Plant-Based Diets and Metabolic Syndrome Components: The Questions That Still Need to Be Answered—A Narrative Review
Abstract
1. Introduction
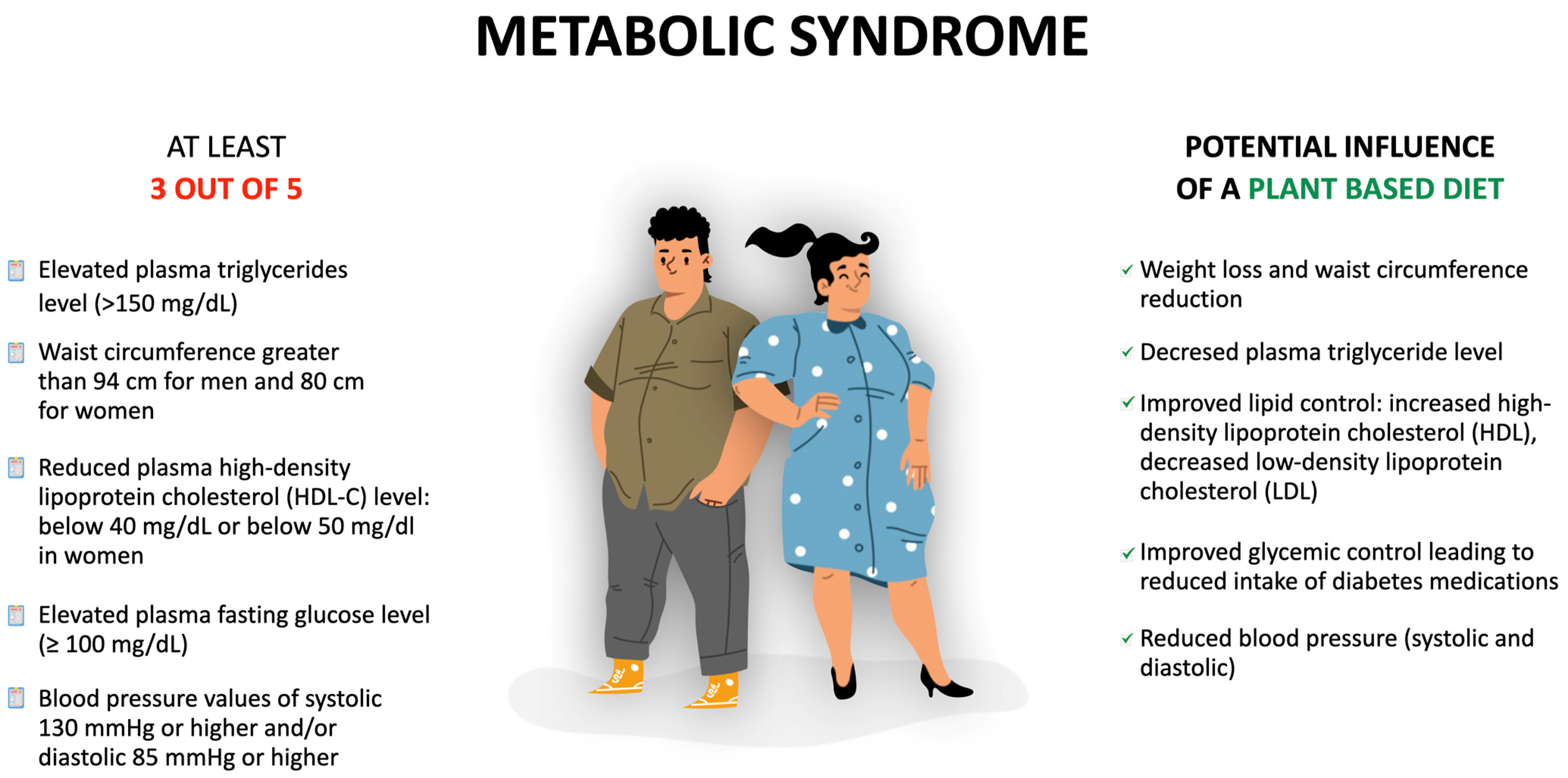
- Waist circumference exceeding 94 cm in men and 80 cm in women;
- High plasma triglycerides level—at least 150 mg/dL;
- Lowered plasma high-density lipoprotein cholesterol (HDL-C) level—less than 40 mg/dL in men or less than 50 mg/dL in women;
- Fasting plasma glucose level of at least l00 mg/dL;
- Systolic blood pressure (SBP) of at least 130 mmHg and/or diastolic blood pressure (DBP) of at least 85 mmHg.
