Surgical Repair of Bile Duct Injuries Due to Cholecystectomy—An Experience from a Referral Center in Slovenia
Abstract
1. Introduction
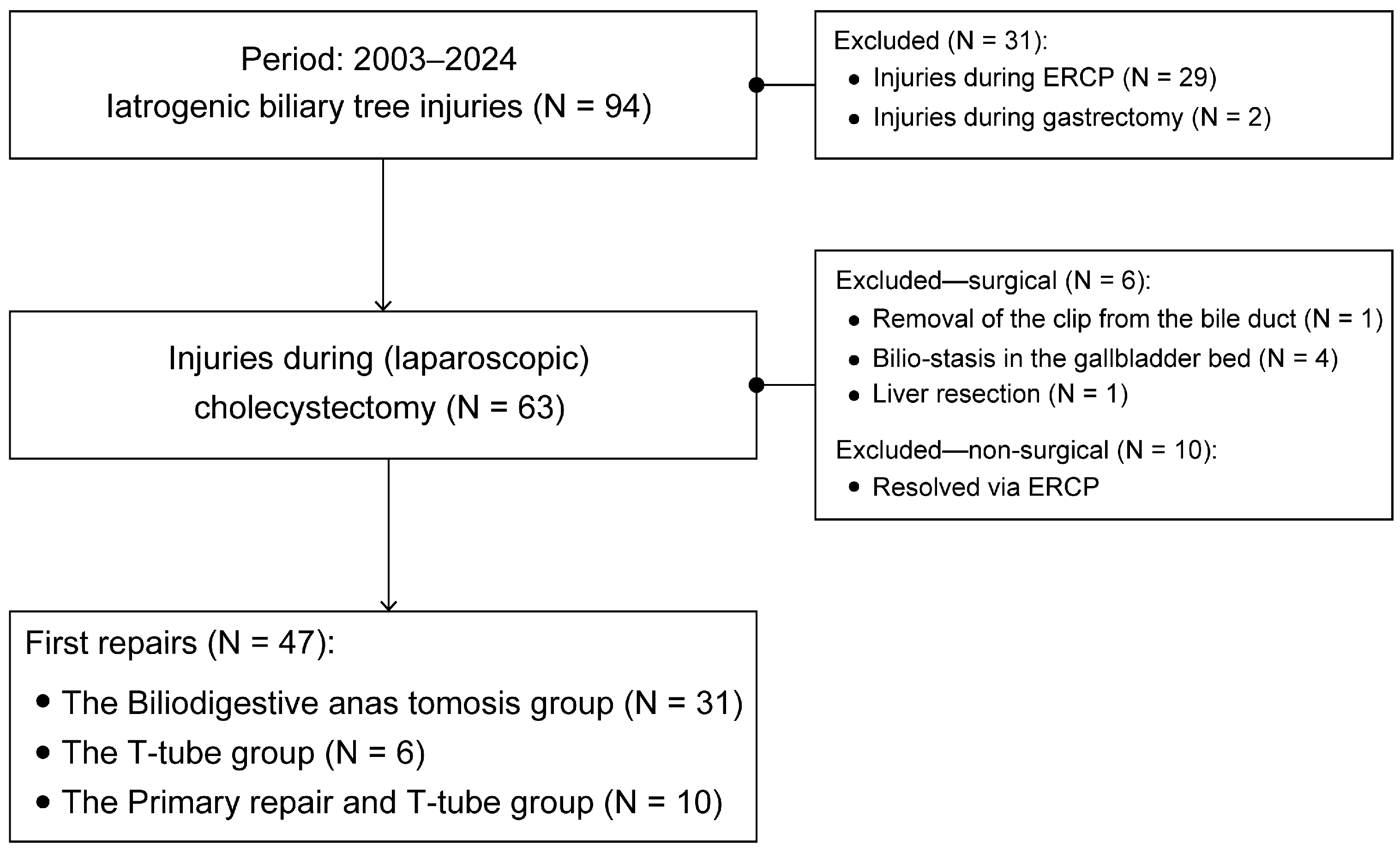
2. Materials and Methods
- T-tube placement.
