Disparities in Colorectal Cancer Mortality and Survival Trends Among Hispanics Living in Puerto Rico (2000–2021): A Comparison Between Early-Onset and Average-Onset Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Study Population
2.2. Study Variables
2.3. Case Ascertainment
2.4. Statistical Analysis
3. Results
3.1. CRC Mortality by Racial and Ethnic Group
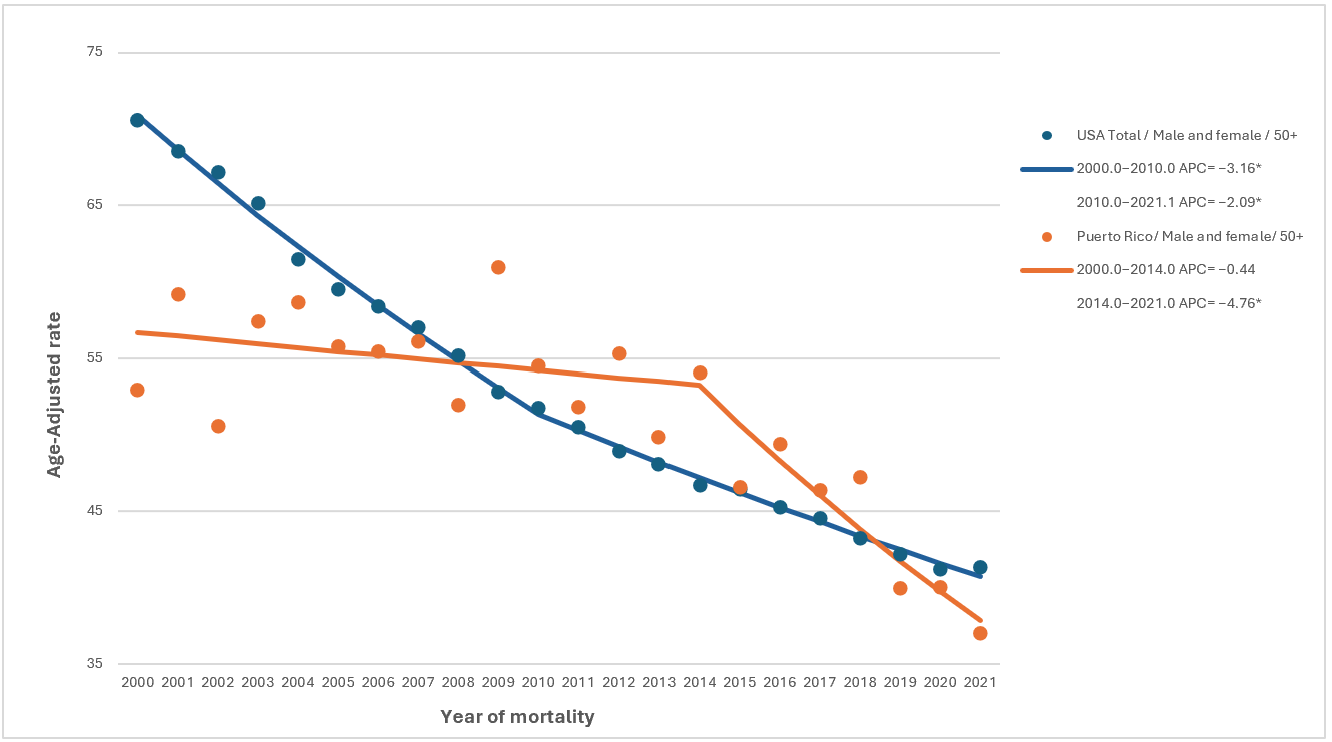
3.2. Age-Adjusted Average Annual Percent Changes (AAPC) by Racial and Ethnic Group
3.3. Disparities in Relative Survival by Age and Stage at Diagnosis
3.4. Relative Survival Analysis by Sex
4. Discussion
4.1. Overall and Average-Onset CRC Trends
4.2. Early-Onset CRC Trends
4.3. Key Contributor to CRC Disparities in PRH
4.4. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CRC | Colorectal Cancer |
| EOCRC | Early-Onset Colorectal Cancer |
| U.S. | United States |
| PR | Puerto Rico |
| USH | Hispanics living in the United States |
| PRH | Hispanics residing in Puerto Rico |
| NHW | Non-Hispanic Whites |
| NHB | Non-Hispanic Blacks |
| NHAPI | Non-Hispanic Asian or Pacific Islanders |
| NHAI/AN | U.S. Non-Hispanic American Indians/Alaska Natives |
| SEER | Puerto Rico Central Cancer Registry and the Surveillance, Epidemiology, and End Results |
| PRCCR | Puerto Rico Central Cancer Registry |
| AAPC | Average Annual Percent Change |
| NCI | National Cancer Institute |
| NAACCR | North American Association of Central Cancer Registries |
| CI | Confidence Intervals |
References
- Siegel, R.L.; Wagle, N.S.; Cercek, A.; Smith, R.A.; Jemal, A. Colorectal cancer statistics, 2023. CA Cancer J. Clin. 2023, 73, 233–254. [Google Scholar] [CrossRef] [PubMed]
- Austin, H.; Henley, S.J.; King, J.; Richardson, L.C.; Eheman, C. Changes in colorectal cancer incidence rates in young and older adults in the United States: What does it tell us about screening. Cancer Causes Control 2014, 25, 191–201. [Google Scholar] [CrossRef]
