Caseload per Year in Robotic-Assisted Minimally Invasive Esophagectomy: A Narrative Review
Abstract
Simple Summary
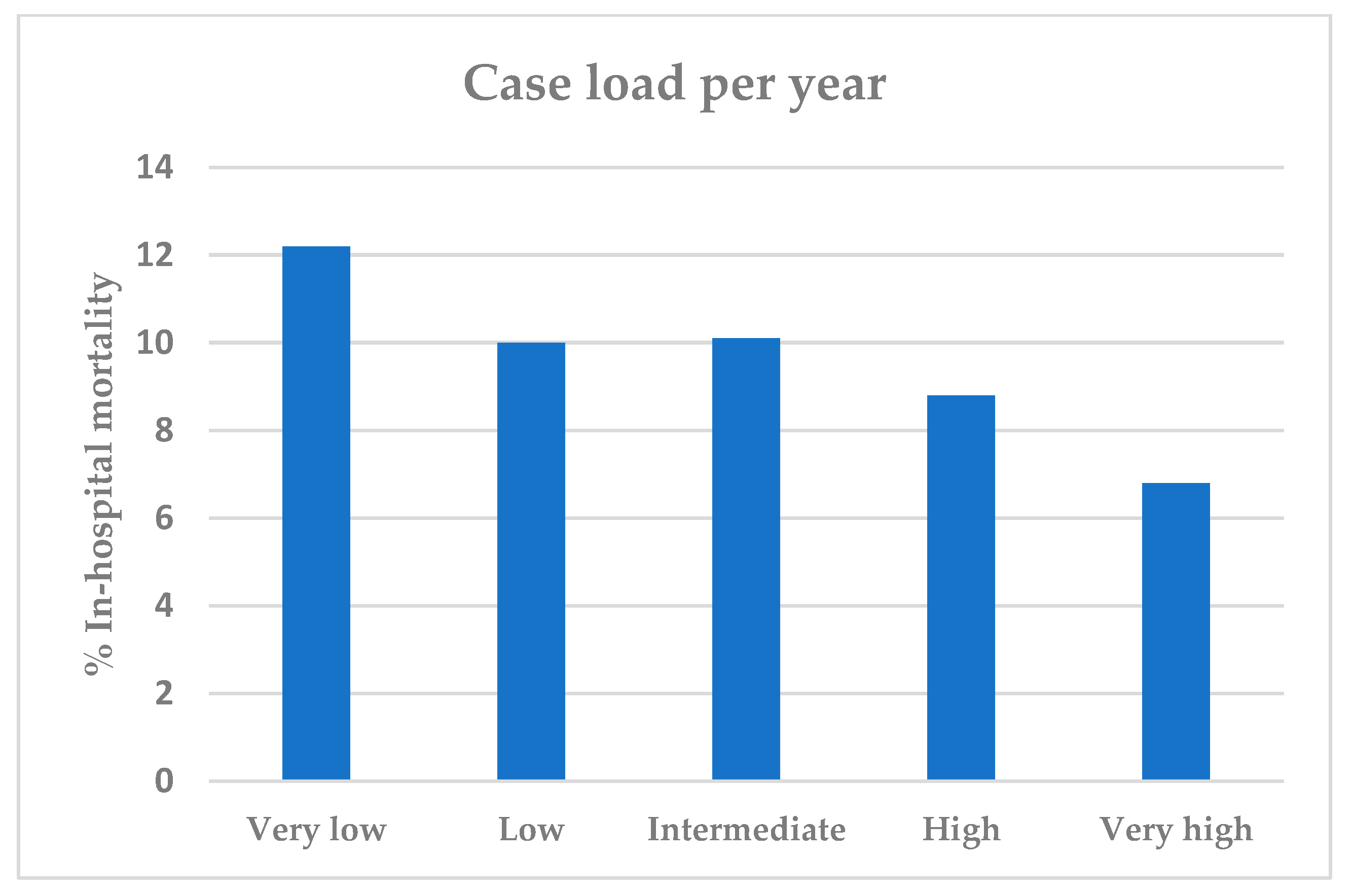
Abstract
1. Introduction
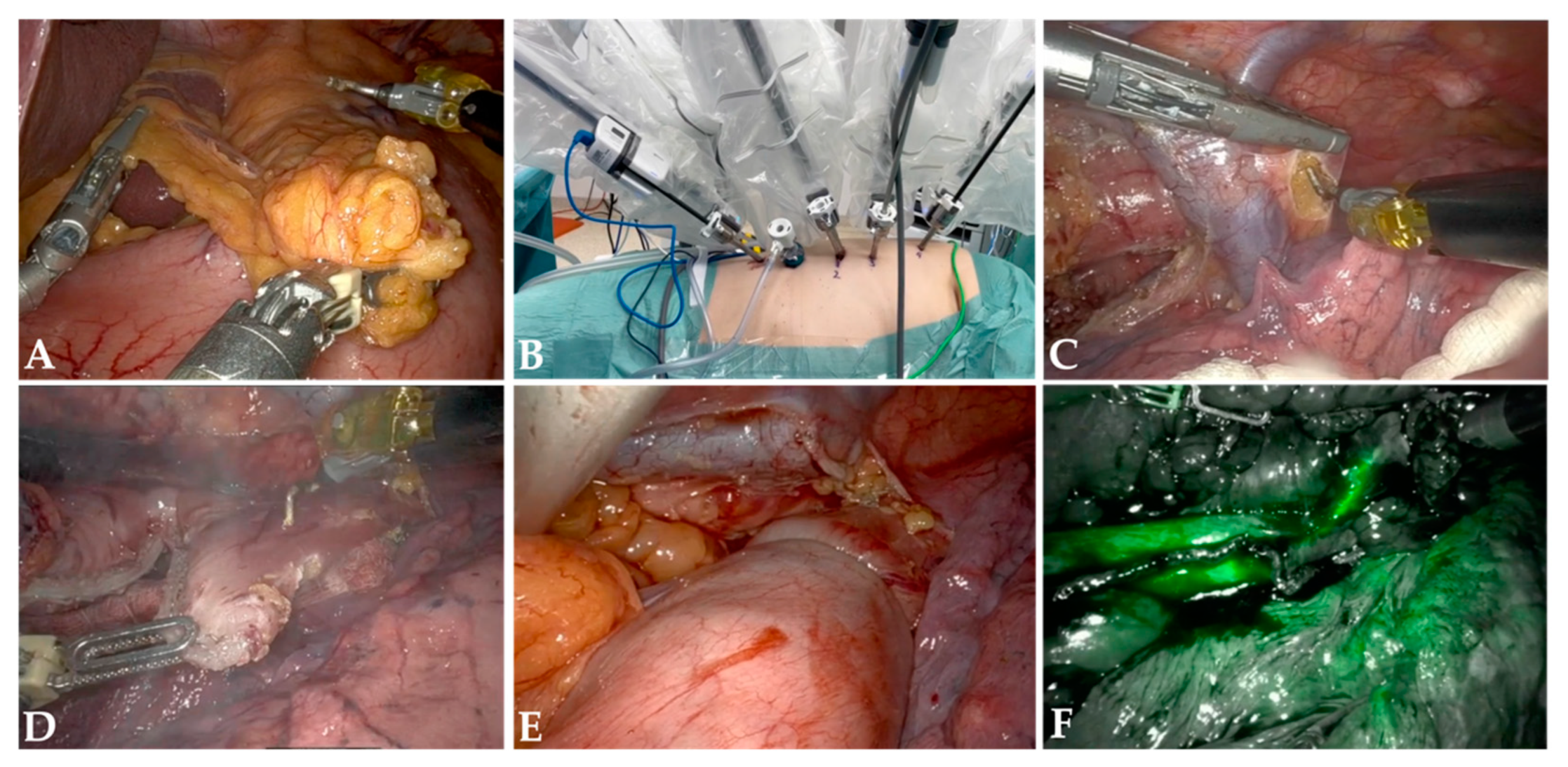
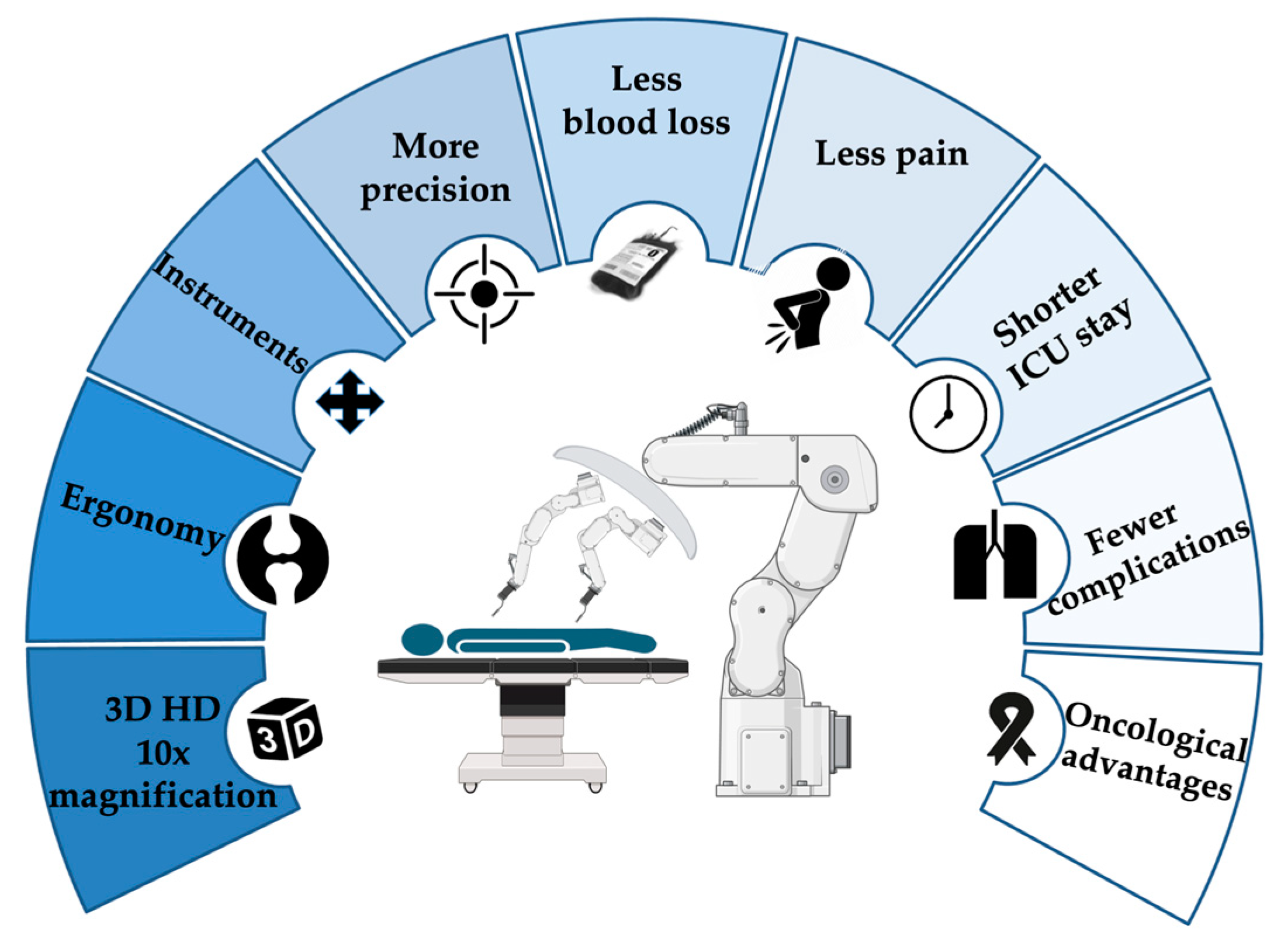
2. Rationale for RAMIE
3. Caseload Requirements Across Europe
4. Quality and Complication Management
4.1. Quality Management
4.2. Complication Management
5. Influence of Caseload on Surgical Performance, Training, and Learning Curves in RAMIE
6. Conclusions
7. Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Baum, P.; Diers, J.; Lichthardt, S.; Kastner, C.; Schlegel, N.; Germer, C.-T.; Wiegering, A. Mortality and complications following visceral surgery: A nationwide analysis based on the diagnostic categories used in German hospital invoicing data. Dtsch. Ärzteblatt Int. 2019, 116, 739. [Google Scholar]
- Pieper, D.; Mathes, T.; Neugebauer, E.; Eikermann, M. State of evidence on the relationship between high-volume hospitals and outcomes in surgery: A systematic review of systematic reviews. J. Am. Coll. Surg. 2013, 216, 1015–1025.e18. [Google Scholar] [CrossRef] [PubMed]
- Nimptsch, U.; Haist, T.; Krautz, C.; Grützmann, R.; Mansky, T.; Lorenz, D. Hospital volume, in-hospital mortality, and failure to rescue in esophageal surgery: An analysis of german hospital discharge data. Dtsch. Ärzteblatt Int. 2018, 115, 793. [Google Scholar]
- Schoffer, O.; Roessler, M.; Bierbaum, V. Wirksamkeit der Versorgung in Onkologischen Zentren (WiZen), Gemeinsamer Bundesausschuss, Berlin. 2022. Available online: https://innovationsfonds.g-ba.de/downloads/beschluss-dokumente/268/2022-10-17_WiZen_Ergebnisbericht.pdf (accessed on 21 July 2024).
- Bundesausschuss, G. Regelungen des Gemeinsamen Bundesausschusses Gemäß § 136b Absatz 1 Satz 1 Nummer 2 SGB V für nach § 108 SGB V zugelassene Krankenhäuser Berlin. 2023. Available online: https://www.g-ba.de/downloads/62-492-3365/Mm-R_2023-12-21_iK-2024-02-15.pdf (accessed on 20 July 2024).
- IQTIG. Folgenabschätzungen zu Mindestmengen Komplexe Eingriffe am Organsystem Ösophagus. 2020. Available online: https://iqtig.org/downloads/berichte/2020/IQTIG_Folgenabschaetzungen-Mm_OEsophagus_Ergaenzungsauftrag_2020-12-15_barrierefrei.pdf (accessed on 20 July 2024).
- Amtlicher Teil des Bundesanzeigers. Beschluss des Gemeinsamen Bundesausschusses über eine Änderung der Mindestmengenregelungen: Änderung der Nr. 3 der Anlage. 2021. Available online: https://www.g-ba.de/downloads/39-261-4622/2020-12-17_Mm-R_Oesophagus_BAnz.pdf (accessed on 20 July 2024).
- AOK Bundesverband. Mindestmengen-Transparenzliste 2024. Bundesweit. 2023. Available online: https://www.aok.de/pp/hintergrund/mindestmengen/mindestmengen-transparenzkarte-2024/ (accessed on 12 September 2024).
- Baum, P.; Lenzi, J.; Diers, J.; Rust, C.; Eichhorn, M.E.; Taber, S.; Germer, C.-T.; Winter, H.; Wiegering, A. Risk-adjusted mortality rates as a quality proxy outperform volume in surgical oncology—A new perspective on hospital centralization using national population-based data. J. Clin. Oncol. 2022, 40, 1041–1050. [Google Scholar] [CrossRef] [PubMed]
