Abstract
Background/Objectives: This study aimed to develop a machine learning (ML) algorithm that can predict unplanned reoperations and surgical/medical complications after vestibular schwannoma (VS) surgery. Methods: All pre- and peri-operative variables available in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database (n = 110), except those directly related to our outcome variables, were used as input variables. A deep neural network model consisting of seven layers was developed using the Keras open-source library, with a 70:30 breakdown for training and testing. The feature importance of input variables was measured to elucidate their relative permutation effect in the ML model. Results: Of the 1783 patients with VS undergoing surgery, unplanned reoperation, surgical complications, and medical complications were seen in 8.5%, 5.2%, and 6.2% of patients, respectively. The deep neural network model had area under the curve of receiver operating characteristics (ROC-AUC) of 0.6315 (reoperation), 0.7939 (medical complications), and 0.719 (surgical complications). Accuracy, specificity, and negative predictive values of the model for all outcome variables ranged from 82.1 to 96.6%, while positive predictive values and sensitivity ranged from 16.7 to 51.5%. Variables such as the length of stay post-operation until discharge, days from operation to discharge, and the total hospital length of stay had the highest permutation importance. Conclusions: We developed an effective ML algorithm predicting unplanned reoperation and surgical/medical complications post-VS surgery. This may offer physicians guidance into potential post-surgical outcomes to allow for personalized medical care plans for VS patients.
1. Introduction
Vestibular schwannomas (VSs) are benign tumors that account for over 90% of cranial nerve schwannomas and 6–8% of intracranial tumors [1,2,3]. Since surgical resections of VS present with major challenges, many studies have characterized the complications and reoperations following VS surgery [4,5,6,7]. While the safety of this procedure has significantly improved over the past years because of advancements in surgical techniques [8], risks remain and complications and reoperations following VS surgery continue to be a substantial burden on patients and the healthcare system. This has heightened the importance of improving post-VS surgery predictive capabilities to minimize surgical outcome risk.
Recent developments in machine learning (ML) and increases in available annotated medical data have allowed for the successful application of these technologies to many fields of medicine [9,10,11]. Artificial neural networks (ANNs) are one type of ML that outperform traditional statistical methods when manipulating large datasets with an inherent nonlinear distribution that is not well understood [12]. Since many clinical variables, such as risk factors or treatment outcomes, possess multivariate causes, ANN’s features make it a strong candidate for predictive analyses in a wide variety of medical disciplines. However, it has yet to be applied to predictions of post-surgical outcomes for VS surgery.
Given such information, the aim of this study was to develop an ANN algorithm, specifically a deep neural network (DNN), that can predict unplanned reoperation, surgical complications, and medical complications after VS surgery. The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database was used to train and validate the algorithm. Such technology could serve as a useful predictive tool for mitigating the effect of given problems on patients and healthcare infrastructure alike.
2. Materials and Methods
Reporting 30-day morbidity and mortality information for many surgical operations, the ACS-NSQIP database was retrospectively reviewed for data from the years 2007 to 2019. A total of 1783 patients with a diagnosis of VS undergoing surgery were identified using the ICD-9 and ICD-10 codes 225.1 and D33.3. Out of these patients, we selected those who specifically underwent head and neck surgery according to current procedural terminology (CPT) codes related to VS surgery (see Table 1).

Table 1.
List of procedures and associated CPT codes related to VS surgery. CTBC, Craniectomy, Trephination, and Bone Flap Craniotomy; IPF, Infratentorial or Posterior Fossa; CBTC = Craniectomy, Bone Flap Craniotomy, and Transtemporal Excision; PJM, Posterior Cranial Fossa, Jugular Foramen, or Midline Skull Base; IPP, Infratemporal Fossa, Parapharyngeal Space, or Petrous Apex; PCF, Posterior Cranial Fossa, Clivus, or Foramen Magnum.
Three primary outcomes of interest were predicted: the occurrence of an unplanned reoperation, surgical complications, and medical complications. For reoperations, we used the “RETURNOR” variable, which indicates an unplanned reoperation. Multiple variables, such as blood transfusions within 72 h, wound disruptions, the occurrences of superficial surgical site infections (SSIs), organ/space SSIs, and deep SSIs, were used to determine surgical complications. Finally, medical complications included occurrences of renal insufficiency, pneumonia, being on ventilation for more than 48 h, unplanned reintubation, myocardial infarction, urinary tract infections, deep vein thrombosis, pulmonary embolism, acute renal failure, cerebrovascular accidents with neurological deficits, septic shock, cardiac arrest requiring cardiopulmonary resuscitation, or sepsis.