- Siegel, R.L.; Fedewa, S.A.; Anderson, W.F.; Miller, K.D.; Ma, J.; Rosenberg, P.S.; Jemal, A. Colorectal Cancer Incidence Patterns in the United States, 1974–2013. J. Natl. Cancer Inst. 2017, 109, djw322. [Google Scholar] [CrossRef]
- Wu, C.W.K.; Lui, R.N. Early-onset colorectal cancer: Current insights and future directions. World J. Gastrointest. Oncol. 2022, 14, 230–241. [Google Scholar] [CrossRef]
- Roshandel, G.; Ghasemi-Kebria, F.; Malekzadeh, R. Colorectal Cancer: Epidemiology, Risk Factors, and Prevention. Cancers 2024, 16, 1530. [Google Scholar] [CrossRef]
- Done, J.Z.; Fang, S.H. Young-onset colorectal cancer: A review. World J. Gastrointest. Oncol. 2021, 13, 866. [Google Scholar] [CrossRef]
- Siegel, R.L.; Jakubowski, C.D.; Fedewa, S.A.; Davis, A.; Azad, N.S. Colorectal Cancer in the Young: Epidemiology, Prevention, Management. Am. Soc. Clin. Oncol. Educ. Book 2020, 40, e75–e88. [Google Scholar] [CrossRef]
- Gausman, V.; Bornblase, D.; Anand, S.; Hayes, R.B.; O’Connell, K.; Du, M.; Liang, P.S. Risk Factors Associated with Early-Onset Colorectal Cancer. Clin. Gastroenterol. Hepatol. 2020, 18, 2759. [Google Scholar] [CrossRef]
- Low, E.E.; Demb, J.; Liu, L.; Earles, A.; Bustamante, R.; Willimas, C.D.; Provenzale, D.; Kaltenbach, T.; Gawron, A.J.; Martinez, M.E.; et al. Risk Factors for Early-Onset Colorectal Cancer. Gastroenterology 2020, 159, 501. [Google Scholar] [CrossRef] [PubMed]
- Colorectal Cancer Risk Factors. Available online: https://www.cdc.gov/colorectal-cancer/risk-factors/index.html (accessed on 13 October 2025).
- Colorectal Cancer Risk Factors. Available online: https://www.cancer.org/cancer/types/colon-rectal-cancer/causes-risks-prevention/risk-factors.html (accessed on 9 October 2024).