- Turner, M.; Fielding, S.; Ong, Y.; Dibben, C.; Feng, Z.; Brewster, D.H.; Black, C.; Lee, A.; Murchie, P. A cancer geography paradox? Poorer cancer outcomes with longer travelling times to healthcare facilities despite prompter diagnosis and treatment: A data-linkage study. Br. J. Cancer 2017, 117, 439–449. [Google Scholar] [CrossRef]
- Iness, A.N.; Abaricia, J.O.; Sawadogo, W.; Iness, C.M.; Duesberg, M.; Cyrus, J.; Prasad, V. The effect of hospital visitor policies on patients, their visitors, and health care providers during the COVID-19 pandemic: A systematic review. Am. J. Med. 2022, 135, 1158–1167.e3. [Google Scholar] [CrossRef]
- Lang, H.; Grimminger, P.P.; Meyer, H.-J. Mindestmengenregelungen in der Chirurgie aus Sicht der Fachgesellschaft (DGCH). Der Chir. 2022, 93, 342–348. [Google Scholar] [CrossRef]
- Nüssler, N.C.; Klier, T.; Ruppert, R. Mindestmengen aus der Sicht einer Klinik der Schwerpunktversorgung. Der Chir. 2022, 93, 356–361. [Google Scholar] [CrossRef]
- Schardey, J.; Huber, T.; Kappenberger, A.S.; Horné, F.; Beger, N.; Weniger, M.; Werner, J.; Kühn, F.; Wirth, U. Erwartete Effekte der neuen Weiterbildungsordnung in der Allgemein-und Viszeralchirurgie. Die Chir. 2023, 94, 155–163. [Google Scholar] [CrossRef]
- Grimminger, P.; Fuchs, H. Minimal-invasive und robotisch assistierte Operationstechniken in der onkologischen Magen-und Ösophaguschirurgie. Der Chir. 2017, 88, 1017. [Google Scholar] [CrossRef]
- Hoelzen, J.P.; Fortmann, L.; Roy, D.; Szardenings, C.; Holstein, M.; Eichelmann, A.-K.; Rijcken, E.; Frankauer, B.E.; Barth, P.; Wardelmann, E. Robotic-assisted esophagectomy with total mesoesophageal excision enhances R0-resection in patients with esophageal cancer: A single-center experience. Surgery 2024, 176, 721–729. [Google Scholar] [CrossRef]
- Kingma, B.F.; Hadzijusufovic, E.; Van der Sluis, P.C.; Bano, E.; Lang, H.; Ruurda, J.P.; van Hillegersberg, R.; Grimminger, P.P. A structured training pathway to implement robot-assisted minimally invasive esophagectomy: The learning curve results from a high-volume center. Dis. Esophagus 2020, 33, doaa047. [Google Scholar] [CrossRef] [PubMed]
- Boone, J.; Schipper, M.E.I.; Moojen, W.A.; Borel Rinkes, I.H.M.; Cromheecke, G.J.E.; van Hillegersberg, R. Robot-assisted thoracoscopic oesophagectomy for cancer. Br. J. Surg. 2009, 96, 878–886. [Google Scholar] [CrossRef] [PubMed]
- van der Sluis, P.C.; Ruurda, J.P.; Verhage, R.J.J.; van der Horst, S.; Haverkamp, L.; Siersema, P.D.; Borel Rinkes, I.H.M.; ten Kate, F.J.W.; van Hillegersberg, R. Oncologic Long-Term Results of Robot-Assisted Minimally Invasive Thoraco-Laparoscopic Esophagectomy with Two-Field Lymphadenectomy for Esophageal Cancer. Ann. Surg. Oncol. 2015, 22, 1350–1356. [Google Scholar] [CrossRef] [PubMed]
- Merboth, F.; Distler, M.; Weitz, J. Robotische Ösophaguschirurgie. Die Chir. 2023, 94, 812–820. [Google Scholar] [CrossRef]
- Manigrasso, M.; Vertaldi, S.; Marello, A.; Antoniou, S.A.; Francis, N.K.; De Palma, G.D.; Milone, M. Robotic esophagectomy. A systematic review with meta-analysis of clinical outcomes. J. Pers. Med. 2021, 11, 640. [Google Scholar] [CrossRef]
- Wee, I.J.Y.; Kuo, L.J.; Ngu, J.C. A systematic review of the true benefit of robotic surgery: Ergonomics. Int. J. Med. Robot. 2020, 16, e2113. [Google Scholar] [CrossRef]
- Whelehan, D.F.; Brown, D.J.; Connelly, T.M.; Ridgway, P.F. Fatigued surgeons: A thematic analysis of the causes, effects and opportunities for fatigue mitigation in surgery. Int. J. Surg. Open 2021, 35, 100382. [Google Scholar] [CrossRef]
