Overview: A Comprehensive Review of Soft Wearable Rehabilitation and Assistive Devices, with a Focus on the Function, Design and Control of Lower-Limb Exoskeletons
Abstract
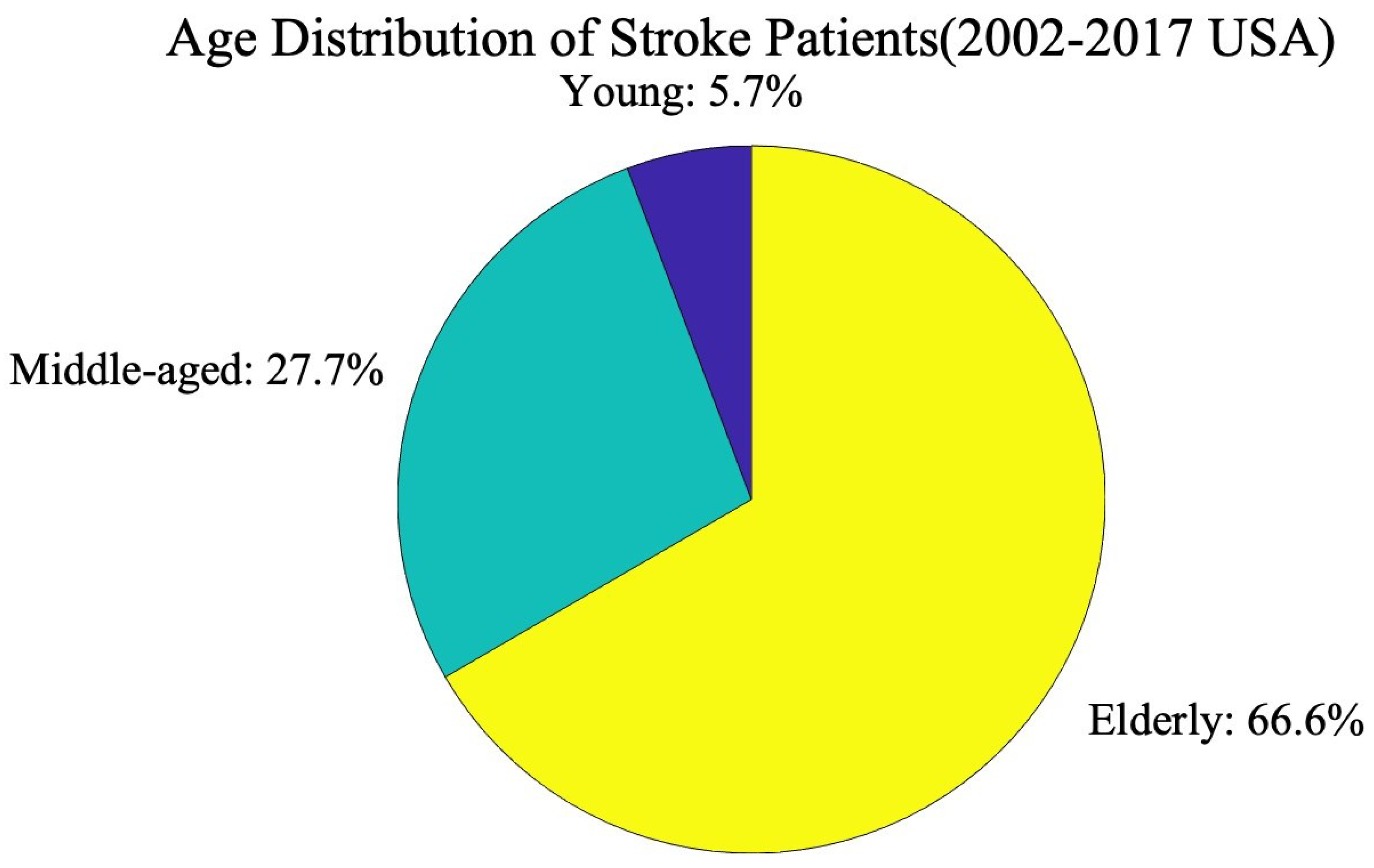
1. Introduction
2. Search Strategy
3. Lower-Limb Bio-Mechanics
3.1. Lower-Limb Joint Movements
3.1.1. Hip Joint
3.1.2. Knee Joint
3.1.3. Ankle Joint
3.2. Lower-Limb Muscles
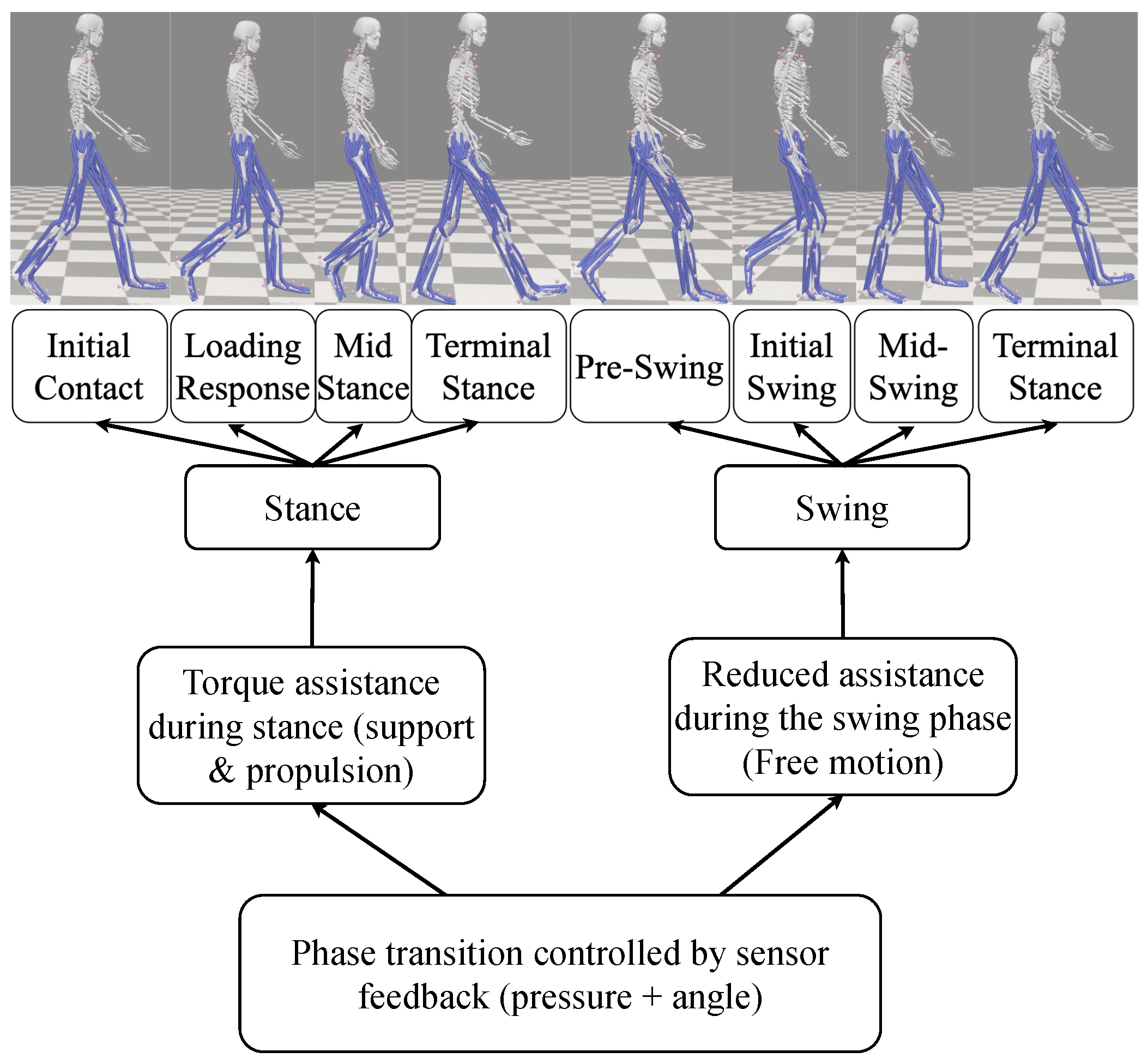
3.3. Gait Analysis
4. Rigid and Soft Exoskeletons
4.1. Active and Passive Exoskeletons
4.2. Lower-Limb Exoskeleton Based on Functions
4.2.1. Rehabilitation Exoskeleton
4.2.2. Enhanced Exoskeleton
4.2.3. Others
4.3. Actuator Types of Lower-Limb Exoskeleton
4.3.1. Electric
4.3.2. Pneumatic
4.3.3. Hydraulic
4.3.4. Cable Driven
4.3.5. Series Elastic Actuation (SEA)
4.4. Sensors Used in Exoskeleton
4.4.1. Dynamic Sensor
4.4.2. Electromyography (EMG) Sensor
4.4.3. Electroencephalography (EEG) Sensors
4.4.4. Encoders
4.4.5. Vision Systems
4.4.6. Recent Advances in Soft and Flexible Sensing Technologies
4.5. Control Strategies of Lower-Limb Exoskeleton
4.5.1. User and Environment Controls
4.5.2. AI-Driven Control Strategies
4.5.3. Continuous Behaviour Control of Robots
4.5.4. Actuator Control Strategy
5. Discussion
5.1. Clinical Trial Status and Details
5.2. Challenges and Future Works
5.2.1. Weight Reduction
5.2.2. Flexibility
5.2.3. Universality
5.2.4. Cost
5.2.5. Energy
5.2.6. Control
5.2.7. Durability Evaluation of Soft Exoskeletons
5.2.8. Future Research Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pinto-Fernandez, D.; Torricelli, D.; del Carmen Sanchez-Villamanan, M.; Aller, F.; Mombaur, K.; Conti, R.; Vitiello, N.; Moreno, J.C.; Pons, J.L. Performance evaluation of lower limb exoskeletons: A systematic review. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 1573–1583. [Google Scholar] [CrossRef]
- Khomami, A.M.; Najafi, F. A survey on soft lower limb cable-driven wearable robots without rigid links and joints. Robot. Auton. Syst. 2021, 144, 103846. [Google Scholar] [CrossRef]
- Dollar, A.M.; Herr, H. Lower extremity exoskeletons and active orthoses: Challenges and state-of-the-art. IEEE Trans. Robot. 2008, 24, 144–158. [Google Scholar] [CrossRef]
- Morris, L.; Diteesawat, R.S.; Rahman, N.; Turton, A.; Cramp, M.; Rossiter, J. The-state-of-the-art of soft robotics to assist mobility: A review of physiotherapist and patient identified limitations of current lower-limb exoskeletons and the potential soft-robotic solutions. J. Neuroeng. Rehabil. 2023, 20, 18. [Google Scholar] [CrossRef] [PubMed]
- Avan, A.; Digaleh, H.; Di Napoli, M.; Stranges, S.; Behrouz, R.; Shojaeianbabaei, G.; Amiri, A.; Tabrizi, R.; Mokhber, N.; Spence, J.D.; et al. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: An ecological analysis from the Global Burden of Disease Study 2017. BMC Med. 2019, 17, 191. [Google Scholar] [CrossRef]
- Khan, S.U.; Khan, M.Z.; Khan, M.U.; Khan, M.S.; Mamas, M.A.; Rashid, M.; Blankstein, R.; Virani, S.S.; Johansen, M.C.; Shapiro, M.D.; et al. Clinical and economic burden of stroke among young, midlife, and older adults in the United States, 2002–2017. Mayo Clin. Proc. Innov. Qual. Outcomes 2021, 5, 431–441. [Google Scholar] [CrossRef]
- Kapsalyamov, A.; Jamwal, P.K.; Hussain, S.; Ghayesh, M.H. State of the art lower limb robotic exoskeletons for elderly assistance. IEEE Access 2019, 7, 95075–95086. [Google Scholar] [CrossRef]
- Kalita, B.; Narayan, J.; Dwivedy, S.K. Development of active lower limb robotic-based orthosis and exoskeleton devices: A systematic review. Int. J. Soc. Robot. 2021, 13, 775–793. [Google Scholar] [CrossRef]
- Tan, C.; Sun, F.; Fang, B.; Kong, T.; Zhang, W. Autoencoder-based transfer learning in brain–computer interface for rehabilitation robot. Int. J. Adv. Robot. Syst. 2019, 16, 1729881419840860. [Google Scholar] [CrossRef]
- Murphy, S.J.; Werring, D.J. Stroke: Causes and clinical features. Medicine 2020, 48, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Aliman, N.; Ramli, R.; Haris, S.M. Design and development of lower limb exoskeletons: A survey. Robot. Auton. Syst. 2017, 95, 102–116. [Google Scholar] [CrossRef]
- Cempini, M.; De Rossi, S.M.M.; Lenzi, T.; Vitiello, N.; Carrozza, M.C. Self-alignment mechanisms for assistive wearable robots: A kinetostatic compatibility method. IEEE Trans. Robot. 2012, 29, 236–250. [Google Scholar] [CrossRef]
