Abstract
Hereditary prostate cancer (HPCa) has the highest heritability of any cancer in men. Interestingly, it occurs in several hereditary syndromes, including breast and ovarian cancer (HBOC) and Lynch syndrome (LS). Several gene mutations related to these syndromes have been identified as biomarkers in HPCa. The goal of this study was to screen for germline mutations in susceptibility genes by using a multigene panel, and to subsequently correlate the results with clinical and laboratory parameters. This was undertaken in 180 HBOC families, which included 217 males with prostate cancer (PCa). Mutational analysis was further extended to 104 family members of mutated patients. Screening of HBOC families revealed that 30.5% harbored germline mutations in susceptibility genes, with 21.6% harboring pathogenic variants (PVs) and 8.9% having variants of uncertain significance (VUS). We found PVs at similar frequency in BRCA1 and BRCA2 genes (8.8% and 9.4%, respectively), while 0.56% of PVs were present in well-established susceptibility genes PALB2, TP53 and RAD51C. Moreover, 0.56% of monoallelic PVs were present in MUTYH, a gene whose function in tumorigenesis in the context of PCa is still unclear. Finally, we reported double heterozygosity (DH) in BRCA1/2 genes in a single family, and found double mutation (DM) present in BRCA2 in a separate family. There was no significant difference between the mean age of onset of PCa in HBOC families with or without germline mutations in susceptibility genes, while the mean survival was highest in mutated patients compared to wild type. Furthermore, PCa is the second most recurrent cancer in our cohort, resulting in 18% of cases in both mutated and non-mutated families. Our investigation shows that PVs were located mostly in the 3′ of BRCA1 and BRCA2 genes, and in BRCA2, most PVs fell in exon 11, suggesting a mutation cluster region relating to risk of HPCa. A total of 65 family members inherited the proband’s mutation; of these, 24 developed cancer, with 41 remaining unaffected.
1. Introduction
Prostate cancer (PCa) is a heterogeneous disease, representing one of the major causes of malignancy-related deaths worldwide, with about 1,600,000 cases and 366,000 deaths annually [1]. Men with first-degree male relatives affected by PCa have at least a two-fold risk of developing PCa compared to men without a family history of PCa [2]. Approximately 5–15% of PCa cases are attributable to hereditary factors [3]. Hereditary prostate cancer (HPCa) has the highest heritability of any cancer in men, with tumorigenesis occurring due to the presence of germline mutations transmitted through autosomal dominant inheritance [4]. In comparison to sporadic cases, HPCa shows an early age of onset, an aggressive disease progression and locally advanced stage, with a higher risk of recurrence after surgery.
HPCa arises in several hereditary syndromes, including hereditary breast and ovarian cancer (HBOC) and Lynch syndrome (LS) [5]. Several genes related to these syndromes, such as DNA damage repair (DDR) genes BRCA1, BRCA2, CHEK2, ATM and PALB2, and DNA mismatch repair (MMR) genes MLH1, MSH2, MSH6 and PMS2, were identified as biomarkers in HPCa. However, mutations in HOXB13, BRP1, NBS1, RAD51C, RAD51D and TP53 genes have been found to confer an increased risk of HPCa [6,7,8,9].
The mutation status of genes involved in HPCa could have potential clinical applications, particularly for the stratification of patients into specific treatment and prognostic groups. Patients who harbor mutations in DDR genes, for example, would likely be more sensitive to a treatment regime that includes PARP inhibitors, whereas the mutational status of MMR genes in metastatic patients could predict their response to immunotherapy [10].
Current guidelines do not adequately inform at what disease stage genetic testing should be performed to identify germline mutations in patients who could potentially benefit from alternative treatment. Moreover, the identification of germline mutations in a patient with HPCa could facilitate the genetic testing of family members at risk of HPCa or other associated cancers.
The goal of the study was to identify germline mutations insusceptibility genes using a multigene panel in HBOC Italian families with at least one case of PCa by correlating clinical and laboratory parameters. Mutational analysis was extended to family members of the mutated patients.
2. Materials and Methods
2.1. Patients
This study was carried out in accordance with the World Medical Association Helsinki Declaration (1964). Informed consent was obtained from all subjects, and the study was approved and conducted according to the ethical guidelines of the University of Campania “Luigi Vanvitelli” (n.469-23/07/2019). The study was conducted at the U.O.C. Clinical and Molecular Pathology, A.O.U. University of Campania “Luigi Vanvitelli”.
We enrolled180 HBOC families that included 217 males with PCa. The probands were affected with prostate, breast, ovarian, colorectal, pancreatic, endometrial, bladder, gastric cancer, or melanoma (Table 1), with an age range of 28–86 years. All selected patients received genetic counselling. Case and family history were collected, and a pedigree was generated for each family. The patients were selected according to the criteria for HBOC syndrome [11], in which mutations occur in high-penetrance BRCA1/2 genes, followed by PALB2, and mutations in genes that confer moderate penetrance risk, such as ATM, CHEK2, RAD51C, RAD50, BRIP1, PTEN, NBN, MRE11A, BARD1, STK11, CDH1, MUTYH and TP53. Peripheral blood samples were collected in two test EDTA tubes from all patients. Mutational analysis was extended to 104 family members of 34 mutated patients.