- Kingma, B.F.; Grimminger, P.P.; van der Sluis, P.C.; van Det, M.J.; Kouwenhoven, E.A.; Chao, Y.-K.; Tsai, C.-Y.; Fuchs, H.F.; Bruns, C.J.; Sarkaria, I.S. Worldwide techniques and outcomes in robot-assisted minimally invasive esophagectomy (RAMIE): Results from the multicenter international registry. Ann. Surg. 2022, 276, e386–e392. [Google Scholar] [CrossRef]
- Hoelzen, J.P.; Sander, K.J.; Sesia, M.; Roy, D.; Rijcken, E.; Schnabel, A.; Struecker, B.; Juratli, M.A.; Pascher, A. Robotic-assisted esophagectomy leads to significant reduction in postoperative acute pain: A retrospective clinical trial. Ann. Surg. Oncol. 2022, 29, 7498–7509. [Google Scholar] [CrossRef]
- Tagkalos, E.; Van Der Sluis, P.; Berlth, F.; Poplawski, A.; Hadzijusufovic, E.; Lang, H.; van Berge Henegouwen, M.; Gisbertz, S.; Müller-Stich, B.P.; Ruurda, J.P. Robot-assisted minimally invasive thoraco-laparoscopic esophagectomy versus minimally invasive esophagectomy for resectable esophageal adenocarcinoma, a randomized controlled trial (ROBOT-2 trial). BMC Cancer 2021, 21, 1060. [Google Scholar] [CrossRef] [PubMed]
- Siaw-Acheampong, K.; Kamarajah, S.; Gujjuri, R.; Bundred, J.; Singh, P.; Griffiths, E. Minimally invasive techniques for transthoracic oesophagectomy for oesophageal cancer: Systematic review and network meta-analysis. BJS Open 2020, 4, 787–803. [Google Scholar] [CrossRef] [PubMed]
- Suda, K.; Ishida, Y.; Kawamura, Y.; Inaba, K.; Kanaya, S.; Teramukai, S.; Satoh, S.; Uyama, I. Robot-assisted thoracoscopic lymphadenectomy along the left recurrent laryngeal nerve for esophageal squamous cell carcinoma in the prone position: Technical report and short-term outcomes. World J. Surg. 2012, 36, 1608–1616. [Google Scholar] [CrossRef] [PubMed]
- Weksler, B.; Sharma, P.; Moudgill, N.; Chojnacki, K.; Rosato, E. Robot-assisted minimally invasive esophagectomy is equivalent to thoracoscopic minimally invasive esophagectomy. Dis. Esophagus 2012, 25, 403–409. [Google Scholar] [CrossRef]
- Park, S.; Hwang, Y.; Lee, H.J.; Park, I.K.; Kim, Y.T.; Kang, C.H. Comparison of robot-assisted esophagectomy and thoracoscopic esophagectomy in esophageal squamous cell carcinoma. J. Thorac. Dis. 2016, 8, 2853. [Google Scholar] [CrossRef]
- He, H.; Wu, Q.; Wang, Z.; Zhang, Y.; Chen, N.; Fu, J.; Zhang, G. Short-term outcomes of robot-assisted minimally invasive esophagectomy for esophageal cancer: A propensity score matched analysis. J. Cardiothorac. Surg. 2018, 13, 52. [Google Scholar] [CrossRef]
- Chao, Y.K.; Hsieh, M.J.; Liu, Y.H.; Liu, H.P. Lymph node evaluation in robot-assisted versus video-assisted thoracoscopic esophagectomy for esophageal squamous cell carcinoma: A propensity-matched analysis. World J. Surg. 2018, 42, 590–598. [Google Scholar] [CrossRef]
- Deng, H.; Luo, J.; Li, S.; Li, G.; Alai, G.; Wang, Y.; Liu, L.; Lin, Y. Does robot-assisted minimally invasive esophagectomy really have the advantage of lymphadenectomy over video-assisted minimally invasive esophagectomy in treating esophageal squamous cell carcinoma? A propensity score-matched analysis based on short-term outcomes. Dis. Esophagus 2019, 32, doy110. [Google Scholar]
