Examining Nutrition Knowledge, Skills, and Eating Behaviours in People with Severe Mental Illness: A Cross-Sectional Comparison among Psychiatric Inpatients, Outpatients, and Healthy Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. Personal Variables
2.2.2. Health Status and Behaviours
2.2.3. Dietary Behaviours and Attitudes
2.2.4. Nutrition Knowledge and Skills
2.3. Statistical Analyses
3. Results
3.1. Characteristics of Participants
3.2. Health Status and Behaviours
3.3. Dietary Behaviours, Attitudes, and Nutrition Knowledge and Skills
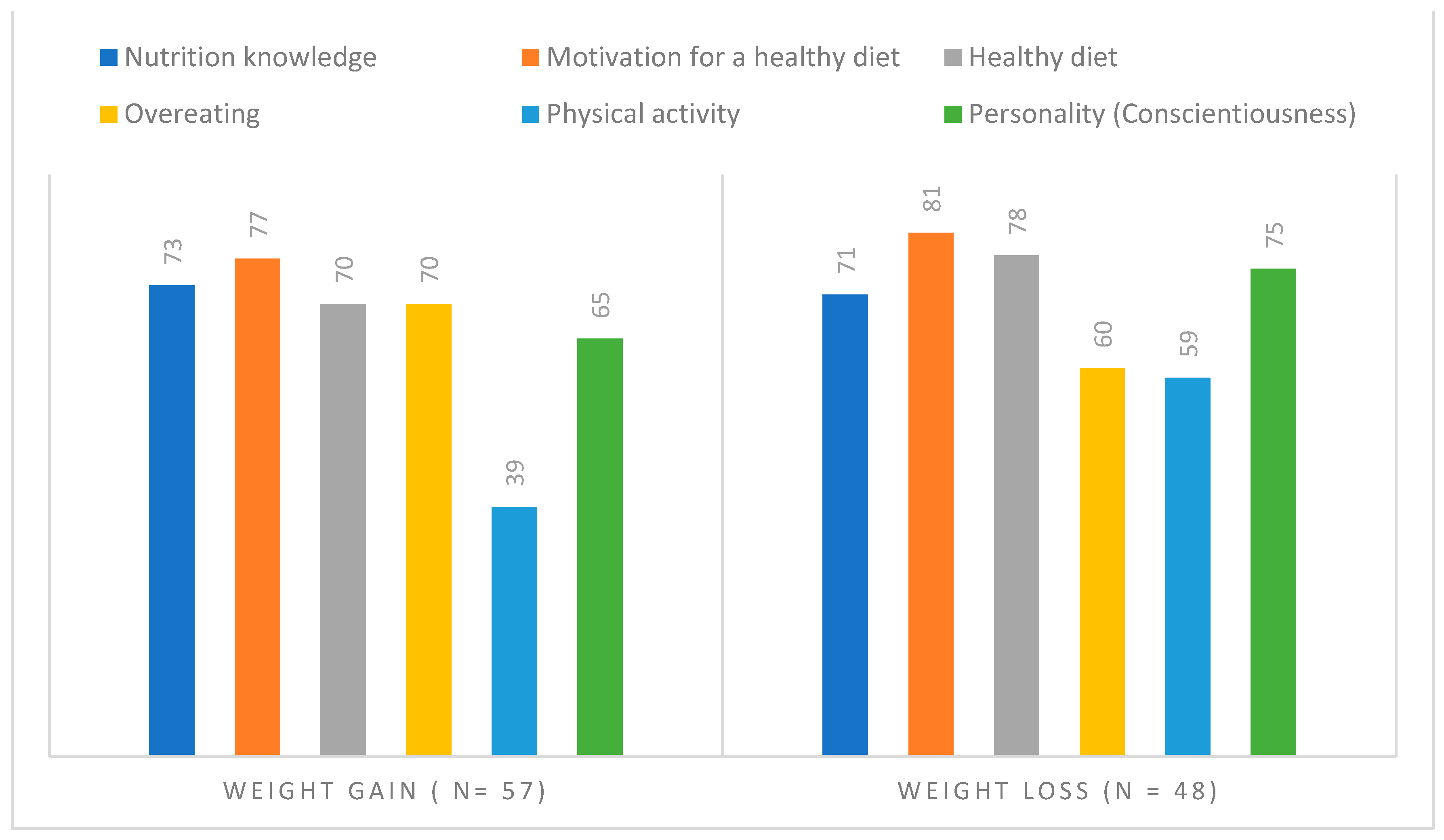
3.4. Differences between Psychiatric Patients with Weight Gain and Loss
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schinnar, A.P.; Rothbard, A.B.; Kanter, R.; Jung, Y.S. An empirical literature review of definitions of severe and persistent mental illness. Am. J. Psychiatry 1990, 147, 1602–1608. [Google Scholar] [CrossRef]
- Thornicroft, G. Premature death among people with mental illness. BMJ 2013, 346, f2969. [Google Scholar] [CrossRef]
- Walker, E.R.; McGee, R.E.; Druss, B.G. Mortality in mental disorders and global disease burden implications: A systematic review and meta-analysis. JAMA Psychiatry 2015, 72, 334–341. [Google Scholar] [CrossRef]
- Bhaskaran, K.; Douglas, I.; Forbes, H.; dos-Santos-Silva, I.; Leon, D.A.; Smeeth, L. Body-mass index and risk of 22 specific cancers: A population-based cohort study of 524 million UK adults. Lancet 2014, 384, 755–765. [Google Scholar] [CrossRef]
- Vancampfort, D.; Stubbs, B.; Mitchell, A.J.; De Hert, M.; Wampers, M.; Ward, P.B.; Rosenbaum, S.; Correll, C.U. Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: A systematic review and meta-analysis. World Psychiatry 2015, 14, 339–347. [Google Scholar] [CrossRef]
- Bak, M.; Fransen, A.; Janssen, J.; van Os, J.; Drukker, M. Almost all antipsychotics result in weight gain: A meta-analysis. PLoS ONE 2014, 9, e94112. [Google Scholar] [CrossRef]
- Zimmermann, U.; Kraus, T.; Himmerich, H.; Schuld, A.; Pollmächer, T. Epidemiology, implications and mechanisms underlying drug-induced weight gain in psychiatric patients. J. Psychiatr. Res. 2003, 37, 193–220. [Google Scholar] [CrossRef]
- De Hert, M.; Detraux, J.; Van Winkel, R.; Yu, W.; Correll, C.U. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat. Rev. Endocrinol. 2012, 8, 114–126. [Google Scholar] [CrossRef]
- Serretti, A.; Mandelli, L.; Laura, M. Antidepressants and body weight: A comprehensive review and meta-analysis. J. Clin. Psychiatry 2010, 71, 979. [Google Scholar] [CrossRef]