Table 1.
Number and tumor type of HBOC probands.
2.2. Mutational Analysis
Genomic DNA from blood samples was extracted using the Wizard Genomic DNA purification kit (Promega Corporation, Madison, WI, USA) according to the manufacturer’s instructions.
For mutational analysis, we used the TruSight Sequencing Cancer Panel on a MiSeq platform (Illumina, HCS, Sophia Genetics, Switzerland) that analyzes 16 genes, BRCA1 (NM_007295), BRCA2 (NM_000059), ATM (NM_000051.4), CHEK2 (NM_007194), PALB2 (NM_024675), RAD51C (NM_058216), RAD50 (NM_002878), BRP1 (NM_001003694.2), PTEN (NM_000314.8), NBN (NM_002485), MRE11A (NM_005591.4), BARD1 (NM_000465.4), STK11 (NM_000455.5), CDH1 (NM_004360), MUTYH (NM_001128425.1) and TP53 (NM 000546). The presence of point mutation was confirmed on the other blood sample by Sanger sequencing, as previously described [12]. Molecular analysis in family members of mutated probands was performed by Sanger sequencing, as previously described [13,14]. The results were analyzed using Mutation Surveyor® software, version 3.24 (Softgenetics, State College, PA, USA).
2.3. Genetic Variant Classification
ClinVar and LOVD databases were used for the identification and classification of genetic variants. Genetic variants found were categorized according to criteria developed by International Agency for Research on Cancer recommendations [15] and categorized into five classes: benign (class I), likely benign (class II), variant of uncertain significance (VUS, class III), likely pathogenic (class IV) and pathogenic variants (PVs, class V).
3. Results
Mutational screening conducted in 180 HBOC families revealed 55 (30.5%) germline mutations in 51 patients. These mutations included 39/180 (21.6%) PV and 16/180 (8.9%) VUS (Figure 1). Moreover, 20/39 (51.3%) of the observed PVs were frameshift, 6/39 (15.4%) intronic variants, 6/39 (15.4%) nonsense, 6/39 (15.4%) missense and 1/39 (2.5%) copy number variation (CNV).
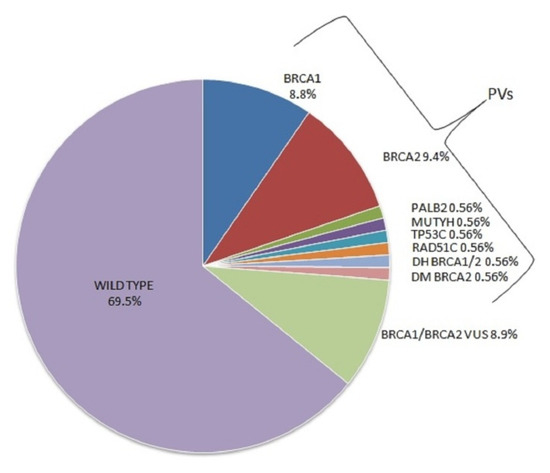
Figure 1.
Pathogenic variants and VUS found in HBOC families.
3.1. Mutations in DNA Damage Repair Genes
From the families carrying PVs, 16/180 (8.8%) harbored a PV in BRCA1, 17/180 (9.4%) in BRCA2, 1/180 (0.56%) in PALB2,1/180 (0.56%) in TP53 and 1/180 (0.56%) in RAD51C. We also observed double heterozygosity (DH) in BRCA1/2 genes (0.56%) in a single family, and found double mutations (DM) present in BRCA2 (0.56%) in a separate family (Figure 1).
The BRCA1 mutation c.5123C>A(p.Ala1708Glu) was found in three separate families and c.5266dupC (p.Gln1756Profs) in four families; the BRCA2 mutation c.4133_4136del (p.Thr1378fs) was observed in two families and c.6468_6469delTC (p.Gln2157Ilefs) in three families.
3.2. Mutations in Base Excision Repair Gene
In the families with observed PVs, 1/180 (0.56%) carried a monoallelic PV in the MUTYH gene (Figure 1). This specific mutation consists of a frameshift deletion in exon 14 of the gene (between nucleotides 1437 and 1439), resulting in the introduction of a premature stop codon at amino acid position 480.It was identified in an 85-year-old woman diagnosed with breast cancer at the age of 65. Figure 2 reports the pedigree analysis of the proband; her brother, affected with prostate cancer, inherited the mutation. In addition, the mutational analysis was extended to the daughter, who was diagnosed with endometrial cancer at 55 years of age, and to the unaffected son of 58 years, revealing that the mutation was also present in both the daughter and son.
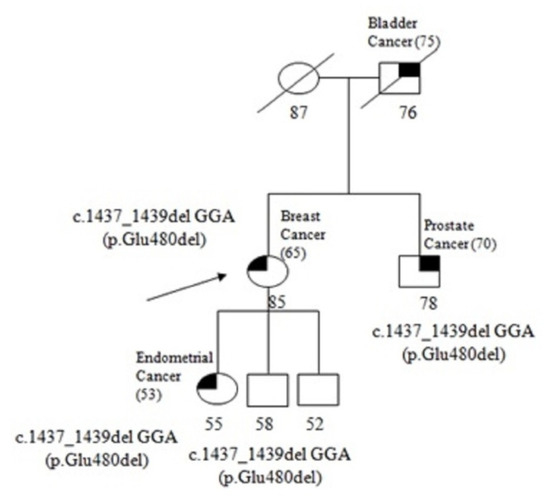
Figure 2.