A total of 110 preoperative, operative, and post-operative variables were selected as input variables. The data were acquired from three separate Excel datasets that contained data concerning medical complications, reoperative cases, and surgical complications. All three datasets were imported into Python and merged into a single dataset. The CASEID (a unique identifier specific to each data entry and unique in structure for each data source) was used to discriminate between the data sources after merging. During the merge, some datasets were found to have available data that other datasets lacked. To resolve this, we consistently prioritized the available data for our analyses.
To prepare for analysis, binary variables, like LOS_binary (length of stay) and ASA_binary (ASA), were label-encoded to simplify the classification process. Multi-class categorical variables were one-hot encoded to keep them interpretable. The main outcome variables—REOPERATION (reoperation), Surg_Comp (surgical complications), and Med_Comp (Medical complications)—were converted to binary indicators, where 1 represented “yes” and 0 represented “No”.
Exploratory Data Analysis (EDA) was conducted to examine the relationships between predictor variables and outcomes. Statistical measures and visualization techniques were used, guided by a custom analyze_x_against_y function that streamlined the analysis of relationships between predictors and outcomes. Categorical variables were dummy-coded to ensure compatibility with machine learning models. Correlation matrices were generated to assess associations between predictors and outcomes. Additionally, mean ratio analysis was used to calculate the proportion of positive cases for each predictor, which helped us identify those variables that possessed strong links to outcomes.
A screening process using area under the curve of receiver operating characteristics (ROC-AUC) scores was employed next to assess each predictor’s ability to distinguish between outcomes. Categorical variables were evaluated using decision tree classifiers, whereas numerical variables were evaluated with logistic regression. Only those variables that possessed an ROC-AUC score of 0.55 or higher were retained for modeling. For predictive modeling, an XGBoost classifier was implemented for each outcome.
The model used a refined set of predictors and a strong classification pipeline. Predictors possessed an ROC-AUC score above 0.55, which included categorical and numerical variables that were selected based on the EDA results. To address any imbalance in the outcome data, the scale_pos_weight parameter was adjusted to improve the model’s accuracy by balancing positive and negative cases in the target variable. Each outcome dataset was split into training (70%) and testing (30%) subsets using stratified sampling. Key hyperparameters (including n_estimators, max_depth, learning_rate, subsample, colsample_bytree, lambda, and alpha) were fine-tuned using the GridSearchCV class to maximize the ROC-AUC score. Additionally, three-fold cross-validation within GridSearchCV improved model reliability by reducing overfitting.
Feature engineering was applied to procedural and work relative value unit (WRVU) codes. Procedural codes (CONCPT) were transformed into a binary matrix, which indicated the presence of each unique code for each case. An aggregated column was added to the matrix to represent the total number of procedures. WRVU codes were processed in a similar way, with counts capturing the extent of interventions each patient received. Each final model incorporated the original variables (e.g., CONCPT, CONWRVU, OTHERCPT, OTHERPROC, OTHERWRVU) to improve predictive accuracy.
Model performance was evaluated using accuracy, sensitivity, specificity, F1 score, ROC-AUC, precision–recall area under the curve (PR-AUC), negative predictive value (NPV), and positive predictive value (PPV). Receiver operating characteristics (ROCs) and precision–recall (PR) curves were plotted to visualize performance, and area under the curve (AUC) values were calculated for both. Feature importance was derived from the final models, and the top 20 predictors were visualized. The best-performing model for each outcome, along with the feature sets used, were saved in an organized directory to ensure reproducibility. The top 10 predictors for each outcome were extracted.
3. Results
This study comprised 1783 patients overall. In total, 765 (42.9%) were male patients and 1018 were female (57.1%). Furthermore, 1289 patients were white (72.3%), 83 (4.66%) were Black or African American, 82 (4.60%) were Asian, and 43 (2.41%) were Hispanic. The mean age of the cohort was 50.4 ± 13.9 years.
