Abstract
The relationship between diet, sleep duration and cardiovascular disease (CVD) has not been well understood. The aim of the present study was to test the potential modifying role of sleep duration in the association between adherence to the Mediterranean-type diet (MD) and CVD risk. The study consisted of n = 313 initially free-of-CVD adults, from the ATTICA cohort study (2002–2022), with available information on sleep habits. Sleep habits were categorized as inadequate and adequate sleep duration (< or ≥7 h/day, respectively). In multi-adjusted analysis, MD adherence was inversely associated with CVD risk [Hazard Ratio-HR per 1/55 in MedDietScore: 0.80, 95% Confidence Interval-CI: 0.65, 0.98]. A significant interaction between sleep duration and MedDietScore was observed (p < 0.001). In subgroup analysis, the protective association between MD adherence and CVD risk was found only in participants who slept adequately, i.e., >7 h/day [HR:0.80, 95%CI: 0.65, 0.98]. Those who had a high adherence to the MD along with adequate sleep habits, had a 70% reduced 20-year CVD risk [HR:0.30, 95%CI: 0.11, 0.80], compared to those who had a low MD adherence and inadequate sleep habits. Sleep duration should be a part of an individual’s lifestyle, together with dietary and other habits, to effectively evaluate CVD risk for future events.
1. Introduction
The relationship between cardiovascular disease (CVD) and the Mediterranean type diet (MD) has been well documented and established in the literature, and has been of interest for the last 60 years [1,2]. Organizations both inside and outside the Mediterranean region, such as the European Society of Cardiology (ESC) and the American Heart Association/American College of Cardiology (AHA/ACC), recommend following a MD or similar diet to prevent the development of CVD [3,4], despite the current decline in the MD adherence that has been observed worldwide [5,6,7,8,9].
The relationship between sleep and health has also gained interest these past years, and has reached a peak these last two decades [10]. Depending on an individual’s age and lifestyle, sleep habits may vary, but it is estimated that humans spend approximately 1/3 of their lives sleeping [10]. Research suggests that sleep is an essential body function that has multiple benefits for health and especially cardio-metabolic health [10,11,12,13,14]. Specifically, both short and long sleep duration has been positively associated with increased CVD risk, in systematic reviews and meta-analyses [11,14]. Makarem et al. (2022) studied objectively the sleep habits (i.e., evaluated via overnight polysomnography, 7-day wrist actigraphy, and validated questionnaires) of 1920 participants from the multi-ethnic study of atherosclerosis (MESA), and found that the addition of sleep, in cardiovascular health scores (defined and computed based on AHA’s “Simple 7”), improved CVD outcome prediction [12]. Afterwards, sleep was acknowledged as an important lifestyle characteristic for CVD prevention by AHA; sleep was included in AHA’s recommended components for acquiring cardiovascular health and diminishing CVD risk, changing AHA’s “Simple 7”, to the newly adopted “Life’s essential 8” [15,16].
Few studies have associated the adherence to the MD with better sleep habits. It has been proposed that this positive association might be explained through the better management of body weight, via the adoption of MD [17,18,19]. Sleep disorders such as sleep apnea have been associated with increased CVD risk [20]. To the best of our knowledge, the relation among MD, sleep and CVD risk has been studied in only one previous study, by Wang et al., in which they evaluated 23,212 individuals from the National Health and Nutrition Examination Survey (NHANES), and found that lower adherence to a MD in the presence of sleep disorders synergistically increase all-cause and CVD mortality [21]. However, it should be clarified that this study examined only sleep disorders, and not normal sleep habits, in relation to mortality (i.e., all-cause and CVD mortality).
Thus, as the relationship among sleep duration, MD adherence and CVD risk (especially non-fatal CVD events) has not been adequately elucidated, the aim of the present study was to evaluate whether sleep duration could act as a moderator in the relationship between the adherence to the MD and CVD risk (fatal/non-fatal CVD events) in a Mediterranean population.
2. Materials and Methods
2.1. Study Design
The ATTICA study is a prospective cohort study, which started in 2001–2002 (baseline) and afterwards had 3 follow-ups at 5, 10, and 20 years (i.e., 2006, 2012, 2022). The study included 3042 adult men and women, from the Attica region, in Greece (including the capital, Athens). The study aimed to assess socio-demographic, clinical, lifestyle, biochemical, and psychological parameters related to CVD, and to explore the associations between the aforementioned factors and long-term CVD incidence. Participants’ characteristics were assessed through face-to-face interviews with the study’s investigators. Details about the study can be found in previously published papers [22,23,24,25].
2.2. Bioethics
The study was carried out in accordance with the Declaration of Helsinki (1989) of the World Medical Association and was approved by the Institutional Ethics committee of Athens Medical School (#017/1.5.2001). All participants were informed about the study aims and provided written consent to participate in the study.
2.3. Baseline and Follow-Up Measurements
2.3.1. Demographic Characteristics
Demographic characteristics included age, sex, and socio-economic status (SES), which was assessed as a combined measure of mean annual income and education. Participants were categorized as of low SES (i.e., those who had up to 9 years of schooling and low/medium income or up to 14 years of schooling and low income), of high SES (i.e., those who had 15 or more years of schooling and high income or 10–14 years of schooling and very high income) and of middle SES (i.e., the rest of the participants).
2.3.2. Clinical Characteristics
Clinical characteristics, CVD, hypertension, hypercholesterolemia and type 2 diabetes mellitus, were assessed similarly in all evaluations, by study investigators, in a clinical setting, and defined according to WHO-ICD-10 [22].
Briefly, at baseline, biochemical characteristics (glucose and lipids) were measured in 12-h fasting blood samples using chromatographic enzymic method in a Technicon automatic analyzer RA-1000 (Dade Behring, Marburg, Germany) [22]. For the measurements, serum was harvested immediately after admission.
Hypercholesterolemia was defined as TC ≥ 200 mg/dL and/or use of hypocholesterolemic agents [26]. Type 2 diabetes mellitus was based on fasting plasma glucose ≥126 mg/dL or use of antidiabetic drugs [27]. Participants’ arterial blood pressure was measured based on three measurements after a >30 min rest period and while in a sitting position, using a manometric device (ELKA aneroid manometric sphygmometer, Von Schlieben Co., Munich, Germany). Hypertension was defined as an average systolic blood pressure/diastolic blood pressure exceeding 140/90 mmHg or use of antihypertensive drugs [28].