- Bonfioli, E.; Berti, L.; Goss, C.; Muraro, F.; Burti, L. Health promotion lifestyle interventions for weight management in psychosis: A systematic review and meta-analysis of randomised controlled trials. BMC Psychiatry 2012, 12, 78. [Google Scholar] [CrossRef]
- Jerome, G.J.; Young, D.R.; Dalcin, A.; Charleston, J.; Anthony, C.; Hayes, J.; Daumit, G.L. Physical activity levels of persons with mental illness attending psychiatric rehabilitation programs. Schizophr. Res. 2009, 108, 252–257. [Google Scholar] [CrossRef]
- Dipasquale, S.; Pariante, C.M.; Dazzan, P.; Aguglia, E.; McGuire, P.; Mondelli, V. The dietary pattern of patients with schizophrenia: A systematic review. J. Psychiatr. Res. 2013, 47, 197–207. [Google Scholar] [CrossRef]
- Firth, J.; Stubbs, B.; Teasdale, S.B.; Ward, P.B.; Veronese, N.; Shivappa, N.; Hebert, J.R.; Berk, M.; Yung, A.R.; Sarris, J. Diet as a hot topic in psychiatry: A population-scale study of nutritional intake and inflammatory potential in severe mental illness. World Psychiatry 2018, 17, 365–367. [Google Scholar] [CrossRef]
- Teasdale, S.B.; Samaras, K.; Wade, T.; Jarman, R.; Ward, P.B. A review of the nutritional challenges experienced by people living with severe mental illness: A role for dietitians in addressing physical health gaps. J. Hum. Nutr. Diet. 2017, 30, 545–553. [Google Scholar] [CrossRef]
- Teasdale, S.B.; Ward, P.B.; Samaras, K.; Firth, J.; Stubbs, B.; Tripodi, E.; Burrows, T.L. Dietary intake of people with severe mental illness: Systematic review and meta-analysis. Br. J. Psychiatry 2019, 214, 251–259. [Google Scholar] [CrossRef]
- Abayomi, J.; Hackett, A. Assessment of malnutrition in mental health clients: Nurses’ judgement vs. a nutrition risk tool. J. Adv. Nurs. 2004, 45, 430–437. [Google Scholar] [CrossRef]
- Risch, L.; Hotzy, F.; Vetter, S.; Hiller, S.; Wallimann, K.; Seifritz, E.; Motteli, S. Assessment of Nutritional Status and Risk of Malnutrition Using Adapted Standard Tools in Patients with Mental Illness and in Need of Intensive Psychiatric Treatment. Int. J. Environ. Res. Public Health 2022, 20, 109. [Google Scholar] [CrossRef]
- de Mestral, C.; Khalatbari-Soltani, S.; Stringhini, S.; Marques-Vidal, P. Perceived barriers to healthy eating and adherence to dietary guidelines: Nationwide study. Clin. Nutr. 2020, 39, 2580–2585. [Google Scholar] [CrossRef]
- Carson, N.E.; Blake, C.E.; Saunders, R.P.; O’Brien, J.C. Influences on the Food Choice Behaviors of Adults With Severe Mental Illness. Occup. Ther. Ment. Health 2013, 29, 361–384. [Google Scholar] [CrossRef]
- Çelik Ince, S.; Partlak Günüşen, N. The views and habits of the individuals with mental illness about physical activity and nutrition. Perspect. Psychiatr. Care 2018, 54, 586–595. [Google Scholar] [CrossRef] [PubMed]
