Effect of Different Printing Designs and Resin Types on the Accuracy of Orthodontic Model
Abstract
1. Introduction
2. Materials and Methods
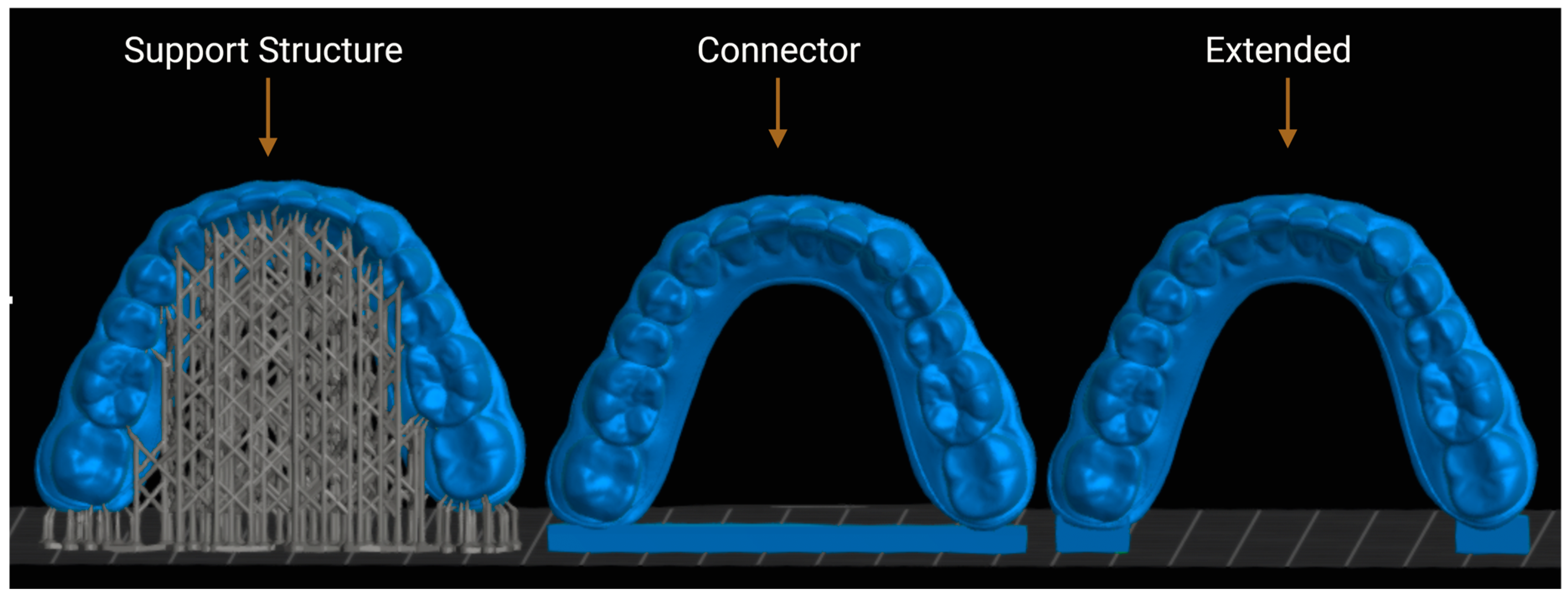
2.1. Model Design and Planning
2.2. Three-Dimensional Printing Process
2.3. Print Optimization
2.4. Post-Print Processing
2.5. Accuracy Assessment
2.6. Statistical Analysis
2.7. Method Error
3. Results
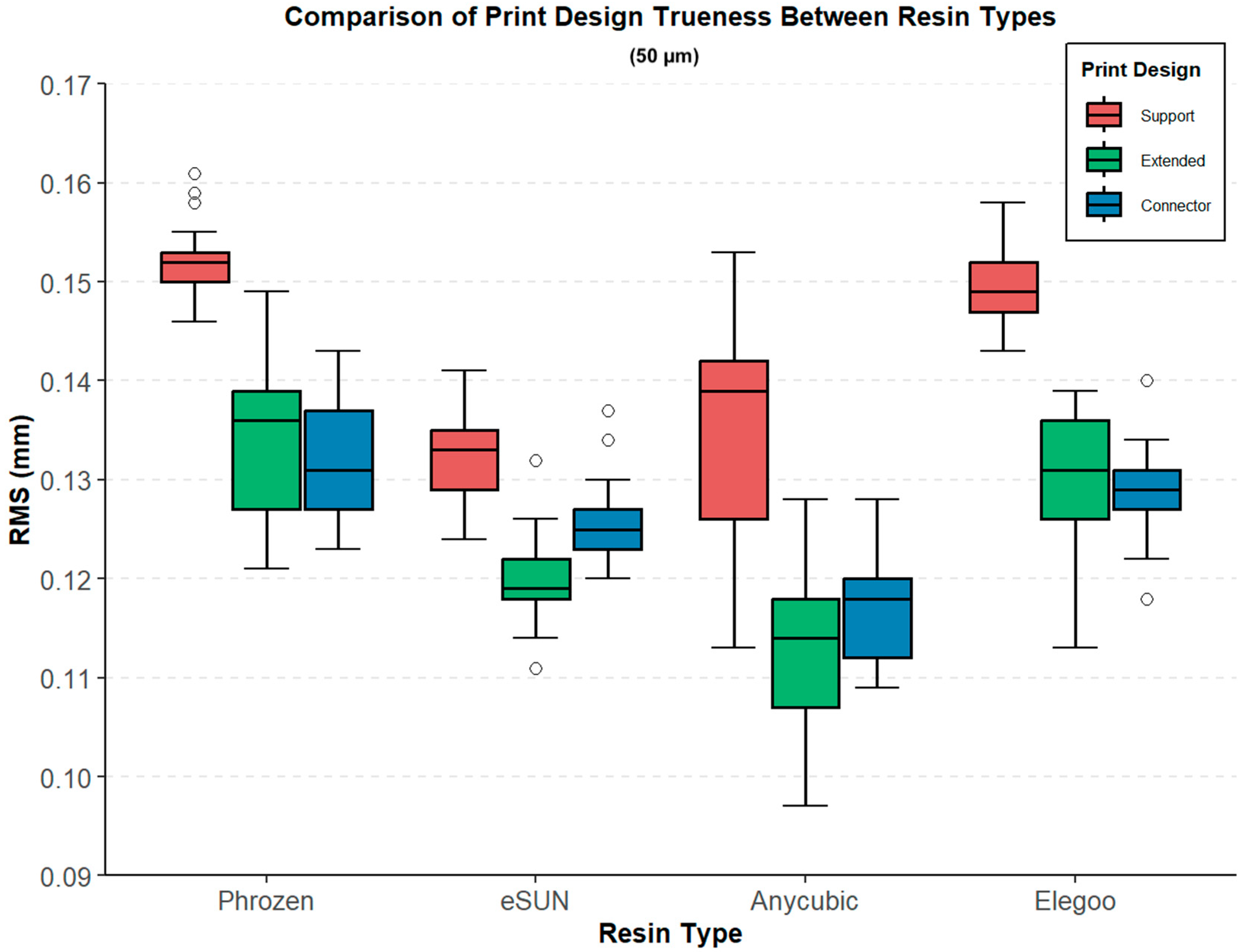
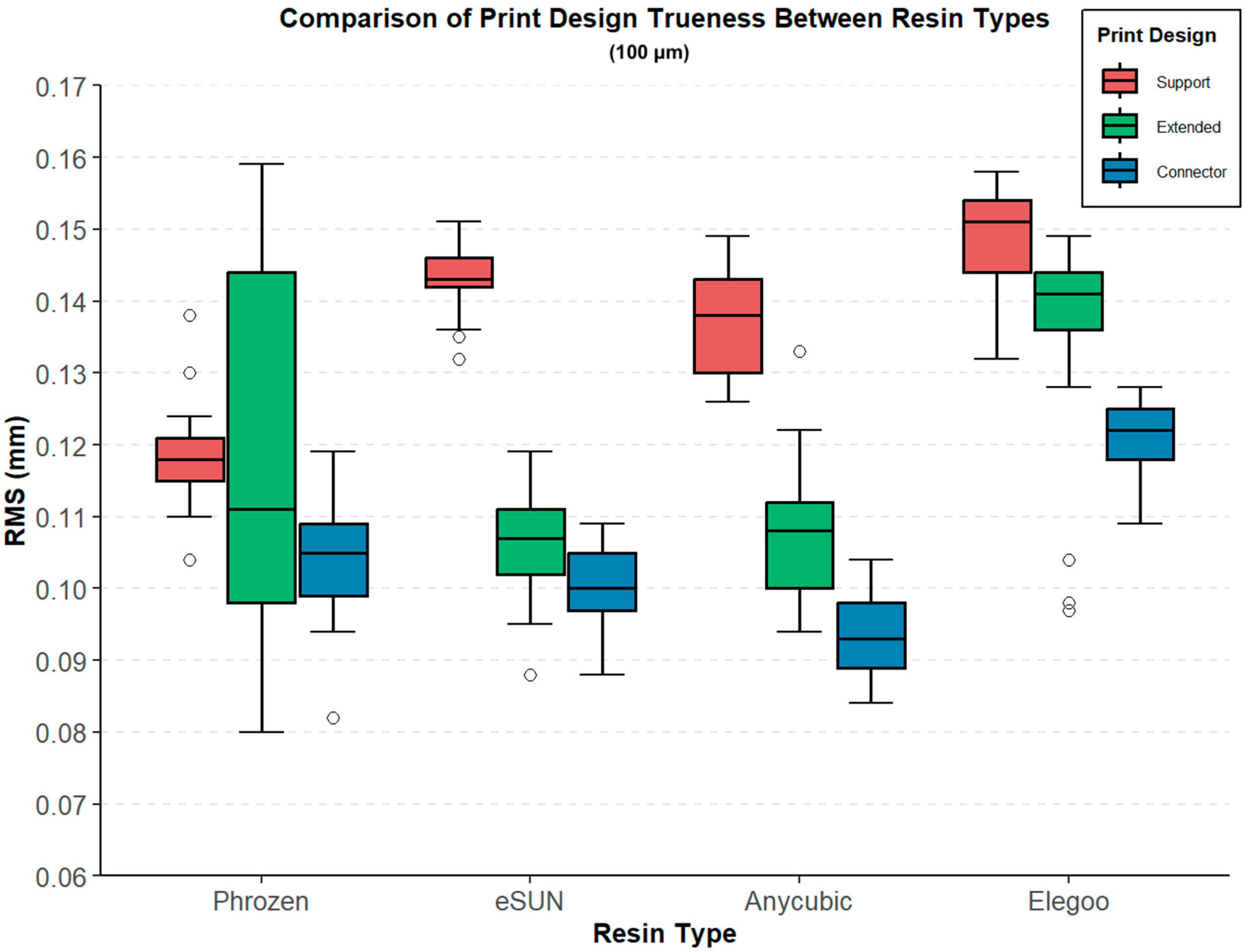
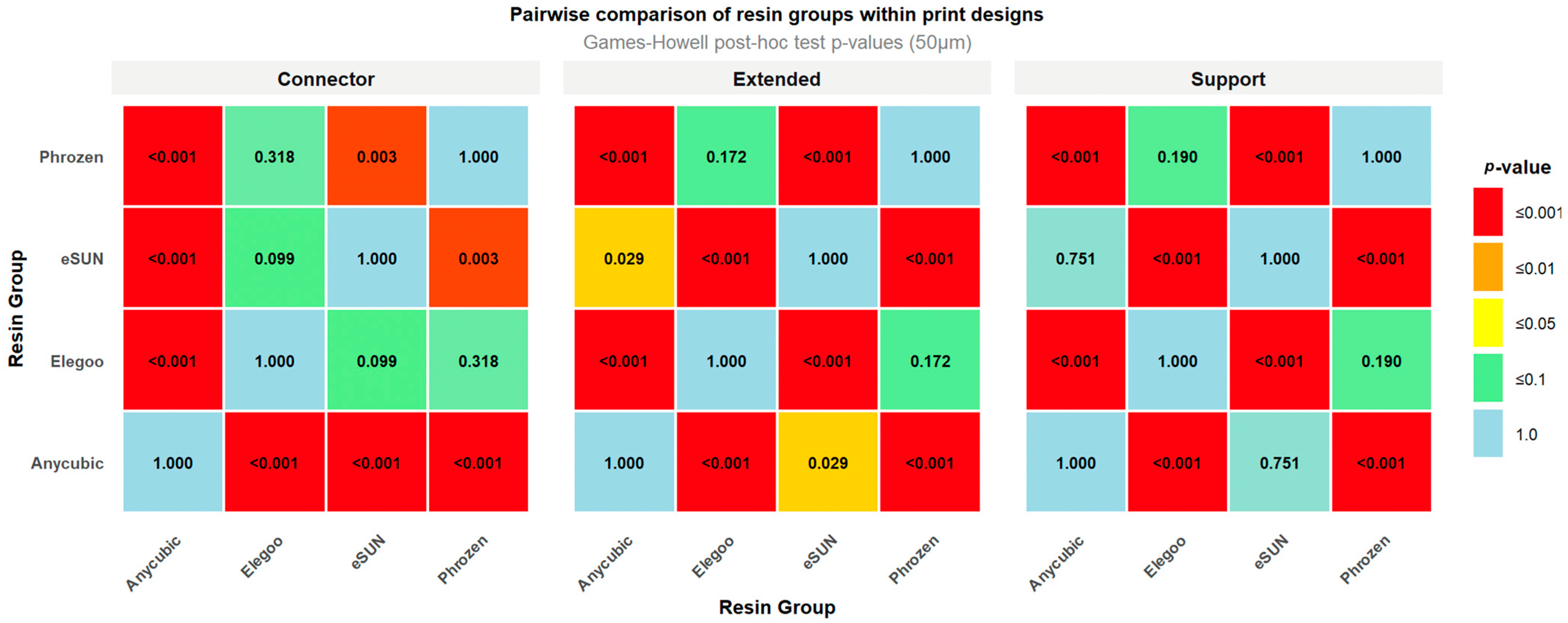
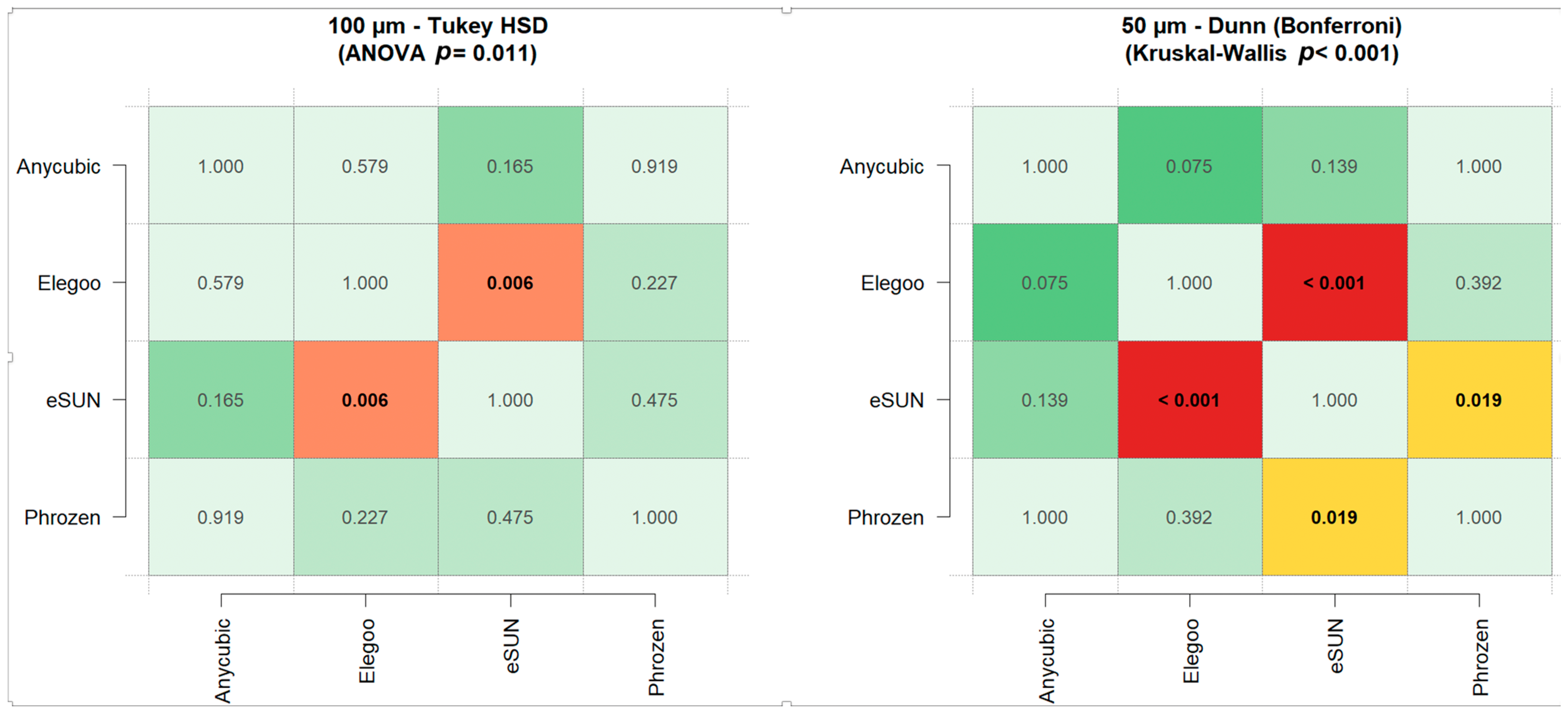
3.1. Resin-Based Comparisons
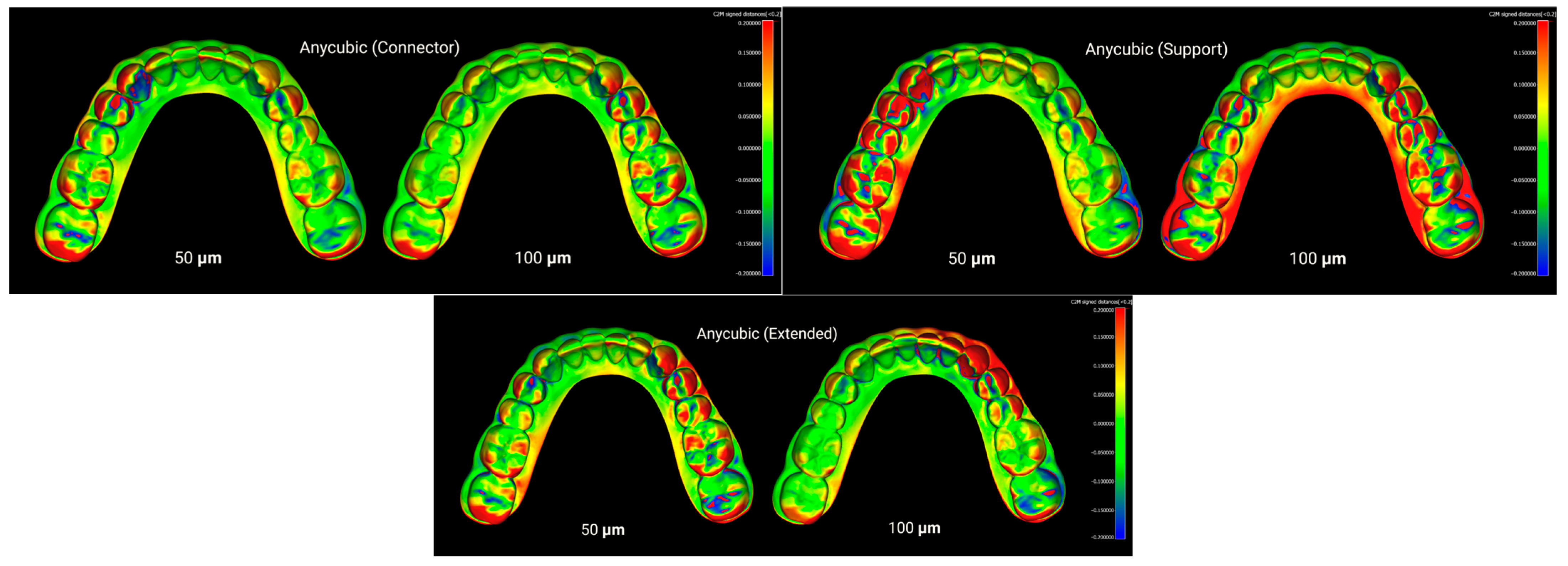
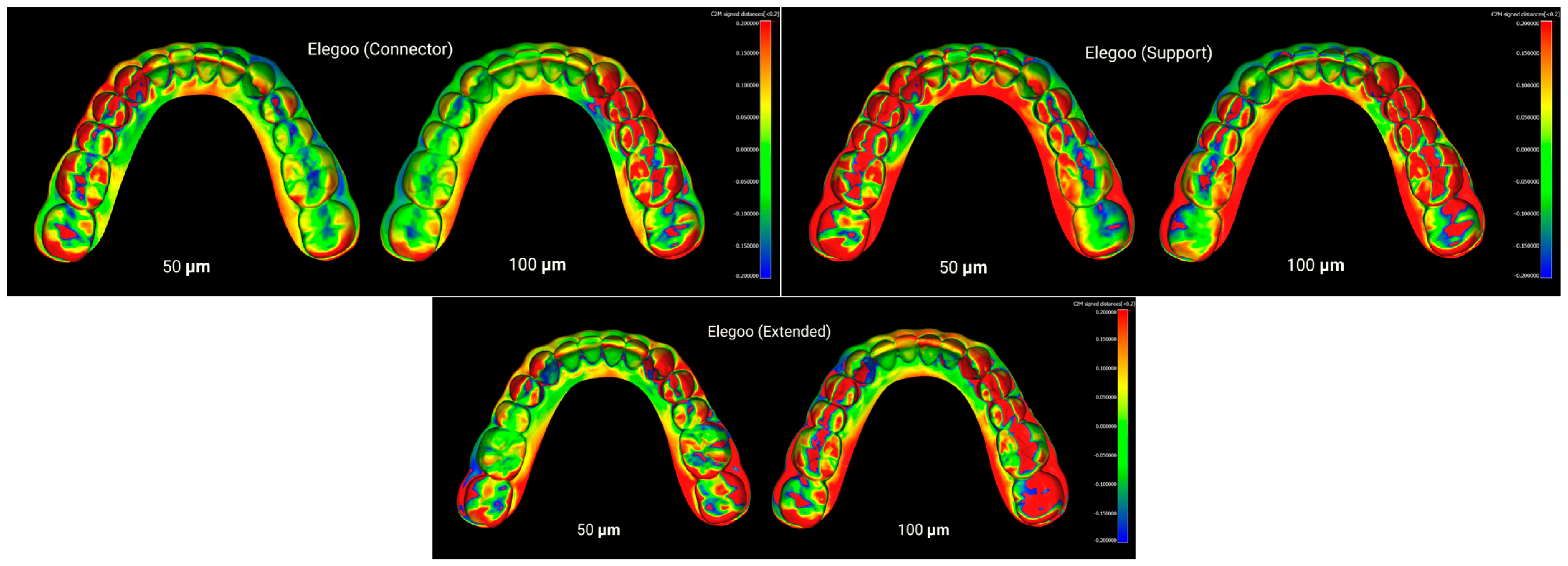
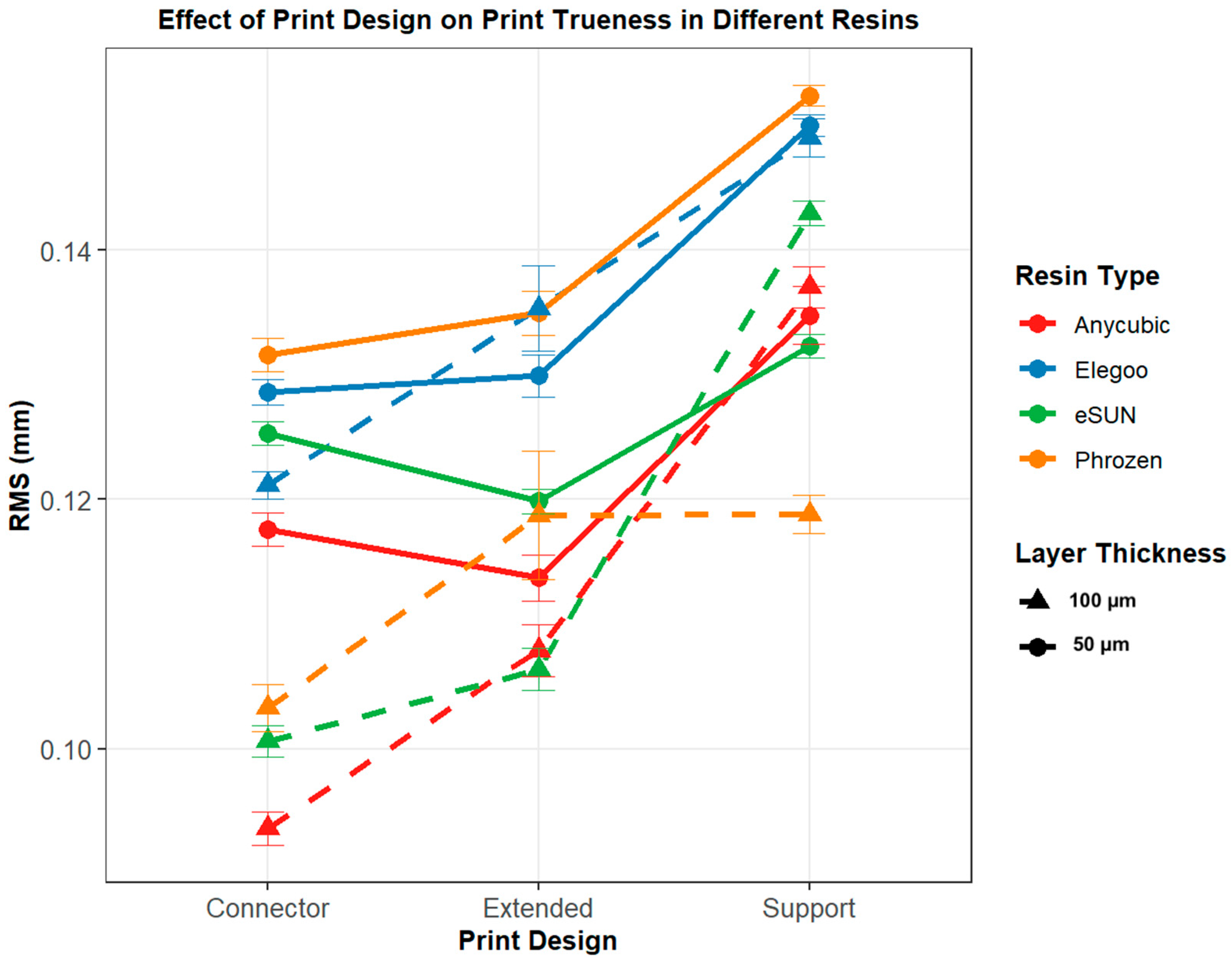
3.2. Print Design-Based Comparison