2.3.3. Anthropometric Characteristics
Body weight and height were measured according to standard procedures. Body mass index (BMI) was computed as weight/height2 (kg/m2). According to BMI measurements at 2002 and 2012, participants’ body weight status were categorized as follows: (i) never overweight/obese: those who had a BMI < 25 kg/m2 at both evaluations, (ii) became overweight/obese: those who had a BMI < 25 at 2002, but ≥25 kg/m2 in 2012, (iii) became non-overweight/obese: those who had a BMI ≥ 25 in 2002, but <25 kg/m2 in 2012, and (iv) always overweight/obese: those who had a BMI ≥ 25 kg/m2 at both evaluations.
2.3.4. Lifestyle Habits
Smoking trajectories were evaluated in the 2002 and 2012 examinations, and participants were categorized into (i) never smoked: those who did not smoke at both evaluations, (ii) started smoking: those who did not smoke in 2002, but smoked in 2012, (iii) stopped smoking: those who smoked in 2002, but did not smoke in 2012, (iv) always smoked: those who smoked at both evaluations. According to their physical activity trajectories (2002–2012), evaluated by the International Physical Activity Questionnaire, participants were categorized as follows: (i) always physically inactive: those who did not engage in physical activity at both evaluations, (ii) started physical activity: those who did not engage in physical activity in 2002, but started being physically active in 2012, (iii) stopped physical activity: those who engaged in physical activity in 2002, but did not in 2012, and (iv) always physically active: those who engaged in physical activity at both evaluations.
2.3.5. Dietary Habits
Participants’ dietary habits were assessed through a validated for the Greek population Food Frequency Questionnaire (FFQ) [29]. Adherence to the MD was evaluated through MedDietScore (range: 1–55, with higher values signifying higher adherence) [30]. MedDietScore has 11 components: 7 typical Mediterranean foods/food groups (i.e., fruits, vegetables, whole grains, potatoes, legumes, fish, and olive oil) which are scored on a positive scale (0–5, for very rare to very frequent consumption), 3 non-Mediterranean foods/food groups (full-fat dairy products, poultry, and red meat) which are scored on the opposite scale, and alcohol which is scored on a non-linear scale (0 for consumption of 0 and >7 servings/day, 1 to 5 for consumption of 6–7, 5–6, 4–5, 3–4, and 1–3 servings/day, respectively). Based on participants’ adherence to the MD, 4 trajectories were formed: (i) always close to the MD: median MedDietScore in 2002 and 2012: ≥27, (ii) from close to away: median MedDietScore score in 2002: ≥27, in 2012: <27, (iii) from away to close: median MedDietScore in 2002: <27, in 2012: ≥27, (iv) always away: median MedDietScore value in 2002 and 2012: <27.
2.3.6. Sleep Habits
Sleep habits assessment was conducted in the 2012 examination of the participants. For the purposes of the current study, data on sleep duration (i.e., sleep hours per day) during the past 4 weeks were assessed. Participants were categorized as having inadequate sleep (i.e., those who slept <7 h/day) or adequate sleep (i.e., those who slept ≥7 h/day) [31].
2.4. Study Sample
From the 3042 initially free-of-CVD participants, 2169 were found at the 20-year follow-up. Of them 1988 had complete data on CVD. For details on the ATTICA study participants during 2002–2022 please see Figure 1. However, for the present study, we used a sub-sample of the ATTICA study participants, who had completed a questionnaire on sleep habits during the 10-year follow-up, in 2012 (n = 377). Thus, the sample of the current study was 313 participants who were found at the 20-year follow-up and had complete data on CVD assessment. Differences in the age and sex distribution between this sample and the initial one was not observed (p-value < 0.05).
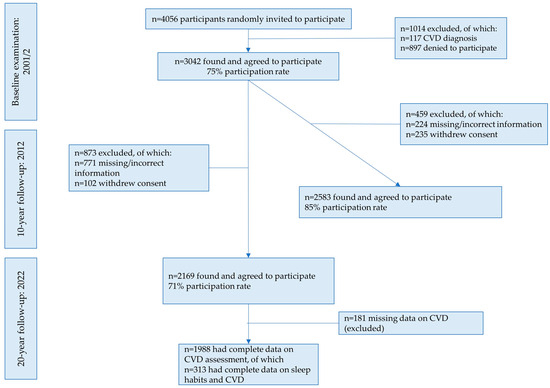
Figure 1.
Flow-chart of the study sample during 2002–2022 (n = 313). Abbreviations: CVD: cardiovascular disease.
This sample was sufficient to obtain a statistical power of 80% or higher to evaluate two-sided statistical hypotheses of hazard ratios of CVD of 1.30 or higher, 0.05 type-I error rate.