- Barre, L.K.; Ferron, J.C.; Davis, K.E.; Whitley, R. Healthy eating in persons with serious mental illnesses: Understanding and barriers. Psychiatr. Rehabil. J. 2011, 34, 304. [Google Scholar] [CrossRef]
- Teasdale, S.B.; Burrows, T.L.; Hayes, T.; Hsia, C.Y.; Watkins, A.; Curtis, J.; Ward, P.B. Dietary intake, food addiction and nutrition knowledge in young people with mental illness. Nutr. Diet. 2020, 77, 315–322. [Google Scholar] [CrossRef]
- Teasdale, S.B.; Ward, P.B.; Rosenbaum, S.; Samaras, K.; Stubbs, B. Solving a weighty problem: Systematic review and meta-analysis of nutrition interventions in severe mental illness. Br. J. Psychiatry 2017, 210, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Mueller-Stierlin, A.S.; Peisser, A.; Cornet, S.; Jaeckle, S.; Lehle, J.; Moerkl, S.; Teasdale, S.B. Exploration of Perceived Determinants of Disordered Eating Behaviors in People with Mental Illness-A Qualitative Study. Int. J. Environ. Res. Public Health 2022, 20, 442. [Google Scholar] [CrossRef]
- Mueller-Stierlin, A.S.; Cornet, S.; Peisser, A.; Jaeckle, S.; Lehle, J.; Moerkl, S.; Teasdale, S.B. Implications of Dietary Intake and Eating Behaviors for People with Serious Mental Illness: A Qualitative Study. Nutrients 2022, 14, 2616. [Google Scholar] [CrossRef] [PubMed]
- Afzal, M.; Siddiqi, N.; Ahmad, B.; Afsheen, N.; Aslam, F.; Ali, A.; Ayesha, R.; Bryant, M.; Holt, R.; Khalid, H.; et al. Prevalence of Overweight and Obesity in People With Severe Mental Illness: Systematic Review and Meta-Analysis. Front. Endocrinol. Lausanne 2021, 12, 769309. [Google Scholar] [CrossRef]
- NICE. National Collaborating Center for Mental Heatlh, Psychosis and Schizophrenia in Adults: Treatment and Management; NICE: London, UK, 2014. [Google Scholar]
- Holt, R.I.G. The Management of Obesity in People with Severe Mental Illness: An Unresolved Conundrum. Psychother Psychosom 2019, 88, 327–332. [Google Scholar] [CrossRef]
- Hotzy, F.; Risch, L.; Motteli, S. Nutritional Needs in Mental Healthcare: Study Protocol of a Prospective Analytic Observational Study Assessing Nutritional Status, Eating Behavior and Barriers to Healthy Eating in Psychiatric Inpatients and Outpatients Compared to Healthy Adults. Front. Psychiatry 2022, 13, 906234. [Google Scholar] [CrossRef]
- Sharma, G. Pros and cons of different sampling techniques. Int. J. Appl. Res. 2017, 3, 749–752. [Google Scholar]
- Limesurvey GmbH. LimeSurvey [Open Source Survey Tool]. Hamburg, Germany. Available online: http://www.limesurvey.org (accessed on 1 January 2023).
