Abstract
Objectives: To evaluate the association between late CVS (placental biopsy, later than 13 weeks of gestations) and complications between sampling and delivery in 8599 cases in the Department of Obstetrics and Gynecology of a private hospital Podobnik, Zagreb, Croatia. Methods: Late chorionic villus sampling under ultrasound guidance was carried out in prospective monocentric cohort study of 7859 (91.4%) cases in the second trimester and 700 (8.6%) cases in the third trimester of pregnancy. Out of 8599 late CVS cases, 1476 (17.2%) were performed because of suspicious ultrasonographic findings. Results: In 43 patients (0.50%), complications were found between sampling and delivery. There were only 12 (0.15%) spontaneous abortions four to six weeks after late CVS (before 28 weeks). We found 190 (2.3%) chromosomal abnormalities. In the group with suspicious ultrasonographic findings, comparing 1476 cases, we found significant oligohydramnios in 375 (25.4%), significant polyhydramnios in 197 (13.3%) and chromosomal abnormalities in 125 (8.5%) cases. Among the 190 patients with chromosomal abnormalities, ultrasonographic findings were detected in 98 (49.2%) after the 22th week of pregnancy. Conclusions: Late CVS is a safe method of invasive prenatal diagnosis with lower spontaneous abortions rate (0.15%). This method, applicable after 13 weeks of gestation, offers a more flexible approach to invasive prenatal diagnosis of chromosome abnormalities, in very specialized fetal-maternal centres for this method.
1. Introduction
The pioneering work of Alvarez [1] demonstrated the possibility of obtaining transabdominal villus sampling from an in situ placenta. Subsequently a variety of methods have been described to villi samples. Hodgal et al. [2] made significant contributions to the feasibility of conducting chromosome studies on the trophoblast. After the reports by Chieri and Aldini [3], Hodgal et al. [2] and Nicolaides et al. [4], we began to offer late chorionic villus sampling to the patients who were late for early chorionic villus sampling and some of those regularly scheduled for amniocentesis to accept the cytogenetic results for three weeks. A rapid karyotype result is of importance when patients who are at an increased risk for fetal chromosome disorders present for prenatal diagnosis near 22 weeks gestation. Similarly, patients who present late in the second trimester with abnormal ultrasound findings or oligohydramnios can be considered candidates for second-trimester chorionic villus sampling due to an increased risk of fetal chromosome abnormalities. The findings may lead to elective termination of pregnancy or in some circumstances vaginal delivery, rather than cesarean The primary aim of this prospective monocentric cohort study was to evaluate the association between invasive prenatal diagnostic procedures and very low spontaneous abortions rate after late CVS. An additional objective was to describe the clinical outcomes of affected pregnancies over a 15-year period at tertiary care centres in the Republic of Croatia.
2. Patients and Methods
Between January 2008 and May 2023, late chorionic villus sampling was performed in a prospective, monocentric, cohort study on 8599 singleton pregnancies from 14–41 weeks of pregnancy. A total of 7799 cases were between 14–28 weeks of pregnancy, and 700 cases were between 29–41 weeks of pregnancy (Figure 1). The indications for tissue sampling are in Table 1. Exclusion criteria involved the detection of embryo death at the first ultrasound, multiple pregnancies, or if they were RH-isoimunized, or untreated cervical infection and cases were offered placental biopsy or amniocentesis for private reasons. Gestational age as determined by the last menstrual period and early ultrasound measurement. Demographic and other perinatal information including obstetrical and genetic history, was collected and extracted from electronic records with standardized reports. The maternal age at sampling from 18–52 years, with 77% of patients over 37. Before sampling, all women underwent accurate clinical and ultrasonic evaluation. When the late CVS was in the second trimester of pregnancy, all women were offered a follow-up ultrasound examination one week after sampling, and again between 16 and 20–22 weeks and 26–28 weeks, when completed and returned the questionnaire about the progress of their pregnancies. When the sampling was in the third trimester of pregnancy, all women were offered a follow-up ultrasound examination one week after sampling and again between 32 and 34 weeks, at 36 weeks and before delivery. The delivery hospitals identified any complications that occurred during pregnancy and delivery, as well as information about the newborn and the placenta. The follow-up of all 8799 patients was completed. Given the variability in outcomes, the management of pregnancies complicated after late CVS should be multidisciplinary, involving fetal medicine specialists, genetic counselors and neonatologists.