- Tagkalos, E.; Goense, L.; Hoppe-Lotichius, M.; Ruurda, J.; Babic, B.; Hadzijusufovic, E.; Kneist, W.; Van Der Sluis, P.; Lang, H.; Van Hillegersberg, R. Robot-assisted minimally invasive esophagectomy (RAMIE) compared to conventional minimally invasive esophagectomy (MIE) for esophageal cancer: A propensity-matched analysis. Dis. Esophagus 2020, 33, doz060. [Google Scholar] [CrossRef]
- Zhang, Y.; Han, Y.; Gan, Q.; Xiang, J.; Jin, R.; Chen, K.; Che, J.; Hang, J.; Li, H. Early outcomes of robot-assisted versus thoracoscopic-assisted Ivor Lewis esophagectomy for esophageal cancer: A propensity score-matched study. Ann. Surg. Oncol. 2019, 26, 1284–1291. [Google Scholar] [CrossRef]
- Chen, J.; Liu, Q.; Zhang, X.; Yang, H.; Tan, Z.; Lin, Y.; Fu, J. Comparisons of short-term outcomes between robot-assisted and thoraco-laparoscopic esophagectomy with extended two-field lymph node dissection for resectable thoracic esophageal squamous cell carcinoma. J. Thorac. Dis. 2019, 11, 3874. [Google Scholar] [CrossRef] [PubMed]
- Motoyama, S.; Sato, Y.; Wakita, A.; Kawakita, Y.; Nagaki, Y.; Imai, K.; Minamiya, Y. Extensive lymph node dissection around the left laryngeal nerve achieved with robot-assisted thoracoscopic esophagectomy. Anticancer Res. 2019, 39, 1337–1342. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Zhang, X.; Li, B.; Hua, R.; Yang, Y.; He, Y.; Ye, B.; Guo, X.; Sun, Y.; Li, Z. Short-and mid-term outcomes of robotic versus thoraco-laparoscopic McKeown esophagectomy for squamous cell esophageal cancer: A propensity score-matched study. Dis. Esophagus 2020, 33, doz080. [Google Scholar] [CrossRef] [PubMed]
- Harbison, G.J.; Vossler, J.D.; Yim, N.H.; Murayama, K.M. Outcomes of robotic versus non-robotic minimally-invasive esophagectomy for esophageal cancer: An American College of Surgeons NSQIP database analysis. Am. J. Surg. 2019, 218, 1223–1228. [Google Scholar]
- Babic, B.; Müller, D.T.; Jung, J.-O.; Schiffmann, L.M.; Grisar, P.; Schmidt, T.; Chon, S.-H.; Schröder, W.; Bruns, C.J.; Fuchs, H.F. Robot-assisted minimally invasive esophagectomy (RAMIE) vs. hybrid minimally invasive esophagectomy: Propensity score matched short-term outcome analysis of a European high-volume center. Surg. Endosc. 2022, 36, 7747–7755. [Google Scholar] [CrossRef]
- Tsunoda, S.; Obama, K.; Hisamori, S.; Nishigori, T.; Okamura, R.; Maekawa, H.; Sakai, Y. Lower Incidence of Postoperative Pulmonary Complications Following Robot-Assisted Minimally Invasive Esophagectomy for Esophageal Cancer: Propensity Score-Matched Comparison to Conventional Minimally Invasive Esophagectomy. Ann. Surg. Oncol. 2021, 28, 639–647. [Google Scholar] [CrossRef]
- Hoelzen, J.P.; Frankauer, B.E.; Szardenings, C.; Roy, D.; Pollmann, L.; Fortmann, L.; Merten, J.; Rijcken, E.; Juratli, M.A.; Pascher, A. Reducing the Risks of Esophagectomies: A Retrospective Comparison of Hybrid versus Full-Robotic-Assisted Minimally Invasive Esophagectomy (RAMIE) Approaches. J. Clin. Med. 2023, 12, 5823. [Google Scholar] [CrossRef]
- Burns, P.B.; Rohrich, R.J.; Chung, K.C. The levels of evidence and their role in evidence-based medicine. Plast. Reconstr. Surg. 2011, 128, 305–310. [Google Scholar] [CrossRef]