2. The Context: What Do We Know about Plant-Based Diets and Their Potential Effects on Metabolic Syndrome Components?
2.1. Plant Based Diet Characteristics
2.2. PBDs Potential Effects on the Components of MetS
2.2.1. Waist Circumference and Body Mass
2.2.2. Lipid Metabolism
2.2.3. Blood Pressure
2.2.4. Glycemia
3. Plant-Based Diets and Their Influence on Metabolic Syndrome Indices—Current Evidence from RCTs Studies
4. Future Perspective
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AHA | American Heart Association |
| BMI | Body Mass Index |
| CI | Confidence interval |
| DASH | Dietary Approaches to Stop Hypertension |
| DBP | Diastolic blood pressure |
| HbA1c | Glycated hemoglobin |
| HDL-C | High-density lipoprotein |
| LDL-C | Low-density lipoprotein |
| MetS | Metabolic Syndrome |
| NCDs | Non-communicable chronic diseases |
| PBDs | Plant-based diets |
| RCTs | Randomized controlled trials |
| SBP | Systolic blood pressure |
| T2DM | Type 2 diabetes mellitus |
| WFPB | Whole-food plant-based diet |
References
- Jia, P.; Shi, Y.; Jiang, Q.; Dai, S.; Yu, B.; Yang, S.; Qiu, G.; Yang, S. Environmental Determinants of Childhood Obesity: A Meta-Analysis. Lancet Glob. Health 2023, 11, S7. [Google Scholar] [CrossRef] [PubMed]
- Dixon, B.N.; Ugwoaba, U.A.; Brockmann, A.N.; Ross, K.M. Associations between the Built Environment and Dietary Intake, Physical Activity, and Obesity: A Scoping Review of Reviews. Obes. Rev. 2021, 22, e13171. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Ng, S.W. The Nutrition Transition to a Stage of High Obesity and Noncommunicable Disease Prevalence Dominated by Ultra-Processed Foods Is Not Inevitable. Obes. Rev. 2022, 23, e13366. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.T.; Loria, C.M.; Smith, S.C. Harmonizing the Metabolic Syndrome: A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; And International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [PubMed]
- Noubiap, J.J.; Nansseu, J.R.; Lontchi-Yimagou, E.; Nkeck, J.R.; Nyaga, U.F.; Ngouo, A.T.; Tounouga, D.N.; Tianyi, F.-L.; Foka, A.J.; Ndoadoumgue, A.L.; et al. Geographic Distribution of Metabolic Syndrome and Its Components in the General Adult Population: A Meta-Analysis of Global Data from 28 Million Individuals. Diabetes Res. Clin. Pract. 2022, 188, 109924. [Google Scholar] [CrossRef]
- Hirode, G.; Wong, R.J. Trends in the Prevalence of Metabolic Syndrome in the United States, 2011–2016. JAMA 2020, 323, 2526–2528. [Google Scholar] [CrossRef]
- Fahed, G.; Aoun, L.; Zerdan, M.B.; Allam, S.; Zerdan, M.B.; Bouferraa, Y.; Assi, H.I. Metabolic Syndrome: Updates on Pathophysiology and Management in 2021. Int. J. Mol. Sci. 2022, 23, 786. [Google Scholar] [CrossRef]
- Tylutka, A.; Morawin, B.; Walas, Ł.; Michałek, M.; Gwara, A.; Zembron-Lacny, A. Assessment of Metabolic Syndrome Predictors in Relation to Inflammation and Visceral Fat Tissue in Older Adults. Sci. Rep. 2023, 13, 89. [Google Scholar] [CrossRef]
- van Namen, M.; Prendergast, L.; Peiris, C. Supervised Lifestyle Intervention for People with Metabolic Syndrome Improves Outcomes and Reduces Individual Risk Factors of Metabolic Syndrome: A Systematic Review and Meta-Analysis. Metabolism 2019, 101, 153988. [Google Scholar] [CrossRef]