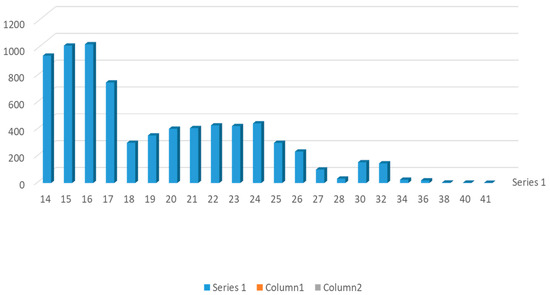
Figure 1.
Number of procedures per week in 8599 patients.

Table 1.
Indication for late CVS in the second and third trimesters of 8599 patients.
The maternal abdomen was prepared with a topical of povidone-iodine, and a sterile drape was placed over it. No local anesthetic was given. Sampling was performed under real-time ultrasonographic guidance using a curvilinear transducer with a frequency of 2.5–5 MHz, protected with a sterile plastic bag. A 20 or 18-gauge spinal needle was introduced through the abdominal maternal wall to the placenta under continuous ultrasound guidance inserted vertically and sometimes obliquely in the placenta. We used a 20-gauge single spinal needle tip for sampling from week 14 to 16 and an 18-gauge needle after week 16. When the echo of the needle was within the placenta, the stylet was removed with a slow movement in the presence of negative pressure, placental tissue was aspirated into a 20 mL syringe containing of culture medium Furthermore, all rhesus-negative women received 50 μg of anti-D administrated after sampling.
Cytogenetic findings [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16] indicated that the sample of villus tissue was immediately transferred a laboratory and examined under a dissecting microscope. An overnight short-term incubation method for three days or a culture method for seven days was used [7,8,11,12,13,14,15,16]. Additionally, fetal heart rate (FHR) was monitored by M-mode in all patients.
Doppler recordings of the uterine artery, the spiral artery, the chorionic artery, the intraplacental arteriole (near the sample place), the umbilical artery, the the ductus venosus, and the middle cerebral artery were performed 10 min prior to sampling and 10 min after procedures in 1300 patients between 14 and 20 weeks [7,8,9,13,14,15,16,17,18,19,20]. Doppler recordings were performed in the same group of patients in which the concentration of maternal serum AFP was measured to evaluate possible fetal vascular damage [6,7,15,16,17,18,19,20]. The study was performed using a GE machine (Voluson E8 and Voluson 10) with a transabdominal probe of 2–5 MHz Once the anatomical position of the investigated area obtained the pulsed wave Doppler sample volume was focused on the structure of interest. The pulsatility index (PI) was calculated automatically, and the mean value was determined. The statistical analysis was carried out using the Student’s t-test and chi-square test. To evaluate statistical significance where applicable, a p-value of <0.05 (two-tailed) was considered statistically significant. Ethical approval was granted by the Ethics Committee of the Podobnik Department of Obstetrics and Gynecology of Zagreb (13 August 2008, No 1–13). Informed consent was obtained from all subjects involved in the study.
3. Results
In 70% of patients the placenta was anterior or fundal, and the success rate of obtaining sample was 99% after the first sampling and 100% after the second sampling. In 30% of patients, the placenta was posterior, and the success rate of obtaining was 98% after the first sampling and 100% after the second sampling. In 35 (0.4%) patients, we found early complications between sampling and delivery (Table 2). Lower back pain and uterine contraction were found in 12 (0.15%) cases in the second trimester of pregnancy and 3 (0.4%) cases in the third trimester of pregnancy. Fever was found in three (0.3%) cases, but no instances of chorioamnionitis developed. There were only 12 (0.15%) spontaneous abortions after late chorionic villus sampling, four to six weeks later. All women were older than 37 years, chorionic villus sampling was carried out in the 14th to 18th weeks and spontaneous abortions after sampling were carried out in the 17th and 24th weeks. Another six women had late chorionic villus sampling after 18th weeks and spontaneous abortions in the 24th week (karyotype was trisomy 21 in four and trisomy 18 in two women, but the parents declined elective abortion). In all 12 women the amount of tissue was between 30 and 50 mg.

Table 2.
Pregnancy outcome after late CVS in 8599 patients.