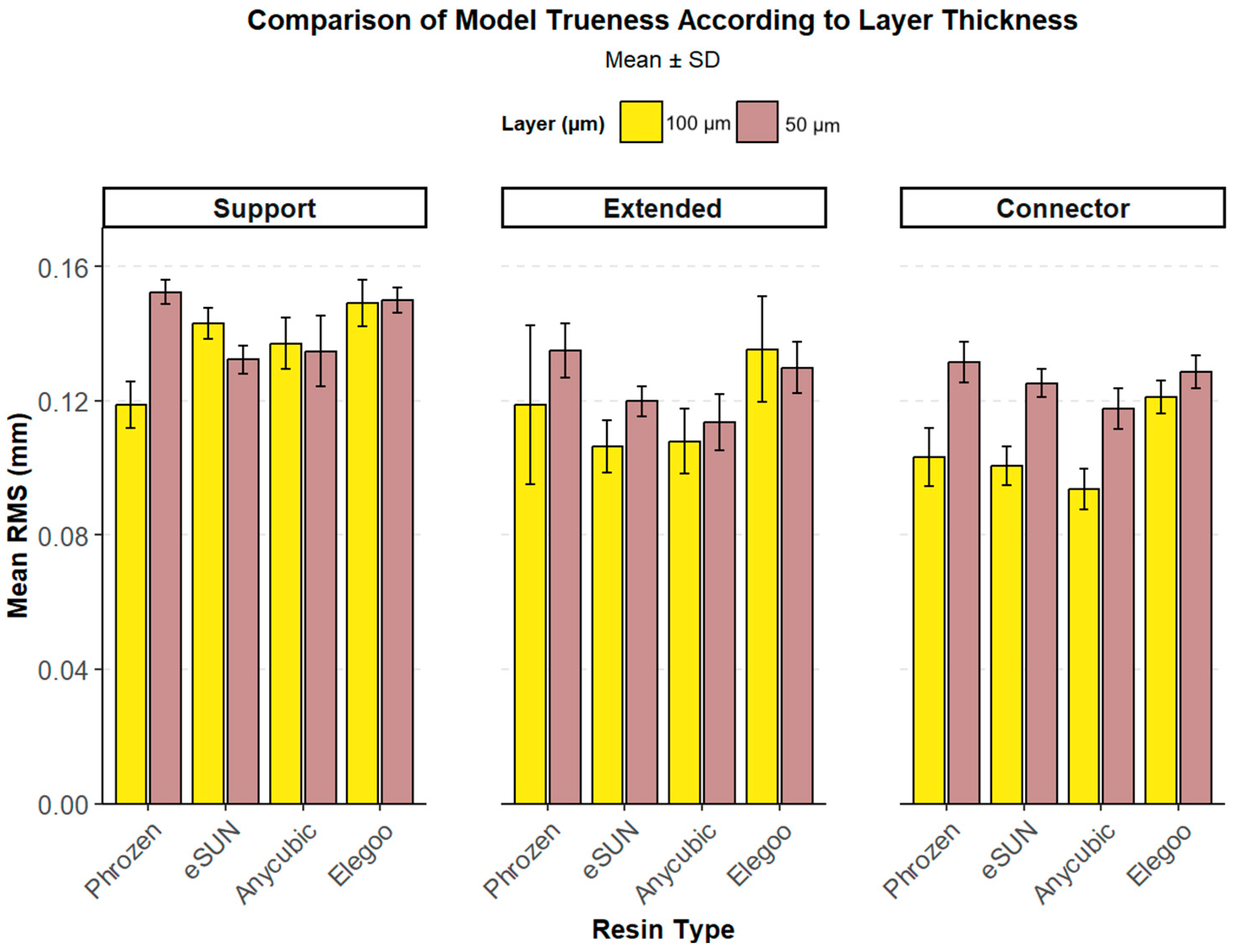
3.3. Layer-Based Comparison
3.4. Evaluation of Precision with Respect to Resins
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Papadimitriou, A.; Mousoulea, S.; Gkantidis, N.; Kloukos, D. Clinical effectiveness of Invisalign® orthodontic treatment: A systematic review. Prog. Orthod. 2018, 19, 37. [Google Scholar] [CrossRef]
- Hartogsohn, C.R.; Sonnesen, L. Clear Aligner Treatment: Indications, Advantages, and Adverse Effects—A Systematic Review. Dent. J. 2025, 13, 40. [Google Scholar] [CrossRef]
- Gassem, A.A.B. Does clear aligner treatment result in different patient perceptions of treatment process and outcomes compared to conventional/traditional fixed appliance treatment: A literature review. Eur. J. Dent. 2022, 16, 274–285. [Google Scholar] [CrossRef]