- Wei, L.; Zhang, H. Do sleep quality and psychological factors link precancerous conditions of colorectal cancer? A retrospective case-control study. Expert Rev. Gastroenterol. Hepatol. 2022, 16, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Bai, X.; Wei, H.; Liu, W.; Coker, O.O.; Gou, H.; Liu, C.; Zhao, L.; Li, C.; Zhou, Y.; Wang, G.; et al. Cigarette smoke promotes colorectal cancer through modulation of gut microbiota and related metabolites. Gut 2022, 71, 2439–2450. [Google Scholar] [CrossRef]
- Ye, P.; Xi, Y.; Huang, Z.; Xu, P. Linking Obesity with Colorectal Cancer: Epidemiology and Mechanistic Insights. Cancers 2020, 12, 1408. [Google Scholar] [CrossRef]
- Veettil, S.K.; Wong, T.Y.; Loo, Y.S.; Playdon, M.C.; Lai, N.M.; Giovannuci, E.L.; Chaiyakunapruk, N. Role of Diet in Colorectal Cancer Incidence: Umbrella Review of Meta-analyses of Prospective Observational Studies. JAMA 2021, 4, e2037341. [Google Scholar] [CrossRef]
- Aykan, N.F. Red Meat and Colorectal Cancer. Oncol. Rev. 2015, 9, 38–44. [Google Scholar] [CrossRef]
- Sivasubramanian, B.P.; Dave, M.; Panchal, V.; Bonsu, J.; Konka, S.; Noei, F.; Nagaraj, S.; Terpari, U.; Savani, P.; Vekaria, P.H.; et al. Comprehensive Review of Red Meat Consumption and the Risk of Cancer. Cereus 2024, 15, e45324. [Google Scholar] [CrossRef] [PubMed]
- Quick Profiles: Puerto Rico. Available online: https://statecancerprofiles.cancer.gov/quick-profiles/index.php?tabSelected=2&statename=puertorico#t=1 (accessed on 9 October 2024).
- Colorectal Cancer Basics. Available online: https://www.cdc.gov/colorectal-cancer/about/?CDC_AAref_Val=https://www.cdc.gov/cancer/colorectal/basic_info/what-is-colorectal-cancer.htm (accessed on 2 October 2024).
- Jiang, Y.; Yuan, H.; Li, Z.; Ji, X.; Shen, Q.; Tuo, J.; Bi, J.; Li, H.; Xiang, Y. Global pattern and trends of colorectal cancer survival: A systematic review of population-based registration data. Cancer Biol. Med. 2022, 19, 186. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Liu, Z.; Li, J.; Tian, S.; Dong, W. Personalizing prognostic prediction in early-onset colorectal cancer. J. Cancer 2020, 11, 6727–6736. [Google Scholar] [CrossRef] [PubMed]
- Cancer in Puerto Rico. Available online: https://rcpr.org/Portals/0/informe%202016-2020%20-%20Ingles%20(2023Dic14).pdf?ver=_7X6jqmJww1gmgdXUg13JA%3D%3D (accessed on 23 October 2024).