Out of the total of 1783 patients, 151 (8.5%) had undergone a reoperation, 111 (6.2%) had experienced medical complications, and 92 (5.2%) had experienced surgical complications. The ROC-AUC value for the predicted occurrence of reoperation in the test dataset was 0.6315. The corresponding accuracy of prediction was 0.8206, the sensitivity was 0.3111, the specificity was 0.8673, the PPV (precision) was 0.1772, the NPV was 0.932, the F1 score was 0.2258, and the PR-AUC was 0.1968. The ROC-AUC score for the predicted occurrence of medical complications in the test dataset was 0.7939, along with an accuracy of 0.8692, a sensitivity of 0.5152, a specificity of 0.8924, a PPV of 0.2394, an NPV of 0.9655, an F1 score of 0.3269, and a PR-AUC of 0.2208. Finally, the ROC-AUC value for the predicted occurrence of surgical complications in the test dataset was 0.719, while the accuracy of prediction was 0.8729, the sensitivity was 0.3571, the specificity was 0.9014, the PPV was 0.1667, the NPV was 0.9621, the F1 score was 0.2273, and the PR-AUC was 0.1795. Table 2 and Figure 1 and Figure 2 relay the evaluation statistics, PR curves, and ROC curves for all predictions.

Table 2.
Model performance statistics for predicting the occurrence of reoperation, medical complications, and surgical complications (classification threshold = 0.55).
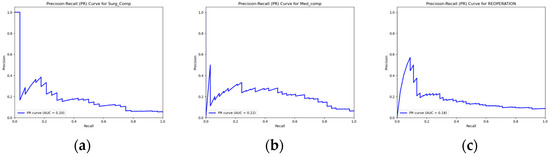
Figure 1.
PR curves for predictions of (a) surgical complications; (b) medical complications; and (c) reoperation.
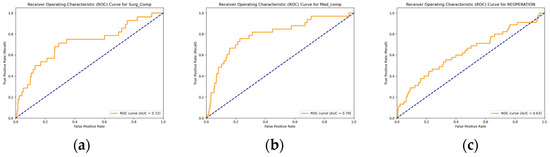
Figure 2.
ROC curve for predictions of (a) surgical complications; (b) medical complications; and (c) reoperation.
Finally, the permutation importance of each variable’s outcome-predicting capabilities was calculated. The top 10 most important features for predicting each outcome are listed in Table 3. Though there was some variance depending on the outcome variables, features including the length of stay post-operation until discharge, days from operation to discharge, and the total hospital length of stay were categorized as the most important predictive features.

Table 3.
The top 10 important variables for predictions of a reoperation occurrence, medical complication, and surgical complication. ALKPHOS, alkaline phosphatase; WBC, white blood count; INR, international normalized ratio; SGOT, Serum Glutamic Oxaloacetic Transaminase; ASA, American Society of Anesthesiologists.
4. Discussion
Reoperations and complications post-surgery undoubtedly place mental and physical tolls on patients [13]. It also places a burden on the healthcare system, given that rehospitalization post-discharge has been estimated to cost USD 17 billion annually in avoidable Medicare expenditures [14]. The Agency for Healthcare Research and Quality has been implemented to combat this issue; however, this has contributed to controversies regarding readmission rates and reimbursements [15]. A high-quality predictive model could mitigate this issue by offering physicians insights into potential post-surgical outcomes and allowing them to devise a more personalized treatment plan. ANN developments have enabled many researchers to apply this technology for predictions of various surgical variables including length of stay, readmission, complication, recurrence, and reoperation among various specialties [10,16,17]. However, similar studies in the literature regarding VS remain very scarce, and to our understanding, our study is one of the first to predict occurrences of reoperation, surgical complications, and medical complications following surgical removal of VS.