- Venezia, P.; Ronsivalle, V.; Rustico, L.; Barbato, E.; Leonardi, R.; Giudice, A.L. Accuracy of orthodontic models prototyped for clear aligners therapy: A 3D imaging analysis comparing different market segments 3D printing protocols. J. Dent. 2022, 124, 104212. [Google Scholar] [CrossRef]
- Khosravi, R.; Gidarakou, I.; Salazar, T. Essential factors in developing an efficient in-office aligner system. Semin. Orthod. 2022, 28, 45–52. [Google Scholar] [CrossRef]
- Bor, S. In-Office Aligner Fabrication. Van Diş Hekim. Derg. 2023, 4, 42–51. [Google Scholar]
- Shah, M.J.; Kubavat, A.K.; Patel, K.V.; Prajapati, N.H. Fabrication of in-house aligner—A review. J. Contemp. Orthod. 2022, 6, 120–124. [Google Scholar] [CrossRef]
- Kessler, A.; Hickel, R.; Reymus, M. 3D printing in dentistry—State of the art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Strub, J.R.; Rekow, E.D.; Witkowski, S. Computer-aided design and fabrication of dental restorations: Current systems and future possibilities. J. Am. Dent. Assoc. 2006, 137, 1289–1296. [Google Scholar] [CrossRef]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.Y.; Lee, E.S.; Jiang, H.B. A review of 3D printing in dentistry: Technologies, affecting factors, and applications. Scanning. 2021, 2021, 9950131. [Google Scholar] [CrossRef] [PubMed]
- Minervino, B.L.; Minervino, B.L.; Barriviera, M.; Curado, M.D.M.; Gandini, L.G. MARPE guide: A case report. J. Contemp. Dent. Pract. 2019, 20, 1102–1107. [Google Scholar] [PubMed]
- Hajeer, M.; Millett, D.T.; Ayoub, A.F.; Siebert, J.P. Applications of 3D imaging in orthodontics: Part I. J. Orthod. 2004, 31, 62–70. [Google Scholar] [CrossRef]
- Paradowska-Stolarz, A.; Wezgowiec, J.; Mikulewicz, M. Comparison of two chosen 3D printing resins designed for orthodontic use: An in vitro study. Materials 2023, 16, 2237. [Google Scholar] [CrossRef]
- ISO 5725-1:2023; Accuracy (Trueness and Precision) of Measurement Methods and Results—Part 1: General Principles and Definitions. International Organization for Standardization: Geneva, Switzerland, 2023.