Pedigree of the proband carrying the monoallelic MUTYH mutation c.1437_1439del GGA (p.Glu480del). The ages at diagnosis are indicated in brackets.
3.3. Genotype–Phenotype Correlation
We observed a mean age of PCa onset of 67.4 years in mutated patients and 68.3 years in non-mutated patients. Of the 217 cases in the cohort, 66 patients died. The mean survival was 8 years and was higher in mutated patients (77.5 years) than in non-mutated patients (74.1 years). Patients who were carriers of VUS were included in the non-mutated patient group (Figure 3).
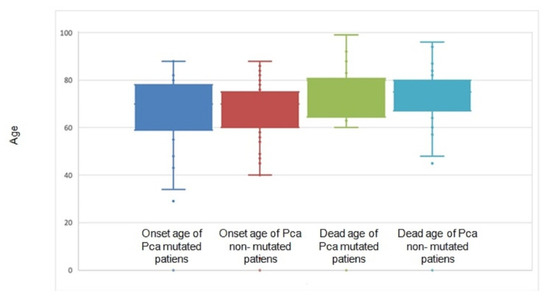
Figure 3.
Onset age of 217 PCa patients. HBOC-mutated families included 49 individuals, and non-mutated families 168 individuals. Age of death of 66 PCa patients is also illustrated in this plot.
The number and percentage of cancer types that occur in mutated and non-mutated HBOC families are shown in Figure 4. PCa is the second most recurrent cancer, resulting in 18% of cases in both mutated and non-mutated families.
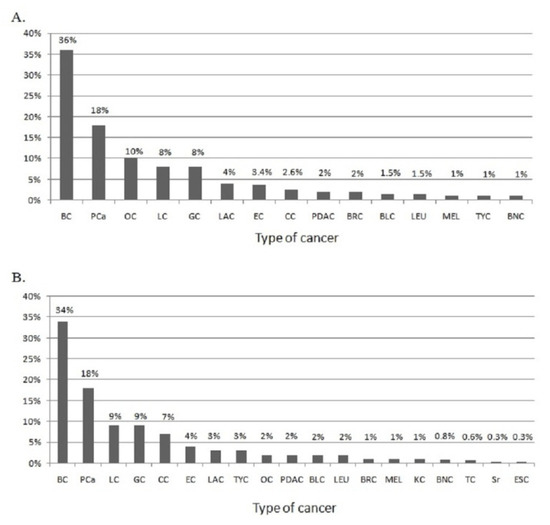
Figure 4.
(A) Cancer types that occur in HBOC-mutated families. (B) Cancer types that occur in HBOC non-mutated families. BC: breast cancer; PCa: prostate cancer; OC: ovarian cancer; LC: lung cancer; GC: gastric cancer; EC: endometrial cancer; LAC: laryngeal cancer; CC: colon cancer; PDAC: pancreatic ductal adenocarcinoma; BRC: brain cancer; BLC: bladder cancer; LEU: leukemia; MEL: melanoma; TYC: thyroid cancer; BNC: bone cancer; KC: kidney cancer; TC: testicular cancer; Sr: sarcoma; ESC: esophageal cancer.
Figure 5 illustrates the location of PVs identified in our cohort in both the BRCA1 and BRCA2 genes. In both genes, the mutations are located throughout the length of gene, mostly in 3′. In BRCA2, most of them fall in exon 11.

Figure 5.
Pathogenic variants found in HBOC families with PCa localized through BRCA1 and BRCA2 genes.
Mutational analysis was extended to 104 family members of 30 proband patients harboring mutations in BRCA1 and/or BRCA2 genes and four proband patients who were carriers of mutations in TP53, PALB2, RAD51C or MUTYH genes. This included both cancer-free family members and family members who were diagnosed with cancer. In the remaining eight families with BRCA mutations, it was not possible to extend the mutational analysis to family members. The results of the genetic testing are summarized in Table 2. A total of 39 family members only displayed the wild-type gene, while 65 had inherited the proband’s mutation. Moreover, 24 of the 65 individuals who inherited the mutations of the proband developed cancer. The analysis was also conducted in families with DH and DM, showing that these pathogenic variants co-segregate.

Table 2.
Results of mutational analysis conducted in family members of 34HBOC-mutated patients, with all pathogenic variants identified. The names of mutations are reported in bold.
4. Discussion
The main findings of the present study are as follows. (1) This is one of the few studies focused on Italian patients with hereditary prostate cancer; we have shown pathogenic germline mutations in five susceptibility genes and a monoallelic frameshift mutation in MUTYH, a potentially pathogenic monoallelic mutation whose significance in PCa has not been established. (2) The mutational frequency between BRCA1 and BRCA2 genes was similar, and higher than previously reported. (3) We observed frequent PVs in the 3′ of both BRCA1 and BRCA2, and a large number of PVs in BRCA2 were present in exon 11 of the gene, suggesting a mutation cluster region relating to risk of HPCa. (4) MUTYH could be related to overall HPCa risk. (5) The mean age of onset in PCa cases that recur in HBOC families was no different in mutated PCa patients versus non-mutated, while the mean survival was highest in mutated patients compared to wild type. (6) PCa is the second most recurrent cancer from our cohort, resulting in 18% of cases in both mutated and non-mutated families.