Our DNN algorithm reached an AUC-ROC of 0.6315, 0.7939, and 0.719 for predicting occurrences of reoperation, medical complications, and surgical complications, respectively. These results match those of other studies that utilized ANN algorithms to predict post-operation factors for other surgical procedures such as those in orthopedic surgery and neurosurgery [16,17]. Medical outcomes are dependent on a variety of factors, of which many of these are often based on complex relationships that may not be explicit. ANN is poised for these scenarios, since no previous knowledge regarding the importance of specific input variables is needed, and the model can also detect relationships between input and output variables automatically [18,19]. In contrast, other ML techniques, such as logistic regressions and random forest classifiers, perform well when the input dataset is relatively streamlined to include minimal variables that are known to be important in predicting the outcome variable [18]. Though it is oftentimes difficult to assess which types of algorithms are best suited for each task at hand, our results clearly show that a DNN algorithm was able to predict post-surgical VS complications and reoperations in the present study.
An interesting and meaningful aspect of our study was the characterization of variables that highly influenced the algorithm’s ability to predict occurrences of complications and reoperations. These variables could be monitored for future treatments of VS to potentially improve patient outcomes. Variable importance for ANN classifications cannot be currently measured directly, and hence, we utilized a method that measures model performance when a specific variable is removed from the dataset. Variables with a higher decrease in performance were regarded as more important. It was therefore notable that the length of stay post-operation until discharge, days from operation to discharge, and the total hospital length of stay were determined as the most important variables for predictions. Though this method provides insights into the importance of individual variables, it is important to note that it does not provide an explanation of how each variable precisely influences the prediction. ML explainability and interpretation is a topic that is under extensive investigation, and there is currently no method that extracts the true importance of each variable [20]. Hence, these findings should be referenced with caution.
While the negative predictive value of our model was very high, averaging at 0.953 between the three variables at a classification threshold of 0.55, the positive predictive value was relatively low, averaging at 0.194. This indicates that our DNN model was particularly proficient in identifying cases that were not followed by post-operative complications or reoperations and that positive cases were more difficult to predict given the variables inputted into the model. Patients with head and neck cancer have been identified as a high-risk group for readmission, with their rates ranging between 6% and 26.5% [21,22,23,24]. Though the Hospital Readmissions Reduction Program (HRRP) has not been implemented for head and neck surgery, many studies have pointed out the likeliness of the program expanding to cover such procedures in the future [25,26]. Our study has illustrated that a significant part of complication or reoperation negative VS cases were highly predictable. Hence, a predictive model based on the ANN algorithm developed through this study may become useful in the future for developing a stratified model in which hospitals will be penalized for post-surgical incidences only for cases that were predicted to have a low probability of such events occurring.
Similar predictive indices have been considered before, such as the LACE+ (length of stay, acuity, comorbidities, and emergency presentations) index, which predicts an early death or urgent readmission after hospital discharge [27]. Furthermore, the University of Kansas Health Systems and Atrium Health have both successfully implemented predictive programs that analyze clinical and socioeconomic factors after hospital discharge, resulting in a successful reduction in their readmission rates [28]. Nonetheless, neither program has employed ML techniques. Incorporating the predictive capacity of ANN or alternate ML algorithms into such frameworks could improve the quality of these risk-stratification models, allowing healthcare professionals to appropriately measure the risk of post-surgical outcomes, thereby benefiting not only the healthcare system but also patients by providing them with more information and tailored guidance regarding their treatment.
Despite the many findings, it is important to mention several limitations of our study. The performance of classifiers is inherently rooted in the quality of the training dataset, which, in the case of this present study, was the ACS-NSQIP database. Most datasets are subject to errors, and this is no different for the NSQIP database, as shown by a previous study that reported inaccuracies in CPT coding among neurosurgical procedures [29]. This database also may not be generalizable to all intended patients, given that the database only included a maximum of 708 hospitals [30]. Furthermore, the input variables of our model are limited to those included in the database. This inevitably omits potentially relevant variables for predicting post-surgical VS incidents, such as the presence of NF2 mutation status, tumor size or location, or surgical approaches, which could all impact the outcome of treatment [31,32].
A class imbalance also existed between cases of patients who presented without any post-surgical reoperations or complications and those who did, with all percentages being below 8.5%. Future adjustments, such as increasing the size of the dataset, may improve positive case detection and balance. On a similar note, the NSQIP database presented a plethora of missing data. Though we maneuvered this challenge by prioritizing the available data, in future studies, a more complete dataset could improve the performance of the algorithm.