- Gonzalez-Pons, M.; Torres, M.; Perez, J.; Velez, A.; Betancourt, J.P.; Marcano, L.; Soto-Salgado, M.; Cruz-Correa, M. Colorectal Cancer Survival Disparities among Puerto Rican Hispanics: A Comparison to Racial/Ethnic Groups in the United States. Cancer Clin. Oncol. 2016, 5, 29. [Google Scholar] [CrossRef]
- Borrero-Garcia, L.D.; Moro-Carrion, M.; Torres-Cintron, C.R.; Centeno-Girona, H.; Perez, V.; Santos-Colon, T.; Gonzalez-Pons, M. Disparities in Colorectal Cancer Incidence Trends Among Hispanics Living in Puerto Rico (2000–2021): A Comparison with Surveillance, Epidemiology, and End Results (SEER) Database. Cancer Med. 2025, 14, e70851. [Google Scholar] [CrossRef]
- Zavala, V.A.; Bracci, P.M.; Carethers, J.M.; Carvajal-Carmona, L.; Coggins, N.B.; Cruz-Correa, M.R.; Davis, M.; de Smith, A.J.; Dutil, J.; Figueiredo, J.C.; et al. Cancer health disparities in racial/ethnic minorities in the United States. Br. J. Cancer 2021, 124, 315–332. [Google Scholar] [CrossRef]
- Demb, J.; Gomez, S.L.; Canchola, A.J.; Qian, A.; Murphy, J.D.; Winn, R.A.; Banegas, M.P.; Gupta, S.; Martinez, M.E. Racial and Ethnic Variation in Survival in Early-Onset Colorectal Cancer. JAMA Netw. Open 2024, 11, e2446820. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 7–34. [Google Scholar] [CrossRef]
- Miller, K.D.; Goding Sauer, A.; Ortiz, A.P.; Fedewa, S.A.; Pinheiro, P.S.; Tortolero-Luna, G.; Martinez-Tyson, D.; Jemal, A.; Siegel, R.L. Cancer Statistics for Hispanics/Latinos, 2018. CA Cancer J. Clin. 2018, 68, 425–445. [Google Scholar] [CrossRef] [PubMed]
- Race and Ethnicity in the United States: 2010 Census and 2020 Census. Available online: https://www.census.gov/library/visualizations/interactive/race-and-ethnicity-in-the-united-state-2010-and-2020-census.html (accessed on 15 October 2024).
- Detailed Races and Ethnicities in the United States and Puerto Rico: 2020 Census. Available online: https://www.census.gov/library/visualizations/interactive/detailed-race-ethnicities-2020-census.html (accessed on 15 October 2024).
- Carethers, J.M. Racial and ethnic disparities in colorectal cancer incidence and mortality. Adv. Cancer Res. 2021, 151, 197–229. [Google Scholar] [PubMed]
- Colorectal Cancer Is a Major Public Health Problem. Available online: https://nccrt.org/our-impact/data-and-progress/ (accessed on 6 October 2025).
- Law No. 107, 5 June 2012. Available online: https://bvirtualogp.pr.gov/ogp/Bvirtual/leyesreferencia/PDF/107-2012.pdf (accessed on 29 October 2025).
- Quality of Care in Puerto Rico. Available online: https://www.medicaid.gov/state-overviews/puerto-rico.html (accessed on 19 October 2025).
- Ortiz-Ortiz, K.J.; Ramírez-García, R.; Cruz-Correa, M.; Ríos-González, M.Y.; Ortiz, A.P. Effects of Type of Health Insurance Coverage on Colorectal Cancer Survival in Puerto Rico: A Population-Based Study. PLoS ONE 2014, 9, e96746. [Google Scholar] [CrossRef]