- Primary sutures of the bile ducts with a T-tube placement.
- BDA was performed in a Roux-en-Y manner for complete transections of the bile ducts. The surgical technique was applied as described by the reference [23].
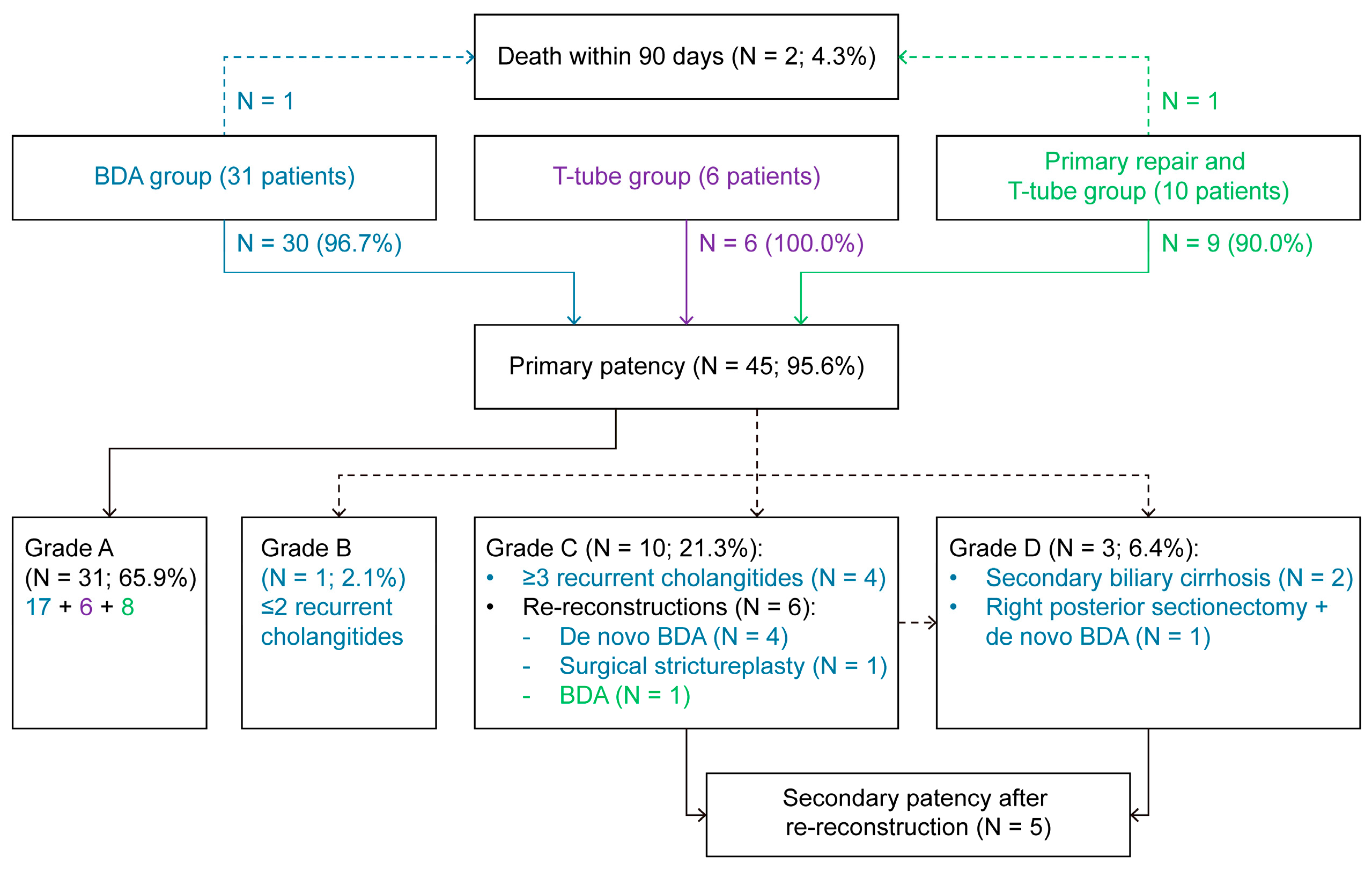
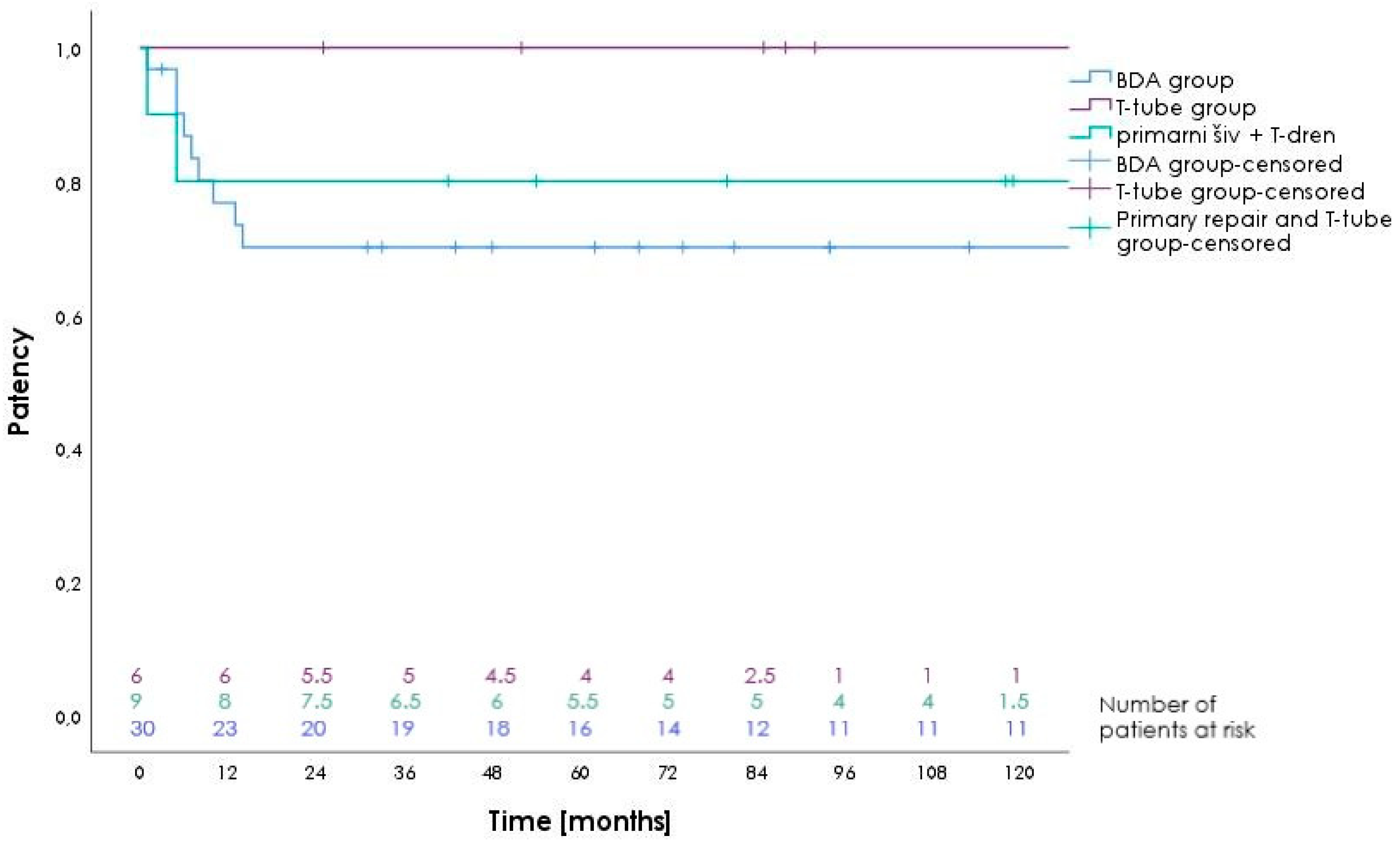
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sparkman, R.S. 100th Anniversary of the First Cholecystectomy: A Reprinting of the 50th Anniversary Article From the Archives of Surgery, July 1932. Arch. Surg. 1982, 117, 1525. [Google Scholar] [CrossRef] [PubMed]
- Blum, C.A.; Adams, D.B. Who did the first laparoscopic cholecystectomy? J. Minim. Access Surg. 2011, 7, 165–168. [Google Scholar] [CrossRef] [PubMed]
- de’Angelis, N.; Catena, F.; Memeo, R.; Coccolini, F.; Martínez-Pérez, A.; Romeo, O.M.; De Simone, B.; Di Saverio, S.; Brustia, R.; Rhaiem, R.; et al. 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J. Emerg. Surg. 2021, 16, 30. [Google Scholar] [CrossRef] [PubMed]
- Way, L.W.; Stewart, L.; Gantert, W.; Liu, K.; Lee, C.M.; Whang, K.; Hunter, J.G. Causes and prevention of laparoscopic bile duct injuries: Analysis of 252 cases from a human factors and cognitive psychology perspective. Ann. Surg. 2003, 237, 460–469. [Google Scholar] [CrossRef]
- Pekolj, J. Introduction. In Fundamentals of Bile Duct Injuries: From Prevention to Multidisciplinary Management; Pekolj, J., Ardiles, V., Glinka, J., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 1–5. [Google Scholar]
- Manatakis, D.K.; Antonopoulou, M.I.; Tasis, N.; Agalianos, C.; Tsouknidas, I.; Korkolis, D.P.; Dervenis, C. Critical View of Safety in Laparoscopic Cholecystectomy: A Systematic Review of Current Evidence and Future Perspectives. World J. Surg. 2023, 47, 640–648. [Google Scholar] [CrossRef]
- Strasberg, S.M. A perspective on the critical view of safety in laparoscopic cholecystectomy. Ann. Laparosc. Endosc. Surg. 2017, 2, 91. [Google Scholar] [CrossRef]