5. Conclusions
A robust ML algorithm predicting unplanned reoperation and surgical or medical complications following VS surgery was developed. The model possessed an ROC-AUC of 0.6315, 0.7939, and 0.719 for prediction reoperation, medical complications, and surgical complications, respectively. Variables deemed to be most important for making predictions included those such as the length of stay post-operation until discharge, days from operation to discharge, and the total hospital length of stay. The above findings may offer physicians insights into potential post-surgical outcomes, though further investigations incorporating new algorithms and databases may be needed for the clinical implementation of a more personalized treatment plan for VS patients.
Author Contributions
Conceptualization, H.R.D. and M.A.; methodology, A.D., M.L., T.P. and M.A.; software, A.D. and M.L.; validation, A.D., K.B., M.L., T.P. and M.A.; formal analysis, A.D., M.L. and T.P.; investigation, A.D., K.B., M.L., T.P. and M.A.; data curation, A.D., M.L., T.P. and M.A.; writing—original draft preparation, A.D., K.B. and M.A.; writing—review and editing, A.D., K.B., M.L., T.P., H.R.D. and M.A.; visualization, M.L.; supervision, H.R.D. and M.A.; project administration, M.A.; funding acquisition, M.A. All authors have read and agreed to the published version of the manuscript.
Funding
M.A. was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, via Grant TL1TR001415.
Institutional Review Board Statement
Ethical review and approval were waived for this study given the public nature of the ACS-NSQIP database.
Informed Consent Statement
Informed consent was obtained from all surveyed participants, and any patient-identifying information was removed from the datasets.
Data Availability Statement
The data that support the findings of this study are available from the corresponding authors upon reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Skolnik, A.D.; Loevner, L.A.; Sampathu, D.M.; Newman, J.G.; Lee, J.Y.; Bagley, L.J.; Learned, K.O. Cranial Nerve Schwannomas: Diagnostic Imaging Approach. Radiographics 2016, 36, 1463–1477. [Google Scholar] [CrossRef]
- Bal, J.; Bruneau, M.; Berhouma, M.; Cornelius, J.F.; Cavallo, L.M.; Daniel, R.T.; Froelich, S.; Jouanneau, E.; Meling, T.R.; Messerer, M.; et al. Management of non-vestibular schwannomas in adult patients: A systematic review and consensus statement on behalf of the EANS skull base section. Part I: Oculomotor and other rare non-vestibular schwannomas (I, II, III, IV, VI). Acta Neurochir. 2022, 164, 285–297. [Google Scholar] [CrossRef]
- Reznitsky, M.; Petersen, M.M.B.S.; West, N.; Stangerup, S.E.; Cayé-Thomasen, P. Epidemiology of Vestibular Schwannomas—Prospective 40-Year Data from an Unselected National Cohort. Clin. Epidemiol. 2019, 11, 981–986. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Ahmed, A.K.; Bi, W.L.; Dawood, H.Y.; Iorgulescu, J.B.; Corrales, C.E.; Dunn, I.F.; Smith, T.R. Predicting Readmission and Reoperation for Benign Cranial Nerve Neoplasms: A Nationwide Analysis. World Neurosurg. 2019, 121, e223–e229. [Google Scholar] [CrossRef]
- Schackert, G.; Ralle, S.; Martin, K.D.; Reiss, G.; Kowalski, M.; Sobottka, S.B.; Hennig, S.; Podlesek, D.; Sandi-Gahun, S.; Juratli, T.A. Vestibular Schwannoma Surgery: Outcome and Complications in Lateral Decubitus Position Versus Semi-sitting Position—A Personal Learning Curve in a Series of 544 Cases over 3 Decades. World Neurosurg. 2021, 148, e182–e191. [Google Scholar] [CrossRef] [PubMed]