- Prinz, U.; Nutzinger, D.O.; Schulz, H.; Petermann, F.; Braukhaus, C.; Andreas, S. Comparative psychometric analyses of the SCL-90-R and its short versions in patients with affective disorders. BMC Psychiatry 2013, 13, 104. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Kroenke, K.; Herzog, W.; Gräfe, K. Measuring depression outcome with a brief self-report instrument: Sensitivity to change of the Patient Health Questionnaire (PHQ-9). J. Affect. Disord. 2004, 81, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Rammstedt, B.; John, O.P. Kurzversion des big five inventory (BFI-K). Diagnostica 2005, 51, 195–206. [Google Scholar] [CrossRef]
- Mötteli, S.; Siegrist, M.; Keller, C. Women’s social eating environment and its associations with dietary behavior and weight management. Appetite 2017, 110, 86–93. [Google Scholar] [CrossRef]
- Mötteli, S.; Barbey, J.; Keller, C.; Bucher, T.; Siegrist, M. Measuring practical knowledge about balanced meals: Development and validation of the brief PKB-7 scale. Eur. J. Clin. Nutr. 2016, 70, 505–510. [Google Scholar] [CrossRef]
- Birchwood, M.; Smith, J.O.; Cochrane, R.; Wetton, S.; Copestake, S. The social functioning scale the development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Br. J. Psychiatry 1990, 157, 853–859. [Google Scholar] [CrossRef]
- Szalay, L.B.; Deese, J. Subjective Meaning and Culture: An Assessment through word Associations; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1978. [Google Scholar]
- Keller, C.; van der Horst, K. Dietary restraint, ambivalence toward eating, and the valence and content of spontaneous associations with eating. Appetite 2013, 62, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Bucher, T.; Hartmann, C.; Rollo, M.E.; Collins, C.E. What is nutritious snack food? A comparison of expert and layperson assessments. Nutrients 2017, 9, 874. [Google Scholar] [CrossRef]
- Deroover, K.; Bucher, T.; Vandelanotte, C.; de Vries, H.; Duncan, M.J. Practical nutrition knowledge mediates the relationship between sociodemographic characteristics and diet quality in adults: A cross-sectional analysis. Am. J. Health Promot. 2020, 34, 59–62. [Google Scholar] [CrossRef]
- Lavelle, F.; McGowan, L.; Hollywood, L.; Surgenor, D.; McCloat, A.; Mooney, E.; Caraher, M.; Raats, M.; Dean, M. The development and validation of measures to assess cooking skills and food skills. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 118. [Google Scholar] [CrossRef]
- Motteli, S.; Hotzy, F. The Assessment of Cooking Skills and Food Skills and Their Relationship with Nutrition Knowledge, Attitude toward a Healthy Diet and Food Intake: Results of a German Validation Study. Nutrients 2022, 14, 3157. [Google Scholar] [CrossRef]
- Freeman, D.; Sheaves, B.; Waite, F.; Harvey, A.G.; Harrison, P.J. Sleep disturbance and psychiatric disorders. Lancet Psychiatry 2020, 7, 628–637. [Google Scholar] [CrossRef] [PubMed]