We identified mutations in 21.6% of HBOC families; mutations in BRCA1 and BRCA2 were found at similar frequency in our cohort. The percentage of mutations found is higher than reported in previous studies that have previously demonstrated that most mutations present were primarily in BRCA2, 1.2–5.3%, while BRCA1 mutations were found in 0.9–1.25% of HPCa patients [16,17,18,19,20,21,22,23,24,25,26]. The difference in mutation prevalence could be influenced by the selection of the patients included; indeed, studies including only HPCa patients report a lower mutation rate than studies including HPCa families. We also identified a family that had DM in both BRCA1 and BRCA2 genes, with a separate family harboring two mutations in BRCA2. These pathogenic variants co-segregate and do not generate a worse phenotype than a single mutation [27].
Patients who were carriers of genes with VUS, where the variants were not classified as either benign or pathogenic, were difficult to interpret in terms of clinical management. The evaluation of their pathogenic significance needs to be corroborated by further experimental evidence. Co-segregation analysis and in silico analysis may be helpful to improve VUS classification [28,29].
Previous studies proposed that mutations in BRCA2 exon 11 were closely related to breast/ovarian cancer risk and aggressiveness [30]. Patel et al. hypothesized that the region between c.7914 and 3’ of the BRCA2 gene is a cluster region associated with an increased risk of developing prostate cancer [31]; however, only one of the mutations found in our patients falls in that region. In the present study, most of the PVs fell in the 3′ of both BRCA1 and in BRCA2 genes and in exon 11 of BRCA2 gene, suggesting a mutation cluster region relating to risk of HPCa. Additional research is expected to confirm this association.
PVs in low-penetrance genes, PALB2, RAD51C and TP53, are present in 0.56% of families. This is in line with previously published studies indicating mutations in other genes in about 0.1–0.2% of cases [19,32]. Despite the rarity of reported PALB2 alterations, recent findings have supported an increasing role of PALB2 in PCa, particularly in metastatic cases [33]. TP53 genetic alterations were reported in 3–12.5% of cases which were considered late events and associated with metastatic castrate-resistant prostate cancer (mCRPC) [34]; however, other studies reported an inactivation of TP53 at a high frequency in primary as well as metastatic castration-naïve PCa [35].
Biallelic MUTYH mutations have been linked to MUTYH-associated polyposis syndrome (MAP). In the past few years, monoallelic MUTYH PVs have been found in patients with gastric, liver, endometrial, breast, ovarian and pancreatic cancer [36,37], and this has led to several studies investigating the impact of germline monoallelic MUTYH PVs in tumorigenesis. We found that 0.56% of families showed a monoallelic frameshift MUTYH PV, while a previous study reported MUTYH PVs in 2.37% of patients with a family history of prostate cancer [38]. Our results suggest an involvement of monoallelic MUTYH mutations in PCa onset; however, additional studies are required.
Mutated and non-mutated patients had a similar mean age of onset, although HPCa showed a trend towards an earlier onset age compared to sporadic cases [39]. No difference has been reported in overall survival between HPCa and sporadic PCa [2]. However, previously, Castro et al. described that BRCA1/2 mutations confer a more aggressive PCa phenotype and lower survival. Additionally, Narod et al. observed a median survival from diagnosis of 4.0 years for men with BRCA2 mutation in antithesis to 8.0 years for men with BRCA1 mutation, a factor that was recommended to be considered for the clinical management of patients [40,41,42]. We found an average survival of 8 years in PCa patients, with a similar average age of death between mutated and non-mutated. This difference could be due to the size of cohort as well as different clinical aspects of the enrolled patients. BRCA2 germline mutation provided a greater contribution to increased PCa risk compared to BRCA1. Carriers of BRCA2 mutations have an 8.6-foldelevated risk of developing HPCa compared to non-carriers; the relative risk of HPCa developing in BRCA1 mutation carriers is increased 3.8-fold [43,44]. BRCA2 pathogenic variants have also been associated with an increased risk of high-grade disease and progression to mCRPC [2]. Here, in HBOC families, PCa occurs in 18% of cancer cases, making it the second most recurrent cancer. The frequency of PCa was equal in both mutated and non-mutated families. Interestingly, there was no significant difference in prostate cancer development between non-mutated HBOC families and HBOC families that harbored mutations in BRCA, PALB2, RAD51C, TP53 and MUTYH genes. This is likely because the categorized “non-mutated” HBOC families could be carriers of pathogenic mutations in genes not yet identified. Screening for mutation in BRCA1 and BRCA2 has the potential to help in the stratification of patients to more targeted therapies. Indeed, patients with mutations in the BRCA genes have a better response to PARP inhibitors. This led the Food and Drug Administration (FDA) to approve the drug Olaparib for patients with mCRPC who harbor mutation in BRCA1/BRCA2 and/or ATM genes. MMR-mutated patients can benefit from immunotherapy, with the FDA having recently approved PD-L1 inhibitor pembrolizumab (KEYTRUDA) for the treatment of patients with microsatellite instability-high (MSI-H)/MMR-deficient [45,46,47].