- van der Sluis, P.C.; van der Horst, S.; May, A.M.; Schippers, C.; Brosens, L.A.A.; Joore, H.C.A.; Kroese, C.C.; Haj Mohammad, N.; Mook, S.; Vleggaar, F.P.; et al. Robot-assisted Minimally Invasive Thoracolaparoscopic Esophagectomy Versus Open Transthoracic Esophagectomy for Resectable Esophageal Cancer: A Randomized Controlled Trial. Ann. Surg. 2019, 269, 621–630. [Google Scholar] [CrossRef]
- Banks, K.C.; Hsu, D.S.; Velotta, J.B. Outcomes of minimally invasive and robot-assisted esophagectomy for esophageal cancer. Cancers 2022, 14, 3667. [Google Scholar] [CrossRef]
- Harriott, C.B.; Angeramo, C.A.; Casas, M.A.; Schlottmann, F. Open versus hybrid versus totally minimally invasive Ivor Lewis esophagectomy: Systematic review and meta-analysis. J. Thorac. Cardiovasc. Surg. 2022, 164, e233–e254. [Google Scholar] [CrossRef] [PubMed]
- Perry, R.; Barbosa, J.P.; Perry, I.; Barbosa, J. Short-term outcomes of robot-assisted versus conventional minimally invasive esophagectomy for esophageal cancer: A systematic review and meta-analysis of 18,187 patients. J. Robot. Surg. 2024, 18, 125. [Google Scholar] [CrossRef] [PubMed]
- Esagian, S.M.; Ziogas, I.A.; Skarentzos, K.; Katsaros, I.; Tsoulfas, G.; Molena, D.; Karamouzis, M.V.; Rouvelas, I.; Nilsson, M.; Schizas, D. Robot-Assisted Minimally Invasive Esophagectomy versus Open Esophagectomy for Esophageal Cancer: A Systematic Review and Meta-Analysis. Cancers 2022, 14, 3177. [Google Scholar] [CrossRef]
- Na, K.J.; Kang, C.H.; Park, S.; Park, I.K.; Kim, Y.T. Robotic esophagectomy versus open esophagectomy in esophageal squamous cell carcinoma: A propensity-score matched analysis. J. Robot. Surg. 2022, 16, 841–848. [Google Scholar] [CrossRef] [PubMed]
- Andreou, A.; Biebl, M.; Struecker, B.; Chopra, S.S.; Denecke, C.; Thuss-Patience, P.C.; Sturm, P.; Sauer, I.M.; Bahra, M.; Pratschke, J. Laparoscopic Surgery Increases Return to Intended Oncologic Treatment after Resection for Gastric and Esophageal Cancer and Improves Outcomes. J. Am. Coll. Surg. 2016, 223, e46–e47. [Google Scholar] [CrossRef]
- Pointer Jr, D.T.; Felder, S.I.; Powers, B.D.; Dessureault, S.; Sanchez, J.A.; Imanirad, I.; Sahin, I.; Xie, H.; Naffouje, S.A. Return to intended oncologic therapy after colectomy for stage III colon adenocarcinoma: Does surgical approach matter? Color. Dis. 2023, 25, 1760–1770. [Google Scholar] [CrossRef]
- Liu, Q.; Li, M.; Gao, Y.; Jiang, T.; Han, B.; Zhao, G.; Lin, C.; Lau, W.Y.; Zhao, Z.; Liu, R. Effect of robotic versus open pancreaticoduodenectomy on postoperative length of hospital stay and complications for pancreatic head or periampullary tumours: A multicentre, open-label randomised controlled trial. Lancet Gastroenterol. Hepatol. 2024, 9, 428–437. [Google Scholar] [CrossRef]
- Association of Surgeons of the Netherlands (NVvH). Normering Chirurgische Behandelingen 3.0. 2012. Available online: https://heelkunde.nl/themas/thema?dossierid=688148&title=Normering (accessed on 21 July 2024).
- Dikken, J.L.; Dassen, A.E.; Lemmens, V.E.P.; Putter, H.; Krijnen, P.; van der Geest, L.; Bosscha, K.; Verheij, M.; van de Velde, C.J.H.; Wouters, M.W.J.M. Effect of hospital volume on postoperative mortality and survival after oesophageal and gastric cancer surgery in the Netherlands between 1989 and 2009. Eur. J. Cancer 2012, 48, 1004–1013. [Google Scholar] [CrossRef]
