Development of an Exercise Rehabilitation Functional Group for Individualized Exercise After Lumbar Spine Surgery
Abstract
1. Introduction
2. Materials and Methods
2.1. Trial Design and Ethics
2.2. Study Aims
2.3. Sample Size
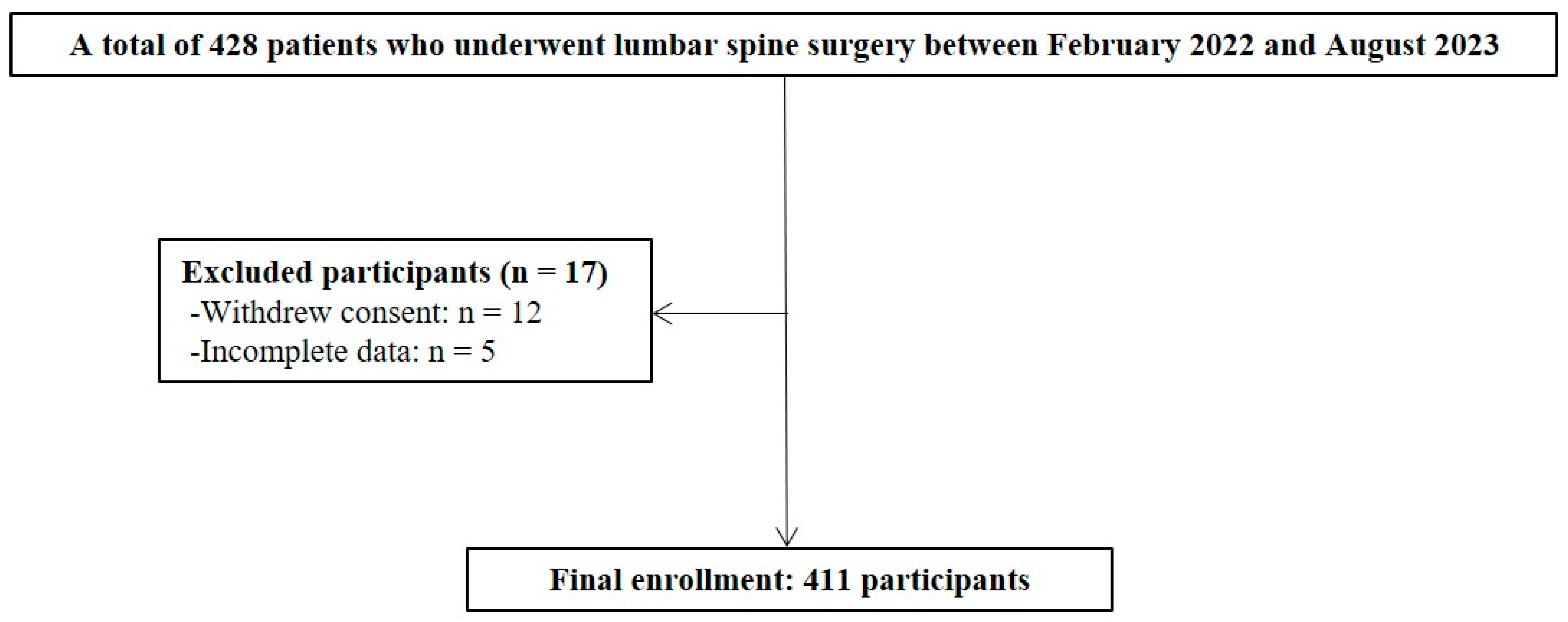
2.4. Participant Recruitment
2.5. Time Frame
2.6. ERFG Parameters and Assessment
2.7. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Overall Results of Parameters and ERFG Categorization
- (1)
- Mean range of motion of the lumbar spine: 74.24 ± 25.30°;
- (2)
- Mean strength of flex/extension: 15.71 ± 5.14 kg;
- (3)
- Mean endurance of flexion/extension: 95.80 ± 35.66 s;
- (4)
- Mean flexibility of the whole body: 3.30 ± 10.65 cm;
- (5)
- Mean cardiopulmonary capability: 433.91 ± 118.75 m;
- (6)
- Mean gait with affected single leg: 36.26 ± 5.98%;
- (7)
- Median single-leg balance of affected side: 13.60 (IQR, 3.02–32.00) seconds;
- (8)
- Mean coordination capability: 8.21 ± 3.23 s;
- (9)
- Mean EuroQol 5-Dimension 5-Level version: 9.39 ± 4.17,
- (10)
- Mean visual analog scale for low back pain: 3.78 ± 2.55.