- Lundgren, J.D.; Rempfer, M.V.; Brown, C.E.; Goetz, J.; Hamera, E. The prevalence of night eating syndrome and binge eating disorder among overweight and obese individuals with serious mental illness. Psychiatry Res. 2010, 175, 233–236. [Google Scholar] [CrossRef]
- Lundgren, J.D.; Allison, K.C.; O’Reardon, J.P.; Stunkard, A.J. A descriptive study of non-obese persons with night eating syndrome and a weight-matched comparison group. Eat. Behav. 2008, 9, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Delormier, T.; Frohlich, K.L.; Potvin, L. Food and eating as social practice—Understanding eating patterns as social phenomena and implications for public health. Sociol. Health Ill. 2009, 31, 215–228. [Google Scholar] [CrossRef] [PubMed]
- Ruddock, H.K.; Brunstrom, J.M.; Vartanian, L.R.; Higgs, S. A systematic review and meta-analysis of the social facilitation of eating. Am. J. Clin. Nutr. 2019, 110, 842–861. [Google Scholar] [CrossRef] [PubMed]
- Javaras, K.N.; Williams, M.; Baskin-Sommers, A.R. Psychological Interventions Potentially Useful for Increasing Conscientiousness. Personal. Disord. 2019, 10, 13–24. [Google Scholar] [CrossRef]
- Fryers, T.; Melzer, D.; Jenkins, R. Social inequalities and the common mental disorders: A systematic review of the evidence. Soc. Psychiatry Psychiatr. Epidemiol. 2003, 38, 229–237. [Google Scholar] [CrossRef]
| Sociodemographic Variables | Psychiatric Inpatients (n = 65) | Psychiatric Outpatients (n = 67) | Healthy Adults (n = 64) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Gender, female | 32 | 49 | 34 | 51 | 32 | 50 |
| Age > 40 years | 32 | 49 | 34 | 51 | 32 | 50 |
| Swiss nationality | 46 | 79 | 45 | 79 | 46 | 79 |
| Education | ||||||
| Compulsory schooling | 14 | 22 | 9 | 13 | 2 | 3 |
| Vocational education | 22 | 34 | 30 | 45 | 15 | 23 |
| Matura (high school exit exam) | 7 | 11 | 6 | 9 | 5 | 8 |
| Higher vocational education | 8 | 12 | 8 | 12 | 21 | 33 |
| University | 14 | 21 | 14 | 21 | 21 | 33 |
| Source of income | ||||||
| Salary | 21 | 32 | 32 | 47 | 52 | 81 |
| Disability pension | 18 | 28 | 5 | 8 | 0 | 0 |
| Social-welfare benefits | 12 | 18 | 15 | 22 | 2 | 3 |
| Support by family | 9 | 14 | 10 | 15 | 9 | 14 |
| Savings | 3 | 5 | 5 | 8 | 0 | 0 |
| Unknown | 2 | 3 | 0 | 0 | 1 | 2 |
| Financial possibilities for nutrition | ||||||
| Far too little | 5 | 8 | 10 | 15 | 0 | 0 |
| Too little | 4 | 6 | 10 | 15 | 2 | 3 |
| Just sufficient | 15 | 23 | 15 | 22 | 6 | 9 |
| Adequate | 41 | 63 | 32 | 48 | 56 | 88 |
| Housing situation | ||||||
| Alone | 21 | 32 | 29 | 43 | 13 | 20 |
| Together with others | 37 | 57 | 38 | 57 | 51 | 80 |
| Residential care home | 6 | 9 | 0 | 0 | 0 | 0 |
| Homeless | 1 | 2 | 0 | 0 | 0 | 0 |
| Variables | Inpatients (n = 65) | Outpatients (n = 67) | Healthy Adults (n = 64) | |||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | F | p | |
| SCL-K-9 | 1.8 a | 0.8 | 2.0 a | 0.9 | 0.7 b | 0.5 | 54.41 | <0.001 |