- Chiu, S.J.; Hickman, S.J.; Pepper, I.M.; Tan, J.H.Y.; Yianni, J.; Jefferis, J.M. Neuro-Ophthalmic Complications of Vestibular Schwannoma Resection: Current Perspectives. Eye Brain 2021, 13, 241–253. [Google Scholar] [CrossRef]
- Goshtasbi, K.; Abouzari, M.; Moshtaghi, O.; Maducdoc, M.; Lehrich, B.M.; Lin, H.W.; Djalilian, H.R. Risk Recall of Complications Associated with Vestibular Schwannoma Treatment. Otolaryngol. Head Neck Surg. 2019, 161, 330–335. [Google Scholar] [CrossRef] [PubMed]
- Zanoletti, E.; Mazzoni, A.; Martini, A.; Abbritti, R.V.; Albertini, R.; Alexandre, E.; Baro, V.; Bartolini, S.; Bernardeschi, D.; Bivona, R. Surgery of the lateral skull base: A 50-year endeavour. Acta Otorhinolaryngol. Ital. 2019, 39 (Suppl. S1), S1–S146. [Google Scholar] [CrossRef]
- Goyal, A.; Ngufor, C.; Kerezoudis, P.; McCutcheon, B.; Storlie, C.; Bydon, M. Can machine learning algorithms accurately predict discharge to nonhome facility and early unplanned readmissions following spinal fusion? Analysis of a national surgical registry. J. Neurosurg. Spine 2019, 31, 568–578. [Google Scholar] [CrossRef] [PubMed]
- Merath, K.; Hyer, J.M.; Mehta, R.; Farooq, A.; Bagante, F.; Sahara, K.; Tsilimigras, D.I.; Beal, E.; Paredes, A.Z.; Wu, L.; et al. Use of Machine Learning for Prediction of Patient Risk of Postoperative Complications After Liver, Pancreatic, and Colorectal Surgery. J. Gastrointest. Surg. 2020, 24, 1843–1851. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, Y.; Tsuzuki, T.; Akatsuka, J.; Ueki, M.; Morikawa, H.; Numata, Y.; Takahara, T.; Tsuyuki, T.; Tsutsumi, K.; Nakazawa, R.; et al. Automated acquisition of explainable knowledge from unannotated histopathology images. Nat. Commun. 2019, 10, 5642. [Google Scholar] [CrossRef]
- Chen, J.H.; Asch, S.M. Machine Learning and Prediction in Medicine—Beyond the Peak of Inflated Expectations. N. Engl. J. Med. 2017, 376, 2507–2509. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.; Faiz, O.; Davis, R.; Almoudaris, A.; Vincent, C. Surgical complications and their impact on patients’ psychosocial well-being: A systematic review and meta-analysis. BMJ Open 2016, 6, e007224. [Google Scholar] [CrossRef]
- Hamadi, H.Y.; Martinez, D.; Palenzuela, J.; Spaulding, A.C. Magnet Hospitals and 30-Day Readmission and Mortality Rates for Medicare Beneficiaries. Med. Care 2021, 59, 6–12. [Google Scholar] [CrossRef]
- Agency for Healthcare Research and Quality. Preventing Avoidable Readmissions. Available online: https://www.ahrq.gov/patient-safety/resources/improve-discharge/index.html (accessed on 25 September 2020).
- Biron, D.R.; Sinha, I.; Kleiner, J.E.; Aluthge, D.P.; Goodman, A.D.; Sarkar, I.N.; Cohen, E.; Daniels, A.H. A Novel Machine Learning Model Developed to Assist in Patient Selection for Outpatient Total Shoulder Arthroplasty. J. Am. Acad. Orthop. Surg. 2020, 28, e580–e585. [Google Scholar] [CrossRef]
- Karhade, A.V.; Thio, Q.C.; Ogink, P.T.; Shah, A.A.; Bono, C.M.; Oh, K.S.; Saylor, P.J.; Schoenfeld, A.J.; Shin, J.H.; Harris, M.B.; et al. Development of Machine Learning Algorithms for Prediction of 30-Day Mortality After Surgery for Spinal Metastasis. Neurosurgery 2019, 85, E83–E91. [Google Scholar] [CrossRef]
- Sheth, V.; Tripathi, U.; Sharma, A. A Comparative Analysis of Machine Learning Algorithms for Classification Purpose. Procedia Comput. Sci. 2022, 215, 422–431. [Google Scholar] [CrossRef]
- Hassanipour, S.; Ghaem, H.; Arab-Zozani, M.; Seif, M.; Fararouei, M.; Abdzadeh, E.; Sabetian, G.; Paydar, S. Comparison of artificial neural network and logistic regression models for prediction of outcomes in trauma patients: A systematic review and meta-analysis. Injury 2019, 50, 244–250. [Google Scholar] [CrossRef]