- Tsolakis, I.A.; Gizani, S.; Panayi, N.; Antonopoulos, G.; Tsolakis, A.I. Three-dimensional printing technology in orthodontics for dental models: A systematic review. Children 2022, 9, 1106. [Google Scholar] [CrossRef]
- Caussin, E.; Moussally, C.; Le Goff, S.; Fasham, T.; Troizier-Cheyne, M.; Tapie, L.; Dursun, E.; Attal, J.P.; François, P. Vat photopolymerization 3D printing in dentistry: A comprehensive review of actual popular technologies. Materials 2024, 17, 950. [Google Scholar] [CrossRef]
- Horvath, J. A brief history of 3D printing, in Mastering 3D printing. In Mastering 3D Printing; Springer: Berlin/Heidelberg, Germany, 2014; pp. 3–10. [Google Scholar]
- Piedra-Cascón, W.; Krishnamurthy, V.R.; Att, W.; Revilla-León, M. 3D printing parameters, supporting structures, slicing, and post-processing procedures of vat-polymerization additive manufacturing technologies: A narrative review. J. Dent. 2021, 109, 103630. [Google Scholar] [CrossRef]
- Grassia, V.; Ronsivalle, V.; Isola, G.; Nucci, L.; Leonardi, R.; Lo Giudice, A. Accuracy (trueness and precision) of 3D printed orthodontic models finalized to clear aligners production, testing crowded and spaced dentition. BMC Oral Health 2023, 23, 352. [Google Scholar] [CrossRef] [PubMed]
- Harikrishnan, S.; Subramanian, A.K. 3D printing in orthodontics: A narrative review. J. Int. Oral Health 2023, 15, 15–27. [Google Scholar]
- Gao, H.; Yang, Z.; Lin, W.S.; Tan, J.; Chen, L. The effect of build orientation on the dimensional accuracy of 3d-printed mandibular complete dentures manufactured with a multijet 3d printer. J. Prosthodont. 2021, 30, 684–689. [Google Scholar] [CrossRef]
- Loflin, W.A.; English, J.D.; Borders, C.; Harris, L.M.; Moon, A.; Holland, J.N.; Kasper, F.K. Effect of print layer height on the assessment of 3D-printed models. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 283–289. [Google Scholar] [CrossRef]
- Zhu, F.; Yu, L.; Hu, M.; Ding, Z.; Ma, H.; Feng, X.; Gao, Y.; Cao, Y. Influence of 3D printing angles on the accuracy of indirect adhesion transfer models: An in vitro study. Sci. Rep. 2025, 15, 9012. [Google Scholar] [CrossRef] [PubMed]
- Arnold, C.; Monsees, D.; Hey, J.; Schweyen, R. Surface quality of 3D-printed models as a function of various printing parameters. Materials 2019, 12, 1970. [Google Scholar] [CrossRef]
- Unkovskiy, A.; Bui, P.H.B.; Schille, C.; Geis-Gerstorfer, J.; Huettig, F.; Spintzyk, S. Objects build orientation, positioning, and curing influence dimensional accuracy and flexural properties of stereolithographically printed resin. Dent. Mater. 2018, 34, e324–e333. [Google Scholar] [CrossRef] [PubMed]
- Oğuz, F.; Bor, S. An Evaluation of the Performance of Low-Cost Resin Printers in Orthodontics. Biomimetics 2025, 10, 249. [Google Scholar] [CrossRef]
- Ling, L.; Lai, T.; Chung, P.T.; Sabet, S.; Tran, V.; Malyala, R. A Novel 3D-Printing Model Resin with Low Volumetric Shrinkage and High Accuracy. Polymers 2025, 17, 610. [Google Scholar] [CrossRef]
- Hata, K.; Ikeda, H.; Nagamatsu, Y.; Masaki, C.; Hosokawa, R.; Shimizu, H. Development of Dental Poly(methyl methacrylate)-Based Resin for Stereolithography Additive Manufacturing. Polymers 2021, 13, 4435. [Google Scholar] [CrossRef]
- Li, J.; Li, J.; Chan, W.Y.; Yee, K.K.; Cheuk, K.L.K. Photopolymer Composition for 3D Printing. U.S. Patent US9902860B1, 1 March 2018. [Google Scholar]
- Ko, J.; Bloomstein, R.D.; Briss, D.; Holland, J.N.; Morsy, H.M.; Kasper, F.K.; Huang, W. Effect of build angle and layer height on the accuracy of 3-dimensional printed dental models. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 451–458. [Google Scholar] [CrossRef]
- ElShebiny, T.; Matthaios, S.; Menezes, L.M.; Tsolakis, I.A. Effect of printing technology, layer height, and orientation on assessment of 3D-printed models. J. World Fed. Orthod. 2024, 13, 169–174. [Google Scholar] [CrossRef]
- Alshamrani, A.A.; Raju, R.; Ellakwa, A. Effect of printing layer thickness and postprinting conditions on the flexural strength and hardness of a 3D-printed resin. BioMed Res. Int. 2022, 2022, 8353137. [Google Scholar] [CrossRef] [PubMed]
- Namano, S.; Kanazawa, M.; Katheng, A.; Trang, B.N.H.; Hada, T.; Komagamine, Y.; Iwaki, M.; Minakuchi, S. Effect of support structures on the trueness and precision of 3D printing dentures: An in vitro study. J. Prosthodont. Res. 2024, 68, 114–121. [Google Scholar] [CrossRef]
- Zhou, Q.-Y.; Park, J.; Koltun, V. Open3D: A modern library for 3D data processing. arXiv 2018, arXiv:1801.09847. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 2013. [Google Scholar]
- Dawood, A.; Marti, B.M.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef]