- Zanotto, D.; Akiyama, Y.; Stegall, P.; Agrawal, S.K. Knee joint misalignment in exoskeletons for the lower extremities: Effects on user’s gait. IEEE Trans. Robot. 2015, 31, 978–987. [Google Scholar] [CrossRef]
- Amigo, L.E.; Casals, A.; Amat, J. Design of a 3-DoF joint system with dynamic servo-adaptation in orthotic applications. In Proceedings of the 2011 IEEE International Conference on Robotics and Automation, Shanghai, China, 9–13 May 2011; IEEE: Piscataway, NJ, USA, 2011; pp. 3700–3705. [Google Scholar]
- Sanchez-Villamañan, M.d.C.; Gonzalez-Vargas, J.; Torricelli, D.; Moreno, J.C.; Pons, J.L. Compliant lower limb exoskeletons: A comprehensive review on mechanical design principles. J. Neuroeng. Rehabil. 2019, 16, 55. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Choi, J.; Kim, S.J.; Seo, K.H.; Kim, J. Design of an Inflatable Wrinkle Actuator With Fast Inflation/Deflation Responses for Wearable Suits. IEEE Robot. Autom. Lett. 2020, 5, 3799–3805. [Google Scholar] [CrossRef]
- Park, Y.L.; Chen, B.r.; Young, D.; Stirling, L.; Wood, R.J.; Goldfield, E.; Nagpal, R. Bio-inspired active soft orthotic device for ankle foot pathologies. In Proceedings of the 2011 IEEE/RSJ International Conference on Intelligent Robots and Systems, San Francisco, CA, USA, 25–30 September 2011; IEEE: Piscataway, NJ, USA, 2011; pp. 4488–4495. [Google Scholar]
- Asbeck, A.T.; Dyer, R.J.; Larusson, A.F.; Walsh, C.J. Biologically-inspired soft exosuit. In Proceedings of the 2013 IEEE 13th International Conference on Rehabilitation Robotics (ICORR), Seattle, WA, USA, 24–26 June 2013; IEEE: Piscataway, NJ, USA, 2013; pp. 1–8. [Google Scholar]
- Tucker, M.R.; Olivier, J.; Pagel, A.; Bleuler, H.; Bouri, M.; Lambercy, O.; del R Millan, J.; Riener, R.; Vallery, H.; Gassert, R. Control strategies for active lower extremity prosthetics and orthotics: A review. J. Neuroeng. Rehabil. 2015, 12, 1. [Google Scholar] [CrossRef]
- Yan, T.; Cempini, M.; Oddo, C.M.; Vitiello, N. Review of assistive strategies in powered lower-limb orthoses and exoskeletons. Robot. Auton. Syst. 2015, 64, 120–136. [Google Scholar] [CrossRef]
- Chen, B.; Ma, H.; Qin, L.-Y.; Gao, F.; Chan, K.-M.; Law, S.-W.; Qin, L.; Liao, W.-H. Recent developments and challenges of lower extremity exoskeletons. J. Orthop. Transl. 2016, 5, 26–37. [Google Scholar] [CrossRef]
- Shi, D.; Zhang, W.; Zhang, W.; Ding, X. A review on lower limb rehabilitation exoskeleton robots. Chin. J. Mech. Eng. 2019, 32, 1–11. [Google Scholar] [CrossRef]
- Panizzolo, F.A.; Galiana, I.; Asbeck, A.T.; Siviy, C.; Schmidt, K.; Holt, K.G.; Walsh, C.J. A biologically-inspired multi-joint soft exosuit that can reduce the energy cost of loaded walking. J. Neuroeng. Rehabil. 2016, 13, 43. [Google Scholar] [CrossRef]
- Li, Z.; Li, X.; Li, Q.; Su, H.; Kan, Z.; He, W. Human-in-the-loop control of soft exosuits using impedance learning on different terrains. IEEE Trans. Robot. 2022, 38, 2979–2993. [Google Scholar] [CrossRef]
- Di Natali, C.; Poliero, T.; Sposito, M.; Graf, E.; Bauer, C.; Pauli, C.; Bottenberg, E.; De Eyto, A.; O’Sullivan, L.; Hidalgo, A.F.; et al. Design and evaluation of a soft assistive lower limb exoskeleton. Robotica 2019, 37, 2014–2034. [Google Scholar] [CrossRef]
- Totaro, M.; Poliero, T.; Mondini, A.; Lucarotti, C.; Cairoli, G.; Ortiz, J.; Beccai, L. Soft smart garments for lower limb joint position analysis. Sensors 2017, 17, 2314. [Google Scholar] [CrossRef]
- Madeti, B.K.; Chalamalasetti, S.R.; Bolla Pragada, S.S.s.r. Biomechanics of knee joint—A review. Front. Mech. Eng. 2015, 10, 176–186. [Google Scholar] [CrossRef]
- Anderson, F.C.; Pandy, M.G. Dynamic optimization of human walking. J. Biomech. Eng. 2001, 123, 381–390. [Google Scholar] [CrossRef]
- Rajagopal, A.; Dembia, C.L.; DeMers, M.S.; Delp, S.L.; Hicks, J.L.; Delp, S.L. Full-body musculoskeletal model for muscle-driven simulation of human gait. IEEE Trans. Biomed. Eng. 2016, 63, 2068–2079. [Google Scholar] [CrossRef] [PubMed]
- Pamungkas, D.S.; Caesarendra, W.; Soebakti, H.; Analia, R.; Susanto, S. Overview: Types of lower limb exoskeletons. Electronics 2019, 8, 1283. [Google Scholar] [CrossRef]
- Zarins, B.; Rowe, C.R.; Harris, B.A.; Watkins, M.P. Rotational motion of the knee. Am. J. Sport. Med. 1983, 11, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Brockett, C.L.; Chapman, G.J. Biomechanics of the ankle. Orthop. Trauma 2016, 30, 232–238. [Google Scholar] [CrossRef]
- Rydell, N. Biomechanics of the hip-joint. Clin. Orthop. Relat. Res. 1973, 92, 6–15. [Google Scholar] [CrossRef]