- Daly, S.C.; Deziel, D.J.; Li, X.; Thaqi, M.; Millikan, K.W.; Myers, J.A.; Bonomo, S.; Luu, M.B. Current practices in biliary surgery: Do we practice what we teach? Surg. Endosc. 2016, 30, 3345–3350. [Google Scholar] [CrossRef]
- Dahmane, R.; Morjane, A.; Starc, A. Anatomy and surgical relevance of Rouviere’s sulcus. Sci. World J. 2013, 2013, 254287. [Google Scholar] [CrossRef]
- Lockhart, S.; Singh-Ranger, G. Rouviere’s sulcus-Aspects of incorporating this valuable sign for laparoscopic cholecystectomy. Asian J. Surg. 2018, 41, 1–3. [Google Scholar] [CrossRef]
- Basukala, S.; Thapa, N.; Tamang, A.; Shah, K.B.; Rayamajhi, B.B.; Ayer, D.; Karki, S.; Basukala, B.; Sharma, S.; Dhakal, S. Rouviere’s sulcus—An anatomical landmark for safe laparoscopic cholecystectomy: A cross-sectional study. Ann. Med. Surg. 2022, 75, 103404. [Google Scholar] [CrossRef]
- Brunt, L.M.; Deziel, D.J.; Telem, D.A.; Strasberg, S.M.; Aggarwal, R.; Asbun, H.; Bonjer, J.; McDonald, M.; Alseidi, A.; Ujiki, M.; et al. Safe Cholecystectomy Multi-society Practice Guideline and State of the Art Consensus Conference on Prevention of Bile Duct Injury During Cholecystectomy. Ann. Surg. 2020, 272, 3–23. [Google Scholar] [CrossRef] [PubMed]
- Marichez, A.; Adam, J.P.; Laurent, C.; Chiche, L. Hepaticojejunostomy for bile duct injury: State of the art. Langenbecks Arch. Surg. 2023, 408, 107. [Google Scholar] [CrossRef] [PubMed]
- Bonds, M.; Rocha, F. Cholecystectomy techniques and postoperative problems. In Blumgart’s Surgery of the Liver, Biliary Tract, and Pancreas, 7th ed.; Jarnagin, W.R., Allen, P.J., Chapman, W.C., D’Angelica, M.I., DeMatteo, R.P., Do, R.K.G., Vauthey, J.-N., Blumgart, L.H., Eds.; Elsevier: Philadelphia, PA, USA, 2023; pp. 494–504. [Google Scholar]
- Post cholecystectomy bile duct injury: Early, intermediate or late repair with hepaticojejunostomy—An E-AHPBA multi-center study. HPB 2019, 21, 1641–1647. [CrossRef]
- Atay, A.; Gungor, F.; Sur, Y.; Gunes, O.; Dilek, F.H.; Karasu, Ş.; Dilek, O.N. Management of hepatic artery trauma during hepato-pancreato-biliary procedures: Evolving approaches, clinical outcomes, and literature review. Ulus. Travma Acil Cerrahi Derg. 2022, 28, 1549–1557. [Google Scholar] [CrossRef]