3.3. Correlation Between Parameters
3.4. Safety and Side Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| EQ-5D-5L | EuroQol-5 Dimension 5-Level version |
| IQR | interquartile range |
| VAS | visual analog scale |
References
- Katz, J.N.; Zimmerman, Z.E.; Mass, H.; Makhni, M.C. Diagnosis and management of lumbar spinal stenosis: A review. JAMA 2022, 327, 1688–1699. [Google Scholar] [CrossRef] [PubMed]
- Abdi, A.; Bagheri, S.R.; Shekarbeigi, Z.; Usefvand, S.; Alimohammadi, E. The effect of repeated flexion-based exercises versus extension-based exercises on the clinical outcomes of patients with lumbar disk herniation surgery: A randomized clinical trial. Neurol. Res. 2023, 45, 28–40. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Y.; Ding, Y.; Fu, B.; Ma, G.; Cui, H.; Li, M.; Yu, Y.; Guan, L. The effectiveness of postoperative exercise based on gait analysis compared with conventional exercise in patients with lumbar spinal stenosis: A randomized clinical trial. J. Back Musculoskelet. Rehabil. 2023, 36, 1399–1409. [Google Scholar] [CrossRef]
- Jentoft, E.S.; Kvåle, A.; Assmus, J.; Moen, V.P. Effect of information and exercise programmes after lumbar disc surgery: A randomized controlled trial. Physiother. Res. Int. 2020, 25, e1864. [Google Scholar] [CrossRef] [PubMed]
- Master, H.; Pennings, J.S.; Coronado, R.A.; Bley, J.; Robinette, P.E.; Haug, C.M.; Skolasky, R.L.; Riley, L.H.; Neuman, B.J.; Cheng, J.S.; et al. How many steps per day during the early postoperative period are associated with patient-reported outcomes of disability, pain, and opioid use after lumbar spine surgery? Arch. Phys. Med. Rehabil. 2021, 102, 1873–1879. [Google Scholar] [CrossRef]
- Chakravarthy, V.; Yokoi, H.; Manlapaz, M.R.; Krishnaney, A.A. Enhanced recovery in spine surgery and perioperative pain management. Neurosurg. Clin. N. Am. 2020, 31, 81–91. [Google Scholar] [CrossRef]
- Kernc, D.; Strojnik, V.; Vengust, R. Early initiation of a strength training based rehabilitation after lumbar spine fusion improves core muscle strength: A randomized controlled trial. J. Orthop. Surg. Res. 2018, 13, 151. [Google Scholar] [CrossRef]
- Bagheri, R.; Takamjani, I.E.; Dadgoo, M.; Sarrafzadeh, J.; Ahmadi, A.; Pourahmadi, M.R.; Jafarpisheh, A.S. A protocol for clinical trial study of the effect of core stabilization exercises on spine kinematics during gait with and without load in patients with non-specific chronic low back pain. Chiropr. Man. Ther. 2017, 25, 31. [Google Scholar] [CrossRef]
- Lamoth, C.J.; Meijer, O.G.; Daffertshofer, A.; Wuisman, P.I.; Beek, P.J. Effects of chronic low back pain on trunk coordination and back muscle activity during walking: Changes in motor control. Eur. Spine J. 2006, 15, 23–40. [Google Scholar] [CrossRef]