The concentration of total mean AFP) levels increased after sampling in 25 (0.5%) patients from 500 patients in whom serum samples were obtained before and after sampling. Ten of them were spontaneous abortions after sampling, and all ten had chromosomal aberrations. However, no correlation was found between AFP elevation, placental hematoma and fever after sampling.
Cytogenetic findings were obtained in 8599 (99.9%) placental samples. In 10 cases, metaphases were unsuitable for study. The over-night direct method was utilized in 60.0%, culture in 20.9%, and culture and over-night technique in 19.1% of the same group of patients (Table 3). We found chromosomal aberration in 190 (2.2%): trisomy 21 (68 cases), trisomy 18 (35 cases), trisomy 16 (6 cases), trisomy 13 (33 cases), monosomy X (27 cases), 46XXY (21 cases) and in 25 (0.3%) patient mosaicisms were found. These mosaicisms were confirmed (in 15 cases) or not confirmed (in 10 cases) in fetal blood sampling by cordocentesis. The total fetal loss in all cases was 150 (1.8%), in 57 (8.1%) women in whom late chorionic villus sampling was performed in the second trimester of pregnancy and 5 (0.5%) in women in whom late chorionic villus sampling was performed in the third trimester of pregnancy. In the group with suspicious ultrasonographic findings, comprising 1476 cases, we found significant oligohydramnios in 375 (25.4%), significant polyhydramnios in 197 (13.3%) and chromosomal abnormalities in 125 (8.5%) cases (Table 4). Among the 60 patients with chromosomal abnormalities, ultrasonographic findings were detected in 10 (16.7%) after the twentieth week of pregnancy. In all 10 cases, the obstetric management was changed of abnormal cytogenetic results and abnormal ultrasonographic findings. Five of those had an elective abortion, three fetuses with ultrasonographic abnormalities and oligohydramnios detected between 28 and 32 weeks were stillborn, and two had an early neonatal death. The concurrent fetal abnormalities detected in this study expectedly resulted in a higher proportion of total fetal loss. We did not see any serious limb abnormalities after late chorionic villus sampling.

Table 3.
Cytogenetic techniques performed.

Table 4.
Cytogenetic aberration found in pregnancies with suspicious ultrasound findings.
Color Doppler was used to investigate the uteroplacental and fetal vessels in 1300 (30.0%) pregnancies between 14 and 20 weeks of gestation (Table 5). The main uterine artery, the spiral arteries, the umbilical artery, the chorionic artery, the intraplacental arteriole (near the sample place), the ductus venosus, and the middle cerebral artery were investigated. There were no significant differences in mean pulsatility indices (PISs) between maternal and fetal circulation before and after sampling. The preliminary data of 50 trisomic fetuses (forty trisomy 21, five trisomy 18 and five trisomy 13) have abnormally increased umbilical PIs in the umbilical artery and ductus venosus and abnormally decreased PIs in the middle cerebral artery (Table 6).

Table 5.
Pulsatility indices (PIs) values for maternal and fetal circulation before and after CVS.

Table 6.
Pulsatility indices (PIs) values in maternal and fetal circulation before and after late CVS in fetuses with chromosome abnormalities.
