JBI. JBI Manual for Evidence Synthesis. Refined.site. 2021. Available online: https://jbi-global-wiki.refined.site/space/MANUAL (accessed on 16 August 2025).
- Thomas, J.; Harden, A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med. Res. Methodol. 2008, 8, 45. [Google Scholar] [CrossRef]
- Allsop, D.B.; Chelladurai, J.M.; Kimball, E.R.; Marks, L.D.; Hendricks, J.J. Qualitative Methods with Nvivo Software: A Practical Guide for Analyzing Qualitative Data. Psych 2022, 4, 142–159. [Google Scholar] [CrossRef]
- Yuan, J.; Cong, Y.; Yao, S.; Dai, C.; Li, Y. Research on the thermal comfort of the elderly in rural areas of cold climate, China. Adv. Build. Energy Res. 2022, 16, 612–642. [Google Scholar] [CrossRef]
- Xu, S.; Zhang, T.; Fukuda, H.; He, J.; Bao, X. Comprehensive Study of Residential Environment Preferences and Characteristics among Older Adults: Empirical Evidence from China. Buildings 2024, 14, 2175. [Google Scholar] [CrossRef]
- Xie, X.; Yang, Q.; Gao, W. Field measurement and questionnaire survey on indoor environment in typical coastal villages of Qingdao (China) during the heating period. Case Stud. Therm. Eng. 2021, 26, 101048. [Google Scholar] [CrossRef]
- Sudarsanam, N.; Kannamma, D. Investigation of summertime thermal comfort at the residences of elderly people in the warm and humid climate of India. Energy Build. 2023, 291, 113151. [Google Scholar] [CrossRef]
- Su, Y.; Gong, A.; Wang, C.; Han, Y.; Gao, W. Exploring thermal comfort for the older adults: A comparative study in Dalian City’s diverse living environments. Front. Arch. Res. 2025, 14, 812–824. [Google Scholar] [CrossRef]
- Qiao, D.; Wu, S.; Xiang, L.; Zhang, N. Association of residential environment with depression and anxiety symptoms among older adults in China: A cross-sectional population-based study. Build. Environ. 2024, 257, 111535. [Google Scholar] [CrossRef]
- Grudzińska, M.; Stabryła, R.; Siwek, K.; Bartoszek, K.; Wankiewicz, J. Perception of Summer Conditions in Prefabricated Multifamily Buildings Occupied by Middle-Aged and Elderly People Based on Monitoring of Dwellings in Warm-Summer Humid Continental Climate. Appl. Sci. 2024, 14, 11505. [Google Scholar] [CrossRef]
- Lv, Y.; Zhu, R.; Xie, J.; Yoshino, H. Indoor environment and the blood pressure of elderly in the cold region of China. Indoor Built Environ. 2022, 31, 2482–2498. [Google Scholar] [CrossRef]
- Liu, F.; Li, Y.; Gao, X.; Du, J. The Association between Perceived Housing Environment and Health and Satisfaction among the Older Adults during the COVID-19 Pandemic: A Cross-Sectional Survey in Northern China. Buildings 2023, 13, 2875. [Google Scholar] [CrossRef]
- Li, H.; Xu, G.; Chen, J.; Duan, J. Investigating the Adaptive Thermal Comfort of the Elderly in Rural Mutual Aid Homes in Central Inner Mongolia. Sustainability 2022, 14, 6802. [Google Scholar] [CrossRef]
- Kajjoba, D.; Olupot, P.W.; Kirabira, J.B.; Wesonga, R.; Ssemuddu, J.B.; Mugwanya, R.; Kasedde, H. Impact of natural ventilation on the subjective thermal comfort in low-income tropical housing. Next Res. 2025, 2, 100170. [Google Scholar] [CrossRef]
- Kajjoba, D.; Kasedde, H.; Kirabira, J.B.; Wesonga, R.; Mugwanya, R.; Lwanyaga, J.D.; Olupot, P.W. Impact of natural ventilation and outdoor environment on indoor air quality and occupant health in low-income tropical housing. Energy Rep. 2024, 12, 4184–4194. [Google Scholar] [CrossRef]
- Jiao, Y.; Yu, H.; Yu, Y.; Wang, Z.; Wei, Q. Adaptive thermal comfort models for homes for older people in Shanghai, China. Energy Build. 2020, 215, 109918. [Google Scholar] [CrossRef]
- Gong, X.; Yu, Y.; Lai, S.; Wang, X.; Duan, X.; Liu, J.; Wang, W. A Field Investigation on Summer Thermal Comfort of Occupants of Rural Houses in the North Area of Hot Summer and Warm Winter Zone, China. Buildings 2025, 15, 715. [Google Scholar] [CrossRef]