- Peiris, C.L.; van Namen, M.; O’Donoghue, G. Education-Based, Lifestyle Intervention Programs with Unsupervised Exercise Improve Outcomes in Adults with Metabolic Syndrome. A Systematic Review and Meta-Analysis. Rev. Endocr. Metab. Disord. 2021, 22, 877–890. [Google Scholar] [CrossRef]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT–Lancet Commission on Healthy Diets from Sustainable Food Systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef] [PubMed]
- Hemler, E.C.; Hu, F.B. Plant-Based Diets for Personal, Population, and Planetary Health. Adv. Nutr. 2019, 10, S275–S283. [Google Scholar] [CrossRef] [PubMed]
- Weston, L.J.; Kim, H.; Talegawkar, S.A.; Tucker, K.L.; Correa, A.; Rebholz, C.M. Plant-Based Diets and Incident Cardiovascular Disease and All-Cause Mortality in African Americans: A Cohort Study. PLoS Med. 2022, 19, e1003863. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, J.; Cappuccio, F.P. Plant-Based Dietary Patterns for Human and Planetary Health. Nutrients 2022, 14, 1614. [Google Scholar] [CrossRef]
- Andersen, C.J.; Fernandez, M.L. Dietary Strategies to Reduce Metabolic Syndrome. Rev. Endocr. Metab. Disord. 2013, 14, 241–254. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Martínez, P.; Mikhailidis, D.P.; Athyros, V.G.; Bullo, M.; Couture, P.; Covas, M.I.; de Koning, L.; Delgado-Lista, J.; Díaz-López, A.; Drevon, C.A.; et al. Lifestyle Recommendations for the Prevention and Management of Metabolic Syndrome: An International Panel Recommendation. Nutr. Rev. 2017, 75, 307–326. [Google Scholar] [CrossRef] [PubMed]
- Farhadnejad, H.; Emamat, H.; Teymoori, F.; Tangestani, H.; Hekmatdoost, A.; Mirmiran, P. Role of Dietary Approaches to Stop Hypertension Diet in Risk of Metabolic Syndrome: Evidence from Observational and Interventional Studies. Int. J. Prev. Med. 2021, 12, 24. [Google Scholar] [PubMed]
- Steckhan, N.; Hohmann, C.D.; Kessler, C.; Dobos, G.; Michalsen, A.; Cramer, H. Effects of Different Dietary Approaches on Inflammatory Markers in Patients with Metabolic Syndrome: A Systematic Review and Meta-Analysis. Nutrition 2016, 32, 338–348. [Google Scholar] [CrossRef]
- Papadaki, A.; Nolen-Doerr, E.; Mantzoros, C.S. The Effect of the Mediterranean Diet on Metabolic Health: A Systematic Review and Meta-Analysis of Controlled Trials in Adults. Nutrients 2020, 12, 3342. [Google Scholar] [CrossRef]
- Calton, E.K.; James, A.P.; Pannu, P.K.; Soares, M.J. Certain Dietary Patterns Are Beneficial for the Metabolic Syndrome: Reviewing the Evidence. Nutr. Res. 2014, 34, 559–568. [Google Scholar] [CrossRef]
- Cubas-Basterrechea, G.; Elío, I.; Alonso, G.; Otero, L.; Gutiérrez-Bardeci, L.; Puente, J.; Muñoz-Cacho, P. Adherence to the Mediterranean Diet Is Inversely Associated with the Prevalence of Metabolic Syndrome in Older People from the North of Spain. Nutrients 2022, 14, 4536. [Google Scholar] [CrossRef] [PubMed]
- Melina, V.; Craig, W.; Levin, S. Position of the Academy of Nutrition and Dietetics: Vegetarian Diets. J. Acad. Nutr. Diet. 2016, 116, 1970–1980. [Google Scholar] [CrossRef] [PubMed]
- Messina, V.K.; Burke, K.I. Position of the American Dietetic Association: Vegetarian Diets. J. Am. Diet. Assoc. 2009, 109, 1266–1282. [Google Scholar] [CrossRef]
- Figueroa, C.; Echeverría, G.; Villarreal, G.; Martínez, X.; Ferreccio, C.; Rigotti, A. Introducing Plant-Based Mediterranean Diet as a Lifestyle Medicine Approach in Latin America: Opportunities within the Chilean Context. Front. Nutr. 2021, 8, 680452. [Google Scholar] [CrossRef] [PubMed]