- Zhang, Z.; Beck, M.W.; Winkler, D.A.; Huang, B.; Sibanda, W.; Goyal, H. Opening the black box of neural networks: Methods for interpreting neural network models in clinical applications. Ann. Transl. Med. 2018, 6, 216. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Meza, G.; McKee, S.; Carlton, D.; Yang, A.; Govindaraj, S.; Iloreta, A. Association of Surgical and Hospital Volume and Patient Characteristics with 30-Day Readmission Rates. JAMA Otolaryngol. Head Neck Surg. 2019, 145, 328–337. [Google Scholar] [CrossRef]
- Graboyes, E.M.; Yang, Z.; Kallogjeri, D.; Diaz, J.A.; Nussenbaum, B. Patients undergoing total laryngectomy: An at-risk population for 30-day unplanned readmission. JAMA Otolaryngol. Head Neck Surg. 2014, 140, 1157–1165. [Google Scholar] [CrossRef] [PubMed]
- Ferrandino, R.; Garneau, J.; Roof, S.; Pacheco, C.; Poojary, P.; Saha, A.; Chauhan, K.; Miles, B. The national landscape of unplanned 30-day readmissions after total laryngectomy. Laryngoscope 2018, 128, 1842–1850. [Google Scholar] [CrossRef] [PubMed]
- Dziegielewski, P.T.; Boyce, B.; Manning, A.; Agrawal, A.; Old, M.; Ozer, E.; Teknos, T.N. Predictors and costs of readmissions at an academic head and neck surgery service. Head Neck 2016, 38 (Suppl. S1), E502–E510. [Google Scholar] [CrossRef]
- Bur, A.M.; Brant, J.A.; Mulvey, C.L.; Nicolli, E.A.; Brody, R.M.; Fischer, J.P.; Cannady, S.B.; Newman, J.G. Association of Clinical Risk Factors and Postoperative Complications With Unplanned Hospital Readmission After Head and Neck Cancer Surgery. JAMA Otolaryngol. Head Neck Surg. 2016, 142, 1184–1190. [Google Scholar] [CrossRef] [PubMed]
- Goel, A.N.; Raghavan, G.; St John, M.A.; Long, J.L. Risk Factors, Causes, and Costs of Hospital Readmission After Head and Neck Cancer Surgery Reconstruction. JAMA Facial Plast. Surg. 2019, 21, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Rajaguru, V.; Han, W.; Kim, T.H.; Shin, J.; Lee, S.G. LACE Index to Predict the High Risk of 30-Day Readmission: A Systematic Review and Meta-Analysis. J. Pers. Med. 2022, 12, 545. [Google Scholar] [CrossRef] [PubMed]
- Cryts, A. How Two Health Systems Use Predictive Analytics to Reduce Readmissions. Managed Healthcare Executive Website. 2018. Available online: https://www.managedhealthcareexecutive.com/view/how-two-health-systems-use-predictive-analytics-reduce-readmissions (accessed on 6 September 2020).
- Rolston, J.D.; Han, S.J.; Chang, E.F. Systemic inaccuracies in the National Surgical Quality Improvement Program database: Implications for accuracy and validity for neurosurgery outcomes research. J. Clin. Neurosci. 2017, 37, 44–47. [Google Scholar] [CrossRef]
- American College of Surgeons. ACS NSQIP Participant Use Data File. American College of Surgeons Website. 2017. Available online: https://www.facs.org/quality-programs/acs-nsqip/participant-use (accessed on 7 September 2020).
- Patel, V.A.; Dunklebarger, M.; Banerjee, K.; Shokri, T.; Zhan, X.; Isildak, H. Surgical Management of Vestibular Schwannoma: Practice Pattern Analysis via NSQIP. Ann. Otol. Rhinol. Laryngol. 2020, 129, 230–237. [Google Scholar] [CrossRef]
- Mahboubi, H.; Maducdoc, M.M.; Yau, A.Y.; Ziai, K.; Ghavami, Y.; Badran, K.W.; Al-Thobaiti, M.; Brandon, B.; Djalilian, H.R. Vestibular Schwannoma Excision in Sporadic versus Neurofibromatosis Type 2 Populations. Otolaryngol. Head Neck Surg. 2015, 153, 822–831. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).