Furthermore, clinical trials undertaken with prostate cancer patients who are carriers of a mutant PALB2 have demonstrated a positive response to Olaparib treatments, particularly for patients with resistance to treatment [33,48].
TP53 mutations have been associated with an unfavorable response to antiandrogens, abiraterone and enzalutamide, although this mechanism remains to be elucidated. Whether and to what extent TP53 alterations affect the response to the PARP inhibitor Olaparib is currently unclear [35].
Surveillance should be conducted regularly with PSA assay, urological examination and/or magnetic resonance imaging annually, starting from age 41. In our cohort, the 41 unaffected HBOC family members who inherited the proband’s mutation have an increased risk of developing PCa or other related tumors. The potential consequences relating to tumorigenesis could be reduced through the early detection of the cancer. Therefore, all 41 unaffected HBOC family members who are carriers of the proband’s mutations were enrolled in an active surveillance program for PCa and other related tumors in our hospital. Women with BRCA1, BRCA2, PALB2 and RAD51C mutations were enrolled in a surveillance program for breast, ovarian and colon cancer development, whereas men with BRCA1, BRCA2, PALB2 and RAD51C mutations were enrolled in a surveillance program targeting breast, prostate, colon, laryngeal and pancreatic cancer.
5. Conclusions
In this study, one of the few studies focused on Italian patients with hereditary prostate cancer, we showed pathogenic germline mutations in five susceptibility genes in HBOC probands. In addition, we founded a monoallelic frameshift mutation in MUTYH gene, suggesting an involvement of monoallelic MUTYH mutations in PCa onset. Testing family members of mutated patients gives them the opportunity to optin to surveillance programs for HPCa and other HBOC-related tumors, decreasing the potential consequences relating to cancer development through early detection.
Author Contributions
Conceptualization, M.T.V.; methodology, G.C., L.A. and L.P.; writing—original draft preparation, M.T.V., M.-M.T. and G.D.; critical revision, A.M.M.; supervision, M.T.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was carried out in accordance with the World Medical Association Helsinki Declaration, adopted in 1964 and amended in 1975, 1983, 1989, 1996 and 2000. Informed consent was obtained from all subjects, and the study was approved and conducted according to the ethical guidelines of the University of Campania “Luigi Vanvitelli” (no.469-23/07/2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
We thank Claudio Napoli, Department of Advanced Medical and Surgical Sciences, University of Campania “Luigi Vanvitelli”, Naples (Italy), for critical revision of the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Rebello, R.J.; Oing, C.; Knudsen, K.E.; Loeb, S.; Johnson, D.C.; Reiter, R.E.; Gillessen, S.; Van der Kwast, T.; Bristow, R.G. Prostate cancer. Nat. Rev. Dis. Prim. 2021, 7, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Heidegger, I.; Tsaur, I.; Borgmann, H.; Surcel, C.; Kretschmer, A.; Mathieu, R.; De Visschere, P.; Valerio, M.; Bergh, R.C.V.D.; Ost, P.; et al. EAU-YAU Prostate Cancer Working Party. Hereditary prostate cancer—Primetime for genetic testing? Cancer Treat. Rev. 2019, 81, 101927. [Google Scholar] [CrossRef] [PubMed]
- Vietri, M.; D’Elia, G.; Caliendo, G.; Resse, M.; Casamassimi, A.; Passariello, L.; Albanese, L.; Cioffi, M.; Molinari, A. Hereditary Prostate Cancer: Genes Related, Target Therapy and Prevention. Int. J. Mol. Sci. 2021, 22, 3753. [Google Scholar] [CrossRef] [PubMed]
- Rebbeck, T.R. Prostate Cancer Genetics: Variation by Race, Ethnicity, and Geography. Semin. Radiat. Oncol. 2016, 27, 3–10. [Google Scholar] [CrossRef]
- Barber, L.E.; Gerke, T.; Markt, S.C.; Peisch, S.F.; Wilson, K.M.; Ahearn, T.U.; Giovannucci, E.L.; Parmigiani, G.; Mucci, L.A. Family History of Breast or Prostate Cancer and Prostate Cancer Risk. Clin. Cancer Res. 2018, 24, 5910–5917. [Google Scholar] [CrossRef]