- Traynor, G.; Shearn, A.I.; Milano, E.G.; Ordonez, M.V.; Velasco Forte, M.N.; Caputo, M.; Schievano, S.; Mustard, H.; Wray, J.; Biglino, G. The use of 3D-printed models in patient communication: A scoping review. J. 3D Print. Med. 2022, 6, 13–23. [Google Scholar] [CrossRef] [PubMed]
- Czajkowska, M.; Walejewska, E.; Zadrożny, Ł.; Wieczorek, M.; Święszkowski, W.; Wagner, L.; Mijiritsky, E.; Markowski, J. Comparison of dental stone models and their 3D printed acrylic replicas for the accuracy and mechanical properties. Materials 2020, 13, 4066. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Ronsivalle, V.; Rustico, L.; Aboulazm, K.; Isola, G.; Palazzo, G. Evaluation of the accuracy of orthodontic models prototyped with entry-level LCD-based 3D printers: A study using surface-based superimposition and deviation analysis. Clin. Oral Investig. 2022, 26, 303–312. [Google Scholar] [CrossRef]
- Favero, C.S.; English, J.D.; Cozad, B.E.; Wirthlin, J.O.; Short, M.M.; Kasper, F.K. Effect of print layer height and printer type on the accuracy of 3-dimensional printed orthodontic models. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Pauls, A.; Hornberg, A. Accuracy of soy-based resins for dental 3D printing. Angle Orthod. 2024, 94, 574–580. [Google Scholar] [CrossRef] [PubMed]
- Ledingham, A.D.; English, J.D.; Akyalcin, S.; Cozad, B.; Ontiveros, J.C.; Kasper, F.K. Accuracy and mechanical properties of orthodontic models printed 3-dimensionally from calcium sulfate before and after various postprinting treatments. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 1056–1062. [Google Scholar] [CrossRef]
- Hazeveld, A.; Slater, J.J.H.; Ren, Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 108–115. [Google Scholar] [CrossRef]
- Della Bona, A.; Cantelli, V.; Britto, V.T.; Collares, K.F.; Stansbury, J.W. 3D printing restorative materials using a stereolithographic technique: A systematic review. Dent. Mater. 2021, 37, 336–350. [Google Scholar] [CrossRef]
- Hada, T.; Kanazawa, M.; Iwaki, M.; Arakida, T.; Minakuchi, S. Effect of printing direction on stress distortion of three-dimensional printed dentures using stereolithography technology. J. Mech. Behav. Biomed. Mater. 2020, 110, 103949. [Google Scholar] [CrossRef]
- Rubayo, D.D.; Phasuk, K.; Vickery, J.M.; Morton, D.; Lin, W.S. Influences of build angle on the accuracy, printing time, and material consumption of additively manufactured surgical templates. J. Prosthet. Dent. 2021, 126, 658–663. [Google Scholar] [CrossRef]
- Stansbury, J.W.; Idacavage, M.J. 3D printing with polymers: Challenges among expanding options and opportunities. Dent. Mater. 2016, 32, 54–64. [Google Scholar] [CrossRef]
- Camardella, L.T.; Vilella, O.V.; Breuning, H. Accuracy of printed dental models made with 2 prototype technologies and different designs of model bases. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 1178–1187. [Google Scholar] [CrossRef]
- Shi, K.; Cai, C.; Wu, Z.; Yong, J. Slicing and support structure generation for 3D printing directly on B-rep models. Vis. Comput. Ind. Biomed. Art 2019, 2, 3. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Ye, C.; Wu, S.; Guo, K.; Mo, J. Sloping wall structure support generation for fused deposition modeling. Int. J. Adv. Manuf. Technol. 2009, 42, 1074–1081. [Google Scholar] [CrossRef]
- Wang, W.; Wang, T.Y.; Yang, Z.; Liu, L.; Tong, X.; Deng, J.; Chen, F.; Liu, X. Cost-effective printing of 3D objects with skin-frame structures. ACM Trans. Graph. 2013, 32, 1–10. [Google Scholar] [CrossRef]
- Vanek, J.; Galicia, J.A.G.; Benes, B. Clever support: Efficient support structure generation for digital fabrication. Comput. Graph. Forum 2014, 33, 117–125. [Google Scholar] [CrossRef]
- Jiang, J.; Xu, X.; Stringer, J. Support structures for additive manufacturing: A review. J. Manuf. Mater. Process. 2018, 2, 64. [Google Scholar] [CrossRef]
- Arnold, C.; Riß, L.; Hey, J.; Schweyen, R. Dimensional accuracy of different three-dimensional printing models as a function of varying the printing parameters. Materials 2024, 17, 3616. [Google Scholar] [CrossRef]
- Namano, S.; Kanazawa, M.; Qi, K.; Trang, B.N.H.; Sone, K.P.; Iwaki, M.; Komagamine, Y.; Minakuchi, S. Effects of support-structure design and postpolymerization protocols on dimensional changes in three-dimensionally printed complete dentures. J. Prosthet. Dent. 2025, 134, 190.e1–190.e9. [Google Scholar] [CrossRef] [PubMed]
- Çakmak, G.; Cuellar, A.R.; Donmez, M.B.; Abou-Ayash, S.; Lu, W.E.; Schimmel, M.; Yilmaz, B. Effect of printing layer thickness on the trueness of 3-unit interim fixed partial dentures. J. Prosthet. Dent. 2024, 131, 718–725. [Google Scholar] [CrossRef]
- Pszczółkowski, B.; Dzadz, Ł. Analysis of the İnfluence of UV Light Exposure Time on Hardness and Density Properties of SLA Models. Tech. Sci./Univ. Warm. Mazury Olszt. 2020, 23, 175–184. [Google Scholar]