- Janssen, E.R.C.; Punt, I.M.; Clemens, M.J.; Staal, J.B.; Hoogeboom, T.J.; Willems, P.C. Current prehabilitation programs do not improve the postoperative outcomes of patients scheduled for lumbar spine surgery: A systematic review with meta-analysis. J. Orthop. Sports Phys. Ther. 2021, 51, 103–114. [Google Scholar] [CrossRef]
- Son, S.; Yoo, B.R.; Jeong, Y.M. Digital therapeutics-based lumbar core exercise for patients with low back pain: A prospective exploratory pilot study. Digit. Health 2024, 10, 20552076231218154. [Google Scholar] [CrossRef] [PubMed]
- Kjeken, I.; Berdal, G.; Bø, I.; Dager, T.; Dingsør, A.; Hagfors, J.; Hamnes, B.; Eppeland, S.G.; Fjerstad, E.; Mowinckel, P.; et al. Evaluation of a structured goal planning and tailored follow-up programme in rehabilitation for patients with rheumatic diseases: Protocol for a pragmatic, stepped-wedge cluster randomized trial. BMC Musculoskelet. Disord. 2014, 15, 153. [Google Scholar] [CrossRef]
- Frey, M.; Greene, R.; De Carvalho, D. What is the best way to collect maximum forward lumbar spine flexion values for normalizing posture to range of motion? J. Biomech. 2020, 103, 109706. [Google Scholar] [CrossRef]
- Schendel, M.J.; Wood, K.B.; Buttermann, G.R.; Lewis, J.L.; Ogilvie, J.W. Experimental measurement of ligament force, facet force, and segment motion in the human lumbar spine. J. Biomech. 1993, 26, 427–438. [Google Scholar] [CrossRef] [PubMed]
- Ng, J.K.; Kippers, V.; Richardson, C.A.; Parnianpour, M. Range of motion and lordosis of the lumbar spine: Reliability of measurement and normative values. Spine 2001, 26, 53–60. [Google Scholar] [CrossRef]
- García-Vaquero, M.P.; Barbado, D.; Juan-Recio, C.; López-Valenciano, A.; Vera-Garcia, F.J. Isokinetic trunk flexion-extension protocol to assess trunk muscle strength and endurance: Reliability, learning effect, and sex differences. J. Sport. Health Sci. 2020, 9, 692–701. [Google Scholar] [CrossRef] [PubMed]
- Ito, T.; Shirado, O.; Suzuki, H.; Takahashi, M.; Kaneda, K.; Strax, T.E. Lumbar trunk muscle endurance testing: An inexpensive alternative to a machine for evaluation. Arch. Phys. Med. Rehabil. 1996, 77, 75–79. [Google Scholar] [CrossRef]
- Mayorga-Vega, D.; Merino-Marban, R.; Viciana, J. Criterion-related validity of sit-and-reach tests for estimating hamstring and lumbar extensibility: A meta-analysis. J. Sports Sci. Med. 2014, 13, 1–14. [Google Scholar]
- Agarwala, P.; Salzman, S.H. Six-minute walk test: Clinical role, technique, coding, and reimbursement. Chest 2020, 157, 603–611. [Google Scholar] [CrossRef]
- Mahzoun Alzakerin, H.; Halkiadakis, Y.; Morgan, K.D. Characterizing gait pattern dynamics during symmetric and asymmetric walking using autoregressive modeling. PLoS ONE 2020, 15, e0243221. [Google Scholar] [CrossRef]
- Kozinc, Ž.; Löfler, S.; Hofer, C.; Carraro, U.; Šarabon, N. Diagnostic balance tests for assessing risk of falls and distinguishing older adult fallers and non-fallers: A systematic review with meta-analysis. Diagnostics 2020, 10, 667. [Google Scholar] [CrossRef] [PubMed]