- Vietri, M.T.; D’Elia, G.; Caliendo, G.; Casamassimi, A.; Resse, M.; Passariello, L.; Cioffi, M.; Molinari, A.M. Double mutation of APC and BRCA1 in an Italian family. Cancer Genet. 2020, 244, 32–35. [Google Scholar] [CrossRef]
- Vietri, M.T.; D’Elia, G.; Caliendo, G.; Casamassimi, A.; Federico, A.; Passariello, L.; Cioffi, M.; Molinari, A.M. Prevalence of mutations in BRCA and MMR genes in patients affected with hereditary endometrial cancer. Med. Oncol. 2021, 38, 1–10. [Google Scholar] [CrossRef]
- Vietri, M.T.; Molinari, A.M.; De Paola, M.L.; Cantile, F.; Fasano, M.; Cioffi, M. Identification of a novel in-frame deletion in BRCA2 and analysis of variants of BRCA1/2 in Italian patients affected with hereditary breast and ovarian cancer. Clin. Chem. Lab. Med. (CCLM) 2012, 50, 2171–2180. [Google Scholar] [CrossRef]
- Vietri, M.T.; D’Elia, G.; Benincasa, G.; Ferraro, G.; Caliendo, G.; Nicoletti, G.F.; Napoli, C. DNA methylation and breast cancer: A way forward (Review). Int. J. Oncol. 2021, 59, 1–12. [Google Scholar] [CrossRef]
- Das, S.; Salami, S.S.; Spratt, D.E.; Kaffenberger, S.D.; Jacobs, M.F.; Morgan, T.M. Bringing Prostate Cancer Germline Genetics into Clinical Practice. J. Urol. 2019, 202, 223–230. [Google Scholar] [CrossRef]
- González-Santiago, S.; the SEOM Hereditary Cancer Working Group; Cajal, T.R.Y.; Aguirre, E.; Alés-Martínez, J.E.; Andrés, R.; Balmaña, J.; Graña, B.; Herrero, A.; Llort, G.; et al. SEOM clinical guidelines in hereditary breast and ovarian cancer (2019). Clin. Transl. Oncol. 2019, 22, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Vietri, M.T.; Molinari, A.M.; Caliendo, G.; De Paola, M.L.; D’Elia, G.; Gambardella, A.L.; Petronella, P.; Cioffi, M. Double heterozygosity in the BRCA1 and BRCA2 genes in Italian family. Clin. Chem. Lab. Med. 2013, 51, 2319–2324. [Google Scholar] [CrossRef] [PubMed]
- Vietri, M.T.; Caliendo, G.; Schiano, C.; Casamassimi, A.; Molinari, A.M.; Napoli, C.; Cioffi, M. Analysis of PALB2 in a cohort of Italian breast cancer patients: Identification of a novel PALB2 truncating mutation. Fam. Cancer 2015, 14, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Vietri, M.T.; Caliendo, G.; Casamassimi, A.; Cioffi, M.L.; De Paola, M.; Napoli, C.; Molinari, A.M. A novel PALB2 truncating mutation in an Italian family with male breast cancer. Oncol. Rep. 2015, 33, 1243–1247. [Google Scholar] [CrossRef]
- Plon, S.E.; Eccles, D.M.; Easton, D.; Foulkes, W.D.; Genuardi, M.; Greenblatt, M.S.; Hogervorst, F.B.; Hoogerbrugge, N.; Spurdle, A.B.; Tavtigian, S.V.; et al. Sequence variant classification and reporting: Recommendations for improving the interpretation of cancer susceptibility genetic test results. Hum. Mutat. 2008, 29, 1282–1291. [Google Scholar] [CrossRef]
- Pilarski, R. The Role of BRCA Testing in Hereditary Pancreatic and Prostate Cancer Families. Am. Soc. Clin. Oncol. Educ. Book 2019, 39, 79–86. [Google Scholar] [CrossRef]
- Sokolova, A.O.; Cheng, H.H. Genetic Testing in Prostate Cancer. Curr. Oncol. Rep. 2020, 22, 5. [Google Scholar] [CrossRef]
- Zhen, J.T.; Syed, J.; Nguyen, K.A.; Leapman, M.S.; Agarwal, N.; Ms, K.B.; Llor, X.; Hofstatter, E.; Shuch, B. Genetic testing for hereditary prostate cancer: Current status and limitations. Cancer 2018, 124, 3105–3117. [Google Scholar] [CrossRef]
- Pritchard, C.C.; Mateo, J.; Walsh, M.F.; De Sarkar, N.; Abida, W.; Beltran, H.; Garofalo, A.; Gulati, R.; Carreira, S.; Eeles, R.; et al. Inherited DNA-Repair Gene Mutations in Men with Metastatic Prostate Cancer. N. Engl. J. Med. 2016, 375, 443–453. [Google Scholar] [CrossRef]
- Gandaglia, G.; Briganti, A.; Montorsi, F. Reimagining prostate cancer screening: The IMPACT of germline mutations. Lancet Oncol. 2021, 22, 1491–1492. [Google Scholar] [CrossRef]
- Costa, D.; Scognamiglio, M.; Fiorito, C.; Benincasa, G.; Napoli, C. Genetic background, epigenetic factors and dietary interventions which influence human longevity. Biogerontology 2019, 20, 605–626. [Google Scholar] [CrossRef] [PubMed]