- Aspden, R.M.; Rudman, K.; Meakin, J.R. A mechanism for balancing the human body on the hips. J. Biomech. 2006, 39, 1757–1759. [Google Scholar] [CrossRef]
- Mow, V.C.; Ateshian, G.A.; Spilker, R.L. Biomechanics of diarthrodial joints: A review of twenty years of progress. J. Biomech. Eng. 1993, 115, 460–467. [Google Scholar] [CrossRef]
- Benedetti, M.G.; Bonato, P.; Catani, F.; D’Alessio, T.; Knaflitz, M.; Marcacci, M.; Simoncini, L. Myoelectric activation pattern during gait in total knee replacement: Relationship with kinematics, kinetics, and clinical outcome. IEEE Trans. Rehabil. Eng. 1999, 7, 140–149. [Google Scholar] [CrossRef]
- Messier, S.P.; Loeser, R.F.; Hoover, J.L.; Semble, E.L.; Wise, C.M. Osteoarthritis of the knee: Effects on gait, strength, and flexibility. Arch. Phys. Med. Rehabil. 1992, 73, 29–36. [Google Scholar] [PubMed]
- Childs, J.D.; Sparto, P.J.; Fitzgerald, G.K.; Bizzini, M.; Irrgang, J.J. Alterations in lower extremity movement and muscle activation patterns in individuals with knee osteoarthritis. Clin. Biomech. 2004, 19, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Romanes, G.J. Cunningham’s Manual of Practical Anatomy; Oxford University Press: Oxford, UK, 1986. [Google Scholar]
- Grimston, S.K.; Nigg, B.M.; Hanley, D.A.; Engsberg, J.R. Differences in ankle joint complex range of motion as a function of age. Foot Ankle 1993, 14, 215–222. [Google Scholar] [CrossRef]
- Nordin, M.; Frankel, V.H. Basic Biomechanics of the Musculoskeletal System; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2001. [Google Scholar]
- Burdett, R. Forces predicted at the ankle during running. Med. Sci. Sport. Exerc. 1982, 14, 308–316. [Google Scholar] [CrossRef] [PubMed]
- Inman, V.T. Functional aspects of the abductor muscles of the hip. JBJS 1947, 29, 607–619. [Google Scholar]
- Bartlett, J.L.; Sumner, B.; Ellis, R.G.; Kram, R. Activity and functions of the human gluteal muscles in walking, running, sprinting, and climbing. Am. J. Phys. Anthropol. 2014, 153, 124–131. [Google Scholar] [CrossRef]
- Kaplan, E.B. Some aspects of functional anatomy of the human knee joint. Clin. Orthop. Relat. Res. 1962, 23, 18–29. [Google Scholar]
- LaPrade, R.F.; Wentorf, F. Diagnosis and treatment of posterolateral knee injuries. Clin. Orthop. Relat. Res. (1976–2007) 2002, 402, 110–121. [Google Scholar] [CrossRef]
- Whittle, M.W. Clinical gait analysis: A review. Hum. Mov. Sci. 1996, 15, 369–387. [Google Scholar] [CrossRef]
- Moon, D.; Esquenazi, A. Instrumented gait analysis: A tool in the treatment of spastic gait dysfunction. JBJS Rev. 2016, 4, e1. [Google Scholar] [CrossRef] [PubMed]
- Kazerooni, H.; Racine, J.L.; Huang, L.; Steger, R. On the Control of the Berkeley Lower Extremity Exoskeleton (BLEEX). In Proceedings of the 2005 IEEE International Conference on Robotics and Automation, Barcelona, Spain, 18–22 April 2005; pp. 4353–4360. [Google Scholar] [CrossRef]
- Wang, S.; Wang, L.; Meijneke, C.; van Asseldonk, E.; Hoellinger, T.; Cheron, G.; Ivanenko, Y.; La Scaleia, V.; Sylos-Labini, F.; Molinari, M.; et al. Design and Control of the MINDWALKER Exoskeleton. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 23, 277–286. [Google Scholar] [CrossRef]
- Sethi, D.; Bharti, S.; Prakash, C. A comprehensive survey on gait analysis: History, parameters, approaches, pose estimation, and future work. Artif. Intell. Med. 2022, 129, 102314. [Google Scholar] [CrossRef] [PubMed]
- Long, Y.; Cai, Z.; Guo, H. AES-SEA and bionic knee based lower limb exoskeleton design and LQR-Virtual tunnel control. J. Bionic Eng. 2025, 22, 1231–1248. [Google Scholar] [CrossRef]
- Zhang, L.; Song, G.; Yang, C.; Zou, C.; Cheng, H.; Huang, R.; Qiu, J.; Yin, Z. A Parallel Compliant Leg for energy efficient walking of exoskeleton–walker systems. Mechatronics 2024, 98, 103110. [Google Scholar] [CrossRef]
- Ju, H.; Li, H.; Guo, S.; Fu, Y.; Zhang, Q.; Zheng, T.; Zhao, J.; Zhu, Y. J-Exo: An exoskeleton with telescoping linear actuators to help older people climb stairs and squat. Sens. Actuators A Phys. 2024, 366, 115034. [Google Scholar] [CrossRef]
- Wei, D.; Wei, X.; Zhang, Z.; Gao, T.; Mo, X.; Verstraten, T.; Vanderborght, B.; Dong, D. Bionic Ankle Tensegrity Exoskeleton with Considerable Load Bearing Capability. IEEE Trans. Med. Robot. Bionics 2023, 5, 1057–1066. [Google Scholar] [CrossRef]
- Sarajchi, M.; Sirlantzis, K. Design and control of a single-leg exoskeleton with gravity compensation for children with unilateral cerebral palsy. Sensors 2023, 23, 6103. [Google Scholar] [CrossRef]