- Quarta, S.; Massaro, M.; Chervenkov, M.; Ivanova, T.; Dimitrova, D.; Jorge, R.; Andrade, V.; Philippou, E.; Zisimou, C.; Maksimova, V.; et al. Persistent Moderate-to-Weak Mediterranean Diet Adherence and Low Scoring for Plant-Based Foods across Several Southern European Countries: Are We Overlooking the Mediterranean Diet Recommendations? Nutrients 2021, 13, 1432. [Google Scholar] [CrossRef]
- Hargreaves, S.M.; Rosenfeld, D.L.; Moreira, A.V.B.; Zandonadi, R.P. Plant-Based and Vegetarian Diets: An Overview and Definition of These Dietary Patterns. Eur. J. Nutr. 2023, 62, 1109–1121. [Google Scholar] [CrossRef]
- Zhang, S.; Xu, M.; Zhang, W.; Liu, C.; Chen, S. Natural Polyphenols in Metabolic Syndrome: Protective Mechanisms and Clinical Applications. Int. J. Mol. Sci. 2021, 22, 6110. [Google Scholar] [CrossRef]
- Kent, G.; Kehoe, L.; Flynn, A.; Walton, J. Plant-Based Diets: A Review of the Definitions and Nutritional Role in the Adult Diet. Proc. Nutr. Soc. 2022, 81, 62–74. [Google Scholar] [CrossRef]
- Oncina-Cánovas, A.; Vioque, J.; González-Palacios, S.; Martínez-González, M.Á.; Salas-Salvadó, J.; Corella, D.; Zomeño, D.; Martínez, J.A.; Alonso-Gómez, Á.M.; Wärnberg, J.; et al. Pro-Vegetarian Food Patterns and Cardiometabolic Risk in the PREDIMED-Plus Study: A Cross-Sectional Baseline Analysis. Eur. J. Nutr. 2022, 61, 357–372. [Google Scholar] [CrossRef]
- Wang, D.D.; Li, Y.; Nguyen, X.M.T.; Song, R.J.; Ho, Y.L.; Hu, F.B.; Willett, W.C.; Wilson, P.; Cho, K.; Gaziano, J.M.; et al. Degree of Adherence to Plant-Based Diet and Total and Cause-Specific Mortality: Prospective Cohort Study in the Million Veteran Program. Public Health Nutr. 2023, 26, 381–392. [Google Scholar] [CrossRef]
- Parker, H.W.; Vadiveloo, M.K. Diet Quality of Vegetarian Diets Compared with Nonvegetarian Diets: A Systematic Review. Nutr. Rev. 2019, 77, 144–160. [Google Scholar] [CrossRef] [PubMed]
- Fontes, T.; Rodrigues, L.M.; Ferreira-Pêgo, C. Comparison between Different Groups of Vegetarianism and Its Associations with Body Composition: A Literature Review from 2015 to 2021. Nutrients 2022, 14, 1853. [Google Scholar] [CrossRef]
- Churuangsuk, C.; Hall, J.; Reynolds, A.; Griffin, S.J.; Combet, E.; Lean, M.E.J. Diets for Weight Management in Adults with Type 2 Diabetes: An Umbrella Review of Published Meta-Analyses and Systematic Review of Trials of Diets for Diabetes Remission. Diabetologia 2022, 65, 14–36. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Wang, J.; Chen, S.; Wei, Z.; Li, Z.; Zhao, S.; Lu, W. Comparison of Vegetarian Diets and Omnivorous Diets on Plasma Level of HDL-c: A Meta-Analysis. PLoS ONE 2014, 9, e92609. [Google Scholar] [CrossRef] [PubMed]
- Barnard, N.D.; Levin, S.M.; Yokoyama, Y. A Systematic Review and Meta-Analysis of Changes in Body Weight in Clinical Trials of Vegetarian Diets. J. Acad. Nutr. Diet. 2015, 115, 954–969. [Google Scholar] [CrossRef] [PubMed]
- Turner-McGrievy, G.M.; Davidson, C.R.; Wingard, E.E.; Wilcox, S.; Frongillo, E.A. Comparative Effectiveness of Plant-Based Diets for Weight Loss: A Randomized Controlled Trial of Five Different Diets. Nutrition 2015, 31, 350–358. [Google Scholar] [CrossRef]
- Saintila, J.; Lozano López, T.E.; Ruiz Mamani, P.G.; White, M.; Huancahuire-Vega, S. Health-Related Quality of Life, Blood Pressure, and Biochemical and Anthropometric Profile in Vegetarians and Nonvegetarians. J. Nutr. Metab. 2020, 2020, 3629742. [Google Scholar] [CrossRef]