- Sarno, F.; the International Network Medicine Consortium; Benincasa, G.; List, M.; Barabasi, A.-L.; Baumbach, J.; Ciardiello, F.; Filetti, S.; Glass, K.; Loscalzo, J.; et al. Clinical epigenetics settings for cancer and cardiovascular diseases: Real-life applications of network medicine at the bedside. Clin. Epigenetics 2021, 13, 1–38. [Google Scholar] [CrossRef] [PubMed]
- Maiorino, M.I.; Schisano, B.; Di Palo, C.; Vietri, M.T.; Cioffi, M.; Giugliano, G.; Giugliano, D.; Esposito, K. Interleukin-20 circulating levels in obese women: Effect of weight loss. Nutr. Metab. Cardiovasc. Dis. 2010, 20, 180–185. [Google Scholar] [CrossRef]
- Cioffi, M.; Riegler, G.; Vietri, M.T.; Pilla, P.; Caserta, L.; Carratù, R.; Sica, V.; Molinari, A.M. Serum p53 antibodies in patients affected with ulcerative colitis. Inflamm. Bowel. Dis. 2004, 10, 606–611. [Google Scholar] [CrossRef] [PubMed]
- Bellastella, G.; Maiorino, M.I.; De Bellis, A.; Vietri, M.T.; Mosca, C.; Scappaticcio, L.; Pasquali, D.; Esposito, K.; Giugliano, D. Serum but not salivary cortisol levels are influenced by daily glycemic oscillations in type 2 diabetes. Endocrine 2016, 53, 220–226. [Google Scholar] [CrossRef]
- Pritzlaff, M.; Tian, Y.; Reineke, P.; Stuenkel, A.J.; Allen, K.; Gutierrez, S.; Jackson, M.; Dolinsky, J.S.; LaDuca, H.; Xu, J.; et al. Diagnosing hereditary cancer predisposition in men with prostate cancer. Genet. Med. 2020, 22, 1517–1523. [Google Scholar] [CrossRef]
- Vietri, M.T.; Caliendo, G.; D’Elia, G.; Resse, M.; Casamassimi, A.; Minucci, P.B.; Ioio, C.D.; Cioffi, M.; Molinari, A.M. Five Italian Families with Two Mutations in BRCA Genes. Genes 2020, 11, 1451. [Google Scholar] [CrossRef]
- Iversen, E.S.; Lipton, G.; Hart, S.N.; Lee, K.Y.; Hu, C.; Polley, E.C.; Pesaran, T.; Yussuf, A.; LaDuca, H.; Chao, E.; et al. An integrative model for the comprehensive classification of BRCA1 and BRCA2 variants of uncertain clinical significance. npj Genom. Med. 2022, 7, 1–8. [Google Scholar] [CrossRef]
- Lyra, P.C.M.; Nepomuceno, T.C.; de Souza, M.L.M.; Machado, G.F.; Veloso, M.F.; Henriques, T.B.; dos Santos, D.Z.; Ribeiro, I.G.; Ribeiro, R.S.; Rangel, L.B.A.; et al. Integration of functional assay data results provides strong evidence for classification of hundreds of BRCA1 variants of uncertain significance. Genet. Med. 2020, 23, 306–315. [Google Scholar] [CrossRef]
- Edwards, S.M.; Evans, D.G.; Hope, Q.; Norman, A.R.; Barbachano, Y.; Bullock, S.; Kote-Jarai, Z.; Meitz, J.; Falconer, A.; Osin, P.; et al. UK Genetic Prostate Cancer Study Collaborators and BAUS Section of Oncology. Pros-tate cancer in BRCA2 germline mutation carriers is associated with poorer prognosis. Br. J. Cancer 2010, 7, 918–924. [Google Scholar] [CrossRef]
- Patel, V.L.; Busch, E.L.; Friebel, T.M.; Cronin, A.; Leslie, G.; McGuffog, L.; Adlard, J.; Agata, S.; Agnarsson, B.A.; Ahmed, M.; et al. Association of Genomic Domains in BRCA1 and BRCA2 with Prostate Cancer Risk and Aggressiveness. Cancer Res. 2020, 80, 624–638. [Google Scholar] [CrossRef] [PubMed]
- Paulo, P.; Pinto, P.; Peixoto, A.; Santos, C.; Pinto, C.; Rocha, P.; Veiga, I.; Soares, G.; Machado, C.; Ramos, F.; et al. Validation of a Next-Generation Sequencing Pipeline for the Molecular Diagnosis of Multiple Inherited Cancer Predisposing Syndromes. J. Mol. Diagn. 2017, 19, 502–513. [Google Scholar] [CrossRef] [PubMed]
- Horak, P.; Weischenfeldt, J.; von Amsberg, G.; Beyer, B.; Schütte, A.; Uhrig, S.; Gieldon, L.; Klink, B.; Feuerbach, L.; Hübschmann, D.; et al. Response to olaparib in a PALB2 germline mutated prostate cancer and genetic events associated with resistance. Mol. Case Stud. 2019, 5, a003657. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Guo, H.; Zhu, Y.; Xia, Y.; Cui, J.; Shi, K.; Fan, Y.; Shi, B.; Chen, S. TP53 alterations of hormone-naïve prostate cancer in the Chinese population. Prostate Cancer Prostatic Dis. 2020, 24, 482–491. [Google Scholar] [CrossRef]