- Steffen, T.M.; Hacker, T.A.; Mollinger, L. Age- and gender-related test performance in community-dwelling elderly people: Six-minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys. Ther. 2002, 82, 128–137. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Obradovic, M.; Lal, A.; Liedgens, H. Validity and responsiveness of EuroQol-5 dimension (EQ-5D) versus Short Form-6 dimension (SF-6D) questionnaire in chronic pain. Health Qual. Life Outcomes 2013, 11, 110. [Google Scholar] [CrossRef]
- Shafshak, T.S.; Elnemr, R. The visual analogue scale versus numerical rating scale in measuring pain severity and predicting disability in low back pain. J. Clin. Rheumatol. 2021, 27, 282–285. [Google Scholar] [CrossRef] [PubMed]
- Jeoung, B.; Pyun, D.Y. Investigating functional fitness of older adults in Korea in the period 2013–2018. Sci. Rep. 2022, 12, 6073. [Google Scholar] [CrossRef]
- Dal Farra, F.; Arippa, F.; Arru, M.; Cocco, M.; Porcu, E.; Tramontano, M.; Monticone, M. Effects of exercise on balance in patients with non-specific low back pain: A systematic review and meta-analysis. Eur. J. Phys. Rehabil. Med. 2022, 58, 423–434. [Google Scholar] [CrossRef]
- Suh, J.H.; Kim, H.; Jung, G.P.; Ko, J.Y.; Ryu, J.S. The effect of lumbar stabilization and walking exercises on chronic low back pain: A randomized controlled trial. Medicine 2019, 98, e16173. [Google Scholar] [CrossRef] [PubMed]
- Helmhout, P.H.; Witjes, M.; Nijhuis-VAN DER Sanden, R.W.; Bron, C.; van Aalst, M.; Staal, J.B. The effects of lumbar extensor strength on disability and mobility in patients with persistent low back pain. J. Sports Med. Phys. Fitness 2017, 57, 411–417. [Google Scholar] [CrossRef]
- Shahtahmassebi, B.; Hebert, J.J.; Hecimovich, M.; Fairchild, T.J. Trunk exercise training improves muscle size, strength, and function in older adults: A randomized controlled trial. Scand. J. Med. Sci. Sports 2019, 29, 980–991. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Chen, C.; Du, S.; Tang, Y.; Li, K.; Yu, X.; Tan, J.; Zhang, C.; Rong, Z.; Xu, J.; et al. Assessment of isokinetic trunk muscle strength and its association with health-related quality of life in patients with degenerative spinal deformity. BMC Musculoskelet. Disord. 2020, 21, 827. [Google Scholar] [CrossRef] [PubMed]
- Chesterton, P.; Payton, S.; McLaren, S. Acute effects of centrally- and unilaterally applied posterior-anterior mobilizations of the lumbar spine on lumbar range of motion, hamstring extensibility and muscle activation. J. Back Musculoskelet. Rehabil. 2018, 31, 1013–1023. [Google Scholar] [CrossRef] [PubMed]
- Javadian, Y.; Behtash, H.; Akbari, M.; Taghipour-Darzi, M.; Zekavat, H. The effects of stabilizing exercises on pain and disability of patients with lumbar segmental instability. J. Back Musculoskelet. Rehabil. 2012, 25, 149–155. [Google Scholar] [CrossRef]