- Jakše, B.; Jakše, B.; Godnov, U.; Pinter, S. Nutritional, Cardiovascular Health and Lifestyle Status of ‘Health Conscious’ Adult Vegans and Non-Vegans from Slovenia: A Cross-Sectional Self-Reported Survey. Int. J. Environ. Res. Public Health 2021, 18, 5968. [Google Scholar] [CrossRef]
- Kahleova, H.; Fleeman, R.; Hlozkova, A.; Holubkov, R.; Barnard, N.D. A Plant-Based Diet in Overweight Individuals in a 16-Week Randomized Clinical Trial: Metabolic Benefits of Plant Protein. Nutr. Diabetes 2018, 8, 58. [Google Scholar] [CrossRef]
- Kahleova, H.; Tura, A.; Hill, M.; Holubkov, R.; Barnard, N.D. A Plant-Based Dietary Intervention Improves Beta-Cell Function and Insulin Resistance in Overweight Adults: A 16-Week Randomized Clinical Trial. Nutrients 2018, 10, 189. [Google Scholar] [CrossRef]
- Kahleova, H.; Rembert, E.; Alwarith, J.; Yonas, W.N.; Tura, A.; Holubkov, R.; Agnello, M.; Chutkan, R.; Barnard, N.D. Effects of a Low-Fat Vegan Diet on Gut Microbiota in Overweight Individuals and Relationships with Body Weight, Body Composition, and Insulin Sensitivity. A Randomized Clinical Trial. Nutrients 2020, 12, 2917. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.Y.; Huang, C.C.; Hu, F.B.; Chavarro, J.E. Vegetarian Diets and Weight Reduction: A Meta-Analysis of Randomized Controlled Trials. J. Gen. Intern. Med. 2016, 31, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Shah, B.; Newman, J.D.; Woolf, K.; Ganguzza, L.; Guo, Y.; Allen, N.; Zhong, J.; Fisher, E.A.; Slater, J. Anti-Inflammatory Effects of a Vegan Diet versus the American Heart Association–Recommended Diet in Coronary Artery Disease Trial. J. Am. Heart Assoc. 2018, 7, e011367. [Google Scholar] [CrossRef] [PubMed]
- Melgar, B.; Diaz-Arocutipa, C.; Huerta-Rengifo, C.; Piscoya, A.; Barboza, J.J.; Hernandez, A. V Vegetarian Diets on Anthropometric, Metabolic and Blood Pressure Outcomes in People with Overweight and Obesity: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Obes. 2023, 47, 903–910. [Google Scholar] [CrossRef]
- Pieters, M.; Swanepoel, A.C. The Effect of Plant-based Diets on Thrombotic Risk Factors. Pol. Arch. Intern. Med. 2021, 131, 16123. [Google Scholar] [CrossRef]
- Najjar, R.S.; Feresin, R.G. Plant-Based Diets in the Reduction of Body Fat: Physiological Effects and Biochemical Insights. Nutrients 2019, 11, 2712. [Google Scholar] [CrossRef]
- Sofi, F.; Dinu, M.; Pagliai, G.; Cesari, F.; Gori, A.M.; Sereni, A.; Becatti, M.; Fiorillo, C.; Marcucci, R.; Casini, A. Low-Calorie Vegetarian versus Mediterranean Diets for Reducing Body Weight and Improving Cardiovascular Risk Profile. Circulation 2018, 137, 1103–1113. [Google Scholar] [CrossRef]
- Del Re, A.; Aspry, K. Update on Plant-Based Diets and Cardiometabolic Risk. Curr. Atheroscler. Rep. 2022, 24, 173–183. [Google Scholar] [CrossRef]
- Termannsen, A.D.; Clemmensen, K.K.B.; Thomsen, J.M.; Nørgaard, O.; Díaz, L.J.; Torekov, S.S.; Quist, J.S.; Færch, K. Effects of Vegan Diets on Cardiometabolic Health: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Obes. Rev. 2022, 23, e13462. [Google Scholar] [CrossRef]