- Zhang, Z. An Adaptive Lower Limb Rehabilitation Exoskeleton Robot Designing Scheme. In Proceedings of the 2022 3rd International Conference on Intelligent Design (ICID), Xi’an, China, 21–23 October 2022; IEEE: Piscataway, NJ, USA, 2022; pp. 244–248. [Google Scholar]
- Liu, L.; Wang, J.; Wu, J.; Dong, L.; Wang, X.; Tian, M. Lower limb-assisted exoskeleton to support walking up and down stairs. In Proceedings of the 2022 28th International Conference on Mechatronics and Machine Vision in Practice (M2VIP), Nanjing, China, 16–18 November 2022; IEEE: Piscataway, NJ, USA, 2022; pp. 1–6. [Google Scholar]
- He, Z.; Chen, S.; Zhang, X.; Huang, G.; Wang, J. Structural Design and Analysis of Unpowered Exoskeleton for Lower Limb. In Proceedings of the 2021 IEEE International Conference on Robotics and Biomimetics (ROBIO), Sanya, China, 6–10 December 2021; IEEE: Piscataway, NJ, USA, 2021; pp. 237–242. [Google Scholar]
- Wang, T.; Zhu, Y.; Zheng, T.; Sui, D.; Zhao, S.; Zhao, J. PALExo: A parallel actuated lower limb exoskeleton for high-load carrying. IEEE Access 2020, 8, 67250–67262. [Google Scholar] [CrossRef]
- Zhou, L.; Chen, W.; Chen, W.; Bai, S.; Wang, J. A Novel Portable Lower Limb Exoskeleton for Gravity Compensation during Walking. In Proceedings of the 2020 IEEE International Conference on Robotics and Automation (ICRA), Paris, France, 31 May–31 August 2020; pp. 768–773. [Google Scholar] [CrossRef]
- Koseki, K.; Mutsuzaki, H.; Yoshikawa, K.; Endo, Y.; Maezawa, T.; Takano, H.; Yozu, A.; Kohno, Y. Gait training using the Honda Walking Assistive Device® in a patient who underwent total hip arthroplasty: A single-subject study. Medicina 2019, 55, 69. [Google Scholar] [CrossRef]
- Tian, M.; Wang, X.; Wang, J.; Gan, Z. Design of A Lower Limb Exoskeleton Driven by Tendon-sheath Artificial Muscle. In Proceedings of the 2019 IEEE International Conference on Robotics and Biomimetics (ROBIO), Dali, China, 6–8 December 2019; pp. 2037–2042. [Google Scholar] [CrossRef]
- Ortiz, J.; Di Natali, C.; Caldwell, D.G. XoSoft: Design of a novel soft modular exoskeleton. In Soft Robotics in Rehabilitation; Elsevier: Amsterdam, The Netherlands, 2021; pp. 165–198. [Google Scholar]
- Hartigan, C.; Kandilakis, C.; Dalley, S.; Clausen, M.; Wilson, E.; Morrison, S.; Etheridge, S.; Farris, R. Mobility outcomes following five training sessions with a powered exoskeleton. Top. Spinal Cord Inj. Rehabil. 2015, 21, 93–99. [Google Scholar] [CrossRef]
- Sankai, Y. Leading Edge of Cybernics: Robot Suit HAL. In Proceedings of the 2006 SICE-ICASE International Joint Conference, Busan, Republic of Korea, 18–21 October 2006; pp. P-1–P-2. [Google Scholar] [CrossRef]
- de la Tejera, J.A.; Bustamante-Bello, R.; Ramirez-Mendoza, R.A.; Izquierdo-Reyes, J. Systematic review of exoskeletons towards a general categorization model proposal. Appl. Sci. 2020, 11, 76. [Google Scholar] [CrossRef]
- Zoss, A.; Kazerooni, H.; Chu, A. On the mechanical design of the Berkeley Lower Extremity Exoskeleton (BLEEX). In Proceedings of the 2005 IEEE/RSJ International Conference on Intelligent Robots and Systems, Edmonton, AB, Canada, 2–6 August 2005; IEEE: Piscataway, NJ, USA, 2005; pp. 3465–3472. [Google Scholar]
- Graf, E.S.; Bauer, C.M.; Power, V.; de Eyto, A.; Bottenberg, E.; Poliero, T.; Sposito, M.; Scherly, D.; Henke, R.; Pauli, C.; et al. Basic functionality of a prototype wearable assistive soft exoskeleton for people with gait impairments: A case study. In Proceedings of the 11th Pervasive Technologies Related to Assistive Environments Conference, Corfu, Greece, 26–29 June 2018; pp. 202–207. [Google Scholar]
- Gopura, R.; Kiguchi, K.; Bandara, D. A brief review on upper extremity robotic exoskeleton systems. In Proceedings of the 2011 6th international Conference on Industrial and Information Systems, Kandy, Sri Lanka, 16–19 August 2011; IEEE: Piscataway, NJ, USA, 2011; pp. 346–351. [Google Scholar]
- Matthew, R.P.; Mica, E.J.; Meinhold, W.; Loeza, J.A.; Tomizuka, M.; Bajcsy, R. Introduction and initial exploration of an active/passive exoskeleton framework for portable assistance. In Proceedings of the 2015 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Hamburg, Germany, 28 September–2 October 2015; IEEE: Piscataway, NJ, USA, 2015; pp. 5351–5356. [Google Scholar]
- Exoskeleton Report Ekso Indego. 2024. Available online: https://exoskeletonreport.com/product/indego/ (accessed on 16 July 2024).