- Dikken, J.L.; van Sandick, J.W.; Allum, W.H.; Johansson, J.; Jensen, L.S.; Putter, H.; Coupland, V.H.; Wouters, M.W.J.M.; Lemmens, V.E.P.; van de Velde, C.J.H. Differences in outcomes of oesophageal and gastric cancer surgery across Europe. Br. J. Surg. 2012, 100, 83–94. [Google Scholar] [CrossRef]
- Fuchs, H.F.; Harnsberger, C.R.; Broderick, R.C.; Chang, D.C.; Sandler, B.J.; Jacobsen, G.R.; Bouvet, M.; Horgan, S. Mortality after esophagectomy is heavily impacted by center volume: Retrospective analysis of the Nationwide Inpatient Sample. Surg. Endosc. 2017, 31, 2491–2497. [Google Scholar] [CrossRef]
- Jensen, L.S.; Parvaiz, I.; Utzon, J.; Andersen, K.B.; Olsen, P.S.; Kehlet, H. Esophageal resections in Denmark 1997–2000. Ugeskr. Læger 2002, 164, 4423–4427. [Google Scholar] [PubMed]
- Ketel, M.H.; Klarenbeek, B.R.; Abma, I.; Belgers, E.H.; Coene, P.-P.L.; Dekker, J.W.T.; Van Duijvendijk, P.; Emous, M.; Gisbertz, S.S.; Haveman, J.W. Nationwide Association of Surgical Performance of Minimally Invasive Esophagectomy with Patient Outcomes. JAMA Netw. Open 2024, 7, e246556. [Google Scholar] [CrossRef] [PubMed]
- Kjaer, D.W.; Larsson, H.; Svendsen, L.B.; Jensen, L.S. Changes in treatment and outcome of oesophageal cancer in Denmark between 2004 and 2013. Br. J. Surg. 2017, 104, 1338–1345. [Google Scholar] [CrossRef] [PubMed]
- Milstein, A.; Galvin, R.; Delbanco, S.; Salber, P.; Buck, C., Jr. Improving the safety of health care: The leapfrog initiative. Eff. Clin. Pract. 2000, 3, 6. [Google Scholar]
- Varagunam, M.; Hardwick, R.; Riley, S.; Chadwick, G.; Cromwell, D.; Groene, O. Changes in volume, clinical practice and outcome after reorganisation of oesophago-gastric cancer care in England: A longitudinal observational study. Eur. J. Surg. Oncol. 2018, 44, 524–531. [Google Scholar] [CrossRef]
- Varghese Jr, T.K.; Wood, D.E.; Farjah, F.; Oelschlager, B.K.; Symons, R.G.; MacLeod, K.E.; Flum, D.R.; Pellegrini, C.A. Variation in esophagectomy outcomes in hospitals meeting Leapfrog volume outcome standards. Ann. Thorac. Surg. 2011, 91, 1003–1010. [Google Scholar] [CrossRef]
- Kroneman, M.; Boerma, W.; van den Berg, M.; Groenewegen, P.; de Jong, J.; van Ginneken, E. Netherlands: Health System Review. Health Syst. Transit. 2016, 18, 1–240. [Google Scholar]
- Magnussen, J.; Martinussen, P.E. From Centralization to Decentralization, and Back: Norwegian Health Care in a Nordic Perspective. In Federalism and Decentralization in European Health and Social Care; Costa-Font, J., Greer, S.L., Eds.; Palgrave Macmillan UK: London, UK, 2013; pp. 101–120. [Google Scholar]
- Hue, J.J.; Bachman, K.C.; Worrell, S.G.; Gray, K.E.; Linden, P.A.; Towe, C.W. Outcomes of robotic esophagectomies for esophageal cancer by hospital volume: An analysis of the national cancer database. Surg. Endosc. 2021, 35, 3802–3810. [Google Scholar] [CrossRef]
- Di, J.; Lu, X.-S.; Sun, M.; Zhao, Z.-M.; Zhang, C.-D. Hospital volume-mortality association after esophagectomy for cancer: A systematic review and meta-analysis. Int. J. Surg. 2024, 110, 3021–3029. [Google Scholar] [CrossRef]
- Birkmeyer, J.D.; Stukel, T.A.; Siewers, A.E.; Goodney, P.P.; Wennberg, D.E.; Lucas, F.L. Surgeon volume and operative mortality in the United States. N. Engl. J. Med. 2003, 349, 2117–2127. [Google Scholar] [CrossRef]