2.5. Statistical Analysis
For the statistical analyses, STATA version 17 (STATA Corp, College Station, TX, USA) was used. Categorical variables are presented as frequencies, while continuous variables as mean values ± standard deviation for normally distributed variables (i.e., age) or as median (interquartile range—IQR) for non-normally distributed variables (i.e., MedDietScore at 2002 and 2012). Continuous variables were tested for normality through probability–probability (P-P) plots. Associations between categorical variables were tested using the chi-squared test. After controlling for equality of variances using Levene’s test, comparisons of mean values of normally distributed variables (i.e., age) between CVD and CVD-free participants or between participants with adequate or inadequate sleep habits were performed using Student’s t-test. Comparisons of mean values of non-normally distributed variables (i.e., MedDietScore at 2002 and 2012) between CVD and CVD-free participants or between participants with adequate or inadequate sleep were performed using the Mann–Whitney non-parametric test. Among the four groups of concomitant MD adherence and sleep habits (i.e., low MD adherence and inadequate sleep, low MD and adequate sleep, high MD and inadequate sleep, high MD and adequate sleep), comparisons of mean values of normally distributed variables (i.e., age) were performed using one way analysis of variance (ANOVA), while for non-normally distributed ones (i.e., MedDietScore at 2002 and 2012), the Kruskal–Wallis non-parametric test was used. p-values from post-hoc comparisons were adjusted using the Bonferroni rule. Hazard ratios (HR) and their corresponding 95% confidence intervals (95% CIs) for MedDietScore in relation to CVD within the 20-year period were taken from multivariable Cox-regression analysis. Multiple hazards models were used to progressively adjust for potential confounding factors. Models used included Model 1: crude model, Model 2: adjusted for age, sex and SES, Model 3: Model 2 and further adjustment for hypertension, hypercholesterolemia, diabetes, family history of CVD, Model 4: Model 3+ trajectories of body weight, physical activity level, MD adherence, smoking habits, and Model 5: Model 4+ adequate sleep. Time to CVD event was recorded on annual basis. Participants with missing values were excluded from the analysis. A significant interaction was observed between MedDietScore and sleep habits; therefore, a subgroup analysis was performed in order to evaluate the relationship between MedDietScore and 20-year CVD risk, according to sleep habits (adequate and inadequate sleep). Additionally, the classification and regression tree (CART) analysis was used to determine the most significant factors between CVD incidence and several contributing factors, including MD adherence, sleep habits, age, and sex [32]. Lastly, multiple hazards models (models 1–4), were also used to evaluate the relationship between the concomitant adherence to the MD and sleep habits, with CVD risk.
3. Results
During the 20-year follow-up, approximately 31.6% of the participants (n = 99) developed a CVD event. Participants slept a total of mean (standard deviation) 6.3 (1.2) hours per day. The majority of the participants (i.e., 57.5%) reported inadequate sleep habits (i.e., slept < 7 h/day); at this point it should be noted that sleeping hours refer to total hours per day, but mid-day nap was not reported in the studied sample.
3.1. Baseline and Longitudinal Participants’ Characteristics by CVD Status at 20-Year Follow-Up
Participants’ characteristics, both at baseline and longitudinally, by cardiovascular disease status in the 20-year follow-up are presented in Table 1. Participants who developed CVD during the 20 years, compared to participants who did not, were mainly older participants, and a higher percentage of them had a history of hypertension, hypercholesterolemia, and diabetes mellitus both at baseline and in the follow-up. Moreover, a lower percentage of the participants slept adequately (in 2012), and a higher percentage started smoking (in 2012), were overweight or obese, physically inactive, and away from the MD (during 2002–2012) (Table 1).

Table 1.
Baseline and longitudinal characteristics by cardiovascular disease status at the 20-year follow-up in the ATTICA study sub-sample (n = 313).
3.2. Baseline and Longitudinal Participants’ Characteristics by Sleep Habits
Participants’ characteristics by sleep habits at the 10-year follow-up are shown in Table 2. Participants who had adequate sleep (≥7 h/day), compared to participants who had inadequate sleep (<7 h/day), were younger, had a higher SES, a higher history of hypertension (at baseline and in 2022), a higher history of hypercholesterolemia (in 2022), and a higher MedDietScore (at baseline and in 2012) (Table 2).

Table 2.
Baseline and longitudinal characteristics by sleep habits during the 10-year follow-up in the ATTICA study sub-sample (n = 313).
3.3. Baseline and Longitudinal Participants’ Characteristics by Concomitant Adherence to the Mediterranean Diet and Sleep Habits
Participants’ characteristics by concomitant adherence to the MD and sleep habits at the 10-year follow-up are shown in Table 3. Between the four groups (low MD adherence and inadequate sleep, low MD and adequate sleep, high MD and inadequate sleep, and high MD and adequate sleep), differences were observed concerning age, sex, SES, history of clinical characteristics, trajectories of body weight, and MD adherence. In the high MD adherence and adequate sleep category, compared to the low MD and inadequate sleep category, participants were more likely to be younger, women, of a high SES, were less likely to have a history of clinical conditions, and had (initially or continuously) a higher adherence to the MD and a normal weight (Table 3). Those in the high MD and inadequate sleep group, compared to those in the low MD and adequate sleep, were more likely to be younger, women, of middle SES, and to have a better weight status in the long-term (Table 3).

Table 3.
Baseline and longitudinal characteristics according to Mediterranean diet adherence and sleep habits of the study participants (n = 313) at the 10-year follow-up.
3.4. Mediterranean Diet and 20-Year CVD Incidence
Results from Cox proportional hazards models, investigating the association between the MD and 20-year CVD incidence, are presented in Table 4. In Models 1–4, the adherence to the MD, per 1/55 increase of MedDietScore was inversely associated with a reduction on CVD risk, varying from 15% in the crude model (Model 1) to 9% in the fully adjusted model (Model 4).

Table 4.
Results from Cox proportional hazards models evaluating the association between adherence to the Mediterranean-type diet and cardiovascular disease risk (n = 313).
3.5. The Moderating Role of Adequate Sleep in the Association between MD Adherence and CVD Incidence
The addition of adequate sleep in Model 5, modified the association between adherence to the MD and CVD, making it insignificant (Table 4, Model 5). Afterwards, subgroup analyses were performed (p-for-interaction between MedDietScore and sleep duration <0.001), concerning the association between CVD risk and MD adherence according to sleep habits (adequate and inadequate sleep) (Table 5). It was found that sleep habits moderated the protective effects of the MD against CVD risk, as MedDietScore was inversely associated with CVD risk only in participants who slept adequately (≥7 h/day) (Table 5).

Table 5.
Subgroup analyses evaluating the relationship between Mediterranean-type diet adherence and cardiovascular disease risk stratified by adequate sleep habits (n = 313).
For a more straightforward and clinically relevant depiction, Figure 2 presents the classification tree concerning CVD incidence in relation to MD adherence, sleep habits, and age and sex; no differences by age and sex were observed.
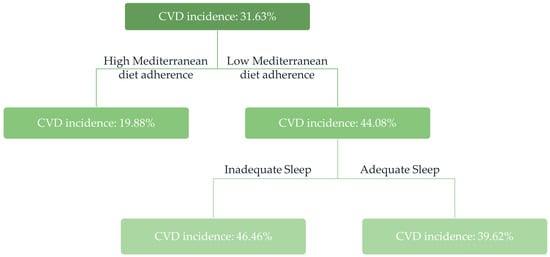
Figure 2.