- Mashable. FDA Approves Robotic Exoskeleton for Paralyzed Individuals: ReWalk. 2024. Available online: https://mashable.com/archive/fda-approves-robotic-exoskeleton-paralyzed-rewalk (accessed on 16 July 2024).
- UC Health Ekso™ Frequently Asked Questions. 2024. Available online: https://www.uchealth.com/services/outpatient-rehab/ekso-bionics-technology/ekso-frequently-asked-questions/ (accessed on 16 July 2024).
- Cost Charts How Much Does an Exoskeleton Cost? 2024. Available online: https://costcharts.com/exoskeleton/ (accessed on 16 July 2024).
- Gardner, A.D.; Potgieter, J.; Noble, F.K. A review of commercially available exoskeletons’ capabilities. In Proceedings of the 2017 24th International Conference on Mechatronics and Machine Vision in Practice (M2VIP), Auckland, New Zealand, 21–23 November 2017; pp. 1–5. [Google Scholar] [CrossRef]
- Riemer, R.; Nuckols, R.W.; Sawicki, G.S. Extracting electricity with exosuit braking. Science 2021, 372, 909–911. [Google Scholar] [CrossRef]
- Donelan, J.M.; Li, Q.; Naing, V.; Hoffer, J.A.; Weber, D.; Kuo, A.D. Biomechanical energy harvesting: Generating electricity during walking with minimal user effort. Science 2008, 319, 807–810. [Google Scholar] [CrossRef]
- Ding, S.; Ouyang, X.; Liu, T.; Li, Z.; Yang, H. Gait event detection of a lower extremity exoskeleton robot by an intelligent IMU. IEEE Sens. J. 2018, 18, 9728–9735. [Google Scholar] [CrossRef]
- Zhou, L.; Chen, W.; Chen, W.; Bai, S.; Zhang, J.; Wang, J. Design of a passive lower limb exoskeleton for walking assistance with gravity compensation. Mech. Mach. Theory 2020, 150, 103840. [Google Scholar] [CrossRef]
- Qiu, S.; Pei, Z.; Wang, C.; Tang, Z. Systematic review on wearable lower extremity robotic exoskeletons for assisted locomotion. J. Bionic Eng. 2023, 20, 436–469. [Google Scholar] [CrossRef]
- Meuleman, J.; van Asseldonk, E.; van Oort, G.; Rietman, H.; van der Kooij, H. LOPES II—Design and Evaluation of an Admittance Controlled Gait Training Robot With Shadow-Leg Approach. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 24, 352–363. [Google Scholar] [CrossRef]
- Kalinowska, A.; Berrueta, T.A.; Zoss, A.; Murphey, T. Data-Driven Gait Segmentation for Walking Assistance in a Lower-Limb Assistive Device. In Proceedings of the 2019 International Conference on Robotics and Automation (ICRA), Montreal, QC, Canada, 20–24 May 2019; pp. 1390–1396. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Andrews, A.W. Normal walking speed: A descriptive meta-analysis. Physiotherapy 2011, 97, 182–189. [Google Scholar] [CrossRef]
- Asbeck, A.T.; De Rossi, S.M.; Holt, K.G.; Walsh, C.J. A biologically inspired soft exosuit for walking assistance. Int. J. Robot. Res. 2015, 34, 744–762. [Google Scholar] [CrossRef]
- Nasiri, R.; Shushtari, M.; Rouhani, H.; Arami, A. Virtual Energy Regulator: A Time-Independent Solution for Control of Lower Limb Exoskeletons. IEEE Robot. Autom. Lett. 2021, 6, 7699–7705. [Google Scholar] [CrossRef]
- Tefertiller, C.; Hays, K.; Jones, J.; Jayaraman, A.; Hartigan, C.; Bushnik, T.; Forrest, G.F. Initial outcomes from a multicenter study utilizing the indego powered exoskeleton in spinal cord injury. Top. Spinal Cord Inj. Rehabil. 2018, 24, 78–85. [Google Scholar] [CrossRef]
- Prassler, E.; Baroncelli, A. Team ReWalk Ranked First in the Cybathlon 2016 Exoskeleton Final [Industrial Activities]. IEEE Robot. Autom. Mag. 2017, 24, 8–10. [Google Scholar] [CrossRef]
- Zeilig, G.; Weingarden, H.; Zwecker, M.; Dudkiewicz, I.; Bloch, A.; Esquenazi, A. Safety and tolerance of the ReWalk™ exoskeleton suit for ambulation by people with complete spinal cord injury: A pilot study. J. Spinal Cord Med. 2012, 35, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Beyl, P.; Van Damme, M.; Van Ham, R.; Vanderborght, B.; Lefeber, D. Pleated Pneumatic Artificial Muscle-Based Actuator System as a Torque Source for Compliant Lower Limb Exoskeletons. IEEE/ASME Trans. Mechatronics 2014, 19, 1046–1056. [Google Scholar] [CrossRef]
- Bogue, R. Robotic exoskeletons: A review of recent progress. Ind. Robot. Int. J. 2015, 42, 5–10. [Google Scholar] [CrossRef]
- Sposito, M.; Poliero, T.; Di Natali, C.; Ortiz, J.; Pauli, C.; Graf, E.; De Eyto, A.; Bottenberg, E.; Caldwell, D. Evaluation of xosoft beta-1 lower limb exoskeleton on a post stroke patient. In Proceedings of the Sixth National Congress of Bioengineering, Milan, Italy, 25–27 June 2018; pp. 25–27. [Google Scholar]
- Tan, X.; Zhang, B.; Liu, G.; Zhao, X.; Zhao, Y. Cadence-insensitive soft exoskeleton design with adaptive gait state detection and iterative force control. IEEE Trans. Autom. Sci. Eng. 2021, 19, 2108–2121. [Google Scholar] [CrossRef]
- Vallery, H.; Veneman, J.; Van Asseldonk, E.; Ekkelenkamp, R.; Buss, M.; Van Der Kooij, H. Compliant actuation of rehabilitation robots. IEEE Robot. Autom. Mag. 2008, 15, 60–69. [Google Scholar] [CrossRef]
- Tiboni, M.; Borboni, A.; Vérité, F.; Bregoli, C.; Amici, C. Sensors and Actuation Technologies in Exoskeletons: A Review. Sensors 2022, 22, 884. [Google Scholar] [CrossRef]
- Costa, N.; Bezdicek, M.; Brown, M.; Gray, J.O.; Caldwell, D.G.; Hutchins, S. Joint motion control of a powered lower limb orthosis for rehabilitation. Int. J. Autom. Comput. 2006, 3, 271–281. [Google Scholar] [CrossRef]
- Wehner, M.; Quinlivan, B.; Aubin, P.M.; Martinez-Villalpando, E.; Baumann, M.; Stirling, L.; Holt, K.; Wood, R.; Walsh, C. A lightweight soft exosuit for gait assistance. In Proceedings of the 2013 IEEE International Conference on Robotics and Automation, Karlsruhe, Germany, 6–10 May 2013; pp. 3362–3369. [Google Scholar] [CrossRef]
- Lee, S.; Kim, J.; Baker, L.; Long, A.; Karavas, N.; Menard, N.; Galiana, I.; Walsh, C.J. Autonomous multi-joint soft exosuit with augmentation-power-based control parameter tuning reduces energy cost of loaded walking. J. Neuroeng. Rehabil. 2018, 15, 66. [Google Scholar] [CrossRef] [PubMed]