4. Discussion
In our study there were only 12 (0.15%) spontaneous abortions after late CVS sampling. There were no spontaneous abortions after sampling in the latest 1000 pregnancies with cytogenetically and sonographically normal fetuses, to allow meaningful conclusions about the safety of the procedure. In comparison Holzgreve et al. [8,9] report a loss rate of 2.3% in 728 pregnancies from 24 centres after late CVS sampling. Smidt-Jensen et al. [21] reported one (0.7%) fetal loss in a group of 139 sonographically and cytogenetically normal fetuses 20 weeks after sampling. In our group the spontaneous abortion rate after late CVS sampling is low and compatible with mh Smit-Jensen et al. and Jahoda et al. [22] studies. Our study showed a decrease in the fetal loss rate with advancing gestational age and the relationship between fetal loss and maternal age. In younger women this rate was not influenced by gestational age. Holzgreve et al. [8,9] found as many as 20% of chromosomal aberrations in cases with sonographic abnormalities. Chromosomal aberrations have been seen in as many as 32% of fetuses with an abnormal fetal echography, compatible with 33.3% in our series. Among the 60 patients with suspicious ultrasound findings or intrauterine growth retardation detected after the twenty weeks of pregnancy, 10 (16.7%) fetuses had chromosomal abnormalities. We did not find a correlation between AFP elevation, placental hematoma, Doppler measurements, and spontaneous abortion rate after late chorionic villus sampling. Our results are in agreement with previous studies in which a marked rise in AFP after early and late CVS was not associated with fetal demise. The risk of spontaneous abortion after the second trimester transabdominal chorionic villus sampling is 0.4% to 3.2% [5,6,7,8,9,10,12,16,17,21,23,24,25,26,27,28,29,30,31,32,33,34]. In our study, there were only 12 (0.15%) spontaneous abortion after sampling. Chromosomal aberrations have been seen in as many as 32% of fetuses with an abnormal fetal echography, compatible with 33.3% in our series. Among the 60 patients with suspicious ultrasound findings or intrauterine growth retardation detected after the twenty weeks of pregnancy, 10 (16.7%) fetuses had chromosomal abnormalities. In all 10 of these cases, the obstetric management was changed because of abnormal cytogenetic results. The primary aim of this prospective monocentric cohort study was to evaluate the association between invasive prenatal diagnostic procedures (late CVS) and very lower spontaneous abortions rate after late CVS, in our cases in 0.15%, The problem while late CVS don’t change classical amniocentesis after 15 weeks of gestations, were in cytogenetic laboratories which done not briefly short technique for three days or culture methods for seven days. That is the reason why our study was larger in the world. On this day there were only 15.000 late CVS, and we had lower complications after late CVS procedures in 8599 cases.
In our laboratory, more than 5 mg of placental tissue was needed to perform the cytogenetic studies [12,18,22,27,28,29,35,36], The mitotic index on placental villi decreased with increasing gestational age: Saura et al. [5] reported a result at 35 weeks, Nicolaides et al. [4] reported results at 37 weeks and in our hands 41 weeks gestation seems to be limited, to approximately one metaphase on the 500 cells [12,16]. Many cytogenetic laboratories need approximately 30–50 mg of placental tissue and this massive sampling is a reason way had spontaneous abortion after late CVS in 1–3.2% patients. That was a reason why late CVS don’t change classical amniocentesis after 15 weeks of gestation. Mosaicisms are considered to occur with a frequency of approximately 1–2%, with confirmation not typically occurring in most patients [3,4,6,7,10,12,16,17,24,25,27,28,29,30,31,32,33,34,36,37,38,39,40,41]. In our study we found mosaicisms in 0.3% of cases. These mosaicisms were confirmed (in 15 cases) or not confirmed (in 10 cases from fetal blood sampling by cordocentesis [12,18,21,22,27,28,35,36,42].
We did not find a correlation between AFP elevation, placental hematoma, Doppler measurements and spontaneous abortion late chorionic villus sampling. Therefore, the amount of fetomaternal bleeding in the second and third trimester may be in the same range as in the first trimester. Our results are in agreement with previous studies in which a marked rise in AFP after early and late CVS was not associated with fetal demise [12,20,21,25,27,28,29,30,36].
To evaluate possible fetal vascular damage, we assessed fetal and maternal circulation using color Doppler and measured AFP in maternal serum. There were no significant differences in mean pulsatility indices between maternal and fetal circulation before and after late chorionic villus sampling. This suggested that uteroplacental and fetal blood flow were also not affected by placental biopsy procedures and the subsequent fetal loss rate was not the result of pathological alterations in uteroplacental and fetal vasculature. Given the variability in outcomes, the management of pregnancies complicated by fetal structural abnormalities should be multidisciplinary, involving fetal medicine specialists, genetic counsellors and neonatologists.
Late CVS applicable after 13 weeks of gestation, offers a more flexible approach to invasive prenatal diagnosis of chromosome abnormalities, in very specialized fetal-maternal centres for this method.
Author Contributions
Conceptualization: P.P., M.P. and I.B.-Z. made substantial contributions to the conception of the work, drafting the work, and revising it critically for important intellectual content and its final approval; I.L., K.K., D.J. and Z.S. enrolled patients, acquired clinical data, and made substantial contributions to analysis and data interpretation; Z.S. and I.L. made substantial contributions to data interpretation, critical revision of the article, the analysis and interpretation of data. P.P., M.P. and I.B.-Z. contributed to the interpretation of data and the revision of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
The research did not receive external funding.