Classification tree model studying CVD incidence in relation to MD adherence, sleep habits, and age and sex in the ATTICA study sample during 2002–2022 (n = 313). Adequate sleep is defined as ≥7 h/day, and inadequate sleep as <7 h/day. Low MD adherence was defined as MedDietScore during 2012 <27 (median), and high MD adherence as MedDietScore during 2012 ≥27 (median). Abbreviations: CVD: cardiovascular disease, MD: Mediterranean-type diet.
3.6. Mediterranean Diet Adherence and Sleep Habits in Relation to CVD Risk
Table 6 depicts results from Cox proportional hazards models, evaluating the association between the adherence to the MD and sleep habits in relation to 20-year CVD incidence. In the crude model, both high adherence to the MD and inadequate or adequate sleep was inversely associated with 20-year CVD risk. However, in the fully adjusted model (Model 4), only those who had a high adherence to the MD along with adequate sleep habits had a 70% reduced risk to develop CVD during the 20 years of follow-up, compared to those who had a low MD adherence and inadequate sleep habits (Table 6).

Table 6.
Results from Cox proportional hazards models evaluating the association between the concomitant adherence to the Mediterranean type diet and sleep habits and cardiovascular disease risk (n = 313).
4. Discussion
This study aimed to evaluate the potential modifying role of sleep duration in the relationship between the adherence to the MD and CVD risk. It was found that sleep duration (hours sleeping/day) modifies this relationship, and that, in specific, adherence to the MD was protective against CVD risk, in multi-adjusted models, only in participants who had adequate sleep habits (i.e., those who were sleeping ≥ 7 h/day), but not in those who had inadequate sleep habits (i.e., those who were sleeping < 7 h/day). Moreover, those who reported a high adherence to the MD along with adequate sleep habits, had a 70% reduced 20-year risk to develop CVD [HR: 0.30, 95%CI: 0.11, 0.80], compared to those who had a low MD adherence and inadequate sleep habits. Despite the limitations this cohort study may carry, to the best of our knowledge, this is the first study to propose a moderating role of sleep in the well-established protective effect of the MD against CVD, therefore suggesting that an individual’s overall lifestyle, sleep habits included, should be addressed to effectively reduce CVD risk, as it has also been suggested recently by the American Heart Association [16].
4.1. Sleep Duration and Cardiovascular Disease
Sleep duration has shown a U- or J-shaped relationship with CVD; both short sleep duration (i.e., usually less than 5–6 h/night), as well as long sleep duration (i.e., usually more than 7–8 h/night) have been associated with an increased CVD risk [10,11,14,33,34]. It has been observed that approximately 33% of adults in the US reported inadequate sleep habits in 2017 (i.e., slept less than 6 h/night) [35]. In our study, an even higher percentage (58%) compared to the US adults, had inadequate sleep (i.e., <7 h/day) in 2012, potentially attributed to secular lifestyle trends such as having multiple jobs, working shifts or irregular hours [10,36]. Moreover, our study sample slept less compared to another sample of Greek adults, from the Hellenic National Nutrition and Health Survey (HNNHS) (i.e., mean hours sleeping: 6.3 vs. 7 h/night) [37]; this could be attributed to the fact that our study had older participants, as sleep habits change during the aging process, independently of other factors [38].
It should be noted that, in this study, we used the threshold of 7 h of sleep duration per day. This was based on systematic reviews and meta-analyses, which have revealed that sleeping less than 6 h/day or more than 8–9 h/day, is positively associated with increased CVD risk, compared to 6 to 8 h/day [10,11,14,33]. Moreover, the American Academy of Sleep Medicine and Sleep Research Society recommend that adults should sleep more than 7 h per day for optimal health, and the American Heart Association recommends sleeping 7–9 h/night to prevent CVD [16,39]. In addition, we only categorized sleep as adequate or inadequate, because only a small percentage (i.e., 1.6%) slept more than 9 h/day. In other studies, regarding long sleep duration, it has been proposed that depression and low SES are factors that might influence the relationship between long sleep duration and increased mortality [40].
Moreover, mid-day nap was not reported in the studied sample. In addition, instead of total sleep duration, most studies evaluate the association between midday-naps or siestas (i.e., day-time naps, usually taken in the early afternoon and/or after the midday meal in the Mediterranean lifestyle) and health [41,42,43,44]. Daytime naps have shown mixed results in the literature concerning mortality and CVD risk, depending on the reason people have daytime naps; if the reason is for stress-relief, as it was common in the Mediterranean lifestyle, daytime naps might have beneficial effects, but if the reason is to fix inadequate night sleep due to symptoms such as depression or cognitive decline, daytime naps might not suffice to reverse the increased CVD risk associated with these diseases [10,41,42]. Thus, future studies on the effect of daytime naps on CVD risk should consider overall sleep habits and either use sleep duration as a covariate or differentiate results by sleep duration.
4.2. The Importance of Sleep for Cardiovascular Health
Sleep helps the body and mind to function and perform well during the day; sleep could be considered as the best thing one could do by doing “nothing”. Most recently, the World Sleep Society Global Sleep Health Taskforce emphasized the need to integrate sleep in public health campaigns [45]. Moreover, short sleep might modulate the association between established risk factors (such as hypertension, diabetes mellitus, dyslipidemia) and CVD [46,47]. Chronic inadequate sleep may lead to electrocardiographic abnormalities, enhanced release of norepinephrine, inhibited muscle sympathetic nerve activity, enhanced cardiac sympathetic drive, deterioration of vascular structure and function, arterial stiffness, and increased oxidative stress levels as well as increases in blood pressure, glucose dysregulation, decreased insulin sensitivity, weight gain, and disrupted circadian rhythm [36,48,49,50].