- Sridhar, E.P.; Erel, V.; Nasirian, A.; Wijesundara, M.B.; Rahman, M. Design, development, and evaluation of a pneumatically actuated soft wearable robotic elbow exoskeleton for reducing muscle activity and perceived workload. J. Rehabil. Assist. Technol. Eng. 2025, 12, 20556683251347517. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Yang, D.; Chen, J.; Dai, Y.; Jiang, L.; Xie, S.; Liu, H. Using Zone Inflation and Volume Transfer to Design a Fabric-based Pneumatic Exosuit with both Efficiency and Wearability. arXiv 2024, arXiv:2410.11341. [Google Scholar] [CrossRef]
- Feng, M.; Yang, D.; Ren, L.; Wei, G.; Gu, G. X-crossing pneumatic artificial muscles. Sci. Adv. 2023, 9, eadi7133. [Google Scholar] [CrossRef]
- Beil, J.; Perner, G.; Asfour, T. Design and control of the lower limb exoskeleton KIT-EXO-1. In Proceedings of the 2015 IEEE International Conference on Rehabilitation Robotics (ICORR), Singapore, 11–14 August 2015; pp. 119–124. [Google Scholar] [CrossRef]
- Yu, S.; Huang, T.H.; Yang, X.; Jiao, C.; Yang, J.; Chen, Y.; Yi, J.; Su, H. Quasi-Direct Drive Actuation for a Lightweight Hip Exoskeleton with High Backdrivability and High Bandwidth. IEEE/ASME Trans. Mechatronics 2020, 25, 1794–1802. [Google Scholar] [CrossRef] [PubMed]
- Jiang, W.; Ma, B.; Zhang, X.; Liu, H.; Wang, Z. Overview of lower extremity exoskeleton technology. In IOP Conference Series: Earth and Environmental Science; IOP Publishing: Bristol, UK, 2021; Volume 714, p. 032027. [Google Scholar]
- Ortiz, J.; Poliero, T.; Cairoli, G.; Graf, E.; Caldwell, D.G. Energy efficiency analysis and design optimization of an actuation system in a soft modular lower limb exoskeleton. IEEE Robot. Autom. Lett. 2017, 3, 484–491. [Google Scholar] [CrossRef]
- Choi, H.; Seo, K.; Hyung, S.; Shim, Y.; Lim, S.C. Compact hip-force sensor for a gait-assistance exoskeleton system. Sensors 2018, 18, 566. [Google Scholar] [CrossRef]
- Susanto, S.; Simorangkir, I.T.; Analia, R.; Pamungkas, D.S.; Soebhakti, H.; Sani, A.; Caesarendra, W. Real-time identification of knee joint walking gait as preliminary signal for developing lower limb exoskeleton. Electronics 2021, 10, 2117. [Google Scholar] [CrossRef]
- Chandrapal, M.; Chen, X.; Wang, W.; Stanke, B.; Pape, N.L. Preliminary evaluation of intelligent intention estimation algorithms for an actuated lower-limb exoskeleton. Int. J. Adv. Robot. Syst. 2013, 10, 147. [Google Scholar] [CrossRef]
- Wang, C.; Wu, X.; Wang, Z.; Ma, Y. Implementation of a Brain-Computer Interface on a Lower-Limb Exoskeleton. IEEE Access 2018, 6, 38524–38534. [Google Scholar] [CrossRef]
- Jones, C.L.; Wang, F.; Morrison, R.; Sarkar, N.; Kamper, D.G. Design and Development of the Cable Actuated Finger Exoskeleton for Hand Rehabilitation Following Stroke. IEEE/ASME Trans. Mechatronics 2014, 19, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.T.; Chang, C.C.; Sun, P.Y.; Lee, C.L.; Lin, T.C.; Yen, C.K.; Yang, Y.S. Development of multi-axis motor control systems for lower limb robotic exoskeleton. J. Med Biol. Eng. 2019, 39, 752–763. [Google Scholar] [CrossRef]
- Peng, N.; Meng, W.; Wei, Q.; Ai, Q.; Liu, Q.; Xie, S. Wearable Optical Fiber Sensors for Biomechanical Measurement in Medical Rehabilitation: A Review. IEEE Sens. J. 2023, 23, 12455–12469. [Google Scholar] [CrossRef]
- Zhu, P.; Li, Z.; Pang, J.; He, P.; Zhang, S. Latest developments and trends in electronic skin devices. Soft Sci. 2024, 4, 17. [Google Scholar] [CrossRef]
- Karasheva, M.; Saudanbekova, A.; Utepbergen, A.; Akkulova, S.; Niyetkaliyev, A.; Ozhikenov, K.; Ozhiken, A.; Alimbayev, C.; Shylmyrza, U.; Aimukhanbetov, Y. Sensor-driven control strategies for post-stroke shoulder rehabilitation exoskeletons: A systematic review. MethodsX 2025, 15, 103648. [Google Scholar] [CrossRef]
- Baud, R.; Manzoori, A.R.; Ijspeert, A.; Bouri, M. Review of control strategies for lower-limb exoskeletons to assist gait. J. NeuroEng. Rehabil. 2021, 18, 119. [Google Scholar] [CrossRef]
- Bayon, C.; Ramírez, O.; Serrano, J.I.; Del Castillo, M.; Pérez-Somarriba, A.; Belda-Lois, J.M.; Martínez-Caballero, I.; Lerma-Lara, S.; Cifuentes, C.; Frizera, A.; et al. Development and evaluation of a novel robotic platform for gait rehabilitation in patients with Cerebral Palsy: CPWalker. Robot. Auton. Syst. 2017, 91, 101–114. [Google Scholar] [CrossRef]
- Yeung, L.F.; Ockenfeld, C.; Pang, M.K.; Wai, H.W.; Soo, O.Y.; Li, S.W.; Tong, K.Y. Design of an exoskeleton ankle robot for robot-assisted gait training of stroke patients. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; pp. 211–215. [Google Scholar] [CrossRef]
- Laschowski, B.; McNally, W.; Wong, A.; McPhee, J. Preliminary Design of an Environment Recognition System for Controlling Robotic Lower-Limb Prostheses and Exoskeletons. In Proceedings of the 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019; pp. 868–873. [Google Scholar] [CrossRef]
- Krausz, N.E.; Lenzi, T.; Hargrove, L.J. Depth sensing for improved control of lower limb prostheses. IEEE Trans. Biomed. Eng. 2015, 62, 2576–2587. [Google Scholar] [CrossRef]
- Wang, X.; Xie, J.; Guo, S.; Li, Y.; Sun, P.; Gan, Z. Deep reinforcement learning-based rehabilitation robot trajectory planning with optimized reward functions. Adv. Mech. Eng. 2021, 13, 16878140211067011. [Google Scholar] [CrossRef]
- Luo, S.; Androwis, G.; Adamovich, S.; Nunez, E.; Su, H.; Zhou, X. Robust walking control of a lower limb rehabilitation exoskeleton coupled with a musculoskeletal model via deep reinforcement learning. J. Neuroeng. Rehabil. 2023, 20, 34. [Google Scholar] [CrossRef]
- Lin, C.J.; Sie, T.Y. Design and experimental characterization of artificial neural network controller for a lower limb robotic exoskeleton. Actuators 2023, 12, 55. [Google Scholar] [CrossRef]