- Huang, R.C.; Girardi, F.P.; Cammisa, F.P., Jr.; Lim, M.R.; Tropiano, P.; Marnay, T. Correlation between range of motion and outcome after lumbar total disc replacement: 8.6-year follow-up. Spine 2005, 30, 1407–1411. [Google Scholar] [CrossRef]
- Lee, K. The relationship of trunk muscle activation and core stability: A biomechanical analysis of Pilates-based stabilization exercise. Int. J. Environ. Res. Public Health 2021, 18, 12804. [Google Scholar] [CrossRef]
- Salik Sengul, Y.; Yilmaz, A.; Kirmizi, M.; Kahraman, T.; Kalemci, O. Effects of stabilization exercises on disability, pain, and core stability in patients with non-specific low back pain: A randomized controlled trial. Work 2021, 70, 99–107. [Google Scholar] [CrossRef]
- van Dillen, L.R.; Lanier, V.M.; Steger-May, K.; Wallendorf, M.; Norton, B.J.; Civello, J.M.; Czuppon, S.L.; Francois, S.J.; Roles, K.; Lang, C.E. Effect of motor skill training in functional activities vs strength and flexibility exercise on function in people with chronic low back pain: A randomized clinical trial. JAMA Neurol. 2021, 78, 385–395. [Google Scholar] [CrossRef]
- Hayden, J.A.; Ellis, J.; Ogilvie, R.; Stewart, S.A.; Bagg, M.K.; Stanojevic, S.; Yamato, T.P.; Saragiotto, B.T. Some types of exercise are more effective than others in people with chronic low back pain: A network meta-analysis. J. Physiother. 2021, 67, 252–262. [Google Scholar] [CrossRef] [PubMed]
- Ulger, O.; Oz, M.; Ozel Asliyuce, Y. The effects of yoga and stabilization exercises in patients with chronic low back pain: A randomized crossover study. Holist. Nurs. Pract. 2023, 37, E59–E68. [Google Scholar] [CrossRef]
- Nazir, S.N.B.; Pereira, F.A.; Muhammad, A.; Shamsi, I.I.; Khan, M.U. The relationship between fear-avoidance beliefs, disability, and physical capacity in patients with chronic low back pain. Mediterr. J. Rheumatol. 2022, 33, 305–310. [Google Scholar] [CrossRef]
- Kuo, A.D.; Donelan, J.M. Dynamic principles of gait and their clinical implications. Phys. Ther. 2010, 90, 157–174. [Google Scholar] [CrossRef]
- Alshehri, M.A.; van den Hoorn, W.; Klyne, D.M.; Hodges, P.W. Postural control of the trunk in individuals with and without low back pain during unstable sitting: A protocol for a systematic review with an individual participant data meta-analysis. PLoS ONE 2022, 17, e0268381. [Google Scholar] [CrossRef] [PubMed]
- Kuo, Y.L.; Huang, K.Y.; Chiang, P.T.; Lee, P.Y.; Tsai, Y.J. Steadiness of spinal regions during single-leg standing in older adults with and without chronic low back pain. PLoS ONE 2015, 10, e0128318. [Google Scholar] [CrossRef] [PubMed]
- Tidstrand, J.; Horneij, E. Inter-rater reliability of three standardized functional tests in patients with low back pain. BMC Musculoskelet. Disord. 2009, 10, 58. [Google Scholar] [CrossRef]