- Perera, M.T.; Silva, M.A.; Hegab, B.; Muralidharan, V.; Bramhall, S.R.; Mayer, A.D.; Buckels, J.A.; Mirza, D.F. Specialist early and immediate repair of post-laparoscopic cholecystectomy bile duct injuries is associated with an improved long-term outcome. Ann. Surg. 2011, 253, 553–560. [Google Scholar] [CrossRef]
- de Reuver, P.R.; Grossmann, I.; Busch, O.R.; Obertop, H.; van Gulik, T.M.; Gouma, D.J. Referral pattern and timing of repair are risk factors for complications after reconstructive surgery for bile duct injury. Ann. Surg. 2007, 245, 763–770. [Google Scholar] [CrossRef]
- Stilling, N.M.; Fristrup, C.; Wettergren, A.; Ugianskis, A.; Nygaard, J.; Holte, K.; Bardram, L.; Sall, M.; Mortensen, M.B. Long-term outcome after early repair of iatrogenic bile duct injury. A national Danish multicentre study. HPB 2015, 17, 394–400. [Google Scholar] [CrossRef]
- Plahuta, I.; Šarenac, Ž.; Golob, M.; Turk, Š.; Ilijevec, B.; Magdalenić, T.; Potrč, S.; Ivanecz, A. Laparoscopic and Open Distal Pancreatectomy-An Initial Single-Institution Experience with a Propensity Score Matching Analysis. Life 2025, 15, 97. [Google Scholar] [CrossRef]
- Ivanecz, A.; Plahuta, I.; Mencinger, M.; Perus, I.; Magdalenic, T.; Turk, S.; Potrc, S. The learning curve of laparoscopic liver resection utilising a difficulty score. Radiol. Oncol. 2021, 56, 111–118. [Google Scholar] [CrossRef]
- Cho, J.Y.; Baron, T.H.; Carr-Locke, D.L.; Chapman, W.C.; Costamagna, G.; de Santibanes, E.; Dominguez Rosado, I.; Garden, O.J.; Gouma, D.; Lillemoe, K.D.; et al. Proposed standards for reporting outcomes of treating biliary injuries. HPB 2018, 20, 370–378. [Google Scholar] [CrossRef]
- Bredbeck, B.C.; Cho, C.S. Bile duct exploration and biliary-enteric anastomosis. In Blumgart’s Surgery of the Liver, Biliary Tract, and Pancreas, 7th ed.; Jarnagin, W.R., Allen, P.J., Chapman, W.C., D’Angelica, M.I., DeMatteo, R.P., Do, R.K.G., Vauthey, J.-N., Blumgart, L.H., Eds.; Elsevier: Philadelphia, PA, USA, 2023; pp. 459–470. [Google Scholar]