4.3. Diet, Sleep, and Cardiovascular Disease
Sleep and diet might reciprocally and multi-directionally affect CVD risk [51,52]. Studies have shown that short sleep duration or lower sleep quality is associated with lower diet quality and adherence to MD [52,53,54,55] and that better dietary habits and greater adherence to MD might be associated with better sleep habits [51,55,56]. The increase in the availability of tryptophan (a precursor of serotonin and melatonin) and its uptake by the brain, after consumption of carbohydrates and especially fruits, vegetables and wholegrains, that are abundant and usually contribute the largest proportion of energy intake in the Mediterranean dietary pattern, have been associated with better sleep habits (i.e., decreased sleep latency, time to sleep initiation, and better sleep quality) [51,52,57,58,59,60]. Moreover, the consumption of foods containing tryptophan such as milk, fatty fish, kiwis, and cherries, have been associated with better sleep habits [52].
Sleep loss might adversely influence dietary behaviors, lead to weight gain and an elevated risk for CVD through the dysregulation of ghrelin and leptin as well as the consumption of high-energy or high-fat foods, due to the need to have energy to stay awake, increased time and opportunities to eat, greater sensitivity to food reward, and psychological distress [61]. Additionally, the gut microbiome might also play a role in the relationship between sleep, dietary habits, and CVD risk [51]. Mediterranean type diets are rich in probiotics and prebiotics and following such diets is related to better gut microbiome profiles, while the relationship between sleep and the gut microbiome might be reciprocal; evidence suggests that sleep influences the gut microbiome, and some studies have proposed that the gut microbiome composition might also affect sleep habits [51,62,63].
It should be mentioned that the relationship between the adherence to the MD along with sleep habits and CVD is rarely explored. Recently, in the National Health and Nutrition Examination Survey (NHANES), it was found that lower adherence to a MD and sleep disorders synergistically increased all-cause and CVD mortality [21]. This study seems to be in line with our observation that sleep duration modifies the association between adherence to the MD and CVD risk. Moreover, our study results suggest that the protective effect of MD against CVD is clearly outspoken in those who sleep adequately. The interrelation between diet, sleep and CVD is a relationship that warrants further research, through clinical studies and epidemiological studies with bigger samples.
4.4. Strengths and Limitations
The ATTICA study has a long follow-up and multiple assessments, that allowed the inclusion of trajectories of clinical and lifestyle characteristics as covariates in the relationship among sleep, MD, and CVD. However, some limitations should be noted. The ATTICA study was not designed to study specifically sleep habits, as is the case for most epidemiological studies which have reported data on sleep habits. Sleep habits were assessed only once, in 2012 (during the 3rd evaluation), therefore trajectories of sleep habits could not be computed, and changes in sleep habits (e.g., due to different working hours or stress levels) could have affected our results. Moreover, sleep habits were self-reported by the use of a validated questionnaire, provided by study investigators, and not by other direct measurements (e.g., polysomnography), but this is common in epidemiological studies that assess sleep characteristics such as sleep duration or sleep quality. Additionally, we assessed sleep duration as adequate or inadequate sleep (because only a small percentage, i.e., 1.6%, slept more than 9 h/day) and did not take into consideration day-time naps. The relatively small sample size of the current study could be another limitation; men and women were analyzed together, and this fact might have masked potential sex-differences. However, it should also be noted that although the sample was not of a large size, the effects of sleep are clearly outspoken. Furthermore, dietary habits were assessed by an FFQ; although, this FFQ was validated for the Greek population and provided by study investigators, some measurement error could have existed.
5. Conclusions
In conclusion, in this study, it was found that sleep duration was a moderator in the well-established relationship between MD adherence and CVD risk. Therefore, sleep should have a place among other lifestyle habits that are recommended in clinical practice as well as public health actions, for an individual to acquire and maintain better cardiovascular health.
Author Contributions
Conceptualization, E.D.; methodology, C.C., C.P., C.T., E.L., P.P.S. and D.P.; formal analysis, E.D.; investigation, E.D., C.V., F.B., E.V., K.K. and E.K.; writing—original draft preparation, E.D.; writing—review and editing, D.P.; supervision, D.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of Athens Medical School (#017/1.5.2001).
Informed Consent Statement
Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions.
Acknowledgments