- Buraschi, R.; Pollet, J.; Villafañe, J.H.; Piovanelli, B.; Negrini, S. Temporal and kinematic analyses of timed up and go test in chronic low back pain patients. Gait Posture 2022, 96, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Hirano, K.; Imagama, S.; Hasegawa, Y.; Ito, Z.; Muramoto, A.; Ishiguro, N. Impact of low back pain, knee pain, and timed up-and-go test on quality of life in community-living people. J. Orthop. Sci. 2014, 19, 164–171. [Google Scholar] [CrossRef]
| Variable | Value |
|---|---|
| Mean age, years | 67.22 ± 11.55 |
| Male:Female | 129:282 |
| Interval from surgery, days | 21.48 ± 15.23 |
| Height, cm | 160.50 ± 8.76 |
| Weight, kg | 64.09 ± 18.06 |
| Body mass index, kg/m2 | 24.56 ± 5.44 |
| Skeletal muscle mass, kg | 23.88 ± 15.15 |
| Total body fat mass, kg | 20.15 ± 7.25 |
| Total body fat percentage, % | 30.53 ± 9.68 |
| Alcohol, yes (%) | 117 (28.5%) |
| Smoking, yes (%) | 70 (17.0%) |
| Baseline status of exercise, none:irregular:regular (%) | 151 (36.7%):157 (38.2%):103 (25.1%) |
| Variable | Value |
|---|---|
| Range of motion of the lumbar spine, ° | 74.24 ± 25.30 |
| Trunk muscle strength, kg | |
| Flexion | 14.04 ± 4.89 |
| Extension | 17.38 ± 5.92 |
| Mean | 15.71 ± 5.14 |
| Trunk muscle endurance, seconds | 42.95 ± 30.26 |
| Flexion | 94.86 ± 37.80 |
| Extension | 96.75 ± 36.00 |
| Mean | 95.80 ± 35.66 |
| Flexibility of the whole body, cm | 3.30 ± 10.65 |
| Cardiopulmonary capability, m | 433.91 ± 118.75 |
| Gait pattern, % | |
| Affected side | 36.26 ± 5.98 |
| Healthy side | 39.53 ± 5.15 |
| Mean | 37.90 ± 5.57 |
| Single-leg balance, seconds | |
| Affected side | 13.60 (IQR, 3.02–32.00) |
| Healthy side | 8.58 (IQR, 4.00–41.81) |
| Mean | 10.42 (IQR, 3.74–37.31) |
| Coordination capability, seconds | 8.21 ± 3.23 |
| Quality of life (EQ-5D-5L) | 9.39 ± 4.17 |
| Degree of pain (VAS) | 3.78 ± 2.55 |
| Variable | 1st Grade (Very Poor) | 2nd Grade (Poor) | 3rd Grade (Average) | 4th Grade (Good) | 5th Grade (Very Good) | |
|---|---|---|---|---|---|---|
| Range of motion of the lumbar spine, ° | ||||||
| Male | ≤48.5 | 48.6–58.6 | 58.7–92.2 | 92.3–115.4 | ≥115.5 | |
| Female | ≤40.9 | 40.8–53.9 | 54.0–89.2 | 89.3–111.9 | ≥112.0 | |
| Trunk muscle strength, kg | ||||||
| Male | ≤13.1 | 13.2–16.1 | 16.2–22.2 | 22.3–24.7 | ≥24.8 | |
| Female | ≤8.2 | 8.3–10.6 | 10.7–12.2 | 12.3–17.3 | ≥17.4 | |
| Trunk muscle endurance, seconds | ||||||
| Male | ≤25.2 | 25.3–31.6 | 31.7–76.0 | 76.1–119.9 | ≥120.0 | |
| Female | ≤19.9 | 20.0–25.8 | 25.9–74.1 | 74.2–119.9 | ≥120.0 | |
| Flexibility of the whole body, cm | ||||||
| Male | ≤−13.0 | −12.9–−8.0 | −8.1–4.6 | 4.7–10.3 | ≥10.4 | |
| Female | ≤−11.7 | −11.6–−0.8 | −0.9–13.2 | 13.3–19.2 | ≥19.3 | |
| Cardiorespiratory capability, m | ||||||
| Male | ≤356.2 | 376.3–411.2 | 411.3–539.9 | 540.0–601.9 | ≥602 | |
| Female | ≤272.7 | 272.8–359.9 | 360.0–493.1 | 493.2–553.2 | ≥553.3 | |
| Gait pattern, % | ||||||
| Male | ≤32.0 | 32.1–36.8 | 36.9–40.5 | 40.6–42.2 | ≥42.3 | |
| Female | ≤31.9 | 42.0–36.4 | 36.5–40.1 | 40.2–47.2 | ≥47.3 | |
| Single-leg balance, seconds | ||||||
| Male | ≤2.1 | 2.2–3.9 | 4.0–42.6 | 42.7–67.2 | ≥67.3 | |