- Strasberg, S.M.; Hertl, M.; Soper, N.J. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J. Am. Coll. Surg. 1995, 180, 101–125. [Google Scholar] [PubMed]
- Miura, F.; Okamoto, K.; Takada, T.; Strasberg, S.M.; Asbun, H.J.; Pitt, H.A.; Gomi, H.; Solomkin, J.S.; Schlossberg, D.; Han, H.S.; et al. Tokyo Guidelines 2018: Initial management of acute biliary infection and flowchart for acute cholangitis. J. Hepatobiliary Pancreat. Sci. 2018, 25, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibanes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef]
- Otto, W.; Sierdziński, J.; Smaga, J.; Kornasiewicz, O.; Dudek, K.; Zieniewicz, K. Actuarial Patency Rates of Hepatico-Jejunal Anastomosis after Repair of Bile Duct Injury at a Reference Center. J. Clin. Med. 2022, 11, 3396. [Google Scholar] [CrossRef]
- Habibzadeh, F. Statistical Data Editing in Scientific Articles. J. Korean Med. Sci. 2017, 32, 1072–1076. [Google Scholar] [CrossRef]
- Bewick, V.; Cheek, L.; Ball, J. Statistics review 12: Survival analysis. Crit. Care 2004, 8, 389. [Google Scholar] [CrossRef]
- Molinari, M. Traumatic Bile Duct Injuries. In Actual Problems of Emergency Abdominal Surgery; Garbuzenko, D.V., Ed.; IntechOpen: Rijeka, Croatia, 2016. [Google Scholar]
- Breznik, S.; Slanič, A.; Ivanecz, A.; Lučev, J. Bilhemia After Percutaneous Liver Tumor Core Biopsy With the Percutaneous Embolization of Bilio-venous Fistula With Coils and Onyx. Cureus 2024, 16, e61414. [Google Scholar] [CrossRef] [PubMed]
- Bektas, H.; Schrem, H.; Winny, M.; Klempnauer, J. Surgical treatment and outcome of iatrogenic bile duct lesions after cholecystectomy and the impact of different clinical classification systems. Br. J. Surg. 2007, 94, 1119–1127. [Google Scholar] [CrossRef]
- Šileikis, A.; Žulpaitė, R.; Šileikytė, A.; Lukšta, M. Postcholecystectomy bile duct injuries: Evolution of surgical treatment. Pol. Prz. Chir. 2019, 91, 14–21. [Google Scholar] [CrossRef]
- Kapoor, V.K. (Ed.) Post-Cholecystectomy Bile Duct Injury; Springer: Singapore, 2020; p. 264. [Google Scholar]