The authors would like to thank the ATTICA study group of investigators: Dimitrios Dalmyras, Petros Spyridonas Adamidis, Amalia Despoina Koutsogianni, Georgia Anastasiou, Asimina Loukina, Giorgos Metzantonakis, Evangelinos Michelis, Manolis Kambaxis, Kyriakos Dimitriadis, Ioannis Andrikou, Amalia Sofianidi, Natalia Sinou, Aikaterini Skandali, and Christina Sousouni, for their assistance on the 20-year follow-up, as well as Ekavi N. Georgousopoulou, Natassa Katinioti, Labros Papadimitriou, Constantina Masoura, Spiros Vellas, Yannis Lentzas, Manolis Kambaxis, Konstadina Palliou, Vassiliki Metaxa, Agathi Ntzouvani, Dimitris Mpougatsas, Nikolaos Skourlis, Christina Papanikolaou, Georgia-Maria Kouli, Aimilia Christou, Adella Zana, Maria Ntertimani, Aikaterini Kalogeropoulou, Evangelia Pitaraki, Alexandros Laskaris, Mihail Hatzigeorgiou, and Athanasios Grekas, Efi Tsetsekou, Carmen Vassiliadou, George Dedoussis, Marina Toutouza-Giotsa, Constadina Tselika and Sia Poulopoulou, and Maria Toutouza for their assistance in the initial and follow-up evaluations.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Moro, E. The Mediterranean Diet from Ancel Keys to the UNESCO Cultural Heritage. A Pattern of Sustainable Development between Myth and Reality. Procedia Soc. Behav. Sci. 2016, 223, 655–661. [Google Scholar] [CrossRef]
- Keys, A.; Menotti, A.; Karvonen, M.J.; Aravanis, C.; Blackburn, H.; Buzina, R.; Djordjevic, B.S.; Dontas, A.S.; Fidanza, F.; Keys, M.H. The Diet and 15-Year Death Rate in the Seven Countries Study. Am. J. Epidemiol. 1986, 124, 903–915. [Google Scholar] [CrossRef] [PubMed]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on Cardiovascular Disease Prevention in Clinical Practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, e563–e595. [Google Scholar] [CrossRef]
- da Silva, R.; Bach-Faig, A.; Raidó Quintana, B.; Buckland, G.; Vaz de Almeida, M.D.; Serra-Majem, L. Worldwide Variation of Adherence to the Mediterranean Diet, in 1961–1965 and 2000–2003. Public Health Nutr. 2009, 12, 1676–1684. [Google Scholar] [CrossRef] [PubMed]
- Vilarnau, C.; Stracker, D.M.; Funtikov, A.; da Silva, R.; Estruch, R.; Bach-Faig, A. Worldwide Adherence to Mediterranean Diet between 1960 and 2011. Eur. J. Clin. Nutr. 2019, 72, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Obeid, C.A.; Gubbels, J.S.; Jaalouk, D.; Kremers, S.P.J.; Oenema, A. Adherence to the Mediterranean Diet among Adults in Mediterranean Countries: A Systematic Literature Review. Eur. J. Nutr. 2022, 61, 3327–3344. [Google Scholar] [CrossRef]
- Damigou, E.; Faka, A.; Kouvari, M.; Anastasiou, C.; Kosti, R.I.; Chalkias, C.; Panagiotakos, D. Adherence to a Mediterranean Type of Diet in the World: A Geographical Analysis Based on a Systematic Review of 57 Studies with 1,125,560 Participants. Int. J. Food Sci. Nutr. 2023, 74, 799–813. [Google Scholar] [CrossRef]
- Godos, J. Decreasing Adherence to the Mediterranean Diet: Health and Environmental Foe. Int. J. Food Sci. Nutr. 2023, 74, 797–798. [Google Scholar] [CrossRef]
- Cappuccio, F.P.; Miller, M.A. Sleep and Cardio-Metabolic Disease. Curr. Cardiol. Rep. 2017, 19, 110. [Google Scholar] [CrossRef]
- Cappuccio, F.P.; Cooper, D.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Sleep Duration Predicts Cardiovascular Outcomes: A Systematic Review and Meta-Analysis of Prospective Studies. Eur. Heart J. 2011, 32, 1484–1492. [Google Scholar] [CrossRef] [PubMed]
- Makarem, N.; Castro-Diehl, C.; St-Onge, M.-P.; Redline, S.; Shea, S.; Lloyd-Jones, D.; Ning, H.; Aggarwal, B. Redefining Cardiovascular Health to Include Sleep: Prospective Associations With Cardiovascular Disease in the MESA Sleep Study. J. Am. Heart Assoc. 2022, 11, e025252. [Google Scholar] [CrossRef] [PubMed]
- Grandner, M.A.; Alfonso-Miller, P.; Fernandez-Mendoza, J.; Shetty, S.; Shenoy, S.; Combs, D. Sleep: Important Considerations for the Prevention of Cardiovascular Disease. Curr. Opin. Cardiol. 2016, 31, 551–565. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Jin, X.; Shan, Z.; Li, S.; Huang, H.; Li, P.; Peng, X.; Peng, Z.; Yu, K.; Bao, W.; et al. Relationship of Sleep Duration with All-Cause Mortality and Cardiovascular Events: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. J. Am. Heart Assoc. 2017, 6, e005947. [Google Scholar] [CrossRef] [PubMed]
- American Heart Association. Life’s Simple 7—American Heart Association—Workplace Health Playbook. Available online: https://playbook.heart.org/lifes-simple-7/ (accessed on 1 October 2023).
- American Heart Association. Life’s Essential 8. Available online: https://www.heart.org/en/healthy-living/healthy-lifestyle/lifes-essential-8 (accessed on 1 October 2023).
- Scoditti, E.; Tumolo, M.R.; Garbarino, S. Mediterranean Diet on Sleep: A Health Alliance. Nutrients 2022, 14, 2998. [Google Scholar] [CrossRef] [PubMed]
- Muscogiuri, G.; Barrea, L.; Aprano, S.; Framondi, L.; Di Matteo, R.; Laudisio, D.; Pugliese, G.; Savastano, S.; Colao, A. Sleep Quality in Obesity: Does Adherence to the Mediterranean Diet Matter? Nutrients 2020, 12, 1364. [Google Scholar] [CrossRef]
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Després, J.-P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation 2021, 143, e984–e1010. [Google Scholar] [CrossRef]
- Tietjens, J.R.; Claman, D.; Kezirian, E.J.; De Marco, T.; Mirzayan, A.; Sadroonri, B.; Goldberg, A.N.; Long, C.; Gerstenfeld, E.P.; Yeghiazarians, Y. Obstructive Sleep Apnea in Cardiovascular Disease: A Review of the Literature and Proposed Multidisciplinary Clinical Management Strategy. J. Am. Heart Assoc. 2019, 8, e010440. [Google Scholar] [CrossRef]