| PHQ-D | 13.5 a | 6.3 | 16.3 b | 5.1 | 4.5 c | 3.3 | 96.47 | <0.001 |
| Sum score of prescribed psychiatric medication | 2.9 a | 2.7 | 1.6 b | 2.0 | 0.0 c | 0.0 | 37.67 | <0.001 |
| Personality (Big 5 factors) | ||||||||
| Extraversion | 3.4 | 1.1 | 2.9 | 0.9 | 3.8 | 0.8 | 15.21 | <0.001 |
| Compatibility | 3.3 | 0.8 | 3.1 | 0.8 | 3.5 | 0.7 | 4.64 | 0.011 |
| Conscientiousness | 3.7 | 0.7 | 3.2 | 0.9 | 3.8 | 0.6 | 9.52 | <0.001 |
| Neuroticism | 3.4 | 0.9 | 3.9 | 0.8 | 2.4 | 0.8 | 51.73 | <0.001 |
| Openness | 4.0 | 0.7 | 3.9 | 1.0 | 3.8 | 0.7 | 1.17 | 0.313 |
| Physical activity (number of days per week) | 3.4 ab | 2.4 | 3.0 a | 2.6 | 4.3 b | 1.9 | 5.27 | 0.006 |
| Subjective evaluation of nutritional status | 6.6 a | 2.3 | 5.5 b | 2.2 | 8.2 c | 1.5 | 29.18 | <0.001 |
| BMI (kg/m2) | 25.3 a | 5.0 | 27.9 b | 5.3 | 24.0 a | 3.7 | 11.50 | <0.001 |
| WHR (cm) | 91.27 a | 8.0 | 89.62 ab | 10.6 | 85.78 b | 11.0 | 5.20 | 0.006 |
| Variables | Inpatients (n = 65) | Outpatients (n = 67) | Healthy Adults (n = 64) | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | Pearson Chi-Square | p | |
| Experienced weight change in last 3–6 months | 38.72 (4) | <0.001 | ||||||
| Weight gain | 18 a | 28 | 39 b | 58 | 17 a | 27 | ||
| No change | 19 a | 29 | 8 b | 12 | 36 c | 56 | ||
| Weight loss | 28 a | 43 | 20 ab | 30 | 11 b | 17 | ||
| Nutrition-related diseases (e.g., diabetes, celiac disease, food allergies) | 12 ab | 19 | 24 a | 36 | 11 b | 17 | 7.86 (2) | 0.020 |
| Food intolerances | 21 ab | 32 | 34 a | 51 | 15 b | 23 | 11.12 (2) | 0.004 |
| Smokers | 21 a | 60 | 35 a | 52 | 13 b | 20 | 23.12 (2) | <0.001 |
| Medical treatment due to mental problems in last 3–6 months | 21 a | 97 | 67 a | 100 | 3 b | 5 | 196.11 | <0.001 |
| Medical treatment due to physical problems in last 3–6 months | 21 a | 62 | 40 a | 60 | 16 b | 25 | 21.91 (2) | <0.001 |
| Previous experience with nutrition counselling | 21 a | 46 | 34 a | 51 | 11 b | 17 | 18.17 (2) | <0.001 |
| Variables (Possible Scale Range) | Inpatients (n = 65) | Outpatients (n = 67) | Healthy Adults (n = 64) | |||||
|---|---|---|---|---|---|---|---|---|
| n or M | % or SD | n or M | % or SD | n or M | % or SD | F or Pearson Chi-Square | p | |
| Food intake | ||||||||
| Portions of vegetables and salad per week | 17.0 | 11.5 | 14.1 | 11.0 | 20.6 | 12.7 | ||
| Portions of fruits per week | 8.9 | 7.5 | 7.3 | 7.4 | 7.7 | 7.3 | ||
| Portions of juice per week | 4.6 | 6.1 | 2.6 | 4.8 | 2.3 | 3.6 | ||
| Portions of sweets per week | 7.1 | 7.8 | 10.6 | 12.0 | 8.8 | 8.6 | ||
| Portions of sugary drinks per week | 6.1 | 9.3 | 9.5 | 13.9 | 2.5 | 5.1 | ||
| Portions of sugary food (juice, sweets, drinks) per week | 17.8 | 16.6 | 22.7 | 18.8 | 13.6 | 12.3 | 5.22 | 0.006 |
| Meal structure | ||||||||
| Breakfast | 46 | 71 | 35 | 52 | 43 | 67 | ||
| Mid-morning snack | 20 | 31 | 11 | 16 | 15 | 23 | ||
| Lunch | 56 | 86 | 46 | 69 | 61 | 95 | ||