- Hoag, J.R.; Resio, B.J.; Monsalve, A.F.; Chiu, A.S.; Brown, L.B.; Herrin, J.; Blasberg, J.D.; Kim, A.W.; Boffa, D.J. Differential safety between top-ranked cancer hospitals and their affiliates for complex cancer surgery. JAMA Netw. Open 2019, 2, e191912. [Google Scholar] [CrossRef] [PubMed]
- Oshikiri, T.; Nakamura, T.; Hasegawa, H.; Yamamoto, M.; Kanaji, S.; Yamashita, K.; Matsuda, T.; Sumi, Y.; Fujino, Y.; Tominaga, M.; et al. Standardizing procedures improves and homogenizes short-term outcomes after minimally invasive esophagectomy. Langenbeck’s Arch. Surg. 2018, 403, 221–234. [Google Scholar] [CrossRef]
- Peters, A.K.; Juratli, M.A.; Roy, D.; Merten, J.; Fortmann, L.; Pascher, A.; Hoelzen, J.P. Factors Influencing Postoperative Complications Following Minimally Invasive Ivor Lewis Esophagectomy: A Retrospective Cohort Study. J. Clin. Med. 2023, 12, 5688. [Google Scholar] [CrossRef] [PubMed]
- El-Sourani, N.; Miftode, S.; Bockhorn, M. Endoscopic vacuum therapy for anastomotic leakage after esophagectomy: A retrospective analysis at a tertiary university center. Surg. Open Sci. 2023, 11, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Gao, Y.; Chang, R.; Juma, A.N.; Chen, W.; Zhang, C. Analysis of risk factors and classification of aortic fistula after esophagectomy. J. Surg. Res. 2018, 229, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Okamura, A.; Watanabe, M.; Fukudome, I.; Yamashita, K.; Yuda, M.; Hayami, M.; Imamura, Y.; Mine, S. Surgical team proficiency in minimally invasive esophagectomy is related to case volume and improves patient outcomes. Esophagus 2018, 15, 115–121. [Google Scholar] [CrossRef]
- Prasad, P.; Wallace, L.; Navidi, M.; Phillips, A.W. Learning curves in minimally invasive esophagectomy: A systematic review and evaluation of benchmarking parameters. Surgery 2022, 171, 1247–1256. [Google Scholar] [CrossRef]
- Vijayakumar, A.; Abdel-Rasoul, M.; Hekmat, R.; Merritt, R.E.; D’Souza, D.M.; Jackson, G.P.; Kneuertz, P.J. National learning curves among robotic thoracic surgeons in the United States: Quantifying the impact of procedural experience on efficiency and productivity gains. J. Thorac. Cardiovasc. Surg. 2024, 167, 869–879.e2. [Google Scholar] [CrossRef]
- van Workum, F.; Fransen, L.; Luyer, M.D.; Rosman, C. Learning curves in minimally invasive esophagectomy. World J. Gastroenterol. 2018, 24, 4974–4978. [Google Scholar] [CrossRef]
- Schmidt, T.; Babic, B.; Bruns, C.J.; Fuchs, H.F. Chirurgische Therapie des Ösophaguskarzinoms–neue Technologien, moderne Konzepte. Der Chir. Z. Fur Alle Geb. Der Oper. Medizen 2021, 92, 1100. [Google Scholar] [CrossRef]
- Mehta, A.; Ng, J.C.; Awuah, W.A.; Huang, H.; Kalmanovich, J.; Agrawal, A.; Abdul-Rahman, T.; Hasan, M.M.; Sikora, V.; Isik, A. Embracing robotic surgery in low-and middle-income countries: Potential benefits, challenges, and scope in the future. Ann. Med. Surg. 2022, 84, 104803. [Google Scholar] [CrossRef] [PubMed]
- Müller, D.T.; Brunner, S.; Straatman, J.; Babic, B.; Eckhoff, J.A.; Reisewitz, A.; Storms, C.; Schiffmann, L.M.; Schmidt, T.; Schröder, W. Analysis of training pathway to reach expert performance levels based on proficiency-based progression in robotic-assisted minimally invasive esophagectomy (RAMIE). Surg. Endosc. 2023, 37, 7305–7316. [Google Scholar] [CrossRef] [PubMed]