- Wang, Y.; Fan, H.; Ren, Z.; Liu, X.; Niu, X. Sleep Disorder, Mediterranean Diet, and All-Cause and Cause-Specific Mortality: A Prospective Cohort Study. BMC Public. Health 2023, 23, 904. [Google Scholar] [CrossRef]
- Pitsavos, C.; Panagiotakos, D.B.; Chrysohoou, C.; Stefanadis, C. Epidemiology of Cardiovascular Risk Factors in Greece: Aims, Design and Baseline Characteristics of the ATTICA Study. BMC Public. Health 2003, 3, 32. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Pitsavos, C.; Chrysohoou, C.; Skoumas, I.; Stefanadis, C. Prevalence and Five-Year Incidence (2001–2006) of Cardiovascular Disease Risk Factors in a Greek Sample: The ATTICA Study. Hell. J. Cardiol. 2009, 50, 388–395. [Google Scholar]
- Panagiotakos, D.B.; Georgousopoulou, E.N.; Pitsavos, C.; Chrysohoou, C.; Metaxa, V.; Georgiopoulos, G.A.; Kalogeropoulou, K.; Tousoulis, D.; Stefanadis, C.; ATTICA Study Group. Ten-Year (2002–2012) Cardiovascular Disease Incidence and All-Cause Mortality, in Urban Greek Population: The ATTICA Study. Int. J. Cardiol. 2015, 180, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Damigou, E.; Kouvari, M.; Chrysohoou, C.; Barkas, F.; Kravvariti, E.; Pitsavos, C.; Skoumas, J.; Michelis, E.; Liberopoulos, E.; Tsioufis, C.; et al. Lifestyle Trajectories Are Associated with Incidence of Cardiovascular Disease: Highlights from the ATTICA Epidemiological Cohort Study (2002–2022). Life 2023, 13, 1142. [Google Scholar] [CrossRef] [PubMed]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the Management of Dyslipidaemias: Lipid Modification to Reduce Cardiovascular Risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2022. Diabetes Care 2021, 45, S17–S38. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018, 71, e13–e115. [Google Scholar] [CrossRef] [PubMed]
- Katsouyanni, K.; Rimm, E.B.; Gnardellis, C.; Trichopoulos, D.; Polychronopoulos, E.; Trichopoulou, A. Reproducibility and Relative Validity of an Extensive Semi-Quantitative Food Frequency Questionnaire Using Dietary Records and Biochemical Markers among Greek Schoolteachers. Int. J. Epidemiol. 1997, 26, S118. [Google Scholar] [CrossRef] [PubMed]
- Panagiotakos, D.B.; Pitsavos, C.; Stefanadis, C. Dietary Patterns: A Mediterranean Diet Score and Its Relation to Clinical and Biological Markers of Cardiovascular Disease Risk. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 559–568. [Google Scholar] [CrossRef]
- Fichten, C.S.; Creti, L.; Amsel, R.; Bailes, S.; Libman, E. Time Estimation in Good and Poor Sleepers. J. Behav. Med. 2005, 28, 537–553. [Google Scholar] [CrossRef]
- Breiman, L. Classification and Regression Trees; Routledge: New York, NY, USA, 2017; ISBN 978-1-315-13947-0. [Google Scholar]
- Gardner, C.D.; Vadiveloo, M.K.; Petersen, K.S.; Anderson, C.A.M.; Springfield, S.; Van Horn, L.; Khera, A.; Lamendola, C.; Mayo, S.M.; Joseph, J.J.; et al. Popular Dietary Patterns: Alignment With American Heart Association 2021 Dietary Guidance: A Scientific Statement from the American Heart Association. Circulation 2023, 147, 1715–1730. [Google Scholar] [CrossRef]
- Yamagata, K.; Yamagata, L.M.; Abela, M. A Review Article of the Cardiovascular Sequalae in Esport Athletes: A Cause for Concern? Hell. J. Cardiol. 2022, 68, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, C.M.; Frochen, S.E.; Walsemann, K.M.; Ailshire, J.A. Are U.S. Adults Reporting Less Sleep? Findings from Sleep Duration Trends in the National Health Interview Survey, 2004–2017. Sleep 2019, 42, zsy221. [Google Scholar] [CrossRef] [PubMed]
- Covassin, N.; Singh, P. Sleep Duration and Cardiovascular Disease Risk: Epidemiologic and Experimental Evidence. Sleep. Med. Clin. 2016, 11, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Michas, G.; Magriplis, E.; Micha, R.; Chourdakis, M.; Koutelidakis, A.; Dimitriadis, G.; Panagiotakos, D.; Zampelas, A. Prevalence and Factors Associated with Smoking in a Nationally Representative Sample of Greek Adults: The Hellenic National Nutrition and Health Survey (HNNHS). Hell. J. Cardiol. 2022, 67, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Vitiello, M.V.; Gooneratne, N. Sleep in Normal Aging. Sleep Med. Clin. 2018, 13, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.M.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 2015, 38, 843–844. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.R.; Malhotra, A.; Gottlieb, D.J.; White, D.P.; Hu, F.B. Correlates of Long Sleep Duration. Sleep 2006, 29, 881–889. [Google Scholar] [CrossRef]
- Chen, S.; Hu, Z.; He, L.; Bai, X.; Li, H.; Xu, X.; Hu, S.; Chen, L. Relationship Between Daytime Napping and Cardiovascular Disease: A Two-Sample Mendelian Randomization Study. Hell. J. Cardiol. 2023, in press. [Google Scholar] [CrossRef]
- Sun, J.; Ma, C.; Zhao, M.; Magnussen, C.G.; Xi, B. Daytime Napping and Cardiovascular Risk Factors, Cardiovascular Disease, and Mortality: A Systematic Review. Sleep Med. Rev. 2022, 65, 101682. [Google Scholar] [CrossRef]
- Georgousopoulou, E.N.; Mellor, D.D.; Naumovski, N.; Polychronopoulos, E.; Tyrovolas, S.; Piscopo, S.; Valacchi, G.; Anastasiou, F.; Zeimbekis, A.; Bountziouka, V.; et al. Mediterranean Lifestyle and Cardiovascular Disease Prevention. Cardiovasc. Diagn. Ther. 2017, 7, S39–S47. [Google Scholar] [CrossRef]