- Teroerde, M.; Nientiedt, C.; Duensing, A.; Hohenfellner, M.; Stenzinger, A.; Duensing, S.; Bott, S.R.J.; Ng, K.L. Revisiting the Role of p53 in Prostate Cancer. In Prostate Cancer; Exon Publications: Brisbane, Australia, 2021; Chapter 8. [Google Scholar]
- D’Elia, G.; Caliendo, G.; Casamassimi, A.; Cioffi, M.; Molinari, A.M.; Vietri, M.T. APC and MUTYH Analysis in FAP Patients: A Novel Mutation in APC Gene and Genotype-Phenotype Correlation. Genes 2018, 9, 322. [Google Scholar] [CrossRef]
- Vietri, M.T.; D’Elia, G.; Caliendo, G.; Albanese, L.; Signoriello, G.; Napoli, C.; Molinari, A.M. Pancreatic Cancer with Mutation in BRCA1/2, MLH1, and APC Genes: Phenotype Correlation and Detection of a Novel Germline BRCA2 Mutation. Genes 2022, 13, 321. [Google Scholar] [CrossRef]
- Nicolosi, P.; Ledet, E.; Yang, S.; Michalski, S.; Freschi, B.; O’Leary, E.; Esplin, E.D.; Nussbaum, R.L.; Sartor, O. Prevalence of Germline Variants in Prostate Cancer and Implications for Current Genetic Testing Guidelines. JAMA Oncol. 2019, 5, 523–528. [Google Scholar] [CrossRef]
- Thalgott, M.; Kron, M.; Brath, J.M.; Ankerst, D.P.; Thompson, I.M.; Gschwend, J.E.; Herkommer, K. Men with family history of prostate cancer have a higher risk of disease recurrence after radical prostatectomy. World J. Urol. 2017, 36, 177–185. [Google Scholar] [CrossRef]
- Castro, E.; Goh, C.; Olmos, D.; Saunders, E.; Leongamornlert, D.; Tymrakiewicz, M.; Mahmud, N.; Dadaev, T.; Govindasami, K.; Guy, M.; et al. Germline BRCA Mutations Are Associated with Higher Risk of Nodal Involvement, Distant Metastasis, and Poor Survival Outcomes in Prostate Cancer. J. Clin. Oncol. 2013, 31, 1748–1757. [Google Scholar] [CrossRef]
- Castro, E.; Goh, C.; Leongamornlert, D.; Saunders, E.; Tymrakiewicz, M.; Dadaev, T.; Govindasami, K.; Guy, M.; Ellis, S.; Frost, D.; et al. Effect of BRCA Mutations on Metastatic Relapse and Cause-specific Survival After Radical Treatment for Localised Prostate Cancer. Eur. Urol. 2015, 68, 186–193. [Google Scholar] [CrossRef]
- Narod, S.A.; Neuhausen, S.; Vichodez, G.; Armel, S.; Lynch, H.T.; Ghadirian, P.; Cummings, S.; Olopade, O.; Stoppa-Lyonnet, D.; Couch, F.; et al. Rapid progression of prostate cancer in men with a BRCA2 mutation. Br. J. Cancer 2008, 99, 371–374. [Google Scholar] [CrossRef] [PubMed]
- Ren, Z.-J.; Cao, D.-H.; Zhang, Q.; Ren, P.-W.; Liu, L.-R.; Wei, Q.; Wei, W.-R.; Dong, Q. First-degree family history of breast cancer is associated with prostate cancer risk: A systematic review and meta-analysis. BMC Cancer 2019, 19, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Vietri, M.T.; Caliendo, G.; D’Elia, G.; Resse, M.; Casamassimi, A.; Minucci, P.B.; Cioffi, M.; Molinari, A.M. BRCA and PALB2 mutations in a cohort of male breast cancer with one bilateral case. Eur. J. Med Genet. 2020, 63, 103883. [Google Scholar] [CrossRef]
- Marabelle, A.; Le, D.T.; Ascierto, P.A.; Di Giacomo, A.M.; De Jesus-Acosta, A.; Delord, J.-P.; Geva, R.; Gottfried, M.; Penel, N.; Hansen, A.R.; et al. Efficacy of Pembrolizumab in Patients with Noncolorectal High Microsatellite Instability/Mismatch Repair–Deficient Cancer: Results From the Phase II KEYNOTE-158 Study. J. Clin. Oncol. 2020, 38, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Montisci, A.; Vietri, M.T.; Palmieri, V.; Sala, S.; Donatelli, F.; Napoli, C. Cardiac Toxicity Associated with Cancer Immunotherapy and Biological Drugs. Cancers 2021, 13, 4797. [Google Scholar] [CrossRef] [PubMed]
- Montisci, A.; Palmieri, V.; Liu, J.E.; Vietri, M.T.; Cirri, S.; Donatelli, F.; Napoli, C. Severe Cardiac Toxicity Induced by Cancer Therapies Requiring Intensive Care Unit Admission. Front. Cardiovasc. Med. 2021, 8, 713694. [Google Scholar] [CrossRef]
- Carreira, S.; Porta, N.; Arce-Gallego, S.; Seed, G.; Llop-Guevara, A.; Bianchini, D.; Rescigno, P.; Paschalis, A.; Bertan, C.; Baker, C.; et al. Biomarkers Associating with PARP Inhibitor Benefit in Prostate Cancer in the TOPARP-B Trial. Cancer Discov. 2021, 11, 2812–2827. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).