Institutional Review Board Statement
Ethical approval was granted by the Ethics Committee of the Podobnik Department of Obstetrics and Gynecology of Zagreb (13 August 2008, No 1–13).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available from the corresponding author on request.
Acknowledgments
We thank the patients and families for their cooperation. The authors wish to acknowledge all the research staff and participants involved in this study.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- Alvarez, H. Diagnosis of hydatiform mole by transabdominal placental biopsy. Am. J. Obstet. Gynecol. 1960, 96, 38–41. [Google Scholar]
- Buijtendijk, M.F.; Bet, B.B.; Leeflang, M.M.; Shah, H.; Reuvekamp, T.; Goring, T.; Docter, D.; Timmerman, M.G.; Dawood, Y.; Lugthart, M.A.; et al. Diagnostic accuracy of ultrasound screening for fetal structural abnormalities during the first and second trimester of pregnancy in low-risk and unselected populations. Cochrane Database Syst. Rev. 2024, 5, CD014715. [Google Scholar] [CrossRef] [PubMed]
- Fryburg, J.S.; Dimaio, M.S.; Yang-Feng, L.; Mahoney, J. Follow-up of pregnancies complicated by placental mosaicism diagnosed by chorionic villus sampling. Prenat. Diagn. 1993, 13, 481–494. [Google Scholar] [CrossRef] [PubMed]
- Beta, J.; Zhang, W.; Geris, S.; Kostiv, S.; Kolekar, R. Procedure-related risk of miscarriage following chorionic villus sampling and amniocentesis. Ultrasound Obstet. Gynecol. 2019, 54, 452–457. [Google Scholar] [CrossRef] [PubMed]
- Hodgdal, C.K.; Doran, T.A.; Shime, J.; Wilson, S.; Teshima, I. Transabdominal chorionic villus sampling in the second trimester. Am. J. Obstet. Gyne. 1968, 158, 345–349. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Yang, F.; Chang, Q.; Jia, B.; Xu, Y.; Wu, R.; Li, L.; Chen, W.; Yin, A.; Huang, F.; et al. Positive predictive value estimates for noninvasive prenatal testing from data of a prenatal diagnosis laboratory and literature review. Mol. Cytogenet. 2022, 15, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Holzgreve, W.; Miny, O.; Gerlach, B.; Westendrop, A.; Ahlert, D.; Horst, J. Benefits of placental biopsies for rapid karyotyping in the second and third trimester (late chorionic villus sampling) in high-risk pregnancies. Am. J. Obstet. Gynecol. 1990, 162, 1188–1192. [Google Scholar] [CrossRef] [PubMed]
- Holzgreve, W.; Miny, P.; Schloo, R. “Late CVS” international registry compilation of data from 24 centres. Prenat. Daign. 1990, 10, 59–167. [Google Scholar] [CrossRef] [PubMed]
- Philip, J.; Silver, R.K.; Wilson, R.; Thom, E.A.; Zachary, J.M.; Mohide, P. Late first-trimester invasive prenatal diagnosis: Results of an international randomized trial. Obstet. Gynecol. 2004, 103, 1164–1173. [Google Scholar] [CrossRef] [PubMed]
- Pijepers, L.; Jahoda, M.G.J.; Reuss, A.; Wladimiroff, W.J.; Sach, E.S. Transabdominal chorionic villus sampling in the second and third trimester of pregnancy to determine fetal karyotype. Br. Med. J. 1988, 297, 822–823. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.P.; Young, I.D. Second trimester chorionic villus biopsy. Lancet 1986, 1, 969–972. [Google Scholar] [CrossRef]
- Constantine, G.; Fowlie, A.; Pearson, J. Placental biopsy in the third trimester of pregancy. Prenat. Diagn. 1992, 12, 783–788. [Google Scholar] [CrossRef] [PubMed]
- Moni, G.; Juculano, A.R. ISOUOG Practice guidelines invasive procedures for prenatal diagnosis. Ultrasound Obstet. Gynecol. 2017, 49, 414–415. [Google Scholar]