- Liang, P.S.; Mayer, J.D.; Wakefield, J.; Ko, C.W. Temporal Trends in Geographic and Sociodemographic Disparities in Colorectal Cancer Among Medicare Patients, 1973–2010. J. Rural Health 2016, 33, 361. [Google Scholar] [CrossRef] [PubMed]
- Carethers, J.M.; Doubeni, C.A. Causes of Socioeconomic Disparities in Colorectal Cancer and Intervention Framework and Strategies. Gastroenterology 2020, 158, 354–367. [Google Scholar] [CrossRef]
- Bailey, C.E.; Hu, C.Y.; You, Y.N.; Bednarski, B.K.; Rodriguez-Bigas, M.A.; Skibber, J.M.; Cantor, S.B.; Chang, G.J. Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975–2010. JAMA Surg. 2015, 150, 17–22. [Google Scholar] [CrossRef]
- Molmenti, C.L.S.; Jacobs, E.T.; Gupta, S.; Thomson, C.A. Early-Onset Colorectal Cancer: A Call for Greater Rigor in Epidemiologic Studies. Cancer Epidemiol. Biomark. Prev. 2022, 31, 507–511. [Google Scholar] [CrossRef]
- Zaki, T.A.; Liang, P.S.; May, F.P.; Murphy, C.C. Racial and Ethnic Disparities in Early-Onset Colorectal Cancer Survival. Clin. Gastroenterol. Hepatol. 2022, 21, 506. [Google Scholar] [CrossRef]
- Pérez-Mayoral, J.; Soto-Salgado, M.; Shah, E.; Kittles, R.; Stern, M.C.; Olivera, M.I.; Gonzalez-Pons, M.; Rodriguez-Quilichinni, S.; Torres, M.; Reyes, J.S.; et al. Association of genetic ancestry with colorectal tumor location in Puerto Rican Latinos. Hum. Genom. 2019, 13, 12. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Ling, Z.; Li, L. The Intestinal Microbiota and Colorectal Cancer. Front. Immunol. 2020, 11, 615056. [Google Scholar] [CrossRef] [PubMed]
- Carter Paulson, E.; Wirtalla, C.; Armstrong, K.; Mahmoud, N.N. Gender influences treatment and survival in colorectal cancer surgery. Dis. Colon Rectum 2009, 52, 1982–1991. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | CRC Mortality | X2 (Degrees of Freedom) | ||||||
|---|---|---|---|---|---|---|---|---|
| PRH | NHW | NHB | NHAI/AN | NHAPI | USH | U.S. | ||
| Total cases | 14,371 | 905,347 | 151,133 | 6185 | 31,746 | 72,000 | 1,168,778 | |
| Sex, n (%) | ||||||||
| Male | 7949 (55.3) | 466,099 (51.5) | 76,907 (50.9) | 3348 (54.1) | 16,500 (52.0) | 40,101 (55.7) | 604,324 (51.7) | 607.78 * (6) |
| Female | 6422 (44.7) | 439,248 (48.5) | 74,226 (49.1) | 2837 (45.9) | 15,246 (48.0) | 31,899 (44.3) | 564,454 (48.3) | |
| Age at death, n (%) | ||||||||
| 20–49 | 885 (6.2) | 48,857 (5.4) | 14,342 (9.5) | 652 (10.5) | 3409 (10.7) | 8794 (12.2) | 76,207 (6.5) | 9.0 × 103 * (6) |
| ≥50 | 13,486 (93.8) | 856,490 (94.6) | 136,791 (90.5) | 5533 (89.5) | 28,337 (89.3) | 63,206 (87.8) | 1,092,571 (93.5) | |
| Characteristics | CRC Age-Adjusted Mortality AAPC (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|