- Foscolou, A.; D’Cunha, N.M.; Naumovski, N.; Tyrovolas, S.; Rallidis, L.; Matalas, A.-L.; Polychronopoulos, E.; Sidossis, L.S.; Panagiotakos, D. Midday Napping and Successful Aging in Older People Living in the Mediterranean Region: The Epidemiological Mediterranean Islands Study (MEDIS). Brain Sci. 2019, 10, 14. [Google Scholar] [CrossRef] [PubMed]
- Lim, D.C.; Najafi, A.; Afifi, L.; Bassetti, C.L.; Buysse, D.J.; Han, F.; Högl, B.; Melaku, Y.A.; Morin, C.M.; Pack, A.I.; et al. The Need to Promote Sleep Health in Public Health Agendas across the Globe. Lancet Public Health 2023, 8, e820–e826. [Google Scholar] [CrossRef]
- Miller, M.A.; Cappuccio, F.P. Biomarkers of Cardiovascular Risk in Sleep-Deprived People. J. Hum. Hypertens. 2013, 27, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Global Cardiovascular Risk Consortium; Magnussen, C.; Ojeda, F.M.; Leong, D.P.; Alegre-Diaz, J.; Amouyel, P.; Aviles-Santa, L.; De Bacquer, D.; Ballantyne, C.M.; Bernabé-Ortiz, A.; et al. Global Effect of Modifiable Risk Factors on Cardiovascular Disease and Mortality. N. Engl. J. Med. 2023, 389, 1273–1285. [Google Scholar] [CrossRef] [PubMed]
- Yatsu, S.; Kasai, T.; Naito, R.; Matsumoto, H.; Murata, A.; Shitara, J.; Shiroshita, N.; Kato, M.; Kawana, F.; Sato, A.; et al. Impact of Sleep-Disordered Breathing on Overnight Changes in Arterial Stiffness in Patients with Acute Heart Failure. Hypertens. Res. 2023, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Amisaki, R.; Kato, M.; Fujiyama, M.; Matsuda, E.; Hattori, Y.; Hirai, M.; Yanagihara, K.; Kinugasa, Y.; Yamamoto, K. Difficulty Initiating Sleep in Patients with Heart Failure: Impact of Left Atrial Pressure. J. Cardiol. 2022, 80, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, M.; Kasai, T.; Naito, R.; Sato, A.; Ishiwata, S.; Yatsu, S.; Shitara, J.; Matsumoto, H.; Murata, A.; Kato, T.; et al. Overnight Changes in Uric Acid, Xanthine Oxidoreductase and Oxidative Stress Levels and Their Relationships with Sleep-Disordered Breathing in Patients with Coronary Artery Disease. Hypertens. Res. 2023, 46, 2293–2301. [Google Scholar] [CrossRef]
- St-Onge, M.-P.; Zuraikat, F.M. Reciprocal Roles of Sleep and Diet in Cardiovascular Health: A Review of Recent Evidence and a Potential Mechanism. Curr. Atheroscler. Rep. 2019, 21, 11. [Google Scholar] [CrossRef]
- Frank, S.; Gonzalez, K.; Lee-Ang, L.; Young, M.C.; Tamez, M.; Mattei, J. Diet and Sleep Physiology: Public Health and Clinical Implications. Front. Neurol. 2017, 8, 393. [Google Scholar] [CrossRef]
- Campanini, M.Z.; Guallar-Castillón, P.; Rodríguez-Artalejo, F.; Lopez-Garcia, E. Mediterranean Diet and Changes in Sleep Duration and Indicators of Sleep Quality in Older Adults. Sleep 2017, 40, zsw083. [Google Scholar] [CrossRef]
- Mamalaki, E.; Anastasiou, C.A.; Ntanasi, E.; Tsapanou, A.; Kosmidis, M.H.; Dardiotis, E.; Hadjigeorgiou, G.M.; Sakka, P.; Scarmeas, N.; Yannakoulia, M. Associations between the Mediterranean Diet and Sleep in Older Adults: Results from the Hellenic Longitudinal Investigation of Aging and Diet Study. Geriatr. Gerontol. Int. 2018, 18, 1543–1548. [Google Scholar] [CrossRef] [PubMed]
- Castro-Diehl, C.; Wood, A.C.; Redline, S.; Reid, M.; Johnson, D.A.; Maras, J.E.; Jacobs, D.R.; Shea, S.; Crawford, A.; St-Onge, M.-P. Mediterranean Diet Pattern and Sleep Duration and Insomnia Symptoms in the Multi-Ethnic Study of Atherosclerosis. Sleep 2018, 41, zsy158. [Google Scholar] [CrossRef] [PubMed]
- Jaussent, I.; Dauvilliers, Y.; Ancelin, M.-L.; Dartigues, J.-F.; Tavernier, B.; Touchon, J.; Ritchie, K.; Besset, A. Insomnia Symptoms in Older Adults: Associated Factors and Gender Differences. Am. J. Geriatr. Psychiatry 2011, 19, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Peuhkuri, K.; Sihvola, N.; Korpela, R. Diet Promotes Sleep Duration and Quality. Nutr. Res. 2012, 32, 309–319. [Google Scholar] [CrossRef] [PubMed]
- Markus, C.R.; Jonkman, L.M.; Lammers, J.H.C.M.; Deutz, N.E.P.; Messer, M.H.; Rigtering, N. Evening Intake of Alpha-Lactalbumin Increases Plasma Tryptophan Availability and Improves Morning Alertness and Brain Measures of Attention. Am. J. Clin. Nutr. 2005, 81, 1026–1033. [Google Scholar] [CrossRef] [PubMed]
- Silber, B.Y.; Schmitt, J. Effects of Tryptophan Loading on Human Cognition, Mood, and Sleep. Neurosci. Biobehav. Rev. 2010, 34, 387–407. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Rodríguez, A.; Rubio-Arias, J.Á.; Ramos-Campo, D.J.; Reche-García, C.; Leyva-Vela, B.; Nadal-Nicolás, Y. Psychological and Sleep Effects of Tryptophan and Magnesium-Enriched Mediterranean Diet in Women with Fibromyalgia. Int. J. Environ. Res. Public. Health 2020, 17, 2227. [Google Scholar] [CrossRef]
- Chaput, J.-P. Sleep Patterns, Diet Quality and Energy Balance. Physiol. Behav. 2014, 134, 86–91. [Google Scholar] [CrossRef]
- Mitsou, E.K.; Kakali, A.; Antonopoulou, S.; Mountzouris, K.C.; Yannakoulia, M.; Panagiotakos, D.B.; Kyriacou, A. Adherence to the Mediterranean Diet Is Associated with the Gut Microbiota Pattern and Gastrointestinal Characteristics in an Adult Population. Br. J. Nutr. 2017, 117, 1645–1655. [Google Scholar] [CrossRef]
- Haro, C.; García-Carpintero, S.; Rangel-Zúñiga, O.A.; Alcalá-Díaz, J.F.; Landa, B.B.; Clemente, J.C.; Pérez-Martínez, P.; López-Miranda, J.; Pérez-Jiménez, F.; Camargo, A. Consumption of Two Healthy Dietary Patterns Restored Microbiota Dysbiosis in Obese Patients with Metabolic Dysfunction. Mol. Nutr. Food Res. 2017, 61, 1700300. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).