- Jenkins, D.J.A.; Wong, J.M.; Kendall, C.W.C.; Esfahani, A.; Ng, V.W.Y.; Leong, T.C.K.; Faulkner, D.A.; Vidgen, E.; Paul, G.; Mukherjea, R.; et al. Effect of a 6-Month Vegan Low-Carbohydrate (‘Eco-Atkins’) Diet on Cardiovascular Risk Factors and Body Weight in Hyperlipidaemic Adults: A Randomised Controlled Trial. BMJ Open 2014, 4, 3505. [Google Scholar] [CrossRef]
- Koch, C.A.; Kjeldsen, E.W.; Frikke-Schmidt, R. Vegetarian or Vegan Diets and Blood Lipids: A Meta-Analysis of Randomized Trials. Eur. Heart J. 2023, 44, 2609–2622. [Google Scholar] [CrossRef] [PubMed]
- Yokoyama, Y.; Levin, S.M.; Barnard, N.D. Association between Plant-Based Diets and Plasma Lipids: A Systematic Review and Meta-Analysis. Nutr. Rev. 2017, 75, 683–698. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Zheng, J.; Yang, B.; Jiang, J.; Fu, Y.; Li, D. Effects of Vegetarian Diets on Blood Lipids: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Am. Heart Assoc. 2015, 4, e002408. [Google Scholar] [CrossRef] [PubMed]
- Nardocci, M.; Polsky, J.Y.; Moubarac, J.C. Consumption of Ultra-Processed Foods Is Associated with Obesity, Diabetes and Hypertension in Canadian Adults. Can. J. Public Health 2021, 112, 421–429. [Google Scholar] [CrossRef] [PubMed]
- Filippini, T.; Malavolti, M.; Whelton, P.K.; Vinceti, M. Sodium Intake and Risk of Hypertension: A Systematic Review and Dose–Response Meta-Analysis of Observational Cohort Studies. Curr. Hypertens. Rep. 2022, 24, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, J.; Gaskin, E.; Ji, C.; Miller, M.A.; Cappuccio, F.P. The Effect of Plant-Based Dietary Patterns on Blood Pressure: A Systematic Review Andmeta-Analysis of Controlled Intervention Trials. J. Hypertens. 2021, 39, 23–37. [Google Scholar] [CrossRef]
- Dybvik, J.S.; Svendsen, M.; Aune, D. Vegetarian and Vegan Diets and the Risk of Cardiovascular Disease, Ischemic Heart Disease and Stroke: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Eur. J. Nutr. 2023, 62, 51–69. [Google Scholar] [CrossRef]
- Kahleova, H.; Levin, S.; Barnard, N. Cardio-Metabolic Benefits of Plant-Based Diets. Nutrients 2017, 9, 848. [Google Scholar] [CrossRef]
- van Nielen, M.; Feskens, E.J.M.; Rietman, A.; Siebelink, E.; Mensink, M. Partly Replacing Meat Protein with Soy Protein Alters Insulin Resistance and Blood Lipids in Postmenopausal Women with Abdominal Obesity. J. Nutr. 2014, 144, 1423–1429. [Google Scholar] [CrossRef]
- Belinova, L.; Kahleova, H.; Malinska, H.; Topolcan, O.; Vrzalova, J.; Oliyarnyk, O.; Kazdova, L.; Hill, M.; Pelikanova, T. Differential Acute Postprandial Effects of Processed Meat and Isocaloric Vegan Meals on the Gastrointestinal Hormone Response in Subjects Suffering from Type 2 Diabetes and Healthy Controls: A Randomized Crossover Study. PLoS ONE 2014, 9, e107561. [Google Scholar] [CrossRef]
- Klementova, M.; Thieme, L.; Haluzik, M.; Pavlovicova, R.; Hill, M.; Pelikanova, T.; Kahleova, H. A Plant-Based Meal Increases Gastrointestinal Hormones and Satiety More than an Energy-and Macronutrient-Matched Processed-Meat Meal in T2d, Obese, and Healthy Men: A Three-Group Randomized Crossover Study. Nutrients 2019, 11, 157. [Google Scholar] [CrossRef] [PubMed]
- Åberg, S.; Mann, J.; Neumann, S.; Ross, A.B.; Reynolds, A.N. Whole-Grain Processing and Glycemic Control in Type 2 Diabetes: A Randomized Crossover Trial. Diabetes Care 2020, 43, 1717–1723. [Google Scholar] [CrossRef] [PubMed]