| PRH | NHW | NHB | NHAI/AN | NHAPI | USH | U.S. | ||
| Male | 20–49 yo | 2.77 * (0.92 to 4.95) | 1.15 * (0.86 to 1.61) | −0.79 * (−1.26 to −0.12) | ** | 0.86 * (0.03 to 1.84) | 1.80 * (1.02 to 2.47) | 0.63 * (0.38 to 1.08) |
| ≥50 yo | −1.54 * (−2.46 to −0.48) | −2.68 * (−2.77 to −2.59) | −2.69 * (−2.84 to −2.54) | −1.36 * (−2.06 to −0.50) | −2.17 * (−2.43 to −1.85) | −1.72 * (−1.88 to −1.52) | −2.65 * (−2.73 to −2.58) | |
| Overall (≥20 yo) | −1.33 * (−2.27 to −0.23) | −2.38 * (−2.44 to −2.31) | −2.52 * (−2.67 to −2.35) | −0.097 * (−1.56 to −0.25) | −1.92 * (−2.18 to −1.60) | −1.51 * (−1.65 to −1.33) | −2.39 * (−2.46 to −2.31) | |
| Female | 20–49 yo | 0.14 (−1.32 to 1.57) | 1.24 * (0.83 to 1.66) | −0.99 * (−1.46 to −0.52) | ** | −0.04 (−0.88 to 0.97) | 0.06 (−0.57 to 1.13) | 0.47 * (0.19 to 0.87) |
| ≥50 yo | −2.17 * (−2.90 to −1.48) | −2.55 * (−2.65 to −2.45) | −3.21 * (−3.43 to −2.98) | −1.01 (−2.38 to 1.07) | −1.94 * (−2.44 to −1.32) | −1.83 * (−2.17 to −1.58) | −2.66 * (−2.79 to −2.53) | |
| Overall (≥20 yo) | −1.87 * (−2.82 to −0.79) | −2.25 * (−2.34 to −2.15) | −3.01 * (−3.21 to −2.81) | −0.73 (−2.16 to 1.45) | −1.76 * (−2.23 to −1.17) | −1.61 * (−1.89 to −1.36) | −2.39 * (−2.51 to −2.28) | |
| Overall | 20–49 yo | 1.58 * (0.41 to 2.83) | 1.16 * (0.85 to 1.58) | −0.93 * (−1.30 to −0.38) | 2.87 * (1.30 to 4.78) | 0.77 (−0.03 to 1.57) | 1.53 * (0.89 to 2.31) | 0.57 * (0.38 to 0.81) |
| ≥50 yo | −1.90 * (−2.52 to −1.29) | −2.55 * (−2.62 to −2.47) | −2.89 * (−3.02 to −2.75) | −1.28 * (−2.08 to −0.07) | −2.01 * (−2.28 to −1.67) | −1.77 * (−1.91 to −1.59) | −2.61 * (−2.71 to −2.51) | |
| Overall (≥20 yo) | −1.56 * (−2.39 to −0.70) | −2.27 * (−2.35 to −2.19) | −2.70 * (−2.82 to −2.58) | −0.92 (−1.75 to 0.45) | −1.79 * (−2.06 to −1.46) | −1.52 * (−1.67 to −1.33) | −2.35 * (−2.43 to −2.25) | |
| Characteristics | PRH (n = 6996) % Survival (CI) | NHW (n = 80,511) % Survival (CI) | NHB (n = 14,101) % Survival (CI) | NHAI/AN (n = 1071) % Survival (CI) | NHAPI (n = 11,846) % Survival (CI) | USH (n = 16,463) % Survival (CI) |
|---|---|---|---|---|---|---|
| Age group | ||||||
| 20–49 yo | 64.6 (60.8–68.1) | 69.5 (68.5–70.5) | 58.9 (56.6–61.1) | 65.1 (56.9–72.2) | 68.0 (65.5–70.3) | 63.4 (61.5–65.2) |
| ≥50 yo | 62.6 (61.2–64.0) | 66.8 (66.3–67.2) | 58.8 (57.7–59.8) | 65.5 (61.5–69.1) | 67.5 (66.4–68.5) | 64.9 (63.9–65.8) |
| Stage at Diagnosis | ||||||
| Localized | 85.5 (83.7–87.2) | 91.0 (90.4–91.5) | 87.0 (85.5–88.3) | 91.4 (85.5–95.0) | 89.9 (88.6–91.1) | 88.8 (87.6–89.9) |
| Regional | 61.1 (59.0–63.2) | 73.6 (73.0–74.2) | 69.4 (67.9–70.9) | 71.3 (65.4–76.4) | 74.7 (73.2–76.1) | 72.7 (71.4–73.9) |
| Distant | 11.8 (9.9–13.9) | 15.4 (14.8–16.0) | 11.3 (10.3–12.4) | 16.1 (11.6–21.3) | 17.0 (15.4–18.6) | 15.7 (14.5–17.0) |