- Gabel, C.; Sigsgaard, T.; Petersen, S.; Elholm, G. The prevalence and association of measured and perceived indoor air quality, housing characteristics, and residents’ behavior and health. Front. Environ. Health 2024, 3, 1358546. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, B.; Caneparo, L.; Meng, Q.; Guo, W.; Liu, X. Physical Environment Study on Social Housing Stock in Italian Western Alps for Healthy and Sustainable Communities. Land 2023, 12, 1468. [Google Scholar] [CrossRef]
- Arentshorst, M.; Peine, A. From niche level innovations to age-friendly homes and neighbourhoods: A multi-level analysis of challenges, barriers and solutions. Technol. Anal. Strat. Manag. 2018, 30, 1325–1337. [Google Scholar] [CrossRef]
- Fan, G.; Xie, J.; Liu, J.; Yoshino, H. Investigation of indoor environmental quality in urban dwellings with schoolchildren in Beijing, China. Indoor Built Environ. 2017, 26, 694–716. [Google Scholar] [CrossRef]
- Giamalaki, M.; Kolokotsa, D. Understanding the thermal experience of elderly people in their residences: Study on thermal comfort and adaptive behaviors of senior citizens in Crete, Greece. Energy Build. 2019, 185, 76–87. [Google Scholar] [CrossRef]
- Tamiya, N.; Noguchi, H.; Nishi, A.; Reich, M.R.; Ikegami, N.; Hashimoto, H.; Shibuya, K.; Kawachi, I.; Campbell, J.C. Population ageing and wellbeing: Lessons from Japan’s long-term care insurance policy. Lancet 2011, 378, 1183–1192. [Google Scholar] [CrossRef]
- Tong, X.; Wang, B.; Dai, W.T.; Cao, J.J.; Ho, S.S.H.; Kwok, T.C.; Lui, K.H.; Lo, C.M.; Ho, K.F. Indoor air pollutant exposure and determinant factors controlling household air quality for elderly people in Hong Kong. Air Qual. Atmos. Health 2018, 11, 695–704. [Google Scholar] [CrossRef]
- Kim, J.-Y.; Sung-Jun, P. AI-Driven Biophilic Façade Design for Senior Multi-Family Housing Using LoRA and Stable Diffusion. Buildings 2025, 15, 1546. [Google Scholar] [CrossRef]
- Umishio, W.; Ikaga, T.; Fujino, Y.; Ando, S.; Kubo, T.; Nakajima, Y.; Kagi, N.; Hoshi, T.; Suzuki, M.; Kario, K.; et al. Spatial and temporal indoor temperature differences at home and perceived coldness in winter: A cross-sectional analysis of the nationwide Smart Wellness Housing survey in Japan. Environ. Int. 2024, 186, 108630. [Google Scholar] [CrossRef]
- Hashemi, A.; Dungrani, M. Indoor Environmental Quality and Health Implications of Building Retrofit and Occupant Behaviour in Social Housing. Sustainability 2025, 17, 264. [Google Scholar] [CrossRef]
- ISO 28803:2012; Ergonomics of the Thermal Environment—Application of International Standards to People with Special Requirements. International Organization for Standardization: Geneva, Switzerland, 2012.
- Li, Y.; Gu, Y.; Li, Z.; Zhang, X.; Gao, W.; Xiao, F. Study on the challenge and influence of the built thermal environment on elderly health in rural areas: Evidence from Shandong, China. Build. Simul. 2023, 16, 1345–1360. [Google Scholar] [CrossRef]
- Zheng, W.J.; Yao, H.Y.; Liu, J.J.; Yu, S.C. Developing a Subjective Evaluation Scale for Assessing the Built Environments of China’s Hygienic City Initiative. Biomed. Environ. Sci. 2021, 34, 372–378. [Google Scholar] [CrossRef]
- Yang, M.; Yaman, R.; Ismail, F.Z. Age-inclusive urban design: A review of sustainable retrofit strategies for elderly well-being. J. Infrastruct. Policy Dev. 2024, 8, 3797. [Google Scholar] [CrossRef]
- Oswald, F.; Wahl, H.-W.; Schilling, O.; Nygren, C.; Fänge, A.; Sixsmith, A.; Sixsmith, J.; Széman, Z.; Tomsone, S.; Iwarsson, S. Relationships Between Housing and Healthy Aging in Very Old Age. Gerontologist 2007, 47, 96–107. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).