- Daffos, F.; Capella-Pavlosky, M.; Forstier, F. A new procedure for fetal blood sampling in utero: Preliminary results of fifty-three cases. Am. J. Obstet. Gynecol. 1983, 146, 985–988. [Google Scholar] [CrossRef] [PubMed]
- Dalpra, L.; Nocera, G.; Tibiletti, M.G.; Martinoli, E.; Oldrini, A.; Agosti, S. “Late” chorionic villus sampling:cytogenetic aspects. Prenat. Diagn. 1993, 13, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Salsi, G.; Grati, F.R.; Bellussi, F.; Pompilii, E.; Maggi, F.; Simoni, G.; D’Ambrosi, F.; Orsi, M.; Gentile, M.; Rembouskos, G.; et al. Risk of fetal loss in pregnancies undergoing midtrimester amniocentesis after inonclusive chorionic villus sampling. Fetal. Diagn. Ther. 2019, 46, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Hackett, G.A.; Smith, J.H.; Rebello, M.T.; Gray, C.T.H.; Rooney, D.E.; Beard, R.W.; Loeffler, F.E.; Coleman, D.V. Early amniocentesis at 11–14 weeks gestation for the diagnosis of fetal chromosomal abnormality, a clinical evaluation. Prenat. Diagn. 1991, 11, 311–315. [Google Scholar] [CrossRef] [PubMed]
- Podobnik, M.; Ciglar, S.; Singer, Z.; Gebauer, B.; Podgajski, M. Doppler assessment of fetal circulation during late chorionic villus sampling in high risk pregnancies. Prenat. Neonatal Med. 1998, 3 (Suppl. S1), 9. [Google Scholar]
- Los, F.J.; Beekhuis, J.R.; Marrink, J.; Hagenaars, A.M.; Reuss, A.; Wladimiroff, J.W. Origin of raised maternal serum alpha-fetoprotein leveles in second-trimester oligohydramnios. Prenat. Diagn. 1992, 12, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Gosden, C.; Nicolaides, K.H.; Rodek, C.H. Fetal blood sampling in investigation of chromosome mosaicism in amniotic fluid cell culture. Lancet 1988, 1, 613–617. [Google Scholar] [CrossRef] [PubMed]
- Odibo, A.O.; Gray, D.L.; Dicke, J.M.; Stamilio, D.M.; Macones, G.A.; Crane, J.P. Revisiting the Fetal Loss Rate After Second-Trimester Genetic Amniocentesis: A single center’s 16-year experience. Obstet. Gynecol. 2008, 11, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Overbeek, T.E.; Hop, W.C.J.; Den Ouden, M.; Pijpers, L.; Jahoda, M.G.J.; Wladimiroff, J.W. Spontaneous abortion rate and advanced maternal age:consequences for prenatal diagnosis. Lancet 1990, 336, 27–29. [Google Scholar] [CrossRef] [PubMed]
- Chieri, P.R.; Aldini, A.J.R. Feasibility of placental biopsy in the second trimester for fetal diagnosis. Am. J. Obstet. Gynecol. 1989, 160, 581–583. [Google Scholar] [CrossRef] [PubMed]
- Alfirevic, Z.; Navaratnam, K.; Mujezinovic, F. Amniocentesis and chorionic villus sampling for prenatal diagnosis. Cochrane Database Syst. Rev. 2017, 9, CD003252. [Google Scholar] [CrossRef] [PubMed]
- Bakker, M.; Birnie, E.; Robles de Medina, P.; Sollie, K.M.; Pajkrt, E.; Bilardo, C.M. Total pregnancy loss after chorionic villus sampling and amniocentesis: A cohort study. Ultrasound Obstet. Gynecol. 2017, 49, 599–606. [Google Scholar]
- Podobnik, M.; Ciglar, S.; Singer, Z.; Podobnik-Šarkanji, S.; Duic, Z.; Skalak, D. Transabdominal chorionic villus sampling in the second and third trimester of hihg-risk pregnancies. Prenat. Diagn. 1997, 17, 125–133. [Google Scholar] [CrossRef]
- Basarn, S.; Pawlowitzki, I.H.; Horst, J.; Holzgreve, W. Rapid karyotiping for prenatal diagnosis in the second and third trimester of pregnancy. Prenat. Diagn. 1988, 8, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Beta, J.; Lesmes-Heredia, C.; Bedeti, C.; Alolekar, R. Risk of miscarriage folowing amniocentesis of chorion villus sampling: A systematic review of literature. Minerva Gynecol. 2018, 20, 215–219. [Google Scholar]