- Törnqvist, B.; Strömberg, C.; Akre, O.; Enochsson, L.; Nilsson, M. Selective intraoperative cholangiography and risk of bile duct injury during cholecystectomy. Br. J. Surg. 2015, 102, 952–958. [Google Scholar] [CrossRef]
- Goldstein, S.D.; Lautz, T.B. Fluorescent Cholangiography During Laparoscopic Cholecystectomy: Shedding New Light on Biliary Anatomy. JAMA Surg. 2020, 155, 978–979. [Google Scholar] [CrossRef] [PubMed]
- Durowicz, S.; Kozicki, I.; Ciesielski, A.; Tarnowski, W. Excision of a part of the bile duct as an iatrogenic injury typical for laparoscopic cholecystectomy—Characteristics, treatment and long-term results, based on own material. Wideochir. Inne Tech. Maloinwazyjne 2020, 15, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Barbier, L.; Souche, R.; Slim, K.; Ah-Soune, P. Long-term consequences of bile duct injury after cholecystectomy. J. Visc. Surg. 2014, 151, 269–279. [Google Scholar] [CrossRef] [PubMed]
- Törnqvist, B.; Strömberg, C.; Persson, G.; Nilsson, M. Effect of intended intraoperative cholangiography and early detection of bile duct injury on survival after cholecystectomy: Population based cohort study. BMJ 2012, 345, e6457. [Google Scholar] [CrossRef]
- Fingerhut, A.; Dziri, C.; Garden, O.J.; Gouma, D.; Millat, B.; Neugebauer, E.; Paganini, A.; Targarona, E. ATOM, the all-inclusive, nominal EAES classification of bile duct injuries during cholecystectomy. Surg. Endosc. 2013, 27, 4608–4619. [Google Scholar] [CrossRef]
- Martínez-Mier, G.; Moreno-Ley, P.I.; Mendez-Rico, D. Factors associated with patency loss and actuarial patency rate following post-cholecystectomy bile duct injury repair: Long-term follow-up. Langenbecks Arch. Surg. 2020, 405, 999–1006. [Google Scholar] [CrossRef]
- Lindemann, J.; Krige, J.E.J.; Kotze, U.; Jonas, E. Factors leading to loss of patency after biliary reconstruction of major laparoscopic cholecystectomy bile duct injuries: An observational study with long-term outcomes. HPB 2020, 22, 1613–1621. [Google Scholar] [CrossRef]