- Pickering, O.J.; van Boxel, G.I.; Carter, N.C.; Mercer, S.J.; Knight, B.C.; Pucher, P.H. Learning curve for adoption of robot-assisted minimally invasive esophagectomy: A systematic review of oncological, clinical, and efficiency outcomes. Dis. Esophagus 2023, 36, doac089. [Google Scholar] [CrossRef] [PubMed]
- van der Sluis, P.C.; Ruurda, J.P.; van der Horst, S.; Goense, L.; van Hillegersberg, R. Learning Curve for Robot-Assisted Minimally Invasive Thoracoscopic Esophagectomy: Results from 312 Cases. Ann. Thorac. Surg. 2018, 106, 264–271. [Google Scholar] [CrossRef]
- Hernandez, J.M.; Dimou, F.; Weber, J.; Almhanna, K.; Hoffe, S.; Shridhar, R.; Karl, R.; Meredith, K. Defining the Learning Curve for Robotic-assisted Esophagogastrectomy. J. Gastrointest. Surg. 2013, 17, 1346–1351. [Google Scholar] [CrossRef]
| Author | Year | Country | Complications (%, RAMIE vs. MIE) | |||
|---|---|---|---|---|---|---|
| Pulmonary | RN Injury | Anastomotic Leak | Chyle Leak | |||
| Suda [28] | 2012 | Japan | 6 vs. 20 | 38 vs. 75 | 38 vs. 10 | 0 vs. 10 |
| Weksler [29] | 2012 | USA | 9.1 vs. 15 | 9.1 vs. 3.8 | 9.1 vs. 15 | NA |
| Park [30] | 2016 | Korea | 13 vs. 24 | 8.1 vs. 2.3 | NA | 7.6 vs. 1.6 |
| He [31] | 2018 | China | 19 vs. 7.4 | 15 vs. 11 | 11 vs. 3.7 | 0 vs. 3.7 |
| Chao [32] | 2018 | Taiwan | 5.9 vs. 18 | 21 vs. 29 | 0 vs. 5.9 | NA |
| Deng [33] | 2019 | China | 9.6 vs. 7.7 | 14 vs. 7.7 | 5.8 vs. 3.8 | 0 vs. 1.9 |
| Tagkalos [34] | 2019 | Germany | 12 vs. 18 | NA | 12 vs. 18 | NA |
| Zhang [35] | 2019 | China | 6.1 vs. 7.6 | 6.1 vs. 4.5 | 7.6 vs. 4.5 | 0 vs. 1.5 |
| Chen [36] | 2019 | China | 15 vs. 24 | 13 vs. 32 | 9.3 vs. 3.7 | 1.9 vs. 3.7 |
| Motoyama [37] | 2019 | Japan | 0 vs. 0 | 24 vs. 47 | 5 vs. 8 | 5 vs. 3 |
| Yang [38] | 2019 | China | 8.9 vs. 13 | 29 vs. 15 | 12 vs. 14 | 1.5 vs. 0.7 |
| Harbison [39] | 2019 | USA | 11 vs. 19 | NA | 14 vs. 15 | 3 vs. 2.2 |
| Babic [40] | 2021 | Germany | 8.5 vs. 8.5 | NA | 7.9 vs. 11 | NA |
| Tsunoda [41] | 2021 | Japan | 18 vs. 44 | 7 vs. 20 | 18 vs. 18 | NA |
| Kingma [24] | 2022 | The Netherlands, Germany, Taiwan, USA, France, Hong Kong, Brazil, UK, Italy | 25 vs. 33 | 2 vs. 6 | 20 vs. 22 | 5 vs. 6 |
| Hoelzen [42] | 2023 | Germany | 7.6 vs. 20.6 | NA | 14.2 vs. 22.2 | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Büdeyri, I.; El-Sourani, N.; Eichelmann, A.-K.; Merten, J.; Juratli, M.A.; Pascher, A.; Hoelzen, J.P. Caseload per Year in Robotic-Assisted Minimally Invasive Esophagectomy: A Narrative Review. Cancers 2024, 16, 3538. https://doi.org/10.3390/cancers16203538
Büdeyri I, El-Sourani N, Eichelmann A-K, Merten J, Juratli MA, Pascher A, Hoelzen JP. Caseload per Year in Robotic-Assisted Minimally Invasive Esophagectomy: A Narrative Review. Cancers. 2024; 16(20):3538. https://doi.org/10.3390/cancers16203538
Chicago/Turabian StyleBüdeyri, Ibrahim, Nader El-Sourani, Ann-Kathrin Eichelmann, Jennifer Merten, Mazen A. Juratli, Andreas Pascher, and Jens P. Hoelzen. 2024. "Caseload per Year in Robotic-Assisted Minimally Invasive Esophagectomy: A Narrative Review" Cancers 16, no. 20: 3538. https://doi.org/10.3390/cancers16203538
APA StyleBüdeyri, I., El-Sourani, N., Eichelmann, A.-K., Merten, J., Juratli, M. A., Pascher, A., & Hoelzen, J. P. (2024). Caseload per Year in Robotic-Assisted Minimally Invasive Esophagectomy: A Narrative Review. Cancers, 16(20), 3538. https://doi.org/10.3390/cancers16203538