| Male % Survival (CI) | Female % Survival (CI) | Overall % Survival (CI) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1-year | 3-year | 5-year | 1-year | 3-year | 5-year | 1-year | 3-year | 5-year | |
| PRH | 85.5 (81.2–88.8) | 66.8 (61.5–71.6) | 61.0 (55.5–66.1) | 88.5 (84.5–91.5) | 75.6 (70.5–79.9) | 68.3 (62.9–73.1) | 86.9 (84.1–89.3) | 71.1 (67.5–74.4) | 64.6 (60.8–68.1) |
| NHW | 91.3 (90.4–92.1) | 76.2 (74.9–77.4) | 68.2 (66.8–69.5) | 92.7 (91.8–93.5) | 78.9 (77.6–80.2) | 71.1 (69.6–72.6) | 91.9 (91.3–92.5) | 77.4 (76.5–78.3) | 69.5 (68.5–70.5) |
| NHB | 87.3 (84.9–89.3) | 64.9 (61.7–67.9) | 54.3 (50.9–57.5) | 90.0 (88.0–91.7) | 70.8 (67.8–73.6) | 63.2 (60.1–66.2) | 88.7 (87.2–90.0) | 67.9 (65.8–70.0) | 58.9 (56.6–61.1) |
| NHAI/AN | 91.2 (82.4–95.7) | 74.7 (63.4–82.9) | 63.7 (51.8–73.3) | 83.7 (73.3–90.3) | 73.9 (62.3–82.5) | 66.7 (54.5–76.3) | 87.7 (81.4–91.9) | 74.3 (66.6–80.6) | 65.1 (56.9–72.2) |
| NHAPI | 91.6 (89.5–93.3) | 75.1 (72.0–78.0) | 64.9 (61.5–68.1) | 93.6 (91.6–95.2) | 79.1 (75.9–81.9) | 71.5 (68.0–74.7) | 92.5 (91.1–93.7) | 77.0 (74.8–79.0) | 68.0 (65.5–70.3) |
| USH | 91.0 (89.4–92.3) | 71.8 (69.4–74.1) | 60.9 (58.3–63.4) | 92.9 (91.4–94.2) | 75.2 (72.8–77.5) | 66.3 (63.5–68.8) | 91.9 (90.8–92.8) | 73.4 (71.7–75.0) | 63.4 (61.5–65.2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montalvo-Pacheco, C.; Torres-Cintrón, C.R.; Moró-Carrión, M.; Centeno-Girona, H.; Borrero-García, L.D.; González-Pons, M. Disparities in Colorectal Cancer Mortality and Survival Trends Among Hispanics Living in Puerto Rico (2000–2021): A Comparison Between Early-Onset and Average-Onset Disease. Life 2025, 15, 1742. https://doi.org/10.3390/life15111742
Montalvo-Pacheco C, Torres-Cintrón CR, Moró-Carrión M, Centeno-Girona H, Borrero-García LD, González-Pons M. Disparities in Colorectal Cancer Mortality and Survival Trends Among Hispanics Living in Puerto Rico (2000–2021): A Comparison Between Early-Onset and Average-Onset Disease. Life. 2025; 15(11):1742. https://doi.org/10.3390/life15111742
Chicago/Turabian StyleMontalvo-Pacheco, Camille, Carlos R. Torres-Cintrón, Marilyn Moró-Carrión, Hilmaris Centeno-Girona, Luis D. Borrero-García, and María González-Pons. 2025. "Disparities in Colorectal Cancer Mortality and Survival Trends Among Hispanics Living in Puerto Rico (2000–2021): A Comparison Between Early-Onset and Average-Onset Disease" Life 15, no. 11: 1742. https://doi.org/10.3390/life15111742
APA StyleMontalvo-Pacheco, C., Torres-Cintrón, C. R., Moró-Carrión, M., Centeno-Girona, H., Borrero-García, L. D., & González-Pons, M. (2025). Disparities in Colorectal Cancer Mortality and Survival Trends Among Hispanics Living in Puerto Rico (2000–2021): A Comparison Between Early-Onset and Average-Onset Disease. Life, 15(11), 1742. https://doi.org/10.3390/life15111742