| Variable | Total (N = 47) | BDA Group (N = 31) | T-Tube Group (N = 6) | Primary Repair and T-Tube Group (N = 10) |
|---|---|---|---|---|
| Male sex | 23 (48.9) | 17 (54.8) | 3 (50.0) | 3 (30.0) |
| Age [years] | 65 (18) | 60 (20) | 69 (16) | 68 (13) |
| BMI [kg/m2] | 29 (7) | 29 (5) | 36 (3) | 28 (2) |
| ASA 3 and 4 | 14 (29.8) | 10 (32.3) | 2 (33.3) | 2 (20.0) |
| Method | ||||
| open | 7 (15.0) | 4 (12.9) | 1 (16.7) | 2 (20.0) |
| laparoscopic | 20 (42.5) | 13 (41.9) | 3 (50.0) | 4 (40.0) |
| conversion | 20 (42.5) | 14 (45.2) | 2 (33.3) | 4 (40.0) |
| Elective surgery | 30 (63.8) | 19 (61.3) | 4 (66.7) | 7 (70.0) |
| Clinical Presentation | Total (N = 47) | BDA Group (N = 31) | T-Tube Group (N = 6) | Primary Repair and T-Tube Group (N = 10) |
|---|---|---|---|---|
| During index surgery | 16 (34.0) | 9 (29.0) | 2 (33.3) | 5 (50.0) |
| Icterus/holangitis | 12 (25.5) | 12 (38.7) | 0 (0.0) | 0 (0.0) |
| Bile in drain | 11 (23.4) | 7 (22.6) | 3 (50.0) | 1 (10.0) |
| Biliary peritonitis | 7 (14.9) | 2 (6.5) | 1 (16.7) | 4 (40.0) |
| Hemorrhagic shock | 1 (2.1) | 1 (3.2) | 0 (0.0) | 0 (0.0) |
| Time of the repair | ||||
| During index surgery | 16 (34.0) | 9 (29.0) | 2 (33.3) | 5 (50.0) |
| Early (day 1–7) | 15 (31.9) | 10 (61.3) | 4 (66.7) | 1 (10.0) |
| Intermediate (1–6 weeks) | 10 (21.3) | 6 (19.4) | 4 (40.0) | |
| Late (>6 weeks) | 6 (12.7) | 6 (19.4) | ||
| Grade of Injury | Total (N = 47) | BDA Group (N = 31) | T-Tube Group (N = 6) | Primary Repair and T-Tube Group (N = 10) |
|---|---|---|---|---|
| B | 2 (4.3) | 2 (6.5) | ||
| C | 5 (10.6) | 5 (50.0) | ||
| D | 11 (23.4) | 6 (100.0) | 5 (50.0) | |
| E1 | 4 (8.5) | 4 (12.9) | ||
| E2 | 12 (25.5) | 12 (38.7) | ||
| E3 | 5 (10.6) | 5 (16.1) | ||
| E4 | 3 (6.4) | 3 (9.7) | ||
| E5 | 5 (10.6) | 5 (16.1) |
| Grade of Injury | Total (N = 47) | BDA Group (N = 31) | T-Tube Group (N = 6) | Primary Repair and T-Tube Group (N = 10) |
|---|---|---|---|---|
| CD 1 | 2 (4.3) | 2 (6.5) | ||
| CD 2 | 7 (14.9) | 5 (16.1) | 2 (20.0) | |
| CD 3a | 2 (4.3) | 1 (3.2) | 1 (16.7) | |