- Saura, A.; Longy, M.; Horovitz, J.; Vergnaud, A.; Grison, O. Direct chromosome analysis in the second and third trimesters by placental biopsy in 30 pregnancies. Br. J. Obstet. Gynecol. 1989, 96, 1215–1218. [Google Scholar] [CrossRef] [PubMed]
- Jahoda, M.G.J.; Brandenburg, H.; Reuss, A.; Cohen-Overbeek, T.E.; Wladimiroff, J.W.; Los, F.J.; Sachs, E.S. Transcervical (TC) and transabdominal(TA) CVS for prenatal diagnosis in Roterdam:expirience with 3611 cases. Prenat. Diagn. 1991, 11, 559–561. [Google Scholar] [CrossRef] [PubMed]
- Ledbetter, D.H.; Martin, H.O.; Verlinsky, Y. Citogenetic results of chorionic villus sampling: High success rate and diagnostic accuracy in the United States collaborative study. Am. J. Obstet. Gynecol. 1990, 162, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Wolstenholme, J.; Hoogwrf, A.M.; Sherdian, H.; Maher, E.J.; Little, D.J. Practical experience using transabdominal chorionic villus biopsies taken after 16 weeks gestation for rapid prenatal diagnosis of chromosomal abnormalities. Prenat. Diagn. 1989, 9, 357–359. [Google Scholar] [CrossRef] [PubMed]
- Salomon, L.J.; Sotiriadis, A.; Wulff, C.B.; Odibo, A.; Alolekar, R. Risk of miscarriage following amniocentesis or chorionic villus saqmpling:Systematic review of literature and updated meta analysis. Ultrasound Obstet. Gynecol. 2019, 54, 442–451. [Google Scholar] [CrossRef] [PubMed]
- Smidt-Jensen, S.; Lundsten, C.; Lind, A.M.; Dinesen, K.; Philip, J. Transabdominal chrionic villus sampling in the second and third trimester of pregnancy:chromosome quality, reporting time, and feto-maternal bleeding. Prenat Diagn. 1993, 13, 957–969. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A.; Wapner, R.; Davis, G.H.; Jackson, L.G. Mosaicism in chorionic villus sampling: An association with poor perinatal outcome. Obstet. Gynecol. 1990, 75, 573–577. [Google Scholar] [PubMed]
- McCormack, M.J.; Mackenzie, W.E.; Rushton, D.I.; Newton, J.R. Clinical and patological factors in spontaneous abortion following chorionic villus sampling. Prenat. Diagn. 1991, 11, 841–846. [Google Scholar] [CrossRef] [PubMed]
- Nicolaides, K.; Soothil, P.W.; Rodeck, C.H.; Waren, R.C.; Gosden, C.M. Why confine chorionic villus (placental) biopsy to the first trimester. Lancet 1986, 1, 543–544. [Google Scholar] [CrossRef] [PubMed]
- Akolekar, R.; Beta, J.; Picciarelli, G.; Ogilvie, C.; D’Antonio, F. Procedure-related risk of miscarriage following amniocentesis and chorionic villus sampling: A systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2014, 45, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Ammala, P.; Hiilesma, K.; Liukkonen, S.; Saisto, T.; Teramo, K.; Koskull, H. Randomized trial comparing first-trimester transcervical chorionic villus sampling and second-trimester amniocentesis. Prenat. Diagn. 1993, 13, 919–927. [Google Scholar] [CrossRef] [PubMed]
- Reilly, K.; Doyle, S.; Hamilton, K.; Susan, S.; Kulby, M.; Mone, F. Pitfalls of prenatal diagnosis associated with mosaicism. Obstet. Gynecol. 2022, 25, 28–37. [Google Scholar] [CrossRef]
- Jauniaux, E.; Campbell, S. Antenatal diagnosis of placental infarctus by ultrasonography. J. Clin. Ultrasound. 1991, 19, 58–61. [Google Scholar] [CrossRef] [PubMed]
- Ganshirt-Ahlert, D.; Pohlishmidt, M.; Gal, A.; Horst, J.; Miny, P.; Holzgreve, W. Transabdominal placental biopsy in the second and thirdtrimester of pregnancy: What is the risk of maternal contamination in DNA diagnosis. Obstet. Gynecol. 1990, 75, 320–323. [Google Scholar] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).