| Female | ≤1.9 | 2.0–3.7 | 3.8–36.7 | 36.8–84.0 | ≥84.1 | |
| Coordination capability, seconds | ||||||
| Male | ≤5.4 | 5.5–6.0 | 6.1–8.0 | 8.1–9.0 | ≥9.1 | |
| Female | ≤5.0 | 5.1–6.9 | 7.0–11.9 | 12.0–13.9 | ≥14.0 | |
| Quality of life (EQ-5D-5L) | ≥16 | 12–15 | 6–11 | 4–5 | ≤3 | |
| Degree of pain (VAS) | ≥8 | 6–7 | 3–5 | 1–2 | 0 |
| Variable | Range of Motion of the Lumbar Spine | Trunk Muscle Strength | Trunk Muscle Endurance | Flexibility of the Whole Body | Cardiorespiratory Capability | Gait Pattern | Single-Leg Balance | Coordination Capability | Quality of Life (EQ-5D-5L) | Degree of Pain (VAS) |
|---|---|---|---|---|---|---|---|---|---|---|
| Range of motion of the lumbar spine | 0.264 | 0.070 | 0.246 | 0.089 | 0.231 | −0.333 | 0.202 | −0.202 | −0.142 | |
| <0.001 | 0.159 | <0.001 | <0.001 | 0.086 | <0.001 | <0.001 | <0.001 | 0.004 | ||
| Trunk muscle strength | 0.289 | −0.025 | 0.453 | 0.138 | 0.335 | −0.403 | −0.200 | −0.400 | ||
| <0.001 | 0.629 | <0.001 | 0.008 | <0.001 | <0.001 | <0.001 | <0.001 | |||
| Trunk muscle endurance | 0.132 | 0.238 | 0.015 | 0.222 | −0.305 | −0.172 | −0.247 | |||
| 0.010 | <0.001 | 0.772 | <0.001 | <0.001 | <0.001 | <0.001 | ||||
| Flexibility of the whole body | 0.106 | 0.017 | −0.077 | −0.106 | −0.107 | −0.006 | ||||
| 0.037 | 0.746 | 0.133 | 0.037 | 0.036 | 0.903 | |||||
| Cardiorespiratory capability | 0.245 | 0.514 | −0.728 | −0.289 | −0.244 | |||||
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
| Gait pattern | 0.152 | −0.264 | −0.034 | −0.104 | ||||||
| 0.004 | <0.001 | 0.477 | 0.047 | |||||||
| Single-leg balance | −0.431 | −0.188 | −0.216 | |||||||
| <0.001 | <0.001 | <0.001 | ||||||||
| Coordination capability | 0.279 | 0.181 | ||||||||
| <0.001 | <0.001 | |||||||||
| Quality of life (EQ-5D-5L) | 0.430 | |||||||||
| <0.001 | ||||||||||
| Degree of pain (VAS) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Son, S.; Park, H.B.; Yoo, C.J.; Kim, M.-H.; Yoo, B.R.; Sim, J.A. Development of an Exercise Rehabilitation Functional Group for Individualized Exercise After Lumbar Spine Surgery. Life 2025, 15, 943. https://doi.org/10.3390/life15060943
Son S, Park HB, Yoo CJ, Kim M-H, Yoo BR, Sim JA. Development of an Exercise Rehabilitation Functional Group for Individualized Exercise After Lumbar Spine Surgery. Life. 2025; 15(6):943. https://doi.org/10.3390/life15060943
Chicago/Turabian StyleSon, Seong, Han Byeol Park, Chan Jong Yoo, Moon-Hee Kim, Byung Rhae Yoo, and Jae Ang Sim. 2025. "Development of an Exercise Rehabilitation Functional Group for Individualized Exercise After Lumbar Spine Surgery" Life 15, no. 6: 943. https://doi.org/10.3390/life15060943
APA StyleSon, S., Park, H. B., Yoo, C. J., Kim, M.-H., Yoo, B. R., & Sim, J. A. (2025). Development of an Exercise Rehabilitation Functional Group for Individualized Exercise After Lumbar Spine Surgery. Life, 15(6), 943. https://doi.org/10.3390/life15060943