- Thomas, M.S.; Puglisi, M.; Malysheva, O.; Caudill, M.A.; Sholola, M.; Cooperstone, J.L.; Fernandez, M.L. Eggs Improve Plasma Biomarkers in Patients with Metabolic Syndrome Following a Plant-Based Diet—A Randomized Crossover Study. Nutrients 2022, 14, 2138. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.; Xu, J.; Agarwal, U.; Gonzales, J.; Levin, S.; Barnard, N.D. A Multicenter Randomized Controlled Trial of a Plant-Based Nutrition Program to Reduce Body Weight and Cardiovascular Risk in the Corporate Setting: The GEICO Study. Eur. J. Clin. Nutr. 2013, 67, 718–724. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.M.; Kim, S.A.; Lee, I.K.; Kim, J.G.; Park, K.G.; Jeong, J.Y.; Jeon, J.H.; Shin, J.Y.; Lee, D.H. Effect of a Brown Rice Based Vegan Diet and Conventional Diabetic Diet on Glycemic Control of Patients with Type 2 Diabetes: A 12-Week Randomized Clinical Trial. PLoS ONE 2016, 11, e0155918. [Google Scholar] [CrossRef] [PubMed]
- Wright, N.; Wilson, L.; Smith, M.; Duncan, B.; McHugh, P. The BROAD Study: A Randomised Controlled Trial Using a Whole Food Plant-Based Diet in the Community for Obesity, Ischaemic Heart Disease or Diabetes. Nutr. Diabetes 2017, 7, e256. [Google Scholar] [CrossRef]
- Crosby, L.; Rembert, E.; Levin, S.; Green, A.; Ali, Z.; Jardine, M.; Nguyen, M.; Elliott, P.; Goldstein, D.; Freeman, A.; et al. Changes in Food and Nutrient Intake and Diet Quality on a Low-Fat Vegan Diet Are Associated with Changes in Body Weight, Body Composition, and Insulin Sensitivity in Overweight Adults: A Randomized Clinical Trial. J. Acad. Nutr. Diet. 2022, 122, 1922–1939. [Google Scholar] [CrossRef]
- Derbyshire, E.J. Flexitarian Diets and Health: A Review of the Evidence-Based Literature. Front. Nutr. 2017, 3, 55. [Google Scholar] [CrossRef]
- Chidambaram, A.G.; Josephson, M. Clinical Research Study Designs: The Essentials. Pediatr. Investig. 2019, 3, 245–252. [Google Scholar] [CrossRef]
- Bakaloudi, D.R.; Halloran, A.; Rippin, H.L.; Oikonomidou, A.C.; Dardavesis, T.I.; Williams, J.; Wickramasinghe, K.; Breda, J.; Chourdakis, M. Intake and Adequacy of the Vegan Diet. A Systematic Review of the Evidence. Clin. Nutr. 2021, 40, 3503–3521. [Google Scholar] [CrossRef]
- Wang, T.; Masedunskas, A.; Willett, W.C.; Fontana, L. Vegetarian and Vegan Diets: Benefits and Drawbacks. Eur. Heart J. 2023, 44, 3423–3439. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wiśniewska, K.; Okręglicka, K.M.; Nitsch-Osuch, A.; Oczkowski, M. Plant-Based Diets and Metabolic Syndrome Components: The Questions That Still Need to Be Answered—A Narrative Review. Nutrients 2024, 16, 165. https://doi.org/10.3390/nu16010165
Wiśniewska K, Okręglicka KM, Nitsch-Osuch A, Oczkowski M. Plant-Based Diets and Metabolic Syndrome Components: The Questions That Still Need to Be Answered—A Narrative Review. Nutrients. 2024; 16(1):165. https://doi.org/10.3390/nu16010165
Chicago/Turabian StyleWiśniewska, Klaudia, Katarzyna Małgorzata Okręglicka, Aneta Nitsch-Osuch, and Michał Oczkowski. 2024. "Plant-Based Diets and Metabolic Syndrome Components: The Questions That Still Need to Be Answered—A Narrative Review" Nutrients 16, no. 1: 165. https://doi.org/10.3390/nu16010165
APA StyleWiśniewska, K., Okręglicka, K. M., Nitsch-Osuch, A., & Oczkowski, M. (2024). Plant-Based Diets and Metabolic Syndrome Components: The Questions That Still Need to Be Answered—A Narrative Review. Nutrients, 16(1), 165. https://doi.org/10.3390/nu16010165