- Ge, W.; Zhao, J.; Wang, F.; Xu, C.; Yang, Z.; She, J. Experimental design of lower-limb movement recognition based on support vector machine. In Proceedings of the 2022 41st Chinese Control conference (CCC), Hefei, China, 25–27 July 2022; IEEE: Piscataway, NJ, USA, 2022; pp. 6493–6497. [Google Scholar]
- Charbuty, B.; Abdulazeez, A. Classification based on decision tree algorithm for machine learning. J. Appl. Sci. Technol. Trends 2021, 2, 20–28. [Google Scholar] [CrossRef]
- Imura, T.; Iwamoto, Y.; Inagawa, T.; Imada, N.; Tanaka, R.; Toda, H.; Inoue, Y.; Araki, H.; Araki, O. Decision tree algorithm identifies stroke patients likely discharge home after rehabilitation using functional and environmental predictors. J. Stroke Cerebrovasc. Dis. 2021, 30, 105636. [Google Scholar] [CrossRef]
- Coser, O.; Tamantini, C.; Soda, P.; Zollo, L. AI-based methodologies for exoskeleton-assisted rehabilitation of the lower limb: A review. Front. Robot. AI 2024, 11, 1341580. [Google Scholar] [CrossRef]
- Walsh, C.J.; Pasch, K.; Herr, H. An autonomous, underactuated exoskeleton for load-carrying augmentation. In Proceedings of the 2006 IEEE/RSJ International Conference on Intelligent Robots and Systems, Beijing, China, 9–15 October 2006; pp. 1410–1415. [Google Scholar] [CrossRef]
- Shushtari, M.; Foellmer, J.; Arami, A. Human–exoskeleton interaction portrait. J. NeuroEng. Rehabil. 2024, 21, 152. [Google Scholar] [CrossRef] [PubMed]
- Xiong, D.; Zhang, D.; Chu, Y.; Zhao, Y.; Zhao, X. Intuitive Human-Robot-Environment Interaction with EMG Signals: A Review. IEEE/CAA J. Autom. Sin. 2024, 11, 1075–1091. [Google Scholar] [CrossRef]
- Beyl, P.; Knaepen, K.; Duerinck, S.; Van Damme, M.; Vanderborght, B.; Meeusen, R.; Lefeber, D. Safe and compliant guidance by a powered knee exoskeleton for robot-assisted rehabilitation of gait. Adv. Robot. 2011, 25, 513–535. [Google Scholar] [CrossRef]
- Beyl, P.; Van Damme, M.; Cherelle, P.; Lefeber, D. Safe and compliant guidance in robot-assisted gait rehabilitation using Proxy-based Sliding Mode Control. In Proceedings of the 2009 IEEE International Conference on Rehabilitation Robotics, Kyoto, Japan, 23–26 June 2009; pp. 277–282. [Google Scholar] [CrossRef]
- Villa-Parra, A.C.; Delisle-Rodriguez, D.; Souza Lima, J.; Frizera-Neto, A.; Bastos, T. Knee impedance modulation to control an active orthosis using insole sensors. Sensors 2017, 17, 2751. [Google Scholar] [CrossRef]
- Su, D.; Hu, Z.; Wu, J.; Shang, P.; Luo, Z. Review of adaptive control for stroke lower limb exoskeleton rehabilitation robot based on motion intention recognition. Front. Neurorobot. 2023, 17, 1186175. [Google Scholar] [CrossRef]
- Anselmino, E.; Mazzoni, A.; Micera, S. EMG-based prediction of step direction for a better control of lower limb wearable devices. Comput. Methods Programs Biomed. 2024, 254, 108305. [Google Scholar] [CrossRef] [PubMed]
- Mashud, G.; Hasan, S.; Alam, N. Advances in Control Techniques for Rehabilitation Exoskeleton Robots: A Systematic Review. Actuators 2025, 14, 108. [Google Scholar] [CrossRef]
- Miller, L.E.; Zimmermann, A.K.; Herbert, W.G. Clinical effectiveness and safety of powered exoskeleton-assisted walking in patients with spinal cord injury: Systematic review with meta-analysis. Med. Devices Evid. Res. 2016, 9, 455–466. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Eguren, D.; Luu, T.P.; Contreras-Vidal, J.L. Risk management and regulations for lower limb medical exoskeletons: A review. Med. Devices Evid. Res. 2017, 10, 89–107. [Google Scholar] [CrossRef]
- Contreras-Vidal, J.L.; Bhagat, N.A.; Brantley, J.; Cruz-Garza, J.G.; He, Y.; Manley, Q.; Nakagome, S.; Nathan, K.; Tan, S.H.; Zhu, F.; et al. Powered exoskeletons for bipedal locomotion after spinal cord injury. J. Neural Eng. 2016, 13, 031001. [Google Scholar] [CrossRef]
- Kozlowski, A.; Bryce, T.; Dijkers, M. Time and effort required by persons with spinal cord injury to learn to use a powered exoskeleton for assisted walking. Top. Spinal Cord Inj. Rehabil. 2015, 21, 110–121. [Google Scholar] [CrossRef]
- Sale, P.; Russo, E.F.; Russo, M.; Masiero, S.; Piccione, F.; Calabrò, R.S.; Filoni, S. Effects on mobility training and de-adaptations in subjects with spinal cord injury due to a wearable robot: A preliminary report. BMC Neurol. 2016, 16, 12. [Google Scholar] [CrossRef]







| Country | Lower-Limb Soft Exoskeleton | Lower-Limb Exoskeleton |
|---|---|---|
| China | 55 | 1283 |
| Italy | 18 | 200 |
| United States | 17 | 471 |
| Germany | 15 | 118 |
| United Kingdom | 13 | 119 |
| India | 2 | 149 |
| Spain | 4 | 146 |
| No. | Title | Authors | Citations | Reference |
|---|---|---|---|---|
| 1 | State of the Art and Future Directions for Lower Limb Robotic Exoskeletons | Kapsalyamov, A.; Jamwal, P.K.; Hussain, S.; et al. | 761 | [7] |
| 2 | Control Strategies for Active Lower Extremity Prosthetics and Orthotics: A Review | Tucker, M.R.; Olivier, J.; Vallery, H.; et al. | 719 | [19] |
| 3 | Review of Assistive Strategies in Powered Lower-Limb Orthoses and Exoskeletons | Yan, T.; Cempini, M.; Oddo, C.M.; Vitiello, N. | 635 | [20] |
| 4 | Recent Developments and Challenges of Lower Extremity Exoskeletons | Chen, B.; Ma, H.; Qin, L.; Liao, W. | 434 | [21] |
| 5 | A Review on Lower Limb Rehabilitation Exoskeleton Robots | Shi, D.; Zhang, W.; Ding, X. | 432 | [22] |
| No. | Title | Authors | Citations | Reference |
|---|---|---|---|---|
| 1 | A Review on Lower Limb Rehabilitation Exoskeleton Robots | Shi, D.; Zhang, W.; Ding, X. | 432 | [22] |
| 2 | A Biologically-Inspired Multi-Joint Soft Exosuit That Can Reduce the Energy Cost of Loaded Walking | Panizzolo, F.A.; Galiana, I.; Asbeck, A.T.; Walsh, C.J. | 269 | [23] |