| Afternoon snack | 18 | 28 | 24 | 36 | 22 | 34 | ||
| Dinner | 63 | 97 | 58 | 87 | 61 | 95 | ||
| Late snack | 22 | 34 | 29 | 43 | 17 | 27 | ||
| Night eating | 16 a | 25 | 17 a | 25 | 5 b | 8 | ||
| Sum of main meals (0–3) | 2.5 a | 0.7 | 2.1 b | 0.7 | 2.6 a | 0.6 | 11.57 | <0.001 |
| Diet | ||||||||
| Individualised diet (e.g., gluten-free, lactose-free, low in sugar, rich in protein, etc.) | 28 | 43 | 29 | 43 | 36 | 56 | 2.95 | 0.228 |
| Dieting (caloric restriction due to weight or health) | 26 | 40 | 36 | 54 | 35 | 55 | 3.52 | 0.172 |
| Eating habits (1–4) | ||||||||
| Nutrition-related activities | 3.1 a | 0.7 | 3.1 a | 0.7 | 3.5 b | 0.6 | 7.27 | <0.001 |
| Healthy eating | 3.0 ab | 0.8 | 2.8 a | 0.7 | 3.1 b | 0.6 | 3.76 | 0.025 * |
| Overeating | 2.6 | 0.8 | 2.6 | 0.8 | 2.9 | 0.6 | 2.86 | 0.060 |
| Social eating | 2.6 a | 0.8 | 2.2 b | 0.9 | 3.1 c | 0.8 | 20.38 | <0.001 |
| Attitudes | ||||||||
| Implicit feelings towards nutrition (1–7) | 5.4 ab | 1.4 | 5.0 b | 1.5 | 5.9 a | 1.2 | 6.46 | 0.002 |
| Importance of eating a healthy and balanced diet (1–10) | 8.2 | 1.8 | 8.0 | 2.0 | 8.6 | 1.4 | 2.49 | 0.086 |
| Knowledge and skills | ||||||||
| Practical nutrition knowledge (0–7) | 4.5 a | 1.6 | 5.3 b | 1.5 | 5.0 ab | 1.5 | 4.53 | 0.012 |
| Confidence in cooking skills (0–98) | 50.6 a | 25.0 | 65.7 b | 23.0 | 60.9 b | 21.1 | 7.27 | <0.001 |
| Confidence in food skills (0–133) | 64.6 a | 27.7 | 76.4 b | 24.8 | 74.6 ab | 25.1 | 3.95 | 0.021 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mötteli, S.; Provaznikova, B.; Vetter, S.; Jäger, M.; Seifritz, E.; Hotzy, F. Examining Nutrition Knowledge, Skills, and Eating Behaviours in People with Severe Mental Illness: A Cross-Sectional Comparison among Psychiatric Inpatients, Outpatients, and Healthy Adults. Nutrients 2023, 15, 2136. https://doi.org/10.3390/nu15092136
Mötteli S, Provaznikova B, Vetter S, Jäger M, Seifritz E, Hotzy F. Examining Nutrition Knowledge, Skills, and Eating Behaviours in People with Severe Mental Illness: A Cross-Sectional Comparison among Psychiatric Inpatients, Outpatients, and Healthy Adults. Nutrients. 2023; 15(9):2136. https://doi.org/10.3390/nu15092136
Chicago/Turabian StyleMötteli, Sonja, Barbora Provaznikova, Stefan Vetter, Matthias Jäger, Erich Seifritz, and Florian Hotzy. 2023. "Examining Nutrition Knowledge, Skills, and Eating Behaviours in People with Severe Mental Illness: A Cross-Sectional Comparison among Psychiatric Inpatients, Outpatients, and Healthy Adults" Nutrients 15, no. 9: 2136. https://doi.org/10.3390/nu15092136
APA StyleMötteli, S., Provaznikova, B., Vetter, S., Jäger, M., Seifritz, E., & Hotzy, F. (2023). Examining Nutrition Knowledge, Skills, and Eating Behaviours in People with Severe Mental Illness: A Cross-Sectional Comparison among Psychiatric Inpatients, Outpatients, and Healthy Adults. Nutrients, 15(9), 2136. https://doi.org/10.3390/nu15092136