- Pszczółkowski, B.; Zaborowska, M. Effect of Layer Exposure Time in SLA-LCD Printing on Surface Topography, Hardness and Chemical Structure of UV-Cured Photopolymer. Lubricants 2025, 13, 406. [Google Scholar] [CrossRef]
- Shen, M.; Zhao, W.; Xing, B.; Sing, Y.; Gao, S.; Wang, C.; Zhao, Z. Effects of exposure time and printing angle on the curing characteristics and flexural strength of ceramic samples fabricated via digital light processing. Ceram. Int. 2020, 46, 24379–24384. [Google Scholar] [CrossRef]
- Dicks, J.A.; Hoosain, M.I.; Mbele, O. Multi-Objective parametric optimisation of masked stereolithography additive manufacturing using the response surface method. S. Afr. J. Ind. Eng. 2024, 35, 52–65. [Google Scholar] [CrossRef]





| Resin Category | Resin Name and Type | Manufacturer (Location) | Print Orientation | Print Design Types (Support, Extended, Connector) |
|---|---|---|---|---|
| Orthodontic Resin | Elegoo Orthodontic Resin | Elegoo Inc. (Shenzhen, China) | Vertical | N = 21/design |
| Orthodontic Resin | eSUN Orthodontic Resin | Shenzhen Esun Industrial Co., Ltd. (Shenzhen, China) | Vertical | N = 21/design |
| Dental Model Resin | Phrozen Water-Washable Dental Model Resin | Phrozen Tech Co., Ltd. (Hsinchu City, Taiwan) | Vertical | N = 21/design |
| General Purpose Resin | Anycubic DLP Craftsman Resin (Beige) | Anycubic (Shenzhen, China) | Vertical | N = 21/design |
| Design | Resin Type | Mean ± SD | Min–Max | p-Value |
|---|---|---|---|---|
| Support | Anycubic | 0.135 ± 0.011 | 0.113–0.152 | <0.001 *** |
| Elegoo | 0.150 ± 0.004 | 0.143–0.158 | ||
| eSUN | 0.132 ± 0.004 | 0.126–0.139 | ||
| Phrozen | 0.152 ± 0.004 | 0.145–0.161 | ||
| Extended | Anycubic | 0.114 ± 0.008 | 0.097–0.125 | <0.001 *** |
| Elegoo | 0.130 ± 0.008 | 0.115–0.144 | ||
| eSUN | 0.120 ± 0.004 | 0.114–0.127 | ||
| Phrozen | 0.135 ± 0.008 | 0.122–0.149 | ||
| Connector | Anycubic | 0.118 ± 0.006 | 0.109–0.130 | <0.001 *** |
| Elegoo | 0.129 ± 0.005 | 0.121–0.137 | ||
| eSUN | 0.125 ± 0.004 | 0.119–0.133 | ||
| Phrozen | 0.132 ± 0.006 | 0.123–0.143 |
| Design | Resin Group | Mean ± SD | Min–Max | p-Value |
|---|---|---|---|---|
| Support | Anycubic | 0.137 ± 0.008 | 0.122–0.148 | <0.001 *** |
| Elegoo | 0.149 ± 0.007 | 0.136–0.158 | ||
| eSUN | 0.143 ± 0.005 | 0.136–0.153 | ||
| Phrozen | 0.119 ± 0.007 | 0.104–0.130 | ||
| Extended | Anycubic | 0.108 ± 0.010 | 0.089–0.125 | <0.001 *** |
| Elegoo | 0.135 ± 0.016 | 0.113–0.159 | ||
| eSUN | 0.106 ± 0.008 | 0.092–0.119 | ||
| Phrozen | 0.119 ± 0.024 | 0.080–0.157 | ||
| Connector | Anycubic | 0.094 ± 0.006 | 0.082–0.103 | <0.001 *** |
| Elegoo | 0.121 ± 0.005 | 0.112–0.128 | ||
| eSUN | 0.101 ± 0.006 | 0.092–0.111 | ||
| Phrozen | 0.103 ± 0.009 | 0.089–0.118 |
| Resin | Design | Test Used | p-Value (Sig.) |
|---|---|---|---|
| Anycubic | Support | Paired t-test | 0.4902 (ns) |
| Anycubic | Extended | Paired t-test | 0.0586 (ns) |
| Anycubic | Connector | Paired t-test | <0.001 (***) |
| Elegoo | Support | Paired t-test | 0.5798 (ns) |
| Elegoo | Extended | Paired t-test | 0.1595 (ns) |
| Elegoo | Connector | Wilcoxon signed-rank | <0.001 (***) |
| eSUN | Support | Paired t-test | <0.001 (***) |
| eSUN | Extended | Paired t-test | <0.001 (***) |
| eSUN | Connector | Paired t-test | <0.001 (***) |
| Phrozen | Support | Paired t-test | <0.001 (***) |
| Phrozen | Extended | Wilcoxon signed-rank | 0.0105 (*) |
| Phrozen | Connector | Paired t-test | <0.001 (***) |
| Resin Group | N | Mean | SD | Median | IQR |
|---|---|---|---|---|---|
| Anycubic | 30 | 0.074 | 0.113 | 0.050 | 0.019 |
| Elegoo | 30 | 0.086 | 0.132 | 0.061 | 0.021 |
| eSUN | 30 | 0.047 | 0.012 | 0.043 | 0.018 |
| Phrozen | 30 | 0.073 | 0.091 | 0.052 | 0.025 |
| Resin Group | N | Mean | SD | Min | Max |
|---|---|---|---|---|---|
| Anycubic | 30 | 0.055 | 0.011 | 0.032 | 0.086 |
| Elegoo | 30 | 0.059 | 0.013 | 0.036 | 0.093 |
| eSUN | 30 | 0.049 | 0.010 | 0.034 | 0.077 |
| Phrozen | 30 | 0.053 | 0.013 | 0.031 | 0.079 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bor, S.; Oğuz, F. Effect of Different Printing Designs and Resin Types on the Accuracy of Orthodontic Model. Polymers 2025, 17, 2724. https://doi.org/10.3390/polym17202724
Bor S, Oğuz F. Effect of Different Printing Designs and Resin Types on the Accuracy of Orthodontic Model. Polymers. 2025; 17(20):2724. https://doi.org/10.3390/polym17202724
Chicago/Turabian StyleBor, Sabahattin, and Fırat Oğuz. 2025. "Effect of Different Printing Designs and Resin Types on the Accuracy of Orthodontic Model" Polymers 17, no. 20: 2724. https://doi.org/10.3390/polym17202724
APA StyleBor, S., & Oğuz, F. (2025). Effect of Different Printing Designs and Resin Types on the Accuracy of Orthodontic Model. Polymers, 17(20), 2724. https://doi.org/10.3390/polym17202724