| 3 | Human-in-the-Loop Control of Soft Exosuits Using Impedance Learning on Different Terrains | Li, Z.; Li, X.; Kan, Z.; He, W. | 126 | [24] |
| 4 | Design and Evaluation of a Soft Assistive Lower-Limb Exoskeleton | Di Natali, C.; Poliero, T.; Sposito, M.; Ortiz, J.; Caldwell, D.G. | 103 | [25] |
| 5 | Soft Smart Garments for Lower-Limb Joint Position Analysis | Totaro, M.; Poliero, T.; Beccai, L.; Ortiz, J.L.; et al. | 90 | [26] |
| Joints | DoFs | Movement | Degree (°) |
|---|---|---|---|
| Hips | 3 | Flexion–extension | −30 to 120 |
| Abduction–adduction | −50 to 30 | ||
| Internal–external rotation | −40 to 40 | ||
| Knees | 2 | Flexion–extension | 0 to 120 |
| Rotation | −45 to 25 | ||
| Ankles | 3 | Plantar flexion–dorsiflexion | 40 to 50, −10 to 20 |
| Abduction–adduction | −40 to 30 | ||
| Eversion–inversion | −12 to 23 |
| Year | Name | Body Joints | Actuator | Drive Mode | Soft and Rigid | DOFs (Left + Right) | Purpose | Subject Population |
|---|---|---|---|---|---|---|---|---|
| 2025 | AES-SEA lower-limb exoskeleton [52] | Knee Hip (active drive), Ankle (passive drive) | Electric motor | Electric (cable-driven) | Rigid | 3 (2 active + 1 passive) | Gait rehabilitation and motion assistance | Healthy adults |
| 2024 | Parallel Compliant Leg (PCL) [53] | Hip knee ankle | Electric motor | Spring | Soft and rigid | 3 + 3 | Rehabilitation of paraplegic patients | Healthy subject and simulations |
| 2024 | J-Exo [54] | Hip, knee, ankle | Electric motor | Telescopic pole | Rigid | 3 + 3 | Help older people climb stairs and squat | 6 healthy subjects |
| 2023 | BATE [55] | Ankle | N/A | Bowden cable | Soft and rigid | 3 + 3 | Helps support the ankle joint | Experimental platform to simulate the BATE loading process. |
| 2023 | Single-leg exoskeleton (SLE) for children with CP [56] | Hip knee ankle | Electric motor | Gear | Rigid | 3 | Help children with CP | Prototype |
| 2022 | Adaptive lower-limb rehabilitation exoskeleton [57] | Hip knee ankle | servo motor | Hydraulic connecting rod | Rigid | 3 + 3 | Patients with lower-extremity injuries | Prototype |
| 2022 | N/A [58] | Hip knee ankle | Electric motor | cable drive | Soft | N/A | Going up and down stairs | Healthy subject |
| 2021 | unpowered exoskeleton [59] | Hip knee ankle | N/A | Spring | Rigid | 3 + 3 | The load is transferred to the ground | Prototype |
| 2020 | PALExo [60] | Hip knee ankle | Electric motor | Hydraulic pressure | Rigid | 6 + 6 | Carry high loads | Healthy subject |
| 2020 | N/A [61] | Hip Knee | Electric motor | Gear and link | Rigid | 2 + 2 | Gravity compensation | Healthy subject and simulations |
| 2019 | Honda walking assist (HWA) [62] | Hip | Electric motor | trochanter | Rigid | 1 + 1 | Stroke | 5 paralytic |
| 2019 | SEU-EXO [63] | Hip, knee, ankle | Electric motor | Tendon-sheath artificial muscle | Rigid and soft | 3 + 3 | Assist the elderly and patients with lower-limb diseases | Healthy subject |
| 2016 | XoSoft [64] | Hip knee ankle | Electric motor | Cord | Soft | N/A | Assist the elderly and patients to walk | More than 20 patients (including elderly, stroke patients, etc.). |
| 2015 | Indego [65] | Hip knee | Electric motor | Gear and link | Rigid | 2 + 2 | Assisting patients with spinal cord injury | 16 SCI subjects |
| 2006 | HAL [66] | Hip knee ankle elbows shoulders | Electric motor | Gear and link | Rigid | 5 + 5 | Medical, rescue, load | Healthy subject |
| 2004 | BLEEX [49] | Hip knee | Electric motor | Gear and link | Rigid | 2 + 2 | Enhance the load capacity of the user | Healthy subject |
| Name | Weight (kg) | Cost (dollar) | Battery Life (h) |
|---|---|---|---|
| Rewalk | 23.3 | 77,000 | 2 |
| Indego | 12 | 80,000 | 1.5 |
| Ekso | 23 | 100,000 | 4 |
| Advantage | Disadvantage | Torque Output | Response Time | |
|---|---|---|---|---|
| Lighter in mass | Limited power output | |||
| Cable-driven | Flexible | Less durable | 800 mm/s (Max Speed) [98] | |
| Lower cost | High friction | |||
| Provide strong power support | Requires an air pump, which adds weight. | 4.39 Nm on 21 PSI [99] | 0.22 s [99] | |
| Pneumatic driven | Good dynamic response | The complexity and air tightness requirements are high. | 9.1 Nm on 100 Kpa [100] | 0.5 s [100] |
| Soft and comfortable | Efficient gas management systems are required. | <0.2 s from 0 to 100 Kpa [101] | ||
| Precise control | Higher cost | 120 Nm [102] | 0.001 s [102] | |
| Motor-driven | Technology is mature | Heavier | 17.5 Nm [103] | 0.016 s [103] |
| Support larger payloads | Hard exoskeletons may not be wearable around the clock. | 100 Nm [50] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guo, W.; Katiyar, S.A.; Davis, S.; Nefti-Meziani, S. Overview: A Comprehensive Review of Soft Wearable Rehabilitation and Assistive Devices, with a Focus on the Function, Design and Control of Lower-Limb Exoskeletons. Machines 2025, 13, 1020. https://doi.org/10.3390/machines13111020
Guo W, Katiyar SA, Davis S, Nefti-Meziani S. Overview: A Comprehensive Review of Soft Wearable Rehabilitation and Assistive Devices, with a Focus on the Function, Design and Control of Lower-Limb Exoskeletons. Machines. 2025; 13(11):1020. https://doi.org/10.3390/machines13111020
Chicago/Turabian StyleGuo, Weilin, Shiv Ashutosh Katiyar, Steve Davis, and Samia Nefti-Meziani. 2025. "Overview: A Comprehensive Review of Soft Wearable Rehabilitation and Assistive Devices, with a Focus on the Function, Design and Control of Lower-Limb Exoskeletons" Machines 13, no. 11: 1020. https://doi.org/10.3390/machines13111020
APA StyleGuo, W., Katiyar, S. A., Davis, S., & Nefti-Meziani, S. (2025). Overview: A Comprehensive Review of Soft Wearable Rehabilitation and Assistive Devices, with a Focus on the Function, Design and Control of Lower-Limb Exoskeletons. Machines, 13(11), 1020. https://doi.org/10.3390/machines13111020