| CD 3b | 2 (4.3) | 2 (6.5) | ||
| CD 4a | 1 (2.1) | 1 (3.2) | ||
| CD 4b | 3 (6.4) | 2 (6.5) | 1 (10.0) | |
| CD 5 | 2 (4.3) | 1 (3.2) | 1 (10.0) | |
| Overall morbidity | 19 (40.4) | 14 (45.2) | 1 (16.7) | 4 (40.0) |
| Severe morbidity ≥ CD 3a | 10 (21.3) | 7 (22.6) | 1 (16.7) | 2 (20.0) |
| Time Frame | Total (N = 47) | BDA Group (N = 31) | T-Tube Group (N = 6) | Primary Repair and T-Tube Group (N = 10) |
|---|---|---|---|---|
| During index surgery | 1 (6.25%) | 11.1% 3b | ||
| Early (day 1–7) | 5 (33.3%) | 30.0% 3b, 2 pts 4b | 25.0% 3a | 20.0% 5 |
| Intermediate (1–6 weeks) | 3 (30.0%) | 50.0% 3a, 4a, 5 | 25.0% 4b | |
| Late (>6 weeks) |
| BDA Group (N = 31) | T-Tube Group (N = 6) | Primary Repair and T-Tube Group (N = 10) | |
|---|---|---|---|
| 1 year | 77.0% | 100.0% | 80.0% |
| 3 years | 70.0% | 100.0% | 80.0% |
| 5 years | 70.0% | 100.0% | 80.0% |
| 10 years | 70.0% | 100.0% | 80.0% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Plahuta, I.; Turk, Š.; Lovrenčič Petreski, B.; Magdalenić, T.; Potrč, S.; Ivanecz, A. Surgical Repair of Bile Duct Injuries Due to Cholecystectomy—An Experience from a Referral Center in Slovenia. Life 2025, 15, 874. https://doi.org/10.3390/life15060874
Plahuta I, Turk Š, Lovrenčič Petreski B, Magdalenić T, Potrč S, Ivanecz A. Surgical Repair of Bile Duct Injuries Due to Cholecystectomy—An Experience from a Referral Center in Slovenia. Life. 2025; 15(6):874. https://doi.org/10.3390/life15060874
Chicago/Turabian StylePlahuta, Irena, Špela Turk, Barbara Lovrenčič Petreski, Tomislav Magdalenić, Stojan Potrč, and Arpad Ivanecz. 2025. "Surgical Repair of Bile Duct Injuries Due to Cholecystectomy—An Experience from a Referral Center in Slovenia" Life 15, no. 6: 874. https://doi.org/10.3390/life15060874
APA StylePlahuta, I., Turk, Š., Lovrenčič Petreski, B., Magdalenić, T., Potrč, S., & Ivanecz, A. (2025). Surgical Repair of Bile Duct Injuries Due to Cholecystectomy—An Experience from a Referral Center in Slovenia. Life, 15(6), 874. https://doi.org/10.3390/life15060874








